Abstract
Globally, liver cancer is the sixth most common cause of cancer mortality, with hepatocellular carcinoma (HCC) being the most common type of primary liver cancer. Emerging evidence states that diet is recognised as a potential lifestyle-related risk factor for the development of HCC. The aim of this systematic review is to determine whether there is an association between diet and the development of HCC. Using the PRISMA guidelines, three databases (MEDLINE Complete, CINAHL and Embase) were systematically searched, and studies published until July 2020 were included. Thirty observational studies were selected. The protocol was registered with PROSPERO (CRD42019135240). Higher adherence to the Mediterranean dietary pattern, Alternative Healthy Eating Index-2010, the Urban Prudent Dietary Pattern, the Traditional Cantonese Dietary Pattern, intake of vegetables, wholegrains, fish, poultry, coffee, macronutrients such as monounsaturated fats and micronutrients such as vitamin E, vitamin B9, β-carotene, manganese and potassium were associated with a reduced risk of HCC. The results suggest a potential role of diet in the development of HCC. Further quantitative research needs to be undertaken within a range of populations to investigate diet and the relationship with HCC risk.
1. Introduction
Liver cancer is the seventh leading cause of cancer-related mortality in Australia, and the incidence continues to increase [1,2,3]. Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer (PLC), accounting for approximately 90% of all cases [4,5,6]. HCC most commonly occurs in patients with liver cirrhosis [7,8] particularly in the setting of chronic hepatitis B virus (HBV) and hepatitis C virus (HCV) infections, dietary aflatoxin exposure, excessive alcohol consumption, tobacco smoking, and metabolic-associated fatty liver disease (MAFLD) [1,9]. Liver cirrhosis confers a very high risk of developing HCC, with between 5% and 30% of cirrhotic patients being diagnosed with HCC within the first five years [4]. Other identified risk factors for HCC include obesity, diabetes and MAFLD [10]. Diet has been recognised as a potential lifestyle-related risk factor for the development of HCC [11,12,13,14,15,16]. A healthy diet may play a preventative role in the development of some cancers, while a poor diet has been shown to increase cancer risk [11,14]. However, there is no clear consensus of what a protective diet is composed of for HCC risk [11].
Epidemiological evidence on the association of fruit and vegetable intake with gastrointestinal cancers suggests a protective role of a plant-based diet [11,12] Similarly, a positive association between increased processed meat consumption and breast cancer has been described [13]. However, little research has investigated the effect of diet on the development of HCC. The research that does exist is inconsistent and focuses on specific nutrients rather than food groups or dietary patterns. Thus, we identified the importance of focusing on dietary food groups (including macro- and micronutrients) and patterns in HCC prevention. Several reviews in the past have attempted to elucidate the potential association between nutrition and HCC [2,17,18,19]. However, there are no recent and or systematic literature reviews using the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines performed to date. Thus, the aim of the present systematic review is to determine whether there is an association between diet and dietary patterns, and the development of HCC.
2. Materials and Methods
2.1. Search Terms and Strategy
In accordance with the PRISMA guidelines, a systematic search of MEDLINE Complete, CINAHL and EMBASE databases was conducted to source articles published from inception to July 2020. The protocol was registered with PROSPERO (International Prospective Register of Systematic Reviews), registration number CRD42019135240, prior to commencement. The research question was structured in accordance with the PICOS (Population, Intervention, Comparator, Outcome and Study Design) criteria (Table 1). The initial database searches were conducted by AB, GC and SS. Search terms used for the study selection were ‘diet*’ OR ‘diet* pattern*’ OR ‘diet* intervention’ OR ‘nutrient*’ OR ‘diet* intake’ OR ‘nutrition’ OR ‘calorie restrict*’ OR ‘hypercaloric’ OR ‘food*’ AND ‘hepatocellular carcinoma’ OR ‘HCC’ OR ‘liver cancer’ OR ‘liver tumo*’ OR ‘hepatoma’.

Table 1.
PICOS criteria for inclusion and exclusion of studies.
2.2. Eligibility Criteria
Studies were included if they were written in the English language, included HCC as an outcome (either HCC prevalence at baseline or assessed risk at the conclusion of the study) and had a primary focus on associations between diet and HCC. Observational studies were included to determine dietary intake and the risk of HCC development. Articles were excluded if they were: not human studies, abstract only, review articles, focused on specific compounds such as aflatoxin or supplements rather than overall dietary patterns or food groups, focused on other mediating variables such as serum biomarkers, investigated other liver diseases such as MAFLD and cirrhosis or investigated broader lifestyle patterns such as physical activity or weight management and did not report on specific dietary patterns or components.
2.3. Study Selection Process
Abstract and title screening was conducted for all articles found in the initial search, and duplicates and articles which did not meet the eligibility criteria were excluded. Full-text screening was conducted by two independent reviewers. Conflicts were resolved through consensus. All articles accepted from the full-text screen were included in the systematic review. All inclusions are outlined in the PRISMA flowchart in Figure 1.
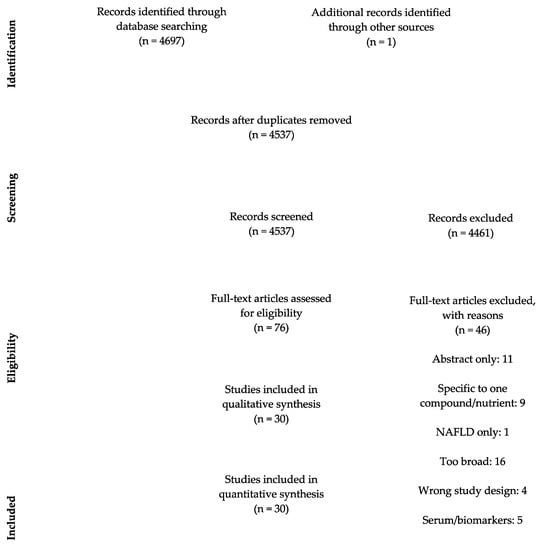
Figure 1.
PRISMA flowchart of study selection process. NAFLD: Non-alcoholic fatty liver disease.
2.4. Data Extraction
The information extracted from 30 studies included the following: setting, duration, study design, population characteristics (age, sex, BMI, comorbidities), dietary patterns assessed in the study, dietary data assessment methods and outcomes.
2.5. Quality Assessment and Risk of Bias
The Academy of Nutrition and Dietetics Evidence Analysis Library Quality Criteria Checklist was used to assess overall quality and risk of bias. The questions are shown in Table 2. The risk of bias was conducted in duplicate independently for each study. Key questions assessed the studies overall relevance and validity. More specifically, these included whether the selection of participants was free from bias, whether groups were comparable, whether method of handling withdrawals/dropouts was described, whether blinding was used to prevent bias, whether interventions were described in detail with outcomes clearly defined, whether the statistical analysis was appropriate, whether conclusions were supported by results and whether funding and sponsorship may have introduced additional bias. A positive score was given to a study if it was rated yes for the majority of the above questions. Disagreements within the assessments were resolved through consensus.

Table 2.
Risk of bias questions.
2.6. Data Analysis
Qualitative and quantitative analyses were carried out. For qualitative analysis, we assessed and reported differences in dietary patterns or foods studied and populations characteristics such as ethnicities or geographical areas. For quantitative analysis, statistical measures, including the use of multi-variate controls, dietary intake categorisation, confidence intervals and hazard ratios were assessed along with overall findings of each study. These were then compared with other studies’ findings and grouped in order to analyse the number of consistent or inconsistent findings across studies. Data were considered statistically significant if the reported p-value was <0.05. A meta-analysis was not carried out for studies in this review.
3. Results
3.1. Study Selection
The literature search process is shown in Figure 1. The initial search resulted in 4698 articles, of which 4461 articles did not fit the inclusion criteria. Seventy-six studies were eligible for full text screening and 46 of these were excluded for the following reasons: abstract only (n = 11), included only one nutrient (n = 9), wrong article type or study design (n = 4), too broad such as studying overall lifestyle habits rather than a focus on diet (n = 16), looking at MAFLD not HCC (n = 1) and looking at serum/biomarkers (n = 5). There were 30 observational studies included in the systematic review [4,7,10,14,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
3.2. Study Characteristics
The data extracted from the included 30 articles are presented in Table 3. All studies were observational and of these: seventeen were cohort, [20,21,22,27,28,29,30,31,32,34,35,38,41,42,43,44,45]; seven were case–control, [4,14,23,33,37,39,40] and six were cohort with nested case–control subset [7,10,24,25,26,36]. In total the 30 studies included 5,222,534 participants aged between 25–85 years across 22 countries including Asian, American and European populations. There were differences according to geographical regions and dietary patterns and components within this review. In particular, the MED pattern indicated protective effects amongst European and American populations [14,30,32]. The Chinese Healthy Eating Index and the Cantonese Dietary Pattern in Asian countries where they are habitually consumed were associated with lower HCC prevalence [23,39]. High-fat dairy products such as butter were associated with HCC prevalence within the American population [25,44] whereas no associations with dairy consumption were observed in the European population [37]. Asian countries such as Japan, who are amongst the highest consumers of soy food [7], indicated lower rates of HCC with increased soy and tofu intake [7]. There appeared to be no differences in food groups including red meat, white meat and fish, vegetables, fruits and coffee intake based on geography. The study periods ranged from 2 to 32 years. The study follow-up period ranged from 4 to 32 years. Four out of 30 studies did not report follow-up periods [23,37,39,40]. Twenty-three out of thirty studies specified HCC as the main type of PLC [4,7,14,20,21,22,24,25,26,27,28,29,30,31,32,33,35,36,37,38,40,43,44] and of remaining seven studies, five reported >85% of participants with HCC [10,23,34,39,42]. The remaining two studies referred generally to PLC [41,45]; however, given the known rates it is likely the majority comprised of HCC cases. The articles were published between 2000 and 2020. Figure 2 summarises the dietary patterns, food groups and nutrients and their associated risk with HCC based on this review.

Table 3.
Summary of studies (n = 30) evaluating the association between diet and hepatocellular carcinoma risk.
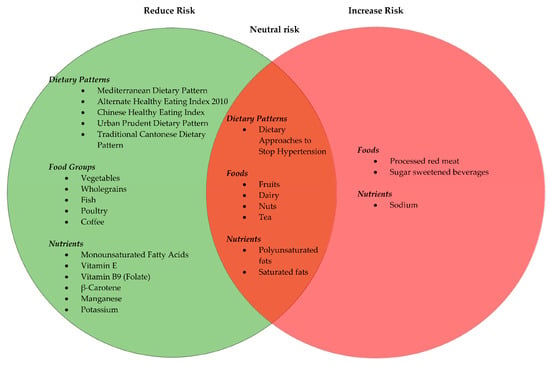
Figure 2.
A summary of dietary patterns, food groups and nutrients and the associated risk with hepatocellular carcinoma based on observational studies included in this systematic review.
3.3. Dietary Guidelines and Dietary Patterns
Six studies assessed and identified that there was a relationship between a priori dietary patterns as determined by dietary indices and the risk of HCC [14,22,23,30,32,39]. From this group, two studies were conducted in South China [23,39], one in North-Eastern Italy and Athens, Greece [14], and three in the United States [22,30,32], with a total participant count of 842,270. Adherence to the Mediterranean dietary pattern is reported to be protective against HCC in several studies [14,22,30,32]. A statistically significant association was found between the Mediterranean score and incidence of HCC, with a score of greater than or equal to five (scored out of nine) demonstrating a significant reduction in the risk of HCC when compared with Mediterranean score less than or equal to three (ORs = 0.51, 95% CI: 0.34–0.75, p < 0.001) [27] and (HR = 0.62; 95% CI: 0.47–0.84; P trend = 0.0002) [30]. Additionally, the Alternate Mediterranean Diet (aMED) score was associated with a non-significant lower risk of HCC (HR = 0.75; 95% CI, 0.49–1.15; P trend = 0.18) [32]. The aMED score is an adaption of the original Mediterranean diet score, based on the intake of 9 items including vegetables, legumes, fruit and nuts, dairy, cereals, meat and meat products, fish, alcohol and monounsaturated to saturated fatty acid ratio [46]. The aMED score also includes nine components, excluding potato products, separating fruits and nuts into two groups, removes the dairy group, includes whole-grains products, red and processed meats and assigns alcohol intake. The aMED also takes into consideration the chronic disease risk [46,47]. The Chinese Healthy Eating Index and the Healthy Eating Index-2015 (HEI-2015) are designed to assess adherence to the 2016 Dietary Guidelines for the Chinese population and the 2015–2020 Dietary Guidelines for the USA population, respectively, with higher scores (0–100) indicating better adherence to the guidelines. Higher adherence to Chinese or American Dietary Guidelines was significantly associated with lower risk of HCC (p < 0.001) [23] and (p = 0.03) [30]. The Alternative Healthy Eating Index-2010 (AHEI-2010) is based on the original HEI and includes additional dietary components that predict chronic disease risk, with higher scores (0 to 110 points) associated with lower risk of incident HCC. Greater adherence to the AHEI-2010 was significantly associated with a reduced risk (HR = 0.61, 95% CI: 0.39–0.95, P trend = 0.03) [32]. Similarly, the Urban Prudent Dietary Pattern and the Traditional Cantonese Dietary Pattern were associated with significantly decreased risk of HCC (p < 0.002), while the High Meat and Preserved Food Pattern was associated with increased HCC risk (p < 0.001). Additionally, a null association was reported between Dietary Approaches to Stop Hypertension Diet and HCC risk (HR = 0.90, 95% CI: 0.59–1.36, p = 0.61) [32].
3.3.1. Vegetables and Fruits
High consumption of vegetables with a 100 g/day increment in intake [20] or more than 3–4+ vegetables per week [38] has shown a non-significant trend to reduced risk of HCC [20,38,45]. However, no associations were seen with fruit consumption [20,37,43,45]. A specific subgroup of vegetables including celery (p = 0.03), mushrooms (p = 0.03), allium vegetables (Chinese chives, onions, garlic, garlic shoots) (p < 0.01), composite vegetables (asparagus-lettuce, garland chrysanthemum) (p < 0.01), legumes and legume products (p = 0.04), squash and carrots, had a significant inverse association, indicating protective effects against HCC [45]. Potato intake was associated with reduced HCC mortality in women, whereas frequent intake of potatoes cooked in soy sauce increased HCC mortality in men [38].
3.3.2. Red Meat, White Meat and Fish
Processed meat and red meat intake were associated with an increased risk of HCC [4,31]. A positive association was found between processed red meat and HCC risk, where higher contribution to total calorie intake from processed red meat (comparing highest to lowest tertile intake) indicated significant findings, reporting an 84% increased HCC risk (HR = 1.84, 95% CI: 1.16–2.92, p = 0.04) [31].
Conversely, higher intake (3.5 servings/week) of white meat demonstrated a 39% lower risk of HCC (comparing highest to lowest tertile intake, HR = 0.61, 95% CI: 0.40–0.91, p = 0.02) [31] and a protective association (HR = 0.52, 95% CI: 0.36–0.77) with HCC incidence [27]. USA cohort studies, the Nurses’ Health Study (NHS) and Health Professionals Follow-up Study (HPFS) further examined the type of white meat (i.e., poultry) intake, reporting a significantly protective association (HR = 0.60, 95% CI: 0.40–0.90, p = 0.01) with HCC [31]. However, some studies did not report any association [26,31]. Greater consumption of fish was associated with reduced risk of HCC [26,31]. Each daily 20 g of fish consumption correlated with a reduction in HCC development (HR = 0.80, 95% CI: 0.69–0.97). [26] The European Prospective Investigation into Cancer and Nutrition (EPIC) and, NHS and HPFS studies reported that substituting 20 g/day in place of fish for meat resulted in a 16% decrease in HCC risk [26], and substitution of poultry or fish for processed red meat was associated with a decrease in risk of HCC (HR = 0.79, 95% CI:0.61–1.02) [31].
3.3.3. Dairy and Soy
Two large cohort studies, one conducted in the USA and the other using data from EPIC and NHS, and HPFS showed that higher total dairy product intake was associated with a statistically significant higher risk of HCC [25,44]. However, the association differed by the type of dairy products consumed [30]. Higher intake of dairy products (>381.7 g/day) showed increased HCC risk in the EPIC study (highest vs. lowest tertile, HR = 1.66, 95% CI: 1.13–2.43, P trend = 0.012) [25], and NHS and HPFS study (HR = 1.85, 95% CI: 1.19–2.88; p = 0.009) [44]. Additionally, significant positive HCC risk association was observed for high-fat dairy (p = 0.008), butter (p = 0.04) and milk (P trend = 0.049) [25,44]. Intake of yoghurt showed a trend to lower HCC risk [44] and indicated no association in another study [25]. This discrepancy may be attributed to the differences in the content of insulin-like growth factor (IGF-1) and aflatoxin in milk, cheese and yoghurt. Although the European Food Safety Authority reports low aflatoxin M1 levels in milk samples; due to the high consumption of milk in Europe, the daily ingestion of aflatoxin M1 remains significant [25]. Conversely, no significant associations were found between dairy consumption and HCC risk based on the results of two case–control studies [4,37]. Increased intake of soy foods was found to reduce risk of HCC in a cohort-based, nested case–control study conducted within the Japanese population [7]. Intake of miso soup (>17.1 g/day) or tofu (>76.3 g/day) more than 5 times/week was associated with 50% lower HCC risk, when compared to less than once a week [7]. This reduction in crude HCC risk was 0.89 for miso soup and 0.92 for tofu, per additional serving [7]. Increased intake of dairy products, particularly high fat, appears to be associated with increased risk of HCC. However, there is much heterogeneity in types and quantity of consumption thus, further studies are warranted.
3.3.4. Wholegrains
Wholegrain intake is associated with decreased HCC risk (highest versus lowest tertile: HR = 0.63, 95% CI: 0.41–0.96, p = 0.04) with daily intake range of 17.86–33.28 g/day [4,43]. Surprisingly, a significant positive association was found between cereal intake and HCC risk (highest versus lowest tertile OR = 1.87, 95% CI: 1.09–3.22, p = 0.035) in the CiRCE study [4]. The dietary glycemic index, glycemic load, and carbohydrate intake did not find any association with HCC in a Chinese population [42].
3.3.5. Nuts
In two large USA prospective cohorts, NHS and HPFS, higher total nut (HR = 0.84, 95% CI, 0.56–1.26), walnuts (p = 0.19) and peanuts (p = 0.90) consumption was not strongly associated with HCC risk [35]. Whereas, an increased intake (mean 1.25 serving per week) of tree nuts (including hazelnuts, almonds, macadamias, pecans, cashews and pistachios) reported a suggestive association with lower HCC risk (HR = 0.64, 95% CI: 0.43–0.95) [35]. Overall, nut consumption did not indicate a strong association with HCC risk.
3.3.6. Beverages
Coffee
Coffee consumption has been shown by a number of studies to be associated with reduced risk of HCC incidence [21,28,29,34,38,41]. The Takayama Study revealed that coffee intake twice per day or more had a significantly lower risk of HCC when compared with non-drinkers (HR = 0.4, 95% CI: 0.20–0.79, p = 0.03) [41]. Daily coffee drinkers had a 51% lower HCC risk than those who abstained (HR = 0.49, 95% CI: 0.36–0.66, p < 0.001) [28], and a dose response was shown with those consuming greater than two cups/day having a statistically significant reduction in risk of HCC (p = 0.49) [34]. Consumption of decaffeinated coffee showed no significant association with HCC risk [41].
Tea
The MEC study demonstrated that increased tea intake (>475.1 mL/day for females, >480 mL/day for males) was associated with lower HCC risk (HR = 0.41, 95% CI: 0.22–0.78, p = 0.003) [21]. Other studies investigated in this review did not report any association between tea and the risk of HCC [29,38,40,41].
Sugar-Sweetened Beverages
A positive association between HCC risk and carbonated/soft drink beverages was seen in large Asian and European cohorts (OR = 2.44, 95% CI: 1.17–5.09, p = 0.021) [4]. Compared to non-consumers, consumption of >6 servings/week (6 × 330 mL can) of soft drinks was significantly associated with higher HCC risk (HR = 1.83, 95%CI: 1.11–3.02, p = 0.01) [10]. Consumption of juice less than 200 mL glass a week was associated with lower HCC risk (HR = 0.60, 95% CI: 0.38–0.95, p = 0.02) when compared to non-consumers [10].
Alcohol
Alcohol was reported as a major risk factor for HCC. However, many studies failed to show a significant positive association with HCC risk [4,7,10,14,20,21,22,23,24,25,26,27,28,29,33,34,36,37,38,39,40,41,42,43,45]. This was because the relationship between alcohol consumption and HCC is difficult to interpret, as the risk often depends on the quantity and duration of alcohol consumption along with other factors such as age, gender, presence of viral hepatitis, cirrhosis and metabolic syndrome [4]. In the methodology of most studies, alcohol was reported as a potential confounding factor and was adjusted.
3.3.7. Macronutrients
Fats
Monounsaturated fats are associated with reduced HCC risk, as shown in a large prospective European cohort (HR = 0.71, 95% CI: 0.55–0.92) with intake range from 22.05 to 43.35 g/day, and a similar study in Greece (OR = 0.47, 95% CI: 0.25–0.87) [24,37]. Saturated fat in red meat increased the risk of HCC (HR = 1.87, 95% CI: 1.23–2.85); suggesting that the association with red meat may be as a result of saturated fat [27]. On the contrary, no direct association of HCC risk with saturated fat intake was shown in case-control study from Italy [36]. A strong protective association was identified between HCC risk and polyunsaturated fatty acids (OR = 0.48, 95% CI: 0.24–0.94) with the effect postulated to be due to linoleic acid (OR = 0.35, 95% CI: 0.18–0.69, p < 0.01) [33]. Omega-6 PUFA intake demonstrated a significant dose-dependent, positive association with HCC risk in Singaporean Chinese (HR = 1.49, 95% CI: 1.08–2.07, p = 0.02) and omega-3 PUFA conferred no association [36]. Overall, the data suggest that monounsaturated and polyunsaturated fatty acids were associated with reduced HCC risk in comparison to saturated fats, which displayed no impact or positive HCC risk associations.
3.3.8. Micronutrients
Vitamin E (p = 0.017), vitamin B9 (folate) (p = 0.036), β-carotene (p = 0.03), manganese (p = 0.038) and potassium (p = 0.004) in the diet have shown a significant negative correlation with HCC risk [4,38]. Sodium intake was significantly associated with an increased HCC risk (p = 0.043) [4]. Dietary iron (mean: 13.9 mg/day) intake was associated with increased HCC risk (p = 0.01); however, the association was weakened when contribution of wine was excluded [33]. Thus, it may be difficult to come to a conclusion due to confounding factors such as wine and red meat intake.
3.4. Risk of Bias
The risk of bias of the included observational studies was assessed by The Academy of Nutrition and Dietetics Evidence Analysis Library (EAL) Quality Criteria Checklist and is outlined in Table 4. The Quality Criteria Checklist: Primary Research has ten validity questions based on the Agency for Healthcare Research and Quality domains for research studies. Studies can score a positive (+) which indicates that the report has addressed issues of inclusion/exclusion, bias, generalisability, and data collection and analysis, negative (−) which indicates issues were not addressed adequately, or neutral [48] which indicates that the study is neither strong nor weak. Overall, the included studies were considered to be at low risk of bias as they showed a positive quality rating.

Table 4.
Critical appraisal of the 30 studies with the use of the Quality Criteria Checklist.
4. Discussion
To our knowledge, this is the first robust and most up-to-date systematic review following the PRISMA guidelines, evaluating the association between diet and dietary patterns and HCC risk. The results show that diet plays an important role in HCC occurrence. Consumption of dietary patterns such as the MED pattern, the AHEI-2010, the Urban Prudent Dietary Pattern and the Traditional Cantonese Dietary Pattern, foods such as vegetables, poultry, fish, wholegrains, and coffee, and micronutrients such as vitamin E, vitamin B9, β-carotene, manganese and potassium may have a potential benefit in reducing the development of HCC. Some fats, including monounsaturated fats, may also have beneficial effects. Additionally, it can be inferred that sugar-sweetened beverages including soft drinks/carbonated beverages and processed red meat consumption may increase HCC risk. Whilst some dietary patterns including the DASH diet and foods such as nuts (e.g., walnuts and peanuts) indicate a null association.
Some of the important risk factors for HCC have been modified over the last decade, including the treatment of chronic hepatitis B and hepatitis C viruses with direct acting antiviral agents, and it is expected that the rate of HCC related to these factors will decrease. However, increasingly HCC is related to obesity and fatty liver, and with the current obesity epidemic the incidence is not likely to improve. It is possible that the changes in diet and dietary patterns that are related to the increase in obesity may also be having a direct effect on HCC pathogenesis. Some of these mechanisms were included in studies such as the reduction in HCC risk with intake of yellow vegetables in patients with hepatitis B (HBV) or hepatitis C (HCV) infection [49]. The carotenoids, in particular β-carotene, have been shown to neutralise free radicals in the liver tissue, thus decreasing carcinogenesis in patients with hepatitis and preventing the progression of HBV and HCV related HCC [49,50].
Fruit and vegetable intake are associated with a lower incidence of conditions such as obesity, diabetes and other cancers [20,33,51,52]. Surprisingly, our review found no consistent relationship between fruit intake and HCC. This may be as a result of the observational study designs and different methods used to obtain dietary information.
Meat intake is affected by important confounders, such as gender, body mass, smoking and HBV and HCV status [53]. Red meat has high amounts of carcinogens, including haem iron, which in excess induces fibrosis and cirrhosis [33,54]. Red meat also has high cholesterol and saturated fat content, related to known cancer risk factors such as obesity, diabetes and metabolic syndrome. In addition to this, processing and preservation of meat forms potential carcinogenic chemicals such as N-nitroso compounds [53]. By contrast, fish and poultry are lower in saturated fat and cholesterol and are higher in polyunsaturated fatty acids, which inhibit tumour-necrosis factor and inflammation; playing a protective role in hepatocarcinogenesis [53,55].
Omega-6 polyunsaturated fatty acids may increase HCC risk by their association with individuals who are overweight, obese and/ or have diabetes [36]. Additionally, the metabolism of omega-6 polyunsaturated fatty acid produces pro-inflammatory products including lipid mediators and indirectly C-reactive protein; which have been implicated in causing fibrosis in MAFLD, subsequently cirrhosis and ultimately HCC [24,27,55]. Another consideration is that the sources of monounsaturated fats in the United States are generally from meat and/or meat products compared to Europe where the main sources are oils and added fats [56,57].
Dairy consumption has been associated with several cancers such as gastric cancer [19]. This may at least be part attributable to the presence of saturated fat, IGF-1 and other contaminants [58]. Potential carcinogenic contaminants include bracken fern, which is added to feedstuff and passed into milk [58]. Calcium and vitamin D found in dairy products may also increase the circulation of IGF-1, which plays an important role in cell proliferation and carcinogenesis [25], leading to the development of breast cancer [59]. Future studies are recommended in experimental and prospective settings.
In the Japanese population, weekly consumption of phytoestrogen, isoflavone, present in large amounts in miso and tofu revealed a 50% reduction in HCC risk [7]. Isoflavone is believed to interact with estrogen, inhibiting its effect on cell proliferation and inducing apoptosis [7]. Miso and tofu consumption in a Japanese population was quantified, but did not include tofu included in mixed meals or natto, another soy product consumed in the common Japanese diet, resulting in possible underestimation of the effects of tofu [7]. Given the large popularity of fermented soy products in Japanese culture, the difference observed between the quartiles in this study were small, warranting further research in non-Japanese populations.
The varying results on wholegrain consumption can be attributed to the different sample sizes, demographics, and cultural differences between American and European populations [4,43]. Moreover, the different study designs (i.e., case control versus cohort) and the dietary assessment methods may also be a possible explanation for the unexpected results. Nuts are nutrient-dense foods rich in unsaturated fats, vegetable protein, vitamins, folate, fiber, and minerals [35]. Although studies do not support a strong association with higher nut (e.g., walnuts and peanuts) consumption and reduced HCC risk, it is plausible that higher intake might influence HCC risk through mechanisms related to insulin resistance and inflammation [35,60]. Nuts are associated with lower risk of type II diabetes, a risk factor for HCC [61].
High carbohydrate intake leads to a high circulation of endogenous insulin, and thus insulin influencing IGF-1, a known carcinogen [62]. However, it remains unclear whether carbohydrates affect the risk of developing HCC specifically. Sugar-sweetened beverages, juices, and soft drinks consumption are associated with overall cancers including HCC [63]. This may be explained by the effect of sugary drinks on weight gain and obesity [63], but also hyperinsulinaemia and type 2 diabetes, thus increasing the risk of diabetes-related carcinomas (liver, pancreas, breast) [63]. The high glucose and fructose cause a rapid increase in insulin levels and accelerate the formation of fat in the liver [64]. It is also likely that people who consume high levels of sugar-sweetened beverages have poorer diet quality [10].
Coffee constituents such as chlorogenic acid may account for the hepato-protective effects of coffee with HCC [48]. It also contains antioxidants and phenolic compounds which have anticarcinogenic properties [65].
The Mediterranean diet has been shown to have benefits in health, longevity and decreased mortality. The diet exerts anti-inflammatory effects as it is lower in saturated fat, refined sugar and dairy, and higher in unsaturated fatty acids, fruits and vegetables, wholegrains and fish [65,66,67]. Foods consumed in the Chinese culture are associated with a lower HCC risk which may be due to the higher consumption of soy products, seafood, traditional soups and herbal teas, possibly via the increased antioxidants in these foods [23,39].
This systematic review had several notable strengths, with an overall positive risk of bias assessment score (Table 4). Data were synthesized from twenty-one different countries across Europe, Asia and North America, enrolling a large sample size of participants. Additionally, twenty-six out of 30 studies used a validated tool to collect and assess dietary information, including food frequency questionnaires, diet history questionnaires, country-specific questionnaires and centre-specific questionnaires. The limitations arise from using observational studies, predominantly cohort and case–control design; and that the food frequency questionnaires were conducted at a single point in time to assess long-term usual diet. Another limitation stems from the lack of evidence available from prospective studies, where more high-quality studies including generalisable populations assessing the association between HCC risk and diet and dietary pattern over time are required to affirm the findings from this review. Additionally, dietary studies are complicated by virtue and it remains challenging for researchers to interpret diet holistically. For example, consumption of one food is perceived to lead to adverse health outcomes, such as processed meat; however, it is hard to understand whether this was a result of an overall poor diet or the role of processed meat itself. The complex interconnections between foods, nutrients and dietary patterns imply that no individual element can provide a complete picture on nutrition and thus health status. The whole diet approach i.e., dietary patterns, which incorporates a combination of food groups, have been demonstrated to be beneficial and in fact more robust compared to assessment of individual nutrients. The reason for this being, that dietary patterns represent how foods are consumed, which is not in isolation as individual nutrients, rather as whole foods in meals and as such dietary patterns better account for the synergistic effect of the food matrix [68,69,70]. However, there were only a few studies included within this systematic review that assessed dietary patterns.
5. Conclusions
Current epidemiological evidence supports that diet and dietary patterns are relevant factors related to the risk of HCC. Certain dietary patterns including the Mediterranean diet, the Alternative Healthy Eating Index-2010, the Urban Prudent Dietary Pattern, the Traditional Cantonese Dietary Pattern, foods including vegetables, wholegrains, fish, poultry, coffee, macronutrients including monounsaturated fatty acids, and micronutrients including vitamin E, vitamin B9, β-carotene, manganese and potassium may lead to reduced risk of HCC. This provides a basis for determining what types of dietary interventions may reduce the development of HCC. However, what the benefits are to high-risk individuals such as those who already have HBV or cirrhosis remains unknown. Future prospective studies should be well-designed and include large and diverse geographical regions including participants with differing socioeconomic status-, ethnic-, race-based populations. Heterogeneity between high-risk populations (e.g., high-risk family cohorts, patients with cirrhosis) should be included and characterized, as should family history, genetics, and other modifiable lifestyle factors (e.g., physical activity) to ensure data account for high-risk groups and are more widely representative and generalisable. Future studies may also consider examining diets holistically through assessment into dietary patterns. Healthier dietary patterns may reduce the prevalence of HCC risk based on the findings from this study, albeit the current literature is limited. Additionally, studies should consider investigating key dietary patterns (including traditional dietary patterns) such as the MED, the AHEI-2010, the Cantonese Dietary Pattern and DASH as shown by Lan et al. 2018 [39] and Ma et al. 2019 [32]. It appears, based on our assessment of dietary patterns into geographical regions, that selecting a pattern that best reflects the traditional, habitual dietary intake of a given population is most appropriate. Researchers may consider expanding to other dietary patterns as applicable, which are shown to be protective for disease prevention, but not yet HCC such as vegetarian/vegan, plant-based diets and Nordic dietary patterns may also be worth exploring to elucidate HCC risk. As components of all lifestyle behaviours are integrated, designing studies that correlate all aspects of a healthy diet are recommended.
Author Contributions
E.S.G. conceptualized this study and was involved in design, drafting and critical review. E.S.G., S.S. (Surbhi Sood), A.B., G.C., M.H., W.S.C., and S.S. (Sonal Sudan) conducted the review, data extraction, risk of bias and drafted this study. A.J.N. drafted and critically reviewed this study. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Not applicable as this was a review.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| HBV | hepatitis B virus |
| HCV | hepatitis C virus |
| HCC | hepatocellular carcinoma |
| IGF-1 | insulin-like growth factor |
| MAFLD | metabolic-associated fatty liver disease |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analysis |
| PLC | primary liver cancer |
| PUFA | polyunsaturated fatty acids |
References
- Rowe, J.H.; Ghouri, Y.A.; Mian, I. Review of hepatocellular carcinoma: Epidemiology, etiology, and carcinogenesis. J. Carcinog. 2017, 16, 1. [Google Scholar] [CrossRef] [PubMed]
- Koumbi, L. Dietary factors can protect against liver cancer development. World J. Hepatol. 2017, 9, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare, Commonwealth of Australia. Liver Cancer Statistics Canberra. 2019. Available online: https://liver-cancer.canceraustralia.gov.au/statistics (accessed on 19 April 2019).
- Rizk, M.; Guilloteau, A.; Mouillot, T.; Thiéfin, G.; Bronowicki, J.-P.; Richou, C.; Doffoel, M.; Assaf, M.D.; Hillon, P.; Cottet, V. Dietary components modulate the risk of hepatocellular carcinoma in cirrhotic patients. Nutr. Res. 2019, 61, 82–94. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.; Torre, L.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Torre, L.; Bray, F.; Siegel, R.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef]
- Sharp, G.B.; Lagarde, F.; Mizuno, T.; Sauvaget, C.; Fukuhara, T.; Allen, N.; Suzuki, G.; Tokuoka, S. Relationship of hepatocellular carcinoma to soya food consumption: A cohort-based, case-control study in Japan. Int. J. Cancer 2005, 115, 290–295. [Google Scholar] [CrossRef]
- McGlynn, K.; Petrick, J.; London, W. Global epidemiology of hepatocellular carcinoma: An emphasis on demo-graphic and regional variability. Clin. Liver Dis. 2015, 19, 223–238. [Google Scholar] [CrossRef]
- Donato, F.; Boffetta, P.; Puoti, M. A meta-analysis of epidemiological studies on the combined effect of hepatitis B and C virus infections in causing hepatocellular carcinoma. Int. J. Cancer 1998, 75, 347–354. [Google Scholar] [CrossRef]
- Stepien, M.; Duarte-Salles, T.; Fedirko, V.; Trichopoulou, A.; Lagiou, P.; Bamia, C.; Overvad, K.; Tjønneland, A.; Hansen, L.; Boutron-Ruault, M.-C.; et al. Consumption of soft drinks and juices and risk of liver and biliary tract cancers in a European cohort. Eur. J. Nutr. 2016, 55, 7–20. [Google Scholar] [CrossRef]
- Key, T.J.; Schatzkin, A.; Willett, W.C.; Allen, N.E.; Spencer, E.A.; Travis, R.C. Diet, nutrition and the prevention of cancer. Public Health Nutr. 2004, 7, 187–200. [Google Scholar] [CrossRef]
- Vogtmann, E.; Xiang, Y.-B.; Li, H.-L.; Levitan, E.; Yang, G.; Waterbor, J.; Gao, J.; Cai, H.; Xie, L.; Wu, Q.-J.; et al. Fruit and vegetable intake and the risk of colorectal cancer: Results from the Shanghai Men’s Health Study. Cancer Causes Control 2013, 24, 1935–1945. [Google Scholar] [CrossRef] [PubMed]
- Farvid, M.S.; Stern, M.C.; Norat, T.; Sasazuki, S.; Vineis, P.; Weijenberg, M.P.; Wolk, A.; Wu, K.; Stewart, B.W.; Cho, E. Consumption of red and processed meat and breast cancer incidence: A systematic review and meta-analysis of prospective studies. Int. J. Cancer 2018, 143, 2787–2799. [Google Scholar] [CrossRef] [PubMed]
- Turati, F.; Trichopoulos, D.; Polesel, J.; Bravi, F.; Rossi, M.; Talamini, R.; Franceschi, S.; Montella, M.; Trichopoulou, A.; La Vecchia, C.; et al. Mediterranean diet and hepatocellular carcinoma. J. Hepatol. 2014, 60, 606–611. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, H.; Bording-Jorgensen, M.; Dijk, S.; Wine, E. The complex interplay between chronic inflammation, the microbiome, and cancer: Understanding disease progression and what we can do to prevent it. Cancers 2018, 10, 83. [Google Scholar] [CrossRef]
- Montella, M.; Crispo, A.; Giudice, A. HCC, diet and metabolic factors: Diet and HCC. Hepat. Mon. 2011, 11, 159. [Google Scholar]
- Mandair, D.S.; Rossi, R.E.; Pericleous, M.; Whyand, T.; Caplin, M. The impact of diet and nutrition in the preven-tion and progression of hepatocellular carcinoma. Expert Rev. Gastroenterol. Hepatol. 2014, 8, 369–382. [Google Scholar] [CrossRef]
- Schutte, K.K.; Schulz, C.; Malfertheiner, P. Nutrition and Hepatocellular Cancer. Gastrointest. Tumors 2016, 2, 188–194. [Google Scholar] [CrossRef]
- Yang, W.; Zeng, X.; Liu, Z.; Zhao, Q.; Tan, Y.; Gao, J.; Li, H.-L.; Xiang, Y.-B. Diet and liver cancer risk: A narrative review of epidemio-logical evidence. Br. J. Nutr. 2020, 124, 330–340. [Google Scholar] [CrossRef]
- Bamia, C.; Lagiou, P.; Jenab, M.; Aleksandrova, K.; Fedirko, V.; Trichopoulos, D.; Overvad, K.; Tjønneland, A.; Olsen, A.; Clavel-Chapelon, F.; et al. Fruit and vegetable consumption in relation to hepatocellular carcinoma in a multi-centre, European cohort study. Br. J. Cancer 2015, 112, 1273–1282. [Google Scholar] [CrossRef]
- Bamia, C.; Lagiou, P.; Jenab, M.; Trichopoulou, A.; Fedirko, V.; Aleksandrova, K.; Pischon, T.; Overvad, K.; Olsen, A.; Tjønneland, A.; et al. Coffee, tea and decaffeinated coffee in relation to hepatocellular carcinoma in a European population: Multicentre, prospective cohort study. Int. J. Cancer 2015, 136, 1899–1908. [Google Scholar] [CrossRef]
- Bogumil, D.; Park, S.-Y.; Le Marchand, L.; Haiman, C.A.; Wilkens, L.R.; Boushey, C.J.; Setiawan, V.W. High-Quality Diets Are Associated with Reduced Risk of Hepatocellular Carcinoma and Chronic Liver Disease: The Multiethnic Cohort. Hepatol. Commun. 2019, 3, 437–447. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.-Y.; Zhang, D.-M.; Wang, X.-Y.; Lan, Q.-Y.; Liao, G.-C.; Liu, Z.-Y.; Zhang, D.-M.; Zhang, Y.; Chen, Y.-M.; Zhu, H.-L. Adherence to the Chinese or American Dietary Guidelines is associated with a Lower Risk of Primary Liver Cancer in China: A Case-Control Study. Nutrients 2018, 10, 1113. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Salles, T.; Fedirko, V.; Stepien, M.; Aleksandrova, K.; Bamia, C.; Lagiou, P.; Laursen, A.S.D.; Hansen, L.; Overvad, K.; Tjønneland, A.; et al. Dietary fat, fat subtypes and hepatocellular carcinoma in a large European cohort. Int. J. Cancer 2015, 137, 2715–2728. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Salles, T.; Fedirko, V.; Stepien, M.; Trichopoulou, A.; Bamia, C.; Lagiou, P.; Lukanova, A.; Trepo, E.; Overvad, K.; Tjønneland, A.; et al. Dairy products and risk of hepatocellular carcinoma: The European Prospective Investigation into Cancer and Nutrition. Int. J. Cancer 2014, 135, 1662–1672. [Google Scholar] [CrossRef]
- Fedirko, V.; Trichopolou, A.; Bamia, C.; Duarte-Salles, T.; Trepo, E.; Aleksandrova, K.; Nöthlings, U.; Lukanova, A.; Lagiou, P.; Boffetta, P.; et al. Consumption of fish and meats and risk of hepatocellular carcinoma: The European Prospective Investigation into Cancer and Nutrition (EPIC). Ann. Oncol. 2013, 24, 2166–2173. [Google Scholar] [CrossRef] [PubMed]
- Freedman, N.D.; Cross, A.J.; McGlynn, K.A.; Abnet, C.C.; Park, Y.; Hollenbeck, A.R.; Schatzkin, A.; Everhart, J.E.; Sinha, R. Association of Meat and Fat Intake with Liver Disease and Hepatocellular Carcinoma in the NIH-AARP Cohort. J. Natl. Cancer Inst. 2010, 102, 1354–1365. [Google Scholar] [CrossRef] [PubMed]
- Inoue, M.; Yoshimi, I.; Sobue, T.; Tsugane, S.; Group, J. Influence of coffee drinking on subsequent risk of hepatocel-lular carcinoma: A prospective study in Japan. J. Natl. Cancer Inst. 2005, 97, 293–300. [Google Scholar] [CrossRef]
- Johnson, S.; Koh, W.; Wang, R.; Govindarajan, S.; Yu, M.; Yuan, J. Coffee consumption and reduced risk of hepatocel-lular carcinoma: Findings from the Singapore Chinese Health Study. Cancer Causes Control 2011, 22, 503–510. [Google Scholar] [CrossRef]
- Li, W.; Park, Y.; McGlynn, K.; Hollenbeck, A.; Taylor, P.; Goldstein, A.M.; Freedman, N.D. Index-based dietary patterns and risk of incident hepa-tocellular carcinoma and mortality from chronic liver disease in a prospective study. Hepatology 2014, 60, 588–597. [Google Scholar] [CrossRef]
- Ma, Y.; Yang, W.; Li, T.; Liu, Y.; Simon, T.G.; Sui, J.; Wu, K.; Giovannucci, E.L.; Chan, A.T.; Zhang, X. Meat intake and risk of hepatocellular carcinoma in two large US prospective cohorts of women and men. Int. J. Epidemiol. 2019, 48, 1863–1871. [Google Scholar] [CrossRef]
- Ma, Y.; Yang, W.; Simon, T.; Smith-Warner, S.; Fung, T.; Sui, J. Dietary Patterns and Risk of Hepatocellular Car-cinoma Among U.S. Men Women Hepatol. 2019, 70, 577–586. [Google Scholar]
- Polesel, J.; Talamini, R.; Montella, M.; Maso, L.; Crovatto, M.; Parpinel, M.; Franceschi, S.; Izzo, F.; Tommasi, L.G.; Serraino, D.; et al. Nutrients intake and the risk of hepatocel-lular carcinoma in Italy. Eur. J. Cancer 2007, 43, 2381–2387. [Google Scholar] [CrossRef]
- Setiawan, V.; Wilkens, L.; Lu, S.; Hernandez, B.; Le-Marchand, L.; Henderson, B. Association of coffee intake with re-duced incidence of liver cancer and death from chronic liver disease in the US multiethnic cohort. Gastroenterology 2015, 148, 15. [Google Scholar] [CrossRef] [PubMed]
- Sui, J.; Yang, W.; Ma, Y.; Li, T.Y.; Simon, T.G.; Meyerhardt, J.A.; Liang, G.; Giovannucci, E.L.; Chan, A.T.; Zhang, X. A Prospective Study of Nut Consumption and Risk of Primary Hepatocellular Carcinoma in the U.S. Women and Men. Cancer Prev. Res. 2019, 12, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Koh, W.-P.; Dan, Y.; Goh, G.-B.; Jin, A.; Wang, R.; Yuan, J.-M. Dietary fatty acids and risk of hepatocellular carcinoma in the Singapore Chinese health study. Liver Int. 2016, 36, 893–901. [Google Scholar] [CrossRef] [PubMed]
- Kuper, H.; Tzonou, A.; Lagiou, P.; Mucci, L.; Trichopoulos, D.; Stuver, S.; Trichopoulou, A. Diet and Hepatocellular Carcinoma: A Case-Control Study in Greece. Nutr. Cancer 2000, 38, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Kurozawa, Y.; Ogimoto, I.; Shibata, A.; Nose, T.; Yoshimura, T.; Suzuki, H.; Sakata, R.; Fujita, Y.; Ichikawa, S.; Iwai, N.; et al. Dietary habits and risk of death due to hepatocellular carcinoma in a large scale cohort study in Japan. Univariate analysis of JACC study data. Kurume Med. J. 2004, 51, 141–149. [Google Scholar] [CrossRef]
- Lan, Q.-Y.; Liao, G.-C.; Zhou, R.-F.; Chen, P.-Y.; Wang, X.-Y.; Chen, M.-S.; Chen, Y.-M.; Zhu, H.-L. Dietary patterns and primary liver cancer in Chinese adults: A case-control study. Oncotarget 2018, 9, 27872–27881. [Google Scholar] [CrossRef]
- Montella, M.; Polesel, J.; La Vecchia, C.; Maso, L.D.; Crispo, A.; Crovatto, M.; Casarin, P.; Izzo, F.; Tommasi, L.G.; Talamini, R.; et al. Coffee and tea consumption and risk of hepatocellular carcinoma in Italy. Int. J. Cancer 2007, 120, 1555–1559. [Google Scholar] [CrossRef]
- Tamura, T.; Wada, K.; Konishi, K.; Goto, Y.; Mizuta, F.; Koda, S.; Hori, A.; Tanabashi, S.; Matsushita, S.; Tokimitsu, N.; et al. Coffee, Green Tea, and Caffeine Intake and Liver Cancer Risk: A Prospective Cohort Study. Nutr. Cancer 2018, 70, 1210–1216. [Google Scholar] [CrossRef]
- Vogtmann, E.; Li, H.L.; Shu, X.O.; Chow, W.H.; Ji, B.T.; Cai, H.; Gao, J.; Zhang, W.; Gao, Y.T.; Zheng, W.; et al. Dietary glycemic load, glycemic index, and carbohydrates on the risk of primary liver cancer among Chinese women and men. Ann. Oncol. 2013, 24, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Ma, Y.; Liu, Y.; Smith-Warner, S.; Simon, T.; Chong, D.; Qi, Q.; Meyerhardt, J.A.; Giovannucci, E.L.; Chan, A.T.; et al. Association of Intake of Whole Grains and Dietary Fiber with Risk of Hepatocellular Carcinoma in US Adults. JAMA Oncol. 2019, 5, 879–886. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Sui, J.; Ma, Y.; Simon, T.G.; Chong, D.; Meyerhardt, J.A.; Willett, W.C.; Giovannucci, E.L.; Chan, A.T.; Zhang, X. A prospective study of dairy product intake and the risk of hepatocellular carcinoma in U.S. men and women. Int. J. Cancer 2020, 146, 1241–1249. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Xiang, Y.; Li, H.; Yang, G.; Cai, H.; Ji, B.; Gao, Y.T.; Zheng, W.; Shu, X.O. Vegetable-based dietary pattern and liver cancer risk: Results from the Shanghai women’s and men’s health studies. Cancer Sci. 2013, 104, 1353–1361. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, S.; Harmon, B.E.; Ollberding, N.J.; Wilkens, L.R.; Monroe, K.R.; Kolonel, L.N.; Le Marchand, L.; Boushey, C.J.; Maskarinec, G. Among 4 Diet Quality Indexes, Only the Alternate Mediterranean Diet Score Is Associated with Better Colorectal Cancer Survival and Only in African American Women in the Multiethnic Cohort. J. Nutr. 2016, 146, 1746–1755. [Google Scholar] [CrossRef]
- Fung, T.T.; McCullough, M.L.; Newby, P.; Manson, J.E.; Meigs, J.B.; Rifai, N. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 2005, 82, 163–173. [Google Scholar] [CrossRef]
- Bøhn, S.K.; Blomhoff, R.; Paur, I. Coffee and cancer risk, epidemiological evidence, and molecular mechanisms. Mol. Nutr. Food Res. 2013, 58, 915–930. [Google Scholar] [CrossRef]
- Kurahashi, N.; Inoue, M.; Iwasaki, M.; Tanaka, Y.; Mizokami, M.; Tsugane, S.; for the JPHC Study Group. Vegetable, fruit and antioxidant nutrient consumption and subsequent risk of hepatocellular carcinoma: A prospective cohort study in Japan. Br. J. Cancer 2009, 100, 181–184. [Google Scholar] [CrossRef]
- Latief, U.; Ahmad, R. Role of Dietary Carotenoids in Different Etiologies of Chronic Liver Diseases. In Descriptive Food Science; InTech: Rijeka, Croatia, 2018. [Google Scholar]
- Zhan, J.; Liu, Y.-J.; Cai, L.-B.; Xu, F.-R.; Xie, T.; He, Q.-Q. Fruit and vegetable consumption and risk of cardiovascular disease: A meta-analysis of prospective cohort studies. Crit. Rev. Food Sci. Nutr. 2017, 57, 1650–1663. [Google Scholar] [CrossRef]
- Benetou, V.; Orfanos, P.; Lagiou, P.; Trichopoulos, D.; Boffetta, P.; Trichopoulou, A. Vegetables and Fruits in Rela-tion to Cancer Risk: Evidence from the Greek EPIC Cohort Study. Cancer Epidemiol. Biomark. Prev. 2008, 17, 387. [Google Scholar] [CrossRef]
- Luo, J.; Yang, Y.; Liu, J.; Lu, K.; Tang, Z.; Liu, P.; Liu, L.; Zhu, Y. Systematic review with meta-analysis: Meat consumption and the risk of hepato-cellular carcinoma. Aliment. Pharm. 2014, 39, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Bonkovsky, H. Iron and the Liver. Am. J. Med. Sci. 1991, 301, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Endres, S.; Ghorbani, R.; Kelley, V.; Georgilis, K.; Lonnemann, G.; van der Meer, J.; Cannon, J.G.; Rogers, T.S.; Klempner, M.S.; Weber, P.C.; et al. The Effect of Dietary Supple-mentation with n—3 Polyunsaturated Fatty Acids on the Synthesis of Interleukin-1 and Tumor Necrosis Factor by Mononuclear Cells. N. Engl. J. Med. 1989, 320, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Linseisen, J.; Welch, A.; Ocké, M.; Amiano, P.; Agnoli, C.; Ferrari, P.; Sonestedt, E.; Chajès, V.; Kaaks, R.; Weikert, C.; et al. Dietary fat intake in the European Pro-spective Investigation into Cancer and Nutrition: Results from the 24-h dietary recalls. Eur. J. Clin. Nutr. 2009, 63, 61. [Google Scholar] [CrossRef] [PubMed]
- Cotton, P.A.; Subar, A.F.; Friday, J.E.; Cook, A. Dietary sources of nutrients among US adults, 1994 to 1996. J. Am. Diet. Assoc. 2004, 104, 921–930. [Google Scholar] [CrossRef]
- Wang, S.; Zhou, M.; Ji, A.; Zhang, D.; He, J. Milk/dairy products consumption and gastric cancer: An update me-ta-analysis of epidemiological studies. Oncotarget 2017, 9, 7126. [Google Scholar] [CrossRef][Green Version]
- Zang, J.; Shen, M.; Du, S.; Chen, T.; Zou, S. The Association between Dairy Intake and Breast Cancer in Western and Asian Populations: A Systematic Review and Meta-Analysis. J. Breast Cancer 2015, 18, 313–322. [Google Scholar] [CrossRef]
- Ros, E. Health Benefits of Nut Consumption. Nutrients 2010, 2, 652–682. [Google Scholar] [CrossRef]
- El-Serag, H.; Tran, T.; Everhart, J. Diabetes increases the risk of chronic liver disease and hepatocellular carcinoma. Gastroenterology 2004, 126, 460–480. [Google Scholar] [CrossRef]
- Gnagnarella, P.; Gandini, S.; La Vecchia, C.; Maisonneuve, P. Glycemic index, glycemic load, and cancer risk: A meta-analysis. Am. J. Clin. Nutr. 2008, 87, 1793–1801. [Google Scholar] [CrossRef]
- Chazelas, E.; Srour, B.; Desmetz, E.; Kesse-Guyot, E.; Julia, C.; Deschamps, V.; Druesne-Pecollo, N.; Galan, P.; Hercberg, S.; Latino-Martel, P.; et al. Sugary drink consumption and risk of cancer: Results from NutriNet-Santé prospective cohort. BMJ 2019, 366, 2408. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, X.; Cirillo, P.; Sautin, Y.; McCall, S.; Bruchette, J.L.; Diehl, A.M.; Johnson, R.J.; Abdelmalek, M.F. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J. Hepatol. 2008, 48, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Mediterranean dietary pattern, inflammation and endothelial function: A sys-tematic review and meta-analysis of intervention trials. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 929–939. [Google Scholar] [CrossRef] [PubMed]
- Kastorini, C.-M.; Milionis, H.; Esposito, K.; Giugliano, D.; Goudevenos, J.; Panagiotakos, D. The Effect of Med-iterranean Diet on Metabolic Syndrome and its Components. J. Am. Coll. Cardiol. 2011, 57, 1299. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Abbate, R.; Gensini, G.F.; Casini, A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010, 92, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- George, E.S.; Kucianski, T.; Mayr, H.L.; Moschonis, G.; Tierney, A.C.; Itsiopoulos, C. A Mediterranean Diet Model in Australia: Strategies for Translating the Traditional Mediterranean Diet into a Multicultural Setting. Nutrients 2018, 10, 465. [Google Scholar] [CrossRef]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean diet, its components, and cardiovas-cular disease. Am. J. Med. 2015, 128, 229–238. [Google Scholar] [CrossRef]
- Cespedes, E.; Hu, F. Dietary patterns: From nutritional epidemiologic analysis to national guidelines. Am. J. Clin. Nutr. 2015, 101, 899–900. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).