Immunological Outcomes of Bovine Colostrum Supplementation in Trained and Physically Active People: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Searching Strategies
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
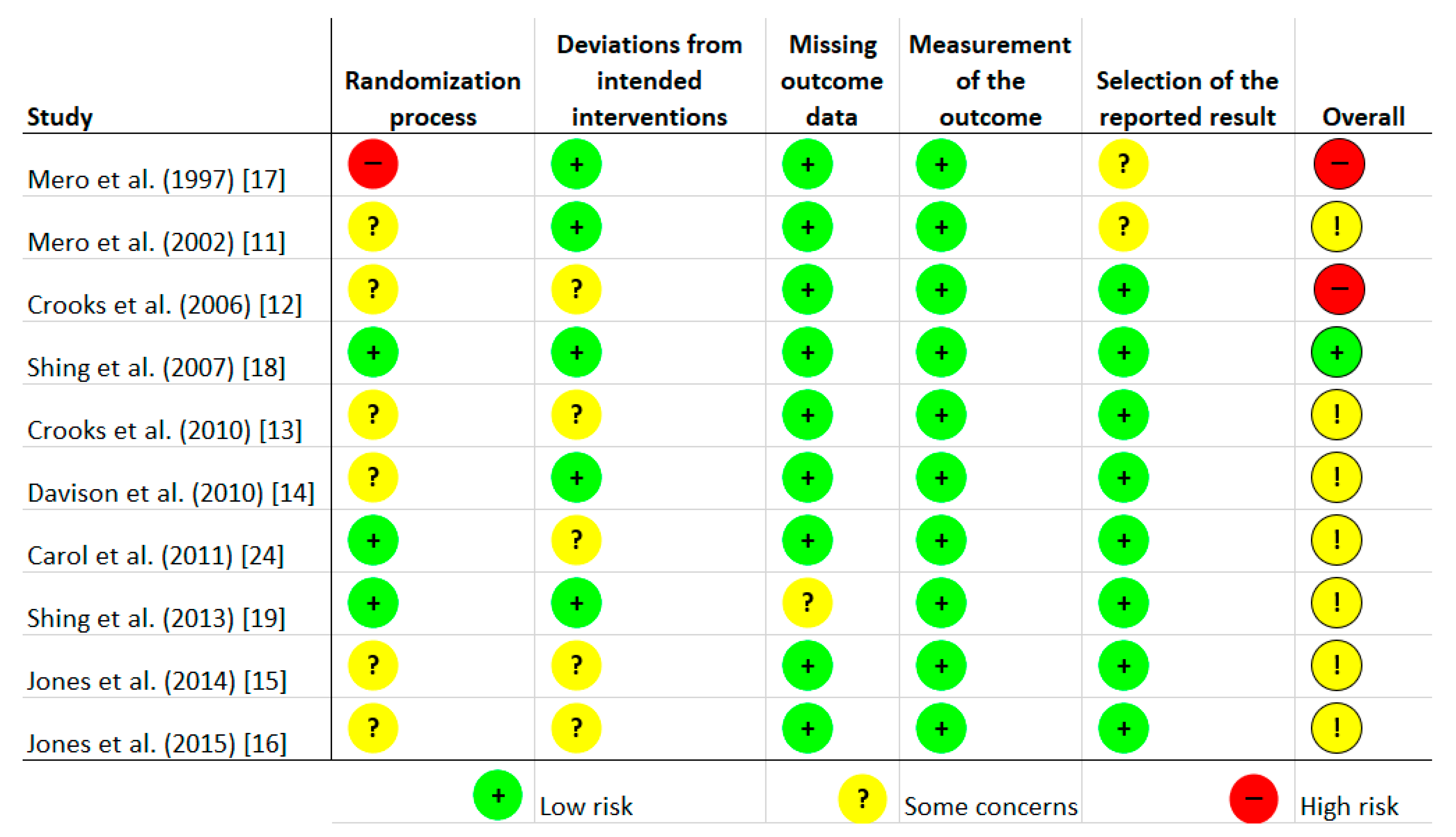
2.4. Quality Assessment of the Experiments
2.5. Statistical Analysis
3. Results
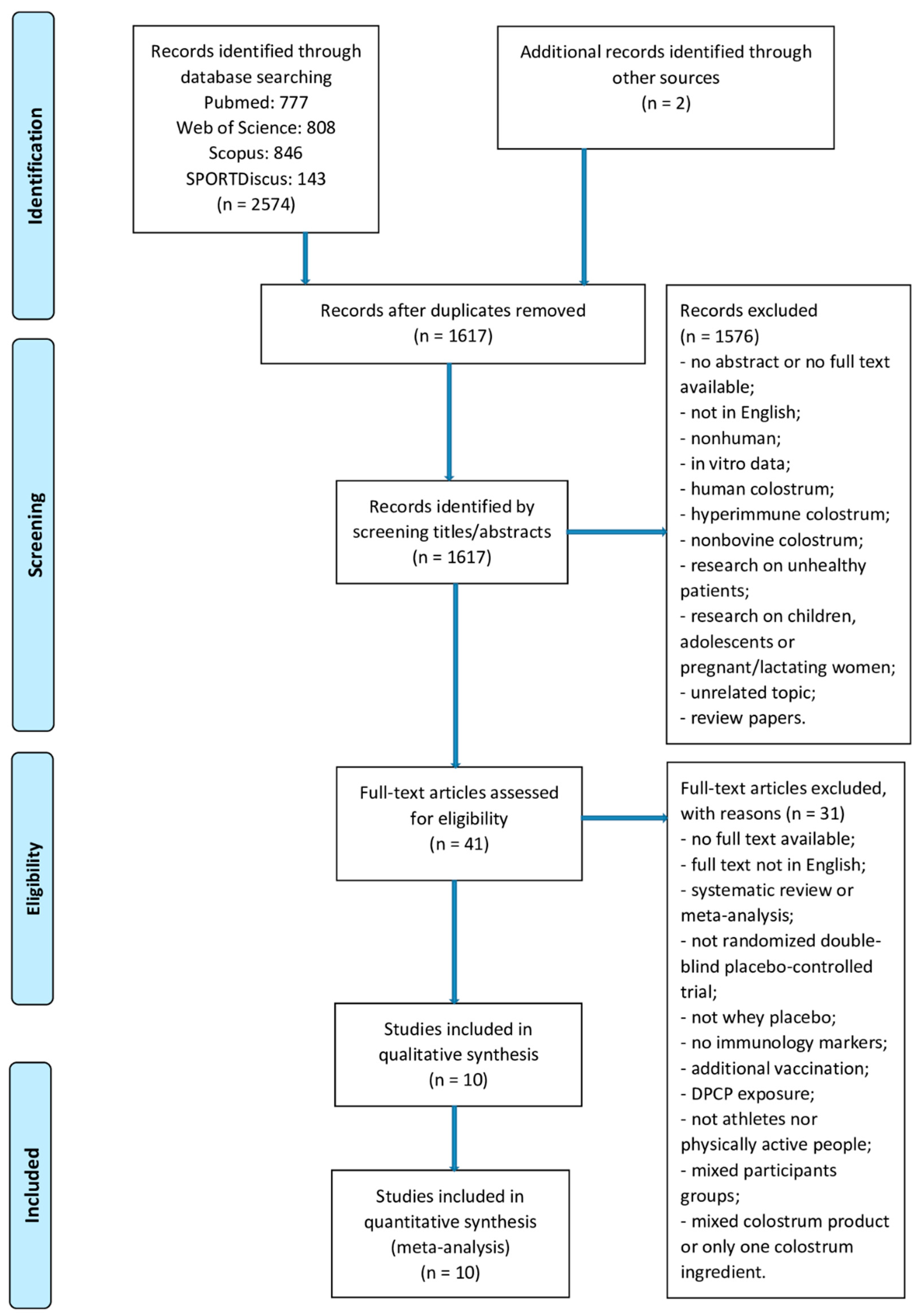
3.1. Main Search
3.2. Study Characteristics
3.3. Effect of Bovine Colostrum (BC) on Immunological Outcomes
3.3.1. Lymphocytes Pre-Exercise
3.3.2. Neutrophils Pre-Exercise
3.3.3. Serum IgA Pre-Exercise
3.3.4. Serum IgG Pre-Exercise
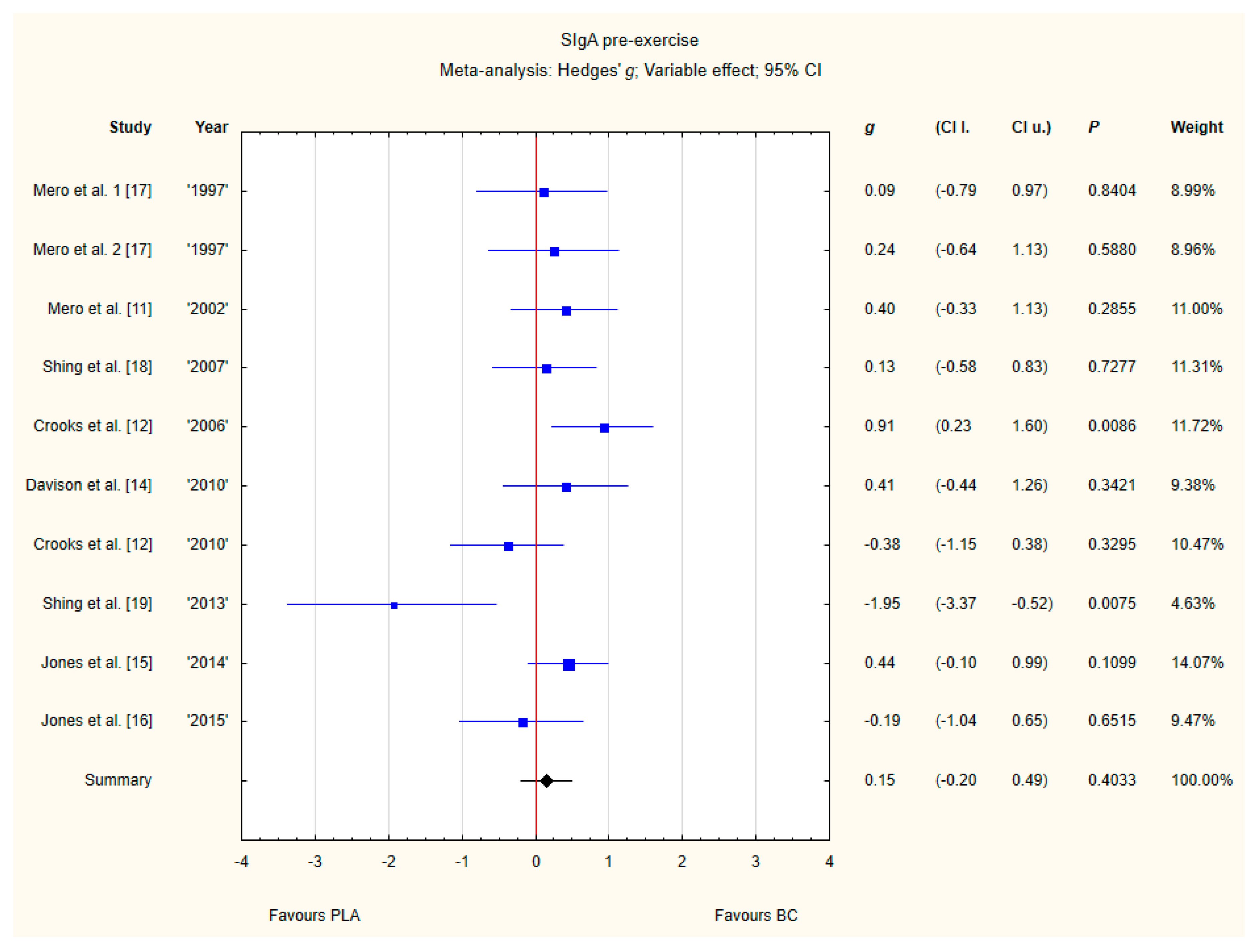
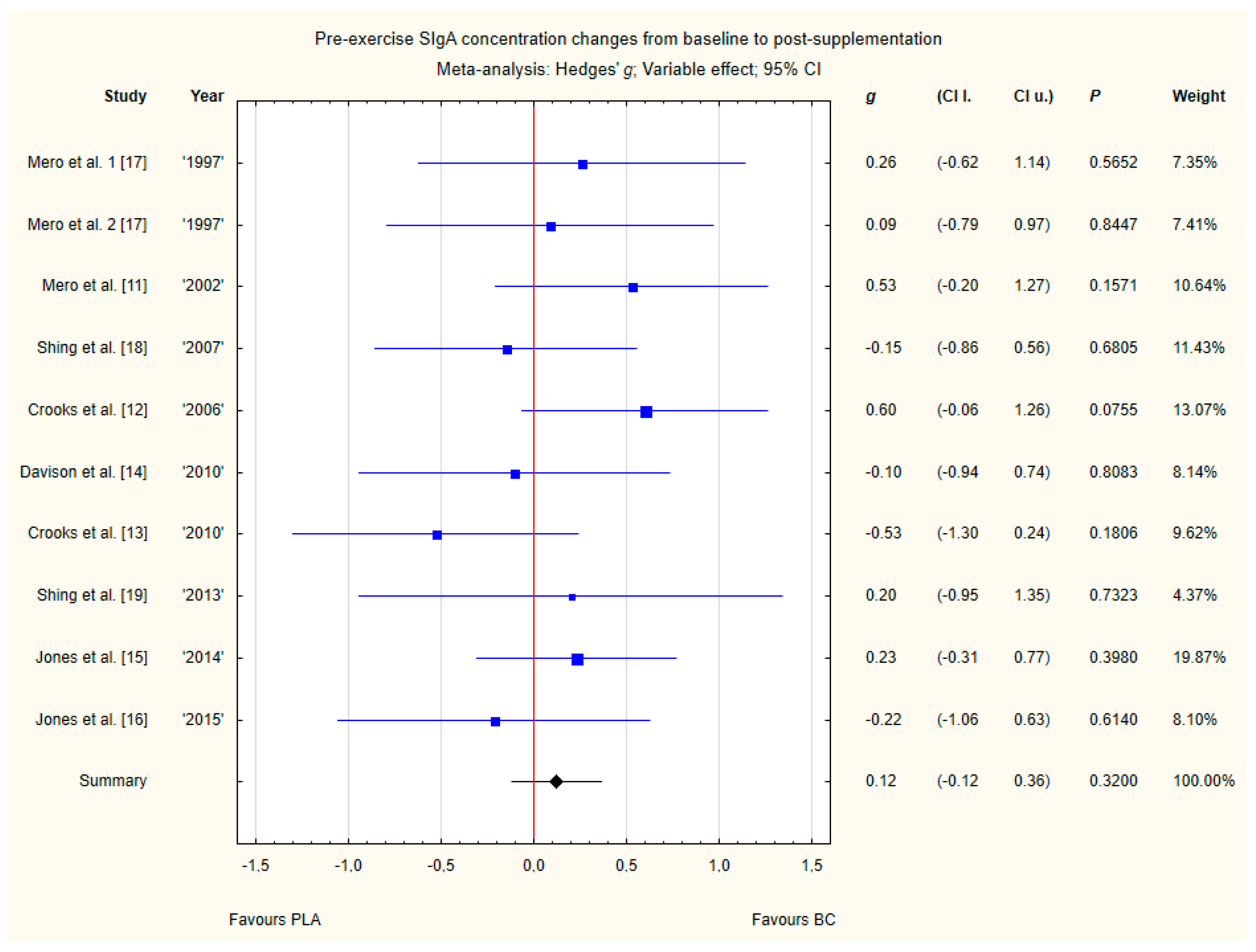
3.3.5. SIgA Pre-Exercise
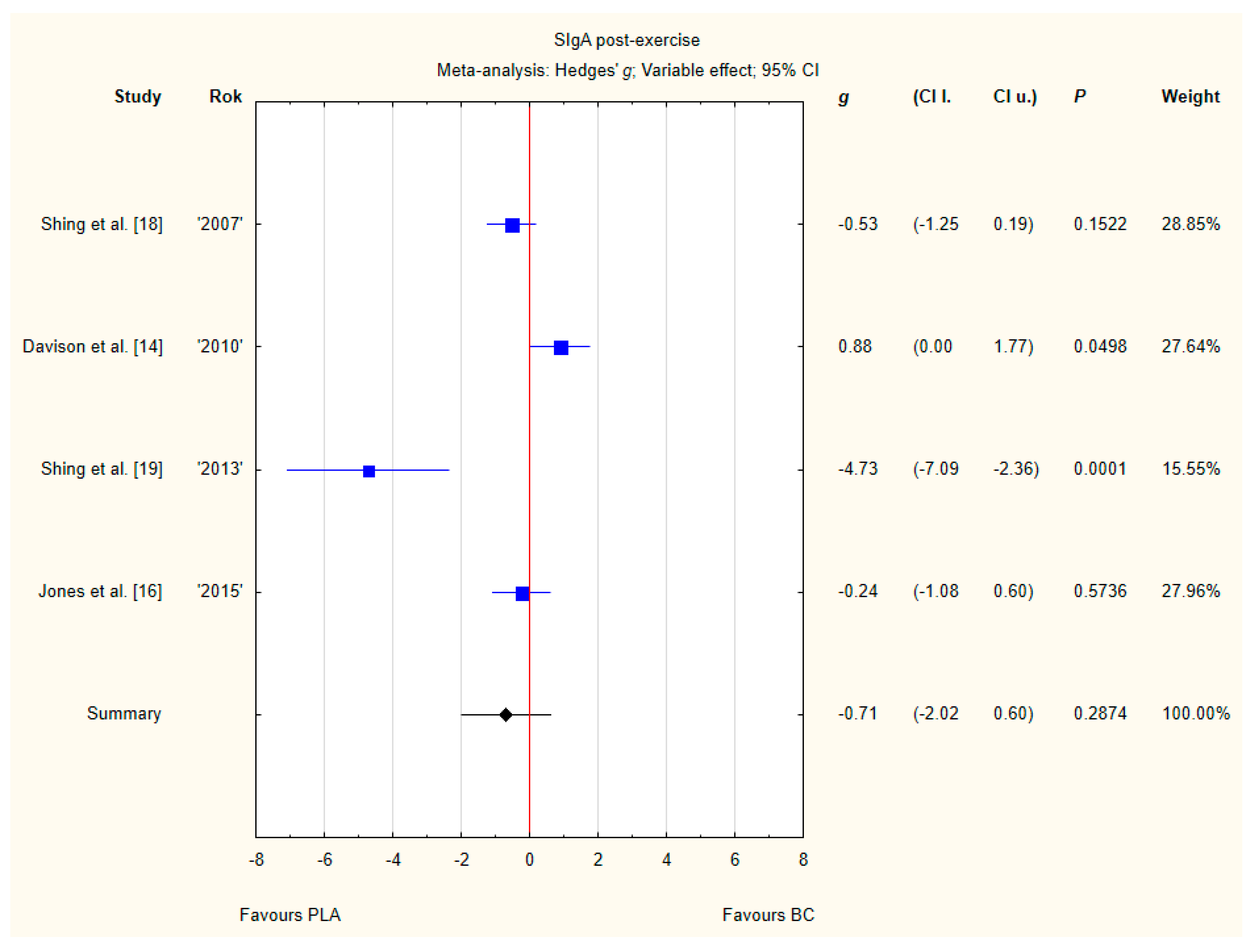
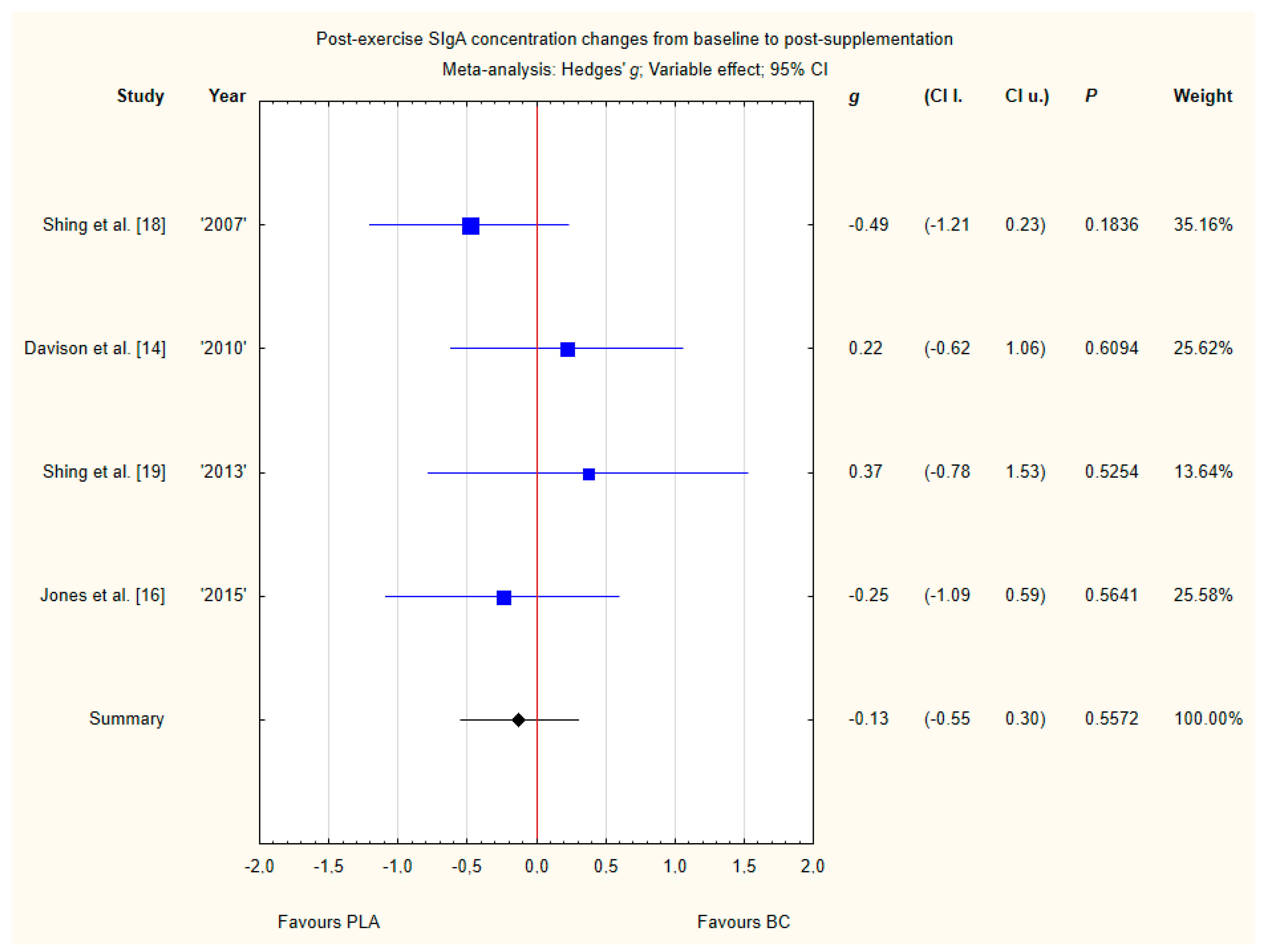
3.3.6. SIgA Post-Exercise
3.3.7. Pre-Exercise Siga Concentration Changes from Baseline to Post-Supplementation
3.3.8. Post-Exercise SIgA Concentration Changes from Baseline to Post-Supplementation
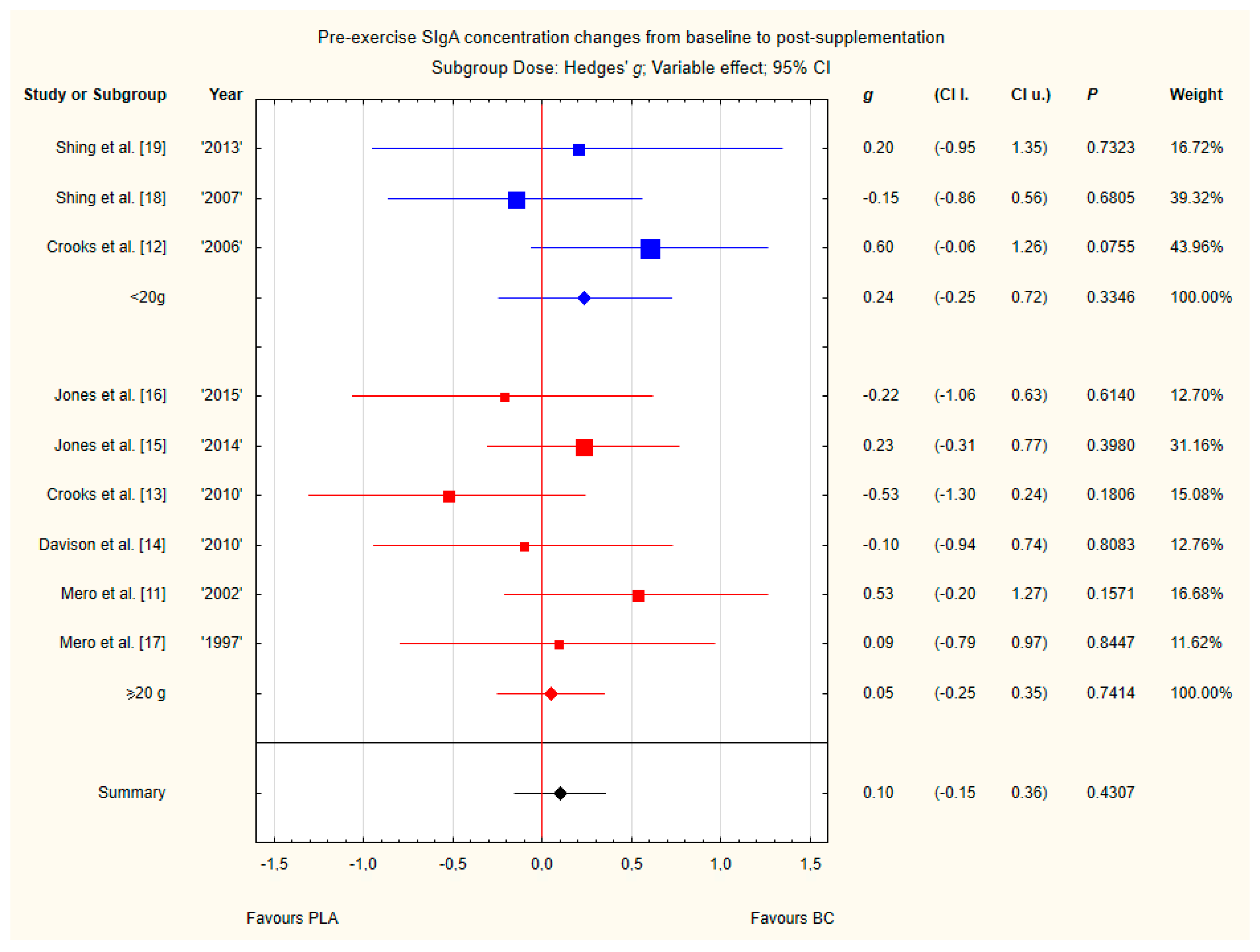
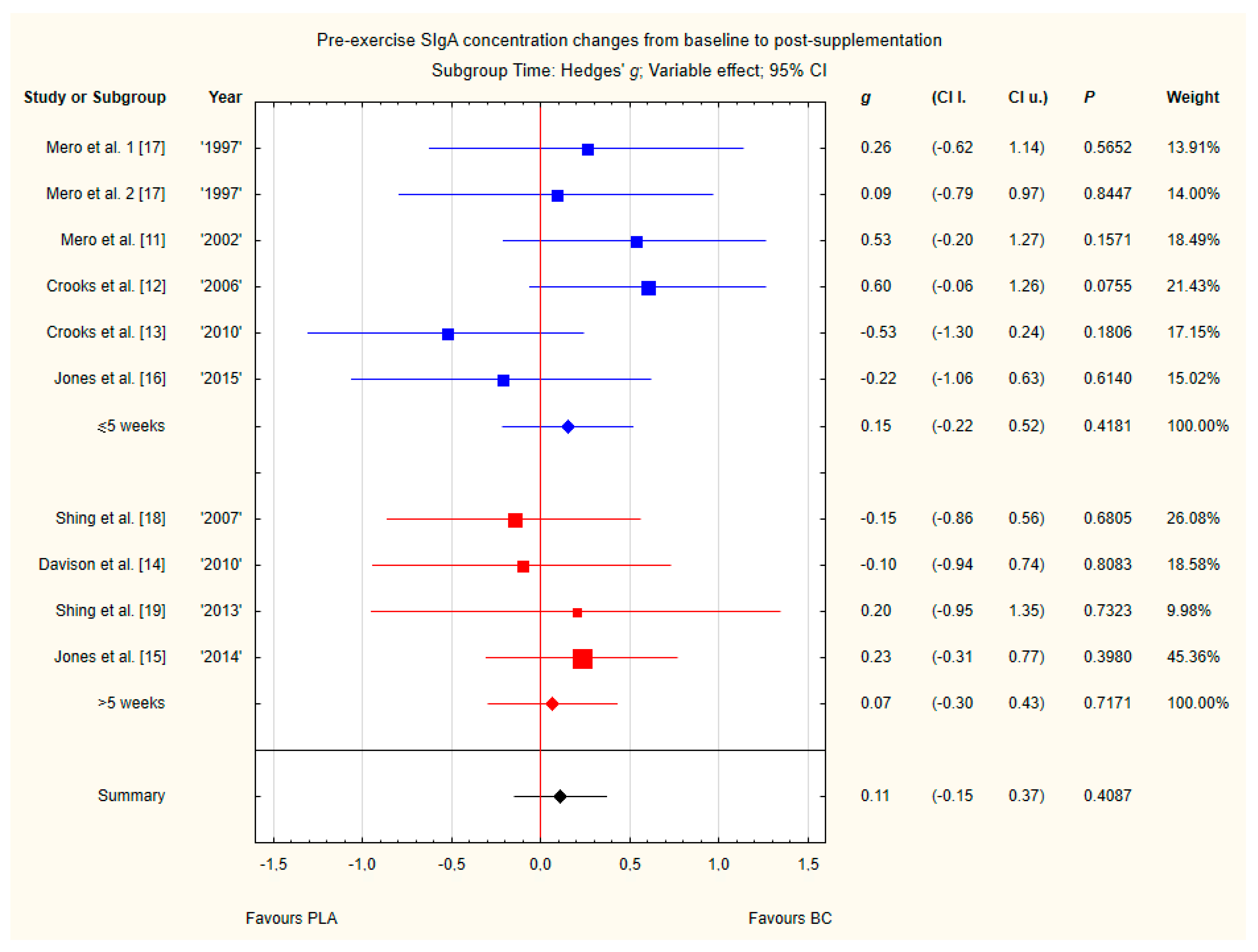
3.4. Subgroup Analyses
3.5. Sensitivity Analyses
4. Discussion
4.1. Effect of BC on Leukocyte Concentrations
4.2. Effect of BC on Serum Immunoglobulin Concentrations
4.3. Effect of BC on SIgA Concentrations
4.4. BC Safety
4.5. Strengths, Limitations, and Future Lines of Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Jones, A.W.; Davison, G. Chapter 15-Exercise, Immunity, and Illness. In Muscle and Exercise Physiology; Zoladz, J.A., Ed.; Academic Press: Cambridge, MA, USA, 2019; pp. 317–344. ISBN 978-0-12-814593-7. [Google Scholar]
- Gleeson, M.; Walsh, N.P. British Association of Sport and Exercise Sciences The BASES expert statement on exercise, immunity, and infection. J. Sports Sci. 2012, 30, 321–324. [Google Scholar] [CrossRef]
- Pyne, D.B.; West, N.P.; Cox, A.J.; Cripps, A.W. Probiotics supplementation for athletes—Clinical and physiological effects. Eur. J. Sport Sci. 2015, 15, 63–72. [Google Scholar] [CrossRef]
- Bermon, S.; Castell, L.M.; Calder, P.C.; Bishop, N.C.; Blomstrand, E.; Mooren, F.C.; Krüger, K.; Kavazis, A.N.; Quindry, J.C.; Senchina, D.S.; et al. Consensus Statement Immunonutrition and Exercise. Exerc. Immunol Rev. 2017, 23, 8–50. [Google Scholar] [PubMed]
- Albers, R.; Bourdet-Sicard, R.; Braun, D.; Calder, P.C.; Herz, U.; Lambert, C.; Lenoir-Wijnkoop, I.; Méheust, A.; Ouwehand, A.; Phothirath, P.; et al. Monitoring immune modulation by nutrition in the general population: Identifying and substantiating effects on human health. Br. J. Nutr. 2013, 110, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Shing, C.M.; Hunter, D.; Stevenson, L. Bovine colostrum supplementation and exercise performance: Potential mechanisms. Sports Med. 2009, 39, 1033–1054. [Google Scholar] [CrossRef] [PubMed]
- Davison, G. Bovine colostrum and immune function after exercise. Med. Sport Sci. 2012, 59, 62–69. [Google Scholar] [PubMed]
- Bagwe, S.; Tharappel, L.J.P.; Kaur, G.; Buttar, H.S. Bovine colostrum: An emerging nutraceutical. J. Complement. Integr. Med. 2015, 12, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Rathe, M.; Müller, K.; Sangild, P.T.; Husby, S. Clinical applications of bovine colostrum therapy: A systematic review. Nutr. Rev. 2014, 72, 237–254. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.W.; March, D.S.; Curtis, F.; Bridle, C. Bovine colostrum supplementation and upper respiratory symptoms during exercise training: A systematic review and meta-analysis of randomised controlled trials. Bmc Sports Sci. Med. Rehabil. 2016, 8, 21. [Google Scholar] [CrossRef]
- Mero, A.; Kähkönen, J.; Nykänen, T.; Parviainen, T.; Jokinen, I.; Takala, T.; Nikula, T.; Rasi, S.; Leppäluoto, J. IGF-I, IgA, and IgG responses to bovine colostrum supplementation during training. J. Appl. Physiol. 2002, 93, 732–739. [Google Scholar] [CrossRef]
- Crooks, C.; Wall, C.R.; Cross, M.L.; Rutherfurd-Markwick, K.J. The effect of bovine colostrum supplementation on salivary IgA in distance runners. Int. J. Sport Nutr. Exerc. Metab. 2006, 16, 47–64. [Google Scholar] [CrossRef] [PubMed]
- Crooks, C.; Cross, M.L.; Wall, C.; Ali, A. Effect of bovine colostrum supplementation on respiratory tract mucosal defenses in swimmers. Int. J. Sport Nutr. Exerc. Metab. 2010, 20, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Davison, G.; Diment, B.C. Bovine colostrum supplementation attenuates the decrease of salivary lysozyme and enhances the recovery of neutrophil function after prolonged exercise. Br. J. Nutr. 2010, 103, 1425–1432. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.W.; Cameron, S.J.S.; Thatcher, R.; Beecroft, M.S.; Mur, L.A.J.; Davison, G. Effects of bovine colostrum supplementation on upper respiratory illness in active males. Brain Behav. Immun. 2014, 39, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.W.; Thatcher, R.; March, D.S.; Davison, G. Influence of 4 weeks of bovine colostrum supplementation on neutrophil and mucosal immune responses to prolonged cycling. Scand. J. Med. Sci. Sports 2015, 25, 788–796. [Google Scholar] [CrossRef] [PubMed]
- Mero, A.; Miikkulainen, H.; Riski, J.; Pakkanen, R.; Aalto, J.; Takala, T. Effects of bovine colostrum supplementation on serum IGF-I, IgG, hormone, and saliva IgA during training. J. Appl. Physiol. 1997, 83, 1144–1151. [Google Scholar] [CrossRef]
- Shing, C.M.; Peake, J.; Suzuki, K.; Okutsu, M.; Pereira, R.; Stevenson, L.; Jenkins, D.; Coombes, J. Effects of bovine colostrum supplementation on immune variables in highly trained cyclists. J. Appl. Physiol. 2007, 102, 1113–1122. [Google Scholar] [CrossRef]
- Shing, C.M.; Peake, J.M.; Suzuki, K.; Jenkins, D.G.; Coombes, J.S. A pilot study: Bovine colostrum supplementation and hormonal and autonomic responses to competitive cycling. J. Sports Med. Phys. Fit. 2013, 53, 490–501. [Google Scholar]
- Jones, A.W.; March, D.S.; Thatcher, R.; Diment, B.; Walsh, N.P.; Davison, G. The effects of bovine colostrum supplementation on in vivo immunity following prolonged exercise: A randomised controlled trial. Eur. J. Nutr. 2017. [Google Scholar] [CrossRef]
- Kotsis, Y.; Mikellidi, A.; Aresti, C.; Persia, E.; Sotiropoulos, A.; Panagiotakos, D.B.; Antonopoulou, S.; Nomikos, T. A low-dose, 6-week bovine colostrum supplementation maintains performance and attenuates inflammatory indices following a Loughborough Intermittent Shuttle Test in soccer players. Eur. J. Nutr. 2018, 57, 1181–1195. [Google Scholar] [CrossRef]
- Główka, N.; Woźniewicz, M.; Durkalec-Michalski, K. Immunological Outcomes of the Bovine Colostrum Supplementation in Physically Active People: A Systematic Review and Meta-analysis PROSPERO 2019 CRD42019125404. Available online: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=125404 (accessed on 3 October 2019).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Carol, A.; Witkamp, R.F.; Wichers, H.J.; Mensink, M. Bovine colostrum supplementation’s lack of effect on immune variables during short-term intense exercise in well-trained athletes. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. Bmc Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0; [updated March 2011]; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Simpson, R.J. The effects of exercise on blood leukocyte numbers. In Exercise Immunology; Routledge: London, UK, 2013. [Google Scholar]
- Gleeson, M. Immune function in sport and exercise. J. Appl. Physiol. 2007, 103, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Steensberg, A.; Toft, A.D.; Bruunsgaard, H.; Sandmand, M.; Halkjaer-Kristensen, J.; Pedersen, B.K. Strenuous exercise decreases the percentage of type 1 T cells in the circulation. J. Appl. Physiol. 2001, 91, 1708–1712. [Google Scholar] [CrossRef]
- Fabbri, M.; Smart, C.; Pardi, R. T lymphocytes. Int. J. Biochem. Cell Biol. 2003, 35, 1004–1008. [Google Scholar] [CrossRef]
- McKune, A.J.; Smith, L.L.; Semple, S.J.; Mokethwa, B.; Wadee, A.A. Immunoglobulin responses to a repeated bout of downhill running. Br. J. Sports Med. 2006, 40, 844–849. [Google Scholar] [CrossRef] [PubMed]
- Siber, G.R.; Schur, P.H.; Aisenberg, A.C.; Weitzman, S.A.; Schiffman, G. Correlation between serum IgG-2 concentrations and the antibody response to bacterial polysaccharide antigens. N. Engl. J. Med. 1980, 303, 178–182. [Google Scholar] [CrossRef]
- Garagiola, U.; Buzzetti, M.; Cardella, E.; Confalonieri, F.; Giani, E.; Polini, V.; Ferrante, P.; Mancuso, R.; Montanari, M.; Grossi, E. Immunological patterns during regular intensive training in athletes: Quantification and evaluation of a preventive pharmacological approach. J. Int. Med. Res. 1995, 23, 85–95. [Google Scholar] [CrossRef]
- Hejazi, K.; Hosseini, S.-R.A. Influence of Selected Exercise on Serum Immunoglobulin, Testosterone and Cortisol in Semi-Endurance Elite Runners. Asian J. Sports Med. 2012, 3, 185. [Google Scholar] [CrossRef]
- Nieman, D.C.; Nehlsen-Cannarella, S.L. The effects of acute and chronic exercise of immunoglobulins. Sports Med. 1991, 11, 183–201. [Google Scholar] [CrossRef] [PubMed]
- Walsh, N.P.; Gleeson, M.; Shephard, R.J.; Gleeson, M.; Woods, J.A.; Bishop, N.C.; Fleshner, M.; Green, C.; Pedersen, B.K.; Hoffman-Goetz, L.; et al. Position statement. Part one: Immune function and exercise. Exerc. Immunol. Rev. 2011, 17, 6–63. [Google Scholar] [PubMed]
- Mackinnon, L. Immunoglobulin, antibody, and exercise. Exerc. Immunol. Rev. 1996, 2, 1–34. [Google Scholar]
- Nieman, D.C.; Henson, D.A.; Fagoaga, O.R.; Utter, A.C.; Vinci, D.M.; Davis, J.M.; Nehlsen-Cannarella, S.L. Change in salivary IgA following a competitive marathon race. Int. J. Sports Med. 2002, 23, 69–75. [Google Scholar] [CrossRef]
- Gleeson, M.; Pyne, D.B. Special feature for the Olympics: Effects of exercise on the immune system: Exercise effects on mucosal immunity. Immunol. Cell Biol. 2000, 78, 536–544. [Google Scholar] [CrossRef]
- Brinkworth, G.D.; Buckley, J.D. Concentrated bovine colostrum protein supplementation reduces the incidence of self-reported symptoms of upper respiratory tract infection in adult males. Eur. J. Nutr. 2003, 42, 228–232. [Google Scholar] [CrossRef]
- Stoeck, M.; Ruegg, C.; Miescher, S.; Carrel, S.; Cox, D.; Von Fliedner, V.; Alkan, S. Comparison of the immunosuppressive properties of milk growth factor and transforming growth factors beta 1 and beta 2. J. Immunol. 1989, 143, 3258–3265. [Google Scholar]
- Chen, S.S.; Li, Q. Transforming growth factor-beta 1 (TGF-beta 1) is a bifunctional immune regulator for mucosal IgA responses. Cell. Immunol. 1990, 128, 353–361. [Google Scholar] [CrossRef]
- Pakkanen, R. Determination of transforming growth factor-beta 2 (TGF-beta 2) in bovine colostrum samples. J. Immunoass. 1998, 19, 23–37. [Google Scholar] [CrossRef]
- Rutherfurd-Markwick, K.J.; Johnson, D.; Cross, M.L.; Gill, H.S. Modified milk powder supplemented with immunostimulating whey protein concentrate (IMUCARE) enhances immune function in mice. Nutr. Res. 2005, 2, 197–208. [Google Scholar] [CrossRef]
- Low, P.P.L.; Rutherfurd, K.J.; Cross, M.L.; Gill, H.S. Enhancement of mucosal antibody responses by dietary whey protein concentrate. Food Agric. Immunol. 2001, 13, 255–264. [Google Scholar] [CrossRef]
- He, F.; Tuomola, E.; Arvilommi, H.; Salminen, S. Modulation of human humoral immune response through orally administered bovine colostrum. Fems Immunol. Med. Microbiol. 2001, 31, 93–96. [Google Scholar] [CrossRef] [PubMed]





| Study | Country | Study Design | Sample Size | Sex, Age (Years) | Inclusion Criteria | Exclusion Criteria | Duration | Intervention Dose | Intervention Additional Info | Placebo (PLA) |
|---|---|---|---|---|---|---|---|---|---|---|
| Mero et al. 1997 [17] | Finland | DB-RCT 1 and crossover | 9 | Only males 25 ± 2.5 2 | Athletes (sprinters, jumpers), drug-free | Use of supplements of amino acids, vitamins, minerals, or creatine monohydrate or any other sport supplement during the study phase | 8 days | 25/125 mL | Drink (containing BC) of 125 mL consumed in a splitdose twice per day (62.5 mL in the morning and 62.5 mL in the evening), not taken in the morning of the test training session but post-session. I treatment: 125 mL Bioenervi drink, II treatment: 25 mL Bioenervi (the drink of 125 mL containing the 25-mL Bioenervi supplement mixed with 100-mL placebo) | 125 mL of ‘normal milk whey’ 5 per day |
| Mero et al. 2002 [11] | Finland | DB-RCT 1 | 30 | BC: males 21.5 ± 0.7 3, females 22.6 ± 1.6 3; PLA: males 21.7 ± 1.9 3, females 22.9 ± 2.6 3 | Athletes (track and field athletes, cross-country skiers, and orienteers), drug-free | Use of supplements of amino acids, vitamins, minerals, or creatine monohydrate, or any other supplement during the study phase | 2 weeks | 20 g | 20 g of BC in a split dose four times per day (5 g) | 20 g of maltodextrin per day |
| Crooks et al. 2006 [12] | New Zealand | DB-RCT 1 | 35 | BC: males 46 (35–57) 4, females 43 (30–53) 4; PLA: males 48 (36–56) 4, females, 51 (41–58) 4 | Recreational distance runners, pack runs ≥ 1 week, marathon training over last 5 years, age < 60 year | Lactose intolerance, allergy to cows milk, use of whey-protein supplements, treatment for any diagnosed condition | 12 weeks | 10 g | 26 g of powdered sachets/day corresponding to 10 g of BC (chocolate powder with 125 ml water) | Skim milk |
| Shing et al. 2007 [18] | Australia | DB-RCT 1 | 29 | Only males BC: 29 ± 1 3 PLA: 27 ± 2 3 | Athletes (cyclists), racing competitively ≥ 2 seasons, consistent training volumes ≥ 2 months | Use of dietary supplements for 1 month prior to study | 5 weeks | 10 g | 10 g of BC per day in the morning with 50 mL water + 100 mL milk. | 10g of whey protein per day |
| Davison et al. 2010 [14] | United Kingdom | DB-RCT 1 | 20 | Only males 25.0 ± 5 2 | None reported | None reported | 4 weeks | 20 g | 20 g of BC per day | PLA containing an isoenergetic and isomacronutrient mixture of milk protein concentrate |
| Crooks et al. 2010 [13] | New Zealand | DB-RCT 1 | 25 | BC: males 17 ± 1 3, females 20 ± 1 3; PLA: males 19 ± 1 3, females 18 ± 1 3 | Athletes (swimmers), participating in training program prior to The Auckland Swimming Championships | Lactose intolerance, allergy to cows’ milk, use of whey-protein, immunological-modulating supplements, treatment for any diagnosed condition | 10 weeks | 20 g | 52 g of powdered sachets per day corresponding to 20 g of BC per day, in a split dose twice per day: 10 g morning & evening, with 125 mL water | Skim milk powder |
| Carol et al. 2011 [24] | The Netherlands | DB-RCT 1 and crossover | 9 | Only males 27.3 ± 4.5 2 | Athletes (cyclists), >2 years of cycling experience, training >3 times/week during > 9 months/year, refraining from using dietary supplements | Allergy to cow’s milk or a known immune disease, signs of infection during the month preceding the study, treatment for any medical condition, use of any drugs, or consume more than two alcoholic beverages per day | 10 days | 25 g | 12.5 g of BC twice a day, with a glass of cold milk or cold buttermilk | Skim milk powder |
| Shing et al. 2013 [19] | Australia | DB-RCT 1 | 10 | Only males BC: 22 ± 3 PLA: 23 ± 2 3 | Athletes (cyclists), racing competitively ≥3 seasons, consistent training volumes ≥ 2 months | None reported | 8 weeks and 5 days | 10 g | 10 g of BC per day, morning with 50 mL water + 100 mL milk | 10 g Whey protein concentrate per day |
| Jones et al. 2014 [15] | United Kingdom | DB-RCT 1 | 53 | Only males BC: 31 ± 14 2 PLA: 32 ± 13 2 | Recreationally active people, ≥3 h moderate-vigorous endurance exercise/ week | Smoking, use of medication or other supplements, infectious illness in 4 weeks prior to study | 12 weeks | 20 g | 20 g of BC per day, in a split dose: 10 g with morning & evening meal | Isoenergetic/isomacronutrient |
| Jones et al. 2015 [16] | United Kingdom | DB-RCT 1 | 20 | Only males 28 ± 8 2 | Recreationally active men | Smoking, allergy to dairy products and reported symptoms of infection or use of any medication or dietary supplements 4 weeks prior to commencement of the study | 4 weeks | 20 g | 20 g of BC per day, in a split dose: 10 g morning & evening on an empty stomach | Isoenergetic/isomacronutrient |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Główka, N.; Durkalec-Michalski, K.; Woźniewicz, M. Immunological Outcomes of Bovine Colostrum Supplementation in Trained and Physically Active People: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 1023. https://doi.org/10.3390/nu12041023
Główka N, Durkalec-Michalski K, Woźniewicz M. Immunological Outcomes of Bovine Colostrum Supplementation in Trained and Physically Active People: A Systematic Review and Meta-Analysis. Nutrients. 2020; 12(4):1023. https://doi.org/10.3390/nu12041023
Chicago/Turabian StyleGłówka, Natalia, Krzysztof Durkalec-Michalski, and Małgorzata Woźniewicz. 2020. "Immunological Outcomes of Bovine Colostrum Supplementation in Trained and Physically Active People: A Systematic Review and Meta-Analysis" Nutrients 12, no. 4: 1023. https://doi.org/10.3390/nu12041023
APA StyleGłówka, N., Durkalec-Michalski, K., & Woźniewicz, M. (2020). Immunological Outcomes of Bovine Colostrum Supplementation in Trained and Physically Active People: A Systematic Review and Meta-Analysis. Nutrients, 12(4), 1023. https://doi.org/10.3390/nu12041023






