Abstract
Digital transformation is the process of using digital technologies for creating or modifying existing business processes and customer experience, leveraging cutting-edge technology to meet changing market needs. Disruptions like the COVID-19 pandemic, regional wars, and climate-driven natural disasters create consequential scenarios, e.g., global supply chain disruption creating further demand–supply mismatch for healthcare enterprises. According to KPMG’s 2021 Healthcare CEO Future Pulse, 97% of healthcare leaders reported that COVID-19 significantly accelerated the digital transformation agenda. Successful digital transformation initiatives, for example, digital twins for supply chains, augmented reality, the IoT, and cybersecurity technology initiatives implemented significantly enhanced resiliency in supply chain and manufacturing operations. However, according to another study conducted by Mckinsey & Company, 70% of digital transformation efforts for healthcare enterprises fail to meet their goals. Healthcare enterprises face unique challenges, such as complex regulatory environments, cultural resistance, workforce IT skills, and the need for data interoperability, which make digital transformation a challenging project. Therefore, this study explored potential barriers, enablers, disruption scenarios, and digital transformation use cases for healthcare enterprises. A structured literature review (SLR), followed by thematic content analysis, was conducted to inform the research objectives. A sample of sixty (n = 60) peer-reviewed journal articles were analyzed using research screening criteria and keywords aligned with research objectives. The key themes for digital transformation use cases identified in this study included information processing capability, workforce enablement, operational efficiency, and supply chain resilience. Collaborative leadership as a change agent, collaboration between information technology (IT) and operational technology (OT), and effective change management were identified as the key enablers for digital transformation of healthcare enterprises. This study will inform digital transformation leaders, researchers, and healthcare enterprises in the development of enterprise-level proactive strategies, business use cases, and roadmaps for digital transformation.
1. Introduction
The past decade has witnessed a convergence of global disruptions including the COVID-19 pandemic, the Russia–Ukraine war, and climate-induced natural disasters which have profoundly impacted how firms operate across sectors. Healthcare enterprises, particularly those involved in medical manufacturing and supply, were disproportionately affected due to surges in demand for critical supplies, global supply chain breakdowns, and heightened market volatility [1]. A study conducted by Deloitte in 2022 highlighted that nearly 60% of healthcare organizations prioritized supply chain resilience post-pandemic, reflecting a significant 13-point increase from earlier stages of the crisis. In response to these disruptions many healthcare organizations accelerated their digital transformation agendas shifting from manual operations to technology-enabled processes to enhance visibility, agility, and resilience. According to KPMG’s 2021 Healthcare CEO Future Pulse, 97% of healthcare leaders acknowledged that COVID-19 significantly accelerated the digital transformation agenda. Defined as a comprehensive shift in mindset, processes, and digital tools, digital transformation plays a critical role in improving organizational resilience through both digitalization and servitization [2,3].
However, despite significant investments in emerging technologies such as artificial intelligence (AI), the Internet of Things (IoT), and blockchain to improve predictive capabilities and supply chain visibility, transformation outcomes often fall short. A 2022 McKinsey report found that approximately 70% of digital transformation efforts fail to achieve their intended goals, largely due to persistent challenges including legacy infrastructure, cultural resistance, and workforce limitations [4]. Moreover, cybersecurity threats further complicated transformation initiatives; nearly 60% of healthcare organizations have experienced ransomware attacks that disrupted supply chain operations and compromised patient care delivery [5,6].
While several studies have identified individual barriers and enablers to digital transformation in healthcare, there remains a critical gap in literature. Specifically, few studies offer an integrated perspective that links disruption scenarios, barriers, enablers, and digital transformation use cases in a cohesive framework. For instance, studies conducted by [2,4,7,8,9] highlight digital transformation enablers, barriers, and organizational success factors but not the disruption scenarios, use cases, enablers, and barriers holistically for healthcare enterprises.
This limits healthcare leaders’ ability to proactively plan for resilience and derive actionable insights for long-term transformation strategies.
This study aimed to address this gap by systematically examining the interrelationships among disruption scenarios, organizational barriers, enabling factors, and applied use cases of digital technologies in healthcare enterprises. The research questions explored in this study were as follows: 1. What are the key disruption scenarios, use cases, enablers, and barriers to digital transformation of healthcare enterprises? 2. How do disruption scenarios drive digital transformation use cases for healthcare enterprises? 3. How can barriers to digital transformation for healthcare enterprises be mitigated with enablers? The goal was to develop a conceptual understanding that not only cataloged these elements but also revealed how they interacted to influence digital transformation outcomes. By doing so, this research offers practical guidance for healthcare executives, technology managers, and policymakers in designing adaptive, resilient, and future-ready digital transformation roadmaps. A sample of n = 60 peer-reviewed journal articles was selected out of n = 90 articles following the research screening criteria including keywords “Digital transformation barriers”, “Healthcare enterprises”, “Digital transformation enablers”, “Digital transformation use-cases” and “Disruption scenarios for healthcare enterprises”. The sample was analyzed following thematic content analysis using NVivo and based on research objectives to identify the key recurring themes for barriers, enablers, disruption scenarios, and digital transformation use cases for healthcare enterprises.
This research paper is organized in five main sections: Section 2 describes background literature defining keywords used for conducting a structured literature review, Section 3 describes methodology for the study, including data collection methods, i.e., structured literature review and data analysis approach used, i.e., thematic content analysis, and Section 4 describes results, categorized under research objectives of the study, i.e., key barriers, enablers, disruption scenarios, and digital transformation use cases for healthcare enterprises.
2. Background
This section provides background on the key terms, based on broader research objectives defining keywords used in the study, “Digital transformation barriers”, “Healthcare enterprises”, “Digital transformation enablers”, “Disruption scenarios for healthcare enterprises”, and “Digital transformation use cases”.
2.1. Digital Transformation Barriers
In defining and understanding barriers to digital transformation it is important to first define digital transformation for an individual enterprise. Therefore, the definition of digital transformation may vary with the scope and objectives of an enterprise. This variation in definition also relates to the range of application of changes and the resulting benefits for the enterprises [10]. Multiple authors have defined digital transformation in the context of different studies. The study conducted by [11] states that “The best understanding of digital transformation is adopting business processes and practices to help the organization compete effectively in an increasingly digital world”. The perception and definition of digital transformation acting as a bridge between information technology and business processes is in line with another study where [12] state, “We define digital transformation as the use of new digital technologies (social media, mobile, analytics or embedded devices) to enable major business improvements (such as enhancing customer experience, streamlining operations or creating new business models)”. Additionally, other studies conducted by [13] defined digital transformation holistically from an organizational perspective: “Digital transformation is an ongoing process of changing the way you do business. It requires foundational investments in skills, projects, infrastructure, and IT systems. It requires mixing people, machines, and business processes, with all the messiness that entails. It also requires continuous monitoring and intervention, from the top, to ensure that both digital leaders and non-digital leaders are making good decisions about their transformation efforts”.
Multiple organizations fail in their digital transformation initiatives due to cultural resistance and lack of collaborative leadership support. Further lack of interoperability among various healthcare IT systems impacts data quality and creates an inability to utilize data effectively for patient care improvements [14]. The study conducted by [15] reported legacy infrastructure and lack of technical IT skills as barriers to the digital transformation of healthcare enterprises.
2.2. Digital Transformation Enablers
A study conducted by [16] categorized enablers or success factors for digital transformation into three categories, i.e., organizational, process, and technology. Upskilling employees in digital tools and fostering a culture of innovation are critical for successful implementation of digital transformation initiatives [14]. A survey conducted by [17] highlighted that small and medium-sized businesses that get good management support are more likely to be successful in implementing digital transformation initiatives. Data quality is another critical success criterion, as highlighted in the study conducted by [18], because healthcare data systems are less interoperable, and cloud infrastructure is a way out, but with extra cybersecurity measures to meet regulatory compliances in healthcare systems. It is important to study the digital transformation enablers for healthcare enterprises, as according to study conducted by Mckinsey & Company 2024, 70% of digital transformation efforts for healthcare enterprises fail to meet their goals.
2.3. Disruption Scenarios for Healthcare Enterprises
The different types of healthcare enterprises include the manufacturing of medical devices, and the technologies and processes used in healthcare patient care systems, including therapy and healthcare services [19]. Medical device manufacturing enterprises have seen uncertainty in demand, supply chain disruptions, and constant pressure due to market volatility during the COVID-19 pandemic [3]. The manufacturing of devices, therapies, vaccines, and healthcare technologies involves complex operations, and ensuring high quality and safety while reducing time to market is a critical challenge faced during disruptions [20]. Digital transformation through digitalization and servitization can improve resilience at operational and organizational levels for healthcare enterprises [21].
Disruption for an enterprise is defined where a change upsets current systems to such a point that the incumbents operating in that system cannot adapt to that change [22]. The last decade has seen multiple disruptions, including the COVID-19 pandemic, territorial wars, and natural disasters based on climate change. Each disruption generates multiple scenarios, e.g., supply chain disruption, demand surge, market volatility, and cybersecurity threats [23]. These scenarios might have cascading effects on medical manufacturing enterprises with sequential sub-scenarios, e.g., raw material supply shortages, lockdown restrictions, unprecedented peaks of demand, long-term outstock, and cybersecurity threats [24]. The healthcare supply chain is heavily reliant on interconnected systems, and this makes it increasingly vulnerable to cyberattacks. Approximately 60% of healthcare organizations have faced ransomware attacks, disrupting supply chain operations and manufacturing schedules [5]. Regulatory compliance and geopolitical factors also cause disruption, as sometimes, heavy reliance on international suppliers for raw materials and components has made healthcare manufacturing susceptible to geopolitical disruptions, such as trade restrictions, territorial wars, epidemics, or climate-based natural disasters [25]. Therefore, healthcare enterprises must understand different disruption scenarios and plan accordingly for digital transformation.
3. Materials and Methods
This section describes the data collection method, which was the structured literature review (SLR) and thematic content analysis approach used for data analytics. The first step of the structured literature review (SLR) followed the framework mentioned in the study [26] defining a unit of analysis which included the keywords used as a research criteria based on the research objectives. The keywords used as screening criteria were “Digital transformation barriers”, “Digital transformation enablers”, “Healthcare enterprises”, and “Disruption scenarios for healthcare enterprises”. This framework [26] delineated the material to be analyzed by defining the initial unit of analysis with keywords as a research criterion, creating analytical categories, defining the material collection (creating and defining categories), pretesting the defined categories, refining pretesting categories, and analyzing the data by coding for thematic analysis. The period of analysis chosen was 2010–2024, and in the review a sample of n = 60 journals was selected out of n = 90 articles which met the keyword-based research criteria. To ensure a systematic and transparent approach to literature selection, this study adopted the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The PRISMA approach enhanced the rigor and replicability of the review process, ensuring the selection of high-quality and relevant studies [24].
The research query was applied across reputable, peer-reviewed databases including Emerald, IEEE Xplore, Taylor & Francis, Inderscience, and ScienceDirect. Boolean operators (“AND”, “OR”) were employed to construct comprehensive search strings, as illustrated in Figure 1. Following the identification stage, the screening process involved the application of predefined inclusion and exclusion criteria grounded in the study’s research objectives and theoretical framework. Titles, abstracts, keywords, and conclusions of the initially retrieved articles (n = 90) were assessed to determine relevance. Based on this screening, 30 articles were excluded, resulting in a final sample of 60 articles for in-depth review. To analyze the selected literature, thematic content analysis was conducted using NVivo 15 software which enabled efficient coding and visualization of data. The themes were categorized based upon research keywords with top-level coding performed by the authors. Themes were further validated by three raters, with each rater coding a representative subset of the data, and results were compared to assess coding consistency. Cohen’s Kappa value, to evaluate agreement levels among the raters, was calculated as K = 0.80, confirming an acceptable degree of consistency and reliability in theme identification [27]. Inter-reliability testing also mitigated selection and conformation biases by validating the extracted key themes.
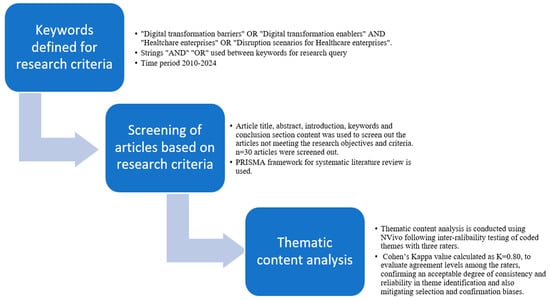
Figure 1.
Structured literature review (SLR) methodology.
Thematic content analysis was based on an inductive approach where recurrent themes based on research objectives were identified and analyzed. Figure 2 highlights the year-wise distribution of the peer-reviewed articles based on the keywords. The period of analysis was from 2010 to 2024.
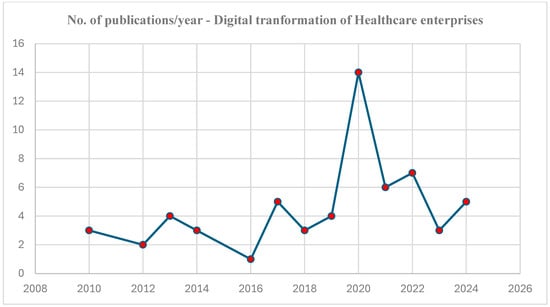
Figure 2.
Peer-reviewed articles published on the digital transformation of healthcare enterprises, n = 60.
Figure 2, highlights the distribution of peer-reviewed articles published on the digital transformation of healthcare enterprises. Fourteen articles, the highest number of articles, were published during the COVID-19 pandemic disruption, 2020, and the second highest number (seven articles) during 2022, a year of another disruptive event, i.e., the Ukraine– Russia territorial war. This trend also highlights that interest in this topic is building up, with numbers increasing with future disruptive events.
Data Analysis (Thematic Content Analysis)
Data analysis was conducted on the sample of n = 60 articles selected through a structured literature review (SLR) methodology. The definition of thematic content analysis as stated by [1] is “content analysis is a research technique for the objective, systematic and quantitative description of the manifest content of communication”. Thematic content analysis was conducted using the NVivo platform [28]. The refined research query connected with string “OR” was used for thematic content analysis and categorizing themes for “Digital transformation of healthcare enterprises” OR “Digital transformation barriers for healthcare enterprises” OR “Digital transformation enablers for healthcare enterprises” OR “Disruption scenarios for healthcare enterprises” OR “Digital transformation use cases for healthcare enterprises”. Recurrent themes were identified and analyzed from the research query results. Recurrent themes are highlighted and described through the word cloud with exact quote descriptions from the literature. The following section, Section 4, describes the results.
4. Results
This section highlights the results of the thematic content analysis conducted to identify and describe key themes based on the research objectives. Key themes are highlighted through word clouds and descriptive analysis shown in the tables.
4.1. Digital Transformation Barriers for Healthcare Enterprises
Resistance to change and the human side of transformation is the most challenging as it relates to people’s needs for steadiness [29]. Resistance to adaptation for changes or new norms is a top barrier cited for moving towards digital transformation [29]. Employees refusing to change their traditional ways of working, which may be due to regulatory compliance, legacy of systems, or inadequate skills provides resistance to change [30]. Regulatory compliance is another key theme and is cited as a barrier where researchers have identified the insufficient development of the regulatory framework and standards as barriers to digital transformation of healthcare enterprises [31]. According to many research studies [32], there is a growing demand for data and tech-savvy executives with excellent analytical skills, and cloud-based business intelligence systems have made progress toward development in healthcare enterprises that utilize predictive and prescriptive analytics. Inadequate workforce skills and a low awareness level of employees in the use and management of emerging technologies, specifically AI/ML, is a significant factor and emergent theme for barriers to digital transformation of healthcare enterprises. Healthcare data are often stored in different formats across different systems, making it difficult to achieve seamless interoperability. Inconsistencies in terminology, coding systems (e.g., ICD-10 vs. SNOMED CT), and data-exchange protocols lead to errors and inefficiencies in patient care and analytics [33]. Without standardized data structures, integrating electronic health records (EHRs) across providers remains a challenge.
The word cloud in Figure 3 highlights the key themes for barriers to digital transformation, which are resistance to change, regulatory compliance, inadequate workforce skills, and inadequate data and data quality.
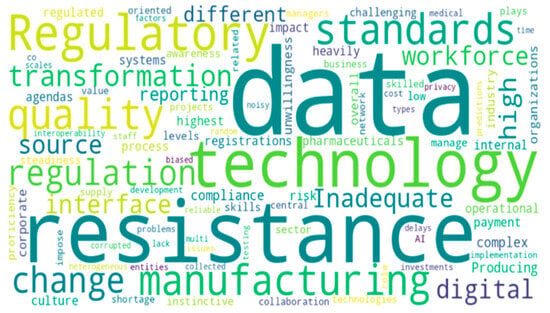
Figure 3.
Themes for barriers to digital transformation of healthcare enterprises.
Descriptive analysis in the Table 1 highlights unwillingness to change due to human factors and the broader impact of changes due to regulatory compliance are the key factors which might be considered proactively to strategize for digital transformation change management [2]. Additionally, inadequate workforce skills and insufficient funding are critical barriers which might be resolved through outsourcing skills and setting innovative community funding e.g., crowdsourcing mechanisms. Increased interest in data usage and the use of BI systems that enable the use of organizational data isolated in operational systems has been highlighted in some studies [34]. Studies have also mentioned the inadequate collaboration between information technology (IT) and operational technology (OT) systems as a key barrier that can be resolved by aligning digital transformation initiatives to foster collaboration between IT and OT [35]. Cloud computing systems, the business intelligence, and virtualization of individual workspaces enable the resolution of this barrier and foster IT and OT collaboration [36].

Table 1.
Descriptive analysis for key themes for barriers to digital transformation of healthcare enterprises.
Table 1.
Descriptive analysis for key themes for barriers to digital transformation of healthcare enterprises.
| Key Themes | Descriptive Analysis | References |
|---|---|---|
| Regulatory compliance | “Producing complex pharmaceuticals is not just a matter of building the required production line or hardware. It also involves a complex manufacturing process, a large team of experts, more time, many detailed steps, and the right regulatory registrations and all of this against the high quality and regulatory standards.” “Researchers have identified the important role of regulation. As the health-care industry is heavily regulated by the government, changes in regulation, especially to payment systems, tend to have a big impact.” | [24,29,37,38] |
| Data quality | “Besides random factors, the data quality in healthcare services could be low due to lack of testing, delays in reporting, different reporting standards, lack of data interoperability between different healthcare data systems.” | [2,30,38] |
| Resistance to change | “Researchers identified organizations’ overall resistance to change as their top operational risk. They are increasingly concerned about their organizations’ unwillingness to change business models and alter core operations in response to dynamic business environments.” | [1,12,38] |
| Inadequate workforce skills | “The issue of inadequate skills and low awareness levels of individuals to manage technology is one of the significant challenges. Especially in the health care and medical device manufacturing sector wherein the proficiency of persons in digital technologies is relatively low.” | [26,33] |
4.2. Digital Transformation Enablers for Healthcare Enterprises
Effective change management is the most important enabler for successful digital transformation. Digital transformation is a major change, and top leadership acting as a change agent is a key theme and an enabler for digital transformation of healthcare enterprises [12]. The two behavioral capacities, which are collaborative visioning and evidence-based improvisation [39], are highlighted as key traits for effective leadership for digital transformation. A study conducted by [40] identified multiple factors, specifically IT competence and experience of workforce with information systems, as success factors for digital transformation. Data interoperability of healthcare systems decreases the ability to obtain and evaluate vast amounts of data and leads to data quality issues [41]. Information technology (IT) and operational technology integration is another key enabler which enables connection between planning and control systems [39]. Transparency is critical for the process-related procedures to systematically identify gaps and potential. Therefore, adequate collaboration between IT and OT is essential [42]. Information technology and operation technology collaboration enables organizations to implement advanced digital solutions like the IoT, cloud computing, and AI-driven automation as highlighted in the descriptive analysis in the Table 2. This improves adaptability to market volatility, supports scalable infrastructure, and accelerates digital transformation [43]. Crowd funding, particularly through platforms like Kickstarter or GoFundMe, serves as a vital tool for early-stage financing, reducing development cycles for healthcare innovations, increasing market validation, and fostering innovation [43]. It allows startups and researchers to bypass traditional funding hurdles, accelerating the implementation of digital solutions such as AI diagnostics, wearable health monitors, and blockchain-based patient data management systems [44].
The word cloud in Figure 4 highlights the key themes for enablers to digital transformation, which are change management, leadership as change agent, IT and OT integration, and IT competence of employees.

Figure 4.
Themes for enablers to digital transformation of healthcare enterprises.

Table 2.
Descriptive analysis for key themes for enablers to digital transformation of healthcare enterprises.
Table 2.
Descriptive analysis for key themes for enablers to digital transformation of healthcare enterprises.
| Key Themes | Descriptive Analysis | References |
|---|---|---|
| Change management | “This is perhaps the most crucial phase, as mismanagement here would be catastrophic to the business. Change management is a collective term for all approaches to prepare, support and help individuals, teams, and organizations in making organizational changes.” | [4,26,34] [4,26,34] |
| Leadership as change agent IT and OT integration Innovation culture and crowdsourcing IT competence of employees | “With regard to the bottom-up approach, the adoption of two behavioral capacities, collaborative visioning and evidence-based improvisation. Leaders should try to achieve quick wins to keep staff motivated.” “Research demonstrates that leaders’ own technology awareness is not a significant factor. This finding is not surprising, given that the leader’s main responsibility is to set the strategic direction and that he or she can rely on technically competent staff to advise and drive the ODT process. ” “Process Management is the connecting element between the company and IT. It effectively and efficiently promotes business-IT alignment by acting as a neutral language that mediates between the two worlds. In the context of digital transformation, transparency must prevail over the process-related procedures in the company to systematically identify weaknesses and potentials.” “The measure “IT/OT integration” enables the connection of machines with planning and control systems. ” “The measure “Innovation Community” leads to better solutions and innovations like a proprietary product development. Innovation Community is a group of people with a sense of belonging and a collective identity who are jointly facilitating innovation.” “The research report medical crowdfunding could be a complementary solution to reduce bankruptcy, if governmental authorities take measures that enable disadvantaged populations to purposefully engage with digital platforms.” “The measure “IT competence of the employees” ensures that employees find their way in the digital age, even in companies affected by change.” “IT competencies are becoming increasingly important as the use of digital technologies are increasing even in the fields of patient care activities that were manual in the past.” | [4,35,45] [26,40,46] [26,43,44] [35,39,40] |
4.3. Key Disruption Scenarios for Healthcare Enterprises
The COVID 19 pandemic, a big disruption faced by the world, resulted in multiple scenarios [26,47,48]. A study conducted by [49] highlighted that the pandemic exacerbated panic buying and therefore demand surges in certain products, causing severe supply chain disruption as a key disruption scenario highlighted in Figure 5. The main supply chain problems cited in the study [49] were flexible manufacturing, inventory management, production quality, and procurement cost optimization. Supply chain disruptions during the COVID-19 pandemic delayed critical medical equipment deliveries, impacting hospitals’ ability to perform procedures. Digitization of supply chain management through IoT tracking and real-time analytics helps healthcare providers to proactively manage risks and maintain service continuity. Internet connectivity issues and cybersecurity threats are cited as potential disruption scenarios [26,50]. Therefore, strong cybersecurity measures are needed to protect patient information with clear policies to ensure safe and equitable use of AI [51]. Cyberattacks like the WannaCry ransomware attack have shut down hospital systems, delaying critical medical procedures and patient care. Emerging zero-trust security models, which require continuous verification of users and devices before granting access, minimize cyber threats as highlighted in descriptive analysis in Table 3. A proactive approach to cybersecurity, including AI-driven real-time threat detection, encrypted data transfers, and strict access controls, is critical to maintaining trust in digital healthcare systems [52].
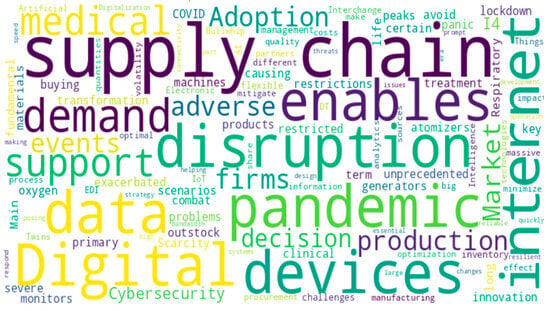
Figure 5.
Themes for disruption scenarios of healthcare enterprises.

Table 3.
Descriptive analysis for key themes for disruption scenarios.
Table 3.
Descriptive analysis for key themes for disruption scenarios.
| Key Themes | Descriptive Analysis | References |
|---|---|---|
| Pandemics (COVID-19) | “Since the pandemic has exacerbated panic buying and unprecedented peaks of demand in certain products, causing severe supply chain problems. In these circumstances, digital transformation and innovation in supply chains have been fundamental to avoid long-term outstock.” “Respiratory support devices such as life-support machines, oxygen generators, atomizers, and monitors are the primary clinical treatment medical devices to combat the pandemic. Thus, from diagnosis to cure, the necessity for medical devices and life-support systems is on the increasing trend. However, the scarcity of key materials and the lockdown restrictions have restricted the production of medical devices.” | [21,26,31] |
| Supply chain disruption | “Main challenges related to supply chain disruption are inventory management, flexible manufacturing, quality production and procurement costs optimization.” “Literature has demonstrated that the adoption of digital technologies such as Electronic Data Interchange (EDI), Artificial Intelligence (AI), Digital Twins (DT) and Internet of Things (IoT) enables supply chain partners to share information and help firms in decision making mitigating the “Bullwhip effect.” “The adoption of big data analytics enables firms to process massive quantities of data from different sources and helps firms to make optimal decisions to minimize the impact of adverse events. Therefore, firms that implement digitalization tend to be more resilient to adverse events. Second, digitalization enables prompt decision making, which helps firms to quickly respond to market changes.” “Cyber-security could turn out to be an essential part of the strategy, design and development, and operations in the I4.0 era. Also, I4.0 systems demand reliable high-speed internet with a large bandwidth, which poses internet connectivity issues during cybersecurity disruptions.” “Healthcare companies are starting to use AI technologies for cybersecurity and to protect sensitive patient data”. | [2,26,34] |
| Market volatility | [26,47,48] | |
| Cybersecurity threats | [50,51,52] |
4.4. Digital Transformation Use Cases for Healthcare Enterprises
Digital-twin technology creates a bridge between the physical and digital world enhancing real-time information sharing. The visibility on understanding past and current processes through digital twins helps to make predictions for capacity planning much quicker and in real time [53]. Digital twins are the most-cited technology with use cases as highlighted in the Figure 6, in operations improvement (high patient demand, increasing wait times, and resource management) and patient care (treatment prediction and trauma management) [54]. A study conducted by [55] used AI-driven digital twins for cancer patient care where digital twins assisted in creating individualized treatment models, predicting disease progression, and optimizing therapy selection. Another study conducted by [56] highlighted artificial intelligence-based approaches for predictive analytics, enhancing clinical trial efficiency by 30% and fostering treatment personalization. Artificial intelligence (AI)-enabled technologies result in enhanced connectivity, transparency, and visibility which further increases the reactivity and resiliency of complex global healthcare supply networks [33]. Smart medical device manufacturing-based use cases of AI-enabled technologies; specifically, processing automation, robotics, driverless trucks, and automated guided vehicles help to achieve social distancing with minimal impact on the factory output and efficiency [57]. Internet of things (IoT)-based AI-powered devices can be used to continuously track patient health metrics for real-time patient monitoring systems and enabling predictive analytics for personalized medicine as highlighted in the descriptive analysis in the Table 4. Augmented reality-based systems can enhance medical training, patient engagement, and remote diagnostics [51]. Augmented reality enables the use of real-time information which can be used to help decision-makers perform complex surgeries.
Figure 6.
Themes for digital transformation use cases of healthcare enterprises.

Table 4.
Descriptive analysis for digital transformation use cases.
Table 4.
Descriptive analysis for digital transformation use cases.
| Key Themes | Descriptive Analysis | References |
|---|---|---|
| Digital twins | “Digital twins originated from manufacturing is proposed for healthcare to enhance clinical decision-making and personalized patient care.” | [53,54,55] |
Artificial intelligence (AI) Internet of Things (IoT) Augmented reality (AR) | “The integration of digital twins with AI can process heterogeneous data which is a challenge improving diagnosis, treatment planning and patient outcomes.” “AI/ML can accelerate new drug discovery by improving and reducing virtual screening cycle times by 40%. AI enhances real time pandemic response and clinical trial optimization.” “AI driven cell and gene therapy is emerging trend for personalized medicine.” “IoT sensors and edge computing devices helps to develop interconnected healthcare systems connecting hospital equipment with patient monitoring systems enabling real time health tracking and data analytics for telemedicine.” “Augmented reality enhances medical training and reduces training time by 50%. Further AR enhances patient engagement and remote diagnostics reducing administrative burden and costs.” | [33,55,56] [51,55,57] [51,57] |
5. Discussion
Digital transformation in healthcare is a multifaceted process influenced by the interplay of disruption scenarios, organizational barriers, enabling factors, and technological use cases. Disruption scenarios such as market volatility, supply chain disruption, and cybersecurity threats are the key catalytic scenarios that necessitate transformation. For instance, market volatility can lead to demand surges or declines, impacting capacity planning and inventory management [21,58]. Supply chain disruptions challenge procurement processes and manufacturing stability, while cybersecurity threats underscore the need for robust data-protection measures [26,59]. Agility in production schedules, alternative sources of supply, and enhanced inbound materials visibility with AI/ML-integrated forecasting and supply chain simulations are some potential strategies for mitigating the supply chain disruption risks [60,61]. This finding resonates with previous studies [53,62] where enhancing big data analytics and processing capability of healthcare enterprises mitigates risks associated with supply chain disruption. Digital transformation enhances information processing capability and operational efficiency through robust cross-departmental collaboration between information technology (IT) and business processes. Organizational barriers, including regulatory compliance issues, data quality concerns, resistance to change, and inadequate technical workforce skills, can impede the effective response to these disruptions. A study [33] highlighted that poor data quality results in duplicate patient records and missing information, leading to fragmented patient histories. This issue hampers decision-making and increases redundant testing, which raises healthcare costs and risks for patients. Enablers such as leadership commitment, effective change management, and collaboration between information technology (IT) and operational technology (OT) are critical for overcoming the barriers. Leadership that fosters a collaborative vision and strategizes for evidence-based improvements can drive successful digital transformation [8]. Moreover, entrepreneurial mindsets and comprehensive knowledge of digital technologies among leaders facilitate the adoption of innovative solutions [12]. A study conducted by [10] supports this finding and highlights that 32 % of digitally transformed companies establish effective external relationships or partnerships through innovation funding.
Cybersecurity threats are critical, and including cybersecurity assessment and prevention strategies to the digital transformation roadmap of an enterprises is an important strategy to adopt. IT technical experts in cybersecurity threat detection and artificial intelligence/machine learning, combined with operations and process-improvement skills can help mitigate risks and ensure resilience for healthcare enterprises [63]. Technological use cases, as highlighted in this study, including AI, digital twins, the Internet of Things (IoT), and augmented reality (AR), provide practical applications to address specific challenges posed by disruption scenarios [9,54]. For instance, AI and predictive analytics can enhance capacity planning and patient care while digital twins can improve operational efficiency and interoperability between IT and OT systems [9]. These technologies, when effectively implemented, can mitigate risks associated with supply chain disruptions and cybersecurity threats. Cloud computing and agile project management online tools like Asana and JIRA can enhance collaboration between IT and OT, which is important for ensuring successful digital transformation [64].
Integrating these constructs into a cohesive theoretical framework highlights the causal mechanisms and interdependencies that drive digital transformation in healthcare. Disruption scenarios create pressures that necessitate change; organizational barriers can hinder or moderate the effectiveness of enabling factors; enablers facilitate the adoption of technological solutions; and use cases operationalize these technologies to achieve transformation outcomes. This integrated approach aligns with [65], that theoretical advancement requires not just identifying constructs, but also elucidating the relationships between them.
6. Conclusions
Emerging technologies, specifically digital twins (DTs), artificial intelligence (AI), and the Internet of Things (IoT) can be used to foster information technology (IT) and operational technology (OT) integration. Predictive analytics, capacity planning, workforce training, real-time patient monitoring, engagement, and cybersecurity threat mitigation are key use cases identified for digital transformation of healthcare enterprises. This is an important finding as it might help c-level and digital transformation executives to develop business cases for their digital transformation roadmap. Supply chain disruption, cybersecurity threats, and market volatility are the key themes identified for disruption scenarios. Emerging technologies like digital twins, AI, the IoT, and augmented reality can be used to mitigate the impact of disruption scenarios and this study will help to develop use cases and test cases. This study will also inform healthcare enterprises towards building resilient global supply chains and accelerating towards their digital transformation journey.
Effective change management, leadership as a change agent, collaboration between IT and OT, and workforce technology skills enablement are identified as the key themes for enablers of digital transformation. This finding is crucial for workforce training, change management, and sustaining digital transformation culture. Digital transformation leadership should possess collaborative, use-case driven, and evidence-based vision for digital transformation of their enterprises, as highlighted in this study.
Resistance to change, regulatory compliance, inadequate workforce skills, and poor collaboration between IT and OT are the key themes for barriers to digital transformation. This study might provide a starting point for healthcare enterprises to develop and define digital transformation goals. How to define digital transformation in the context of your enterprise and develop change initiatives are key questions which this research might help to explore. The findings from this study are qualitative and based on secondary research using structured literature review methodology, and need empirical evidence. The findings of this study are general for different types of healthcare enterprises and do not specifically explore variations in the factors of digital transformation with the size (small, medium, or larger) or type (medical device manufacturing, therapeutics, or patient care) of the enterprise. Future research work might help to validate the themes identified from this study with a survey and empirical evidence exploring variation in the factors for digital transformation among different types of healthcare enterprises. Developing the business case for digital transformation using the use cases mentioned in this study might help to test these cases and understand the potential tangible implications of implementing digital transformation initiatives. Capacity planning, patient care, and workforce training to mitigate potential risks during future disruption scenarios is another important implication of this study.
Author Contributions
Conceptualization, G.S.H. and D.R.; methodology, G.S.H.; validation, D.R., C.L., and G.S.H.; formal analysis, G.S.H.; investigation, G.S.H.; resources, G.S.H., C.L., and D.R.; writing—original draft preparation, G.S.H.; writing—review and editing, C.L. and D.R.; visualization, G.S.H.; supervision, D.R. and C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Narula, S.; Kumar, A.; Prakash, S.; Dwivedy, M.; Puppala, H.; Talwar, V. Modeling and analysis of challenges for industry 4.0 implementation in medical device industry to post COVID-19 scenario. Int. J. Supply Oper. Manag. 2021, 10, 117–135. [Google Scholar]
- Gudergan, G.; Mugge, P. The gap between practice and theory of digital transformation. In Proceedings of the Hawaii International Conference of System Science, Hilton Waikoloa Village, HI, USA, 4–7 January 2017; pp. 1–15. [Google Scholar]
- Zhang, J.; Qi, L. Crisis preparedness of healthcare manufacturing firms during the COVID-19 outbreak: Digitalization and servitization. Int. J. Environ. Res. Public Health 2021, 18, 5456. [Google Scholar] [CrossRef] [PubMed]
- Kraus, S.; Schiavone, F.; Pluzhnikova, A.; Invernizzi, A.C. Digital transformation in healthcare: Analyzing the current state-of-research. J. Bus. Res. 2021, 123, 557–567. [Google Scholar] [CrossRef]
- Mariomontag. Why Are Digital Transformation Failure Rates so High? My Two Cents from Battle Field Scars, Mario Montag. 2024. Available online: https://mariomontag.com/why-are-digital-transformation-failure-rates-so-high-my-two-cents-from-battle-field-scars/ (accessed on 2 January 2025).
- Aguiar, T.; Gomes, S.B.; da Cunha, P.R.; da Silva, M.M. Digital transformation capability maturity model framework. In Proceedings of the 2019 IEEE 23rd International Enterprise Distributed Object Computing Conference (EDOC), Paris, France, 28–31 October 2019; IEEE: New York, NY, USA, 2019; pp. 51–57. [Google Scholar]
- Mauro, M.; Noto, G.; Prenestini, A.; Sarto, F. Digital transformation in healthcare: Assessing the role of digital technologies for managerial support processes. Technol. Forecast. Soc. Change 2024, 209, 123781. [Google Scholar] [CrossRef]
- Brommeyer, M.; Whittaker, M.; Liang, Z. Organizational Factors Driving the Realization of Digital Health Transformation Benefits from Health Service Managers: A Qualitative Study. J. Healthc. Leadersh. 2024, 16, 455–472. [Google Scholar] [CrossRef]
- Channi, H.K.; Shrivastava, P.; Chowdhary, C.L. Digital transformation in healthcare industry: A survey. In Next Generation Healthcare Informatics; Springer Nature: Singapore, 2022; pp. 279–293. [Google Scholar]
- Kane, G.C.; Palmer, D.; Phillips, A.N. Achieving digital maturity. MIT Sloan Manag. Rev. 2017, 59. [Google Scholar]
- Fitzgerald, M.; Kruschwitz, N.; Bonnet, D.; Welch, M. Embracing digital technology: A new strategic imperative. MIT Sloan Manag. Rev. 2014, 55, 1. [Google Scholar]
- Mugge, P.; Abbu, H.; Michaelis, T.L.; Kwiatkowski, A.; Gudergan, G. Patterns of digitization: A practical guide to digital transformation. Res.-Technol. Manag. 2020, 63, 27–35. [Google Scholar] [CrossRef]
- Kitsios, F.; Kapetaneas, N. Digital Transformation in Healthcare 4.0: Critical Factors for Business Intelligence Systems. Information 2022, 13, 247. [Google Scholar] [CrossRef]
- Iyanna, S.; Kaur, P.; Ractham, P.; Talwar, S.; Islam, A.N. Digital transformation of healthcare sector. What is impeding adoption and continued usage of technology-driven innovations by end-users? J. Bus. Res. 2022, 153, 150–161. [Google Scholar] [CrossRef]
- Yeoh, W.; Koronios, A. Critical success factors for business intelligence systems. J. Comput. Inf. Syst. 2010, 50, 23–32. [Google Scholar] [CrossRef]
- Olszak, C.M.; Ziemba, E. Critical success factors for implementing business intelligence systems in small and medium enterprises on the example of upper Silesia, Poland. Interdiscip. J. Inf. Knowl. Manag. 2012, 7, 129–150. [Google Scholar] [CrossRef]
- Dawson, L.; Van Belle, J.P. Critical success factors in South African Business intelligence projects in the insurance industry. In Refereed Proceedings Knowledge Management Conference, Novi Sad, Serbia, 26–28 June 2013; International Institute for Applied Knowledge Management: Aventura, FL, USA, 2013; pp. 65–74. [Google Scholar]
- Lin, T.C.; Sheng, M.L.; Jeng Wang, K. Dynamic capabilities for smart manufacturing transformation by manufacturing enterprises. Asian J. Technol. Innov. 2020, 28, 403–426. [Google Scholar] [CrossRef]
- Sokolov, M. Decision making and risk management in biopharmaceutical engineering—Opportunities in the age of covid-19 and digitalization. Ind. Eng. Chem. Res. 2020, 59, 17587–17592. [Google Scholar] [CrossRef]
- Shaw, B.; Chisholm, O. Creeping through the backdoor: Disruption in medicine and health. Front. Pharmacol. 2020, 11, 818. [Google Scholar] [CrossRef]
- Fang, I.C.; Chen, P.T.; Chiu, H.H.; Lin, C.L.; Su, F.C. Med-tech industry entry strategy analysis under COVID-19 impact. Healthcare 2020, 8, 431. [Google Scholar] [CrossRef]
- NetSuite.com. Top Industry Challenges for Healthcare, Oracle NetSuite. 2024. Available online: https://www.netsuite.com/portal/resource/articles/erp/healthcare-industry-challenges.shtml (accessed on 2 January 2025).
- Mayring, P. Qualitative content analysis: Theoretical foundation, basic procedures and software solution. In Approaches to Qualitative Research in Mathematics Education; Springer: Dordrecht, The Netherlands, 2014. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Sivakumar, P.S. Content Analysis, Thematic Analysis and Hands-on session with NVIVO. Adv. Res. Methodol. Soc. Sci. 2020, 57, 101–118. [Google Scholar]
- Berelson, B. Content Analysis in Communication Research; Free Press: New York, NY, USA, 1952. [Google Scholar]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Medica 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Berman, S.J. Digital transformation: Opportunities to create new business models. Strategy Leadersh. 2012, 40, 16–24. [Google Scholar] [CrossRef]
- Pasupuleti, M.B.; Adusumalli, H.P. Digital Transformation of the High-Technology Manufacturing: An Overview of Main Blockades. Am. J. Trade Policy 2018, 5, 139–142. [Google Scholar]
- Lopes, J.; Braga, J.; Santos, M.F. Adaptive Business Intelligence platform and its contribution as a support in the evolution of Hospital 4.0. Procedia Comput. Sci. 2021, 184, 905–910. [Google Scholar] [CrossRef]
- Bhartiya, S.; Mehrotra, D. Exploring interoperability approaches and challenges in healthcare data exchange. In Smart Health, Proceedings of the International Conference, ICSH 2013, Beijing, China, 3–4 August 2013; Springer: Berlin/Heidelberg, Germany, 2013; pp. 52–65. [Google Scholar]
- O’Sullivan, C.; Rutten, P.; Schatz, C. Why Tech Transfer May Be Critical to Beating COVID-19; McKinsey & Company: New York, NY, USA, 2020. [Google Scholar]
- Gargalo, C.L.; Heras, S.C.D.L.; Jones, M.N.; Udugama, I.; Mansouri, S.S.; Krühne, U.; Gernaey, K.V. Towards the development of digital twins for the bio-manufacturing industry. Adv. Biochem. Eng. Biotechnol. 2021, 176, 1–34. [Google Scholar]
- Rogers, D.L. The Digital Transformation Playbook: Rethink your Business for the Digital Age; Columbia University Press: New York, NY, USA, 2016. [Google Scholar]
- Ali, M.S.; Miah, S.J. Identifying organizational factors for successful business intelligence implementation. Int. J. Bus. Intell. Res. 2018, 9, 47–63. [Google Scholar] [CrossRef]
- Kitsios, F.; Kamariotou, M. Artificial intelligence and business strategy towards digital transformation: A research agenda. Sustainability 2021, 13, 2025. [Google Scholar] [CrossRef]
- Wuest, T.; Kusiak, A.; Dai, T.; Tayur, S.R. Impact of COVID-19 on manufacturing and supply networks—The case for AI-inspired digital transformation. SSRN 2020. SSRN 3593540. [Google Scholar] [CrossRef]
- Butt, J. A conceptual framework to support digital transformation in manufacturing using an integrated business process management approach. Designs 2020, 4, 17. [Google Scholar] [CrossRef]
- Brettel, M.; Friederichsen, N.; Keller, M.; Rosenberg, M. How virtualization, decentralization, and network building change the manufacturing landscape: An Industry 4.0 Perspective. Int. J. Mech. Ind. Sci. Eng. 2014, 8, 37–44. [Google Scholar]
- Stich, V.; Zeller, V.; Hicking, J.; Kraut, A. Measures for a successful digital transformation of SMEs. Procedia CIRP 2020, 93, 286–291. [Google Scholar] [CrossRef]
- Yeoh, W.; Koronios, A.; Gao, J. Managing the implementation of business intelligence systems: Acritical success factors framework. Int. J. Enterp. Inf. Syst. 2008, 4, 79–94. [Google Scholar] [CrossRef]
- Shen, C.C.; Chang, R.E.; Hsu, C.J.; Chang, I.C. How business intelligence maturity enabling hospital agility. Telemat. Inform. 2017, 34, 450–456. [Google Scholar] [CrossRef]
- Kruszyńska-Fischbach, A.; Sysko-Romańczuk, S.; Rafalik, M.; Walczak, R.; Kludacz-Alessandri, M. Organizational E-Readiness for the Digital Transformation of Primary Healthcare Providers during the COVID-19 Pandemic in Poland. J. Clin. Med. 2021, 11, 133. [Google Scholar] [CrossRef]
- da Cunha, M.A.O.; Santos, H.F.; de Carvalho, M.E.L.; Miranda, G.M.D.; de Albuquerque, M.D.S.V.; de Oliveira, R.S.; de Albuquerque, A.F.C.; Penn-Kekana, L.; Kuper, H.; Lyra, T.M. Health care for people with disabilities in the Unified Health System in Brazil: A scoping review. Int. J. Environ. Res. Public Health 2022, 19, 1472. [Google Scholar] [CrossRef] [PubMed]
- Kasoju, N.; Remya, N.S.; Sasi, R.; Sujesh, S.; Soman, B.; Kesavadas, C.; Muraleedharan, C.V.; Varma, P.R.H.; Behari, S. Digital health: Trends, opportunities and challenges in medical devices, pharma and bio-technology. CSI Trans. ICT 2023, 11, 11–30. [Google Scholar] [CrossRef]
- Mhlungu, N.S.; Chen, J.Y.; Alkema, P. The underlying factors of successful organizational digital transformation. S. Afr. J. Inf. Manag. 2019, 21, 10. [Google Scholar] [CrossRef]
- Pirbhulal, S.; Chockalingam, S.; Abie, H.; Lau, N. Cognitive digital twins for improving security in IT-OT enabled healthcare applications. In HCI for Cybersecurity, Privacy and Trust, Proceedings of the International Conference on Human-Computer Interaction, Washington DC, USA, 25–26 June 2025; Springer Nature: Cham, Switzerland, 2024; pp. 153–163. [Google Scholar]
- Ranney, M.L.; Griffeth, V.; Jha, A.K. Critical supply shortages—The need for ventilators and personal protective equipment during the Covid-19 pandemic. N. Engl. J. Med. 2020, 382, e41. [Google Scholar] [CrossRef] [PubMed]
- Livingston, E.; Desai, A.; Berkwits, M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA 2020, 323, 1912–1914. [Google Scholar] [CrossRef]
- Soto-Acosta, P. COVID-19 pandemic: Shifting digital transformation to a high-speed gear. Inf. Syst. Manag. 2020, 37, 260–266. [Google Scholar] [CrossRef]
- Motjolopane, I.; Chanza, M. Digital transformation dimensions for evaluating SMEs’ readiness for big data analytics and artificial intelligence: A review. Int. J. Res. Bus. Soc. Sci. 2023, 12, 583–595. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Medical 4.0 technologies for healthcare: Features, capabilities, and applications. Internet Things Cyber-Phys. Syst. 2022, 2, 12–30. [Google Scholar] [CrossRef]
- Ehrenfeld, J.M. Wannacry, cybersecurity and health information technology: A time to act. J. Med. Syst. 2017, 41, 104. [Google Scholar] [CrossRef] [PubMed]
- Erol, T.; Mendi, A.F.; Doğan, D. The digital twin revolution in healthcare. In Proceedings of the 2020 4th International Symposium on Multidisciplinary Studies and Innovative Technologies (ISMSIT), Istanbul, Turkey, 22–24 October 2020; IEEE: New York, NY, USA, 2020; pp. 1–7. [Google Scholar]
- Elayan, H.; Aloqaily, M.; Guizani, M. Digital twin for intelligent context-aware IoT healthcare systems. IEEE Internet Things J. 2021, 8, 16749–16757. [Google Scholar] [CrossRef]
- Kaul, R.; Ossai, C.; Forkan, A.R.M.; Jayaraman, P.P.; Zelcer, J.; Vaughan, S.; Wickramasinghe, N. The role of AI for developing digital twins in healthcare: The case of cancer care. Wiley Interdiscip. Rev. Data Min. Knowl. Discov. 2023, 13, e1480. [Google Scholar] [CrossRef]
- Chavda, V.P.; Anand, K.; Apostolopoulos, V. (Eds.) Bioinformatics Tools for Pharmaceutical Drug Product Development; John Wiley & Sons: Hoboken, NJ, USA, 2023. [Google Scholar]
- Kusiak, A. Predictive models in digital manufacturing: Research, applications, and future outlook. Int. J. Prod. Res. 2023, 61, 6052–6062. [Google Scholar] [CrossRef]
- Hess, T.; Matt, C.; Benlian, A.; Wiesböck, F. Options for formulating a digital transformation strategy. In Strategic Information Management; Routledge: New York, NY, USA, 2020; pp. 151–173. [Google Scholar]
- Ivanov, D.; Dolgui, A.; Sokolov, B. The impact of digital technology and Industry 4.0 on the ripple effect and supply chain risk analytics. Int. J. Prod. Res. 2019, 57, 829–846. [Google Scholar] [CrossRef]
- Kilpatrick, J.; Barter, L. COVID-19: Managing Supply Chain Risk and Disruption; Deloitte: Toronto, ON, Canada, 2020. [Google Scholar]
- Zavala-Alcívar, A.; Verdecho, M.J.; Alfaro-Saiz, J.J. A conceptual framework to manage resilience and increase sustainability in the supply chain. Sustainability 2020, 12, 6300. [Google Scholar] [CrossRef]
- Scharff, S. From Digital Twin to Improved Patient Experience; Siemens Healthineers: Victoria, Australia, 2010. [Google Scholar]
- Gudergan, G.; Buschmeyer, A. Key aspects of strategy and leadership for business transformation. Bus. Transform. J. 2014, 11, 17–27. [Google Scholar]
- Burton-Jones, A.; Recker, J.; Indulska, M.; Green, P.; Weber, R. Assessing representation theory with a framework for pursuing success and failure. MIS Q. 2017, 41, 1307–1333. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).