- Case Report
Successful Pregnancy in a Woman with a History of Löffler’s Endomyocarditis and Recurrent Ventricular Thrombosis: A Case Report and Literature Review
- Noriko Arakaki,
- Kaoru Kawasaki and
- Noriomi Matsumura
- + 3 authors
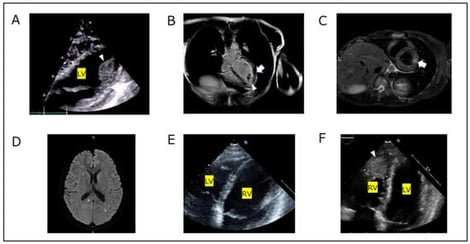
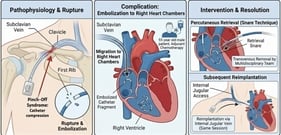
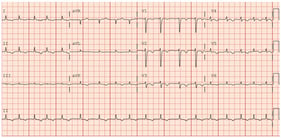
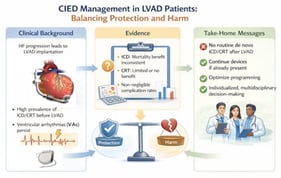
We present the case of a 27-year-old woman diagnosed with Löffler’s endomyocarditis complicated by intraventricular thrombus and cerebral infarction. She was treated with prednisolone and anticoagulation therapy; however, tapering of corticosteroids resulted in recurrence of intraventricular thrombosis. Given disease relapse after medication withdrawal, lifelong anticoagulation was indicated. At 29 years of age, she sought pregnancy counseling. Conception was permitted after stabilization of prednisolone dosage, with a planned switch from a vitamin K antagonist to therapeutic-dose unfractionated heparin during pregnancy. Following disease stabilization, she conceived via artificial insemination. Serial echocardiography at 22 and 34 weeks of gestation demonstrated preserved cardiac function without thrombus recurrence. She delivered a healthy infant by emergency cesarean section at 39 weeks of gestation due to fetal distress. No thrombus recurrence was observed postpartum, and she remained clinically stable during 13 months of follow-up. This represents the case of a successful pregnancy in a woman with a history of recurrent intraventricular thrombosis due to Löffler’s endomyocarditis, highlighting the importance of early diagnosis, sustained immunosuppression, individualized anticoagulation, and multidisciplinary preconception planning.
8 February 2026