Biventricular Takotsubo Cardiomyopathy Complicated with Cardiogenic Shock: A Postoperative Complication Following Non-Cardiac Surgery
Abstract
1. Introduction
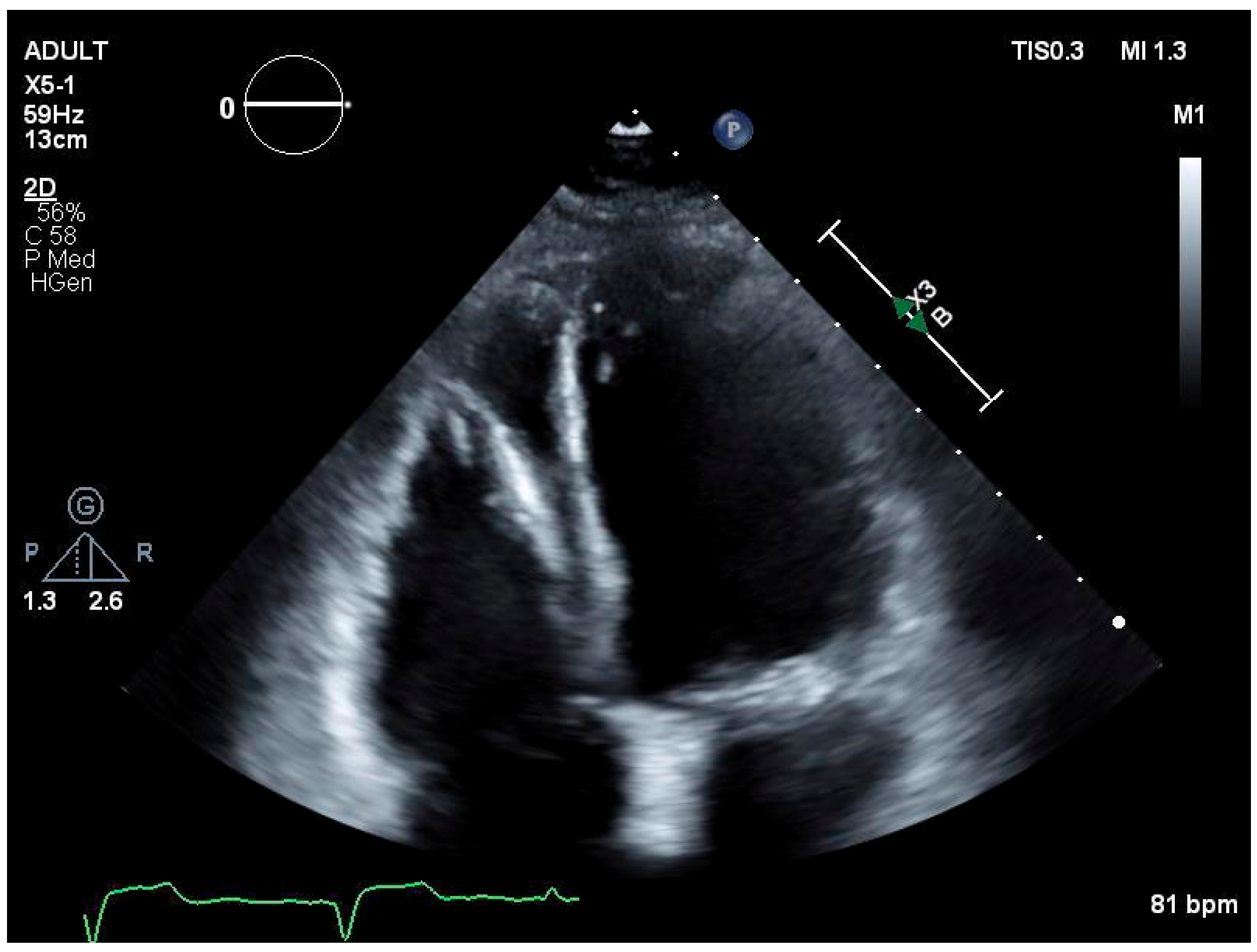
2. Clinical Presentation
2.1. Case History and Examination/Investigations
2.2. Treatment
2.3. Outcomes and Follow-Up
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lyon, A.R.; Bossone, E.; Schneider, B.; Sechtem, U.; Citro, R.; Underwood, S.R.; Sheppard, M.N.; Figtree, G.A.; Parodi, G.; Akashi, Y.J.; et al. Current state of knowledge on Takotsubo syndrome: A Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2016, 18, 8–27. [Google Scholar] [CrossRef] [PubMed]
- Amin, H.Z.; Amin, L.Z.; Pradipta, A. Takotsubo Cardiomyopathy: A Brief Review. J. Med. Life 2020, 13, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Padoan, L.; Sforna, S.; Parise, A.; Barengo, A.; Torlone, F.; Coiro, S.; Riccini, C.; Del Pinto, M.; Cavallini, C. 558 biventricular perioperative takotsubo cardiomiopathy. Eur. Heart J. Suppl. 2022, 24, suac121.568. [Google Scholar] [CrossRef]
- El-Battrawy, I.; Santoro, F.; Stiermaier, T.; Möller, C.; Guastafierro, F.; Novo, G.; Novo, S.; Mariano, E.; Romeo, F.; Romeo, F.; et al. Incidence and Clinical Impact of Right Ventricular Involvement (Biventricular Ballooning) in Takotsubo Syndrome. Chest 2021, 160, 1433–1441. [Google Scholar] [CrossRef] [PubMed]
- de Chazal, H.M.; Del Buono, M.G.; Keyser-Marcus, L.; Ma, L.; Moeller, F.G.; Berrocal, D.; Abbate, A. Stress Cardiomyopathy Diagnosis and Treatment. JACC 2018, 72, 1955–1971. [Google Scholar] [CrossRef] [PubMed]
- Uribarri, A.; Núñez-Gil, I.J.; Conty, D.A.; Vedia, O.; Almendro-Delia, M.; Cambra, A.D.; Martin-Garcia, A.C.; Barrionuevo-Sánchez, M.; Martínez-Sellés, M.; Raposeiras-Roubín, S.; et al. Short- and Long-Term Prognosis of Patients With Takotsubo Syndrome Based on Different Triggers: Importance of the Physical Nature. J. Am. Heart Assoc. 2019, 8, e013701. [Google Scholar] [CrossRef] [PubMed]
- Redfors, B.; Jha, S.; Thorleifsson, S.; Jernberg, T.; Angerås, O.; Frobert, O.; Petursson, P.; Tornvall, P.; Sarno, G.; Ekenbäck, C.; et al. Short- and Long-Term Clinical Outcomes for Patients With Takotsubo Syndrome and Patients With Myocardial Infarction: A Report From the Swedish Coronary Angiography and Angioplasty Registry. J. Am. Heart Assoc. 2021, 10, e017290. [Google Scholar] [CrossRef] [PubMed]
- Agewall, S.; Beltrame, J.F.; Reynolds, H.R.; Niessner, A.; Rosano, G.; Caforio, A.L.P.; De Caterina, R.; Zimarino, M.; Roffi, M.; Kjeldsen, K.; et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur. Heart J. 2016, 38, ehw149–153. [Google Scholar] [CrossRef] [PubMed]
- Gerbaud, E.; Arabucki, F.; Nivet, H.; Barbey, C.; Cetran, L.; Chassaing, S.; Seguy, B.; Lesimple, A.; Cochet, H.; Montaudon, M.; et al. OCT and CMR for the Diagnosis of Patients Presenting With MINOCA and Suspected Epicardial Causes. JACC: Cardiovasc. Imaging 2020, 13, 2619–2631. [Google Scholar] [CrossRef] [PubMed]
- Yalçin, F.; Cagatay, B.; Abraham, M.R.; Garcia, M.J. Stress Septal Sign (Triple S) Preexists in Hypertensive Hearts and Clarifies Critical Diagnostic Strategies. J. Clin. Med. 2025, 14, 6143. [Google Scholar] [CrossRef] [PubMed]
- Boyd, B.M.; Solh, T.M. Takotsubo cardiomyopathy. J. Am. Acad. Physician Assist. 2020, 33, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Pillitteri, M.; Brogi, E.; Piagnani, C.; Bozzetti, G.; Forfori, F. Perioperative management of Takotsubo cardiomyopathy: An overview. J. Anesth. Analg. Crit. Care 2024, 4, 1–15. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Rayamajhi, K.; Parul, F.; Khairy, M.; Rayamajhi, S.; Bandi, A. Biventricular Takotsubo Cardiomyopathy Complicated with Cardiogenic Shock: A Postoperative Complication Following Non-Cardiac Surgery. Hearts 2026, 7, 5. https://doi.org/10.3390/hearts7010005
Rayamajhi K, Parul F, Khairy M, Rayamajhi S, Bandi A. Biventricular Takotsubo Cardiomyopathy Complicated with Cardiogenic Shock: A Postoperative Complication Following Non-Cardiac Surgery. Hearts. 2026; 7(1):5. https://doi.org/10.3390/hearts7010005
Chicago/Turabian StyleRayamajhi, Karuna, Fnu Parul, Mahmoud Khairy, Sumugdha Rayamajhi, and Appa Bandi. 2026. "Biventricular Takotsubo Cardiomyopathy Complicated with Cardiogenic Shock: A Postoperative Complication Following Non-Cardiac Surgery" Hearts 7, no. 1: 5. https://doi.org/10.3390/hearts7010005
APA StyleRayamajhi, K., Parul, F., Khairy, M., Rayamajhi, S., & Bandi, A. (2026). Biventricular Takotsubo Cardiomyopathy Complicated with Cardiogenic Shock: A Postoperative Complication Following Non-Cardiac Surgery. Hearts, 7(1), 5. https://doi.org/10.3390/hearts7010005






