Pulmonary Vein Stenosis in Neonates and Infants: Etiology, Diagnosis and Management
A special issue of Children (ISSN 2227-9067). This special issue belongs to the section "Pediatric Pulmonary and Sleep Medicine".
Deadline for manuscript submissions: closed (30 April 2022) | Viewed by 58808
Special Issue Editor
Special Issue Information
Dear Colleagues,
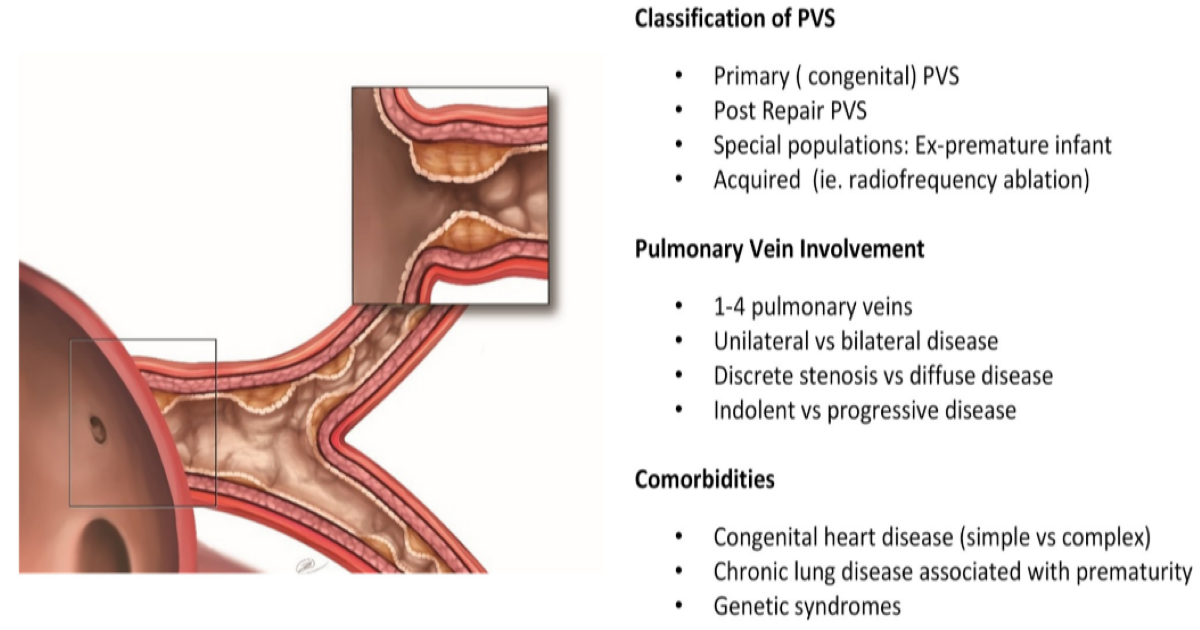
Progressive obliteration of the pulmonary vein lumen, known as pulmonary vein stenosis (PVS), is a rare condition that typically occurs in infants and very young children. PVS can be present at birth, but more commonly develops later in association with congenital heart disease or pulmonary conditions, especially in premature infants, and rarely in isolation. Unlike other congenital heart defects, a hallmark feature of the disease is the rapid recurrence of obstruction even after successful anatomic intervention. When PVS develops in multiple vessels, it rapidly leads to pulmonary edema, pulmonary hypertension, right heart failure, and infant death.
We now know that lumen obliteration occurs from overactivity of myofibroblast-like cells in the neointima of the pulmonary veins, though the inciting etiology is not known. Much progress has been made over the past decade to understand the biology of PVS, refine surgical and catheter-based treatment, reduce cellular activity, and improve survival, towards the elusive goal of PVS prevention.
This Special Issue focuses on the underlying biology that leads to PVS, a deeper understanding of how vessels are affected including pathophysiology and prognosis, diagnostic and treatment strategies, and long-term consequences for the new population of survivors. We welcome original articles and reviews that explore these issues from basic science, clinical, or epidemiologic perspectives. Exploratory papers with leading ideas about causal mechanisms are encouraged.
Codifying what is currently known about PVS, etiology, and treatment is an important step towards improving survival for the growing population of infants affected by this devastating disease.
Prof. Dr. Kathy J. Jenkins
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 250 words) can be sent to the Editorial Office for assessment.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Children is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2400 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- pulmonary vein stenosis
- myofibroblast
- congenital heart defect
- prematurity
- infant
Benefits of Publishing in a Special Issue
- Ease of navigation: Grouping papers by topic helps scholars navigate broad scope journals more efficiently.
- Greater discoverability: Special Issues support the reach and impact of scientific research. Articles in Special Issues are more discoverable and cited more frequently.
- Expansion of research network: Special Issues facilitate connections among authors, fostering scientific collaborations.
- External promotion: Articles in Special Issues are often promoted through the journal's social media, increasing their visibility.
- Reprint: MDPI Books provides the opportunity to republish successful Special Issues in book format, both online and in print.
Further information on MDPI's Special Issue policies can be found here.






