- Article
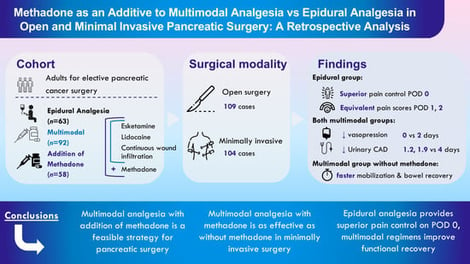
Methadone as an Additive to Multimodal Analgesia vs. Epidural Analgesia in Open and Minimal Invasive Pancreatic Surgery: A Retrospective Analysis
- Tom Pisters,
- Annemarie Akkermans and
- Harm J. Scholten
- + 2 authors
Background: Epidural analgesia (EA) is widely used in pancreatic surgery but is associated with hypotension and delayed recovery. The shift towards minimally invasive surgery has led to the exploration of alternative multimodal analgesia strategies. Methadone, with its unique pharmacological properties, may further optimize recovery. Methods: This retrospective cohort study included 213 patients undergoing pancreatic resection, receiving EA (n = 63), multimodal analgesia without methadone (MA; n = 92), or with methadone (MM; n = 58). MA and MM included intravenous ketamine, lidocaine and continuous wound infiltration. Primary outcome was maximum daily postoperative pain scores. Secondary outcomes included opioid consumption, vasopressor use, mobilization, bowel recovery, urinary catheter duration, and ICU/hospital stay. Results: Compared with EA, pain scores were slightly higher in MM (mean difference 2.22; 95% CI 1.22–3.90; p = 0.01) and in MA (mean difference 2.06; 95% CI 0.99–4.30; p = 0.06). Opioid use was comparable between MM and EA (OR 0.99, 95% CI [0.98, 1.00], p = 0.20), and significantly lower in MA (OR 0.97, 95% CI [0.96, 0.98], p < 0.001). Both MA and MM demonstrated reduced vasopressor requirements (both 0 vs. 2.0 median days) and shorter urinary catheterization durations (MA 1.2 MM 1.9 vs. EA 4.0 median days). MA improved mobilization (0 vs. 1 median days; OR 0.52, p = 0.03) and bowel recovery (OR 0.76, p = 0.02). ICU stay was longer in EA due to routine ICU admission for open surgery. Conclusions: Multimodal analgesia, with or without methadone, offers alternative strategies in pancreatic surgery. While EA provides superior pain control, multimodal regimens are associated with improved functional recovery.
22 January 2026