1. Introduction
Postoperative cognitive dysfunction (POCD) represents a major concern in the context of modern surgical care, particularly in elderly patients undergoing major procedures like thoracic surgery. The incidence of POCD can be as high as 40% in the immediate postoperative period, with a substantial portion of patients experiencing persistent deficits at 3 months [
1]. These cognitive impairments, which can manifest as memory loss, attention deficits, and language difficulties, are linked to prolonged hospital stays, reduced quality of life, and increased long-term morbidity.
One-lung ventilation (OLV), a cornerstone technique in thoracic surgery, presents a unique challenge to cerebral oxygenation. OLV can disrupt the delicate balance of gas exchange and ventilation-perfusion matching, leading to physiological changes that compromise cerebral oxygen delivery [
2]. Factors such as altered hemodynamics, surgical positioning in the lateral decubitus position, and changes in pulmonary vascular resistance can further reduce cerebral perfusion pressure [
2,
3,
4,
5]. This makes the brain particularly vulnerable to hypoxemia and desaturation during the procedure.
Near-infrared spectroscopy (NIRS) has emerged as a valuable tool for continuously and non-invasively monitoring regional cerebral oxygen saturation (rScO
2) [
6]. Unlike peripheral pulse oximetry (SpO
2), which measures systemic oxygenation, NIRS provides real-time feedback on the balance between oxygen supply and demand in the frontal cortex [
3], and early detection of decreased rScO2 enables timely interventions to optimize oxygenation, potentially preventing cerebral desaturation and reducing the risk of POCD [
7,
8,
9]. While NIRS monitoring is a well-established practice in cardiac surgery, its role in thoracic surgery remains relatively underexplored [
10]. Previous studies in non-cardiac surgery have shown a trend toward improved outcomes, including reduced cognitive decline and mortality, with NIRS-guided interventions [
11]. Interestingly, a trend towards benefit was seen across both surgery types, suggesting a potential wider applicability of NIRS [
1,
2,
11].
This study was designed as a prospective, observational pilot to investigate the use of NIRS in thoracic surgery from two perspectives. The first was to determine the relationship between intraoperative NIRS-measured cerebral oxygenation and arterial saturation in patients undergoing OLV for thoracic surgery. The second and primary objective was to investigate the association between intraoperative cerebral desaturation events and subsequent changes in postoperative neurocognitive function.
2. Materials and Methods
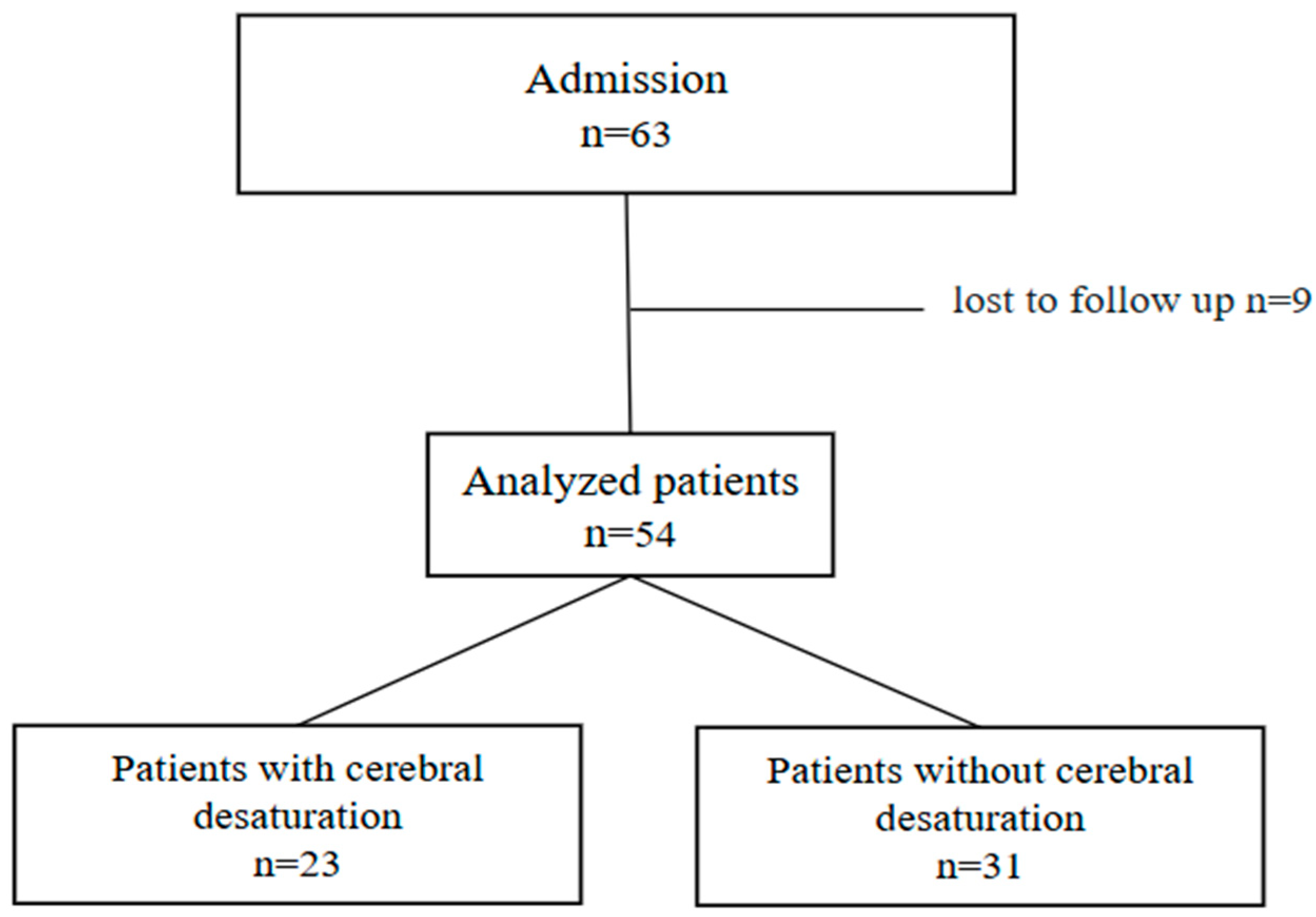
This prospective, observational pilot study was conducted from December 2016 to August 2018 at a university hospital. The study had ethical approval from the Istanbul University Istanbul Faculty of Medicine Clinical Research Ethics Committee (2017/1198), and all participants provided written informed consent. Inclusion criteria were patients aged 18 years or older with an ASA I–III classification, scheduled for a surgical procedure requiring one-lung ventilation. The exclusion criteria were determined as history of major psychiatric disease and dementia or any disease of the central nervous system (meningitis and encephalitis, brain tumors, neurodegenerative, inflammatory, cerebrovascular disease) according to medical records; prior neurosurgical, vascular or cardiac surgeries; drug or alcohol dependence; speech disturbances; vision and hearing impairment; inadequate use of native language; patient’s refusal to participate to the study; and lack of reading and writing skills.
2.1. Perioperative Management
Standard perioperative monitoring included electrocardiography, peripheral oxygen saturation (SpO2), invasive blood pressure monitoring, and temperature measurement. A standardized anesthesia protocol was used for all patients, consisting of induction with midazolam (0.03 mg/kg), fentanyl (2 mg/kg), propofol (2 mg/kg), and rocuronium (0.6 mg/kg). Anesthesia was maintained with sevoflurane (1 MAC) in a mixture of 60% oxygen and 40% air, and ventilation was controlled in pressure control mode.
During OLV, the inspired oxygen fraction (FiO2) was adjusted to maintain SpO2 above 92%. Peripheral desaturation was defined as SpO2 below 90% for longer than two minutes, prompting rescue maneuvers such as increasing FiO2, confirming tube position, and performing lung recruitment. Postoperative pain was managed with various techniques, including thoracic epidural catheters, paravertebral blocks, and intravenous analgesics.
2.2. Cerebral Oximetry Monitoring
Regional cerebral oxygen saturation (rScO2) was measured continuously using an INVOS 5100B™ cerebral oximeter (Somanetics Corp, Troy, MI, USA) with bilateral sensors placed on the forehead. Baseline rScO2 values were recorded while the patient was breathing room air, prior to sedation. Throughout the surgery, rScO2 values were recorded every 15 min.
Cerebral desaturation was defined as a reduction of 20% or more from baseline or an absolute value below 50% for at least 3 min. Patients were divided into two groups based on their intraoperative NIRS measurements: those who experienced cerebral desaturation were included in group D (desaturation), and those who rested in group N.
Upon detecting a desaturation event, a standardized protocol was initiated by the anesthesiologist to restore cerebral oxygenation, including:
Increasing FiO2.
Optimizing hemodynamics with vasopressors or fluids to maintain mean arterial pressure (MAP) above 65 mmHg.
Adjusting ventilation to maintain normocapnia.
Reposition the patient’s head to ensure adequate cerebral venous drainage.
The duration of each desaturation event and the time to recovery were recorded.
2.3. Neurocognitive Examination
Neurocognitive function was assessed using the Addenbrooke’s Cognitive Examination-Revised (ACE-R), a detailed battery that evaluates multiple cognitive domains, including attention, memory, fluency, language, and visuospatial abilities. This comprehensive test was chosen over general screening tools like the Mini-Mental State Examination (MMSE) to provide a more nuanced evaluation of specific cognitive deficits. Testing was performed by trained anesthesiologists under the supervision of a clinical neuropsychologist at three time points: preoperatively (baseline), on the 3rd postoperative day (early POCD), and at the 3rd month post-surgery (late POCD).
2.4. Study Definitions
Cerebral Desaturation: There is wide variation in the published cerebral oxygen desaturation criteria [
1]. Regional cerebral oxygen saturation (rSO
2) was defined as a reduction in regional saturation over a previously established time interval, as described by Slater et al. [
10]. The score accounts for both the depth and duration of desaturation and is calculated by the formula: rSO
2 score = 50% rSO
2—current rSO
2 (%) × time (seconds). A decrease of 20% or more compared to the baseline value, and all values below 50% of the baseline were considered abnormal.
Early and Late Postoperative Cognitive Dysfunction (POCD): Early postoperative cognitive dysfunction (Early-POCD) was defined as a decrease of more than 2 points from baseline in the neurocognitive test battery on the 3rd day after surgery, as detected by the ACE-R test. Late POCD was defined as a decrease of more than 2 points from baseline in the neurocognitive test battery in the 3rd month after surgery, also detected by the ACE-R test.
Postoperative Complications: As postoperative complications, we consider patients with pneumonia or respiratory failure, cardiac complications, bleeding complications, wound infection, pulmonary embolism, or deep vein thrombosis (DVT).
Hypotension is defined as mean arterial pressure (MAP) below 65 mmHg or systolic pressure below 90 mmHg. Hypotension was treated either with ephedrine or a fluid bolus according to the clinician’s decision; in case of persistent hypotension, noradrenaline infusion was initiated.
Peripheral Desaturation: Peripheral desaturation was defined as SpO2 below 90% for longer than 2 min, where we perform rescue maneuvers including increasing FiO2, confirming tube position, and performing lung recruitment maneuvers to raise SpO2; in case of failed maneuvers, two-lung ventilation was initiated.
2.5. Statistical Method
SPSS V22.0 was used for data analysis in this study. Descriptive statistics, including frequency, percentage, mean, standard deviation, minimum, and maximum, were employed to summarize the data. Parametric tests were used for data analysis, including an independent sample t-test for comparing the means of two independent groups, one-way ANOVA for comparing the means of more than two independent groups, a dependent sample t-test for comparing the means of two dependent groups, and repeated measures ANOVA for comparing the means of more than two dependent groups. The significance level for all tests was set at 0.05.
4. Discussion
In this pilot study, we observed that intraoperative cerebral desaturation was found to be associated with both short- and long-term neurocognitive decline –assessed by ACE-R scores- in thoracic surgery under one-lung ventilation (OLV). Moreover, this study showed that reduced cerebral saturation did not necessarily coexist with peripheral desaturation, as the incidence of the former was about 42% and the latter 65%. According to our literature research, this is the first study demonstrating the association of cerebral desaturation and late cognitive dysfunction in thoracic surgery.
Thoracic surgery is commonly associated with impaired gas exchange and especially with hypoxemia due to OLV. Though studies investigating the effect of OLV are still limited compared to cardiac surgery, Mahal et al. explicitly discussed the mechanisms that might contribute to cerebral desaturation during OLV [
2]. These include definite systemic hypoxia and decreased cardiac output due to a mediastinal shift from the lateral decubitus position. Last but not least, hypoxic pulmonary vasoconstriction (HPV) leads to increased pulmonary arterial pressure and, consequently, central venous pressure (CVP), thereby compromising cerebral perfusion pressure. Moreover, earlier studies also noted that changes in carbon dioxide (CO
2) levels can affect cerebral blood flow and create a supply-demand imbalance [
6,
12,
13]. Near-infrared spectroscopy was found to be reliable for a sensitive and direct measure of the cerebral oxygen supply-demand balance [
14,
15]. Our study showed a discrepancy between cerebral and peripheral oxygenation during one-lung ventilation. This issue was underlined in an early study reporting the incompatibility in the reverse face [
16]. Authors declared that cerebral desaturation occurred in the presence of normal peripheral saturation values, which might be explained by decreased heart rate, namely, by hemodynamic disturbance. Conversely, we observed a peripheral desaturation with preserved cerebral oximetry values. We defined peripheral desaturation as 2 min, and intervened rapidly by determining measures to treat. One weak point of this study is the lack of duration for peripheral desaturation. We can speculate that quick management was associated with a lower incidence of cerebral desaturation in this study. Regarding perioperative events, hypotension, which might affect cerebral oxygen saturation, was similar between groups. Meanwhile, hypotension was a frequent finding, occurring in 57.4% of patients, and vasopressor use was lower at 37%. This discrepancy suggests that many hypotensive episodes were effectively managed with fluid resuscitation. The complex relationship between blood pressure and cerebral oxygenation is influenced by multiple factors like age, chronic hypertension, arterial stiffness, and baroreceptor sensitivity [
17,
18,
19]. Suehiro, in two separate studies, used minimum systolic pressure to evaluate its relationship with cerebral oxygenation [
20,
21], while Hemmerling focused on the correlation between cerebral desaturation and relative mean arterial pressure. These findings support the idea that one of the mechanisms of cerebral desaturation during OLV is a drop in cardiac output.
The reported incidence of cerebral desaturation in thoracic anesthesia varies significantly in the literature. While some earlier studies reported rates as high as 70–80% [
6,
12,
20], we observed an incidence of 43%. This result is consistent with more recent literature reporting a rate of approximately 50% [
1,
22]. In fact, the wide discrepancy among studies highlights the lack of a standardized definition for cerebral desaturation. In one of the initial works, Hemmerling et al. defined desaturation at three separate levels–but all considered as “desaturation” [
12], while Tang reported frequencies based on a drop of 15–20% and greater than 20% [
6]. In addition to the reduction ratio, the time component was previously determined by Suehiro, similar to our approach [
20]. Another definition of cerebral desaturation in thoracic surgery for a cohort study marked a decrease of 85–90% of baseline, lasting for more than 15 s [
23]. Interestingly, based on the area under threshold calculation, they proposed a decrease of <90% and <85% for, respectively, left and right sides as thresholds, agreeing that generalizability remains to be determined in other populations. In our study, cerebral desaturation was similarly defined to a well-designed recent cohort in terms of level and duration of cerebral saturation [
20]. Further large trials are obviously needed to define cerebral desaturation and possible treatment algorithms as established in cardiac surgery [
24].
One objective of this paper is to examine neurocognitive decline, which represents a significant and well-documented postoperative complication, including both delirium (POD) and cognitive dysfunction [
11,
25]. Prior studies investigated intraoperative cerebral oxygenation as a key contributing factor in thoracic surgery [
1,
6]. In an early research, neurological recovery was assessed with MMSE values in PACU compared to the preoperative period [
6]. Conversely, Shuehiro et al. affirmed that neurocognitive dysfunction evaluated by MMSE was similar between patients with or without cerebral desaturation in thoracic surgery [
15]. However, authors commented that the decrease from the baseline MMSE was significantly higher in the desaturated group, which showed a correlation with the degree of reduction in MMSE scores. All patients experienced both a cerebral desaturation (beginning with less than15% to more than 25%) and a reduction in MMSE score with a variable degree. The authors concluded that desaturations were positively correlated with cognitive decline, considering the weakness of using only MMSE for screening. A new well-designed study reported an association between delayed neurocognitive recovery in PACU and cerebral oxygen desaturations [
1]. Though delirium follow-up continued for three postoperative days, correlation was significant solely for day 0. A large cohort of 174 patients did not find any association between postoperative delirium for five postoperative days and minimum intraoperative SctO
2; however, any episode of cerebral desaturation (lasting for more than 15 sec) was related to an increased risk of delirium [
23]. Neurocognitive outcome can be evaluated as well with comprehensive cognitive test batteries like the ACE-R, which constitutes a remarkable point of this paper. These test batteries provide a more nuanced picture of cognitive function across multiple domains, including memory, language, and executive function [
26]. According to our literature research, this is the first study in the context of thoracic surgery to demonstrate impaired cognitive function associated with cerebral desaturation, extending into the late postoperative period. Patients who experienced cerebral desaturation showed a notable decrease in their ACE-R scores on both the 3rd postoperative day and at the 3-month follow-up compared to their baseline. Moreover, the analysis of individual cognitive domains revealed a significant decline in fluency in the desaturated group during the late postoperative period. This result may be a key to the resources of rehabilitation strategies based on the specific impaired domain [
27]. Crucially, the primary strength of our study is the longitudinal follow-up. The significant decline in ACE-R scores observed in the desaturated group on postoperative day 3 (POD3) was maintained at the 3-month follow-up. This correlation between early decline and late deficit is highly significant. It supports the conclusion that the POD 3 findings were not merely a transient manifestation of acute postoperative stress or pharmacological effects. Instead, the early cognitive decline appears to function as a harbinger or early indicator of a true, sustained neurocognitive injury initiated by intraoperative cerebral desaturation.
Cerebral oximetry can be considered a remarkable non-invasive monitoring modality for thoracic surgery regarding the particularities of one-lung ventilation and its consequences. Furthermore, our analysis revealed that the Total Desaturation Load (combining depth and duration) significantly correlated with poorer postoperative ACE-R scores. This suggests that long-term cognitive deficits are driven by the cumulative burden of cerebral hypoxemia, rather than the mere presence of a desaturation event. This finding supports the potential neuroprotective role of timely intervention. The standardized, aggressive management initiated immediately upon detecting a desaturation threshold likely mitigated the full extent of neurological injury. Therefore, NIRS serves as a crucial protocol-guiding tool, reinforcing the need for rapid clinical response to terminate the hypoxic insult and improve long-term neurological recovery. Future RCTs should test the efficacy of NIRS-guided, time-to-intervention strategies.
Though NIRS is mostly dedicated to detecting cerebral oxygen changes, intraoperative cerebral desaturation has been shown to have a significant impact on postoperative outcomes in thoracic surgery [
1,
13]. Initially, Kazan et al. affirmed that cerebral desaturation during OLV was correlated with Clavien and SOFA (non-respiratory) scores in fifty patients with an ASA grade of II or III [
13]. Scores were deliberately used for an objective assessment, and excluding surgery-related complications, the respiratory component of SOFA was eliminated to limit lung-surgery-related bias. In a more detailed analysis, Roberts et al. estimated the study population with Thorascore, which consisted of demographic data, ASA grade, preoperative performance, and dyspnea, as well as the extent of surgery [
1]. Patients who experienced cerebral desaturation had significantly higher Thorascores. After risk-adjustment by a patient’s Thorascore, patients with desaturation lasting more than 3 min and below 65% were significantly more prone to have a longer length of stay. The mean difference was 1.35 days, revealing further clinical significance. Authors suggested intraoperative cerebral oximetry as a developing monitoring of optimal recovery for the thoracic surgery population. In line with aforementioned studies, we observed a higher rate of ICU admission in the desaturated group; one should note that surgery-related unplanned admission was excluded. For preoperative status, we used ASA and no other extended scoring, but hypertension was the sole significant preoperative factor in this study. We recognize that chronic hypertension is a critical confounder, as it shifts the cerebral autoregulation curve, rendering patients more vulnerable to cerebral desaturation during hemodynamic fluctuations, such as those encountered during OLV [
17]. There are several reasons why patients with hypertension may be more likely to experience cerebral desaturation, such as pulse pressure, arterial stiffness, baroreceptor sensitivity, endothelial function, and carotid intima-media thickness [
18,
19]. Although our sample size was insufficient to perform a statistically robust subgroup analysis on hypertensive patients (
n = 17), the fact that hypertension was the only significant comorbidity difference between our groups suggests its potential role. Future, larger, and adequately powered multicenter trials must prioritize this specific subgroup analysis to precisely delineate the independent impact of altered cerebral autoregulation on cognitive outcomes. Systemic complications did not show any significant difference, as the study was not primarily designed to detect this issue, and was probably too small.