Cross-Sectional Investigation of Acute Stress Responses to Two Different Laboratory Stress Tests in Male and Female Athletes
Abstract
1. Introduction
2. Results
2.1. Psychobiological Measures
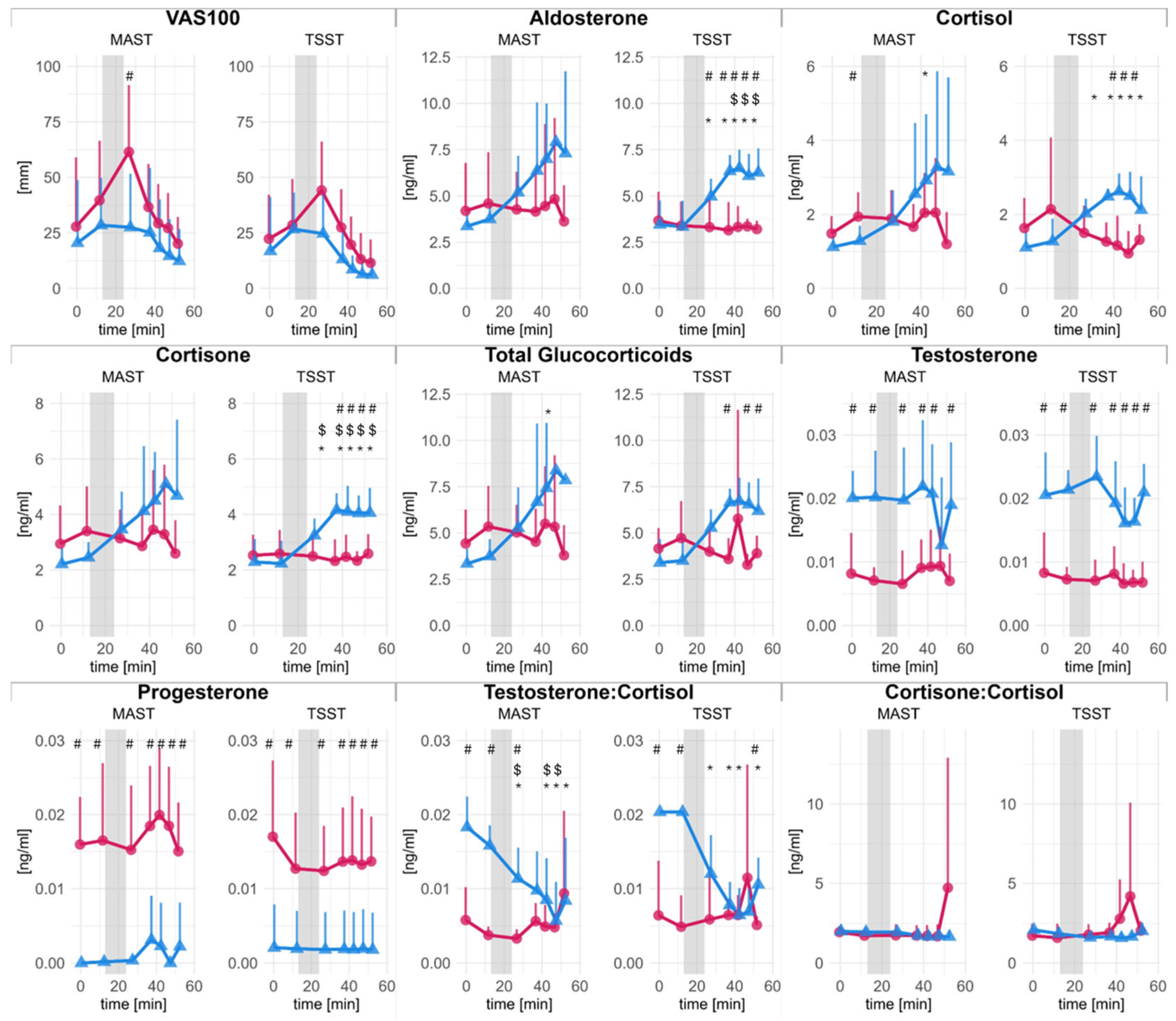
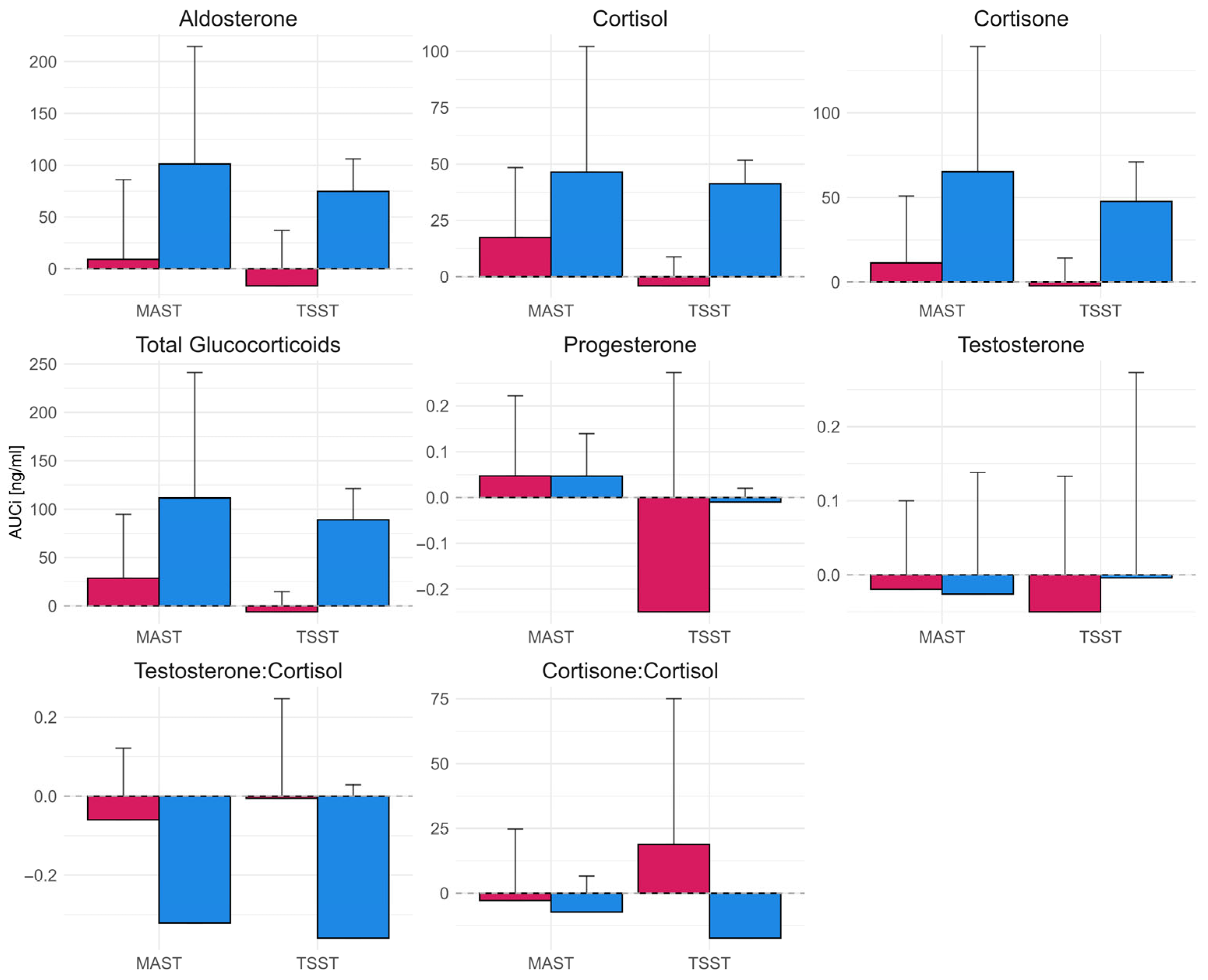
2.1.1. Quantified Hormones
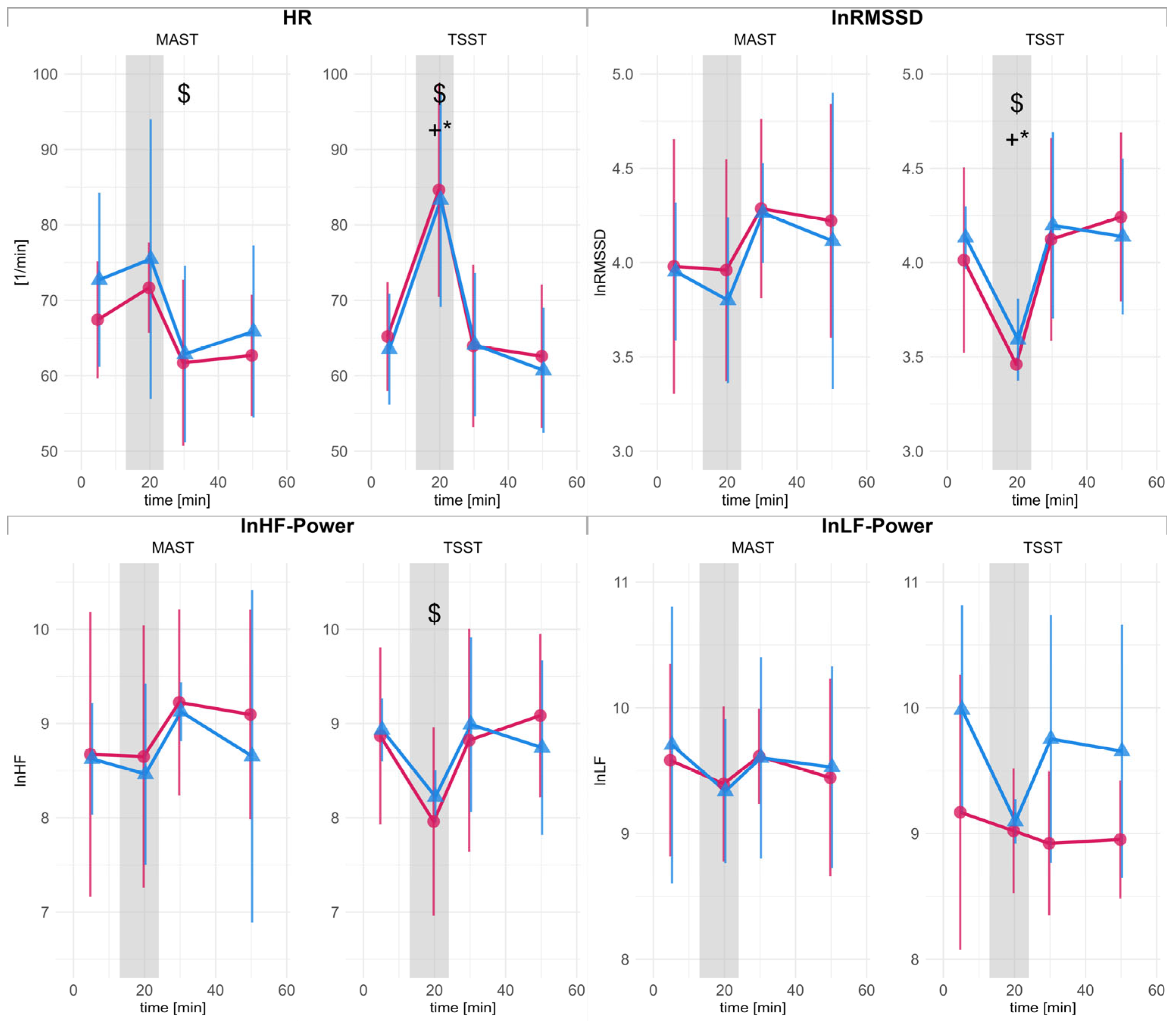
2.1.2. Autonomic Response
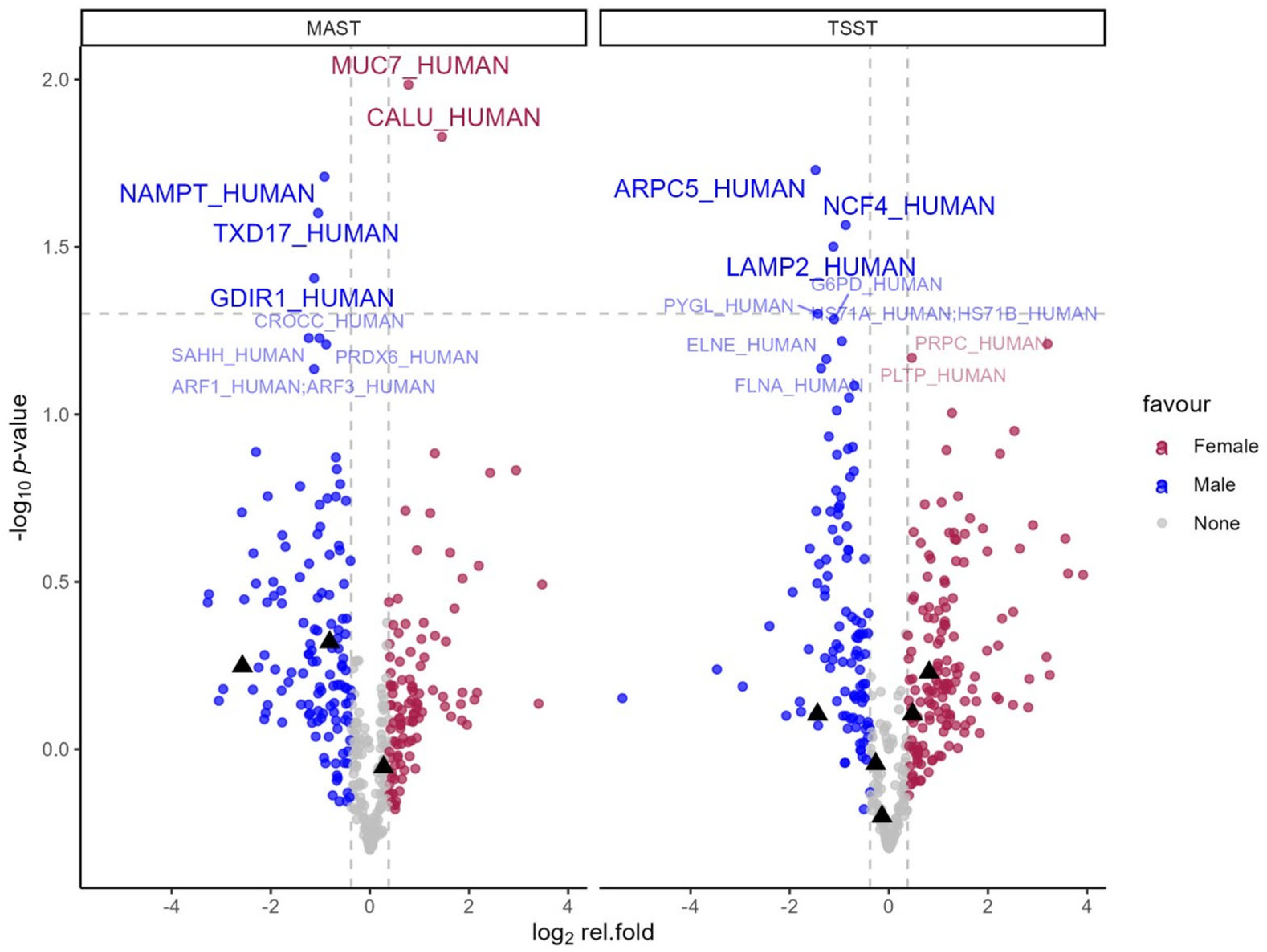
2.1.3. Proteomics
2.2. Self-Reported Measures
2.2.1. STAI-10
2.2.2. VAS100
3. Discussion
3.1. Comparison of TSST and MAST
3.2. Sex Specific Responses
3.3. Summary
4. Materials and Methods
4.1. Participants
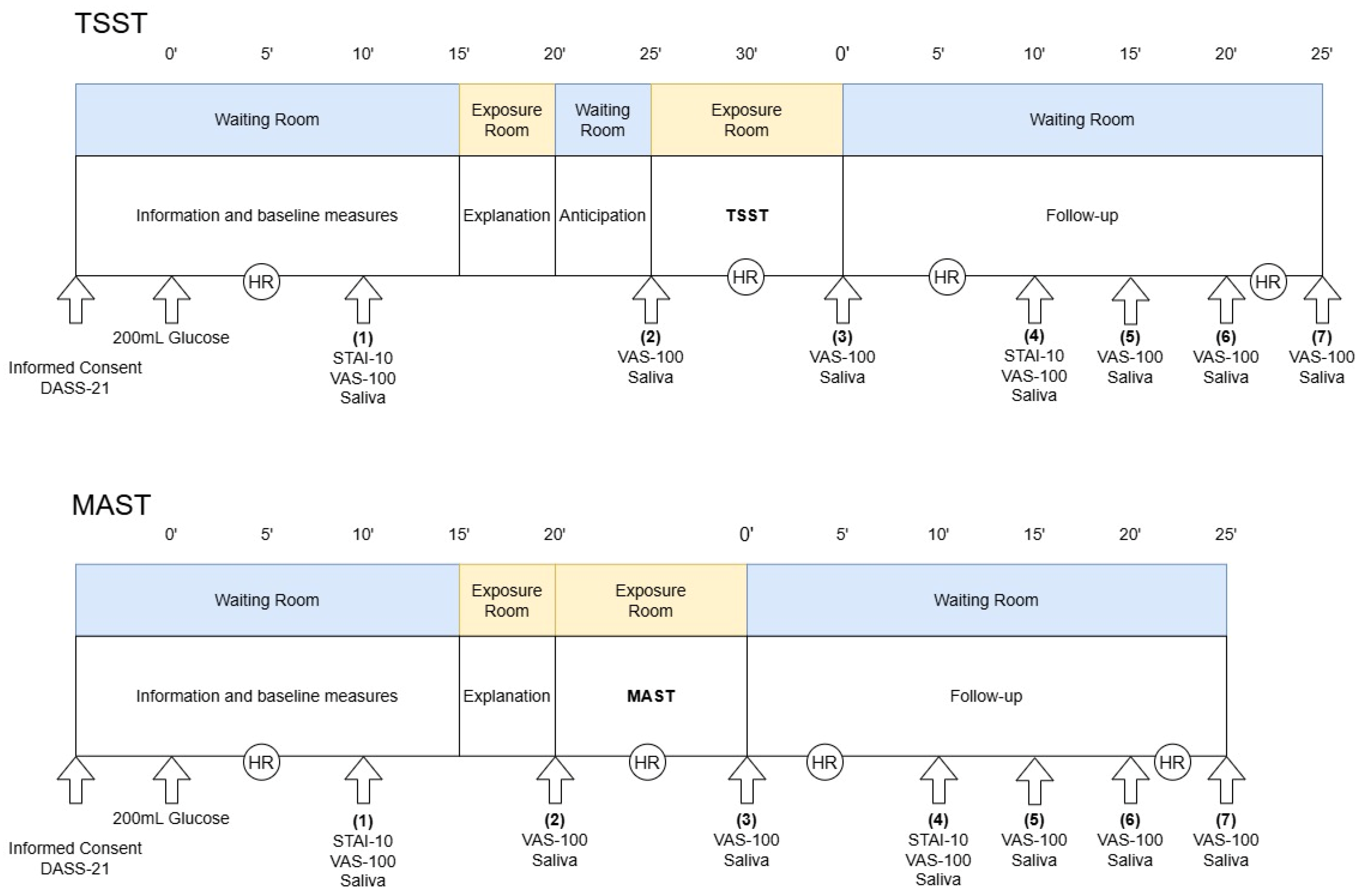
4.2. Procedure
4.2.1. Trier Social Stress Test
4.2.2. Maastricht Acute Stress Test
4.3. Measures
4.3.1. Psychobiological Measures
4.3.2. Self-Reported Measures
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANS | Autonomic nervous system |
| AUCi | Area under the curve with respect to increase |
| Cn:C | Cortisone-to-cortisol-ratio |
| DASS-21 | Depression Anxiety Stress Scale (21-itmes) |
| FDR | False discovery rate |
| HF | High Frequency HRV |
| HPA | Hypothalamic–pituitary–adrenal axis |
| HR | Heart rate |
| HRV | Heart rate variability |
| LF | Low-frequency HRV |
| MAST | Maastricht Acute Stress Test |
| RMSSD | Root mean square of successive differences |
| STAI-10 | State Anxiety Inventory (10-items) |
| T:C | Testosterone-to-cortisol-ratio |
| TSST | Trier Social Stress Test |
| VAS100 | Visual analogue scale (100 mm) |
References
- Spencer-Segal, J.L.; Akil, H. Glucocorticoids and Resilience. Horm. Behav. 2019, 111, 131–134. [Google Scholar] [CrossRef]
- Lupien, S.J.; Ouellet-Morin, I.; Hupbach, A.; Tu, M.T.; Buss, C.; Walker, D.; Pruessner, J.; Mcewen, B.S. Beyond the Stress Concept: Allostatic Load—A Developmental Biological and Cognitive Perspective. In Developmental Psychopathology; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2015; pp. 578–628. ISBN 978-0-470-93939-0. [Google Scholar]
- Theriault, J.E.; Katsumi, Y.; Reimann, H.M.; Zhang, J.; Deming, P.; Dickerson, B.C.; Quigley, K.S.; Barrett, L.F. It’s Not the Thought That Counts: Allostasis at the Core of Brain Function. Neuron 2025, 113, 4107–4133. [Google Scholar] [CrossRef] [PubMed]
- Epel, E.S.; Crosswell, A.D.; Mayer, S.E.; Prather, A.A.; Slavich, G.M.; Puterman, E.; Mendes, W.B. More than a Feeling: A Unified View of Stress Measurement for Population Science. Front. Neuroendocrinol. 2018, 49, 146–169. [Google Scholar] [CrossRef] [PubMed]
- Selye, H. Stress without Distress. Brux. Med. 1976, 56, 205–210. [Google Scholar] [PubMed]
- Segerstrom, S.C.; Miller, G.E. Psychological Stress and the Human Immune System: A Meta-Analytic Study of 30 Years of Inquiry. Psychol. Bull. 2004, 130, 601–630. [Google Scholar] [CrossRef]
- Brotman, D.J.; Golden, S.H.; Wittstein, I.S. The Cardiovascular Toll of Stress. Lancet 2007, 370, 1089–1100. [Google Scholar] [CrossRef]
- Kivimäki, M.; Steptoe, A. Effects of Stress on the Development and Progression of Cardiovascular Disease. Nat. Rev. Cardiol. 2018, 15, 215–229. [Google Scholar] [CrossRef]
- Wirtz, P.H.; von Känel, R. Psychological Stress, Inflammation, and Coronary Heart Disease. Curr. Cardiol. Rep. 2017, 19, 111. [Google Scholar] [CrossRef]
- Gianotti, L.; Belcastro, S.; D’Agnano, S.; Tassone, F. The Stress Axis in Obesity and Diabetes Mellitus: An Update. Endocrines 2021, 2, 334–347. [Google Scholar] [CrossRef]
- Hackett, R.A.; Steptoe, A. Type 2 Diabetes Mellitus and Psychological Stress—A Modifiable Risk Factor. Nat. Rev. Endocrinol. 2017, 13, 547–560. [Google Scholar] [CrossRef]
- Kivimäki, M.; Bartolomucci, A.; Kawachi, I. The Multiple Roles of Life Stress in Metabolic Disorders. Nat. Rev. Endocrinol. 2023, 19, 10–27. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S.; Akil, H. Revisiting the Stress Concept: Implications for Affective Disorders. J. Neurosci. 2020, 40, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.S.Y.; Liu, G.; Liang, D.; Deng, K.; Wu, J.; Yan, J.H. Special Issue–Therapeutic Benefits of Physical Activity for Mood: A Systematic Review on the Effects of Exercise Intensity, Duration, and Modality. J. Psychol. 2019, 153, 102–125. [Google Scholar] [CrossRef]
- Stonerock, G.L.; Hoffman, B.M.; Smith, P.J.; Blumenthal, J.A. Exercise as Treatment for Anxiety: Systematic Review and Analysis. Ann. Behav. Med. Publ. Soc. Behav. Med. 2015, 49, 542–556. [Google Scholar] [CrossRef]
- Mücke, M.; Ludyga, S.; Colledge, F.; Gerber, M. Influence of Regular Physical Activity and Fitness on Stress Reactivity as Measured with the Trier Social Stress Test Protocol: A Systematic Review. Sports Med. 2018, 48, 2607–2622. [Google Scholar] [CrossRef]
- Gerber, M.; Pühse, U. Review Article: Do Exercise and Fitness Protect against Stress-Induced Health Complaints? A Review of the Literature. Scand. J. Public Health 2009, 37, 801–819. [Google Scholar] [CrossRef]
- Martín-Rodríguez, A.; Gostian-Ropotin, L.A.; Beltrán-Velasco, A.I.; Belando-Pedreño, N.; Simón, J.A.; López-Mora, C.; Navarro-Jiménez, E.; Tornero-Aguilera, J.F.; Clemente-Suárez, V.J. Sporting Mind: The Interplay of Physical Activity and Psychological Health. Sports 2024, 12, 37. [Google Scholar] [CrossRef]
- Fuchs, R.; Klaperski, S. Stressregulation durch Sport und Bewegung. In Handbuch Stressregulation und Sport; Fuchs, R., Gerber, M., Eds.; Springer: Berlin, Heidelberg, 2018; pp. 205–226. ISBN 978-3-662-49322-9. [Google Scholar]
- Athanasiou, N.; Bogdanis, G.C.; Mastorakos, G. Endocrine Responses of the Stress System to Different Types of Exercise. Rev. Endocr. Metab. Disord. 2022, 24, 251–266. [Google Scholar] [CrossRef]
- Michael, S.; Graham, K.S.; Davis, G.M. Cardiac Autonomic Responses during Exercise and Post-Exercise Recovery Using Heart Rate Variability and Systolic Time Intervals—A Review. Front. Physiol. 2017, 8, 301. [Google Scholar] [CrossRef] [PubMed]
- Duclos, M.; Tabarin, A. Exercise and the Hypothalamo-Pituitary-Adrenal Axis. In Frontiers of Hormone Research; Lanfranco, F., Strasburger, C.J., Eds.; S. Karger AG: Basel, Switzerland, 2016; Volume 47, pp. 12–26. ISBN 978-3-318-05868-0. [Google Scholar]
- Kudielka, B.M.; Hellhammer, D.H.; Wüst, S. Why Do We Respond so Differently? Reviewing Determinants of Human Salivary Cortisol Responses to Challenge. Psychoneuroendocrinology 2009, 34, 2–18. [Google Scholar] [CrossRef]
- Sothmann, M.S. The Cross-Stressor Adaptation Hypothesis and Exercise Training. In Psychobiology of Physical Activity; Human Kinetics: Champaign, IL, USA, 2006; pp. 149–160. ISBN 978-0-7360-5536-9. [Google Scholar]
- Sothmann, M.S.; Buckworth, J.; Claytor, R.P.; Cox, R.H.; White-Welkley, J.E.; Dishman, R.K. Exercise Training and the Cross-Stressor Adaptation Hypothesis. Exerc. Sport Sci. Rev. 1996, 24, 267–287. [Google Scholar] [CrossRef]
- LeClair, K.B.; Russo, S.J. Using Social Rank as the Lens to Focus on the Neural Circuitry Driving Stress Coping Styles. Curr. Opin. Neurobiol. 2021, 68, 167–180. [Google Scholar] [CrossRef]
- Mason, J.W. A Historical View of the Stress Field. J. Human Stress 1975, 1, 22–36. [Google Scholar] [CrossRef]
- Arvidson, E.; Dahlman, A.S.; Börjesson, M.; Gullstrand, L.; Jonsdottir, I.H. The Effects of Exercise Training on Hypothalamic-Pituitary-Adrenal Axis Reactivity and Autonomic Response to Acute Stress—A Randomized Controlled Study. Trials 2020, 21, 888. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.; Imboden, C.; Beck, J.; Brand, S.; Colledge, F.; Eckert, A.; Holsboer-Trachsler, E.; Pühse, U.; Hatzinger, M. Effects of Aerobic Exercise on Cortisol Stress Reactivity in Response to the Trier Social Stress Test in Inpatients with Major Depressive Disorders: A Randomized Controlled Trial. J. Clin. Med. 2020, 9, 1419. [Google Scholar] [CrossRef] [PubMed]
- Klaperski, S.; Von Dawans, B.; Heinrichs, M.; Fuchs, R. Effects of a 12-Week Endurance Training Program on the Physiological Response to Psychosocial Stress in Men: A Randomized Controlled Trial. J. Behav. Med. 2014, 37, 1118–1133. [Google Scholar] [CrossRef] [PubMed]
- Bae, Y.J.; Reinelt, J.; Netto, J.; Uhlig, M.; Willenberg, A.; Ceglarek, U.; Villringer, A.; Thiery, J.; Gaebler, M.; Kratzsch, J. Salivary Cortisone, as a Biomarker for Psychosocial Stress, Is Associated with State Anxiety and Heart Rate. Psychoneuroendocrinology 2019, 101, 35–41. [Google Scholar] [CrossRef]
- Botía, M.; Escribano, D.; Martínez-Subiela, S.; Tvarijonaviciute, A.; Tecles, F.; López-Arjona, M.; Cerón, J.J. Different Types of Glucocorticoids to Evaluate Stress and Welfare in Animals and Humans: General Concepts and Examples of Combined Use. Metabolites 2023, 13, 106. [Google Scholar] [CrossRef]
- Barel, E.; Abu-Shkara, R.; Colodner, R.; Masalha, R.; Mahagna, L.; Zemel, O.C.; Cohen, A. Gonadal Hormones Modulate the HPA-Axis and the SNS in Response to Psychosocial Stress. J. Neurosci. Res. 2018, 96, 1388–1397. [Google Scholar] [CrossRef]
- Chichinadze, K.; Chichinadze, N. Stress-Induced Increase of Testosterone: Contributions of Social Status and Sympathetic Reactivity. Physiol. Behav. 2008, 94, 595–603. [Google Scholar] [CrossRef]
- Kirschbaum, C.; Pirke, K.M.; Hellhammer, D.H. The ‘Trier Social Stress Test’—A Tool for Investigating Psychobiological Stress Responses in a Laboratory Setting. Neuropsychobiology 1993, 28, 76–81. [Google Scholar] [CrossRef]
- Gu, H.; Ma, X.; Zhao, J.; Liu, C. A Meta-Analysis of Salivary Cortisol Responses in the Trier Social Stress Test to Evaluate the Effects of Speech Topics, Sex, and Sample Size. Compr. Psychoneuroendocrinol. 2022, 10, 100125. [Google Scholar] [CrossRef]
- Dickerson, S.S.; Kemeny, M.E. Acute Stressors and Cortisol Responses: A Theoretical Integration and Synthesis of Laboratory Research. Psychol. Bull. 2004, 130, 355–391. [Google Scholar] [CrossRef]
- Smeets, T.; Cornelisse, S.; Quaedflieg, C.W.E.M.; Meyer, T.; Jelicic, M.; Merckelbach, H. Introducing the Maastricht Acute Stress Test (MAST): A Quick and Non-Invasive Approach to Elicit Robust Autonomic and Glucocorticoid Stress Responses. Psychoneuroendocrinology 2012, 37, 1998–2008. [Google Scholar] [CrossRef]
- Cowley, E.S.; Olenick, A.A.; McNulty, K.L.; Ross, E.Z. “Invisible Sportswomen”: The Sex Data Gap in Sport and Exercise Science Research. Women Sport Phys. Act. J. 2021, 29, 146–151. [Google Scholar] [CrossRef]
- Landen, S.; Hiam, D.; Voisin, S.; Jacques, M.; Lamon, S.; Eynon, N. Physiological and Molecular Sex Differences in Human Skeletal Muscle in Response to Exercise Training. J. Physiol. 2023, 601, 419–434. [Google Scholar] [CrossRef]
- Kraemer, W.J.; Ratamess, N.A.; Hymer, W.C.; Nindl, B.C.; Fragala, M.S. Growth Hormone(s), Testosterone, Insulin-Like Growth Factors, and Cortisol: Roles and Integration for Cellular Development and Growth With Exercise. Front. Endocrinol. 2020, 11, 33. [Google Scholar] [CrossRef] [PubMed]
- Cano Sokoloff, N.; Misra, M.; Ackerman, K.E. Exercise, Training, and the Hypothalamic-Pituitary-Gonadal Axis in Men and Women. Front. Horm. Res. 2016, 47, 27–43. [Google Scholar] [CrossRef] [PubMed]
- Zilioli, S.; Watson, N.V. Testosterone across Successive Competitions: Evidence for a ‘Winner Effect’ in Humans? Psychoneuroendocrinology 2014, 47, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, M.; Alvero-Cruz, J.R.; Solla, J.; García-Bastida, J.; García-Coll, V.; Rivilla, I.; Ruiz, E.; García-Romero, J.; Carnero, E.A.; Clemente-Suárez, V.J. Competition Seriousness and Competition Level Modulate Testosterone and Cortisol Responses in Soccer Players. Int. J. Environ. Res. Public. Health 2020, 17, 350. [Google Scholar] [CrossRef]
- Schwabe, L.; Schächinger, H. Ten Years of Research with the Socially Evaluated Cold Pressor Test: Data from the Past and Guidelines for the Future. Psychoneuroendocrinology 2018, 92, 155–161. [Google Scholar] [CrossRef]
- Chapman, K.; Holmes, M.; Seckl, J. 11β-Hydroxysteroid Dehydrogenases: Intracellular Gate-Keepers of Tissue Glucocorticoid Action. Physiol. Rev. 2013, 93, 1139–1206. [Google Scholar] [CrossRef]
- Allen, A.P.; Kennedy, P.J.; Cryan, J.F.; Dinan, T.G.; Clarke, G. Biological and Psychological Markers of Stress in Humans: Focus on the Trier Social Stress Test. Neurosci. Biobehav. Rev. 2014, 38, 94–124. [Google Scholar] [CrossRef]
- Leal, D.V.; Taylor, L.; Hough, J. Reproducibility of Acute Steroid Hormone Responses in Men to Short-Duration Running. Int. J. Sports Physiol. Perform. 2019, 14, 1430–1437. [Google Scholar] [CrossRef] [PubMed]
- Hackney, A.C.; Walz, E.A. Hormonal Adaptation and the Stress of Exercise Training: The Role of Glucocorticoids. Trends Sport Sci. 2013, 20, 165–171. [Google Scholar] [PubMed]
- Tesarz, J.; Schuster, A.K.; Hartmann, M.; Gerhardt, A.; Eich, W. Pain Perception in Athletes Compared to Normally Active Controls: A Systematic Review with Meta-Analysis. Pain 2012, 153, 1253. [Google Scholar] [CrossRef] [PubMed]
- Ehlers, T.S.; Møller, S.; Hansen, C.C.; Tamariz-Ellemann, A.S.; Vermeulen, T.D.; Shoemaker, J.K.; Gliemann, L.; Hellsten, Y. Sympathetic Activity Is Not a Main Cause of Blood Pressure Reduction with Exercise Training in Un-Medicated Middle-Aged/Older Men. Scand. J. Med. Sci. Sports 2023, 33, 586–596. [Google Scholar] [CrossRef]
- Lamotte, G.; Boes, C.J.; Low, P.A.; Coon, E.A. The Expanding Role of the Cold Pressor Test: A Brief History. Clin. Auton. Res. 2021, 31, 153–155. [Google Scholar] [CrossRef]
- Ifuku, H.; Moriyama, K.; Arai, K.; Shiraishi-Hichiwa, Y. Regulation of Cardiac Function during a Cold Pressor Test in Athletes and Untrained Subjects. Eur. J. Appl. Physiol. 2007, 101, 75–79. [Google Scholar] [CrossRef]
- Hamunen, K.; Kontinen, V.; Hakala, E.; Talke, P.; Paloheimo, M.; Kalso, E. Effect of Pain on Autonomic Nervous System Indices Derived from Photoplethysmography in Healthy Volunteers. BJA Br. J. Anaesth. 2012, 108, 838–844. [Google Scholar] [CrossRef]
- Huang, M.; Yoo, J.-K.; Stickford, A.S.L.; Moore, J.P.; Hendrix, J.M.; Crandall, C.G.; Fu, Q. Early Sympathetic Neural Responses during a Cold Pressor Test Linked to Pain Perception. Clin. Auton. Res. 2021, 31, 215–224. [Google Scholar] [CrossRef]
- Castellani, J.W.; Tipton, M.J. Cold Stress Effects on Exposure Tolerance and Exercise Performance. Compr. Physiol. 2016, 6, 443–469. [Google Scholar] [CrossRef]
- Campbell, J.; Ehlert, U. Acute Psychosocial Stress: Does the Emotional Stress Response Correspond with Physiological Responses? Psychoneuroendocrinology 2012, 37, 1111–1134. [Google Scholar] [CrossRef] [PubMed]
- Dalile, B.; La Torre, D.; Verbeke, K.; Vanm Oudenhove, L.; Vervliet, B. When the Mind Says One Thing, but the HPA Axis Says Another: Lack of Coherence between Subjective and Neuroendocrine Stress Response Trajectories in Healthy Men. Psychoneuroendocrinology 2022, 139, 105692. [Google Scholar] [CrossRef] [PubMed]
- Forcier, K.; Stroud, L.R.; Papandonatos, G.D.; Hitsman, B.; Reiches, M.; Krishnamoorthy, J.; Niaura, R. Links between Physical Fitness and Cardiovascular Reactivity and Recovery to Psychological Stressors: A Meta-Analysis. Health Psychol. 2006, 25, 723–739. [Google Scholar] [CrossRef]
- Jackson, E.M.; Dishman, R.K. Cardiorespiratory Fitness and Laboratory Stress: A Meta-Regression Analysis. Psychophysiology 2006, 43, 57–72. [Google Scholar] [CrossRef] [PubMed]
- Linden, W.; Earle, T.L.; Gerin, W.; Christenfeld, N. Physiological Stress Reactivity and Recovery: Conceptual Siblings Separated at Birth? J. Psychosom. Res. 1997, 42, 117–135. [Google Scholar] [CrossRef]
- Degering, M.; Linz, R.; Puhlmann, L.M.C.; Singer, T.; Engert, V. Revisiting the Stress Recovery Hypothesis: Differential Associations of Cortisol Stress Reactivity and Recovery after Acute Psychosocial Stress with Markers of Long-Term Stress and Health. Brain Behav. Immun.-Health 2023, 28, 100598. [Google Scholar] [CrossRef]
- Liu, J.J.W.; Ein, N.; Peck, K.; Huang, V.; Pruessner, J.C.; Vickers, K. Sex Differences in Salivary Cortisol Reactivity to the Trier Social Stress Test (TSST): A Meta-Analysis. Psychoneuroendocrinology 2017, 82, 26–37. [Google Scholar] [CrossRef]
- Heindl, S.; Holzschneider, J.; Hinz, A.; Sayk, F.; Fehm, H.L.; Dodt, C. Acute Effects of Aldosterone on the Autonomic Nervous System and the Baroreflex Function in Healthy Humans. J. Neuroendocrinol. 2006, 18, 115–121. [Google Scholar] [CrossRef]
- Caroccia, B.; Seccia, T.M.; Barton, M.; Rossi, G.P. Estrogen Signaling in the Adrenal Cortex. Hypertension 2016, 68, 840–848. [Google Scholar] [CrossRef]
- O’Bryan, S.M.; Connor, K.R.; Drummer, D.J.; Lavin, K.M.; Bamman, M.M. Considerations for Sex-Cognizant Research in Exercise Biology and Medicine. Front. Sports Act. Living 2022, 4, 903992. [Google Scholar] [CrossRef]
- Kasiak, P.; Kowalski, T.; Rębiś, K.; Klusiewicz, A.; Ładyga, M.; Sadowska, D.; Wilk, A.; Wiecha, S.; Barylski, M.; Poliwczak, A.R.; et al. Is the Ventilatory Efficiency in Endurance Athletes Different?—Findings from the NOODLE Study. J. Clin. Med. 2024, 13, 490. [Google Scholar] [CrossRef]
- Büttler, R.M.; Bagci, E.; Brand, H.S.; den Heijer, M.; Blankenstein, M.A.; Heijboer, A.C. Testosterone, Androstenedione, Cortisol and Cortisone Levels in Human Unstimulated, Stimulated and Parotid Saliva. Steroids 2018, 138, 26–34. [Google Scholar] [CrossRef]
- Ney, L.J.; Felmingham, K.L.; Nichols, D. Reproducibility of Saliva Progesterone Measured by Immunoassay Compared to Liquid Chromatography Mass Spectrometry. Anal. Biochem. 2020, 610, 113984. [Google Scholar] [CrossRef]
- Sakkas, D.; Howles, C.M.; Atkinson, L.; Borini, A.; Bosch, E.A.; Bryce, C.; Cattoli, M.; Copperman, A.B.; de Bantel, A.F.; French, B.; et al. A Multi-Centre International Study of Salivary Hormone Oestradiol and Progesterone Measurements in ART Monitoring. Reprod. Biomed. Online 2021, 42, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Sacha, J. Why Should One Normalize Heart Rate Variability with Respect to Average Heart Rate. Front. Physiol. 2013, 4, 306. [Google Scholar] [CrossRef] [PubMed]
- Leliavski, A.; Dumbell, R.; Ott, V.; Oster, H. Adrenal Clocks and the Role of Adrenal Hormones in the Regulation of Circadian Physiology. J. Biol. Rhythms 2015, 30, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Kajantie, E.; Phillips, D.I.W. The Effects of Sex and Hormonal Status on the Physiological Response to Acute Psychosocial Stress. Psychoneuroendocrinology 2006, 31, 151–178. [Google Scholar] [CrossRef] [PubMed]
- Nilges, P.; Essau, C. Die Depressions-Angst-Stress-Skalen. Schmerz 2015, 29, 649–657. [Google Scholar] [CrossRef]
- Labuschagne, I.; Grace, C.; Rendell, P.; Terrett, G.; Heinrichs, M. An Introductory Guide to Conducting the Trier Social Stress Test. Neurosci. Biobehav. Rev. 2019, 107, 686–695. [Google Scholar] [CrossRef]
- Zänkert, S.; Kudielka, B.M.; Wüst, S. Effect of Sugar Administration on Cortisol Responses to Acute Psychosocial Stress. Psychoneuroendocrinology 2020, 115, 104607. [Google Scholar] [CrossRef]
- Goodman, W.K.; Janson, J.; Wolf, J.M. Meta-Analytical Assessment of the Effects of Protocol Variations on Cortisol Responses to the Trier Social Stress Test. Psychoneuroendocrinology 2017, 80, 26–35. [Google Scholar] [CrossRef]
- Engert, V.; Efanov, S.I.; Duchesne, A.; Vogel, S.; Corbo, V.; Pruessner, J.C. Differentiating Anticipatory from Reactive Cortisol Responses to Psychosocial Stress. Psychoneuroendocrinology 2013, 38, 1328–1337. [Google Scholar] [CrossRef]
- García Martínez, C.A.; Otero Quintana, A.; Vila, X.A.; Lado Touriño, M.J.; Rodríguez-Liñares, L.; Rodríguez Presedo, J.M.; Méndez Penín, A.J. Heart Rate Variability Analysis with the R Package RHRV; Use R!; Springer International Publishing: Cham, Switzerland, 2024; ISBN 978-3-031-65752-8. [Google Scholar]
- Vila, J.; Palacios, F.; Presedo, J.; Fernandez-Delgado, M.; Felix, P.; Barro, S. Time-Frequency Analysis of Heart-Rate Variability. IEEE Eng. Med. Biol. Mag. 1997, 16, 119–126. [Google Scholar] [CrossRef]
- Adu, P.; Popoola, T.; Iqbal, N.; Medvedev, O.N.; Simpson, C.R. Validating the Depression Anxiety Stress Scales (DASS-21) across Germany, Ghana, India, and New Zealand Using Rasch Methodology. J. Affect. Disord. 2025, 383, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Grimm, J. STAI-Test: State-Trait-Anxiety Inventory (Deutsche Version); MF-Working Paper; Methodenforum der Universität Wien: Wien, Austria, 2009; Volume 2. [Google Scholar]
- Fischer, S.; Doerr, J.M.; Strahler, J.; Mewes, R.; Thieme, K.; Nater, U.M. Stress Exacerbates Pain in the Everyday Lives of Women with Fibromyalgia Syndrome—The Role of Cortisol and Alpha-Amylase. Psychoneuroendocrinology 2016, 63, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Linnemann, A.; Ditzen, B.; Strahler, J.; Doerr, J.M.; Nater, U.M. Music Listening as a Means of Stress Reduction in Daily Life. Psychoneuroendocrinology 2015, 60, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Sattler, F.A.; Nater, U.M.; Mewes, R. Gay Men’s Stress Response to a General and a Specific Social Stressor. J. Neural Transm. 1996, 2021, 1325–1333. [Google Scholar] [CrossRef]
- Ben-Shachar, M.S.; Lüdecke, D.; Makowski, D. Effectsize: Estimation of Effect Size Indices and Standardized Parameters. J. Open Source Softw. 2020, 5, 2815. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and Reporting Effect Sizes to Facilitate Cumulative Science: A Practical Primer for t-Tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Cowen, S.; Ellison, S.L.R. Reporting Measurement Uncertainty and Coverage Intervals near Natural Limits. Analyst 2006, 131, 710–717. [Google Scholar] [CrossRef] [PubMed]
- Pruessner, J.C.; Kirschbaum, C.; Meinlschmid, G.; Hellhammer, D.H. Two Formulas for Computation of the Area under the Curve Represent Measures of Total Hormone Concentration versus Time-Dependent Change. Psychoneuroendocrinology 2003, 28, 916–931. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.H.; Blume, J.D. FDRestimation: Flexible False Discovery Rate Computation in R. F1000Research 2021, 10, 441. [Google Scholar] [CrossRef] [PubMed]
| Sex | N | Age (Years) | BMI (kg/m2) | DASS21-Depression | DASS21-Anxiety | DASS21-Stress |
|---|---|---|---|---|---|---|
| Female | 6 | 30.5 ± 5.0 | 22.8 ± 1.5 | 1.8 ± 2.1 | 0.8 ± 0.7 | 3.5 ± 2.1 |
| Male | 6 | 27.3 ± 4.87 | 25.5 ± 2.4 | 0.7 ± 1.2 | 1.5 ± 1.7 | 1.0 ± 1.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Raidl, P.; Wessner, B.; Methlagl, M.; Csapo, R. Cross-Sectional Investigation of Acute Stress Responses to Two Different Laboratory Stress Tests in Male and Female Athletes. Physiologia 2026, 6, 2. https://doi.org/10.3390/physiologia6010002
Raidl P, Wessner B, Methlagl M, Csapo R. Cross-Sectional Investigation of Acute Stress Responses to Two Different Laboratory Stress Tests in Male and Female Athletes. Physiologia. 2026; 6(1):2. https://doi.org/10.3390/physiologia6010002
Chicago/Turabian StyleRaidl, Peter, Barbara Wessner, Michael Methlagl, and Robert Csapo. 2026. "Cross-Sectional Investigation of Acute Stress Responses to Two Different Laboratory Stress Tests in Male and Female Athletes" Physiologia 6, no. 1: 2. https://doi.org/10.3390/physiologia6010002
APA StyleRaidl, P., Wessner, B., Methlagl, M., & Csapo, R. (2026). Cross-Sectional Investigation of Acute Stress Responses to Two Different Laboratory Stress Tests in Male and Female Athletes. Physiologia, 6(1), 2. https://doi.org/10.3390/physiologia6010002








