Abstract
Public market workers may be disproportionally exposed to SARS-CoV-2 due to interactions with shoppers. We aimed to estimate the seroprevalence of SARS-CoV-2 and determine whether occupation or adherence to preventive practices were associated with exposure. From July to December 2021, we longitudinally surveyed two Guatemalan markets twice. We collected blood to detect anti-S IgA, anti-S IgG, and anti-N IgG using ELISA, and a nasopharyngeal swab to detect SARS-CoV-2 using rRT-PCR. We estimated seroprevalences and assessed associations using generalized estimating equations. Of 229 workers, 109 (48%) participated in the first survey and 87 (38%) in the second. At baseline, 77% were female, 64% were aged <40, and 81% were vendors. Overall, the seroprevalence increased between surveys (61% to 89% for anti-S IgA, 53% to 91% for anti-S IgG, and 22% to 29% for anti-N IgG), but the magnitude differed by vaccination status and antibody type. The prevalence of infections decreased from 13% to 1% and most were asymptomatic. Vendor occupation was associated with IgA and IgG anti-S in males but not females. Using a mask was a protective measure. Most market workers had been exposed to SARS-CoV-2, possibly through asymptomatic individuals. Masking is a protective measure to be prioritized during high transmission.
1. Introduction
Municipal public markets in Guatemala, as in other low- and middle-income countries, are located permanently and are open daily, year-round. Small independent businesses sell essential products in these markets, including vegetables, fruit, meat, fish, poultry, dairy products, spices, grains, prepared foods and beverages, crafts, and other non-food items. These markets contribute to community health, social structure, and economy by offering a variety of fresh foods at affordable prices and in customized quantities, making them a crucial step in the distribution chain of essential supplies, and provide employment as well as a favorable space for local businesses to prosper. The success of the market is driven by its workers, including vendors, vendors’ helpers, administrative staff, maintenance staff, and security forces. Public markets are a resource for the entire population but are primarily used by economically disadvantaged and vulnerable groups [1,2].
Public markets are also prime environments for transmitting airborne infectious diseases such as SARS-CoV-2 within the market and into the community. Transmission results from close interactions between vendors and shoppers during commercial events in a closed environment, especially if individuals are unaware of their infectious status [3,4,5,6,7].
During the COVID-19 pandemic, local authorities recognized the benefit of public markets and allowed them to remain open despite other efforts to control SARS-CoV-2 transmission through massive lockdowns. Thus, public market workers, especially the vendors, became frontline essential non-healthcare workers. To mitigate virus transmission in public markets, local authorities mandated the use of masks, promoted physical distancing, and made alcohol-based sanitizers and disinfectants available [1,2].
Despite recognizing that public market workers have an increased risk of work-related exposure to SARS-CoV-2 [8], studies in low- and middle-income countries, where market dynamics may differ from high-income countries, are lacking. To provide essential information to guide recommendations to control virus spread within public markets and protect the health and economy of workers and the community, we evaluated the SARS-CoV-2 burden on workers in two municipal public markets in Guatemala. This study aimed to estimate the seroprevalence of SARS-CoV-2 in market workers and determine whether occupation, as opposed to other occupations (e.g., helper, administrative, maintenance, or security duties) or adherence to preventive practices, were associated with exposure.
2. Materials and Methods
2.1. Study Design and Population
We conducted a longitudinal cohort with two serosurveys, the first from July to September 2021 and the second from October to December 2022, in workers from two indoor public markets in the municipality of Santa Catarina Pinula, department of Guatemala. The first serosurvey overlapped with the COVID-19 wave occurring in Guatemala from June to October 2021. The wave involved 153,060 cases (4353 per 100,000 persons) and 2821 deaths (124 per 100,000) caused by the Delta lineage B.1.617.2 variant [9]. The study also overlapped with a major national SARS-CoV-2 vaccination campaign directed to the general population that started in September 2021.
The municipality covers 49.29 km2 and is 1550 m above sea level, with a population of 80,582 inhabitants, of which 94.51% are Ladinos, with an average age of 29.72 years. The literacy rate of the municipality is 95.67%, and 88.09% of the population lives in urban areas considered as dormitory towns of Guatemala City [10]. Based on the municipality records, each market receives, on average, 2500 to 3000 shoppers daily. The markets are open daily for 10 h.
2.2. Formative Research
From 8 June to 19 July 2021, we conducted a census to count the number of persons who self-reported being market workers and collected their age group, sex, and occupation.
2.3. Study Population
We invited all market workers aged 18 years or older without conditions affecting the immune system (cancer, infection with the human immunodeficiency virus, autoimmune diseases or who were undergoing chemotherapy or radiotherapy) or without any contraindication to participate and to provide nasopharyngeal or blood samples. The participants worked in two indoor public markets located in Santa Catarina Pinula Municipality (latitude 14.553388, longitude-90.478549) in the department of Guatemala, near the capital city.
2.4. Serosurveys
Study fieldworkers interviewed participants in person regarding sociodemographic and occupational characteristics, general disease risk factors, vaccination status, COVID-19 symptoms (fever, cough, anosmia, and augesia), history of a positive COVID-19 antigen or PCR test, and adoption of preventive practices against COVID-19 in the past month. Preventive practices included a self-reported handshaking avoidance frequency, avoiding in-person social gatherings, cleaning hands for at least 20 s, maintaining a minimum distance of 1.5 m while eating, and ensuring that the mouth and nose are covered with a mask [11]. These variables were measured to be included in the risk factor analysis.
2.5. Antibody Detection Using ELISA
We collected one 4 mL blood sample from each participant in EDTA-coated tubes in each serosurvey and stored it at 2–5 °C until centrifugation for 15 min at 2500 rpm to obtain plasma. Because the time of infection was uncertain, we measured early-onset (IgA anti-S) and late-onset (IgG anti-S) immunoglobulins. We also assessed immunoglobulins triggered by natural infection (IgG anti-N) or by natural infection or vaccination (IgG anti-S and IgA anti-S); in vaccinated people, these tests cannot distinguish between antibodies induced by vaccine or by infection. We used a commercially available indirect ELISA test (Euroimmun, Lübeck, Germany) according to the manufacturer’s instructions for non-automated testing. The sensitivity and specificity of these assays, as reported by the manufacturer, are 94.4% and 99.6% for IgG anti-S; 96.9% and 98.3% for IgA anti-S; and 94.6% and 99.8% for IgG anti-N.
2.6. Viral Detection Using RT-PCR
At each serosurvey, we collected a nasopharyngeal swab in universal transport medium and stored it at 2–5 °C until processing. The samples were centrifuged, and nucleic acid was extracted using Quick-DNA/RNA Viral Kit columns (Zymo, Irvine, CA, USA), according to manufacturer instructions. The eluate was analyzed to detect the SARS-CoV-2 nucleocapsid gene using real-time reverse-transcriptase polymerase-chain-reaction (rRT-PCR), following the US Centers for Disease Control and Prevention (CDC) protocol [12].
2.7. Data Preparation
To estimate socioeconomic status, a potential confounder in our analysis, we classified the participants in wealth tertiles using the first score of a principal component analysis conducted for asset ownership (electricity, solar panels, radio, television, landline, cell phone, refrigerator, washer, dryer, microwave oven, computer, internet, and house). We considered a participant to be fully vaccinated with SARS-CoV-2 after two weeks of receiving all recommended doses in the primary series [13]. The vaccines that were administered to the participants by the Ministry of Health were Sputnik V (Gamaleya Research Institute, Moscow, Russia), Moderna COVID (Moderna, Cambridge MA, USA), Vaxzevria (Oxford-AstraZeneca, Cambridge, UK), and Comirnaty (Pfizer-BioNTech, New York, NY, USA). We dichotomized work activities into those that involve daily interaction with shoppers (e.g., vendors) and those that do not (e.g., individuals in charge of administration, maintenance, security, or general help). Preventive practices against COVID-19 were measured using a five-level Likert frequency scale and were dichotomized for the analysis.
2.8. Seroprevalence
The seroprevalence of each antibody was calculated at each serosurvey and stratified according to vaccination status and sociodemographic and occupational characteristics. To address differences between participants and the census population, we also calculated the seroprevalence standardized by age group, sex, and market reported at the census. We estimated confidence intervals using exact statistics of the binomial distribution.
2.9. Risk Factors Analysis
The primary risk factors studied were vendor occupation and adoption of preventive practices against COVID-19. The directed acyclic graph in Figure 1 shows our hypothesized exposure pathways and potential confounders. To assess the association of vendor occupation with SARS-CoV-2 exposure, we calculated odds ratios (OR) adjusted for sociodemographic and occupational characteristics, in vendors who had received >1 dose of the SARS-CoV-2 vaccine using generalized estimating equations. We also explored effect modification by sex. To assess the association of adopting preventive practices, we repeated the analysis adjusting for the same variables. The analyses were conducted using R, version 4.1.3 (R Foundation for Statistical Computing, Vienna, Austria), and RStudio, version 2022.02.1 + 461 (Rstudio, PBC, Boston, MA, USA).
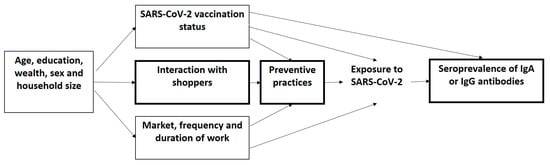
Figure 1.
Directed acyclic graph of the hypothesized paths of interaction between shoppers, preventive behaviors, exposure with SARS-CoV-2, the seroprevalence of IgA or IgG antibodies against SARS-CoV-2, and confounders.
3. Results
3.1. Participants
From 231 censused individuals, 229 (99%) were eligible market workers aged ≥18 years and free of self-reported conditions that would affect their immune systems. Of these eligible workers, 116 (51%) consented to participate in this study, with 109 (48%) providing a blood sample in the first serosurvey and 87 (38%) in the second serosurvey. Despite the relatively low participation rate, the age and sex distributions of the census population did not significantly differ from those who participated in the analyses. The participation rate by market differed significantly, being greater in market B (78%) than in market A (32%) (Supplementary Table S1). The median time between repeated blood sample extractions was 3.0 (interquartile range: 2.9, 3.1) months.
Participants were primarily women (77%, n = 84), <30 years of age (44%, n = 48, range = 18 to 79), had terminal education at the secondary level (61%, n = 67), and were of Ladin (non-indigenous) ethnicity (95%, n = 104). Their households used clean fuels for cooking (99%, n = 108), had no crowding, and the median household size was 5 (IQR: 4 to 6, range = 1 to 16). Most participants worked at market B (57%, n = 62), had worked at markets for 7 to 12 months (50%, n = 54, range = 1 week to 23 years), worked 6 or 7 days a week (73%, n = 80), and were vendors (81%, n = 88). Low physical activity was the most frequent general disease risk factor (36%, n = 39) (Supplementary Table S1 and Table 1).

Table 1.
Characteristics of public market workers in the first and second serosurveys a.
Between the first and second serosurvey, SARS-CoV-2 vaccination increased from 2% (n = 2) fully vaccinated and 9% (n = 10) partially vaccinated to 34% (n = 30) fully vaccinated and 48% (n = 42) partially vaccinated (p-value < 0.001). Of those vaccinated in the second serosurvey, 35% (25/72) received mRNA vaccines, 65% (47/72) viral vector vaccines, and none reported receiving mixed technologies. In the first serosurvey, adherence to preventive practices ranged from 45% (n = 49) for “always washing hands for ≥20 s” to 83% (n = 91) for “always using a mask completely covering the mouth and nose”. In general, the frequency of preventive practices increased between the first and second serosurvey (Table 1).
In the first serosurvey, the prevalence of SARS-CoV-2 infection was 13% (n = 14, 95% CI: 7–21), of which, only 15% (2/13) reported symptoms 14 days before nasopharyngeal swab collection. In comparison, the prevalence of SARS-CoV-2 infection in the second serosurvey was 1% (n = 1, 95% CI: 0–6%), and the participant did not report symptoms.
3.2. Seroprevalence
The seroprevalence of anti-S antibodies increased between serosurveys. IgA anti-S increased from 61% (95% CI: 52%, 71%) to 89% (95% CI: 80%, 94%) and 26% (n = 23) of participants with paired samples seroconverted. IgG anti-S increased from 53% (95% CI: 43%, 63%) to 91% (95% CI: 83%, 96%) and 37% (n = 32) of participants seroconverted. In contrast, anti-N antibodies were less common, only increasing modestly from 22% (95% CI: 15%, 31%) to 29% (95% CI: 20%, 39%); moreover, 15% (n = 13) of participants seroconverted and 7% (n = 6) seroreverted. The coefficient of variation for IgA anti-spike in the first and second surveys was 8% and 4%, for IgG anti-spike was 9% and 3%, and for IgG anti-nucleocapsid was 18% and 17%, respectively. The frequency of different combinations of IgA and IgG antibodies detected in paired blood samples is shown in Supplementary Table S2. The standardized seroprevalences were similar to non-standardized seroprevalences (Table 2).

Table 2.
Seroprevalence of IgA and IgG antibodies to anti-spike protein and IgG anti-nucleocapsid protein at the first serosurvey conducted from 6 July 2021 to 21 September 2021, and at the second serosurvey conducted from 6 October 2021 to 15 December 2021, in workers from two public markets in Guatemala.
Among non-vaccinated individuals, seroprevalence increased from 58% (95% CI: 47%, 68%) to 87% (95% CI: 60%, 98%) for IgA anti-S, from 47% (95% CI: 37%, 58%) to 60% (95% CI: 32%, 48%) for IgG anti-S, and from 21% (95% CI: 13%, 30%) to 40% (95% CI: 16%, 68%) for IgG anti-N. As expected, participants with at least one SARS-CoV-2 vaccine had higher seroprevalence. Seroprevalence by serosurvey, vaccination status, sociodemographic characteristics, and occupational characteristics is shown in Table 2.
3.3. Risk Factors for SARS-CoV-2 Exposure
3.3.1. Vendor Occupation
The effect of vendor occupation on SARS-CoV-2 exposure differed by sex. The adjusted OR for IgA anti-S was 12.4 (95% CI: 2.7, 56.3) for males but 0.7 (95% CI: 0.2, 2.2) for females, and the adjusted OR for IgG anti-S was 13.2 (95% CI: 2.1, 81.8) for males but 0.5 (95% CI: 0.1, 1.8) for females. In contrast, for IgG anti-N, the interaction term between vendor occupation and sex was not statistically significant, nor were the main effects for vendor occupation (Table 3). Of men with non-vendor occupations, 38% (n = 6) worked in market administration, 13% (n = 2) in security, and 51% (n = 8) in maintenance. Of women with non-vendor occupations, 60% (n = 12) worked in market administration, 10% (n = 2) in security, 15% (n = 3) in maintenance, and 15% (n = 3) in general assistance to vendors. Results of the crude analysis and the analysis without the interaction term for sex are available in Supplementary Table S3a–c.

Table 3.
Association of vendor occupation and other sociodemographic and occupational characteristics with SARS-CoV-2 exposure assessed by the seroprevalence of IgA anti-spike protein, IgG anti-spike protein, and IgG anti-nucleocapsid protein in public market workers.
3.3.2. Preventive Behaviors
Always using a mask covering the mouth and nose in the market during the month before the serosurvey reduced the odds of having antibodies against SARS-CoV-2. The adjusted OR for IgA anti-S protein was 0.2 (95% CI: 0.1, 0.9), for IgG anti-S protein was 0.2 (95% CI: 0.0, 0.7), and for IgG anti-N protein was 0.4 (95% CI: 0.2, 1.0) (Table 4). Results of the crude analysis are shown in Supplementary Table S4.

Table 4.
Association between preventive practices and SARS-CoV-2 exposure assessed by antibody seroprevalence. Odds ratios are adjusted for age group, last education level, wealth tertiles, number of household members, market, days per week working at the market, number of months since working in the market, and having received ≥1 vaccine dose.
4. Discussion
To the best of our knowledge, our study is the first in Central America to describe the burden of SARS-CoV-2 on public market workers and determine whether occupations in the market and adherence to preventive practices are associated with SARS-CoV-2 exposure. Although public market workers are essential frontline workers, placing them at high risk of SARS-CoV-2 infection [8], few studies have focused on this population. We assessed SARS-CoV-2 exposure by the presence of antibodies. Our study is unique because it measures IgA in addition to IgG antibodies. IgA is an essential immune response against SARS-CoV-2 by neutralizing virus entry at mucosal surfaces [14,15]. IgA also detects recent viral exposures because the IgA response arises earlier than IgG [16,17].
Antibody seroprevalence ranged from 22% for IgG anti-N in the first serosurvey to 91% for IgG anti-S in the second serosurvey. In comparison, a cross-sectional study conducted in June–July 2020 (one year earlier than our study) in eight public markets in Peru reported that the seroprevalences of IgG/IgM antibodies against SARS-CoV-2 ranged from 27% to 73% [18]. This high variability suggests that contextual characteristics of exposure influence seroprevalence.
In our first survey, more than half of market workers had antibodies against the SARS-CoV-2 S protein. Anti-S antibodies are produced in response to vaccination or natural infection. In Guatemala, as in many countries, vaccination occurred with staggered priorities, starting with frontline health personnel, then older adults and adults with comorbidities, and finally, the general adult population and adolescents [19]. At the time of our first serosurvey in July–October 2021, only 11% of study participants had received a vaccine dose. The high anti-S antibody levels detected in unvaccinated market workers indicate that at least half of them had already been exposed to SARS-CoV-2 through natural infection.
At the time of the second serosurvey, three months after the first serosurvey and one month after the expansion of the vaccination campaign to the general adult population, 82% of the participants had already received at least one dose of the vaccine. As expected, most of those vaccinated had anti-S antibodies, reflecting the vaccine’s effectiveness in inducing virus-specific antibodies. On the other hand, in unvaccinated participants, the seroprevalence of all antibody types, especially IgG anti-N protein, increased during the inter-survey period, suggesting sustained transmission of SARS-CoV-2 and the occurrence of natural infections. In this high transmission setting, vaccination should be prioritized.
For most market workers, exposure could have gone unnoticed because, in the first survey, only 14% of participants reported having tested positive since the start of the pandemic, and few reported symptoms. This is consistent with the rRT-PCR results from the swab tests we conducted during the first survey, with only two of the 14 rRT-PCR-positive workers reporting active COVID-19 infections with related symptoms in the 14 days before swab collection. Market workers may have also experienced mild symptoms, had asymptomatic infections, been in the presymptomatic phase of the disease, or the virus may not have cleared completely from the last infection. Thus, low awareness of SARS-CoV-2 infection status can contribute to virus spread within the market and into the community [6].
The seropositivity was higher for anti-S IgA than for anti-S IgG antibodies, suggesting that some participants had recent SARS-CoV-2 infections, possibly within one or two weeks of when IgA antibodies start to be detected, but IgG antibodies are not yet detectable [20]. The indirect ELISA test used in this study (Euroimmun, Lübeck, Germany) detects IgA antibodies around day 11 from symptom onset and IgG antibodies around day 21 [21]. This result is consistent with the onset of the infection wave that hit the study site in June 2021, about one month before the start of the first survey.
To distinguish antibodies triggered by natural infection (IgG anti-N) from those triggered by vaccination (IgG anti-S), we next measured IgG anti-N antibody positivity [22]; however, the results of this effort were inconsistent. Interpreting these serological results may be challenging due to the involvement of several immune response factors, such as differences in serological test sensitivities, higher antigenicity of S proteins than N proteins, and differing antibody durations after infection or vaccination [16].
We hypothesized that marketplace activities involving routine interaction with shoppers (vendor occupation) would be positively associated with SARS-CoV-2 exposure, measured as antibody seroprevalence. In a cross-sectional study conducted in Minnesota grocery stores, anti-S IgG seropositivity was more than twice as high among workers who had direct contact with shoppers than in workers without direct contact [23]. Interestingly, our study found no association between vendor occupation and antibody seroprevalence among female market workers. However, among men, the odds of anti-S IgA seropositivity were twelve times higher in workers with vendor occupations than in those engaged in non-vendor activities, with a similar result for anti-S IgG antibodies. The difference between the sexes could be because most of the non-vendor men worked in infrastructure maintenance, where there was no interaction with shoppers or other market workers, while women’s non-vendor roles may still have exposed them to vendors and shoppers. Differences in immune response between women and men could also contribute to the observed difference by sex, as women have been shown to develop more B cells than men [24]. Furthermore, in addition to activities in the market, women may be more exposed to the virus when doing household chores and taking care of their family [25]. This shows that women market workers are more vulnerable to exposure to SARS-CoV-2 than men.
Using a mask that covered the nose and mouth was significantly associated with lower seroprevalence (adjusted by having received ≥1 vaccine dose), suggesting that masking effectively reduced virus acquisition in this setting and should continue to be encouraged during high transmission periods to reduce occupational exposure [1]. In addition, between the first and second serosurvey, we observed a significant increase in the percentage of workers who reported always practicing physical distancing when eating and always cleaning their hands with soap and water or alcohol for at least 20 s. This change could be due to several factors, such as a response to the new wave of SARS-CoV-2 that emerged during this period, which motivated workers to self-protect themselves to avoid losing their income, as local authorities closed the stalls of SARS-CoV-2-infected vendors for two weeks, or a change in COVID-19 awareness triggered by participation in the study, as participants received more information about the disease, reinforcement of personal protection measures, and regular health monitoring by study staff.
Regarding the sociodemographic and health-related variables that were evaluated (age, educational level, wealth, number of members in the household, market, days per week at the market, months since working in the market, and having one vaccine dose or more) along with occupation, we identified higher than secondary education and being in a high wealth tertile as statistically significant protective factors. However, the model was specified to address the association between occupation and exposure and only considered the sociodemographic variables as potential confounders, so caution is needed when interpreting associations outside the aim of the model. Further studies are needed to determine why these factors protect against exposure to the virus.
The rapid increase in seropositivity against SARS-CoV-2 observed in the study highlights how rapidly the virus is transmitted in a market environment, which can also occur with other viral respiratory infections. This spread can occur in individuals with or without signs and symptoms of disease, so the authorities of these markets must develop clear protocols to contain possible outbreaks of infection and keep the worker population constantly aware of the need to report suspected cases and initiate the actions defined in these containment protocols. Personal protection measures have been shown to protect against exposure to SARS-CoV-2, especially the correct use of the mask, so its practice should be reinforced during peaks of disease transmission, especially in workers who serve shoppers or who interact with suppliers.
The main limitation of our study was the low participation rate since less than half of market workers consented to participate, causing low precision in our estimates. However, the coefficients of variation calculated for general seroprevalence showed satisfactory values, mainly for IgG anti-S and IgA anti-S antibodies. As perceived by study staff, the main reasons for reluctance to participate were fear of providing blood or swab samples, lack of time to participate, disbelief about COVID-19, and fear of the consequences of getting a positive result, both for their health and for their income. To address potential selection bias, we calculated a standardized seroprevalence by reweighting the study population to the distribution of gender, age, and market location of the whole market population. We found no evidence of selection bias as the standardized seroprevalence was similar to the seroprevalence estimated from the study population. We believe these results can be generalized for similar public municipal markets of low- and middle-income countries. A second limitation pertains to the possibility of non-differential misclassification of the outcome, as infections with a minimum evolution of 11 days for IgA and 24 days for IgG or older than six months might not have been detected with our serological test [21]. Finally, there could also be non-differential misclassification regarding preventive practices because the frequency of adherence to preventive practices reported in the interview may not reflect actual practices.
5. Conclusions
We found that at least half of the unvaccinated market workers had already been exposed to SARS-CoV-2 at the first serological survey, before vaccination, and that the seroprevalence increased rapidly in three months intersurvey both by vaccination or natural infection (seen in unvaccinated participants). These results show a high risk of exposure of market workers to SARS-CoV-2, especially those who interact with shoppers. It highlights the need for the authorities to develop protocols to contain respiratory disease outbreaks in the markets, including vaccination, reinforcement of personal protection measures, especially mask use, and maintenance of awareness about disease transmission among the market community.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/covid3090097/s1, Supplementary Table S1: Baseline characteristics of public market workers who participated in the census (June to July 2021), first serosurvey (July to September 2021) and second serosurvey (October to December 2021); Supplementary Table S2: Frequency of antibody combinations against SARS-CoV-2 detected in paired blood samples collected between 6 July 2021 to 21 September 2021, and from 6 October 2021 to 15 December 2021, in two public markets workers of Guatemala (1 = antibody detected, 0 = antibody not detected); Supplementary Table S3a: Association of vendor occupation with exposure to SARS-CoV-2 assessed by the seroprevalence of IgA anti-spike protein in public market workers; Supplementary Table S3b: Association of vendor with exposure to SARS-CoV-2 assessed by the seroprevalence of IgG anti-spike protein in public markets workers; Supplementary Table S3c: Association of vendor with exposure to SARS-CoV-2 assessed by the seroprevalence of IgG anti-nucleocapsid protein in public markets workers; Supplementary Table S4a: Association of preventive practices with exposure to SARS-CoV-2 assessed by the seroprevalence of IgA anti-spike protein in public markets workers; Supplementary Table S4b: Association of preventive practices with exposure to SARS-CoV-2 assessed by the seroprevalence of IgG anti-spike protein in public markets workers; Supplementary Table S4c: Association of preventive practices with exposure to SARS-CoV-2 assessed by the seroprevalence of IgG anti-nucleocapsid protein in public markets workers.
Author Contributions
Conceptualization: L.M.G., R.M.-C., E.Z. and C.C.-R. Data curation: L.M.G., R.M.-C. and J.C.R. Formal analysis: L.M.G., J.C.R. and R.M.-C. Funding Acquisition: L.M.G., R.M.-C., E.Z. and C.C.-R. Investigation: L.M.G., R.M.-C. and E.M. Methodology: L.M.G., R.M.-C., M.R.L., B.L., J.C.R., E.Z. and C.C.-R. Software: J.C.R. Project Administration: R.M.-C. and L.M.G. Supervision: R.M.-C., L.M.G. and E.M. Validation: R.M.-C. and M.R.L. Visualization: L.M.G. Writing—original draft: L.M.G. and R.M.-C. Writing—review and editing: L.M.G., R.M.-C., C.C.-R., M.R.L., B.L., J.C.R., E.M. and E.Z. All authors have read and agreed to the published version of the manuscript.
Funding
Funding was provided by the Centers for Disease Control and Prevention (CDC) via the Center for Health Studies, Universidad del Valle de Guatemala (CES UVG) Cooperative Agreement Award number: GH002243, Surveillance and Research for the Innovation and Sustainability of Public Health Actions, COVID-19 Supplemental Funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. The study protocol was reviewed and approved by the National Health Ethics Committee of the Ministry of Health of Guatemala under protocol 30-2020 and the Research Ethics Committee of the Center for Health Studies from Universidad del Valle de Guatemala under protocol 221-11-2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to restrictions on permitted uses and disclosure of data.
Acknowledgments
The authors thank the support of market workers; authorities and personnel of the Municipality of Santa Catarina Pinula; and Nazario López, Aura Paniagua, Jaqueline Chávez, and Víctor Sicajau during fieldwork.
Conflicts of Interest
The authors declare no conflict of interest.
References
- OPS. Recomendaciones Para Prevenir la Transmisión de la COVID-19 en Ferias y Mercados de Alimentos; Oranización Panamericana de la Salud: Washington, DC, USA, 2021. [Google Scholar]
- Marchiori, Teresa and Mariana Prandini Assis. The Impact of COVID-19 Laws on Street Vendors and Market Traders: Trends and Insights from Latin America; WIEGO Resource Document No. 21; WIEGO: Manchester, UK, 2021. [Google Scholar]
- Frieden, T.R.; Lee, C.T. Identifying and Interrupting Superspreading Events-Implications for Control of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg. Infect. Dis. 2020, 26, 1059–1066. [Google Scholar] [CrossRef] [PubMed]
- Vasquez-Apestegui, B.V.; Parras-Garrido, E.; Tapia, V.; Paz-Aparicio, V.M.; Rojas, J.P.; Sanchez-Ccoyllo, O.R.; Gonzales, G.F. Association between air pollution in Lima and the high incidence of COVID-19: Findings from a post hoc analysis. BMC Public Health 2021, 21, 1161. [Google Scholar] [CrossRef] [PubMed]
- Lan, F.Y.; Suharlim, C.; Kales, S.N.; Yang, J. Association between SARS-CoV-2 infection, exposure risk and mental health among a cohort of essential retail workers in the USA. Occup. Environ. Med. 2021, 78, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Lan, F.Y.; Wei, C.F.; Hsu, Y.T.; Christiani, D.C.; Kales, S.N. Work-related COVID-19 transmission in six Asian countries/areas: A follow-up study. PLoS ONE 2020, 15, e0233588. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.Z.; Zhou, P.; Han, D.B.; Wang, W.C.; Cui, C.; Zhou, R.; Xu, K.X.; Liu, L.; Wang, X.H.; Bai, X.H.; et al. Investigation on a cluster epidemic of COVID-19 in a supermarket in Liaocheng, Shandong province. Zhonghua Liu Xing Bing Xue Za Zhi 2020, 41, 2024–2028. [Google Scholar] [CrossRef] [PubMed]
- Dooling, K.; Marin, M.; Wallace, M.; McClung, N.; Chamberland, M.; Lee, G.M.; Talbot, H.K.; Romero, J.R.; Bell, B.P.; Oliver, S.E. The Advisory Committee on Immunization Practices’ Updated Interim Recommendation for Allocation of COVID-19 Vaccine—United States, December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 69, 1657–1660. [Google Scholar] [CrossRef] [PubMed]
- MSPAS. Situación de COVID-19 en Guatemala. 2022. Available online: https://tablerocovid.mspas.gob.gt/ (accessed on 26 April 2022).
- INE. XII Censo Nacional de Población y VII de Vivienda. 2018. Available online: https://www.censopoblacion.gt/ (accessed on 26 April 2022).
- Agarwal, A.; Ranjan, P.; Rohilla, P.; Saikaustubh, Y.; Sahu, A.; Dwivedi, S.N.; Aakansha; Baitha, U.; Kumar, A. Development and validation of a questionnaire to assess preventive practices against COVID-19 pandemic in the general population. Prev. Med. Rep. 2021, 22, 101339. [Google Scholar] [CrossRef] [PubMed]
- Corman, V.M.; Landt, O.; Kaiser, M.; Molenkamp, R.; Meijer, A.; Chu, D.K.; Bleicker, T.; Brunink, S.; Schneider, J.; Schmidt, M.L.; et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance 2020, 25, 2000045. [Google Scholar] [CrossRef] [PubMed]
- CDC. Stay Uo to Date with Your COVID-19 Vaccine. 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html?s_cid=11747:cdc%20fully%20vaccinated%20definition:sem.ga:p:RG:GM:gen:PTN:FY22 (accessed on 26 April 2022).
- Sterlin, D.; Mathian, A.; Miyara, M.; Mohr, A.; Anna, F.; Claer, L.; Quentric, P.; Fadlallah, J.; Devilliers, H.; Ghillani, P.; et al. IgA dominates the early neutralizing antibody response to SARS-CoV-2. Sci. Transl. Med. 2021, 13, eadb2223. [Google Scholar] [CrossRef] [PubMed]
- Takamatsu, Y.; Omata, K.; Shimizu, Y.; Kinoshita-Iwamoto, N.; Terada, M.; Suzuki, T.; Morioka, S.; Uemura, Y.; Ohmagari, N.; Maeda, K.; et al. SARS-CoV-2-neutralizing humoral IgA response occurs earlier but modest and diminishes faster compared to IgG response. bioRxiv 2022, 10, e0271622. [Google Scholar] [CrossRef]
- Galipeau, Y.; Greig, M.; Liu, G.; Driedger, M.; Langlois, M.A. Humoral Responses and Serological Assays in SARS-CoV-2 Infections. Front. Immunol. 2020, 11, 610688. [Google Scholar] [CrossRef]
- Padoan, A.; Sciacovelli, L.; Basso, D.; Negrini, D.; Zuin, S.; Cosma, C.; Faggian, D.; Matricardi, P.; Plebani, M. IgA-Ab response to spike glycoprotein of SARS-CoV-2 in patients with COVID-19: A longitudinal study. Clin. Chim. Acta 2020, 507, 164–166. [Google Scholar] [CrossRef]
- Tovar, M.; Peinado, J.; Palomino, S.; Llanos, F.; Ramirez, C.; Valderrama, G.; Calderon, R.I.; Williams, R.B.; Velasquez, G.E.; Mitnick, C.D.; et al. Prevalence of Severe Acute Respiratory Syndrome Coronavirus 2 Antibodies Among Market and City Bus Depot Workers in Lima, Peru. Clin. Infect. Dis. 2022, 74, 343–346. [Google Scholar] [CrossRef]
- MSPAS. Plan Nacional de Vacunación Contra la COVID-19. República de Guatemala; Ministerio de Salud Pública y Asistencia Social: Guatemala City, Guatemala, 2021. [Google Scholar]
- Baumgarth, N.; Nikolich-Zugich, J.; Lee, F.E.; Bhattacharya, D. Antibody Responses to SARS-CoV-2: Let’s Stick to Known Knowns. J. Immunol. 2020, 205, 2342–2350. [Google Scholar] [CrossRef]
- Krone, M.; Gutling, J.; Wagener, J.; Lam, T.T.; Schoen, C.; Vogel, U.; Stich, A.; Wedekink, F.; Wischhusen, J.; Kerkau, T.; et al. Performance of Three SARS-CoV-2 Immunoassays, Three Rapid Lateral Flow Tests, and a Novel Bead-Based Affinity Surrogate Test for the Detection of SARS-CoV-2 Antibodies in Human Serum. J. Clin. Microbiol. 2021, 59, e0031921. [Google Scholar] [CrossRef] [PubMed]
- Theel, E. SARS-CoV-2 Serologic Testing. In Clinical Microbiology Procedures Handbook; Humphries, R.M., Simner, P.J., Eds.; Wiley: Washington, DC, USA, 2021. [Google Scholar]
- Vachon, M.S.; Demmer, R.T.; Yendell, S.; Draeger, K.J.; Beebe, T.J.; Hedberg, C.W. SARS-CoV-2 Seroprevalence Survey in Grocery Store Workers-Minnesota, 2020–2021. Int. J. Environ. Res. Public Health 2022, 19, 3501. [Google Scholar] [CrossRef] [PubMed]
- Qi, S.; Ngwa, C.; Morales Scheihing, D.A.; Al Mamun, A.; Ahnstedt, H.W.; Finger, C.E.; Colpo, G.D.; Sharmeen, R.; Kim, Y.; Choi, H.A.; et al. Sex differences in the immune response to acute COVID-19 respiratory tract infection. Biol. Sex Differ. 2021, 12, 66. [Google Scholar] [CrossRef] [PubMed]
- Aleksanyan, Y.; Weinman, J.P. Women, men and COVID-19. Soc. Sci. Med. 2022, 294, 114698. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).