Abstract
Current rehabilitation protocols for transitioning patients to late-stage recovery, evaluating return-to-play (RTP) clearance, and assessing tendon characteristics exhibit significant heterogeneity. Clinicians frequently interpret and apply research findings based on individual philosophies, resulting in varied RTP criteria and performance expectations. Despite medical clearance, patients recovering from Achilles tendon (AT) injuries often exhibit persistent impairments in muscle volume, tendon structure, and force-generating capacity. Inconsistencies in assessment frameworks, compounded by a lack of quantitative data and the utilization of specific metrics to quantify certain strength characteristics (endurance, maximal, explosive, etc.) and standardized protocols, hinder optimal functional recovery of the plantar flexors during the final stages of rehabilitation and RTP. With this in mind, the aim of this integrative review was to provide an overview of AT rehabilitation, with particular critique around mid-stage strengthening and the use of the heel-raise assessment in milestoning rehabilitation progress. From this critique, new perspectives in mid-stage strengthening are suggested and future research directions identified.
1. Introduction
The Achilles tendon (AT) is the largest, thickest, strongest tendon in the human body, a common tendon shared between the gastrocnemius and soleus muscles of the posterior leg, and is responsible for the transmission of force [,,]. The AT has the capacity to withstand forces up to 11× BW during high-speed running and 15× BW in gymnastic landing [,,]. Despite the strength of the AT, the rupturing of this tendon is a relatively frequent injury, particularly in high-impact sports. Hoeffner et al. (2022), however, contended that despite a sizeable number of people suffering an Achilles tendon rupture (ATR), the evidence-based knowledge of best practice for rehabilitating a rupture remains unclear, and likely explains the reports of persistent muscle weakness, decreased muscle volume, tendon elongation and continued asymmetry with incomplete return to pre-injury levels of form and function [,,,,,].
In terms of injury to the AT, high-force impacts during eccentric loading in dorsiflexion and knee and hip extension are reported to be the primary injury mechanisms []. The most common injuries that occur are tendinopathy at the mid-portion and insertion point of the AT, along with acute ruptures [,]. Various factors have been proposed to explain the injury of the AT, including age, sex, sport type, obesity, antibiotics (fluoroquinolones), over training/lack of recovery, poor vascularization, high external loads from sporting/physical activity, and altered cell response [,,,]. Over the past few decades, the incidence of Achilles tendon rupture (ATR) has increased significantly, rising from 11 to 37 per 100,000 individuals []. In the United States, males accounted for 77.1% (25,374 cases), while females represented 22.9% (7533 cases). The overall incidence was 3.2 and 0.9 per 100,000 persons/year for males and females, respectively. Sports involving rapid changes in direction—such as basketball (42.6%), soccer (9.9%), football (8.4%), tennis (6.9%), and running/hiking/stretching (5.8%)—account for most ATRs []. Activities requiring high-impact movements, intense deceleration, and directional changes (e.g., basketball, gymnastics, football, and volleyball) pose an elevated risk of injury [,].
Treatment for ATR is categorized into surgical and conservative options, with the space of the tendon gap and activity level that the patient is returning to after rehabilitation determining what method a surgeon will suggest, understanding that a gap of 10 mm or greater is the current minimum threshold where surgery is considered []. In terms of rehabilitation options, following an AT rupture there are two options: either a conservative or surgical approach. Conservative treatment typically involves cast immobilization, functional bracing, or a combination of both interventions []. Shorter-term cast immobilization followed by a functional mobilization in a brace leads to a faster increase in dorsiflexion ROM and an expedited return to normal physical activity [,]. The surgical intervention has three main repair options, open, percutaneous, and SpeedBridge, all of which have their benefits and limitations. Following injury there are key principles in the rehab process in respect to the timeline of tendon healing. The healing phases include the acute inflammatory phase (up to 1–2 weeks) in which the inflammatory cells remove injured tissue. Subsequently, there is the proliferative phase (up to 4 weeks), in which fibroblasts produce Type I collagen, increasing tendon strength. Lastly, the transition to the remodeling phase which can last up to 18 months to complete the healing process, and the development of the final tendon structure takes place. The maturation of the tendon depends on the ability to improve tensile strength and elasticity [,,].
Regardless of whether a surgical or non-surgical decision is made on the AT, both options will result in the formulation of treatment plans that provide rehabilitation guidelines for the clinician and patient. Post-operative rehabilitation has been broken into five stages and the guidelines typically progress in a sequenced manner that progress from the acute inflammatory/immediate post-operative phase (up to 2 weeks); early-stage rehabilitation/controlled mobilization—2–6 weeks; mid-stage/intermediate rehabilitation—6–12 weeks; late-stage rehabilitation—12–24 weeks; and the return to sport phase—>24 weeks. However, depending on the practitioner/researcher, the number of stages and timelines will vary. The focus of this article is on the mid-stage rehabilitation phase, particularly the strengthening aspects of this phase. Researchers have reported that after rehabilitation, jumping performance in athletes and running gait patterns are negatively affected by inadequate strength of the plantar flexor [,]. These performance impairments have been attributed to inadequate strength and physiological/morphological changes in the calf musculature, which typically provide the focus of mid-stage rehabilitation []. Given this observation, it may be that aspects of strength assessment and milestoning could be improved during this phase of rehabilitation, with this contention explored in this integrative review.
2. Search Strategy
A hybrid search strategy was used to find the information for this integrative review, which is summarized in Figure 1. The overarching focus was AT rehabilitation rupture programs/protocols, with an emphasis on the mid-stage strengthening phase, from both surgical and conservative pathways. The keywords and different combinations used in the search are listed in Figure 1, as are the relevant sources, which involved both database and website searches for a snapshot of the information needed to write this article. The article has tried to integrate peer-reviewed research with assessments and protocols from clinical online resources, where these clinics have adapted the research to implement into their practices, based on their current understanding and application of the evidence base. It needs to be noted that the quality of the studies were not quantified for two reasons: (1) many of the resources compiled were assessment batteries from clinics and hospitals; and (2) the focus of the section was to highlight the assessments that were currently used in the field and show the commonality alongside the variability in these tests, thereby providing reader’s insight into the challenges associated with AT testing. Given this approach there was limited exploration of the effects of age, BMI, comorbidities, etc., on the assessment of the AT.
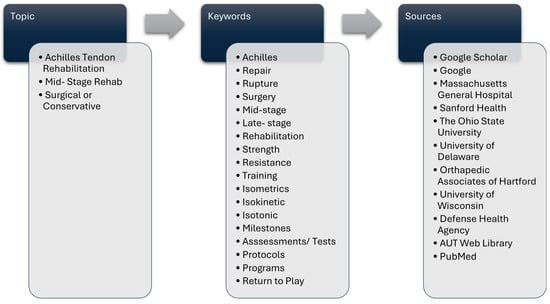
Figure 1.
AT rehabilitation rupture guideline search strategy.
A glossary of terms is provided for the reader to improve clarity and readability (see Table 1).

Table 1.
Glossary of terms.
3. Mid-Stage Treatment of ATR
The mid-stage phase is typified by the termination of cell proliferation, that is, of the extracellular matrix components synthesized []. During the proliferation phase, macrophages and tenocytes synthesize new connective tissue, including Type III collagen fibers, which are mechanically less durable. In this stage, tenocytes primarily proliferate within the epitenon, the connective tissue sheath surrounding the tendon []. During this phase consistent loading is imperative to promote healing and restore function. Normal tendon development and homeostasis are closely linked to the intensity and vector of mechanical loading to which the tissue is exposed. Tendon injury and degeneration may be related to alterations in the way the tendon is loaded. Through loading, the tendon will undergo mechanotransduction, which promotes cellular signaling to restore normal tendon structure and function. During this phase, the AT continues to remodel for (>12 months) after injury or surgery [,]. The repair and regeneration process includes the collagen fibers undergoing a development process and reorienting themselves parallel to the direction of mechanical stress. Conversely, the regenerated tendon tissue exhibits a scar-like structure and reduced biomechanical properties compared to the native healthy tendon [,,]. Moreover, tendon elongation occurs for the first 12 weeks after surgery [], which can cause end-range-of-motion weakness and needs to be accounted for when strengthening the AT. Clinical applications of this process can form the basis of the rehabilitation process following tendon injury [,].
Along with collagen reorganization and improved tensile strength, muscle atrophy represents another key physiological challenge that affects rehabilitation outcomes. As early as five days after inactivity, muscle disuse—particularly in a detrained limb—can cause marked atrophy, reduced strength, and functional decline []. Long-term follow up after AT rupture often reveals a reduction in muscle mass/strength, along with elongation of the tendon, which negatively impacts the single-leg heel-raise test. All these factors negatively affect the RTP rehabilitation process and patient outcomes [,].
The goals of the mid-stage phase are to normalize gait patterns, improve balance, restore closed-chain ankle dorsiflexion ROM, and restore plantar flexor strength. An exemplary table (Marrone et al., 2024) giving clinicians a blueprint of the AT rehabilitation process and summarizing the goals, potential interventions, common milestones and precautions for each of these phases is outlined in Table 2 []. The timelines in this phase are generally consistent between patients recovering from conservative or surgical interventions [,,,]. Key progressions include transitioning to full weight bearing, reducing heel wedge height, and eventually shifting from a brace or boot to athletic footwear. Strengthening is typically initiated using resistance bands or low-intensity isometrics in a seated position to avoid overstretching the AT, especially with the knee extended. The purpose of the ensuing sections is to provide a critical review of the current mid-stage strengthening assessments and milestones and provide suggestions and new perspectives on improving the assessments and metrics used in this phase of rehabilitation.

Table 2.
Current rehabilitation stages for ATR surgical intervention. Reproduced from Marrone (2024), with permission [].
4. Mid-Stage Rehabilitation Strengthening
The strength milestones/goals associated with mid-to-late-stage rehabilitation of the AT have been collated and synthesized in Table 3. These milestones have been loosely grouped under two strength qualities, strength endurance and maximal strength, with the caveat that the maximal-strength measures range from static/isometric/zero-velocity measures to more dynamic/isotonic–isokinetic/higher-velocity measures. The aim of the section is to summarize the protocols and measures used by practitioners and researchers, and to highlight limitations should they exist.

Table 3.
Review of AT strength protocols and assessments.
5. Strength Endurance Protocol Milestones for Clearance into Late-Stage Rehab
In the context of strength endurance training, most practitioners employed isoinertial or isotonic bodyweight exercises. The most commonly used exercise and assessment was the single-leg heel raise, performed with the affected leg and often compared to the non-affected leg. These exercises were typically executed on flat surfaces, low-angle (10°) incline boards, or the edge of a step. The load on the injured limb was monitored by prescribing a target heel height for each repetition, assessed either qualitatively (e.g., visual estimation) or using quantitative technologies such as electrogoniometers [], linear position transducers [], motion capture [], a light beam device [], and elastic band devices []. There was notable disagreement among practitioners regarding the optimal point along the strength continuum to emphasize, and which specific assessment parameters were most appropriate for determining readiness to progress to the next training phase. Strength progression prescriptions varied widely in terms of repetitions, ranging from achieving a single repetition at a height equivalent to the non-injured side [] to five sets of 25 heel raises []. Tempo was rarely addressed; however, some protocols used 60 heel raises per minute [] or 30 heel raises per minute []. All the heel raises tests used isoinertial loading in the form of the patient/subject’s body weight, with an emphasis on the concentric loading phase of the movement pattern—in particular, achieving heel height comparable to the unaffected leg.
With regard to the variables quantified, the number of repetitions or repetitions per minute were the most common measurements. Silbernagel et al. (2010) quantified the work associated with each repetition by measuring the height of each repetition with a linear transducer and providing the total displacement for the set []. Three research/practitioner groups detailed the limb symmetry index as a function of the repetitions performed by the affected and unaffected limbs, with the LSI ranging from 75 to 90% to clear a patient/athlete to progress onto the late stage of the RTP process [,,].
6. Maximal-Strength Protocols/Milestones for Clearance into Late-Stage Rehab and/or Clearance for Return to Play
This section covers strength and power assessments and protocols used to evaluate the Achilles tendon (AT) and surrounding musculature during recovery, whether from an AT rupture treated conservatively or surgically, or from tendinopathy. Maximal strength can be assessed at zero velocity (isometric contractions) or across a range of velocities using isotonic, isoinertial, or isokinetic contractions. In the latter case, when force is measured across a range of velocities, it can also be interpreted as power output (i.e., Power = Force × Velocity). A distinction must be made between power and explosive power—the latter refers to the ability to produce maximal force and velocity in a very short time. Explosive power becomes particularly relevant during the late-stage and return-to-sport phases of rehabilitation due to the high force–high velocity demands of sport-specific movements.
Therefore, maximal strength assessments can be plotted along a continuum of movement velocity, ranging from zero velocity to high-velocity isokinetic/isotonic/isoinertial movements. The isometric testing was conducted from different seated knee positions, either with a bent knee [] or a straight leg []. Along with varying knee positions, different degrees of ankle range of motion (ROM) were utilized, with the most common angles being 20° of dorsiflexion, 0° (neutral), and 20° of plantarflexion [,,]. All practitioners/researchers used peak force or torque as the primary metric of interest. Regarding assessment volume, most researcher/practitioners did not specify details, but those that did reported a range between three sets of 3 s contractions [], two sets of 3–5 s contractions [], and three sets of 6–8 s contractions []. The LSI appeared to have a wide range of progression criteria, with percentages varying from 75% [] to 90% [] for different ankle range-of-motion positions.
Isokinetic assessments were classified into slow- and high-velocity protocols; however, it needs to be noted that the velocities being tested in this phase were nowhere near the velocities associated with limb movement during sprinting. Slow-velocity isokinetic assessments ranged from 24°/s to 96°/s [] with the most common velocities of 30°/s and 60°/s. The conventional metric utilized for these tests was peak torque except when researchers incorporated passive stiffness; to measure passive stiffness an isokinetic dynamometer is typically used to move the plantar flexors at a speed of 5 deg/s from 10° of plantar flexion (neutral) to a static hold at 80% of the participant’s maximal passive dorsiflexion angle. In some cases, researchers attach electrodes to the plantar flexor muscles to ensure that no muscle activity is initiated [,]. The body position differed from prone to supine to seated along with various hip, knee, and ankle positions.
Additionally, higher velocity isokinetic tests ranged from speeds of 120°/s to 240°/s. The volume used ranged from 1 set of 20 repetitions [] to 3 sets of 10 repetitions []. When utilizing these higher velocities and higher repetition schemes, the researchers examined the limb strength deficit of the plantar flexors [,] and included LSI measures.
Lastly, few researchers/practitioners have examined power using isotonic or isoinertial contractions during this phase of AT rehab. Silbernagel et al. (2006) utilized two variations of a single-leg heel raise test (concentric and eccentric–concentric), performing three repetitions at four different predetermined weights, while attaching a linear position transducer to the heel to determine power output [].
7. Summary and Limitations
There seems to be a general consensus on a number of assessments/protocols that researchers and clinicians use from a rehabilitation perspective, during the mid-stage strengthening of the AT. First, the LSI must be above a certain percentage, ranging from 75 to 90%, regarding the number of reps and/or the work performed from the affected side to unaffected side, irrespective of the type of muscle contraction and strength quality measured. Second, performing a heel-raise test at the same height as the unaffected limb for a certain number of repetitions appears to be a common strength milestone. While several aspects of the heel-raise assessment are standardized, significant disagreement remains over optimal parameters for progression in the rehabilitation process, such as repetition number, movement tempo, intensity, lower-limb positioning (straight vs. bent knee), LSI and work-based symmetry percentage [,,,,]. Silbernagel et al. (2010) addressed measurement variability by using a linear position transducer to objectively determine heel-raise height and calculate work-derived LSI []. They found that at 12 months, subjects’ LSI based on heel raise repetitions was 95%; however, when taking into account the work associated with the repetitions, the LSI was 76% []. Clinicians and their patients would benefit from a more nuanced approach to quantifying the HRT, other than counting repetitions or repetitions per unit time.
Regarding maximal strength, research is limited on the appropriate time frame for safe implementation of max-strength testing during AT rehabilitation. At three months, Groetelaers et al. (2014) and Don et al. (2007) examined isometric and isokinetic peak/torque output, respectively [,]. However, Groetelaers et al. (2014) did not report the total value of peak forces, just the LSI measures from different time points []. Don et al. (2007) was the only article that examined and presented peak torque values in the mid-stage strength portion of the rehabilitation process []. In comparison, the ACL rehabilitation literature suggests that isokinetic testing is generally appropriate around 15 weeks post-injury []. Furthermore, there is little agreement on the most suitable methods for measuring strength and the function of the AT and its surrounding musculature in the literature. During mid-stage rehab, one main performance goal is to restore absolute strength to the AT and the MTU []. However, reporting on this objective varies widely across studies. Researchers use different anatomical setups—including varying hip, knee, and ankle positions—and measure strength across diverse ankle joint ranges, making it difficult for clinicians to identify reliable and consistent testing protocols [,,,,,]. Additionally, the volume differs within the research on AT strength assessment following or during the rehabilitation process. Furthermore, this variability represents a significant limitation in the literature surrounding a key performance indicator in the rehab process, which not only has implications for future performance in later stages of rehab but also affects RTP performance and the ability to successfully return to sport at a high level of play months/years after injury. The improper progression of kinetic linking, which requires proper anatomical structure involvement, appropriate ROM, activation, strength, and the coordination of the musculature around the joint, will cause biomechanical dysfunction of the limb and affect gait performance []. The rehab process needs a solid foundation to start with or else the entire process is affected negatively. For example, it has been documented that after an ATR, there is prolonged strength deficit, which can be up to 30% compared with the uninjured [].
In summary, while the heel-raise test is considered a foundational test [], without the use of technology, the tests yield only basic data on heel-raise performance, which fails to optimize clinical decision-making and could potentially delay recovery timelines. The American Physical Therapy Association, published a vision statement, titled: “Vision 2020”, which served as a “call to arms” for the maturation of the physiotherapeutic profession, specifically citing evidence-based medicine as a priority, Sullivan et al. (2011) []. The aim was to improve the objectivity of the examination and intervention processes by implementing modern technologies in the interest of justifying reimbursement in the wake of changing healthcare policies. It has created an initiative to provide physical medicine professionals, such as physiotherapists, with tools that are user-friendly, help synthesize and interpret data yet are also cost-effective choices. This “call to arms” highlights the integration of technology with metrics {# of reps and height of each repetition and the total work (BW × total distance)} that correlate to the neuromuscular outputs of those specific strength qualities targeted during rehabilitation. The next section examines how this approach could be applied in everyday AT rehabilitation practices.
8. Mid-Stage Strengthening of the AT: New Perspectives
Mechanotransduction refers to a process where the body converts mechanical loading into cellular signaling, which ultimately drives tissue remodeling []. Mechanical loading usually comes in the form of a force, whether it be shear, tensile or compressive in nature. If these forces are of sufficient rate, magnitude and duration, they will initiate deformation of the cells in the tissue of interest, the tendon in this case. Signaling proteins within the cells in turn initiate the tissue repair and remodeling process []. As a result, larger and/or stronger tissue will be added. Mechanotransduction is an ongoing process, and if the mechanical stimuli are withdrawn or withheld, then repair and remodeling typically slows, ceases and in a very short time reverts to baseline. Since this process is initiated by mechanical loading, it would seem important to monitor the forces applied and understand the adaptive response thereafter. By adopting such an approach, clinical understanding should be enhanced and patient outcomes expedited. With this in mind, this section is very much couched within a mechanotransducive approach, particularly understanding the mechanical loading applied to the tendon.
Since strength is a very coveted attribute, during the rehabilitation process a thorough understanding of the strength needs of the musculotendinous tissues is needed. Central to the strengthening of any tissue is the principle of progressive overload; systematic and safe loading via a periodized plan is a core tenet of this principle. Such a periodized approach is thought fundamental to efficiently regain those qualities to successfully progress the rehab process []. A simple diagram proposing how various strength qualities can be progressively overloaded during the different stages of ATR rehabilitation is presented in Figure 2. Simply explained, strength training can be progressed by simply manipulating volume as measured by the number of reps performed and/or time under tension in an isometric contraction, and the intensity of contractions as measured by force output or a derivative, e.g., impulse, rate of force development (RFD). It is suggested that strength training is low in intensity and progresses to potentially high volumes (strength endurance training) during early-stage rehab []. This is followed by a decrease in volume and increase in intensity, during the mid-stage rehab phase when the aim is to increase the maximal strength of the tendon. Finally, in late-stage rehab, strength training can be high intensity, low volume in nature; this type of explosive strength training is particularly important for athletes returning to training and play.
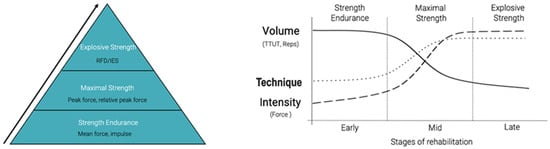
Figure 2.
Proposed periodized plan for the assessment and training of different strength qualities across the various stages of rehabilitation. Key: RFD = rate of force development; IES = index of explosive force; TTUT = time under tension.
It should be noted that the assessment of strength and power has become overwhelmingly complex with the advent of technologies such as force plates, with some force plate manufacturers having nearly 200 variables that can be quantified to describe various movements. The authors suggest that the clinician should funnel variable selection down to five to six variables that they understand the mechanistic underpinning of, ensure that the variable is relevant to the stage of rehabilitation, and know the reliability of the variables they choose to monitor. In this regard it is suggested that the variables detailed in Figure 2 should be used in the different stages of rehabilitation. There is a difficulty in measuring and reporting peak force, which is not the best measure to describe strength endurance or explosive strength capability. Furthermore, when using devices such as force plates that sample at high rates such as 1000 Hz, peak force represents your force capability for 1/1000th of a second; many would argue that is not a measure of overall force capability. To these ends it is recommended that during the strength endurance–early rehabilitation stage, measures such as mean force or total impulse (area under the force/time curve) be used as these variables will better represent changes in overall force capability. As the clinician progresses the rehabilitation of the AT, maximal strength will become a focus and therefore measures such as peak force or relative peak force (peak force/body weight) become relevant. Finally, as the rehabilitation journey nears return to training and sport, explosive strength should then become a priority and can be monitored using measures such as RFD and/or the index of explosive strength (IES = peak force/time to peak force).
Note that all these assessments need to be performed on the unaffected limb as close to the injury or diagnosis date as possible, for various reasons. First, testing the unaffected leg in proximity to the injury diagnosis will provide baseline measures for the affected limb to return to at the various stages of rehabilitation, and provide more accurate limb symmetry indexes. Second, during the rehabilitation process the unaffected side is often neglected, since the main focus of the patient and physical therapist is achieving a milestone with the affected limb; therefore, in some cases these values actually provide baseline measures for the non-injured limb as well. Last, these unaffected baseline measures may provide the tester with parameters for unaffected loading, e.g., a load during the max strength phase of training, asking a patient if they can produce 70% of peak force for10 repetitions.
Finally, the triceps surae has a different muscle fiber composition and biomechanically advantaged positions, meaning that the muscles are activated differently depending on the movement. The soleus and medial and lateral gastrocnemius muscles need to be assessed and trained in particular joint positions to target those specific muscles and maximize the clinical outcome of the patient. Diagrammatic representations of those positions can be observed in Figure 3: the standing position, focused gastrocnemius, and the focused seated position soleus. The reliability of these plantar flexor assessments have been reported previously; however, their utility in clinical practice has yet to be established to the knowledge of the authors [].

Figure 3.
Standing and seated plantarflexion testing.
9. Conclusions
Most ATR programs lack a standardized quantitative milestone approach, which is likely hindering the athlete’s successful and expedient release from rehabilitation and RTP. It is the author’s view that there is a need to implement a different assessment and periodization approach to improve efficiency of the rehabilitation process. The gold standard measuring device in AT rupture rehabilitation testing is the isokinetic dynamometers [,]. Because of the price and space considerations, a limited number of clinicians have access to such technology, and hence there is a need for alternative solutions to enhance the diagnostic process. With the democratization of force plates and a growing interest in portable fixed dynamometry [], clinicians have portable and affordable solutions to instrument and quantify the heel-raise test. Ref. [] is one such example of using a more mechanotransductive approach to quantifying heel-raise assessment. In the previous section we highlighted technology options that could be used, the reliability of which have been published. These advancements in technology enable the clinician to gather reliable and valid data; help deliver detailed training regimens specific to the strength quality of interest; implement targeted rehabilitation interventions; and provide instantaneous feedback. The availability of such information also enables a mechanotransductive–mechanotherapeutic approach to practice, which should advance the profession. However, the use of such technology will require those associated with ATR to understand the value of such a proposition, and develop new milestones and different exercise prescription frameworks, to truly advance patient and clinical outcomes. It needs to be noted that a great deal of research is needed to determine the reliability and validity, as well as the feasibility, of such an approach in a clinical setting.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ballal, M.S.; Walker, C.R.; Molloy, A.P. The anatomical footprint of the Achilles tendon: A cadaveric study. Bone Jt. J. 2014, 96-B, 1344–1348. [Google Scholar] [CrossRef]
- Ekiert, M.; Tomaszewski, K.A.; Mlyniec, A. The differences in viscoelastic properties of subtendons result from the anatomical tripartite structure of human Achilles tendon—Ex vivo experimental study and modeling. Acta Biomater. 2021, 125, 138–153. [Google Scholar] [CrossRef]
- Winnicki, K.; Ochała-Kłos, A.; Rutowicz, B.; Pękala, P.A.; Tomaszewski, K.A. Functional anatomy, histology and biomechanics of the human Achilles tendon—A comprehensive review. Ann. Anat.-Anat. Anz. 2020, 229, 151461. [Google Scholar] [CrossRef] [PubMed]
- Demangeot, Y.; Whiteley, R.; Gremeaux, V.; Degache, F. The load borne by the Achilles tendon during exercise: A systematic review of normative values. Scand. J. Med. Sci. Sports 2023, 33, 110–126. [Google Scholar] [CrossRef]
- Komi, P.V.; Fukashiro, S.; Järvinen, M. Biomechanical Loading of Achilles Tendon During Normal Locomotion. Clin. Sports Med. 1992, 11, 521–531. [Google Scholar] [CrossRef]
- Bonanno, J.; Cheng, J.; Tilley, D.; Abutalib, Z.; Casey, E. Factors Associated With Achilles Tendon Rupture in Women’s Collegiate Gymnastics. Sports Health Multidiscip. Approach 2022, 14, 358–368. [Google Scholar] [CrossRef]
- Hoeffner, R.; Svensson, R.B.; Bjerregaard, N.; Kjær, M.; Magnusson, S.P. Persistent Deficits after an Achilles Tendon Rupture: A Narrative Review. Transl. Sports Med. 2022, 2022, 7445398. [Google Scholar] [CrossRef] [PubMed]
- Eliasson, P.; Agergaard, A.-S.; Couppé, C.; Svensson, R.; Hoeffner, R.; Warming, S.; Warming, N.; Holm, C.; Jensen, M.H.; Krogsgaard, M.; et al. The Ruptured Achilles Tendon Elongates for 6 Months After Surgical Repair Regardless of Early or Late Weightbearing in Combination With Ankle Mobilization: A Randomized Clinical Trial. Am. J. Sports Med. 2018, 46, 2492–2502. [Google Scholar] [CrossRef]
- Rosso, C.; Vavken, P.; Polzer, C.; Buckland, D.M.; Studler, U.; Weisskopf, L.; Lottenbach, M.; Müller, A.M.; Valderrabano, V. Long-term outcomes of muscle volume and Achilles tendon length after Achilles tendon ruptures. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1369–1377. [Google Scholar] [CrossRef] [PubMed]
- Amin, N.H.; Old, A.B.; Tabb, L.P.; Garg, R.; Toossi, N.; Cerynik, D.L. Performance Outcomes After Repair of Complete Achilles Tendon Ruptures in National Basketball Association Players. Am. J. Sports Med. 2013, 41, 1864–1868. [Google Scholar] [CrossRef]
- Barfod, K.W.; Sveen, T.M.; Ganestam, A.; Ebskov, L.B.; Troelsen, A. Severe Functional Debilitations After Complications Associated With Acute Achilles Tendon Rupture With 9 Years of Follow-Up. J. Foot Ankle Surg. 2017, 56, 440–444. [Google Scholar] [CrossRef]
- Suchak, A.A.; Spooner, C.; Reid, D.C.; Jomha, N.M. Postoperative Rehabilitation Protocols for Achilles Tendon Ruptures: A Meta-analysis. Clin. Orthop. 2006, 445, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Petway, A.J.; Jordan, M.J.; Epsley, S.; Anloague, P. Mechanisms of Achilles Tendon Rupture in National Basketball Association Players. J. Appl. Biomech. 2022, 38, 398–403. [Google Scholar] [CrossRef]
- Lantto, I. Acute Achilles Tendon Rupture: Epidemiology and Treatment. 2016. Available online: https://oulurepo.oulu.fi/handle/10024/34866 (accessed on 24 April 2025).
- Egger, A.C.; Berkowitz, M.J. Achilles tendon injuries. Curr. Rev. Musculoskelet. Med. 2017, 10, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Hunt, K.J. Open Reconstructive Strategies for Chronic Achilles Tendon Ruptures. Foot Ankle Clin. 2019, 24, 425–437. [Google Scholar] [CrossRef]
- Cook, J.L.; Khan, K.M.; Purdam, C. Achilles tendinopathy. Man. Ther. 2002, 7, 121–130. [Google Scholar] [CrossRef]
- Hess, G.W. Achilles Tendon Rupture: A Review of Etiology, Population, Anatomy, Risk Factors, and Injury Prevention. Foot Ankle Spec. 2010, 3, 29–32. [Google Scholar] [CrossRef]
- Ganestam, A.; Kallemose, T.; Troelsen, A.; Barfod, K.W. Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3730–3737. [Google Scholar] [CrossRef]
- Lemme, N.J.; Li, N.Y.; DeFroda, S.F.; Kleiner, J.; Owens, B.D. Epidemiology of Achilles Tendon Ruptures in the United States: Athletic and Nonathletic Injuries from 2012 to 2016. Orthop. J. Sports Med. 2018, 6, 2325967118808238. [Google Scholar] [CrossRef]
- Benzie, M. Achilles ruptures and return to sport in gymnastics: An overview. Sci. Gymnast. J. 2024, 16, 29–41. [Google Scholar] [CrossRef]
- Fenech, M.; Ajjikuttira, A.; Edwards, H. Ultrasound assessment of acute Achilles tendon rupture and measurement of the tendon gap. Australas. J. Ultrasound Med. 2024, 27, 106–119. [Google Scholar] [CrossRef]
- Nilsson-Helander, K.; Silbernagel, G.K.; Thomee, R.; Faxen, E.; Olsson, N.; Eriksson, B.I.; Karlsson, J. Acute Achilles tendon rupture: A randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am. J. Sports Med. 2010, 38, 2186–2193. [Google Scholar] [CrossRef]
- Saleh, M.; Marshall, P.D.; Senior, R.; MacFarlane, A. The Sheffield splint for controlled early mobilisation after rupture of the calcaneal tendon. A prospective, randomised comparison with plaster treatment. J. Bone Joint Surg. Br. 1992, 74, 206–209. [Google Scholar] [CrossRef]
- Valkering, K.P.; Aufwerber, S.; Ranuccio, F.; Lunini, E.; Edman, G.; Ackermann, P.W. Functional weight-bearing mobilization after Achilles tendon rupture enhances early healing response: A single-blinded randomized controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1795. [Google Scholar] [CrossRef]
- Galloway, M.T.; Lalley, A.L.; Shearn, J.T. The Role of Mechanical Loading in Tendon Development, Maintenance, Injury, and Repair. J. Bone Joint Surg. Am. 2013, 95, 1620–1628. [Google Scholar] [CrossRef]
- Sakai, T.; Kumagai, K. Molecular dissection of tendon development and healing: Insights into tenogenic phenotypes and functions. J. Biol. Chem. 2025, 301, 108353. [Google Scholar] [CrossRef] [PubMed]
- Maquirriain, J. Achilles Tendon Rupture: Avoiding Tendon Lengthening during Surgical Repair and Rehabilitation. Yale J. Biol. Med. 2011, 84, 289–300. [Google Scholar] [PubMed]
- Zellers, J.A.; Marmon, A.R.; Ebrahimi, A.; Grävare Silbernagel, K. Lower extremity work along with triceps surae structure and activation is altered with jumping after Achilles tendon repair. J. Orthop. Res. 2019, 37, 933–941. [Google Scholar] [CrossRef]
- Brorsson, A.; Willy, R.W.; Tranberg, R.; Grävare Silbernagel, K. Heel-Rise Height Deficit 1 Year After Achilles Tendon Rupture Relates to Changes in Ankle Biomechanics 6 Years After Injury. Am. J. Sports Med. 2017, 45, 3060–3068. [Google Scholar] [CrossRef]
- Pečjak, R.; Kozinc, Ž. Long-Term Deficits in Muscle Composition, Performance and Quality of Movement after Achilles Tendon Rupture: A Review. BioMed 2023, 3, 135–151. [Google Scholar] [CrossRef]
- Chartier, C.; ElHawary, H.; Baradaran, A.; Vorstenbosch, J.; Xu, L.; Efanov, J.I. Tendon: Principles of Healing and Repair. Semin. Plast. Surg. 2021, 35, 211–215. [Google Scholar] [CrossRef] [PubMed]
- DiIorio, S.E.; Young, B.; Parker, J.B.; Griffin, M.F.; Longaker, M.T. Understanding Tendon Fibroblast Biology and Heterogeneity. Biomedicines 2024, 12, 859. [Google Scholar] [CrossRef]
- Stańczak, M.; Kacprzak, B.; Gawda, P. Tendon Cell Biology: Effect of Mechanical Loading. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2024, 58, 677–701. [Google Scholar] [CrossRef]
- Heikkinen, J.; Lantto, I.; Piilonen, J.; Flinkkilä, T.; Ohtonen, P.; Siira, P.; Laine, V.; Niinimäki, J.; Pajala, A.; Leppilahti, J. Tendon Length, Calf Muscle Atrophy, and Strength Deficit After Acute Achilles Tendon Rupture: Long-Term Follow-up of Patients in a Previous Study. J. Bone Jt. Surg. 2017, 99, 1509–1515. [Google Scholar] [CrossRef]
- Mullaney, M.; McHugh, M.; Tyler, T.; Nicholas, S.; Lee, S. Weakness in End-Range Plantar Flexion After Achilles Tendon Repair. Am. J. Sports Med. 2006, 34, 1120–1125. [Google Scholar] [CrossRef]
- Tipton, K.D. Nutritional Support for Exercise-Induced Injuries. Sports Med. Auckl. Nz 2015, 45, 93. [Google Scholar] [CrossRef] [PubMed]
- Zellers, J.; Pohlig, R.; Cortes, D.; Grävare, S.K. Achilles Tendon Cross-sectional Area at 12 Weeks Post-rupture Relates to One-year Heel-rise Height. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2020, 28, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Marrone, W.; Andrews, R.; Reynolds, A.; Vignona, P.; Patel, S.; O’Malley, M. Rehabilitation and Return to Sports after Achilles Tendon Repair. Int. J. Sports Phys. Ther. 2024, 19, 1152–1165. [Google Scholar] [CrossRef]
- Hutchison, A.-M.; Topliss, C.; Beard, D.; Evans, R.; Williams, P. The treatment of a rupture of the Achilles tendon using a dedicated management programme. Bone Jt. J. 2015, 97-B, 510–515. [Google Scholar] [CrossRef]
- Wang, K.C.; Cotter, E.J.; Cole, B.J.; Lin, J.L. Rehabilitation and Return to Play Following Achilles Tendon Repair. Oper. Tech. Sports Med. 2017, 25, 214–219. [Google Scholar] [CrossRef]
- Glazebrook, M.; Rubinger, D. Functional Rehabilitation for Nonsurgical Treatment of Acute Achilles Tendon Rupture. Foot Ankle Clin. 2019, 24, 387–398. [Google Scholar] [CrossRef]
- Saxena, A.; Ewen, B.; Maffulli, N. Rehabilitation of the operated achilles tendon: Parameters for predicting return to activity. J. Foot Ankle Surg. Off. Publ. Am. Coll. Foot Ankle Surg. 2011, 50, 37–40. [Google Scholar] [CrossRef]
- Silbernagel, K.G.; Nilsson-Helander, K.; Thomeé, R.; Eriksson, B.I.; Karlsson, J. A new measurement of heel-rise endurance with the ability to detect functional deficits in patients with Achilles tendon rupture. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 258–264. [Google Scholar] [CrossRef]
- Silbernagel, K.G.; Crossley, K.M. A proposed return-to-sport program for patients with midportion Achilles tendinopathy: Rationale and implementation. J. Orthop. Sports Phys. Ther. 2015, 45, 876–886. [Google Scholar] [CrossRef]
- Binkley, H.M.; Douglass, D.; Phillips, K.; Wise, S.L. Rehabilitation and Return to Sport After Nonsurgical Treatment of Achilles Tendon Rupture. Strength Cond. J. 2020, 42, 90. [Google Scholar] [CrossRef]
- Kasmar, T.; Groth, A.; Miller, T.; Martin, K.; Marulli, T.; VanEtten, L.; Otto, V. Achilles Tendon Repair Clinical Practice Guideline. The Ohio State University Sports Medicine. Available online: https://medicine.osu.edu/-/media/files/medicine/departments/sports-medicine/medical-professionals/knee-ankle-and-foot/achilles-repair-protocol-2020final-002.pdf (accessed on 24 April 2025).
- William Beaumont Army Medical Center Physical Therapy Section. Achilles Tendon Repair: Rehabilitation Protocol. William Beaumont Army Medical Center. Available online: https://william-beaumont.tricare.mil/Portals/149/Achilles%20Repair%20WB08.pdf (accessed on 24 April 2025).
- Sanford Health Physical Therapy Department. Non-Operative Achilles Rupture Rehabilitation Guide-Line. Sanford Health. Available online: https://www.sanfordhealth.org/-/media/org/files/medical-professionals/resources-and-education/non-operative-achilles-rupture-guidelines.pdf (accessed on 24 April 2025).
- Massachusetts General Hospital Sports Medicine Physical Therapy. Rehabilitation Protocol for Achilles Ten-Don Repair. Norwood, MA: Massachusetts General Hospital. Available online: https://www.massgeneral.org/assets/mgh/pdf/orthopaedics/sports-medicine/physical-therapy/rehabilitation-protocol-for-achilles-tendon-repair.pdf (accessed on 24 April 2025).
- University of Delaware Physical Therapy Clinic. Rehab Practice Guidelines for: Achilles Tendon Repair. University of Delaware. Available online: https://bpb-us-w2.wpmucdn.com/sites.udel.edu/dist/c/3448/files/2017/07/Achilles-Jul-28-2017-284wd86.pdf (accessed on 24 April 2025).
- Zellers, J.A.; Cortes, D.H.; Silbernagel, K.G. From acute Achilles tendon rupture to return to play—A case report evaluating recovery of tendon structure, mechanical properties, clinical and functional outcomes. Int. J. Sports Phys. Ther. 2016, 11, 1150–1159. [Google Scholar]
- Groetelaers, R.; Janssen, L.; Velden, J.; Wieland, A.; Amendt, A.; Geelen, P.; Janzing, H. Functional treatment or cast immobilization after minimally invasive repair of an acute Achilles tendon rupture. Foot Ankle Int. 2014, 35, 771–77835. [Google Scholar] [CrossRef]
- Inglis, A.E.; Sculco, T.P. Surgical repair of ruptures of the tendo Achillis. Clin. Orthop. Relat. Res. (1976–2007) 1981, 156, 160. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G.; Maffulli, G.D.; Khanna, A.; Denaro, V. Achilles Tendon Ruptures in Elite Athletes. Foot Ankle Int. 2011, 32, 9–15. [Google Scholar] [CrossRef]
- Leppilahti, J.; Lähde, S.; Forsman, K.; Kangas, J.; Kauranen, K.; Orava, S. Relationship between calf muscle size and strength after achilles rupture repair. Foot Ankle Int. 2000, 21, 330–335. [Google Scholar] [CrossRef]
- Don, R.; Ranavolo, A.; Cacchio, A.; Serrao, M.; Costabile, F.; Iachelli, M.; Camerota, F.; Frascarelli, M.; Santilli, V. Relationship between recovery of calf-muscle biomechanical properties and gait pattern following surgery for achilles tendon rupture. Clin. Biomech. 2007, 22, 211–220. [Google Scholar] [CrossRef]
- Bressel, E.; Larsen, B.T.; McNair, P.J.; Cronin, J. Ankle joint proprioception and passive mechanical properties of the calf muscles after an Achilles tendon rupture: A comparison with matched controls. Clin. Biomech. 2004, 19, 284–291. [Google Scholar] [CrossRef]
- Kaniki, N.; Willits, K.; Mohtadi, N.G.H.; Fung, V.; Bryant, D. A Retrospective Comparative Study With Historical Control to Determine the Effectiveness of Platelet-Rich Plasma as Part of Nonoperative Treatment of Acute Achilles Tendon Rupture. Arthrosc. J. Arthrosc. Relat. Surg. 2014, 30, 1139–1145. [Google Scholar] [CrossRef]
- Jallageas, R.; Bordes, J.; Daviet, J.-C.; Mabit, C.; Coste, C. Evaluation of surgical treatment for ruptured Achilles tendon in 31 athletes. Orthop. Traumatol. Surg. Res. 2013, 99, 577–584. [Google Scholar] [CrossRef]
- Willits, K.; Amendola, A.; Bryant, D.; Mohtadi, N.G.; Giffin, J.R.; Fowler, P.; Kean, C.O.; Kirkley, A. Operative versus Nonoperative Treatment of Acute Achilles Tendon Ruptures: A Multicenter Randomized Trial Using Accelerated Functional Rehabilitation. J. Bone Jt. Surg. 2010, 92, 2767–2775. [Google Scholar] [CrossRef]
- Arslan, A.; Cepni, S.K.; Sahinkaya, T.; May, C.; Mutlu, H.; Parmaksızoğlu, A.S. Functional outcomes of repair of Achilles tendon using a biological open surgical method. ACTA Orthop. Traumatol. Turc. 2014, 48, 563–569. [Google Scholar] [CrossRef]
- Möller, M.; Lind, K.; Movin, T.; Karlsson, J. Calf muscle function after Achilles tendon rupture. A prospective, randomised study comparing surgical and non-surgical treatment. Scand. J. Med. Sci. Sports 2002, 12, 9–16. [Google Scholar] [CrossRef]
- Porter, D.A.; Barnes, A.F.; Rund, A.M.; Kaz, A.J.; Tyndall, J.A.; Millis, A.A. Acute achilles tendon repair: Strength outcomes after an acute bout of exercise in recreational athletes. Foot Ankle Int. 2014, 35, 123–130. [Google Scholar] [CrossRef]
- Öhberg, L.; Lorentzon, R.; Alfredson, H. Good clinical results but persisting side-to-side differences in calf muscle strength after surgical treatment of chronic Achilles tendinosis: A 5-year follow-up. Scand. J. Med. Sci. Sports 2001, 11, 207–212. [Google Scholar] [CrossRef]
- Silbernagel, K.G.; Gustavsson, A.; Thomeé, R.; Karlsson, J. Evaluation of lower leg function in patients with Achilles tendinopathy. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 1207–1217. [Google Scholar] [CrossRef]
- Fernandez, M.R.; Hébert-Losier, K. Devices to measure calf raise test outcomes: A narrative review. Physiother. Res. Int. 2023, 28, e2039. [Google Scholar] [CrossRef]
- Fernandez, M.R.; Athens, J.; Balsalobre-Fernandez, C.; Kubo, M.; Hébert-Losier, K. Concurrent validity and reliability of a mobile iOS application used to assess calf raise test kinematics. Musculoskelet. Sci. Pract. 2023, 63, 102711. [Google Scholar] [CrossRef]
- Schrefl, A.; Kolokythas, N.; Stamm, M.; Erlacher, D.; Schärli, A. Reliability of a standardized protocol of the Single Leg Heel Rise Test. Curr. Issues Sport Sci. CISS 2024, 9, 009. [Google Scholar] [CrossRef]
- Sman, A.D.; Hiller, C.E.; Imer, A.; Ocsing, A.; Burns, J.; Refshauge, K.M. Design and Reliability of a Novel Heel Rise Test Measuring Device for Plantarflexion Endurance. BioMed Res. Int. 2014, 2014, 391646. [Google Scholar] [CrossRef]
- Hébert-Losier, K.; Wessman, C.; Alricsson, M.; Svantesson, U. Updated reliability and normative values for the standing heel-rise test in healthy adults. Physiotherapy 2017, 103, 446–452. [Google Scholar] [CrossRef]
- UW Health Sports Rehabilitation. Achilles Tendon Rehabilitation Guidelines. Available online: https://www.tigerortho.com/pdfs/uw-health/achilles-tendon-rehab-final.pdf (accessed on 24 April 2025).
- Orthopedic Associates of Hartford. Achilles Tendon Rupture Repair Return-to-Sport Protocol. Available online: https://oahct.com/wp-content/uploads/2020/08/OAH-RTS-Achilles-Tendon-Rupture2-0820.pdf (accessed on 24 April 2025).
- Avers, D.; Lott, D.J.; Brown, M.B. Daniels and Worthingham’s Muscle Testing: Techniques of Manual Examination and Performance Testing, 11th ed.; Saunders: Rhodes, NSW, Australia, 2024. [Google Scholar]
- Feiring, D.C.; Ellenbecker, T.S. Single versus multiple joint isokinetic testing with ACL reconstructed patients. Isokinet. Exerc. Sci. 1996, 6, 109–115. [Google Scholar] [CrossRef]
- Draovitch, P.; Patel, S.; Marrone, W.; Grundstein, M.J.; Grant, R.; Virgile, A.; Myslinski, T.; Bedi, A.; Bradley, J.P.; Williams, R.J.; et al. The Return-to-Sport Clearance Continuum Is a Novel Approach Toward Return to Sport and Performance for the Professional Athlete. Arthrosc. Sports Med. Rehabil. 2022, 4, e93–e101. [Google Scholar] [CrossRef]
- Hébert-Losier, K.; Newsham-West, R.J.; Schneiders, A.G.; Sullivan, S.J. Raising the standards of the calf-raise test: A systematic review. J. Sci. Med. Sport 2009, 12, 594–602. [Google Scholar] [CrossRef]
- Sullivan, K.J.; Wallace, J.G., Jr.; O’Neil, M.E.; Musolino, G.M.; Mandich, M.; Studer, M.T.; Bottomley, J.M.; Cormack, J.C.; Nicholson, S.K.; Jensen, G.M.A. Vision for Society: Physical Therapy as Partners in the National Health Agenda. Phys. Ther. 2011, 91, 1664–1672. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.M.; Scott, A. Mechanotherapy: How physical therapists’ prescription of exercise promotes tissue repair. Br. J. Sports Med. 2009, 43, 247–252. [Google Scholar] [CrossRef]
- Baxter, J.R.; Corrigan, P.; Hullfish, T.J.; O’Rourke, P.; Silbernagel, K.G. Exercise Progression to Incrementally Load the Achilles Tendon. Med. Sci. Sports Exerc. 2021, 53, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Hagley, P.; Ryan, C.; Ye-Lee, D.; Cronin, J. Reliability and Asymmetry Associated with Different Plantar Flexion Assessments Using a Portable Fixed Dynamometer. Personal Communication. 2024. Available online: https://www.researchsquare.com/article/rs-4676750/v1 (accessed on 24 April 2025).
- Chester, R.; Costa, M.L.; Shepstone, L.; Donell, S.T. Reliability of isokinetic dynamometry in assessing plantarflexion torque following Achilles tendon rupture. Foot Ankle Int. 2003, 24, 909–915. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).