Abstract
Introduction: Infantile Refsum disease (IRD) is considered one of the milder phenotypes within the Zellweger Spectrum Disorders (ZSDs), a group of peroxisomal biogenesis disorders characterized by a generalized impairment of peroxisomal function. Pathognomonic features of IRD are growth retardation, hearing and cognitive impairment, neuromuscular problems, and craniofacial anomalies. Due to the relatively short lifespan, severe dental anomalies have not been previously reported in association with this disorder. This case report describes a rare manifestation of multiple impacted teeth and near complete edentulism in an adult patient diagnosed with Infantile Refsum disease (IRD). Material and Methods: The patient, a 24-year-old female, presented with a skeletal Class III malocclusion, severe maxillary hypoplasia, and complete impaction of the permanent dentition. The diagnosis of Infantile Refsum disease (IRD) was genetically confirmed and was associated with both neurological and dermatological manifestations. Conclusions: This case underscores that severe disturbances in tooth eruption and impaction may represent underrecognized manifestations of metabolic and genetic disorders such as Infantile Refsum disease (IRD). Dental professionals should remain vigilant to the potential association between systemic conditions and delayed or failed tooth eruption, emphasizing the need for interdisciplinary management and further investigation.
1. Introduction
Infantile Refsum Disease (IRD) is a rare autosomal recessive disorder characterized by defective peroxisomal function. It belongs to the broader group of peroxisome biogenesis disorders (PBDs), collectively known as the Zellweger Spectrum Disorders (ZSDs) [1,2]. To contextualize the rarity of this condition, the combined birth prevalence for the entire PBD-ZSD spectrum is estimated to be approximately 1 in 50,000 live births [3,4].
IRD is part of the Zellweger spectrum disorders (ZSDs), which also include Zellweger syndrome (ZS), neonatal adrenoleukodystrophy (NALD), and rhizomelic chondrodysplasia punctata (https://www.researchgate.net/publication/258994701_Infantile_Refsum_Disease_and_its_Association_with_PEX1-_A_Review (accessed on 7 December 2025)) [5]. While sharing clinical features with other PBDs, IRD is generally considered the mildest phenotype within this spectrum [6].
The clinical presentation of IRD is highly variable. Common features include developmental delay, hepatic dysfunction, sensorineural hearing loss, visual impairment, hemorrhagic episodes, and intracranial bleeding [7,8]. Additional manifestations may include nystagmus, hypotonia, ataxia (including tremors or seizures), growth retardation and intellectual disability, failure to thrive, minor facial dysmorphisms, hepatomegaly, hypocholesterolemia, and mild craniofacial abnormalities.
In a cohort study, involving 31 patients diagnosed with IRD, approximately 33% presented with delayed tooth eruption, dental malposition, and enamel hypoplasia. Despite its classification as a progressive and often life-limiting disorder, advancements in supportive care have allowed some individuals with IRD to survive into adolescence or early adulthood [9]. In recent years, a limited number of reports have described oral manifestations in patients with peroxisomal biogenesis disorders, suggesting that dental anomalies may represent an underrecognized component of their phenotypic spectrum [10]. In particular, enamel hypoplasia, delayed eruption of both primary and permanent dentitions, and mild morphological defects of developing teeth have been documented in pediatric patients affected by disorders within the Zellweger spectrum [11,12]. These alterations are thought to arise from impaired peroxisomal metabolism and consequent disturbances in ameloblast and odontoblast differentiation, as demonstrated in experimental peroxisome-deficient models such as Pex11b-deficient mice [13]. More broadly, clinical overviews of Zellweger spectrum disorders also highlight developmental disturbances that may extend to the craniofacial and dental domains [4,5]. However, the available evidence is sparse and largely confined to early childhood, with no cases reporting severe eruption failure or near-complete edentulism in adulthood [14]. By situating the present case within this limited and predominantly pediatric literature, the novelty of an adult IRD patient exhibiting multiple impacted teeth and profound eruption disturbances becomes more apparent, underscoring the need for greater attention to oral findings in the clinical follow-up of individuals with peroxisomal disorders.
In this case report, we describe a female patient diagnosed with IRD who presented with multiple impacted permanent teeth, a rare and potentially underrecognized manifestation of this systemic disorder. We detail the diagnostic findings and explore the potential relationship between rare metabolic or genetic conditions and disturbances in tooth eruption.
In addition to the rarity of the dental manifestations observed, the case patient is notable for her adult age, which markedly exceeds the average life expectancy typically reported in individuals with IRD.
This unique clinical scenario significantly influenced the therapeutic strategy. Treatment decisions required careful consideration of the balance between optimizing functional and aesthetic outcomes and addressing the ethical implications of pursuing complex, costly, or invasive procedures in a patient with a progressive, multisystem disorder. The paucity of data regarding the long-term prognosis of IRD further highlights the importance of individualized, patient-centered treatment planning, particularly in the context of dental rehabilitation in patients with systemic disease [12].
This case report was prepared in accordance with the CARE (CAse REport) guidelines (Supplementary Material S1) [13].
2. Materials and Methods
2.1. Patient Information and History
A 24-year-old female patient, born in Italy, was referred to the Operative and General Dentistry Unit of the Department of Surgical Sciences for Head and Neck Diseases at the “A. Gemelli Hospital, Università Cattolica del Sacro Cuore” (Rome, Italy).
Informed consent for participation was obtained from the subject involved in the study. Ethical approval was obtained from the Ethics Committee of Fondazione Policlinico Universitario A. Gemelli IRCCS (Protocol No. 0014203/23, 8 May 2023), and all procedures were performed in accordance with the Declaration of Helsinki.
2.2. Diagnostic Assessment and Etiology
The patient was diagnosed with neonatal adrenoleukodystrophy, associated with a homozygous c.2528G>A variant in the PEX1 gene. Her clinical history included micronodular chronic liver disease, mild adrenal insufficiency, sensorineural hearing loss (which required the use of hearing aids in both ears), intellectual disability, retinopathy, and mood disorder. At the age of 11, the patient underwent a day surgery procedure for the extraction of tooth 4.1 due to advanced tooth decays. The patient denied any known allergies. At the time of evaluation, the patient was 24 years old, measured 140 cm in height and weighed 60 kg. She appeared oriented and cooperative. The patient followed a strictly controlled diet aimed at reducing phytanic acid levels and her ongoing therapy included hydrocortisone for the management of secondary adrenal insufficiency, a condition commonly associated with peroxisomal disorders such as IRD [14]. Additionally, she was supplemented with calcium carbonate and cholecalciferol to prevent bone complications, including osteopenia and osteoporosis, which may have resulted from chronic corticosteroid therapy and vitamin D deficiency [15]. The patient was also treated with Sursum and a DHA-rich oil supplement, both of which support peroxisomal function and may contribute to neurological and visual stabilization in IRD [16,17]. Fluoxetine was administered to support natural skin tissue regeneration, potentially counteracting dermatological manifestations associated with the disease [18].
2.3. Clinical Findings and Imaging
Extraoral examination revealed facial asymmetry, a dolichofacial growth pattern, and a concave facial profile (Figure 1a,b). As for the patient’s dental situation, intraoral clinical evaluation showed the presence of teeth 3.1, 5.3, and 7.4, along with a root remnant likely corresponding to 2.5 (Figure 2a,b,c,d,e). She showed a skeletal class III relationship due to the absence of erupted teeth. The patient’s mandible appeared prognathic, while the maxilla was severely hypoplastic [19,20]. The orthopantomography (OPG) revealed the presence of multiple impacted teeth, most of which exhibited abnormal morphology and incomplete development (Figure 3) [21]. The OPG was acquired using standard panoramic settings (66–70 kVp, 8–10 mA, exposure time 12–14 s) to obtain a comprehensive overview of dental development, impactions, and bone morphology. CBCT imaging was performed using a small-to-medium field of view (FOV 8 × 8 cm), 90 kVp, 5 mA, and a voxel size of 0.2 mm, allowing detailed assessment of tooth morphology, root development, and three-dimensional spatial relationships essential for treatment planning. Cone-beam computed tomography (CBCT) confirmed the findings and aided in treatment planning (Figure 4) [22]. Clinical photographs and radiographic records were collected, and the patient was enrolled in a multidisciplinary dental and prosthetic rehabilitation program.
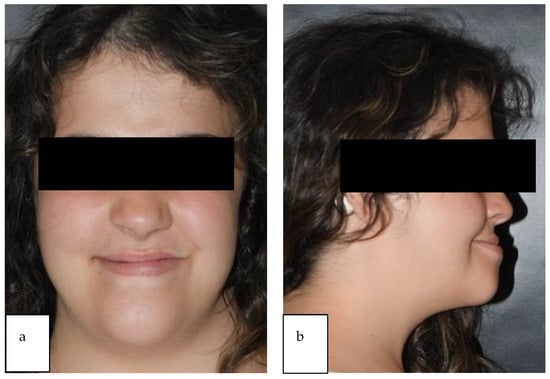
Figure 1.
(a,b): Extraoral pictures. The images display marked facial asymmetry and a dolichofacial growth pattern. The profile view confirms a concave facial profile resulting from severe maxillary retrusion, consistent with the skeletal Class III relationship observed.
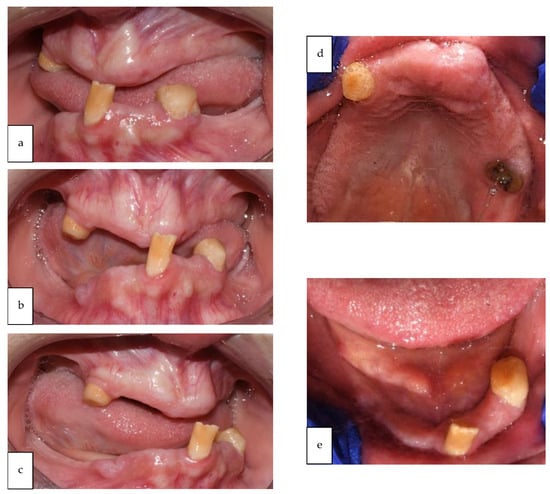
Figure 2.
(a–e): Intraoral pictures. The images illustrate the clinical status of near-complete edentulism.
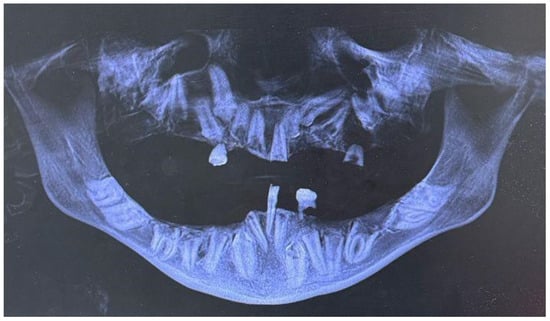
Figure 3.
Orthopantomography (OPG). The OPG image confirms multiple impacted permanent teeth throughout both the upper and lower arches, with abnormal morphology and incomplete root development of the retained elements.
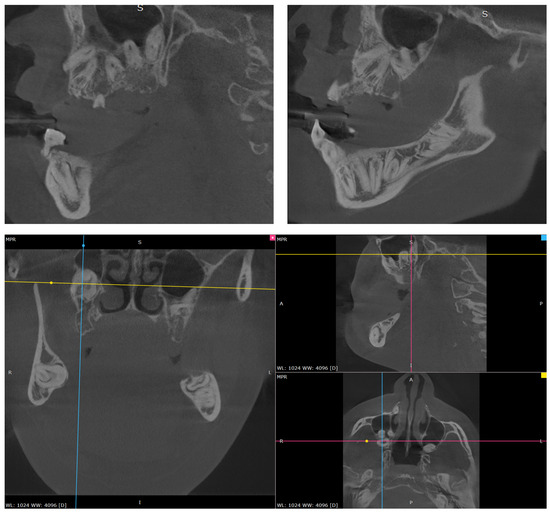
Figure 4.
Multiplanar CBCT reconstructions confirm the three-dimensional precise location and morphological abnormalities of the multiple impacted dental elements.
2.4. Treatment Objectives and Treatment Plan
The primary objectives of treatment were to restore both esthetics and masticatory function. Given the complexity of the patient’s dental situation, a comprehensive treatment plan was proposed, which included the extraction of several impacted teeth and the subsequent placement of a full-arch prosthesis. This approach was considered the most effective solution to achieve optimal functional and esthetic outcomes. The plan also considered the patient’s systemic conditions and overall health status, which were critical factors in determining the feasibility and timing of any invasive intervention.
2.5. Treatment Alternatives
In formulating the treatment plan, both clinical and ethical considerations were carefully assessed. Given the patient’s systemic condition, long-term prognosis, and previously documented intolerance to removable prostheses, the decision-making process involved balancing the invasiveness and cost of full-arch rehabilitation against the feasibility of conservative alternatives. Patient preferences, functional needs, quality-of-life implications, and the potential risks associated with surgical or implant-supported interventions were explicitly considered. A multidisciplinary discussion among prosthodontic, orthodontic, and medical specialists guided the final approach.
As a more conservative alternative, a removable prosthetic solution was discussed. This would have involved fabricating a removable partial denture for the mandibular arch and a complete maxillary denture, to be placed after extraction of the remaining teeth in the upper arch. The advantages and limitations of this approach- including esthetic compromises, potential discomfort, functional limitations, and maintenance requirements- were carefully explained to the patient. Economic considerations were also discussed as part of the decision-making process.
2.6. Treatment Progress
Due to the patient’s systemic conditions and the relatively short life expectancy associated with IRD, the clinicians questioned the indication for a complex and costly intervention, such as full-arch prosthetic rehabilitation. A comprehensive assessment of the liver condition was requested before proceeding with any therapeutic intervention. The patient ultimately declined the conservative removable prosthesis approach, citing personal preferences and economic reasons. In particular, the patient expressed concerns about the discomfort, functional limitations, and maintenance associated with removable dentures, as well as the financial burden. Therefore, no prosthetic treatment was performed. The focus of this case report is on the clinical decision-making process, the evaluation of treatment alternatives, and the rationale behind the management strategy in a patient with complex medical conditions.
3. Results
Despite the patient’s age of 24 years, the observed clinical features were consistent with a diagnosis of Infantile Refsum Disease (IRD). Clinically, the patient presented with a severe state of near-complete edentulism, with only the permanent incisor 3.1 and the retained deciduous teeth 5.3 and 7.4 present in the oral cavity. Skeletally, the patient exhibited a Class III relationship characterized by severe maxillary hypoplasia and mandibular prognathism (Figure 1a,b). The distinguishing aspect of the present case was the patient’s longevity and the unique radiographic finding of multiple impacted permanent teeth (including elements 1.1–1.8, 2.1–2.4, 2.6–2.8, 3.2–3.8, and 4.2–4.8) and near-complete edentulism—a combination not previously reported in association with this disorder (Figure 5). The patient was referred to a multidisciplinary prosthetic rehabilitation program.
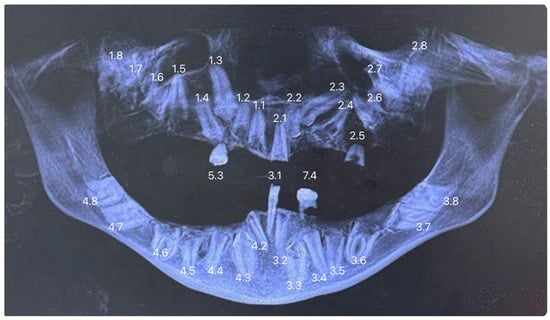
Figure 5.
The Orthopantomography (OPG) image displays the patient’s dentition with numerical labeling of the dental elements, using the standard FDI (Fédération Dentaire Internationale) system.
3.1. Clinical and Skeletal Findings
Extraoral examination revealed facial asymmetry, a dolichofacial growth pattern, and a concave facial profile. The patient presented with a skeletal Class III relationship, which was a consequence of severe maxillary hypoplasia combined with a prognathic appearance of the mandible.
Intraoral clinical evaluation confirmed the state of near-complete edentulism. The only teeth present in the oral cavity were the permanent incisor 3.1, the retained deciduous teeth 5.3 and 7.4, and a root remnant likely corresponding to 2.5. The retention of these deciduous elements in an adult patient indicates a severe failure of the normal permanent tooth eruption sequence.
3.2. Radiographic Findings
Orthopantomography (OPG) and Cone-Beam Computed Tomography (CBCT) confirmed significant dental anomalies. The majority of the permanent dentition was impacted, including all permanent elements from 1.1 to 1.8, 2.1 to 2.4 and 2.8 (maxilla), 3.2 to 3.8, and 4.2 to 4.8 (mandible). Most of these impacted teeth exhibited abnormal morphology and incomplete development. Element 4.1 was absent due to prior extraction for advanced tooth decay at age 11. Such a severe pattern of dental impaction and tooth loss resulted in the observed near-complete edentulism, a finding that severely impaired oral function.
The patient was subsequently enrolled in a multidisciplinary dental and prosthetic rehabilitation program.
4. Discussion
4.1. Interpretation of the Results
Tooth eruption is a complex biological process occurring across a broad chronological range and influenced by multiple factors, including racial, ethnic, sex-related, and individual variability. These parameters are generally taken into account when defining normative eruption standards. The process is regulated by numerous molecular pathways, many of which exhibit overlapping or redundant functions—an intrinsic biological safeguard that ensures eruption can proceed even when a single regulatory molecule is compromised. Among the key mediators involved in tooth eruption are EGF, EGF-R, CSF-1, CSF-1R, IL-1, IL-1R, c-Fos, NF-κB, MCP-1, TGF-β1, PTHrP, Cbfa-1, OPG, and the RANK/RANKL system [23].
In the present case, the patient presented with complete edentulism and multiple impacted permanent teeth, a combination that profoundly affected oral function and likely exerted significant psychosocial consequences. Infantile Refsum disease (IRD) is characterized by defective peroxisomal function, leading to the accumulation of phytanic acid and very-long-chain fatty acids (VLCFAs). This metabolic imbalance results in elevated oxidative stress across several cell types, including those involved in odontogenesis [24]. The dental anomalies observed in our patient—namely, multiple impactions and near-complete edentulism—can be interpreted in light of the essential role of peroxisomes in cell signaling, differentiation, and maintenance of redox homeostasis. Increased oxidative stress has been shown to impair ameloblast and odontoblast function, thereby disrupting enamel formation, dentinogenesis, and the coordinated molecular events required for tooth eruption.
Evidence from peroxisome-deficient animal models, such as Pex11b-deficient mice, demonstrates that impaired peroxisomal activity directly interferes with odontogenesis. These models exhibit reduced expression of amelogenin, a key enamel matrix protein, and vimentin, a structural marker associated with cellular differentiation and intermediate filament integrity. Such alterations lead to enamel hypoplasia, abnormal tooth morphology, and compromised dental follicle integrity—changes that are consistent with the disturbances in eruption observed in IRD patients [25].
Collectively, these molecular and cellular mechanisms offer a coherent explanation for the clinical presentation documented in our patient, characterized by widespread impaction and complete edentulism resulting from disrupted odontogenesis and eruption failure [25].
4.2. Generalization of Results in the Context of the Literature
To date, oral and dental manifestations of Infantile Refsum disease have been rarely documented in the literature. This case report describes a female patient affected by IRD who presented with near-complete edentulism and multiple impacted permanent teeth, a combination of findings not previously reported in association with this condition. This clinical scenario is likely to be rare, in part due to the limited life expectancy typically associated with IRD. In our case, the patient is 24 years old, which is significantly beyond the age typically reported in patients with severe PEX1 mutations, who often do not survive past early childhood. To our knowledge, all previously published reports describing the oral phenotype of Infantile Refsum Disease have involved pediatric patients, generally in early childhood and rarely reaching adolescence. These studies consistently document enamel hypoplasia, delayed dental eruption, and mild morphological anomalies, but only occasionally report impacted teeth and never describe edentulism [24,25]. In contrast, the present case demonstrates a markedly more severe and complex dental presentation, characterized by multiple impacted permanent teeth with incomplete development, profound eruption failure, and near-complete edentulism in a young adult. This striking divergence likely reflects the patient’s unusually prolonged survival, which allowed the full expression of dental abnormalities that may not become clinically evident during childhood. A comparative summary between pediatric cases reported in the literature and the oral findings of the present adult patient is provided in Table 1, underscoring the uniqueness and severity of this case within the existing IRD spectrum.

Table 1.
Oral findings reported in pediatric cases of Infantile Refsum Disease compared with the present adult case.
By documenting this unique combination of dental anomalies in an adult patient, our report provides valuable insights that may help clinicians recognize late-onset or more severe oral manifestations in IRD. Awareness of these possibilities can inform more vigilant dental monitoring and timely, individualized interventions in similar patients.
4.3. Strengths and Limitations
The main limitation of this case report is its single-subject design, which restricts the generalizability of the observations and precludes the development of standardized clinical protocols. Nevertheless, it contributes to the limited body of literature describing dental manifestations in IRD. Prosthetic rehabilitation in this case was particularly challenging, not only due to severe maxillary hypoplasia and the abnormal morphology of the impacted teeth, but also because the patient refused to wear removable prostheses, reporting significant discomfort. This refusal further limited treatment options and highlighted the need for a highly individualized, interdisciplinary approach to care.
4.4. Clinical Implication
From a clinical and ethical standpoint, the treatment of patients with Infantile Refsum disease presents a complex challenge that requires careful, individualized consideration. On one hand, ensuring functional and aesthetic oral outcomes, such as proper occlusion, masticatory efficiency and dental appearance, is essential, as these factors significantly impact the patient’s quality of life. On the other hand, treatment planning must consider both the biological and economic costs, especially in the context of the limited life expectancy often associated with the disease. A multidisciplinary, patient-centered approach is therefore critical to guide therapeutic decisions that are both ethically justified and clinically appropriate [15,17].
This case highlights the clinical relevance of early dental assessment and proactive management in IRD. By documenting severe eruption failure and near-complete edentulism in an adult, it emphasizes the importance of interdisciplinary collaboration and individualized care strategies to optimize functional, aesthetic, and psychosocial outcomes in patients with rare multisystemic disorders.
4.5. Implication for Future Research
Despite its limitations, this case highlights the need for further research into the dental phenotype of IRD and other peroxisomal biogenesis disorders. In rare diseases where robust evidence is lacking, well-documented case reports remain a valuable tool for recognizing clinical patterns, formulating pathophysiological hypotheses, and guiding future research directions.
Larger cohort studies and longitudinal follow-up will be necessary to better understand the prevalence, mechanisms, and management of dental anomalies in IRD, with the goal of developing evidence-based guidelines for clinical practice.
Infantile Refsum disease (IRD) is associated with several distinctive oral manifestations, although these remain poorly characterized in the literature. Enamel hypoplasia is a common finding, characterized by thin or defective enamel layers that increase susceptibility to dental caries and structural fragility [24]. Such enamel defects are thought to result from impaired ameloblast differentiation and mineralization processes [16].
5. Conclusions
This case highlights the importance of including dental assessment in the management of patients with IRD and related peroxisomal disorders. It documents, for the first time, severe eruption failure and near complete edentulism in an adult patient, expanding the recognized oral phenotype of these conditions. These findings underscore the need for early dental involvement and multidisciplinary care.
Further studies in larger cohorts are needed to determine whether eruption disturbances and tooth agenesis represent underrecognized features or potential diagnostic indicators in peroxisomal disorders.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/oral5040103/s1, S1: Care Checklist.
Author Contributions
Conceptualization, P.G.; methodology, E.S.; software, G.G.; validation, F.G.; formal analysis, F.G.; investigation, G.G., F.C.; resources, L.L.; data curation, C.C.N.; writing—original draft preparation, F.C., L.L., C.C.N.; writing—review and editing, E.S., F.G.; supervision, P.G.; visualization, G.G.; project administration, P.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Policlinico Agostino Gemelli—CET Lazio Area 3 (protocol code 5626 and 8 May 2023).
Informed Consent Statement
Informed consent was obtained from the subject involved in the study. Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request. The data are not publicity available due to privacy issues.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Choksi, V.; Hoeffner, E.; Karaarslan, E.; Yalcinkaya, C.; Cakirer, S. Infantile Refsum Disease: Case Report. Am. J. Neuroradiol. 2003, 24, 2082–2084. [Google Scholar]
- Wanders, R.J.; Baes, M.; Ribeiro, D.; Ferdinandusse, S.; Waterham, H.R. The physiological functions of human peroxisomes. Physiol. Rev. 2023, 103, 957–1024. [Google Scholar] [CrossRef]
- Braverman, N.E.; Raymond, G.V.; Rizzo, W.B.; Moser, A.B.; Wilkinson, M.E.; Stone, E.M.; Steinberg, S.J.; Wangler, M.F.; Rush, E.T.; Hacia, J.G.; et al. Peroxisome biogenesis disorders in the Zellweger spectrum: An overview of current diagnosis, clinical manifestations, and treatment guidelines. Mol. Genet. Metab. 2016, 117, 313–321. [Google Scholar] [CrossRef]
- Available online: https://www.researchgate.net/publication/258994701_Infantile_Refsum_Disease_and_its_Association_with_PEX1-_A_Review (accessed on 7 December 2025).
- Kumar, R.; Hodis, B.; De Jesus, O. Refsum Disease; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Gould, S.J.; Valle, D. Peroxisome biogenesis disorders: Genetics and cell biology. Trends Genet. 2000, 16, 340–345. [Google Scholar] [CrossRef]
- Crane, D.I.; Maxwell, M.A.; Paton, B.C. PEX1 mutations in the Zellweger spectrum of the peroxisome biogenesis disorders. Hum Mutat. 2005, 26, 167–175. [Google Scholar] [CrossRef]
- Ramos-Sánchez, R.Y.; López-Fontanet, J.J.; Izquierdo, N. Adult Refsum Disease in Puerto Rico: A Case Report. Cureus 2023, 15, e45426. [Google Scholar] [CrossRef]
- Poll-The, B.T.; Gootjes, J.; Duran, M.; De Klerk, J.B.; Maillette de Buy Wenniger-Prick, L.J.; Admiraal, R.J.; Waterham, H.R.; Wanders, R.J.; Barth, P.G. Peroxisome biogenesis disorders with prolonged survival: Phenotypic expression in a cohort of 31 pa-tients. Am. J. Med. Genet. Part A 2004, 126, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Saccucci, M.; Corridore, D.; Di Carlo, G.; Bonucci, E.; Cicciù, M.; Vozza, I. Assessment of Enamel Color Stability of Resins Infiltration Treatment in Human Teeth: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 11269. [Google Scholar] [CrossRef] [PubMed]
- Azzi, L.; Maurino, V.; Vinci, R.; Croveri, F.; Boggio, A.; Tagliabue, A.; Silvestre-Rangil, J.; Tettamanti, L. ADULT syndrome: Dental features of a very rare condition. Regul. Homeost. Agents 2017, 31 (Suppl. S1), 61–65. [Google Scholar]
- Klouwer, F.C.; Berendse, K.; Ferdinandusse, S.; Wanders, R.J.; Engelen, M.; Poll-The, B.T. Zellweger spectrum disorders: Clinical overview and management approach. Orphanet J. Rare Dis. 2015, 10, 151. [Google Scholar] [CrossRef]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D. The CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development. Glob. Adv. Health Med. 2013, 2, 38–43. [Google Scholar] [CrossRef]
- Gagnon, C.; Hurst, A.C.; Ashraf, A.P. Adrenal Insufficiency in Peroxisomal Disorders: A Single Institution Case Series. Horm. Res. Paediatr. 2023, 96, 439–445. [Google Scholar] [CrossRef]
- Ducki, C.; Wojtkiewicz, M.; Bartoszewicz, M.; Fiedor, P. The Role of Vitamin D in Rare Diseases—A Clinical Review. Biomedicines 2025, 13, 558. [Google Scholar] [CrossRef]
- Moser, A.B.; Jones, D.S.; Raymond, G.V.; Moser, H.W. Plasma and Red Blood Cell Fatty Acids in Peroxisomal Disorders. Neurochem. Res. 1999, 24, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Ciavarella, D.; Lorusso, M.; Fanelli, C.; Ferrara, D.; Esposito, R.; Laurenziello, M.; Esperouz, F.; Lo Russo, L.; Tepedino, M. The Efficacy of the RME II System Compared with a Herbst Appliance in the Treatment of Class II Skeletal Malocclusion in Growing Patients: A Retrospective Study. Dent. J. 2024, 12, 254. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chen, L.; Du, Y.; Huang, D.; Han, H.; Dong, Z. Fluoxetine Ameliorates Atopic Dermatitis-Like Skin Lesions in BALB/c Mice through Reducing Psychological Stress and Inflammatory Response. Front. Pharmacol. 2016, 7, 318. [Google Scholar] [CrossRef]
- Azzi, L.; Croveri, F.; Vinci, R.; Maurino, V.; Boggio, A.; Mantegazza, D.; Farronato, D.; Tagliabue, A.; Silvestre-Rangil, J.; Tettamanti, L. Oral manifestations of selective IgA-deficiency: Review and case-report. J. Biol. Regul. Homeost. Agents 2017, 31 (Suppl. S1), 113–117. [Google Scholar] [PubMed]
- Tepedino, M.; Illuzzi, G.; Laurenziello, M.; Perillo, L.; Taurino, A.M.; Cassano, M.; Guida, L.; Burlon, G.; Ciavarella, D. Craniofacial morphology in patients with obstructive sleep apnea: Cephalometric evaluation. Braz. J. Otorhinolaryngol. 2020, 88, 228–234. [Google Scholar] [CrossRef]
- Di Carlo, G.; Saccucci, M.; Luzzi, V.; Ierardo, G.; Vozza, I.; Sfasciotti, G.; Polimeni, A. Prevalence of maxillary canine impaction in skeletal Class III malocclusions compared to Class I malocclusions. J. Clin. Exp. Dent. 2019, 11, e264–e268. [Google Scholar] [CrossRef]
- Sivolella, S.; Meggiorin, S.; Ferrarese, N.; Lupi, A.; Cavallin, F.; Fiorino, A.; Giraudo, C. CT-based dentulous mandibular alveolar ridge measurements as predictors of crown-to-implant ratio for short and extra short dental implants. Sci. Rep. 2020, 10, 16229. [Google Scholar] [CrossRef]
- Colasante, C.; Jednakowski, J.; Valerius, K.P.; Li, X.; Baumgart-Vogt, E. Peroxisomal dysfunction interferes with odontogenesis and leads to developmentally delayed teeth and defects in distinct dental cells in Pex11b-deficient mice. PLoS ONE 2024, 19, e0313445. [Google Scholar] [CrossRef] [PubMed]
- Tran, D.; Greenhill, W.; Wilson, S. Infantile refsum disease with enamel defects: A case report. Pediatr. Dent. 2011, 33, 266–270. [Google Scholar] [PubMed]
- Acharya, B.S.; Ritwik, P.; Velasquez, G.M.; Fenton, S.J. Medical–dental findings and management of a child with infantile Refsum disease: A case report. Spec. Care Dentistr. 2012, 32, 112–117. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).