Exposure to Endocrine-Disrupting Chemicals and Early Onset of Menarche: A Systematic Review
Abstract
1. Introduction
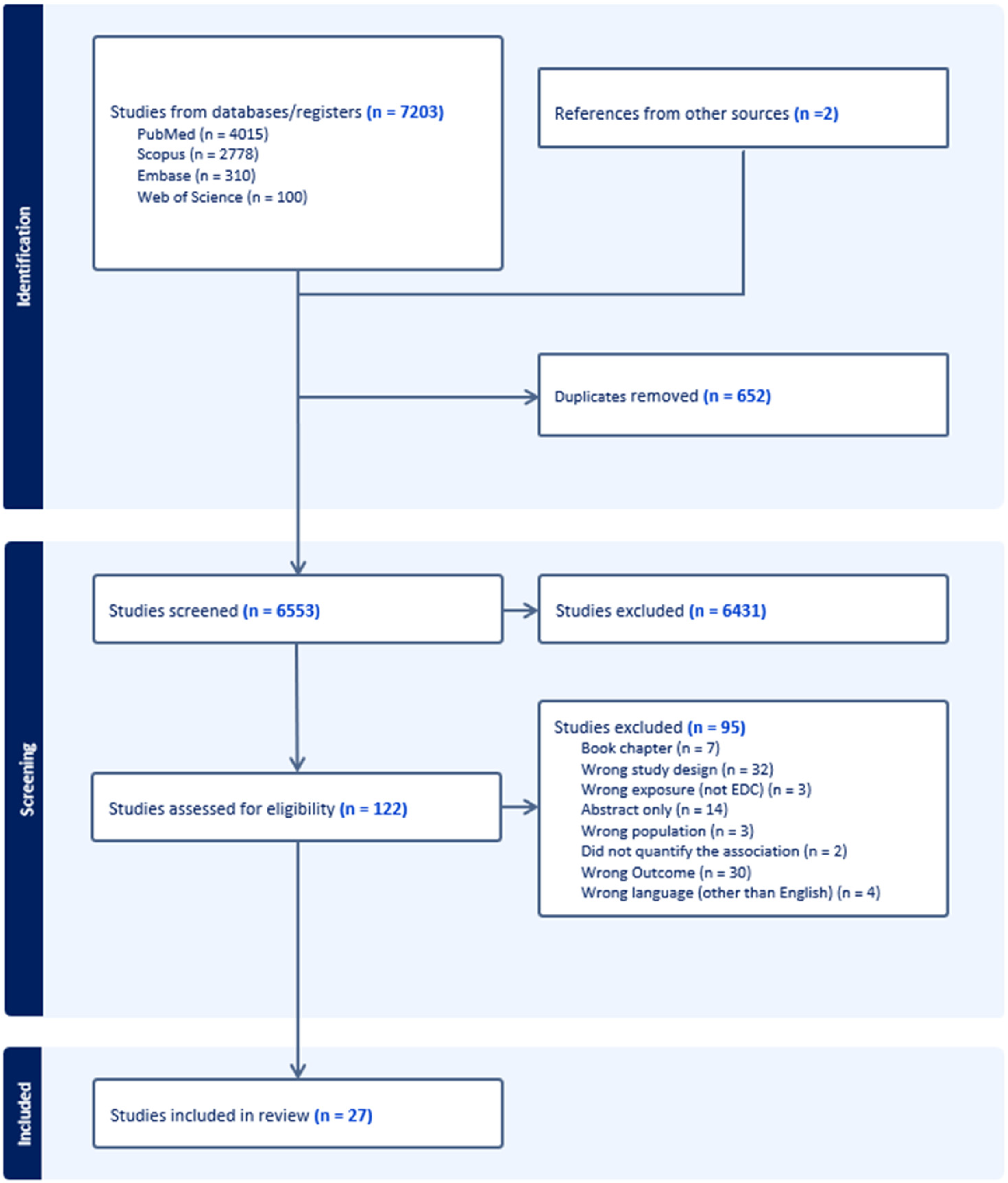
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Strategy
2.3. Inclusion Criteria
2.4. Early Menarche
2.5. Endocrine-Disrupting Chemicals
2.6. Data Extraction and Synthesis
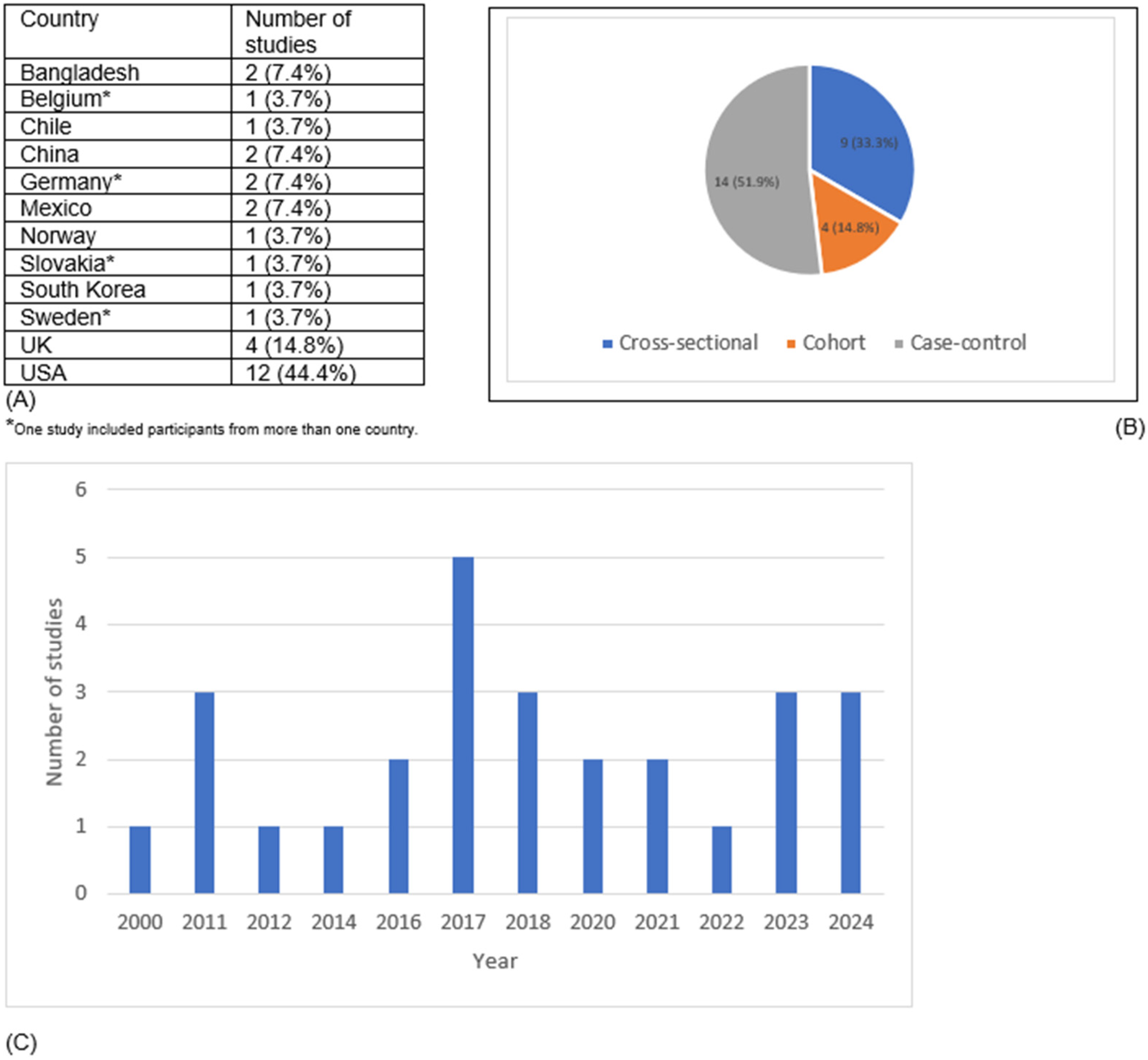
3. Results
3.1. Toxic Metals (Lead, Cadmium, Mercury) and Minerals (Fluoride)
3.2. Personal Care Products and Plasticizing Chemicals (PCPPCs)
3.3. Bisphenol A (BPA)
3.4. Plant-Derived/Organic/Naturally Occurring EDCs (e.g., Phytoestrogen)
3.5. Phenols
3.6. Polybrominated Biphenyls (PBBs), Polychlorinated Biphenyls (PCBs)
3.7. Polybrominated Diphenyl Ether (PBDE)
| References | Year of Publication | Study Design | Country | Study Participants | Sample Size | Exposure | Outcome Definition | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Blanck et al. [43] | 2000 | Retrospective cohort | United States | Female offspring at least 5 years of age as of 1997, born during or after the Michigan PBB incident | n = 327 | Polybrominated diphenyl (PBB) | self-reported age at menarche | Girls who were breastfed and exposed to high levels of PBBs before birth started their periods earlier (around age 11.6) compared to breastfed girls with lower exposure (12.2–12.7 years) and girls who were not breastfed (12.7 years). |
| Marks et al. [44] | 2021 | Case–control | United Kingdom | pregnant women with an expected delivery date between 1 April 1991 and 31 December 1992, from three health districts in the former county of Avon, Great Britain. Mother and daughter | n = 448 | EDCs (poly- and perfluoroalkyl substances (PFAS), polychlorinated biphenyls (PCBs), and organochlorine pesticides (OCPs)) | age at menarche | There is no significant association between prenatal exposure to certain endocrine-disrupting chemicals (PFAS, PCBs, and OCPs) and early menarche (<11.5 years). |
| Harley et al. [45] | 2017 | Cohort | United States | Mothers during pregnancy (n = 263) and their children at age 9 years (n = 522). Mexican-origin families | n = 522, 314 girls | Polybrominated diphenyl ether (PBDE) | timing of menarche by self-report | Childhood PBDE exposure was not associated with any measure of pubertal timing, except for an association of BDE-153 with later menarche. |
| Chen et al. [46] | 2011 | Cross-sectional | United States | NHANES 2003–2004 | n = 271 | blood Polybrominated diphenyl ethers (PBDEs) | age at menarche | Higher serum PBDEs were associated with slightly earlier ages at menarche in multivariable model. Each natural log unit of total BDEs was related to a change of −0.10 (95% CI: −0.33, 0.13) years of age at menarche and a RR of 1.60 (95% CI: 1.12, 2.28) for experiencing menarche before 12 years of age |
| Averina et al. [47] | 2024 | Cross-sectional | Norway | First year high school students aged 12–19 years | n = 1038 | persistent organic pollutants (polyfluroalkyl substances PSA) | self-reported age at menarche | Some PFAS had a positive association to earlier menarche, specifically PFDA and PFUnDA. |
| Christensen et al. [48] | 2011 | Case–control | United Kingdom | female offsprings in the Avon longitudinal study of parents and children (ALSPAC) | n = 448 | polyfluroakyl chemicals (PFCs) during pregnancy | age at menarche | All study participants had nearly ubiquitous exposure to most PFCs examined, but PFC exposure did not appear to be associated with altered age of menarche of their offspring |
| Pinney et al. [49] | 2023 | Cohort | United States | Girls were recruited at 6–8 years of age in 2004–2007 from (a) Mount Sinai School of Medicine, (b) Kaiser Permanente Northern California, and (c) Cincinnati Children’s Hospital/University of Cincinnati | n = 379 | PFAS | thelarche, pubarche, and menarche | PFAS may delay pubertal onset through the intervening effects on BMI and reproductive hormones. The decreases in DHEAS and E1 associated with PFOA represent biological biomarkers of effect consistent with the delay in onset of puberty. |
3.8. Per- and Polyfluoroalkyl Substances (PFAS)
| References | Year of Publication | Study Design | Country | Study Participants | Sample Size | Exposure | Outcome Definition | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Cox et al. [50] | 2023 | Cross-sectional | Sweden, Slovakia, Germany and Belgium | female participants aged 12–18 years in the Human Biomonitoring for Europe initiative(HBM4EU) | n = 514 | Polyfluoakyl (PFA) and phthalates | age at menarche | Urinary DEHP concentrations, particularly 5OH-MEHP is associated with an earlier age of menarche in 12–18-year-old teenage participants. |
| Binder et al. [41] | 2018 | Cohort | Chile | random subset of the longitudinal Growth and Obesity Cohort study | n = 200 | Endocrine-disruptive chemicals (EDCs) phenols and Phthalates | self-reported age at menarche | Higher B1 concentrations of 2,5-dichlorophenol and benzophenone-3 were associated with earlier menarche. Elevated B4 concentrations of monomethyl phthalate were similarly associated with earlier menarche. |
| Cathey et al. [51] | 2020 | Cohort | Mexico | Subset of adolescent children aged 8–14 years from mothers with early life exposure in Mexico to environmental toxicants (ELEMENT) project. | n = 554 | Gestational exposure to Phthalate | tanner staging+ menarche onset | Gestational phthalates exposure is associated with earlier onset and slower progression of sexual maturation outcomes in girls, particularly breast development. |
| Buttke et al. [18] | 2012 | Cross-sectional | United States | NHANES 2003–2008 | n = 1598 | Endocrine-disruptive chemicals (EDCs) phthalates, parabens and phenols | age at menarche | Girls with urinary environmental phenol concentrations above the 75th percentile had significantly lower age of menarche than girls below the 75th percentile. No other significant association was seen between urinary EDC biomarkers and age of menarche. |
| Harley et al. [45] | 2018 | Cohort | United States | Pregnant women recruited in 1999–2000 from community clinics serving California’s Salinas Valley. Eligibility criteria included being at least 18 years of age, <20 weeks gestation, English-or Spanish-speaking, and qualifying for low-income health insurance | n = 338 | Phthalates and parabens found in personal care and consumer products | tanner stage + age at menarche | All biomarkers were detected in more than 90% of samples, except triclosan (73% in prenatal and 69% in peripubertal samples) and butylparaben (detected in less than 40% of samples and therefore excluded from analyses). |
| Watkins et al. [39] | 2017 | Cohort | Mexico | Pregnant women in Mexico City and their children. Our analysis includes women who were recruited from maternity hospitals during their first trimester between 1997 and 2004 and their children | n = 120 | Phthalate and bisphenol A | tanner stage + menarche status | Mean mono-2-ethylhexyl phthalate in the third trimester was associated with higher odds of having a Tanner Stage > 1 for pubic hair development. |
| Wolff et al. [42] | 2016 | Cohort | United States | Black or Hispanic girls mainly from East Harlem in New York City; Cincinnati Children’s Hospital (Cincinnati) that recruited from the greater Cincinnati metropolitan area; and Kaiser Permanente Northern California (California) that recruited members of the KPNC Health Plan in the San Francisco Bay Area. | n = 1051 | Phenols and phthalates | age at menarche | Environmental biomarkers measured ten years before puberty were found to be associated with timing of both breast development and menarche; two others were associated with breast development but not menarche. Six other biomarkers or composite indices were associated with neither. |
| McGuinn et al. [52] | 2014 | Cross-sectional | United States | NHANES 2003–2010 | n = 987 | Urinary bisphenol A (BPA) | age at menarche | No association between BPA and age at menarche in multivariable model including race. |
| Bigambo et al. [35] | 2022 | Cross-sectional | United States | NHANES 2013–2016 females aged 12–19 years | n = 297 | personal care products and plasticizing chemicals (PCPPCs) Phenols, Parabens and phthalates | self-reported age at menarche | The mixture of PCPPCs was significantly associated with reproductive hormones particularly TT and SHBG and early menarche in girls 12–19 years. |
| Kasper-Sonnenberg et al. [38] | 2017 | Cohort | Germany | Eight- to ten-year-old children from the German Duisburg Birth and Bochum Cohort studies | n = 408, girls = 198 | Bisphenol A and phthalates | tanner staging+ menarche onset | Girls started puberty earlier than boys. Breast development and the onset of menstruation were more strongly influenced by metabolite levels than pubic hair growth. BPA showed no consistent association with the individual PFD scales. |
3.9. Phthalates
3.10. Other (e.g., PM2.5 (Particulate Matter), Toxic Metals, Parabens, Pyrethroids, Polycyclic Aromatic Hydrocarbons (PAHs))
| References | Year of Publication | Study Design | Country | Study Participants | Sample Size | Exposure | Outcome Definition | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Malin et al. [33] | 2022 | Cross-sectional | United States | Participants from the National Health and Nutrition Examination Survey (2013–2016) all female | n = 524 | Fluoride | age at menarche | Higher fluoride in drinking water was linked to earlier puberty. Overall, blood fluoride levels were not tied to age of menarche, but among Non-Hispanic Black girls, higher blood fluoride was linked to earlier puberty, about 5 months earlier for every 0.3 µmol/L increase. |
| Li et al. [53] | 2024 | Cohort | China | Chinese girls 10–17 who had reached menarche 146 participants were classified as early menarche | n = 855 | PM2.5 | menarche timing | Higher exposure to PM2.5, sulfate, nitrate, ammonium, and organic matter was linked to increased odds of early menarche, with sulfate appearing to play the most important role. |
| Ye et al. [55] | 2017 | Cohort | China | A total of 305 girls at the ages of 9–15 years old were recruited in Hangzhou, China in this study. | n = 305 | pyrethroids exposure | tanner staging + onset of menarche | Pyrethroid exposure is unlikely to contribute to the observed secular trend of earlier pubertal timing in girls. |
| Choi et al. [31] | 2020 | Cross-sectional | Korea | Subset female children and adolescents from the sixth Korean national health and Nutrition Examination survey (KNHANES) | n = 179 | Lead, mercury and Cadmium | timing of menarche | Higher blood concentrations of lead and mercury were associated with lower age of menarche. |
| Igra et al. [32] | 2023 | Cohort | Bangladesh | Children born to women in the Maternal and Infant Nutrition Interventions trial in MATLAB R2025a | n = 935 | Exposure to Cadmium, Lead, and Arsenic | age at menarche | Long-term childhood cadmium exposure was associated with later menarche, whereas the associations with child lead exposure were inconclusive. Maternal exposure to arsenic, but not cadmium or lead, was associated with later menarche. |
| Igra et al. [56] | 2024 | Cohort | Bangladesh | Pregnant women who received services from the International Centre for Diarrhoeal Disease Research in Bangladesh | n = 582 | Maternal PAH exposure during pregnancy | age at menarche + tanner staging | Girls whose mothers had moderate (second and third quintile) levels of ΣOH-Phe metabolites reached menarche earlier than those with the lowest levels. No link was found for higher quintiles or for other PAH metabolites. |
| James-Todd et al. [36] | 2011 | Cross-sectional | United States | African American, African-Caribbean, Hispanic, and white women | n = 300 | Childhood Hair Product Use | age at menarche | Childhood use of hair oils was associated with earlier recalled age at menarche, independent of year of birth and race/ethnicity. Hair lotions, leave-in conditioners, and other types of products were not associated with an early menarche |
| McDonald et al. [37] | 2018 | Cohort | United States | Women from the New York site of the National Collaborative Perinatal Project, NY-NCPP and women from New York City Multiethnic Breast Cancer Project NYMBCCP | n = 248 | Hair oils, lotions, leave-in conditioners, root stimulators, perms/relaxers, and hair dyes | age at menarche | Childhood use of hair products, especially among African American girls, was linked to earlier menarche. Hair product use in childhood or adulthood showed no strong connection to mammographic density. Non-Hispanic Black women reported higher use than other groups, indicating differences in exposure. |
| Marks et al. [40] | 2017 | Case–control | United Kingdom | Pregnant women with an expected delivery date between 1 April 1991 and 31 December 1992, from three health districts in the former county of Avon, Great Britain. Mother and daughter | n = 370 | Phytoestrogens | age at menarche | Higher levels of enterodiol were linked to later puberty, while enterolactone showed no clear effect. O-DMA, a gut bacteria metabolite of daidzein, was associated with earlier puberty, suggesting gut bacteria may play a role. The study supports the idea that in utero exposure to phytoestrogens could affect pubertal development, as fetal stages are sensitive to endocrine-disrupting compounds. |
| Namulanda et al. [58] | 2016 | Case–control | United Kingdom | Pregnant women living in the Bristol area, in the southwest of England, United Kingdom, with an expected date of delivery from 1 April 1991 to 31 December 1992 and daughters | n = 369 | atrazine analytes | age at menarche | Potential link between in utero exposure to DACT (a degradate of atrazine) and earlier timing of menarche. |
4. Discussion
4.1. Recommendations
4.2. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bajpai, A.; Bansal, U.; Rathoria, R.; Rathoria, E.; Singh, V.; Singh, G.K.; Ahuja, R. A Prospective Study of the Age at Menarche in North Indian Girls, Its Association with the Tanner Stage, and the Secular Trend. Cureus 2023, 15, e45383. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.K.; Fan, H.-Y.; Tsai, M.-C.; Tung, T.-H.; Huynh, Q.T.V.; Huang, S.-Y.; Chen, Y.C. Nutrient Intake through Childhood and Early Menarche Onset in Girls: Systematic Review and Meta-Analysis. Nutrients 2020, 12, 2544. [Google Scholar] [CrossRef]
- Eckert-Lind, C.; Busch, A.S.; Petersen, J.H.; Biro, F.M.; Butler, G.; Bräuner, E.V.; Juul, A. Worldwide Secular Trends in Age at Pubertal Onset Assessed by Breast Development Among Girls: A Systematic Review and Meta-analysis. JAMA Pediatr. 2020, 174, e195881. [Google Scholar] [CrossRef]
- Abe, S.K.; Nishio, M.; Huang, H.-L.; Leung, C.Y.; Islam, R.; Rahman, S.; Saito, E.; Shin, A.; Merritt, M.A.; Choi, J.-Y.; et al. Age at menarche by birth cohort: A pooled analysis of half a million women in Asia. Public Health 2024, 237, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Iwase, M.; Taniyama, Y.; Koyanagi, Y.N.; Kasugai, Y.; Oze, I.; Masuda, N.; Ito, H.; Matsuo, K. A century of change: Unraveling the impact of socioeconomic/historical milestones on age at menarche and other female reproductive factors in Japan. J. Epidemiol. 2024, 34, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Okagbue, H.I.; Samuel, O.W.; Nzeribe, E.C.; Nto, S.E.; Dahunsi, O.E.; Isa, M.B.; Etim, J.; Orya, E.E.; Sampson, S.; Yumashev, A.V. Assessment of the differences in Mean Age at Menarche (MAM) among adolescent girls in rural and urban Nigeria: A systematic review. BMC Public Health 2024, 24, 3468. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; Cook-Wiens, G.; Johnson, B.D.; Braunstein, G.D.; Berga, S.L.; Stanczyk, F.Z.; Pepine, C.J.; Merz, C.N.B.; Shufelt, C.L. Age at Menarche and Risk of Cardiovascular Disease Outcomes: Findings From the National Heart Lung and Blood Institute-Sponsored Women’s Ischemia Syndrome Evaluation. J. Am. Heart Assoc. 2019, 8, e012406. [Google Scholar] [CrossRef]
- Fuhrman, B.J.; Moore, S.C.; Byrne, C.; Makhoul, I.; Kitahara, C.M.; de González, A.B.; Linet, M.S.; Weiderpass, E.; Adami, H.-O.; Freedman, N.D.; et al. Association of the Age at Menarche with Site-Specific Cancer Risks in Pooled Data from Nine Cohorts. Cancer Res. 2021, 81, 2246–2255. [Google Scholar] [CrossRef]
- Lee, J.-S.; Lee, Y.A.; Shin, C.H.; Suh, D.I.; Lee, Y.J.; Yon, D.K. Long-term health outcomes of early menarche in women: An umbrella review. QJM Int. J. Med. 2022, 115, 837–847. [Google Scholar] [CrossRef]
- Edwards, D.R.V.; Baird, D.D.; Hartmann, K.E. Association of Age at Menarche with Increasing Number of Fibroids in a Cohort of Women Who Underwent Standardized Ultrasound Assessment. Am. J. Epidemiol. 2013, 178, 426–433. [Google Scholar] [CrossRef]
- Shirazi, T.N.; Rosinger, A.Y. Reproductive Health Disparities in the USA: Self-Reported Race/Ethnicity Predicts Age of Menarche and Live Birth Ratios, but Not Infertility. J. Racial Ethn. Health Disparities 2021, 8, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Acker, J.; Mujahid, M.; Aghaee, S.; Gomez, S.; Shariff-Marco, S.; Chu, B.; Deardorff, J.; Kubo, A. Neighborhood Racial and Economic Privilege and Timing of Pubertal Onset in Girls. J. Adolesc. Health 2023, 72, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Endocrine Society. Endocrine-Disrupting Chemicals. 2025. Available online: https://www.endocrine.org/advocacy/position-statements/endocrine-disrupting-chemicals (accessed on 29 July 2025).
- Fisher, M.M.; Eugster, E.A. What is in our environment that effects puberty? Reprod. Toxicol. 2014, 44, 7–14. [Google Scholar] [CrossRef]
- Pan, J.; Liu, P.; Yu, X.; Zhang, Z.; Liu, J. The adverse role of endocrine disrupting chemicals in the reproductive system. Front. Endocrinol. 2024, 14, 1324993. [Google Scholar] [CrossRef] [PubMed]
- Lucaccioni, L.; Trevisani, V.; Marrozzini, L.; Bertoncelli, N.; Predieri, B.; Lugli, L.; Berardi, A.; Iughetti, L. Endocrine-disrupting chemicals and their effects during female puberty: A review of current evidence. Int. J. Mol. Sci. 2020, 21, 2078. [Google Scholar] [CrossRef]
- Uldbjerg, C.S.; Koch, T.; Lim, Y.-H.; Gregersen, L.S.; Olesen, C.S.; Andersson, A.-M.; Frederiksen, H.; Coull, B.A.; Hauser, R.; Juul, A.; et al. Prenatal and postnatal exposures to endocrine disrupting chemicals and timing of pubertal onset in girls and boys: A systematic review and meta-analysis. Hum. Reprod. Update 2022, 28, 687–716. [Google Scholar] [CrossRef]
- Buttke, D.E.; Sircar, K.; Martin, C. Exposures to endocrine-disrupting chemicals and age of menarche in adolescent girls in NHANES (2003–2008). Environ. Health Perspect. 2012, 120, 1613–1618. [Google Scholar] [CrossRef]
- Demir, A.; Aydin, A.; Büyükgebiz, A. Thematic Review of Endocrine Disruptors and Their Role in Shaping Pubertal Timing. Children 2025, 12, 93. [Google Scholar] [CrossRef] [PubMed]
- Moodie, J.L.; Campisi, S.C.; Salena, K.; Wheatley, M.; Vandermorris, A.; Bhutta, Z.A. Timing of pubertal milestones in low-and middle-income countries: A systematic review and meta-analysis. Adv. Nutr. 2020, 11, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Leone, T.; Brown, L.J. Timing and determinants of age at menarche in low-income and middle-income countries. BMJ Glob. Health 2020, 5, e003689. [Google Scholar] [CrossRef]
- Ward, J.L.; Harrison, K.; Viner, R.M.; Costello, A.; Heys, M. Adolescent cohorts assessing growth, cardiovascular and cognitive outcomes in low and middle-income countries. PLoS ONE 2018, 13, e0190443. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S. Why should we be concerned about early menarche? Clin. Exp. Pediatr. 2021, 64, 26–27. [Google Scholar] [CrossRef]
- Ibitoye, M.; Choi, C.; Tai, H.; Lee, G.; Sommer, M. Early menarche: A systematic review of its effect on sexual and reproductive health in low-and middle-income countries. PLoS ONE 2017, 12, e0178884. [Google Scholar] [CrossRef]
- Diaz, A.M.R.L.; Laufer, M.R.; Breech, L.L. Menstruation in girls and adolescents: Using the menstrual cycle as a vital sign. Pediatrics 2006, 118, 2245–2250. [Google Scholar] [CrossRef]
- Gore, A.C. Endocrine-disrupting chemicals. JAMA Intern. Med. 2016, 176, 1705–1706. [Google Scholar] [CrossRef]
- Wang, Y.; Qian, H. Phthalates and Their Impacts on Human Health. Healthcare 2021, 9, 603. [Google Scholar] [CrossRef] [PubMed]
- Lucas, A.; Herrmann, S.; Lucas, M. The role of endocrine-disrupting phthalates and bisphenols in cardiometabolic disease: The evidence is mounting. Curr. Opin. Endocrinol. Diabetes Obes. 2022, 29, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Kahn, L.G.; Philippat, C.; Nakayama, S.F.; Slama, R.; Trasande, L. Endocrine-disrupting chemicals: Implications for human health. Lancet Diabetes Endocrinol. 2020, 8, 703–718. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.S. Relationships of Lead, Mercury and Cadmium Levels with the Timing of Menarche among Korean Girls. Child Health Nurs. Res. 2020, 26, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Igra, A.M.; Rahman, A.; Johansson, A.L.; Pervin, J.; Svefors, P.; El Arifeen, S.; Vahter, M.; Persson, L.; Kippler, M. Early Life Environmental Exposure to Cadmium, Lead, and Arsenic and Age at Menarche: A Longitudinal Mother–Child Cohort Study in Bangladesh. Environ. Health Perspect. 2023, 131, 027003. [Google Scholar] [CrossRef] [PubMed]
- Malin, A.J.; Busgang, S.A.; Garcia, J.C.; Bose, S.; Sanders, A.P. Fluoride Exposure and Age of Menarche: Potential Differences Among Adolescent Girls and Women in the United States. Expo. Health 2022, 14, 733–742. [Google Scholar] [CrossRef]
- Harley, K.G.; Berger, K.P.; Kogut, K.; Parra, K.; Lustig, R.H.; Greenspan, L.C.; Calafat, A.M.; Ye, X.; Eskenazi, B. Association of phthalates, parabens and phenols found in personal care products with pubertal timing in girls and boys. Hum. Reprod. 2019, 34, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Bigambo, F.M.; Zhang, M.; Zhang, J.; Yang, X.; Yu, Q.; Wu, D.; Wang, X.; Xia, Y. Exposure to a mixture of personal care product and plasticizing chemicals in relation to reproductive hormones and menarche timing among 12–19 years old girls in NHANES 2013–2016. Food Chem. Toxicol. 2022, 170, 113463. [Google Scholar] [CrossRef]
- James-Todd, T.; Terry, M.B.; Rich-Edwards, J.; Deierlein, A.; Senie, R. Childhood Hair Product Use and Earlier Age at Menarche in a Racially Diverse Study Population: A Pilot Study. Ann. Epidemiol. 2011, 21, 461–465. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.A.; Tehranifar, P.; Flom, J.D.; Terry, M.B.; James-Todd, T. Hair product use, age at menarche and mammographic breast density in multiethnic urban women. Environ. Health 2018, 17, 1. [Google Scholar] [CrossRef] [PubMed]
- Kasper-Sonnenberg, M.; Wittsiepe, J.; Wald, K.; Koch, H.M.; Wilhelm, M. Pre-pubertal exposure with phthalates and bisphenol A and pubertal development. PLoS ONE 2017, 12, e0187922. [Google Scholar] [CrossRef] [PubMed]
- Watkins, D.J.; Sánchez, B.N.; Téllez-Rojo, M.M.; Lee, J.M.; Mercado-García, A.; Blank-Goldenberg, C.; Peterson, K.E.; Meeker, J.D. Phthalate and bisphenol A exposure during in utero windows of susceptibility in relation to reproductive hormones and pubertal development in girls. Environ. Res. 2017, 159, 143–151. [Google Scholar] [CrossRef]
- Marks, K.J.; Hartman, T.J.; Taylor, E.V.; Rybak, M.E.; Northstone, K.; Marcus, M. Exposure to phytoestrogens in utero and age at menarche in a contemporary British cohort. Environ. Res. 2017, 155, 287–293. [Google Scholar] [CrossRef]
- Binder, A.M.; Corvalan, C.; Calafat, A.M.; Ye, X.; Mericq, V.; Pereira, A.; Michels, K.B. Childhood and adolescent phenol and phthalate exposure and the age of menarche in Latina girls. Environ. Health 2018, 17, 32. [Google Scholar] [CrossRef]
- Wolff, M.S.; Pajak, A.; Pinney, S.M.; Windham, G.C.; Galvez, M.; Rybak, M.; Silva, M.J.; Ye, X.; Calafat, A.M.; Kushi, L.H.; et al. Associations of urinary phthalate and phenol biomarkers with menarche in a multiethnic cohort of young girls. Reprod. Toxicol. 2017, 67, 56–64. [Google Scholar] [CrossRef]
- Blanck, H.M.; Marcus, M.; Tolbert, P.E.; Rubin, C.; Henderson, A.K.; Hertzberg, V.S.; Zhang, R.H.; Cameron, L. Age at Menarche and Tanner Stage in Girls Exposed In Utero and Postnatally to Polybrominated Biphenyl. Epidemiology 2000, 11, 641–647. [Google Scholar] [CrossRef]
- Marks, K.J.; Howards, P.P.; Smarr, M.M.; Flanders, W.D.; Northstone, K.; Daniel, J.H.; Calafat, A.M.; Sjödin, A.; Marcus, M.; Hartman, T.J. Prenatal exposure to mixtures of persistent endocrine disrupting chemicals and early menarche in a population-based cohort of British girls. Environ. Pollut. 2021, 276, 116705. [Google Scholar] [CrossRef] [PubMed]
- Harley, K.G.; Rauch, S.A.; Chevrier, J.; Kogut, K.; Parra, K.L.; Trujillo, C.; Lustig, R.H.; Greenspan, L.C.; Sjödin, A.; Bradman, A.; et al. Association of prenatal and childhood PBDE exposure with timing of puberty in boys and girls. Environ. Int. 2017, 100, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.; Chung, E.; DeFranco, E.A.; Pinney, S.M.; Dietrich, K.N. Serum PBDEs and age at menarche in adolescent girls: Analysis of the National Health and Nutrition Examination Survey 2003–2004. Environ. Res. 2011, 111, 831–837. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Averina, M.; Huber, S.; Almås, B.; Brox, J.; Jacobsen, B.K.; Furberg, A.-S.; Grimnes, G. Early menarche and other endocrine disrupting effects of per- and polyfluoroalkyl substances (PFAS) in adolescents from Northern Norway. The Fit Futures study. Environ. Res. 2024, 242, 117703. [Google Scholar] [CrossRef]
- Christensen, K.Y.; Maisonet, M.; Rubin, C.; Holmes, A.; Calafat, A.M.; Kato, K.; Flanders, W.D.; Heron, J.; McGeehin, M.A.; Marcus, M. Exposure to polyfluoroalkyl chemicals during pregnancy is not associated with offspring age at menarche in a contemporary British cohort. Environ. Int. 2011, 37, 129–135. [Google Scholar] [CrossRef]
- Pinney, S.M.; Fassler, C.S.; Windham, G.C.; Herrick, R.L.; Xie, C.; Kushi, L.H.; Biro, F.M. Exposure to Perfluoroalkyl Substances and Associations with Pubertal Onset and Serum Reproductive Hormones in a Longitudinal Study of Young Girls in Greater Cincinnati and the San Francisco Bay Area. Environ. Health Perspect. 2023, 131, 097009. [Google Scholar] [CrossRef] [PubMed]
- Cox, B.; Wauters, N.; Rodríguez-Carrillo, A.; Portengen, L.; Gerofke, A.; Kolossa-Gehring, M.; Lignell, S.; Lindroos, A.K.; Fabelova, L.; Murinova, L.P.; et al. PFAS and Phthalate/DINCH Exposure in Association with Age at Menarche in Teenagers of the HBM4EU Aligned Studies. Toxics 2023, 11, 711. [Google Scholar] [CrossRef]
- Cathey, A.; Watkins, D.J.; Sánchez, B.N.; Tamayo-Ortiz, M.; Solano-Gonzalez, M.; Torres-Olascoaga, L.; Téllez-Rojo, M.M.; Peterson, K.E.; Meeker, J.D. Onset and tempo of sexual maturation is differentially associated with gestational phthalate exposure between boys and girls in a Mexico City birth cohort. Environ. Int. 2020, 136, 105469. [Google Scholar] [CrossRef]
- McGuinn, L.A.; Ghazarian, A.A.; Joseph Su, L.; Ellison, G.L. Urinary bisphenol A and age at menarche among adolescent girls: Evidence from NHANES 2003–2010. Environ. Res. 2015, 136, 381–386. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, D.; Xiong, J.; Cheng, G. Long-term exposure to ambient PM2.5 and its components on menarche timing among Chinese adolescents: Evidence from a representative nationwide cohort. BMC Public Health 2024, 24, 707. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Q.; Wang, W.; Wang, Y.; Zhang, M.; Rao, B.; Ji, X.; Xu, Z.; Wu, S.; Deng, F. Long-term exposures to ambient particulate matter and ozone pollution with lower extremity deep vein thrombosis after surgical operations: A retrospective case-control study in Beijing, China. BMC Public Health 2023, 23, 1956. [Google Scholar] [CrossRef]
- Ye, X.; Pan, W.; Zhao, Y.; Zhao, S.; Zhu, Y.; Liu, W.; Liu, J. Association of pyrethroids exposure with onset of puberty in Chinese girls. Environ. Pollut. 2017, 227, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Igra, A.M.; Trask, M.; Rahman, S.M.; Dreij, K.; Lindh, C.; Krais, A.M.; Persson, L.; Rahman, A.; Kippler, M. Maternal exposure to polycyclic aromatic hydrocarbons during pregnancy and timing of pubertal onset in a longitudinal mother-child cohort in rural Bangladesh. Environ. Int. 2024, 189, 108798. [Google Scholar] [CrossRef]
- Gore, A.C.; Chappell, V.A.; Fenton, S.E.; Flaws, J.A.; Nadal, A.; Prins, G.S.; Toppari, J.; Zoeller, R.T. EDC-2: The Endocrine Society’s Second Scientific Statement on Endocrine-Disrupting Chemicals. Endocr. Rev. 2015, 36, E1–E150. [Google Scholar] [CrossRef] [PubMed]
- Namulanda, G.; Taylor, E.; Maisonet, M.; Barr, D.B.; Flanders, W.D.; Olson, D.; Qualters, J.R.; Vena, J.; Northstone, K.; Naeher, L. In utero exposure to atrazine analytes and early menarche in the Avon Longitudinal Study of Parents and Children Cohort. Environ. Res. 2017, 156, 420–425. [Google Scholar] [CrossRef]
- Wirth, J.J.; Mijal, R.S. Adverse Effects of Low-Level Heavy Metal Exposure on Male Reproductive Function. Syst. Biol. Reprod. Med. 2010, 56, 147–167. [Google Scholar] [CrossRef] [PubMed]
- Hood, R.B.; Hart, J.E.; Laden, F.; Rosner, B.; Chavarro, J.E.; Gaskins, A.J. Exposure to Particulate Matter Air Pollution and Age of Menarche in a Nationwide Cohort of U.S. Girls. Environ. Health Perspect. 2023, 131, 107003. [Google Scholar] [CrossRef]
- Smarr, M.M.; Avakian, M.; Lopez, A.R.; Onyango, B.; Amolegbe, S.; Boyles, A.; Fenton, S.E.; Harmon, Q.E.; Jirles, B.; Lasko, D.; et al. Broadening the Environmental Lens to Include Social and Structural Determinants of Women’s Health Disparities. Environ. Health Perspect. 2024, 132, 15002. [Google Scholar] [CrossRef]
- Osinubi, A.; Angeles, C.P.L.-D.L.; Poitevien, P.; Topor, L.S. Are Black Girls Exhibiting Puberty Earlier? Examining Implications of Race-Based Guidelines. Pediatrics 2022, 150, e2021055595. [Google Scholar] [CrossRef] [PubMed]
- Zota, A.R.; Shamasunder, B. The environmental injustice of beauty: Framing chemical exposures from beauty products as a health disparities concern. Am. J. Obstet. Gynecol. 2017, 217, 418.e1–418.e6. [Google Scholar] [CrossRef] [PubMed]
- Bloom, M.S.; Upadhyaya, S.; Nzegwu, A.W.; Kuiper, J.R.; Buckley, J.P.; Aschner, J.; Barr, D.; Barrett, E.S.; Bennett, D.H.; Dabelea, D.; et al. Racial and ethnic differences in prenatal exposure to environmental phenols and paraben in the ECHO chort. J. Expo. Sci. Environ. Epidemiol. 2025, 35, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Njoku, A.U.; Sampson, N.R. Environment Injustice and Public Health. In Handbook of Social Sciences and Global Public Health; Liamputtong, P., Ed.; Springer International Publishing: Cham, Switzerland, 2023; pp. 1–20. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Njoku, A.; Al-Hassan, M.; Tohura, S.; Albert, K.; Pierce, T.; Sawadogo, W. Exposure to Endocrine-Disrupting Chemicals and Early Onset of Menarche: A Systematic Review. Pollutants 2025, 5, 45. https://doi.org/10.3390/pollutants5040045
Njoku A, Al-Hassan M, Tohura S, Albert K, Pierce T, Sawadogo W. Exposure to Endocrine-Disrupting Chemicals and Early Onset of Menarche: A Systematic Review. Pollutants. 2025; 5(4):45. https://doi.org/10.3390/pollutants5040045
Chicago/Turabian StyleNjoku, Anuli, Mousa Al-Hassan, Sharaban Tohura, Kaleigh Albert, Taryn Pierce, and Wendemi Sawadogo. 2025. "Exposure to Endocrine-Disrupting Chemicals and Early Onset of Menarche: A Systematic Review" Pollutants 5, no. 4: 45. https://doi.org/10.3390/pollutants5040045
APA StyleNjoku, A., Al-Hassan, M., Tohura, S., Albert, K., Pierce, T., & Sawadogo, W. (2025). Exposure to Endocrine-Disrupting Chemicals and Early Onset of Menarche: A Systematic Review. Pollutants, 5(4), 45. https://doi.org/10.3390/pollutants5040045







