A Survey of the Union of European Neonatal and Perinatal Societies on Neonatal Respiratory Care in Neonatal Intensive Care Units
Abstract
1. Introduction
2. Methods
3. Statistics
4. Results
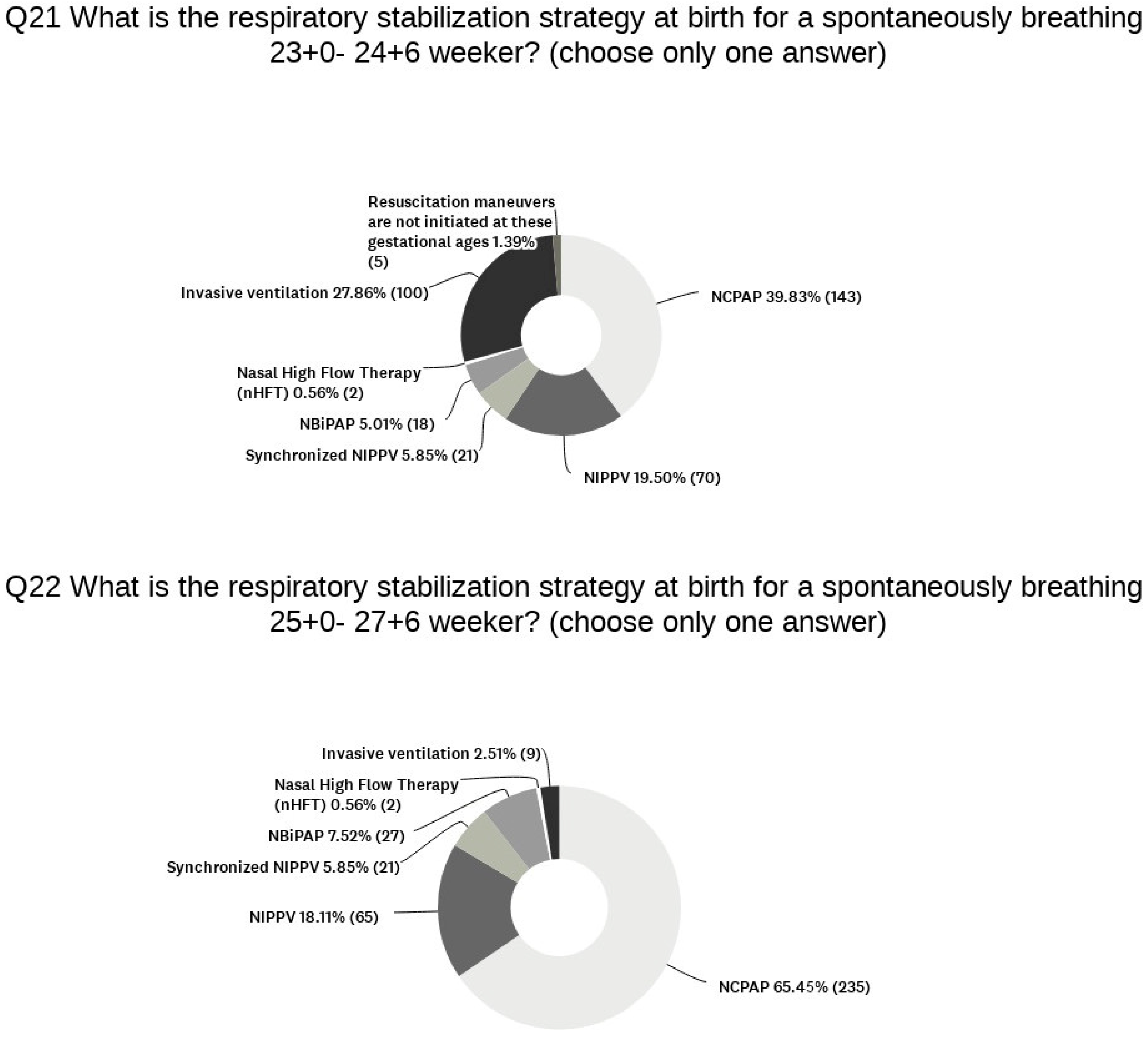
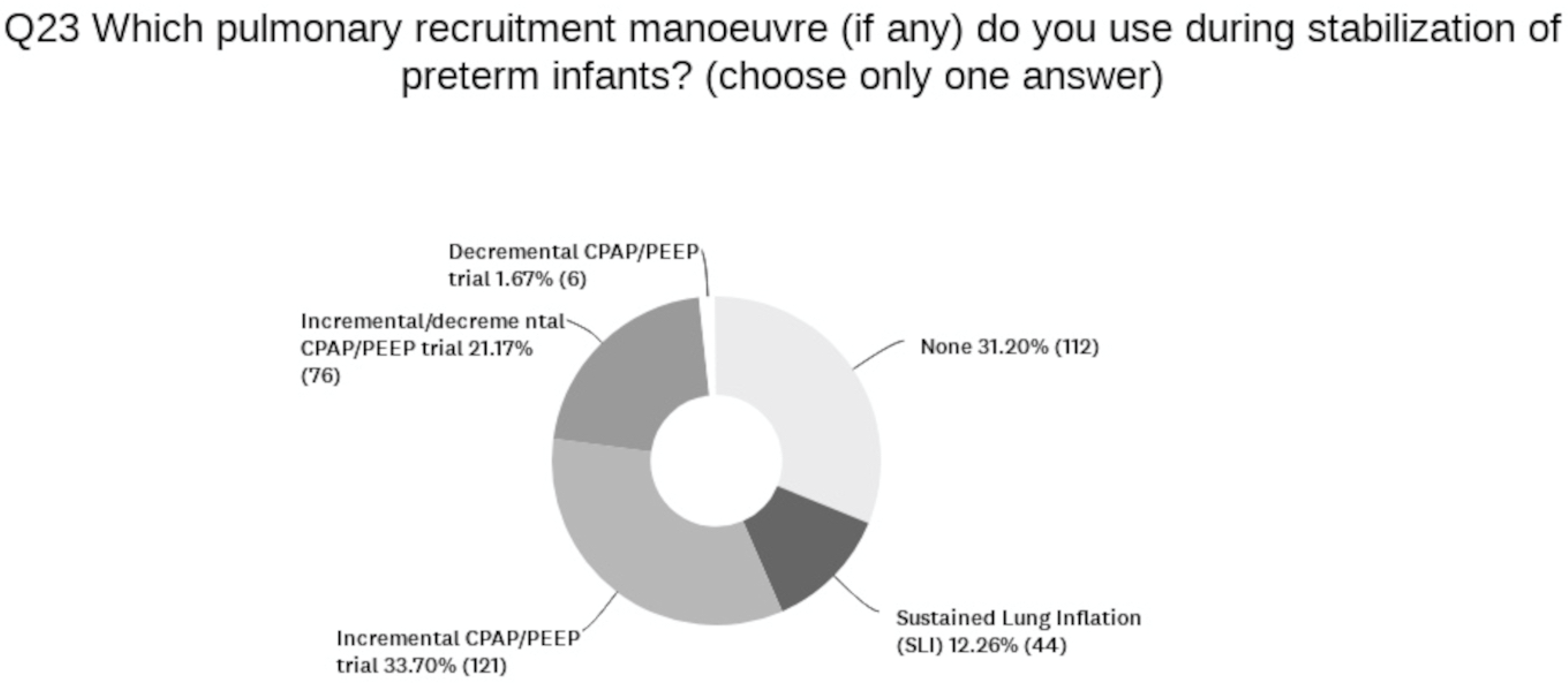
4.1. Devices and Strategies in the Delivery Room
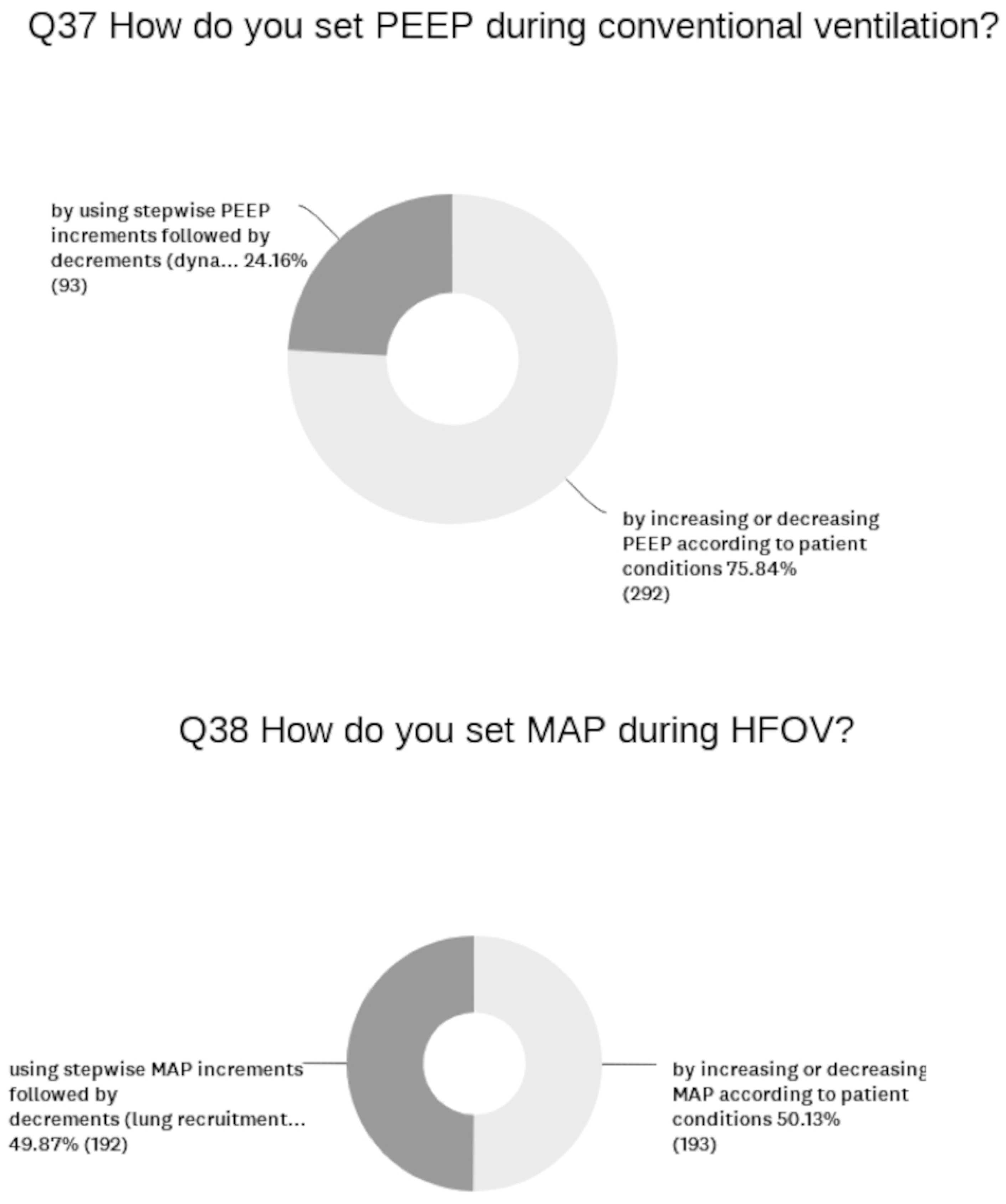
4.2. Devices and Strategies in the NICU
4.3. Drugs for Neonatal Respiratory Diseases
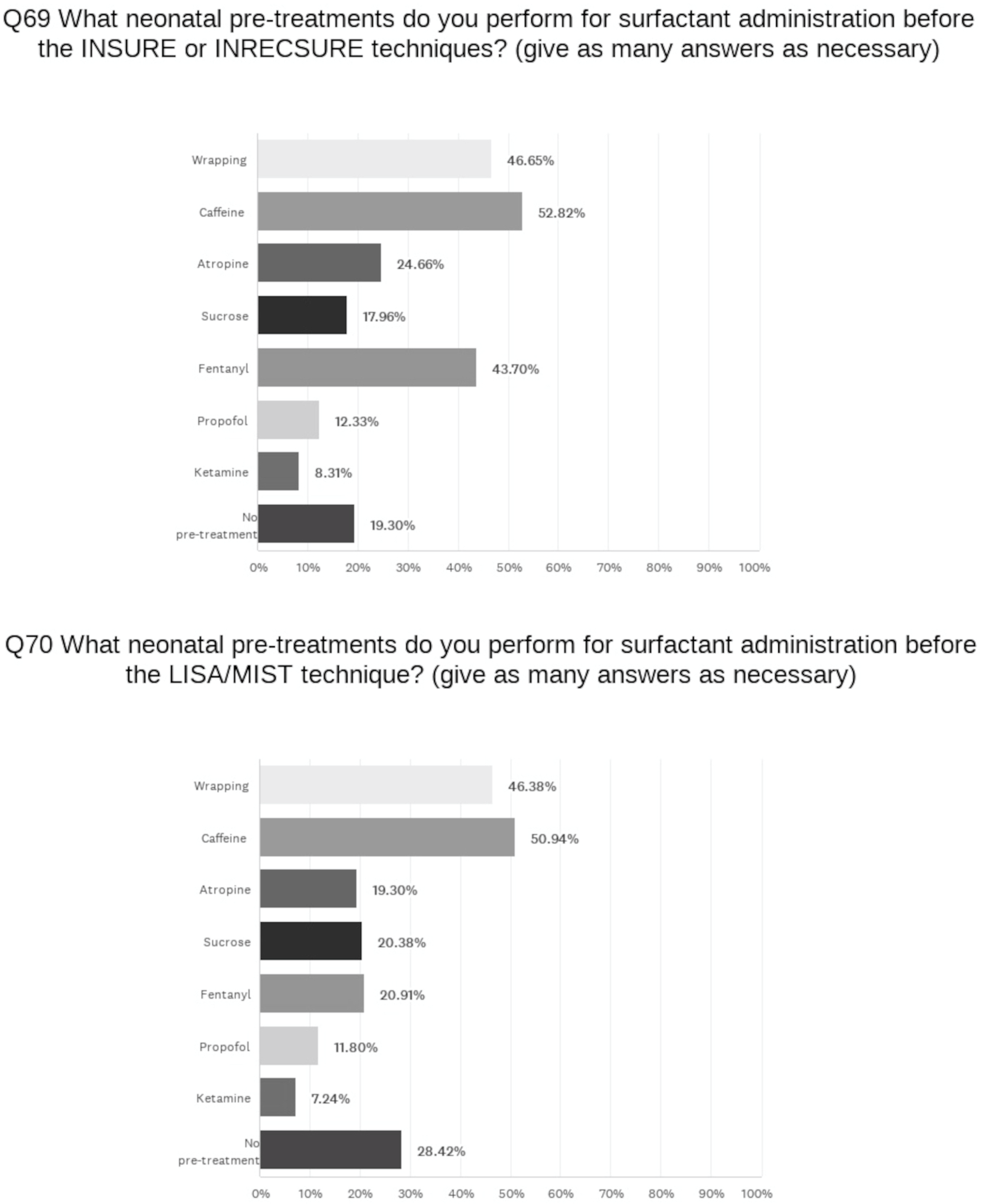
4.3.1. Surfactant
4.3.2. Caffeine
4.3.3. Steroids
4.4. BPD Incidence
4.5. Training
5. Discussion
Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Haumont, D.; Modi, N.; Saugstad, O.D.; Antetere, R.; NguyenBa, C.; Turner, M.; Costeloe, K.; Aelvoet, W. Evaluating preterm care across Europe using the eNewborn European Network database. Pediatr. Res. 2020, 88, 484–495. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Hansen, N.I.; Bell, E.F.; Walsh, M.C.; Carlo, W.A.; Shankaran, S.; Laptook, A.R.; Sánchez, P.J.; Van Meurs, K.P.; Wyckoff, M.; et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network: Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA 2015, 314, 1039–1051. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.S.; Lui, K.; Sjörs, G.; Mirea, L.; Reichman, B.; Adams, M.; Modi, N.; Darlow, B.A.; Kusuda, S.; San Feliciano, L.; et al. Neonatal outcomes of very low birth weight and very preterm neonates: An international comparison. J. Pediatr. 2016, 177, 144–152.e146. [Google Scholar] [CrossRef]
- Rysavy, M.A.; Li, L.; Bell, E.F.; Das, A.; Hintz, S.R.; Stoll, B.J.; Vohr, B.R.; Carlo, W.A.; Shankaran, S.; Walsh, M.C.; et al. Between-hospital variation in treatment and outcomes in extremely preterm infants. N. Engl. J. Med. 2015, 372, 1801–1811. [Google Scholar] [CrossRef]
- Beltempo, M.; Isayama, T.; Vento, M.; Lui, K.; Kusuda, S.; Lehtonen, L.; Sjörs, G.; Håkansson, S.; Adams, M.; Noguchi, A.; et al. Respiratory Management of Extremely Preterm Infants: An International Survey. Neonatology 2018, 114, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Sweet, D.G.; Carnielli, V.P.; Greisen, G.; Hallman, M.; Klebermass-Schrehof, K.; Ozek, E.; Te Pas, A.; Plavka, R.; Roehr, C.C.; Saugstad, O.D.; et al. European Consensus Guidelines on the Management of Respiratory Distress Syndrome: 2022 Update. Neonatology 2023, 120, 3–23. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 29, e34. [Google Scholar] [CrossRef]
- Madar, J.; Roehr, C.C.; Ainsworth, S.; Ersdal, H.; Morley, C.; Rüdiger, M.; Skåre, C.; Szczapa, T.; Te Pas, A.; Trevisanuto, D.; et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 2021, 161, 291–326. [Google Scholar] [CrossRef] [PubMed]
- Aziz, K.; Lee, C.H.C.; Escobedo, M.B.; Hoover, A.V.; Kamath-Rayne, B.D.; Kapadia, V.S.; Magid, D.J.; Niermeyer, S.; Schmölzer, G.M.; Szyld, E.; et al. Part 5: Neonatal Resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S524–S550. [Google Scholar] [CrossRef]
- Vento, G.; Ventura, M.L.; Pastorino, R.; van Kaam, A.H.; Carnielli, V.; Cools, F.; Dani, C.; Mosca, F.; Polglase, G.; Tagliabue, P.; et al. Lung recruitment before surfactant administration in extremely preterm neonates with respiratory distress syndrome (IN-REC-SUR-E): A randomised, unblinded, controlled trial. Lancet Respir. Med. 2021, 9, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Guinsburg, R.; de Almeida, M.F.B.; de Castro, J.S.; Gonçalves-Ferri, W.A.; Marques, P.F.; Caldas, J.P.S.; Krebs, V.L.J.; Souza Rugolo, L.M.S.; de Almeida, J.H.C.L.; Luz, J.H.; et al. T-piece versus self-inflating bag ventilation in preterm neonates at birth. Arch. Dis. Child. Fetal Neonatal Ed. 2018, 103, F49–F55. [Google Scholar] [CrossRef] [PubMed]
- Tribolet, S.; Hennuy, N.; Rigo, V. Ventilation devices for neonatal resuscitation at birth: A systematic review and meta-analysis. Resuscitation 2023, 183, 109681. [Google Scholar] [CrossRef] [PubMed]
- Martherus, T.; Oberthuer, A.; Dekker, J.; Hooper, S.B.; McGillick, E.V.; Kribs, A.; Te Pas, A.B. Supporting breathing of preterm infants at birth: A narrative review. Arch. Dis. Child. Fetal Neonatal Ed. 2019, 104, F102–F107. [Google Scholar] [CrossRef] [PubMed]
- de Medeiros, S.M.; Mangat, A.; Polglase, G.R.; Sarrato, G.Z.; Davis, P.G.; Schmölzer, G.M. Respiratory function monitoring to improve the outcomes following neonatal resuscitation: A systematic review and meta-analysis. Arch. Dis. Child. Fetal Neonatal Ed. 2022, 20, 589–596. [Google Scholar] [CrossRef]
- Fuerch, J.H.; Thio, M.; Halamek, L.P.; Liley, H.G.; Wyckoff, M.H.; Rabi, Y. Resusc. Respiratory function monitoring during neonatal resuscitation: A systematic review. Plus 2022, 12, 100327. [Google Scholar] [CrossRef]
- Cramer, S.J.E.; Kuypers, K.L.A.M.; Martherus, T.; Dekker, J.; Te Pas, A.B. Technology in the delivery room supporting the neonatal healthcare provider’s task. Semin. Fetal Neonatal Med. 2022, 27, 101333. [Google Scholar] [CrossRef]
- Lara-Cantón, I.; Solaz, A.; Parra-Llorca, A.; García-Robles, A.; Vento, M. Optimal Inspired Fraction of Oxygen in the Delivery Room for Preterm Infants. Children 2019, 6, 29. [Google Scholar] [CrossRef]
- Tingay, D.G. Coordinating Principal Investigators. Available online: https://www.polartrial.org.au (accessed on 15 January 2024).
- Tingay, D.G.; Pereira-Fantini, P.M.; Oakley, R.; McCall, K.E.; Perkins, E.J.; Miedema, M.; Sourial, M.; Thomson, J.; Waldmann, A.; Dellaca, R.L.; et al. Gradual Aeration at Birth Is More Lung Protective Than a Sustained Inflation in Preterm Lambs. Am. J. Respir. Crit. Care Med. 2019, 200, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Kirpalani, H.; Ratcliffe, S.J.; Keszler, M.; Davis, P.G.; Foglia, E.E.; Te Pas, A.; Fernando, M.; Chaudhary, A.; Localio, R.; van Kaam, A.H.; et al. Effect of Sustained Inflations vs Intermittent Positive Pressure Ventilation on Bronchopulmonary Dysplasia or Death Among Extremely Preterm Infants: The SAIL Randomized Clinical Trial. JAMA 2019, 321, 1165–1175. [Google Scholar] [CrossRef] [PubMed]
- Nylander Vujovic, S.; Nava, C.; Johansson, M.; Bruschettini, M. Confounding biases in studies on early- versus late-caffeine in preterm infants: A systematic review. Pediatr. Res. 2020, 88, 357–364. [Google Scholar] [CrossRef]
- Trevisanuto, D.; Gizzi, C.; Gagliardi, L.; Ghirardello, S.; Di Fabio, S.; Beke, A.; Buonocore, G.; Charitou, A.; Cucerea, M.; Degtyareva, M.V.; et al. Neonatal Resuscitation Practices in Europe: A Survey of the Union of European Neonatal and Perinatal Societies. Neonatology 2022, 119, 184–192. [Google Scholar] [CrossRef]
- Dani, C.; Cecchi, A.; Remaschi, G.; Mercadante, D.; la Marca, G.; Boni, L.; Mosca, F. Study protocol: Treatment with caffeine of the very preterm infant in the delivery room: A feasibility study. BMJ Open 2020, 10, e040105. [Google Scholar] [CrossRef] [PubMed]
- Moretti, C.; Gizzi, C. Synchronized Nasal Intermittent Positive Pressure Ventilation. Clin. Perinatol. 2021, 48, 745–759. [Google Scholar] [CrossRef] [PubMed]
- Dargaville, P.A.; Gerber, A.; Johansson, S.; De Paoli, A.G.; Kamlin, C.O.; Orsini, F.; Davis, P.G.; Australian and New Zealand Neonatal Network. Incidence and outcome of CPAP failure in preterm infants. Pediatrics 2016, 138, e20153985. [Google Scholar] [CrossRef]
- Chawla, S.; Natarajan, G.; Shankaran, S.; Carper, B.; Brion, L.P.; Keszler, M.; Carlo, W.A.; Ambalavanan, N.; Gantz, M.G.; Das, A.; et al. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J. Pediatr. 2017, 189, 113–119.e2. [Google Scholar] [CrossRef]
- Klingenberg, C.; Wheeler, K.I.; McCallion, N.; Morley, C.J.; Davis, P.G. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst. Rev. 2017, 10, CD003666. [Google Scholar] [CrossRef]
- Sangsari, R.; Saeedi, M.; Maddah, M.; Mirnia, K.; Goldsmith, J.P. Weaning and extubation from neonatal mechanical ventilation: An evidenced-based review. BMC Pulm. Med. 2022, 22, 421. [Google Scholar] [CrossRef] [PubMed]
- Thébaud, B.; Goss, K.N.; Laughon, M.; Whitsett, J.A.; Abman, S.H.; Steinhorn, R.H.; Aschner, J.L.; Davis, P.G.; McGrath-Morrow, S.A.; Soll, R.F.; et al. Bronchopulmonary dysplasia. Nat. Rev. Dis. Primers 2019, 5, 78. [Google Scholar] [CrossRef] [PubMed]
- Sturrock, S.; Williams, E.; Dassios, T.; Greenough, A. Closed loop automated oxygen control in neonates—A review. Acta Paediatr. 2020, 109, 914–922. [Google Scholar] [CrossRef]
- Luo, J.; Shepard, S.; Nilan, K.; Wood, A.; Monk, H.M.; Jensen, E.A.; Harrington, A.T.; Maschhoff, K.; Kirpalani, H.; Feng, Z.; et al. Improved growth and developmental activity post tracheostomy in preterm infants with severe BPD. Pediatr. Pulmonol. 2018, 53, 1237–1244. [Google Scholar] [CrossRef]
- DeMauro, S.B.; D’Agostino, J.A.; Bann, C.; Bernbaum, J.; Gerdes, M.; Bell, E.F.; Carlo, W.A.; D’Angio, C.T.; Das, A.; Higgins, R.; et al. Developmental outcomes of very preterm infants with tracheostomies. J. Pediatr. 2014, 164, 1303–1310.e2. [Google Scholar] [CrossRef]
- Herting, E.; Härtel, C.; Göpel, W. Less invasive surfactant administration: Best practices and unanswered questions. Curr. Opin. Pediatr. 2020, 32, 228–234. [Google Scholar] [CrossRef]
- Roberts, K.D.; Brown, R.; Lampland, A.L.; Leone, T.A.; Rudser, K.D.; Finer, N.N.; Rich, W.D.; Merritt, T.A.; Czynski, A.J.; Kessel, J.M.; et al. Laryngeal mask airway for surfactant administration in neonates: A randomized, controlled trial. J. Pediatr. 2018, 193, 40–46.e1. [Google Scholar] [CrossRef] [PubMed]
- Tingay, D.G.; Togo, A.; Pereira-Fantini, P.M.; Miedema, M.; McCall, K.E.; Perkins, E.J.; Thomson, J.; Dowse, G.; Sourial, M.; Dellacà, R.L.; et al. Aeration strategy at birth influences the physiological response to surfactant in preterm lambs. Arch. Dis. Child. Fetal Neonatal Ed. 2019, 104, F587–F593. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Bao, Y.; Du, L.; Huang, H.; Lv, Q.; Jiang, Y.; Dai, Y.; Chen, Z.; Shi, J.; Shi, Y.; et al. Less invasive surfactant administration versus endotracheal surfactant instillation followed by limited peak pressure ventilation in preterm infants with respiratory distress syndrome in China: Study protocol for a randomized controlled trial. Trials 2020, 21, 516. [Google Scholar] [CrossRef] [PubMed]
- Bezirganoglu, H.; Okur, N.; Buyuktiryaki, M.; Oguz, S.S.; Simsek, G.K.; Canpolat, F.E.; Kutman, G.K. The Effect of Continuous PEEP Administration during Surfactant Instillation on Cerebral Hemodynamics in Intubated Preterm Infants: A NIRS Study. Am. J. Perinatol. 2023, 40, 1537–1542. [Google Scholar] [CrossRef]
- Vliegenthart, R.J.; Ten Hove, C.H.; Onland, W.; van Kaam, A.H. Doxapram Treatment for Apnea of Prematurity: A Systematic Review. Neonatology 2017, 111, 162–171. [Google Scholar] [CrossRef]
- Abiramalatha, T.; Ramaswamy, V.V.; Bandyopadhyay, T.; Somanath, S.H.; Shaik, N.B.; Pullattayil, A.K.; Weiner, G.M. Interventions to Prevent Bronchopulmonary Dysplasia in Preterm Neonates: An Umbrella Review of Systematic Reviews and Meta-analyses. JAMA Pediatr. 2022, 176, 502–516. [Google Scholar] [CrossRef]
- Desplanches, T.; Blondel, B.; Morgan, A.S.; Burguet, A.; Kaminski, M.; Lecomte, B.; Marchand-Martin, L.; Rozé, J.C.; Sagot, P.; Truffert, P.; et al. Volume of Neonatal Care and Survival without Disability at 2 Years in Very Preterm Infants: Results of a French National Cohort Study. J. Pediatr. 2019, 213, 22–29.e4. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moretti, C.; Gizzi, C.; Gagliardi, L.; Petrillo, F.; Ventura, M.L.; Trevisanuto, D.; Lista, G.; Dellacà, R.L.; Beke, A.; Buonocore, G.; et al. A Survey of the Union of European Neonatal and Perinatal Societies on Neonatal Respiratory Care in Neonatal Intensive Care Units. Children 2024, 11, 158. https://doi.org/10.3390/children11020158
Moretti C, Gizzi C, Gagliardi L, Petrillo F, Ventura ML, Trevisanuto D, Lista G, Dellacà RL, Beke A, Buonocore G, et al. A Survey of the Union of European Neonatal and Perinatal Societies on Neonatal Respiratory Care in Neonatal Intensive Care Units. Children. 2024; 11(2):158. https://doi.org/10.3390/children11020158
Chicago/Turabian StyleMoretti, Corrado, Camilla Gizzi, Luigi Gagliardi, Flavia Petrillo, Maria Luisa Ventura, Daniele Trevisanuto, Gianluca Lista, Raffaele L. Dellacà, Artur Beke, Giuseppe Buonocore, and et al. 2024. "A Survey of the Union of European Neonatal and Perinatal Societies on Neonatal Respiratory Care in Neonatal Intensive Care Units" Children 11, no. 2: 158. https://doi.org/10.3390/children11020158
APA StyleMoretti, C., Gizzi, C., Gagliardi, L., Petrillo, F., Ventura, M. L., Trevisanuto, D., Lista, G., Dellacà, R. L., Beke, A., Buonocore, G., Charitou, A., Cucerea, M., Filipović-Grčić, B., Jeckova, N. G., Koç, E., Saldanha, J., Sanchez-Luna, M., Stoniene, D., Varendi, H., ... Mosca, F. (2024). A Survey of the Union of European Neonatal and Perinatal Societies on Neonatal Respiratory Care in Neonatal Intensive Care Units. Children, 11(2), 158. https://doi.org/10.3390/children11020158










