Abstract
Background: Assistive technologies (AT) have been used to improve the daily living conditions of people living with dementia (PWD). Research supports the positive impact of the use of AT such as decreased burden on caregivers and behavioral support for people with dementia. Four reviews in the last six years have analyzed AT and PWD, but none have incorporated the dimension of medical outcomes. Objectives: The purpose of this review is to identify the facilitators, barriers, and medical outcomes commensurate with the use of AT with PWD. Method: This review queried The Cumulative Index of Nursing and Allied Health Literature (CINAHL), Web of Science, Science Direct, and PubMed databases for peer-reviewed publications in the last five years for facilitators, barriers, and medical outcomes commensurate with the use of AT with PWD. The study is reported and conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) and the Kruse Protocol for conducting a systematic review. Results: 48 studies were analyzed. Fourteen types of AT, 17 facilitators, 17 barriers, and 16 medical outcomes were identified in the literature. The two most frequently mentioned ATs were cognitive stimulators (9/48, 19%) and social robots (5/48, 10%). The two most frequently mentioned facilitators were caregivers want AT (8/68, 12%) and enables increased independence (7/68, 10%). The top two barriers were cost (8/75, 11%) and PWD reject AT (8/75, 11%). The top medical outcomes were improved cognitive abilities (6/69, 9%), increased activities of daily living (ADLs), and increased autonomy (each at 5/69, 7%): Zero negative outcomes were reported. Conclusion: The systematic review revealed the positive relations that occur when PWD and their caregivers use AT. Although many reservations surrounding the use of AT exist, a majority of the literature shows a positive effect of its use. Research supports a strong support for AT by caregivers due to many positive medical outcomes, but also a reticence to adopt by PWD. If ATs for PWD are a way to reduce stress on caregivers, barriers of cost and complexity need to be addressed through health policy or grants.
1. Introduction
1.1. Rationale
Dementia describes a group of symptoms affecting a person’s cognitive abilities severely enough to interfere with their daily life [1,2]. Currently, over 46 million people live with dementia, and the numbers are expected to increase with the aging of society to 131.5 million by 2025. Dementia is a condition affecting older people and has an impact on families, care givers and society. Commonly, family members are seen to be the care givers to support people with dementia and are usually untrained for this demanding role. The situation, of increasing numbers of those who suffer from dementia combined with an untrained social network to care for them, is rife for a technological intervention.
The etiology and disease stage of dementia patients can be characterized based on their cognitive, behavioral, motor, and functional symptoms [3]. Research supports the incorporation of technology with dementia patients because it plays a role in preventing their cognitive and physical decline. Technological intervention could further propose solutions to the challenges and barriers that limit care in dementia patients [4].
Various technological interventions have been introduced for functions such as of memory support, safety and security for the patient, training for both the caregiver and patient, care delivery, overall treatment, and social interaction [5]. However, barriers to technological treatment, such as privacy concerns, adaptation, and design choice, could result in a decline of the technology’s effectiveness [6]. Assistive technologies for dementia patients vary in their design: for the occasional use of the patient, by the patient, or on the patient (e.g., caregivers) [7]. Technological interventions for dementia patients could provide quality care measures to accommodate daily needs.
Four reviews in the last six years were published. They recognize the rapidly developing world of intelligent assistive technologies (ATs), and attempted to compile comprehensive lists of such devices and their benefit [8,9,10,11]. Date ranges spanned 5–16 years, and the reviewers included studies of both dementia patients and their carers. However, none of these reviews identified the medical outcomes commensurate with the use of AT, which is a basic requirement for a systematic review [12].
1.2. Objectives
The purpose of this review is to compile a current and comprehensive list of facilitators and barriers to the adoption of, and medical outcomes commensurate with, the use of AT by PWD and their carers to perform activities of daily living independently. The results of this review should enable future studies to explore the modifications required for AT to support people with dementia while providing ease of use for the care givers.
2. Methods
2.1. Protocol and Registration
This review followed the Kruse protocol for conducting a systematic review published in 2019 [13], reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [14]. This review was registered with PROSPERO on 7 May 2020: PROSPERO ID CRD42020182167. In accordance PROSPERO rules, the registration was completed before analysis began.
2.2. Eligibility Criteria
Studies were eligible for this review if participants were diagnosed with dementia or they were care givers (carers) of those with dementia (regardless of stage, gender, race, ethnicity, or age), if the intervention was AT, if they were published in a quality, peer-reviewed journal in the English language in the last five years, and it they report either facilitators to adoption, barriers to adoption, or medical outcomes associated with the use of AT. Five years was chosen due to the rapidly advancing field of AT development. A quality assessment will be performed on each article using the Johns Hopkins Nursing Evidence-Based Practice Rating Scale (JHNEBP) [15]. Any study below IV C will be discarded.
2.3. Information Sources
Reviewers queried four databases: The Cumulative Index of Nursing and Allied Health Literature (CINAHL), PubMed (MEDLINE), Web of Science, and Embase (Science Direct). Databases were filtered for the last five years. Database searches occurred between 1–15 February 2020. We expected to find advances in AT and greater level of adoption of AT due to both availability of these devices and the growing number of PWD. We hoped to find fewer barriers to the adoption of AT for PWD.
2.4. Search
Reviewers initially conducted a search on Google Scholar using general terms. When 10 articles were found on the subject, reviewers collected the key terms from these studies to help form a Boolean search string. Using the PubMed Medical Subject Headings (MeSH), reviewers used the terms gathered from the 10 articles to examine how they were indexed and categorized. Once a Boolean search string was assembled, it was tested out several times in PubMed and customized for maximum, most effective yield. The final search string was (“self-help devices” OR “selfhelp devices” OR “self help devices” OR “assistive technology” OR “telemonitoring” OR “tele-monitoring” telemedicine) AND (dementia OR “cognitive impairment”). We used this same search string for all databases. Reviewers filtered out other reviews and helped the database focus on academic or peer-reviewed journals over the last five years.
2.5. Study Selection
Following the Kruse protocol, reviewers conducted three consensus meetings [13]. The first was to select the group of studies to analyze. Once the search identified a large group to screen, the literature matrix manager downloaded the article details from each research database into an Excel literature matrix which served as the applied form from which to extract data. The group leader assigned workload to the group to ensure all abstracts would be screened by at least two reviewers. Reviewers read their assigned abstracts and screened them against the objective statement making a keep or discard recommendation on the shared spreadsheet. Once all abstracts were screened, the group met to discuss disagreements in recommendations. A final determination was made by the end of the meeting by the group leader, by asking another member of the group to read the abstract. A kappa statistic was calculated based on this process [16].
2.6. Data Collection Process
Once the final group of articles for analysis was identified, the group leader assigned workload to ensure all articles were analyzed by at least two reviewers. Reviewers used the applied form as the data extraction tool to collect Participants, Intervention, Comparison, Outcome, Study design (PICOS) and make general observations. Data items on this spreadsheet were published in the protocol [13]. Reviewers independently analyzed articles, extracting all standardized data items as well as general observations commensurate with the objective statement [13]. At consensus meeting 2, these observations were shared, and a narrative analysis was conducted [17]. The narrative analysis attempts to make sense of the observations. From the observations, common threads were identified. Being mindful of the common threads, or themes, reviewers carefully read their articles another time to flush out additional occurrences. Using the themes, reviewers examined interactions between facilitators, barriers, and medical outcomes to determine if some interventions were more consistently successful or problematic than others.
2.7. Data Items
The applied form collected the following data items: participants, AT intervention, study design, results compared to a control group (where applicable), facilitators and barriers to the use of AT, medical outcomes, sample size, bias within studies, effect size, country of origin, statistics used, a quality assessment from the JHNEBP, and general observations about the article that would help interpret the results [15].
2.8. Risk of Bias within and across Studies
General observations of bias are collected throughout the analysis phase. Bias is discussed in the second consensus meeting along with other observations. Key observations of bias, such as selection bias, are discussed because these could limit the external validity of the results. The JHNEBP was used to assess the risk and quality of each study analyzed. The cumulative evidence from the analysis (selective reporting, etc.) is discussed at the second consensus meeting. The JHNEBP is comprised of five levels for strength of evidence and three levels for quality of evidence. The strength of evidence for level 1 is an experimental study or RCT. Level 2 is strictly for quasi-experimental studies. Level 3 is for non-experimental, qualitative, or meta-synthesis studies. Level 4 is for opinion of nationally recognized experts based on research evidence or consensus panels. Level 5 is for opinions of experts that is not based on research evidence. The quality of evidence is listed as A (high), B (good), or C (low quality or major flaws). Each of these levels contain specifics for research, summative reviews, organizational, and expert opinion. For instance, research in level A must have consistent results with sufficient sample size, adequate control, and definitive conclusions. Research in level B must have reasonably consistent results, sufficient sample size, some control, and definitive conclusions. Research at level C has little evidence with inconsistent results, insufficient sample size, and conclusions that cannot be drawn from the data. Articles with a strength of evidence rating below Level 4 will be screened out. Quality of evidence below level B are highly suspect and must have full consensus of the group to be kept for analysis.
2.9. Summary Measures
The review analyzed studies with qualitative, quantitative, and mixed methods, so the summary measures sought were not consistent. The preferred summary statistic would be the risk ratio, but descriptive statistics and means’ comparisons (student-t) are also sufficient. Summary statistics were discussed at the second consensus meeting.
2.10. Synthesis of Results
This subsection addresses a meta-analysis. This is a systematic review. This section is provided to assure reviewers that PRISMA had been followed. It will be deleted prior to publication, if accepted.
2.11. Additional Analysis
At the second consensus meeting, a narrative analysis will be performed to group observations into themes. These themes will be measured across all articles analyzed and reported in summary statistics in a series of affinity matrices. The narrative analysis summarized themes for facilitators, barriers, and medical outcomes. These will be reported in affinity matrices.
3. Results
3.1. Study Selection
The study selection process performed is illustrated in Figure 1. A kappa statistic was calculated after the first consensus meeting (k = 0.85), which indicates strong agreement [16,18]. After screening, removing duplicates, and assessing for eligibility, the 48 articles chosen for analysis came from CINAHL (16, 33%), Web of Science (16, 33%), PubMed (15, 31%), and Science Direct (1, 2%).
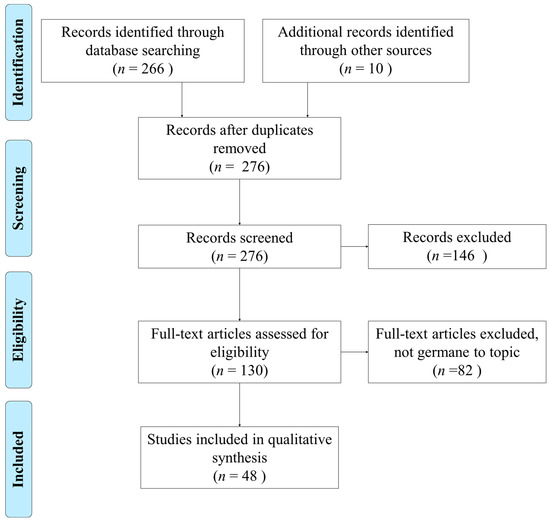
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram of the literature search and selection process.
3.2. Study Characteristics
Using the applied form, reviewers collected several standard items used for summary, such as PICOS. A PICOS table is provided in Table 1. Additional items were collected for analysis, such as forms of AT interventions, facilitators, and barriers to the use of assistive technologies, and the medical outcomes observed from those older adults using AT solutions [13]. These are presented in Table 2. Table 1 and Table 2 lists articles in reverse chronological order: 2019 (4) [3,19,20,21], 2018 (12) [22,23,24,25,26,27,28,29,30,31,32,33], 2017 (14) [34,35,36,37,38,39,40,41,42,43,44,45,46,47], 2016 (11) [48,49,50,51,52,53,54,55,56,57,58], 2015 (7) [59,60,61,62,63,64,65].

Table 1.
PICOS table.

Table 2.
Summary of evidence.
3.3. Risk of Bias within Studies
Reviewers recorded observations of bias at the study level. The most common form of bias was selection bias. Examples of selection bias were all: participants had experience with technology [23], same site [25,28,30,34], or a disproportionately large sample that was male [22,30,36]. These examples of bias limit the external validity of the results.
3.4. Results of Individual Studies
Reviewers collected their observations of intervention and medical outcomes during the analysis phase. The narrative analysis of their observations identified themes. A summary of these themes is listed in Table 1. Repetition in the frame of a theme is due to multiple observations from the same article for that theme. For instance, the theme increased talking comprised observations of “increased utterances” and “increased sustained conversations” [19]. A translation from observations to themes for interventions, medical outcomes, facilitators, and barriers us listed in Table A1, Table A2 and Table A3. Reviewers collected the standard PICOS fields and included them in Table 1. Additional data collected is displayed in Table A4 and Table A5: bias, statistics, country of origin, and quality assessments.
3.5. Synthesis of Results
This subsection addresses meta-analyses. This is a systematic review. This section will be deleted after the review process. It is included to reassure reviewers that we followed the PRISMA checklist.
3.6. Risk of Bias across Studies
Table 3 summarizes the quality indicators identified by the JHNEBP tool [15]. The most prevalent assessment in the strength of evidence (panel a) was level III, followed by I, II, and IV. For quality of evidence (panel b), the most frequently assessed level was level B, followed by A. It is certainly preferable for the strength of evidence to be closer to level I, but that has not resulted from the screening and selection process. This limitation will be addressed later.

Table 3.
Summary of quality assessments.
3.7. Additional Analysis
3.7.1. Interventions of AT
Consensus meeting three identified eight themes and six individual observations that corresponded with AT for PWD. These are listed in Table 4. In the interest of brevity, only the first 60% will be listed. The intervention most often noted was an interview [3,22,23,24,25,29,31,39,43,44,49,57,59,61,63,65]. Researchers interviewed users of AT (PWD and carers) in 16/48 studies (33%). Three of these studies originated in the United Kingdom, two from Norway, two from the Netherlands, and the rest were from single originations: Greece, United States, Pakistan, Finland, Australia, United Kingdom/Italy/Malaysia, Canada, Sweden, and Taiwan. The theme cognitive stimulation (natural language presentation through a Wizard-of-Oz presentation, intelligent cognitive assistant, computerized help information and interaction project, wearable cameras, and evidence-based reasoning and problem solving training) occurred in 9/48 studies (19%) [26,36,37,51,53,54,58,60,65]. Four of these studies originated from the United Kingdom, while the rest were from single originations: France, Scotland, Saudi Arabia, Canada, and Netherlands/Germany/Belgium. Socially assistive robots (artificial intelligence system designed to interact with humans and other robots) were identified in 5/48 studies (10%) [19,35,42,47,62]. These studies all came from single originations: Mexico, Italy/Ireland, Canada, New Zealand, and the United States.

Table 4.
Affinity matrix of ATs.
3.7.2. Facilitators to the Adoption of AT
Fourteen themes and three individual observations were identified as facilitators to the adoption of AT for PWD. These are listed in Table 5. In the interest of brevity, only the top 40% most frequently observed will be reported (other than those not reported). The theme caregivers want AT (AT more ethical than physical barriers, users are open-minded to robotic assistance and sensors, usefulness is high, AT enables PWD to live at home more safely) occurred in 8/68 occurrences (12%) [36,38,39,43,44,47,53,63]. These studies all came from single originations: Australia, Scotland, Canada, United Kingdom, United Kingdom/Italy/Malaysia, Spain, Netherlands, Germany/Belgium, and Taiwan. The theme increased independence (keeps PWD home longer, helps structure everyday events) occurred in 7/68 occurrences (10%) [3,30,40,46,51,53,59]. Three of these studies originated from Sweden, and two were from Canada, while the rest were from single originations: Netherlands, Netherlands/Germany/Belgium. The theme increased safety (increases a sense of security, increases safety) occurred in 6/68 occurrences (9%) [3,25,30,35,41,57]. These studies all came from single originations: Netherlands, Sweden, Norway, United States, New Zealand, and United Kingdom.

Table 5.
Affinity matrix of facilitators to the use of ATs.
3.7.3. Barriers to the Adoption of AT
Eleven themes and six individual observations were identified as barriers to the adoption of AT for PWD. These are listed in Table 6. In the interest of brevity, only the first 50% of the most frequently observed occurrences will be reported (other than those not reported). The theme of cost was identified in 8/75 occurrences (11%) [3,20,35,39,40,52,61]. Two of these studies came from Canada while the rest were from single originations: Netherlands, Australia, New Zealand, Switzerland, and the United Kingdom. The theme PWD do not want AT (PWD reject AT, users do not want a robot, users immediately returned the device, devices are unfamiliar, and participants feel targeted and embarrassed) occurred in 8/75 occurrences (11%) [22,23,24,47,55,62]. Three of these studies originated from the United States, while the others were from single originations: Greece, Canada, Pakistan, Taiwan, and the United Kingdom. The theme complex interfaces (pushing buttons does not always yield the desired result, system was perceived to be complex, complex setup) occurred in 7/75 occurrences (9%) [3,23,25,29,30,51,53]. These studies all came from single originations: Netherlands, Greece, Sweden, Finland, Norway, Canada, Netherlands/Germany/Belgium. The theme development must improve capabilities (false alarms, would only be worn for a few hours due to weight, technical problems, difficult to understand) occurred in 7/75 occurrences (9%) [25,26,29,42,43,48,53]. The theme degenerative nature of dementia complicates the timing of AT used (timing is important – before it is too late, dementia’s progressive nature makes useless today AT that may have been helpful only a short while ago, client’s reduced cognitive and physical abilities greatly reduces the effectiveness of AT more each day) occurred in 7/75 occurrences (9%) [24,25,36,40,42,45,52]. These studies occurred in single originations: Norway, United States, Italy/Ireland, Canada, Scotland, Netherlands, and Switzerland.

Table 6.
Affinity matrix of barriers to the use of ATs.
3.7.4. Medical Outcomes Commensurate with the Adoption of AT
Twelve themes and four individual observations of medical outcomes were recorded commensurate with the adoption of AT. These are listed in Table 7. In the interest of brevity, only the first 40% will be reported. The theme of improved cognitive abilities (reduced sensory loss, increased global cognition, decreased cognitive decline) occurred in 6/69 occurrences (9%) [3,34,56,58,59,60]. Two of these studies originated from the United Kingdom, while the others came from the Netherlands, Australia, Greece, and Sweden. The theme of increased ADLs occurred in 5/69 occurrences (7%) [27,32,44,56,60]. Two of these studies originated from the United Kingdom, while the others came from the United States, Spain, and Greece. The theme of increased autonomy occurred in 5/69 occurrences (7%) [23,25,26,30,59]. Two of these studies originated from Sweden, while the others came from Greece, Norway, and France. The theme of improved memory (helps patients recall past events) occurred in 4/69 occurrences (6%) [34,48,65]. These studies originated from Australia, Sweden, and the United Kingdom. The theme of improved overall health (improved emotional health, improved psychological wellbeing, improved hearing, better tracking of health monitoring through AT) occurred in 4/69 occurrences (6%) [22,33,35,55]. These studies originated from Germany, Pakistan, New Zealand, and the United States. The theme of improved mood (improved emotional wellbeing, improved negative emotions, enabled greater enjoyment) occurred in 4/69 occurrences (6%) [33,34,41,64]. These studies originated from Germany, Australia, British Columbia, and the United States.

Table 7.
Affinity matrix of medical outcomes commensurate with the use of ATs.
3.8. Interactions between Observations
The intervention of eHealth resulted in two instances of increased communication [45,64]. The intervention of cognitive stimulation resulted in two instances of increased independence [51,53]. When researchers interviewed users of AT, there were two instances of PWD do not want AT [22,63] and two instances of increased autonomy [23,25]. The intervention of social robots resulted in two instances of PWD do not want AT [47,62].
4. Discussion
4.1. Summary of Evidence
Fourteen interventions of AT in 48 studies revealed 17 facilitators, 17 barriers, and 16 positive or neutral medical outcomes. The two most frequently mentioned AT were cognitive stimulators (9/48, 19%) and social robots (5/48, 10%). The two most frequently mentioned facilitators were caregivers want AT (8/68, 12%) and enables increased independence (7/68, 10%). The top two barriers were cost (8/75, 11%) and PWD do not want AT (8/75, 11%). The top medical outcomes were improved cognitive abilities (6/69, 9%), increased ADLs, and increased autonomy (each at 5/69, 7%): Zero negative outcomes were reported. Interactions of note occurred with interventions of eHealth and cognitive stimulation, which resulted in multiple observations of increased communication and increased independence, respectively.
Two interesting dichotomies were observed. One study noted no effect in depression, while others noted improved depression [33,41], behavior [24,33,56], mood [33,34,41,64], coping [3,33,62], and decreased stress [25,48]. Also, caregivers want AT [36,38,39,43,44,47,53,63], while PWD do not want AT [22,23,24,47,55,62]. Caregivers feel a sense of relief knowing sensors are in place, and they feel these sensors are more ethical than using physical barriers to prevent elopement, but the complex and foreign nature of the sensors coupled with false alarms cause PWD to reject the same devices that increase their sense of autonomy [23,25,26,30,59].
The observations that AT needs additional development to improve interfaces, reduce false alarms, and improve functionality of devices was no surprise. The challenging aspect to development is seen in the observation that the degenerative nature of AD complicates the timing of AT used. Even the ideal interface, that has been proven effective for a PWD for months, may be obsolete one specific morning due to the degenerative nature of AD, because the PWD may forget how to use it [3,23,52]. Developers might consider AT with phases of simplicity of operation (which might result in reduced capabilities) so that the AT can advance along with the PWD.
Health policy makers should consider augmenting AT development through grants or subsidies. As the aging of society progresses, so will the prevalence of PWD [2]. Development of AT for PWD should be a priority. This corresponds with the theme needs more government involvement.
Social services workers should keep a list of ATs available to PWD at different stages of AD. Caregivers, often spouses or close family, are already experiencing high levels of stress and concern. A general lack of awareness was observed in one study [39]. The combination of more government involvement and funded development should enable such lists to be readily available and regularly updated.
Caregivers should know that AT exists for PWD, and that they are not alone in the struggle to care for their loved ones while also maintaining their own life. AT currently exists, and it improves the quality of life for both PWD and the caregivers [27,32,44,56,60]. The research strongly supports a desire by caregivers for AT. Although a barrier was observed of complex interfaces, several other studies noted the existence AT with simple interfaces with visual and auditory reminders and constant training to control for forgetfulness. Some AT can be provided by the government as part of national health plans.
The findings of this review are commensurate with the other four reviews from the previous six years [8,9,10,11]. The AT reviewed is similar to each of these articles [8]. The decline in memory and cognition is common [9]. One semantic difference is that one review called AT intelligent ATs, and this same review provides an extensive index of AT for clinicians and other stakeholders involved in the management of PWD [10].
The findings in this review are also commensurate with four others from the last year, and the AT reviewed are similar [66,67,68,69,70]. AT interventions can be beneficial to quality of life, social interaction, reducing neuropsychiatric symptoms such as depression, anxiety, and agitation, but continued use of AT becomes problematic due to the progressive nature of dementia [69,70]. Both carers and PWD shared observations on aspects of AT such as ease of use, stability and flexibility of technology, and the importance of privacy and confidentiality [67,68]. One finding that was not in this review was an improvement in pain management, as was found in a review from 2019 [69].
Future research in this area should examine the ethical concerns surrounding AT. If AT yields so many positive medical outcomes, and it is strongly desired by caregivers, why is it also rejected by PWD? Is AT perceived as an annoyance or a bother? Do some view AT as a constraint on liberty? The literature supports the use of AT. It is important for the subject of AT to perceive its value and willingly accept it.
4.2. Limitations
The researchers reviewed papers published between 2015 with 2020 and did not include studies outside this period. One limitation is publication bias for five years. Including some grey literature could have controlled for this limitation. We limited our review to four databases, CINAHL, PubMed, Web of Science, and Science Direct. The intent of including four databases was to mitigate the risk of selection bias. The limitation is that we did not include other databases that might have yielded other articles for consideration.
A team of reviewers determined the articles to be included in the study. This was also done to mitigate the risk of selection bias. The risk of this practice, however, is that the team may have differed in their selection processes. To mitigate this risk, researchers held consensus meetings, identified the research objective, and received multiple reviews for each article. The limitation is that there may not have been enough consensus meetings. The kappa statistic shows the consensus meetings were effective, but a stronger level of agreement is possible.
The assessment of both strength of evidence and quality of evidence was not as high as preferred. The most common strength of evidence was III, while the preference would have been for more level I. To control for this limitation in the future, additional years could have been considered so that more experimental studies or RCTs could have been included in the analysis.
5. Conclusions
The research supports the use of AT with PWD, and many positive or neutral medical outcomes are associated with this practice. This review presents facilitators and barriers associated with the use of AT by PWD, and it presents medical outcomes commensurate with this intervention. It is consistent with other reviews on the same or similar topics. Policy makers and carers should focus on the enablers listed in this review and work to eliminate the barriers to the adoption of AT. Such practice would help policy makers enable additional PWDs and carers to experience the positive aspects of this intervention, for as long as the progressive nature of dementia will allow. Particular focus should be given to helping PWD accept AT based on the positive aspects of their use.
Author Contributions
G.U. was the visualization coordinator and project administrator, who facilitated the project schedule, consensus meetings, milestones, and Figure 1. G.U. analyzed 1/3 of the articles. S.P. was in charge of the literature matrix and tables, and she analyzed 1/3 of articles. K.P. was the editor, to ensure a consistent voice throughout the review, and she analyzed 1/3 of articles. J.F. helped conceptualize the project and analyzed 1/2 of the articles. C.S.K. designed the review, analyzed all articles, and served as senior editor for the project. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| ADL | activity of daily living |
| ADRD | Alzheimer’s disease and related dementia |
| AMSTAR | assessment of multiple systematic reviews |
| AT | Assistive Technology |
| CCT | Computerized Cognitive Training |
| CT | Cognitive Training |
| CDN | COGKNOW Day Navigator |
| CINAHL | Cumulative Index of Nursing and Allied Health Literature |
| CRDL | (not English) Interactive instrument, developed to stimulate communication between users through sound and touch |
| EPD | Electronic Planning Device |
| GCT | General Cognitive Training |
| ICA | Intelligent cognitive assistants |
| JHNEBP | Johns Hopkins Nursing Evidence-Based Practice rating scale |
| MADRS | Montgomery Asberg’s Depression Rating Scales’ |
| MARIO | Not an abbreviation—just the name of a social robot |
| MCI | Mild Cognitive Impairment |
| MeSH | Medical Subject Heading |
| MMSE | Mini Mental Status Evaluation |
| MrNPS | Mood-related Neuropsychiatric Symptoms |
| NHHI | Nursing Home Hearing Handicap Index |
| PICOS | Participants, Intervention, Comparison (results), Outcomes, Study design |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PWD | People with dementia |
| ReaCT | Reasoning and Problem-Solving Cognitive Training |
| ST-CI | Supportive Therapy for Cognitively Impaired Older Adults |
| UCD | User Centered Design |
Key Terms
| Dementia | A progressive, irreversible decline in mental function |
| AT Device | AT device is defined as any item, piece of equipment, or product system whether acquired off the shelf, modified or customized that is used to increase, maintain, or improve functional capabilities of individuals with disabilities. |
| Caregivers or Carers | A caregiver is someone, typically over age 18, who provides care for another. It may be a person who is responsible for the direct care, protection, and supervision of children in a childcare home, or someone who tends to the needs of the elderly or disabled. It is generally one who assists another person who is no longer able to perform the critical tasks of personal or household care necessary for everyday survival. |
Appendix A

Table A1.
Map of Observations for Facilitators to Facilitator Themes.
Table A1.
Map of Observations for Facilitators to Facilitator Themes.
| Authors | Facilitators | Facilitator Themes |
|---|---|---|
| Cruz-Sandoval D. and Favela J. | Not reported | Not reported |
| Thomas N.W.D., et al. | Invisible to participant, No interaction with monitoring device necessary | AT are invisible to users |
| No personal interface necessary | ||
| Kenigsberg P.A., et al. | Increases safety, Increased wellbeing, Increased independence | Increased safety |
| Increased wellbeing | ||
| Increased independence | ||
| Czarnuch S., et al. | Not reported | Not reported |
| Billis A., et al. | continuous training on an individual learning pace | Continuous training |
| Lancioni G.E., et al. | Not reported | Not reported |
| Lancioni G.E., et al. | Increased involvement | Increased involvement |
| Olsson A., et al. | Increases sense of security, Increased independence, Increased self-confidence; Increased mindfulness of medication | Increased safety |
| Increased independence | ||
| Increased self-confidence | ||
| Increased mindfulness | ||
| Nauha L., et al. | Not reported | Not reported |
| Holthe T., et al. | Safety & security, Simple interfaces, Visual reminders, Auditive reminders | Increased safety |
| Simple interfaces | ||
| Visual reminders | ||
| Auditory reminders | ||
| Wilz G., et al. | Not reported | Not reported |
| Valdivieso B., et al. | Not reported | Not reported |
| Collins, M. | 1. Caregiver education: educating the client’s family often allowed for more success than educating the client alone due to cognitive or physical impairments (e.g., the client may not remember the education being provided). 2. Providing repeated demonstration and opportunities to practice with the AT for carryover. 3. Having caregivers and family members practice with the equipment was also seen as beneficial to ensure proper and correct usage. 4. Door locks and alarms to protect patients from elopement. 5. Chair alarms, pull cord alarms, and floor alarms can be used to alert caregivers when a client is trying to get up. 6. Medication dispenser to aid in taking correct type and amt of medication. | Continuous training |
| Remote monitoring | ||
| Visual reminders | ||
| Asghar I., et al. | The happy users termed facilitated communication, travel and timely medication and activities support as major contributions of AT support in their lives; the ATs such as software applications and communication websites helped them to stay connected to their loved ones. At the same time, these ATs also support leisure activities like cognitive games and paintings, pictures as memories etc.; the reminders ATs helped the PWD family members and caregivers to set reminders for the specified times to perform important tasks. | Increased communication |
| Increased involvement | ||
| Visual reminders | ||
| Jouvelot P., et al. | Enables pill dispensing, blood pressure measurement, water self-serving. | Visual reminders |
| Remote monitoring | ||
| Thoma-Lürken T., et al. | Not reported | Not reported |
| Kouroupetroglou C., et al. | Speech can still be used from the robot to trigger responses from PWD by using longer pauses and shorter sentences | Increased communication |
| Jiancaro T., et al. | On Design Approaches, user/human-centered design (UCD/HCD) was ‘‘always’’ recommended, followed closely by participatory design; more than 95% of respondents rated usability as important or higher; cost was also rated as ‘‘very important’’ overall; self-confidence (during use) is another key finding with more than 80% of all respondents rating this as ‘‘important’’ or higher | Increased independence |
| Jarvis F., et al. | The most frequently prescribed items were devices that have been commonly available for many years and are usually low cost such as locks and personal identification bracelets | Simple interfaces |
| More ethical than physical barriers | Caregivers want AT | |
| Dethlefs N., et al. | Enjoyment of activities implies willingness to use the interface. | Caregivers want AT |
| Wang R.H., et al. | Users are open-minded to robotic assistance Care givers want robots | Caregivers want AT |
| Toots A., et al. | Four-month high-intensity functional exercise program had positive effects on gait in participants who tested unsupported compared with when walking aids or living support was used | Increased independence |
| Bahar-Fuchs A., et al. | Not reported | Not reported |
| Kiosses D.N., et al. | PATH participants had significantly greater improvement in MADRS emotions than ST-CI participants; improved negative emotions, between lagged and follow-up interview, significantly predicted reduction in suicidal ideation at follow-up interview | Increased safety |
| Soilemezi D., et al. | Five carers reported using assistive devices, such as baby monitors, sensors (chair, motion), and alarms (telecare, door alarm); a large property was considered helpful as it can offer choices and space to accommodate equipment (or even conversions), and implement various environmental strategies; blocking and locking (doors, cupboards, and cabinets) as a strategy to control behaviors and access to rooms or objects | Caregivers want AT |
| Me R., et al. | Acceptability is high, Usefulness is high | Caregivers want AT |
| Teunissen L., et al. | Increases communication between provider, therapist, family member, and patient | Increased communication |
| Darragh M., et al. | Safety & security | Increased safety |
| Garzon-Maldonado G., et al. | Cost savings of 80 euros per user Caregivers prefer it over in-person High satisfaction | Cost benefits |
| Caregivers want AT | ||
| Fardoun H.M., et al. | Technology enables patients to have all the information on any close person, as a remainder, easing their daily lives, improving their self-esteem and stimulating the patient with novel technology | Increased wellbeing |
| Newton L., et al. | Safety & security | Increased safety |
| Lazarou I., et al. | Not reported | Not reported |
| Egan K.J. and Pot A.M. | Not reported | Not reported |
| Wolters M.K., et al. | Some AT can speak to the person with dementia, which is helpful. | Auditory reminders |
| Hattink B.J., et al. | Rosetta system keeps the person with dementia home longer Gives care givers more security and confidence | Increased independence |
| Caregivers want AT | ||
| Adolfsson P., et al. | How important it was to have self-confidence in mastering and controlling the alterations of the product; user-friendly design; support from colleagues and family members; device enhanced their ability to concentrate and focus, resulting in less stress and forgetfulness; facilitated communication and aided the participants in gaining a better understanding of their disability; providing assistance in the development of the participants’ general abilities, such as changing habitual patterns of behavior. | Increased self-confidence |
| Increased mindfulness | ||
| Czarnuch S., and Mihailidis A. | Enables those with dementia to stay home longer | Increased independence |
| Jupiter T. | Two participants immediately wanted new hearing aids because the study helped them realize their hearing was deficient | Increased mindfulness |
| Boger J., et al. | Interdisciplinary collaboration can result in a more holistic understanding of AT research challenges and enable innovative solutions; computer-based automated tool can significantly reduce the time and effort required to perform product usability analysis; products that are implicitly familiar and usable by older adults could foster independent activity completion, potentially reducing reliance on a caregiver; familiarity plays an important (and perhaps crucial) role in a product’s usability | Simple interfaces |
| Jawaid S., and McCrindle R. | Affordable, especially if a person already owns a smartphone; app can be downloaded and installed within seconds and can be set up for use within minutes by anyone with a small knowledge of how to use a smart phone; only requires the older user to remember the single action of holding the phone close to a tag in order to be reminded of something or to perform an action; same tag can be associated with a number of tasks | Cost benefits |
| Simple interfaces | ||
| Arntzen C., et al. | AT had to: 1. be valuable by addressing practical, emotional, and relational challenges 2. fit well into, or be a better solution for, habitual practice and established strategies 3. generate positive emotions and become a reliable and trustworthy tool 4. interest and engage the family carer. | Increased wellbeing |
| Gibson G., et al. | Some can be provided by social services | Can be provided by government |
| Purves B.A., et al. | The computer serves not only as a capture device for historical stories, but as an integral member of that conversation. | Increased communication |
| Kerssens C., et al. | Helped them relax, enjoy life and reminisce whereas it did not make them feel monitored or watched, nor did they find it to be irritating; brought back good memories | Increased wellbeing |
| Woodberry E., et al. | Sense-Cam showed recall improvement over time in four out of six pts; improved his confidence since he was more assured that he would have something to talk about in social situations | Increased self-confidence |
| Corbett A., et al. | Not reported | Not reported |
| Adolfsson P., et al. | EPDs helped in structuring everyday life events; positive impact of the device on independence, including increased autonomy and self-regulation of everyday activities, as well as enhanced well-being and participation in work and school; respondents needed and received help in organizing such things as time planning/management and in managing time; respondents’ improved volition | Increased independence |
| Increased wellbeing | ||
| Mao H., et al. | Caregivers stated that they would use AT if the technologies were accessible and the cost reasonable; caregivers preferred technologies that prevented accidents or emergencies over technologies that informed them of the occurrence of an accident or that only managed the consequences | Caregivers want AT |

Table A2.
Map of Observations for Barriers to Barrier Themes.
Table A2.
Map of Observations for Barriers to Barrier Themes.
| Authors | Barriers | Barrier Themes |
|---|---|---|
| Cruz-Sandoval D. and Favela J. | Not reported | Not reported |
| Thomas N.W.D., et al. | Not reported | Not reported |
| Kenigsberg P.A., et al. | Cost, Forget how to use it, Complex design, Used infrequently, Liability in case of damage or injury | Cost |
| Users forget how to use them | ||
| Complex interfaces | ||
| Liability concerns | ||
| Czarnuch S., et al. | Cost | Cost |
| Billis A., et al. | Pushing buttons does not always give the desired action, Tend to forget, Social stigma, ethical reasons, Not user friendly, Technical terminology | Complex interfaces |
| Users forget how to use them | ||
| PWD do not want AT | ||
| Ethical concerns | ||
| Technical literacy | ||
| Lancioni G.E., et al. | Not reported | Not reported |
| Lancioni G.E., et al. | Not reported | Not reported |
| Olsson A., et al. | Technical problems frustrate users, Frequent charging of batteries, Poor sound quality on motion sensor | Complex interfaces |
| Poor sound quality | ||
| Limitations of device | ||
| Nauha L., et al. | False alarms, Complex interface, Sound quality | Development must improve capabilities |
| Complex interfaces | ||
| Poor sound quality | ||
| Holthe T., et al. | Timing is important (before it is too late), Because dementia is progressive technology helpful yesterday may be too complicated today, Does not always work properly, In Norway it can take time for AT to be repaired, Information overload, False alarms, Can be buggy, The more complicated the interface the less likely of the success | Degenerative nature of AD complicates timing of AT used |
| Development must improve capabilities | ||
| Needs more government involvement | ||
| Complex interfaces | ||
| Wilz G., et al. | Not reported | Not reported |
| Valdivieso B., et al. | Not reported | Not reported |
| Collins, M. | Client’s reduced cognitive and physical abilities (e.g., visual impairments), and the client’s decreased willingness to use AT | Degenerative nature of AD complicates timing of AT used |
| PWD do not want AT | ||
| Asghar I., et al. | Some PWDs don’t like to adopt ATs as they believe these do not fulfill their requirements, compromise their privacy and result into reduced social circle; small size of texts and fonts used by these ATs as a challenge for them. The small text and font size made it hard to read instruction and act upon them; the volume and heavy weight of smart watches used by the participants made it difficult for them to carry these all the time; participants found learning the operations of reminders based ATs rather difficult and considered it as a challenge for getting proper benefits | PWD do not want AT |
| Font size | ||
| Limitations of device | ||
| Jouvelot P., et al. | Listening pose is not sufficient and needs to be improved | Development must improve capabilities |
| Thoma-Lürken T., et al. | Problems within three domains were consistently described as most important: informal caregiver/social network-related problems (e.g., high load of care responsibility), safety-related problems (e.g., fall risk, wandering), and decreased self-reliance (e.g., problems regarding self-care, lack of day structure) | Safety |
| Kouroupetroglou C., et al. | The fact that MARIO presents verbally all options in a series of questions seem to confuse the PWD, especially those in more advanced stages of the disease. | Degenerative nature of AD complicates timing of AT used |
| Development must improve capabilities | ||
| Jiancaro T., et al. | UCD practices have been developed for user groups with relatively homogeneous characteristics. People with dementia, for example, are a diverse group, and even small subsets of this group tend to have a greater diversity of functionality than is found in groups of able young people | Degenerative nature of AD complicates timing of AT used |
| Cost | ||
| Jarvis F., et al. | 51% (n = 40) overall reported they had not prescribed AT because a client may wander; a lack of awareness by health professionals regarding the different types of AT available has been cited as a barrier to accessing the appropriate equipment in a timely manner for persons with dementia and their carers. | Lack of awareness of availability of AT |
| Cost | Cost | |
| Dethlefs N., et al. | Balancing difficulty of task with advanced stage of dementia | Degenerative nature of AD complicates timing of AT used |
| Wang R.H., et al. | Users do not want a robot, It could decrease interaction with care giver | PWD do not want AT |
| Could decrease interaction with caregiver | ||
| Toots A., et al. | Walking aids appear to conceal changes over time in gait speed | AT could mask changes in gait over time |
| Bahar-Fuchs A., et al. | Not reported | Not reported |
| Kiosses D.N., et al. | Not reported | Not reported |
| Soilemezi D, et al. | Not reported | Not reported |
| Me R., et al. | Intervention not yet in production, Would only be worn a few hours | Development must improve capabilities |
| Teunissen L., et al. | Patients were fascinated by the device, but PWD needed active encouragement to interact with it. | Degenerative nature of AD complicates timing of AT used |
| Darragh M., et al. | Cost | Cost |
| Garzon-Maldonado G., et al. | Not reported | Not reported |
| Fardoun H.M., et al. | Difficulties of reading information in a small screen or taking a proper photo (Some patients were unable to point the smart watch in the right angle to capture the person’s face. Some others even forgot to tap the screen to take the photo) | Font size |
| Newton L., et al. | Not reported | Not reported |
| Lazarou I., et al. | Not reported | Not reported |
| Egan K.J. and Pot A.M. | Education about AT Not enough government involvement Reimbursement from insurance Progressive nature of disease Cost | Users forget how to use them |
| Needs more government involvement | ||
| Cost | ||
| Cost | ||
| Degenerative nature of AD complicates timing of AT used | ||
| Wolters M.K., et al. | Not reported | Not reported |
| Hattink B.J., et al. | Rosetta system has many technical problems Difficult to understand | Development must improve capabilities |
| System was perceived to be complex and hard to work with; Rosetta-portal site which was judged very user-unfriendly, since it often did not work during the trial, gave errors and required persons to try and log-in multiple times | Complex interfaces | |
| Adolfsson P., et al. | Professionals at all levels should provide knowledge on the manageability of the EPD to the user; participants were in most need of the EPDs outdoors, but the outdoor climate often prevented using the device effectively; deficiencies in the EPDs could be related to software issues or that the product was not flexible; product assortment was sometimes seen as limited; did not always have access to software updates and thus could not use the programs that were available in their mobile phone; participants also wished that the technology could be regarded as a natural and obvious support system; | Development must improve capabilities |
| Czarnuch S., and Mihailidis A. | Complex setup | Complex interfaces |
| Jupiter T. | Three participants immediately returned the device. | PWD do not want AT |
| Boger J., et al. | Not reported | Not reported |
| Jawaid S., and McCrindle R. | Not reported | Not reported |
| Arntzen C., et al. | Not reported | Not reported |
| Gibson G., et al. | Those ATs provided by social services are helpful, but the process of obtaining them is very impersonal, Cost | Could decrease interaction with caregiver |
| Cost | ||
| Purves B.A., et al. | Not reported | Not reported |
| Kerssens C., et al. | Care recipients’ inability to use the companion independently due to physical limitations; companion not offering a feature the caregiver had counted on; caregivers ignoring or muting all scheduled shows and not using interventions on demand; care recipients ignoring interventions even when they noticed them and perceived them as positive; care recipients’ unwillingness to share experiences with the caregiver; couples not having enough time or availability to experience the interventions due to circumstances | PWD do not want AT |
| Woodberry E., et al. | One participant felt SenseCam brought attention to him, which he was embarrassed by (didn’t want to wear it) | PWD do not want AT |
| Corbett A., et al. | Not reported | Not reported |
| Adolfsson P., et al. | Not reported | Not reported |
| Mao H., et al. | Persons with dementia are unlikely to use any unfamiliar devices; client-prompting devices were perceived as less useful | PWD do not want AT |

Table A3.
Map of Observations for Medical Outcomes to Outcome Themes.
Table A3.
Map of Observations for Medical Outcomes to Outcome Themes.
| Authors | Medical Outcomes Reported | Medical Outcomes Themes |
|---|---|---|
| Cruz-Sandoval D. and Favela J. | Increased number of utterances and sustained conversations | Increased talking |
| Increased talking | ||
| Thomas N.W.D., et al. | Zero effect on depression | No effect on depression |
| Kenigsberg P.A., et al. | Reduced sensory loss, Reduced isolation, Improved cognitive abilities (memory, judgment, decision making), | Reduced sensory loss |
| Improved coping | ||
| Improved cognitive abilities | ||
| Czarnuch S., et al. | Not reported | Not reported |
| Billis A., et al. | Increase in autonomy | Increased autonomy |
| Lancioni G.E., et al. | Increase in ADLs | Increased ADLs |
| Lancioni G.E., et al. | Increase in step frequency | Increased step frequency |
| Olsson A., et al. | Increase in autonomy, Increased self confidence | Increased autonomy |
| Nauha L., et al. | Not reported | Not reported |
| Holthe T., et al. | Increase in autonomy, Decreased stress | Increased autonomy |
| Decreased stress | ||
| Wilz G., et al. | Improved emotional well-being, Fewer symptoms of depression, Fewer physical health symptoms, Improved coping, Improved behavior | Improved mood |
| Improved depression | ||
| Improved overall health | ||
| Improved coping | ||
| Improved behavior | ||
| Valdivieso B., et al. | Improved quality of life indicators | Increased ADLs |
| Collins, M. | fewer medication errors, Fewer falls, elopement, and fewer kitchen safety incidents | Fewer medication errors |
| Fewer falls | ||
| Improved behavior | ||
| Asghar I., et al. | The use of technology in combination with balanced human care can yield better results for the wellbeing of the PWD; some participants used ATs for health monitoring purposes. These devices helped them to monitor their physical conditions like blood pressure, heartbeat rate, diabetes level, etc., on a regular basis. This continuous health monitoring helped them to adapt a healthier life style | Improved overall health |
| Jouvelot P., et al. | Increased autonomy | Increased autonomy |
| Thoma-Lürken T., et al. | Not reported | Not reported |
| Kouroupetroglou C., et al. | Not reported | Not reported |
| Jiancaro T., et al. | Not reported | Not reported |
| Jarvis F., et al. | Not reported | Not reported |
| Dethlefs N., et al. | Not reported | Not reported |
| Wang R.H., et al. | Not reported | Not reported |
| Toots A., et al. | Improved gait | Increased step frequency |
| Bahar-Fuchs A., et al. | Increase in memory, Increase in global cognition, Increase in learning, Increase in mood | Improved memory |
| Improved cognitive abilities | ||
| Improved mood | ||
| Improved memory | ||
| Kiosses D.N., et al. | Improved negative emotions, Significantly predicted reduction in suicidal ideation at follow-up interview | Improved mood |
| Improved depression | ||
| Soilemezi D., et al. | All the carers recommended the use of equipment as a means to increased quality of life for both the carer and the person with dementia | Increased ADLs |
| Me R., et al. | Not reported | Not reported |
| Teunissen L., et al. | Not reported | Not reported |
| Darragh M, et al. | Improve health and well-being of dementia patients; monitor psychological well-being, | Improved overall health |
| Garzon-Maldonado G., et al. | Not reported | Not reported |
| Fardoun H.M., et al. | Not reported | Not reported |
| Newton L., et al. | Not reported | Not reported |
| Lazarou I., et al. | Improvement in movement intensity, Improved cognitive function, Improved ADLs, Improved behavior | Improved cognitive abilities |
| Improved behavior | ||
| Increased ADLs | ||
| Egan K.J. and Pot A.M. | Not reported | Not reported |
| Wolters M.K., et al. | Improvement to cognitive decline | Improved cognitive abilities |
| Hattink B.J., et al. | Not reported | Not reported |
| Adolfsson P., et al. | Device enhanced their ability to concentrate and focus, resulting in less stress and forgetfulness | Decreased stress |
| Improved memory | ||
| Czarnuch S., and Mihailidis A. | Not reported | Not reported |
| Jupiter T. | Improve hearing | Improved overall health |
| Boger J., et al. | Not reported | Not reported |
| Jawaid S., and McCrindle R. | Not reported | Not reported |
| Arntzen C., et al. | Not reported | Not reported |
| Gibson G., et al. | Not reported | Not reported |
| Purves B.A., et al. | Computer-mediated interactions enable greater engagement and more enjoyment than a traditional method of story capture. | Improved mood |
| Kerssens C., et al. | Made their daily lives easier and made helping their spouse easier | Improved coping |
| Woodberry E., et al. | Help patients recall past events | Improved memory |
| Corbett A., et al. | Significant benefit to activities of daily living in a group of adults older than 60 receiving both the online GCT and ReaCT interventions compared with control, over a period of six months | Increased ADLs |
| Improved cognitive abilities | ||
| Adolfsson P., et al. | Use of EPDs seems to reduce the gap between the challenges the respondents encounter in everyday life and their cognitive disability, increased autonomy | Improved cognitive abilities |
| Increased autonomy | ||
| Mao H., et al. | There were no medical outcomes; the study was done to view the caregivers’ perception on the usefulness of AT devices | Not reported |

Table A4.
Map of Observations for Interventions to Intervention Themes.
Table A4.
Map of Observations for Interventions to Intervention Themes.
| Authors | Intervention | Intervention Theme |
|---|---|---|
| Cruz-Sandoval D. and Favela J. | Socially assistive robots | Social robots |
| Thomas N.W.D., et al. | Telehealth Home-based monitoring Ecological Valid, Ambient, Longitudinal and Unbiased Assessment of Treatment Efficacy in Alzheimer’s Disease (EVALUATE-AD) | Telehealth |
| Kenigsberg P.A., et al. | Several ATs were explored: smart calendar clocks, social robots, auto lighting, computer, smartphone | Interview |
| Czarnuch S., et al. | Predictive model to predict survey results. Survey instrument addressed ATs and ADLs. | Predictive model |
| Billis A., et al. | Interviews about ATs | Interview |
| Lancioni G.E., et al. | Study 1–wireless Bluetooth earpiece linked to the tablet or smartphone. Study 2–walker with technology that provided stimulations and prompts | Mixed interventions |
| Lancioni G.E., et al. | Use of walker with AT | Walker with technology |
| Olsson A., et al. | Sensor technology with individually prerecorded voice reminders as memory support | Sensors with voice |
| Nauha L., et al. | Supportive devices and alarm systems | Interview |
| Holthe T., et al. | Interview to discuss experiences with AT | Interview |
| Wilz G., et al. | Telephone therapy for caregivers | Telephone |
| Valdivieso B., et al. | Telephone-based telehealth which adds technology for remote self-management | Telephone |
| Collins, M. | Interview | Interview |
| Asghar I., et al. | Interview | Interview |
| Jouvelot P., et al. | Lovely User Interface for Servicing Elders | Cognitive stimulation |
| Thoma-Lürken T., et al. | Interview to gain insight into the most important practical problems preventing people with dementia from living at home | Interview |
| Kouroupetroglou C., et al. | MARIO robot | Social robots |
| Jiancaro T., et al. | Exploratory survey with developers | Mixed interventions |
| Jarvis F., et al. | Cross-sectional survey asked about assistive devices for dementia patients | Interview |
| Dethlefs N., et al. | Natural language presentation (Wizard of Oz interface) of cognitive stimulation | Cognitive stimulation |
| Wang R.H., et al. | Robots to assist in daily activities | Social robots |
| Toots A., et al. | Participants were randomized to the high-intensity functional exercise program or a seated attention control activity | Walker with technology |
| Bahar-Fuchs A., et al. | eHealth Tailored and adaptive computer cognitive training in older adults at risk for dementia | eHealth |
| Kiosses D.N., et al. | Two home-delivered psycho-social treatments, Problem Adaptation Therapy (PATH) and Supportive Therapy for Cognitively Impaired Older Adults (ST-CI) | Telehealth |
| Soilemezi D., et al. | Interview with carers in their home | Interview |
| Me R., et al. | Survey on caregivers to assess acceptability, wearability, setting suitability, usability, and general concepts about wearables for navigation for those with dementia. | Interview |
| Teunissen L., et al. | eHealth CRDL, an interactive instrument | eHealth |
| Darragh M., et al. | Survey about a homecare robot | Social robots |
| Garzon-Maldonado G., et al. | Survey instrument asked about a telephone assistive intervention | Telephone |
| Fardoun H.M., et al. | Analyzing pictures taken by a smart watch, which the patient carries, the person in front is recognized and information about him is sent to the watch. | Cognitive stimulation |
| Newton L., et al. | Survey instrument inquired about AT from providers, caregivers, and those with dementia | Interview |
| Lazarou I., et al. | Home monitoring | Tele-monitoring |
| Egan K.J. and Pot A.M. | Focus group to discuss AT | Focus group |
| Wolters M.K., et al. | Intelligent cognitive assistant | Cognitive stimulation |
| Hattink B.J., et al. | Integrates three previous AT research into one modular system which can support dementia patients. Pre-and post-test measures across three countries, questionnaires and interviews. Rosetta was installed in the homes of patients | Cognitive stimulation |
| Adolfsson P, et al. | Electronic planning devices | Electronic planners |
| Czarnuch S., and Mihailidis A. | Intelligent AT, random-decision forest (computer learning) | Cognitive stimulation |
| Jupiter T. | Hearing AT | Hearing AT |
| Boger J., et al. | Self-reporting by asking participants to rate how difficult they found using the tap to be through a verbally administered, single four-point Likert scale question | Interview |
| Jawaid S., and McCrindle R. | Computerized Help Information and Interaction Project (CHIIPS) program | Cognitive stimulation |
| Arntzen C., et al. | Incorporation of AT into everyday life for young people with dementia | Interview |
| Gibson G., et al. | Semi-structured interviews on everyday use of AT | Interview |
| Purves B.A., et al. | Computer Interactive Reminiscence Conversation Aid (CIRCA) | eHealth |
| Kerssens C., et al. | Companion (touch screen technology) that delivers non drug, psychosocial intervention | Social robots |
| Woodberry E., et al. | Wearable camera to improve memory | Cognitive stimulation |
| Corbett A., et al. | Compared evidence-based reasoning and problem-solving cognitive training (ReaCT), general cognitive training (GCT), and a control treatment | Cognitive stimulation |
| Adolfsson P., et al. | Interviewed with support from a study specific guide to explore the subjective experiences of people with cognitive disabilities in relation to the use of EPDs | Interview |
| Mao H., et al. | Questionnaires to determine high perceived usefulness vs low perceived usefulness | Interview |

Table A5.
Observations of Bias, Country of Origin, Statistics Used, and Quality Assessment.
Table A5.
Observations of Bias, Country of Origin, Statistics Used, and Quality Assessment.
| Authors | Bias within Study | Effect Size | Country of Origin | Statistics Used | JHNEBP Quality Assessment | |
|---|---|---|---|---|---|---|
| Strength of Evidence | Quality of Evidence | |||||
| Cruz-Sandoval D. and Favela J. | Single site location | N/A | Mexico | Split-middle trend line | III | B |
| Thomas N.W.D, et al. | Very small sample | N/A | Canada | Descriptive only | III | B |
| Kenigsberg P.A., et al. | Bias in judgment | N/A | Netherlands | Language processing | IV | B |
| Czarnuch S., et al. | Single site location | N/A | Canada | Descriptive only | III | B |
| Billis A., et al. | Single site location Selection bias (all participants had experience with technology) | N/A | Greece | Language processing | III | B |
| Lancioni G.E., et al. | Small sample | Not reported | Unites States | Kolmogorov-Smirnov test | II | B |
| Lancioni G.E., et al. | Convenience sample at one facility only, which limits the external validity | N/A | Italy and Ireland | Kolmogorov-Smirnov test | II | B |
| Olsson A., et al. | Convenience sample at one facility only, which limits the external validity | N/A | Sweden | Language processing | III | B |
| Nauha L., et al. | Tested only in Memory Help apartment or Home environment | N/A | Finland | Carers of older people in Europe (COPE) score of caregivers | II | B |
| Holthe T, et al. | Convenience sample at one facility only, which limits the external validity | N/A | Norway | Language processing | III | B |
| Wilz G., et al. | Sample in one country only | Cohen’s d = 0.2 (small effect) | Germany | Latent variable structural equation model (SEM) | I | A |
| Valdivieso B., et al. | Sample in one country only | N/A | Spain | Language processing | II | B |
| Collins, M. | Small sample size and all participants from Piedmont Triad area of North Carolina; the only inclusion criteria for participating in the current study was being an occupational therapy practitioner | N/A | United States | III | B | |
| Asghar I., et al. | Small sample size | N/A | Pakistan | None listed | III | B |
| Jouvelot P., et al. | Small sample in one country only | N/A | France | Language processing | III | B |
| Thoma-Lürken T., et al. | Not a random sample; participants only had space of sticky note to write answer (could have missed out on more descriptive/clear answers); | N/A | Netherlands | Language processing | III | B |
| Kouroupetroglou C., et al. | Small sample size | Not reported | Italy and Ireland | None listed | III | B |
| Jiancaro T., et al. | Exploratory survey | N/A | Canada | Descriptive statistics and Mann-Whitney U tests | III | B |
| Jarvis F., et al. | Study conducted in only one country | N/A | Australia | Language processing | III | A |
| Dethlefs N., et al. | Small sample | N/A | Scotland | Language processing | III | B |
| Wang R.H., et al. | Social desirability bias | N/A | Canada | Language processing | III | B |
| Toots A., et al. | None found | GROUP A: 4 month ES = −0.05, 7 month ES = 0.04; GROUP B: 4 month ES = 0.20, 7 month ES = 0.16; GROUP C: 4 month ES = 0.29 and −0.33, 7 month ES = 0.47 and −0.50; GROUP D: 4 month ES:.34 and −0.04, 7 month ES = 0.37 and −0.04 | Sweden | Student t-test or the Pearson χ2 test, and Pearson correlation coefficients | I | A |
| Bahar-Fuchs A., et al. | Convenience sample in one city only | N/A | Australia | Descriptive and Cohen’s d | I | A |
| Kiosses D.N., et al. | None reported | 0.75 | United States | None listed | I | B |
| Soilemezi D., et al. | Cross-sectional study and the data were derived from the perspectives of 13 carers, all White, conveniently selected, and heterogeneous in personal and housing conditions | N/A | United Kingdom | None listed | III | B |
| Me R., et al. | Study conducted in only one country | N/A | UK, Italy, and Malaysia | Language processing | III | A |
| Teunissen L., et al. | Person with dementia should live in residential department of the nursing home facility | N/A | Netherlands | Coding framework | III | B |
| Darragh M., et al. | Study conducted in only one city | N/A | New Zealand | Inductive thematic analysis | III | B |
| Garzon-Maldonado G., et al. | Study conducted in one country | N/A | Spain | Descriptive, t-test, and language processing | III | A |
| Fardoun H.M., et al. | None found | N/A | Saudi Arabia | None listed | III | B |
| Newton L., et al. | Conducted in one region of one country only | N/A | United kingdom | Language processing | III | A |
| Lazarou I., et al. | Very small sample, performed at only four homes in the same city | Not reported | Greece | Paired-sample t-test | IV | B |
| Egan K.J. and Pot A.M. | Small sample | N/A | Switzerland | Language processing | IV | A |
| Wolters M.K., et al. | Performed at one location | N/A | United kingdom | Language processing | IV | B |
| Hattink B.J., et al. | Randomized controlled trial in Germany; matched groups in the Netherlands and Belgium; there were significantly more males in the control group than in the experimental group; The professional carers were all female | Small effect size | Netherlands, Germany and Belgium | t-test, Chi Squared, and ANCOVA | I | B |
| The Netherlands, Germany, and Belgium | ||||||
| Adolfsson P., et al. | Small sample | N/A | Sweden | None listed | III | B |
| Czarnuch S., and Mihailidis A. | Performed at one location | Not reported | Canada | Random-decision forest, ANOVA, F-test | II | B |
| Jupiter T. | Performed at one location | Not reported | United States | t-test | III | B |
| Boger J., et al. | Only focused on tap usability; | Not reported | Canada | Likert scale | I | B |
| Jawaid S., and McCrindle R. | Small sample size | Not reported | United Kingdom | None listed | III | B |
| Arntzen C., et al. | Chosen perspectives were deemed suitable in forecasting how new technology is absorbed; small sample size | N/A | Norway | qualitative content analysis | III | B |
| Gibson G., et al. | Performed at one location | N/A | United kingdom | Language processing | III | B |
| Purves B.A., et al. | Very small sample | N/A | British Columbia | Language processing | IV | B |
| Kerssens C., et al. | Small sample | N/A | United States | Barthel index | III | B |
| Woodberry E., et al. | Small sample size. Focused mainly on individuals suffering from AD | N/A | United kingdom | Chi-squared analysis of linear trend | III | B |
| Corbett A., et al. | Only people with access to computer; was biased toward individuals with higher levels of educational attainment; there was a significant dropout between months 3 and 6 | 0.26 | United Kingdom | Histograms and normal Q-Q plots; mixed-effects regression model | I | A |
| Adolfsson P., et al. | Small sample size | N/A | Sweden | III | B | |
| Mao H., et al. | Perspectives of people with dementia were not represented | N/A | Taiwan | None listed | III | B |
References
- Lynn, J.D.; Quinn, E.; Rondón-Sulbarán, J.; Ryan, A.; Martin, S.; McCormack, B. A systematic review of electronic assistive technology within supporting living environments for people with dementia. Dementia 2019, 18, 2371–2435. [Google Scholar] [CrossRef] [PubMed]
- Rathnayake, S.; Moyle, W.; Jones, C.; Calleja, P. mHealth applications as an educational and supportive resource for family carers of people with dementia: An integrative review. Dementia 2019, 18, 3091–3112. [Google Scholar] [CrossRef]
- Kenigsberg, P.A.; Aquino, J.P.; Bérard, A.; Charras, K.; Gzil, F.; Villet, H.; Brémond, F.; Dening, T.; Droës, R.M.; Hicks, B.; et al. Assistive Technologies to Address Capabilities of People with Dementia: From Research to Practice. Dementia 2019, 18, 1568–1595. [Google Scholar] [CrossRef] [PubMed]
- Øksnebjerg, L.; Janbek, J.; Woods, B.; Waldemar, G. Assistive technology designed to support self-management of people with dementia: User involvement, dissemination, and adoption. A scoping review. Int. Psychogeriatr. 2019. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, K.; Freddolino, P.P.; Comas-Herrera, A.; Knapp, M.; Damant, J. Technology-based tools and services for people with dementia and carers: Mapping technology onto the dementia care pathway. Dementia 2019, 18, 725–741. [Google Scholar] [CrossRef]
- Guisado-Fernández, E.; Giunti, G.; Mackey, L.M.; Blake, C.; Caulfield, B.M. Factors Influencing the Adoption of Smart Health Technologies for People With Dementia and Their Informal Caregivers: Scoping Review and Design Framework. JMIR Aging 2019, 2, e12192. [Google Scholar] [CrossRef]
- Ruggiano, N.; Shaw, S.; Bertram, J.; Brown, E.L.; Geldmacher, D.; Clarke, P.; Hristidis, V. The Potential of Information Technology to Navigate Caregiving Systems: Perspectives from Dementia Caregivers. J. Gerontol. Soc. Work 2019, 62, 432–450. [Google Scholar] [CrossRef]
- Evans, J.; Brown, M.; Coughlan, T.; Lawson, G.; Craven, M.P. A Systematic Review of Dementia Focused Assistive Technology. In Human-Computer Interaction: Interaction Technologies, Proceedings of the 17th International Conference, HCI International 2015, Los Angeles, CA, USA, 2–7August, 2015; Springer International Publishing: Cham, Switzerland, 2015; pp. 406–417. [Google Scholar]
- Fleming, R.; Sum, S. Empirical studies on the effectiveness of assistive technology in the care of people with dementia: A systematic review. J. Assist. Technol. 2014, 8, 14–34. [Google Scholar] [CrossRef]
- Ienca, M.; Fabrice, J.; Elger, B.; Wangmo, T.; Caon, M.; Pappagallo, A.S.; Kressig, R.W. Intelligent Assistive Technology for Alzheimer’s Disease and Other Dementias: A Systematic Review. J. Alzheimer’s Dis. 2017, 56, 1301–1340. [Google Scholar] [CrossRef]
- Ienca, M.; Wangmo, T.; Jotterand, F.; Kressig, R.W.; Elger, B. Ethical Design of Intelligent Assistive Technologies for Dementia: A Descriptive Review. Sci. Eng. Ethics 2018, 24, 1035. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S. Writing a Systematic Review for Publication in a Health-Related Degree Program. JMIR Res. Protoc. 2019, 8, e15490. [Google Scholar] [CrossRef] [PubMed]
- David, M.; Alessandro, L.; Jennifer, T.; Douglas, G.A. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar]
- Newhouse, R.P.; Dearholt, S.; Poe, S.; Pugh, L.C.; White, K.M. Organizational Change Strategies for Evidence-Based Practice. Jona J. Nurs. Adm. 2007, 37, 552–557. [Google Scholar] [CrossRef]
- Light, R.J. Measures of response agreement for qualitative data: Some generalizations and alternatives. Psychol. Bull. 1971, 76, 365–377. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar]
- Cruz-Sandoval, D.; Favela, J. Incorporating conversational strategies in a social robot to interact with people with dementia. Dement. Geriatr. Cogn. Disord. 2019, 47, 140–148. [Google Scholar] [CrossRef]
- Czarnuch, S.; Ricciardelli, R.; Mihailidis, A. Informing the development of assistive technologies for persons with dementia by connecting financial measures of wealth to perceptions of task dependence. Technol. Disabil. 2019, 31, 39–49. [Google Scholar] [CrossRef]
- Thomas, N.W.D.; Lindauer, A.; Kaye, J. EVALUATE-AD and Tele-STAR: Novel methodologies for assessment of caregiver burden in a telehealth caregiver intervention - A case study. Dement. Geriatr. Cogn. Disord. 2019, 47, 176–184. [Google Scholar] [CrossRef]
- Asghar, I.; Cang, S.; Yu, H. Usability evaluation of assistive technologies through qualitative research focusing on people with mild dementia. Comput. Hum. Behav. 2018, 79, 192–201. [Google Scholar] [CrossRef]
- Billis, A.; Mantziari, D.; Zilidou, V.; Bamidis, P.D. Co-Creation of an Innovative Vocational Training Platform to Improve Autonomy in the Context of Alzheimer’s Disease. Stud. Health Technol. Inform. 2018, 251, 309–312. [Google Scholar] [PubMed]
- Collins, M.E. Occupational Therapists’ Experience with Assistive Technology in Provision of Service to Clients with Alzheimer’s Disease and Related Dementias. Phys. Occup. Ther. Geriatr. 2018, 36, 179–188. [Google Scholar] [CrossRef]
- Holthe, T.; Jentoft, R.; Arntzen, C.; Thorsen, K. Benefits and burdens: Family caregivers’ experiences of assistive technology (AT) in everyday life with persons with young-onset dementia (YOD). Disabil. Rehabil. Assist. Technol. 2018, 13, 754–762. [Google Scholar] [CrossRef] [PubMed]
- Jouvelot, P.; Wargnier, P.; Benveniste, S.; Rigaud, A.-S. Usability assessment of interaction management support in LOUISE, an ECA-based user interface for elders with cognitive impairment. Technol. Disabil. 2018, 30, 105–126. [Google Scholar] [CrossRef]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; D’Amico, F.; Laporta, D.; Cattaneo, M.G.; Scordamaglia, A.; Pinto, K. Technology-Based Behavioral Interventions for Daily Activities and Supported Ambulation in People With Alzheimer’s Disease. Am. J. Alzheimer’s Dis. Other Dement. 2018, 33, 318–326. [Google Scholar] [CrossRef]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; D’Amico, F.; Pinto, K.; De Vanna, F.; Caffò, A.O. Promoting supported ambulation in persons with advanced Alzheimer’s disease: A pilot study. Disabil. Rehabil. Assist. Technol. 2018, 13, 101–106. [Google Scholar] [CrossRef]
- Nauha, L.; Keranen, N.S.; Kangas, M.; Jamsa, T.; Reponen, J. Assistive technologies at home for people with a memory disorder. Dementia 2018, 17, 909–923. [Google Scholar] [CrossRef]
- Olsson, A.; Persson, A.-C.; Bartfai, A.; Boman, I.-L. Sensor technology more than a support. Scand. J. Occup. Ther. 2018, 25, 79–87. [Google Scholar] [CrossRef]
- Thoma-Lürken, T.; Bleijlevens, M.H.C.; Lexis, M.A.S.; de Witte, L.P.; Hamers, J.P.H. Facilitating aging in place: A qualitative study of practical problems preventing people with dementia from living at home. Geriatr. Nurs. 2018, 39, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Valdivieso, B.; García-Sempere, A.; Sanfélix-Gimeno, G.; Faubel, R.; Librero, J.; Soriano, E.; Peiró, S. The effect of telehealth, telephone support or usual care on quality of life, mortality and healthcare utilization in elderly high-risk patients with multiple chronic conditions. A prospective study. Med. Clin. 2018, 151, 308–314. [Google Scholar] [CrossRef]
- Wilz, G.; Reder, M.; Meichsner, F.; Soellner, R. The Tele.TAnDem Intervention: Telephone-based CBT for Family Caregivers of People with Dementia. Gerontologist 2018, 58, e118–e129. [Google Scholar] [CrossRef]
- Bahar-Fuchs, A.; Webb, S.; Bartsch, L.; Clare, L.; Rebok, G.; Cherbuin, N.; Anstey, K.J. Tailored and Adaptive Computerized Cognitive Training in Older Adults at Risk for Dementia: A Randomized Controlled Trial. J. Alzheimers Dis. 2017, 60, 889–911. [Google Scholar] [CrossRef]
- Darragh, M.; Ahn, H.S.; MacDonald, B.; Liang, A.; Peri, K.; Kerse, N.; Broadbent, E. Homecare Robots to Improve Health and Well-Being in Mild Cognitive Impairment and Early Stage Dementia: Results From a Scoping Study. J. Am. Med. Dir. Assoc. 2017, 18, 1099.e1091–1099.e1094. [Google Scholar] [CrossRef]
- Dethlefs, N.; Milders, M.; Cuayáhuitl, H.; Al-Salkini, T.; Douglas, L. A natural language-based presentation of cognitive stimulation to people with dementia in assistive technology: A pilot study. Inform. Health Soc. Care 2017, 42, 349–360. [Google Scholar] [CrossRef] [PubMed]
- Fardoun, H.M.; Mashat, A.A.; Ramirez Castillo, J. Recognition of familiar people with a mobile cloud architecture for Alzheimer patients. Disabil. Rehabil. 2017, 39, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Garzón-Maldonado, F.J.; Gutiérrez-Bedmar, M.; Serrano-Castro, V.; Requena-Toro, M.V.; Padilla-Romero, L.; García-Casares, N. An assessment of telephone assistance systems for caregivers of patients with Alzheimer disease. Neurol. Engl. Ed. 2017, 32, 595–601. [Google Scholar] [CrossRef]
- Jarvis, F.; Clemson, L.M.; Mackenzie, L. Technology for dementia: Attitudes and practices of occupational therapists in providing assistive technology for way finding. Disabil. Rehabil. Assist. Technol. 2017, 12, 373–377. [Google Scholar] [CrossRef]
- Jiancaro, T.; Jaglal, S.B.; Mihailidis, A. Technology, design and dementia: An exploratory survey of developers. Disabil. Rehabil. Assist. Technol. 2017, 12, 573–584. [Google Scholar] [CrossRef]
- Kiosses, D.N.; Gross, J.J.; Banerjee, S.; Duberstein, P.R.; Putrino, D.; Alexopoulos, G.S. Negative Emotions and Suicidal Ideation during Psychosocial Treatments in Older Adults with Major Depression and Cognitive Impairment. Am. J. Geriatr. Psychiatry 2017, 25, 620–629. [Google Scholar] [CrossRef]
- Kouroupetroglou, C.; Casey, D.; Raciti, M.; Barrett, E.; D’Onofrio, G.; Ricciardi, F.; Giuliani, F.; Greco, A.; Sancarlo, D.; Mannion, A.; et al. Interacting with Dementia: The MARIO Approach. Stud. Health Technol. Inform. 2017, 242, 38–47. [Google Scholar] [PubMed]
- Me, R.C.; Andreoni, G.; Biamonti, A.; Mohd Saad, M.R. Wearable haptic-feedback navigational assistance for people with dementia: Preliminary assessment. Technol. Disabil. 2017, 29, 35–46. [Google Scholar] [CrossRef]
- Soilemezi, D.; Kallitsis, P.; Drahota, A.; Crossland, J.; Stores, R.; Costall, A. The Impact of the Physical Home Environment for Family Carers of People with Dementia: A Qualitative Study. J. Hous. Elder. 2017, 31, 303–333. [Google Scholar] [CrossRef]
- Teunissen, L.; Luyten, T.; de Witte, L. Reconnecting People with Dementia by Using the Interactive Instrument CRDL. Stud. Health Technol. Inform. 2017, 242, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Toots, A.; Littbrand, H.; Holmberg, H.; Nordström, P.; Lundin-Olsson, L.; Gustafson, Y.; Rosendahl, E. Walking Aids Moderate Exercise Effects on Gait Speed in People With Dementia: A Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2017, 18, 227–233. [Google Scholar] [CrossRef]
- Wang, R.H.; Sudhama, A.; Begum, M.; Huq, R.; Mihailidis, A. Robots to assist daily activities: Views of older adults with Alzheimer’s disease and their caregivers. Int. Psychogeriatr. 2017, 29, 67–79. [Google Scholar] [CrossRef]
- Adolfsson, P.; Lindstedt, H.; Pettersson, I.; Hermansson, L.N.; Janeslätt, G. Perception of the influence of environmental factors in the use of electronic planning devices in adults with cognitive disabilities. Disabil. Rehabil. Assist. Technol. 2016, 11, 493–500. [Google Scholar] [CrossRef]
- Arntzen, C.; Holthe, T.; Jentoft, R. Tracing the successful incorporation of assistive technology into everyday life for younger people with dementia and family carers. Dementia 2016, 15, 646–662. [Google Scholar] [CrossRef]
- Boger, J.; Taati, B.; Mihailidis, A. Interdisciplinary development of manual and automated product usability assessments for older adults with dementia: Lessons learned. Disabil. Rehabil. Assist. Technol. 2016, 11, 581–587. [Google Scholar] [CrossRef]
- Czarnuch, S.; Mihailidis, A. Development and evaluation of a hand tracker using depth images captured from an overhead perspective. Disabil. Rehabil. Assist. Technol. 2016, 11, 150–157. [Google Scholar] [CrossRef][Green Version]
- Egan, K.J.; Pot, A.M. Encouraging Innovation for Assistive Health Technologies in Dementia: Barriers, Enablers and Next Steps to Be Taken. J. Am. Med. Dir. Assoc. 2016, 17, 357–363. [Google Scholar] [CrossRef]
- Hattink, B.J.; Meiland, F.J.; Overmars-Marx, T.; de Boer, M.; Ebben, P.W.; van Blanken, M.; Verhaeghe, S.; Stalpers-Croeze, I.; Jedlitschka, A.; Flick, S.E.; et al. The electronic, personalizable Rosetta system for dementia care: Exploring the user-friendliness, usefulness and impact. Disabil. Rehabil. Assist. Technol. 2016, 11, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Jawaid, S.B.; McCrindle, R. Computerised help information and interaction project for people with memory loss and mild dementia. Int. J. Pain Manag. 2016, 9, 265–275. [Google Scholar]
- Jupiter, T. Does Hearing Assistive Technology Provide Benefit to Nursing Home Residents with Dementia? A Pilot Study. J. Acad. Rehabil. Audiol. 2016, 49, 34–39. [Google Scholar]
- Lazarou, I.; Karakostas, A.; Stavropoulos, T.G.; Tsompanidis, T.; Meditskos, G.; Kompatsiaris, I.; Tsolaki, M. A Novel and Intelligent Home Monitoring System for Care Support of Elders with Cognitive Impairment. J. Alzheimer’s Dis. 2016, 54, 1561–1591. [Google Scholar] [CrossRef]
- Newton, L.; Dickinson, C.; Gibson, G.; Brittain, K.; Robinson, L. Exploring the views of GPs, people with dementia and their carers on assistive technology: A qualitative study. BMJ Open 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Wolters, M.K.; Kelly, F.; Kilgour, J. Designing a spoken dialogue interface to an intelligent cognitive assistant for people with dementia. Health Inform. J 2016, 22, 854–866. [Google Scholar] [CrossRef]
- Adolfsson, P.; Lindstedt, H.; Janeslätt, G. How people with cognitive disabilities experience electronic planning devices. NeuroRehabilitation 2015, 37, 379–392. [Google Scholar] [CrossRef]
- Corbett, A.; Owen, A.; Hampshire, A.; Grahn, J.; Stenton, R.; Dajani, S.; Burns, A.; Howard, R.; Williams, N.; Williams, G.; et al. The Effect of an Online Cognitive Training Package in Healthy Older Adults: An Online Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2015, 16, 990–997. [Google Scholar] [CrossRef]
- Gibson, G.; Dickinson, C.; Brittain, K.; Robinson, L. The everyday use of assistive technology by people with dementia and their family carers: A qualitative study. BMC Geriatr. 2015, 15, 89. [Google Scholar] [CrossRef]
- Kerssens, C.; Kumar, R.; Adams, A.E.; Knott, C.C.; Matalenas, L.; Sanford, J.A.; Rogers, W.A. Personalized technology to support older adults with and without cognitive impairment living at home. Am. J. Alzheimer’s Dis. Other Demen. 2015, 30, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Mao, H.F.; Chang, L.H.; Yao, G.; Chen, W.Y.; Huang, W.N. Indicators of perceived useful dementia care assistive technology: Caregivers’ perspectives. Geriatr. Gerontol. Int. 2015, 15, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Purves, B.A.; Phinney, A.; Hulko, W.; Puurveen, G.; Astell, A.J. Developing CIRCA-BC and exploring the role of the computer as a third participant in conversation. Am. J. Alzheimers Dis. Other Demen. 2015, 30, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Woodberry, E.; Browne, G.; Hodges, S.; Watson, P.; Kapur, N.; Woodberry, K. The use of a wearable camera improves autobiographical memory in patients with Alzheimer’s disease. Memory 2015, 23, 340–349. [Google Scholar] [CrossRef]
- Boger, J.; Jackson, P.; Mulvenna, M.; Sixsmith, J.; Sixsmith, A.; Mihailidis, A.; Kontos, P.; Miller Polgar, J.; Grigorovich, A.; Martin, S. Principles for fostering the transdisciplinary development of assistive technologies. Disabil. Rehabil. Assist. Technol. 2017, 12, 480–490. [Google Scholar] [CrossRef]
- Rondon-Sulbaran, J.; Daly-Lynn, J.; Martin, S.; McCormack, B.; Ryan, A. An exploration of the experiences of informal carers supporting a relative living with dementia during and after the move to technology-enriched supported accommodation. Ageing Soc. 2019. [Google Scholar] [CrossRef]
- Van Boekel, L.C.; Wouters, E.J.M.; Grimberg, B.M.; van der Meer, N.J.M.; Luijkx, K.G. Perspectives of Stakeholders on Technology Use in the Care of Community-Living Older Adults with Dementia: A Systematic Literature Review. Healthcare 2019, 7, 73. [Google Scholar]
- Kang, H.S.; Makimoto, K.; Konno, R.; Koh, I.S. Review of outcome measures in PARO robot intervention studies for dementia care. Geriatr. Nurs. 2020, 41, 207–214. [Google Scholar] [CrossRef]
- Sriram, V.; Jenkinson, C.; Peters, M. Carers’ experience of using assistive technology for dementia care at home: A qualitative study. BMJ Open 2020, 10. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).