Abstract
Across the globe, COVID-19 had far-reaching impacts that included healthcare facilities, public health, as well as all forms of transport. Hospitals were experiencing staffing shortages at the same time as patients were experiencing healthcare issues. Consequently, even in developing countries without full access to technology, remote health monitoring became necessary. There was a greater severity of the pandemic in countries with fewer financial and technical resources. It became evident that such remote health monitoring systems that not only allowed the user to monitor their basic health information, but also to communicate that information to healthcare personnel, were essential. In this article, we present an open-source, Internet-of-Things (IoT)-based health monitoring system that is intended to mitigate the basic healthcare challenges posed by remote areas of developing countries. To facilitate remote health monitoring, an IoT server has been configured on an ESP32 chip as part of this study. The microcontroller was also connected to a Max 30100 sensor, a DHT11 sensor, and a global positioning system GPS module. As a result of this, the user is able to measure the heart rate (HR), blood oxygen level (SpO2), human body temperature, ambient temperature and humidity, as well as the location of the user. Through the internet protocol, the important vital signs can be displayed in real time on the dashboard using a private communication network. This article presents the details of a complete system design, implementation, testing, and results. Such systems can help limit the spread of infectious diseases like COVID-19.
1. Introduction
Even though COVID-19 has been declared to be over, as a global health emergency it continues to pose a substantial threat [1]. Everyday, life around the globe has been influenced by COVID-19 devastatingly. During the period of the pandemic, staffing issues in hospitals were widespread. Patients and physicians also maintained social distances and practiced special protective measures, with a significant number of patients not even permitted access to hospitals. It has had far reaching impacts on healthcare systems, mobility, public health, and social behaviors. With the outbreak of the pandemic, digital technologies have also become more prevalent in healthcare [2]. The long-term effects of the pandemic are still being shaped. We recognized that health monitoring, technology, and technology use, however, are important. The growing need for remote health monitoring is realized, even in developing countries without full access to technology. There was a greater hardship experienced by developing countries during the pandemic. This was likely due to a lack of resources to provide care to all affected individuals [3]. There is no doubt that every living individual has a right to and a need for healthcare. In developing countries, however, the healthcare provided to the population is inadequate. Particularly in Pakistan, almost half of the population lacks access to basic healthcare [4]. Rural and remote areas account for a greater proportion of this percentage. A total of 63 percent of Pakistan’s population lives in rural areas [5]. Hospitals, on the other hand, are primarily located in urban areas, whereas primary healthcare facilities are understaffed, poorly equipped, or even inoperative [6,7]. Health monitoring systems are evidently needed, exclusively in remote areas. These systems should enable users to monitor their own health as well as allow healthcare professionals to access and monitor patients remotely. Specifically, this study seeks to provide low-cost solutions for basic health monitoring in remote areas without health facilities to save travel time to urban areas for medical attention.
During the course of this study, the authors have developed an IoT-based health monitoring system. This system allows the user to measure the pulse, blood oxygen level, body temperature, ambient temperature, and humidity levels. Aside from this, it will enable users, as well as health professionals, to access this information as well as the location of the user over the internet protocol (IP) address, using a human machine interface (HMI). As part of the system, the IoT server is configured on an ESP-32 chip. In addition to the ESP-32, a pulse oximeter sensor, a temperature and humidity sensor, and a global positioning system (GPS) module are the part of the hardware components of the system. The system also uses a Wi-Fi router to set up a local TCP/IP wireless network. Furthermore, a computer algorithm is used to process data and visualize it over an internet protocol. The following sections provide an explanation of the system design and some test results.
The remainder of the paper can be summed up along these lines. The second section of this article provides a detailed overview of the literature. The system description can be found in Section 3 of this article. A description of the hardware and technology used is provided in Section 4. In Section 5 and Section 6 we discuss the prototype design and experimental setup of the proposed system. A discussion of the implementation methodology is provided in Section 7. Section 8 contains a description of the tests performed as well as their results. A discussion of the key characteristics of the system is presented in Section 9, which includes an analysis of the system’s power consumption and costs. The article is concluded in Section 10 and future research directions are discussed in Section 11.
2. Related Work
This research has included a comprehensive review of the literature, and a few of the most useful pieces of literature were identified and discussed in this section. According to the authors’ findings in [8], a health monitoring system that uses the IoT is presented primarily for rural areas of Bangladesh. This study addresses affordability and access to healthcare for the public. The primary focus is on COVID-19 patients, diabetic patients, and patients with high blood pressure who do not have instant access to health or emergency clinics for testing. It is also considered by the authors that constant visits to hospitals and the purchase of individual instruments are also very expensive for the general population of the country. Their research led to the development of a system that measures body vitals, including temperature, oxygen saturation levels in the blood, and body temperature. A mobile application was configured in order to visualize the data. Their study also seeks to improve the affordability of healthcare for the general public. Their design is primarily comprised of Arduino UNO, Max30100, LM35, Bluetooth module HC05, and an LCD display. In their developed system, users are limited to viewing health-related data and the mobile application does not allow for simultaneous access by physicians. The authors of [9] developed an IoT-based asthma monitoring system in response to the COVID-19 situation. The system design involved smart sensors, an Arduino UNO, and a mobile application. This study also focused primarily on the rural population of Bangladesh, where people do not have access to adequate healthcare facilities. Asthma patients who are at risk for COVID-19 have been provided with a remote monitoring system intended to overcome challenges in the healthcare system. Medical staff are able to track the condition and emergencies of their patients instantly using a Bluetooth module which transmits information to a mobile application every few seconds. Researchers claim that their research will increase the awareness of asthmatic symptoms and facilitate the effective treatment of asthma anywhere and at any time. This study was conducted over people of diverse medical history, ages, and those who needed constant health observation.
According to another study [10], accurate measurement and timely communication of vital signs are critical to determining a patient’s health status in hospitals, particularly in settings with limited resources. They mainly focused on newborn ill or premature infants who require constant care. Microelectronics and the IoT were used by the authors to develop a hand glove that continuously measures temperature, pulse rate, and pulse oxygen concentration for patients in ICUs. They used STM32F407 microcontroller, ESP8266 as a Wi-Fi module, MAX30100 and LM35. This design incorporates both MAX30100 and LM35 into a glove that is specifically designed for hospital environments. They utilize wearable sensors to measure vital signs and transmit information wirelessly. As a result of these vital signs, an automatic alarm is generated to indicate life-threatening conditions. A further claim of the authors is that their system is both low-cost and reusable for use by different patients. For data visualization, the authors incorporated a website in their design. According to the findings in [11], researchers have developed an IoT-based healthcare system for hospitalized patients. A patient’s room conditions and health indicators are monitored in real-time by the designed system. For measuring carbon monoxide, carbon dioxide, pulse and body temperature, different sensors were used, including MQ-9 for carbon monoxide, MQ-135 for carbon dioxide, and LM35 for body temperature. This study includes a web server that provides access to the system for medical staff. In another study [12], body temperature and respiratory rate are monitored as two of the most important vital signs. ESP8266 Wi-Fi Module and Arduino Mega 2560 were used to implement the monitoring system in an IoT platform. Each vital sign level is determined by two sensor modules, each of which makes use of a temperature sensor. Through Android apps, the design system detects vital signs, analyzes vital signs by age, and displays results wirelessly. According to the authors, the results of their study will reduce the workload of nurses in hospitals and provide more convenient methods for monitoring the vital signs of each patient on a ward. By installing Android apps on any Android device, nurses are able to monitor the patient’s status. Compared to standard measurement equipment or manual observation, the results for both vital signs were almost the same. In this study, LM35 and MLX90614 temperature sensors were used for input by the authors. Two LM35 sensors were used to determine the respiratory rate of the patient, while a sensor, MXL90614, was used to detect the body temperature.
A wearable device that measures COVID-19-related vital signs has been developed by the authors in [13]. There are three layers of functionalities in their system: a wearable IoT sensor layer, a cloud layer with an Application Peripheral Interface (API), and an Android web layer. According to the authors, their design provides an essential platform for monitoring, analyzing, and managing COVID-19 symptoms. Additionally, the work explores the possibility of using a digital remote platform as a wearable device to monitor the health and recovery of an individual who has experienced COVID-19. In this study, all sensor data are received by the MKR 1400 Arduino board. The authors in [14] also highlight the lack of high-quality hospitals and medical personnel in remote areas of developing countries as a major challenge. Based on modern technologies such as the IoT and machine learning, they introduce an innovative and intelligent healthcare system. Using a medical-decision-support system, this system is capable of sensing and processing the data of a patient. Unlike traditional medical care, this system is low-cost for those who live in remote areas. They can use it in order to determine whether they are suffering from a serious health problem and to contact nearby hospitals in order to receive treatment. Their experimental setup included an Arduino UNO, an LM35, and a pulse sensor.
Based on the COVID-19 scenario, the authors of [15] propose a wearable device which measures temperature and heartbeat in real time. Their system consists of a DHT11 for measuring temperature, a pulse sensor for measuring heartbeat, an ultrasonic sensor to maintain social distance, a COVID meter for tracking real time COVID-19 data, in addition to a NodeMCU ESP8266 for processing the data. The system also incorporates a firebase database and an Android application with a Wi-Fi module. Researchers have developed a remote health monitoring system based on the IoT for asthmatic patients in [16]. Patients residing at distant locations can be monitored remotely through remote patient monitoring (RPM), with the data electronically transmitted to healthcare providers for evaluation and consultation. The designed system is capable of measuring oxygen saturation (SpO2), heart rate, body temperature, humidity, volatile gases, room temperature, and electrocardiogram (ECG) using various sensors. This system uses an Android application and a website. To extract data from the patient and send the data to the Firebase Database via Wi-Fi, the authors utilized the NodeMCU ESP8266 as a key component. An artificial intelligence (AI)-based approach to the early diagnosis of COVID-19 is examined in this study. It contributes substantially to the discussion of AI technology for preventing its effects. These include rapid diagnosis and detection, predicting outbreaks, and potential treatment options [17]. The authors in [18] emphasize the limited resources of countries in the context of COVID-19 treatment. They are motivated by the implementation of deep learning and the integration of X-rays and CT scans for the efficiency of analysis and diagnosis. The study from [19] suggests that deep learning can be used to automate the extraction of features from raw sensor data. The researchers used Long Short-Term Memory (LSTM) and smart phone sensor data to solve the Human Activity Recognition (HAR) problem. Table 1 shows the summary of previous work in comparison with the designed system. Another study [20] addresses the shortage of caregivers and healthcare costs in an IoT environment. The study focuses on elderly people with physical limitations in performing daily life activities. On the other hand, a convolutional network-based human posture recognition method is proposed in [21].

Table 1.
Comparison with other studies.
According to the literature reviewed and to the best of the authors’ knowledge, no such IoT-based health monitoring system has been identified that uses an IoT server configured locally using an ESP32 chip, together with a GPS module, pulse oximeter sensors, temperature, and humidity sensors, hosted on a private network. The entire system is installed locally and can be accessed remotely over an internet protocol. Moreover, the system also incorporates the feature of emergency alerts to physicians or other healthcare personnel. Utilizing HMIs, the design system allows users to visualize data and request assistance. The motivation supporting the proposed research work includes (a) a low-cost health monitoring system based on open-source software, (b) low-energy consumption of the proposed system, (c) a high possibility to implement in unserved remote communities, (d) potential application in remote areas without access to the internet and (e) early detection of abnormal health status and post hospitalization care.
This article provides the first and only detailed description of the design and implementation of a health monitoring system that is based on open-source technology. Additionally, the proposed work is novel in its use and application, resulting in the following major key contributions.
- This article demonstrates a novel approach since the authors configured a local IoT server on an ESP32 chip for health monitoring using an internet protocol. Implementation of such a system hosted on private communication channel is particularly effective in remote locations without access to the internet.
- As a pioneer in the implementation of health monitoring systems using open-source technology for remote areas of Pakistan, this study stands out particularly in terms of its design and application.
- The designed system eliminates geographical gaps between the patients and the healthcare workers. It enables the users to measure basic vital signs accurately in real-time and take protective measures ahead of time. Moreover, healthcare workers can also analyze the data and take appropriate actions in good time.
- The use of open-source technology eliminates the need for subscription fees or operating costs associated with the proposed design.
The following section describes the system design.
3. System Design
A description of the hardware and network structure of the proposed open-source, IoT-based health monitoring system is presented in this section.
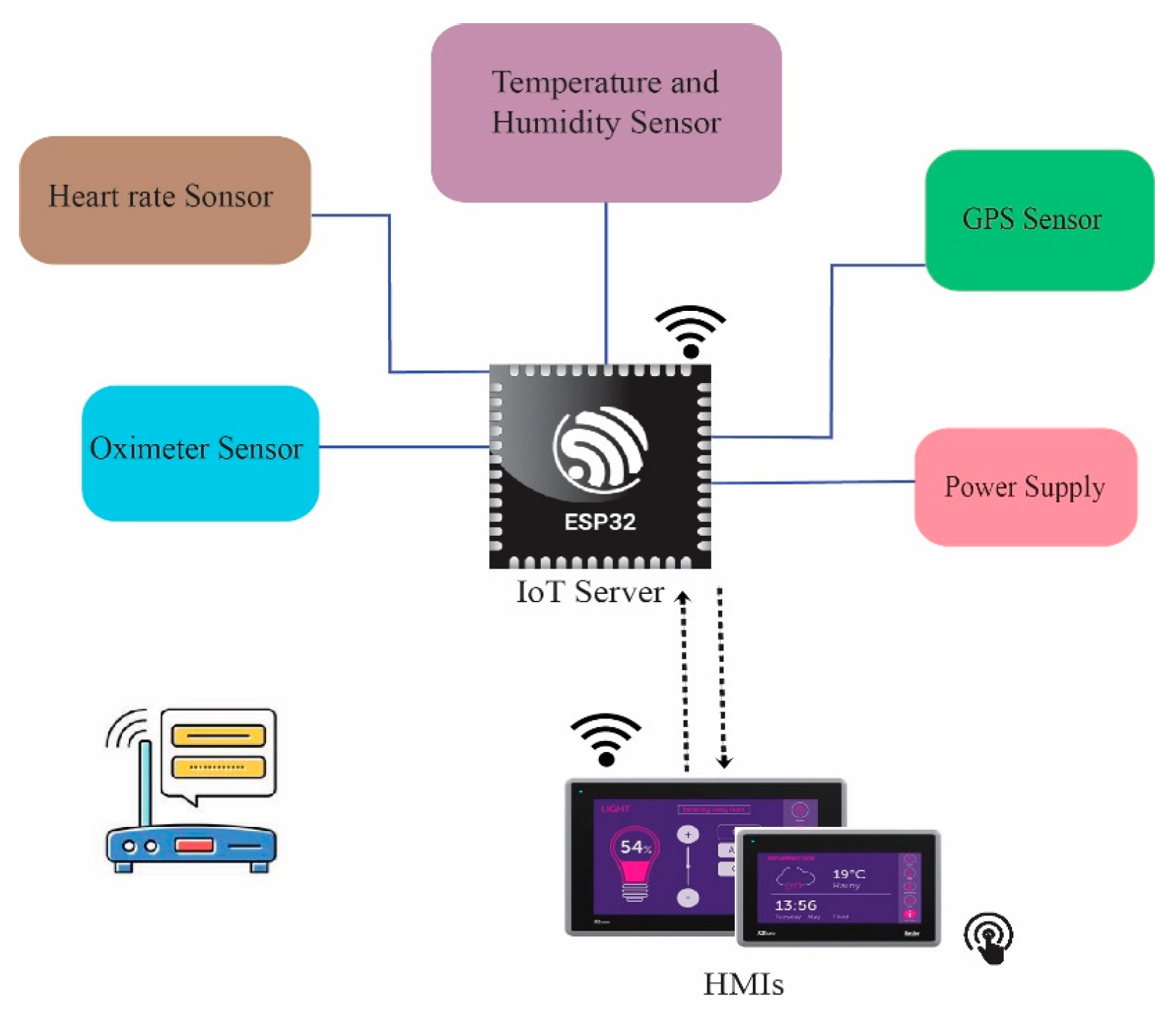
Figure 1 demonstrates an illustration of the proposed system design, which includes an ESP32 microcontroller connected to a power supply, temperature and humidity sensors, pulse oximeter and heart rate sensors, as well as a global position system (GPS) module. Our study involves the configuration of an IoT server using an ESP32 microcontroller. A Wi-Fi router, shown in Figure 1, is used to set up a TCP/IP Wi-Fi-based private network over which the proposed setup is hosted and is accessible via Human Machine Interfaces (HMIs). In order to ensure the security of the network, authentication of users has been configured. To add to this, the foundation of the system is open-source technology.
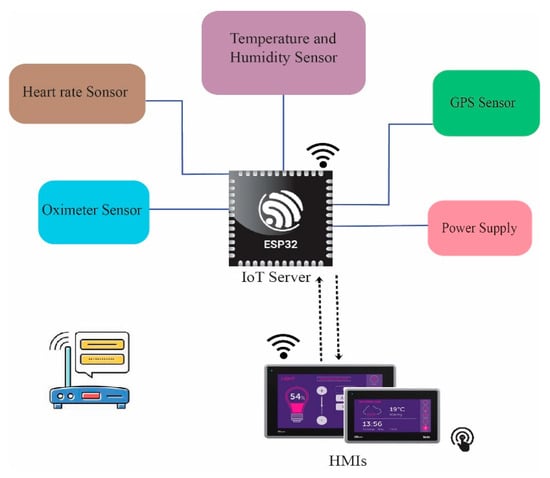
Figure 1.
System Architecture.
Through the sensors, data will be collected. The microcontroller will process the data and send it to the HMIs connected to it. Using the prescribed IP address, the device can be accessed so the caretaker can monitor the patient’s health status and take any necessary action. In addition, the system allows users to create emergency alerts.
4. System Components and Technology Used
An overview of each of the components used in developing the proposed open-source Internet-of-Things-based health monitoring system presented in this section of the paper. As part of the proposed system, an ESP32 microcontroller is used to acquire sensor data. In addition, the data are sent to the IoT server for further processing using the microcontroller. The versatile ESP32 microcontroller serves as the basis for configuring the Internet-of-Things server. Among the other components are a DHT11 sensor, Max30100 sensors, and a GPS module. Due to the fact that the proposed health monitoring system is hosted on a private network, a Wi-Fi router is also one of its essential components described in this section.
4.1. ESP32-WROOM-32
An ESP32 module has a size of 18 by 25.5 mm and is embedded with two low-power Xtensa® 32-bit LX6 microprocessors integrated with a powerful Wi-Fi component conforming to IEEE 802.11 b/g/n standard protocol. Both low-power sensor networks and high-demand applications are supported by this product. As a versatile microcontroller, it is capable of adjusting the clock frequency of the Central Processing Unit (CPU) between 80 MHz and 240 MHz. There are two CPU cores designated as “PRO_CPU” and “APP_CPU” (for “protocol” and “application”, respectively), with each CPU core able to control itself independently. An extensive array of peripherals is integrated into the ESP32, including capacitive touch sensors, hall sensors, UART, SD card interfaces, serial peripheral interfaces (SPI), and serial communication protocols (I2S), as well as serial bus interfaces. Battery-powered applications are compatible with the ESP32 since its sleep current is less than 5 micro-Amperes [22,23]. Integrated Wi-Fi, Bluetooth, and energy-saving features make the device highly adaptable, while the low-cost, low-power microcontroller makes it very cost-effective and a low-power system. This standalone microcontroller can be utilized as a complete system [24]. The reasons that justify the use of the ESP32 in this specific study includes its general purpose input/output (GPIO) pins, its wireless conductivity, its dual core processor, its low power consumption, Arduino IDE compatibility, as well as its open-source nature and its security features such as encryption.
During the course of this study, the ESP32-WROOM-32 was used to develop a local Internet-of-Things server. The server is configured for the monitoring and acquisition of healthcare data. We have connected the ESP32 to a temperature and humidity sensor, pulse oximeter and heart rate sensor, and a GPS module. The server receives real-time required healthcare and location data of patients and displays it onto a dashboard. Patients and healthcare personnel can access the dashboard by connecting to a local internet protocol (IP) address.
4.2. Internet-of-Things (IoT)
A term coined by Kevin Ashton, Executive Director of the Massachusetts Institute of Technology’s Auto-ID Labs in 1999 was the Internet-of-Things [25]. In the IoT, objects are connected with unique identifiers and can communicate with each other with or without the assistance of a computer or the internet. The devices participating in the communication are equipped with sensors that facilitate the communication [26]. An Internet-of-Things (IoT) is characterized by objects equipped with sensors, actuators, and processors that communicate with one another to accomplish a meaningful task. As a result of the Internet-of-Things, a variety of applications have been discovered, including those in healthcare, fitness, education, entertainment, social, energy conservation, environmental monitoring, home automation, and transportation systems. To add to this, human effort has been reduced and quality of life has been improved significantly through the IoT [27]. According to a recent report, the National Intelligence Council and McKinsey Global Institute claim that by 2025, ordinary objects will serve as internet nodes, including furniture, paper documents, food packages, etc. Their vision of the future is based on the integration of technology into the human environment. As things communicate and exchange data autonomously on the Internet-of-Things, no human intervention is required [28]. Furthermore, in Healthcare 4.0, the integration of advanced technologies has enabled healthcare providers to create and improve the quality of healthcare services. From a physical appointment with a physician to remote monitoring and disease prediction, as well as surgery assistive systems, the delivery of healthcare services has evolved substantially [29]. As a part of this study, we have configured an IoT server that acquires data from the sensors, and processes and displays data over the user interface (UI).
4.3. Pulse Oximeter and Heart Rate Sensor
The MAX30100 represents an integrated sensor solution designed for measuring both pulse oximetry and heart rate. It is a comprehensive sensor solution that integrates two LEDs, optimized optics, a photodetector, and low-noise analog signal processing to effectively detect pulse oximetry and heart-rate signals. This sensor solution can operate with power supplies ranging from 1.8 V to 3.3 V and can be powered down with minimal standby current. This feature allows the power supply to remain connected at all times, ensuring continuous functionality of the sensor. Its applications involve fitness assistant devices, wearable devices, and medical monitoring devices. This sensor is designed to meet the demanding requirements by integrating pulse oximetry and heart rate measurement. Despite its small size, the MAX30100 provides excellent optical and electrical performance. A 16-deep FIFO buffer stores the digital output data of the MAX30100, which is fully configurable through software registers. In addition, the FIFO provides a means of connecting the MAX30100 to a microprocessor or microcontroller on a shared bus, allowing data to be read from the registers of the device in a continuous manner. Several technologies are integrated into the SpO2 subsystem of the MAX30100, including ambient light cancellation (ALC), 16-bit sigma delta ADC, and proprietary discrete time filtering. An oversampling sigma delta ADC with a resolution of 16 bits, the SpO2 ADC provides continuous time oversampling. There is a choice of 50Hz or 1kHz for the ADC output data rate. As part of the MAX30100, there is a proprietary discrete time filter that rejects interference at 50 Hz/60 Hz as well as low-frequency residual ambient noise [30].
The MAX30100 sensor incorporates an on-chip temperature sensor that may be utilized for calibrating the temperature dependence of the SpO2 subsystem (optionally). While the wavelength of the IR LED has relatively little effect on the SpO2 algorithm, the wavelength of the red LED is critical to the correct interpretation of the data. As the ambient temperature changes, it is possible to compensate for the SpO2 error using the temperature sensor data. It also integrates red and infrared LED drivers for the generation of LED pulses in order to measure SpO2 and heart rate (HR). With the proper supply voltage, the LED current can be programmed between 0 mA and 50 mA. To optimize measurement accuracy and power consumption, the LED pulse width can be programmed between 200 s and 1.6 ms. A more detailed description of MAX30100 can be found at [30]. During the course of this study, the authors make use of Max30100 to acquire data regarding pulse oximetry and HR based on a number of characteristics and advantages such as integrated light cancellation for measurement accuracy, fast data output, high sampling rate, integrated LED, photosensor, and low power consumption.
4.4. Temperature, Humidity Sensors, and GPS Module
The temperature and humidity sensor DHT11 boasts a temperature and humidity sensor combination with a calibrated digital signal output. It offers excellent long-term stability and reliability through its exclusive digital-signal-acquisition technology and temperature and humidity sensing. An NTC temperature sensor as well as a resistive type of humidity sensor are included in this sensor, which is connected to a high-performance 8-bit microcontroller and offers excellent performance, speed, and anti-interference capabilities. It is imperative that each DHT11 element is strictly calibrated in the laboratory so that humidity calibration can be performed with the highest level of accuracy. In the OTP memory, calibration coefficients are stored as programs which are used by the sensor’s internal signal detection mechanism. Simple and easy system integration is made possible by the single-wire serial interface. Due to its small size, low power consumption, and up to 20 m signal transmission, it is an ideal solution for a wide range of applications, including those in high demand. A 4-pin single row pin package is used for this component. We have selected DHT11 sensors for the course of this study on the basis of their compatibility with the microcontroller and accuracy, which is ±5% for relative humidity and ±2 °C for temperature. Moreover, this sensor consumes a minimal amount of power, consuming a maximum average of 1mA and sample every one second [31].
Additionally, this study utilizes a BN-220GPS module with an antenna that has 72 channels for searching. Using a Chipset u-bloxM8030-KT, the device supports GPSL1, GLONASSL1, BeiDouB1, SBASL1, and GalileoE1 frequencies. It is a 22 mm × 20 mm × 6 mm module with a voltage range of 3.0 V–5.5 V DC and an operating current range of 50 mA at 5.0 V. The operating temperature ranges from −40 °C to +85 °C. In addition to its compatibility with the microcontroller, accuracy, and low power consumption, this module has also been considered appropriate for this study [32]. This is used to provide the patient’s GPS location.
To bring together the TCP/IP wireless network connectivity and the internet protocol for data visualization and transfer between sensors and server, the Tenda Router (N304 V2) and 2.4 GHz operating frequency band were used. The device complies with IEEE 802.11n standards. Aside from supporting TCP/IP and IEEE 802.11b/g/n Wi-Fi standards, the ESP32 microcontroller used in this research also implements an internet protocol and allows for the establishment of a private network. As part of network security, firewall protection is enabled in addition to the Service Set Identifier and password.
5. Prototype Design
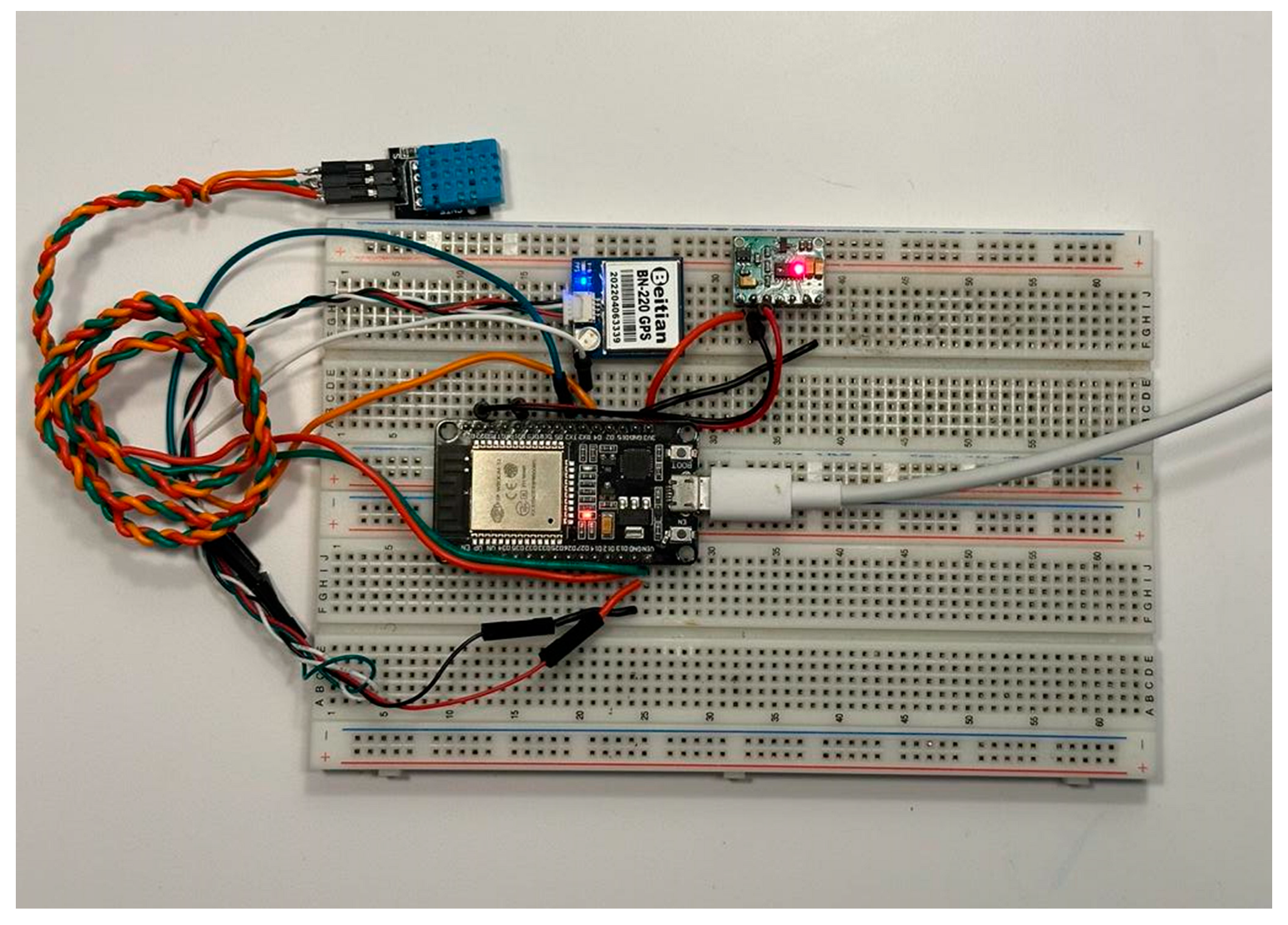
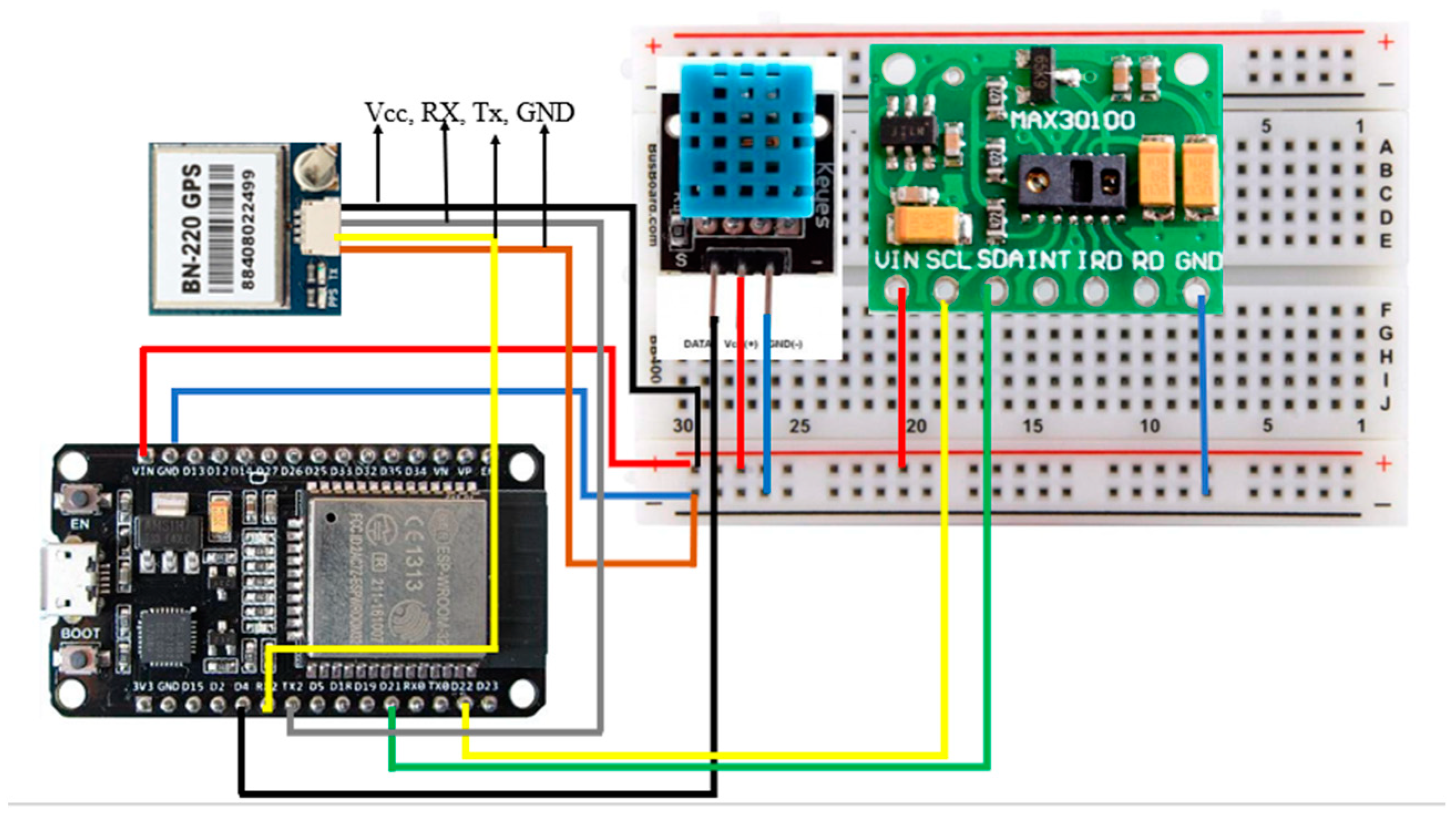
Our objective in this section is to describe the hardware implementation of the proposed open-source Internet-of-Things-based health monitoring system. Figure 2 outlines an ESP32 microcontroller assembled on a Breadboard. The Max30100, temperature, and humidity sensor, and the GPS module are connected to the microcontroller through the jumper wires. In this prototype, circuit design sensors are powered directly by 3.3 volts of ESP32, while ESP32 is powered using +5 V from USB cable. The ESP32 chip is also used here to set up an IoT server for the purpose of data acquisition and visualization. Through the IoT server, both the user and the physician are able to monitor the health status. This also helps the user to create an emergency alert during any critical situation. The sensor data are acquired using the pins of the microcontroller and can be visualized from the internet protocol address. To create a private communication channel, a Wi-Fi router is used as a part of this study. Figure 3 demonstrates the wiring diagram of the proposed system.
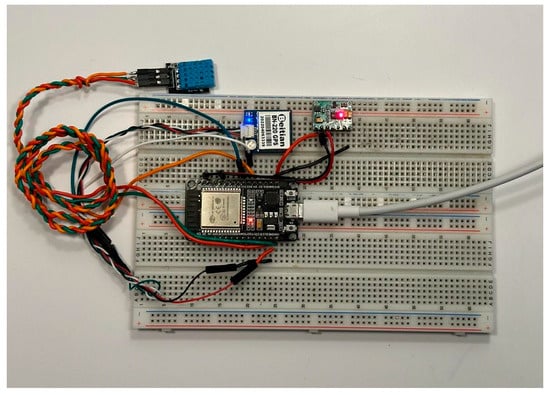
Figure 2.
Hardware implementation of the proposed system.
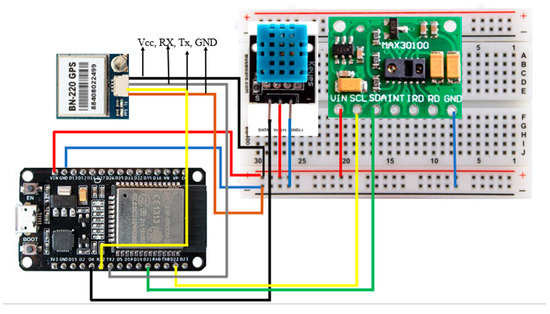
Figure 3.
Wiring diagram of proposed system.
6. Experimental Setup of the Proposed Health Monitoring System
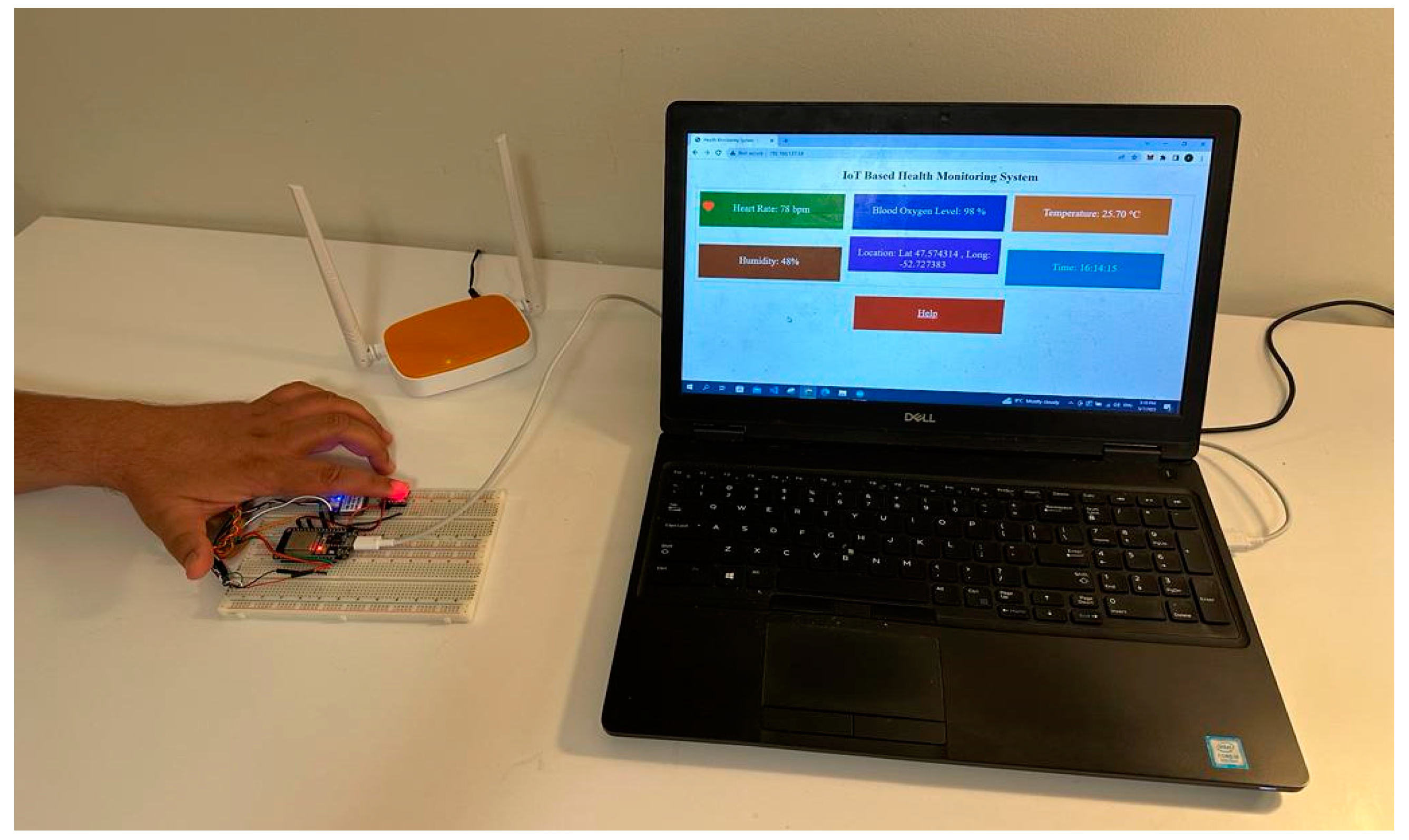
As a preliminary step before their use, the hardware components described in Section 4 were programmed and configured based on their principles of operation. Figure 4 demonstrates a complete experimental set up for the proposed open-source health monitoring system. The experimental setup includes a Wi-Fi router, a temperature and humidity sensor, a GPS module, blood oxygen level and HR sensor, and an ESP32 microcontroller chip fit together on a Breadboard and an HMI. Through the course of this study, the ESP32 microcontroller acts as the main server of the proposed health monitoring system over which the IoT server is set up. The IoT server facilitates the collection and visualization of the data by the users. The set up also involves the use of DHT 11, a temperature and humidity sensor that is utilized here to measure underarm human body temperature, ambient temperature, and humidity levels. Likewise, the purpose of MAX30100 is to gauge the HR and blood oxygen levels. To add to this, a GPS and a Wi-Fi router are part of the proposed system’s experimental setup. The GPS helps in tracking the precise location of the user to reach them in case of emergency and, on the other hand, the Wi-Fi router is used to create a private communication channel over which the proposed system is hosted.
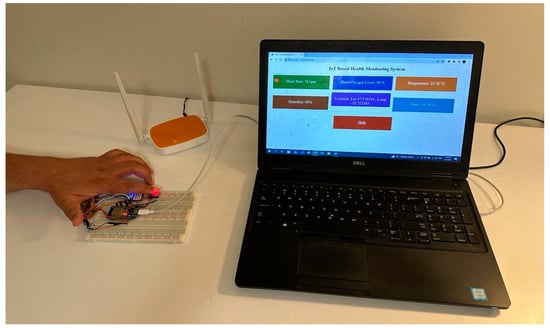
Figure 4.
Experimental setup.
7. Implementation Methodology
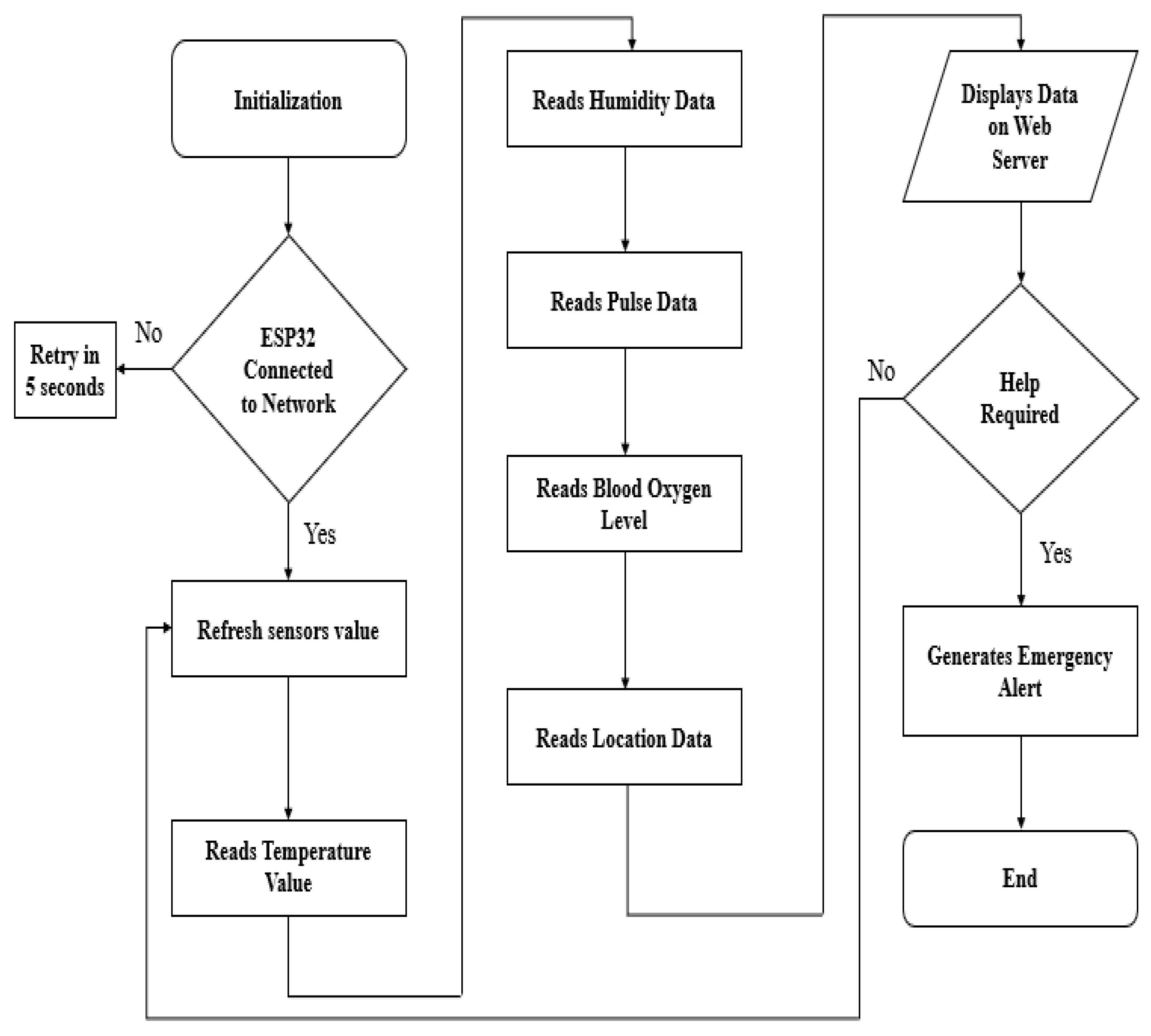
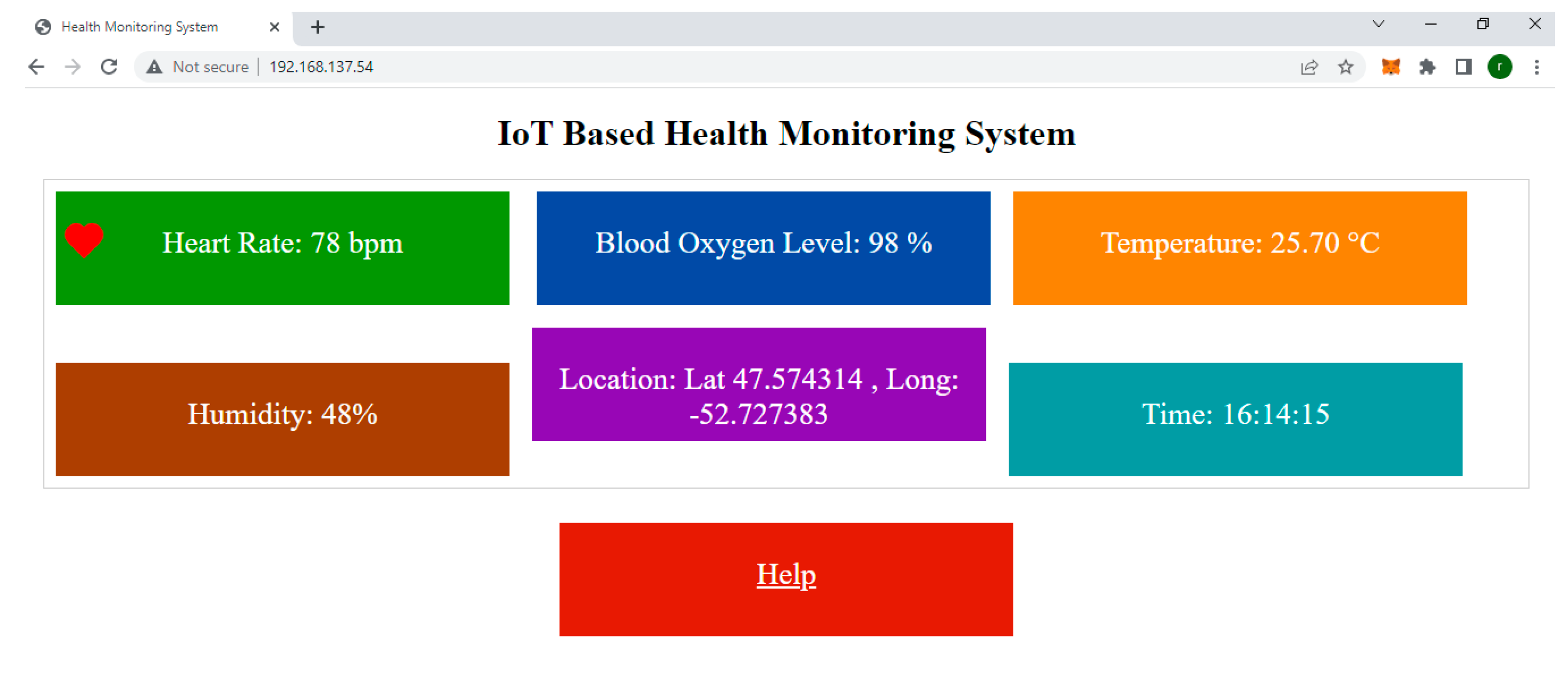
This section of the article illustrates the implementation of the proposed open-source health monitoring system. The proposed study employs the ESP32 microcontroller to set up a local IoT server and obtain data through a GPS module, a temperature and humidity sensor, and a blood oxygen level and HR sensor. The data measurements and collection are carried out with the aid of the Arduino Integrated Development Environment (IDE) programs compiled and uploaded into the ESP32 microcontroller. A private communication network enables the ESP32 to further transmit this data to a local IoT server, accessible through an internet protocol (IP) address. In Algorithm 1, a pseudocode is provided for the implementation methodology and [33,34,35,36] provide the source codes used for this study. According to Algorithm 1, steps 1 to 8 depict the connection process of the ESP32 chip to the private communication network and display the connection status in Arduino IDE serial monitor. Step 10 of Algorithm 1, ESP32, displays the internet protocol address in the Arduino IDE serial monitor, while step 11 is used to refresh the sensor values. In steps 12 to 15, ESP32 reads the sensor data from the connected sensors.
On the other hand, steps 16 to 18 illustrate the data transfer process over an IP address. If the user needs any help, they are able to generate help notifications as well. This process is explained in steps 21 and 22 of the pseudocode. A new process begins upon disconnecting, as illustrated in lines 23 and 24. This system can also be connected to the internet using port forwarding technique. The user can access the server using an IP address on HMIs.
| Algorithm 1 Health monitoring | |
| Initialization: | |
| 1. | While ESP32 is not connected to private network: |
| 2. | Set up ESP32 connection by passing, SSID, and password over private network |
| 3. | End |
| 4. | If ESP32-S3 connection established with local-Wi-Fi |
| 5. | Display “Connected” on Arduino IDE Serial Monitor |
| 6. | Else |
| 7. | Display “Connection failed… retry in 5 s” on Arduino IDE Serial Monitor |
| 8. | Exit |
| 9. | End if |
| 10. | Display IP address on Arduino IDE Serial Monitor |
| 11. | Refresh sensor value |
| 12. | ESP32 reads temperature and humidity data |
| 13. | ESP32 reads pulse rate |
| 14. | ESP32 reads SPO2 value |
| 15. | ESP32 reads location data |
| 16. | ESP32 listens to local IP address |
| 17. | If HTTP request received from a web browser: |
| 18. | respond with HTML/CSS data with sensor values |
| 19. | End if |
| 20. | Update data |
| 21. | If help is required |
| 22. | ESP32 sends notification on web browser |
| 23. | End if |
| 24. | Go to Step 11 |
| end | |
Amongst the key characteristics of the algorithm is that it comprises all the required libraries, including the sensors and Wi-Fi. For data acquisition and transmission to the ESP32 microcontroller, a one-wire protocol and I2C protocol are used. In order to display data over an internet protocol address, it uses the HTTP request response protocol. As part of the algorithm, the process of connecting and terminating is also explained. Figure 5 demonstrates a flowchart describing the complete system’s operation. Moreover, it provides a brief overview of the entire health monitoring process and system.
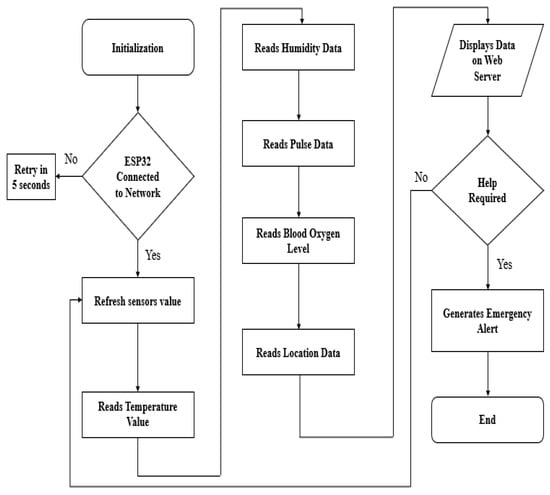
Figure 5.
Flow chart of the proposed system.
8. Results
By setting up the designed prototype to acquire important vital signs data, location data, and ambient temperature and humidity measurements via the dashboard, we have tested the proposed IoT-based open-source health monitoring system and present results in this section of the article. This study involved testing the designed system on five different volunteers who agreed to participate and made themselves available for the study, named here as test participant “A” to test participant “E”. An hours’ worth of measurements was taken. The available and agreed volunteers for this study ranged from 45 and 90 years of age (three male and two female); however, the system itself is not designed to accommodate a particular age group.
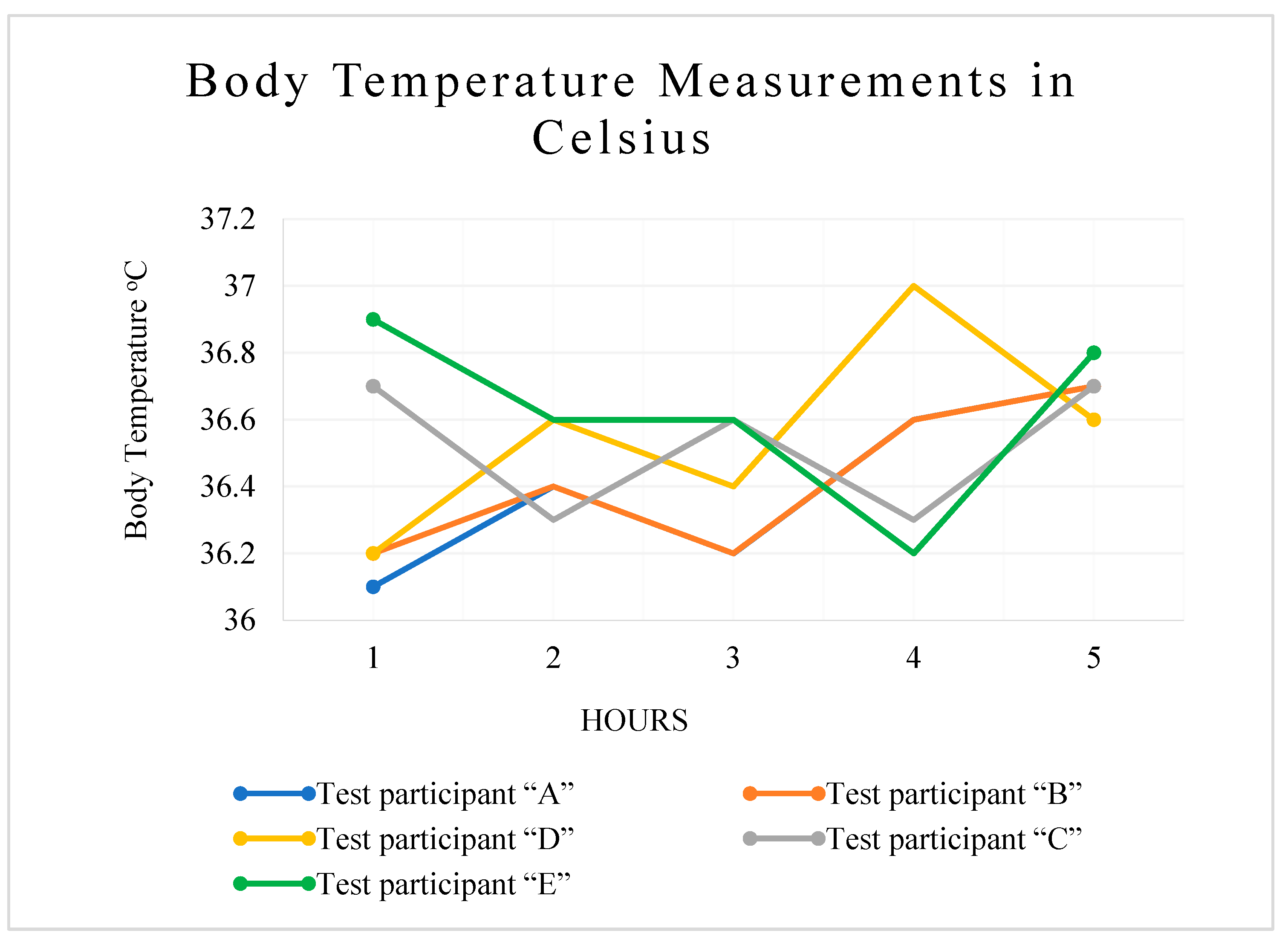
Table 2 depicts the results of body temperature measurements of test participant “A” to test participant “E” obtained using the DHT11 temperature and humidity sensor. During the scope of this study, we used the axillary method of human body temperature measurement. The recommended time for taking body temperature measurements by a DHT11 sensor, realized after taking the body temperature measurements and successfully testing the system, is 30 to 90 s. To ensure correct readings from the sensor, we cleaned the sensor properly before placing it in the axillary region, ensured there was no clothing between the body and the sensor, and placed the sensor in a proper position. To add to this, during the body temperature measurement procedure, the arm position was snug against the body. The body temperature measurements demonstrated in Table 2 and Figure 6 are considered as normal as they do not come under the definition of reportable illness according to the Centers for Disease Control and Prevention, USA [37].

Table 2.
Body temperature measurements in Celsius.
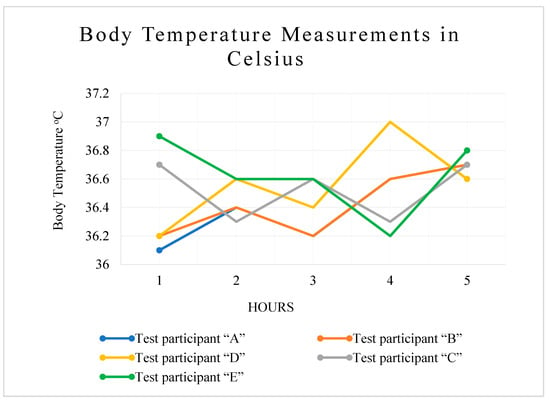
Figure 6.
Human body temperature in °C.
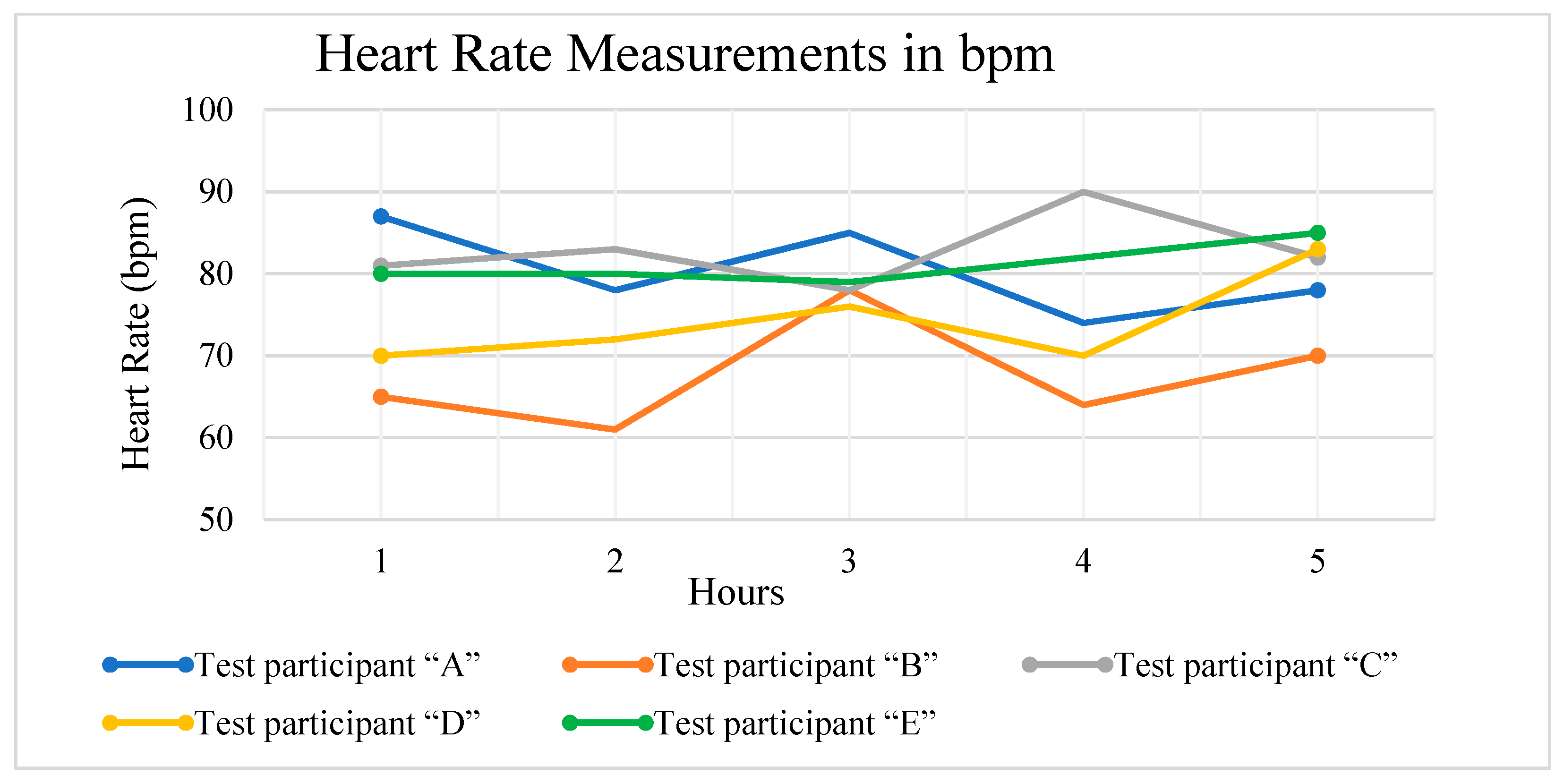
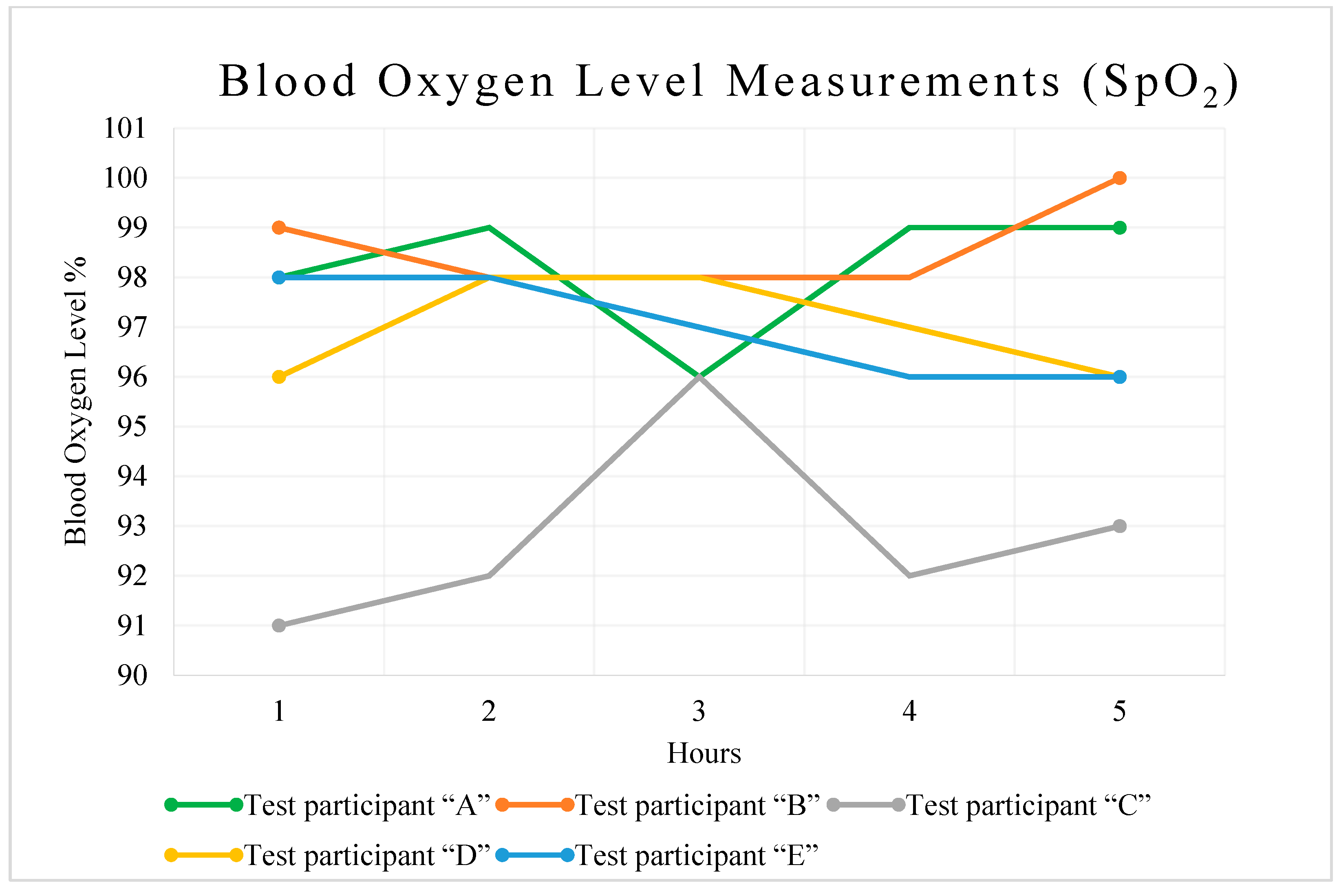
Through the course of this study, we have used Max30100 for the measurement of heart rate and blood oxygen levels. In Max30100, the sampling rate can be configured from 50 samples per second to 100 samples per second. This sensor involves high-intensity LEDs and a photodetector and works in two parts to measure HR and SpO2. As part of our efforts to measure accurate readings of HR and SpO2, we adhered to the manufacturer’s guidelines. Additionally, precautions such as cleaning the finger before positioning the sensor to avoid any grime that can influence the sensor readings and proper placement of the finger on the sensor were taken, and the results are presented in Table 3 and Table 4, and Figure 7 and Figure 8.

Table 3.
Heart rate measurements in bpm.

Table 4.
Blood oxygen level measurement (SpO2).
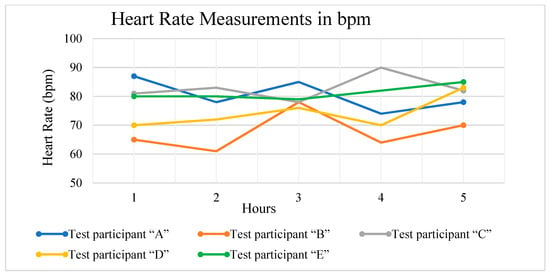
Figure 7.
Heartrate measurement in bpm.
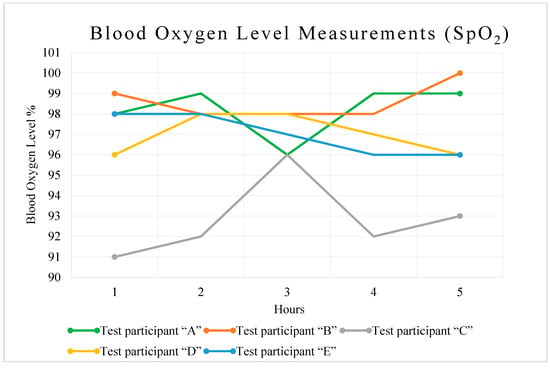
Figure 8.
Blood oxygen level line chart.
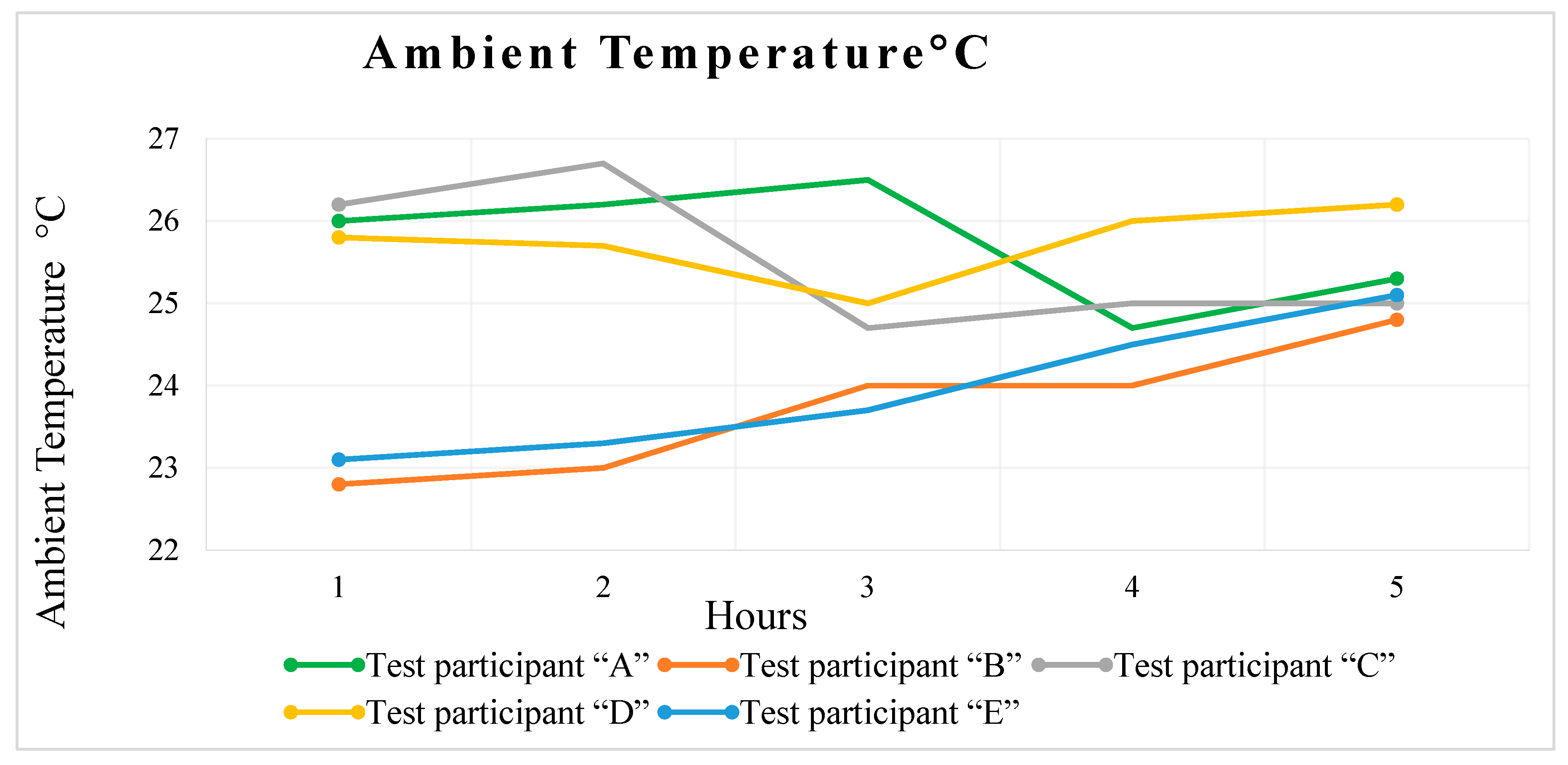
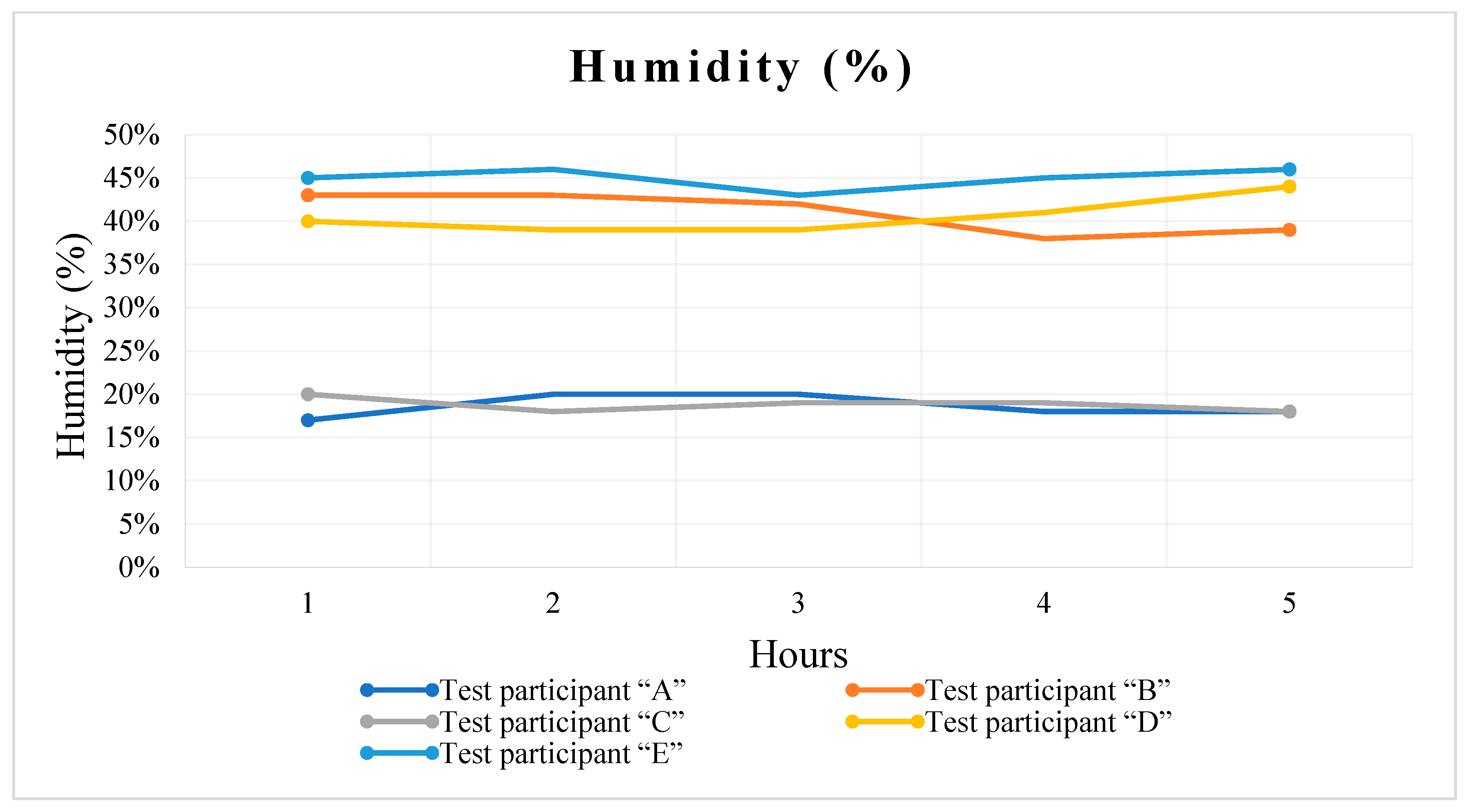
Two purposes have been served by the use of the DHT11 sensor in the scope of this study. In the first instance, we are using it to measure the temperature of the human body, the details of which are presented above in this section. In addition, it is being used to measure the room temperature and humidity data that can be helpful to asthmatic patients. When the humidity level is high, asthmatic symptoms are triggered. Patients with asthma can take necessary precautions and determine treatment plans by monitoring humidity levels. We present the results regarding the measurement of ambient temperature in Figure 9 and Table 5, while humidity measurements are shown in Table 6 and Figure 10. The IoT server status is presented in Figure 11.
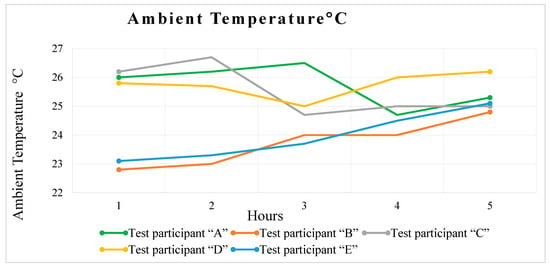
Figure 9.
Ambient temperature, °C.

Table 5.
Ambient temperature in Celsius.

Table 6.
Humidity data.
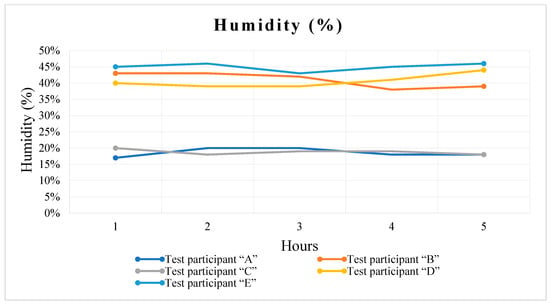
Figure 10.
Humidity data as line chart.
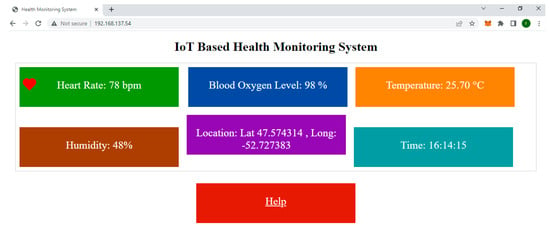
Figure 11.
System status on IoT server.
All hardware components were individually tested before being combined into a complete system setup according to some validation techniques suggested in [38]. This was accomplished by validating the source code of each component using the Arduino IDE and observing the results through an Arduino serial monitor. Following the integration of all of the components, the working of the components and the code were tested using the Arduino IDE and serial monitor. The complete system set up is also validated by comparing the values in the serial monitor with the values in the web-based user interface. Despite the fact that the system is hosted on a private network and is not susceptible to attacks, restricted authorization is enabled using an SSID and a password. Also, the system test results show that the average throughput calculation for the designed system is 17 × 105 bps and the memory usage is (93,752 bytes), which is 27.83% of the total memory.
9. Discussion
In this section, we describe briefly the key features of the IoT-based open-source remote health monitoring solution realized after successful testing of the proposed system.
Low power: In developing a health monitoring system specifically for remote locations, it is critical to consider the power consumption of each hardware component. Our system uses an ESP32 chip as its central server, which consumes 0.6 Watts. There is an overall power consumption of 1.4 Watts for the health monitoring system and 1.7 Watts for the Wi-Fi router. Each hardware component’s power consumption is monitored under operating conditions, and data sheets may be consulted for further information. Table 7 outlines the power consumption of each hardware component used within the scope of this study. Consequently, the designed system can be considered low power.

Table 7.
Power consumption of the system.
Low cost: A low-cost system design is achieved by utilizing readily available and low-cost hardware components. Additionally, the developed system uses open-source technology that eliminates operating costs. In Table 8, the price breakdown of each element used in the study can be obtained. The overall cost of the system is CAD 34.

Table 8.
Price breakdown of system components.
Remote Health Monitoring: The IoT-based remote health monitoring system demonstrated through the course of this article enables the timely detection of abnormal trends in health. Additionally, the UI facilitates physicians or other healthcare personnel to monitor real-time health data, such as vital signs, that can help in the management of chronic health conditions.
Access to healthcare: The designed health monitoring system provides immediate access to healthcare, particularly to the people living in remote areas lacking access to healthcare facilities. Healthcare systems such as these can decrease the cost of healthcare and lower the burden on hospitals by reducing medical procedures and prioritizing patients according to their medical needs. As an additional benefit, users can reduce frequent hospital visits, which results in both time and financial savings.
Security: To ensure users’ data security and integrity, the designed health monitoring systems are protected with a set of security controls such as a Service Set Identifier (SSID), password, and firewall. A further feature of this IoT server is that it is configured locally and is hosted on a local communication network. Therefore, it is not vulnerable to internet traffic.
A valuable guide for future study: The research will contribute significantly to the development of health monitoring and management solutions for underserved remote communities. It is evident that the research described above provides a solid foundation and justification for planning and designing health monitoring systems for remote areas that have no access to the internet.
Intuitive health monitoring system: The designed system aimed to have a user-friendly interface. It does not involve any special training or a dedicated operator to use the proposed system.
Coordination and self-care: Health monitoring systems such as these can enhance patients’ and doctors’ coordination by close monitoring.
Decrease healthcare disparities: The proposed research can bring down healthcare disparities by providing assistance to the elderly, populations in remote areas, the disabled, those who require regular health monitoring, and individuals with mobility constraints.
System limitations: The proposed system is not alert enabled. Considering that the system does not generate any alerts, there is no noticeable delay time at the receiver end, provided that the HMI(s) are not in sleep mode. Other limitations may include the range of the local network, which depends on the range of the router used.
10. Conclusions
Even though healthcare is a fundamental human right, it is unfortunate, however, that populations in developing countries are not able to access basic healthcare facilities. This is because of a lack of government resources, poor infrastructure, or inadequate distribution of resources. A particular focus of this paper is Pakistan, where 50% of the population has no access to medical care, and this percentage increases in rural and remote areas. To add to this, during the peak of COVID-19, healthcare was a challenge for all. Various measures of social distancing and protection were in place, and it became apparent to the world that technology is integral to the advancement of all facets of life. Therefore, an open-source, low-cost health monitoring system is a flexible and appropriate solution for remote and unserved communities.
In the scope of this study, we present the design and implementation of an IoT-based open-source and low-cost health monitoring system. The designed system measures three important vital signs: temperature, HR, and blood oxygen level. Additionally, it integrates distinctive features like measuring ambient temperature, humidity, and the location of the user. Furthermore, the system includes features that allow doctors and other healthcare professionals to be notified in the event of an emergency or need for assistance. An intuitive dashboard has been designed to visualize data over an internet protocol address. The IoT server processes data and transmits it over the IP. The overall set up is hosted on a private communication channel that makes it useful even for regions with no internet access. A power consumption measurement has been conducted under operating conditions, and it has been determined that the system consumes less than four watts of power and the system cost CAD$ 34, which is a fairly low cost for such critical solutions.
Although this study proposes an IoT-based health monitoring system for remote locations in Pakistan, there is a potential for this research to have a substantial impact on the implementation of remote health monitoring systems in other remote areas with limited resources.
11. Future Work
A future research direction will involve the enhancement of the system in order to provide facilities such as respiratory rate measurement and electronic cardiography. Increasing the range of private communication networks can also be part of the future research.
Author Contributions
S.A.: methodology, software and hardware implementation, data curation, writing—original draft. S.P.K. and M.T.I.: conceptualization, resources, supervision, funding acquisition, writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
All the data regarding this research has been provided in references.
Acknowledgments
This paper would like to express gratitude to the College of Home Economics, University of Peshawar and School of Graduate Studies, Memorial University of Newfoundland for providing the opportunities and conducive environment for this study.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| IoT | Internet-of-Things |
| HR | Heart rate |
| GPS | Global Positioning System |
| HMI | Human Machine Interface |
| IP | Internet protocol |
| RPM | Remote Patient Monitoring |
| ECG | Electrocardiogram |
| SPI | Serial Peripheral Interfaces |
| UI | User Interface |
| IDE | Integrated Development Environment |
| SSID | Service Set Identifier |
References
- United Nations. UN News. Available online: https://news.un.org/en/story/2023/05/1136367 (accessed on 26 May 2023).
- Golinelli, D.; Boetto, E.; Carullo, G.; Nuzzolese, A.G.; Landini, M.P.; Fantini, M.P. Adoption of Digital Technologies in Health Care during the COVID-19 Pandemic: Systematic Review of Early Scientific Literature. J. Med. Internet Res. 2020, 22, e22280. [Google Scholar] [CrossRef] [PubMed]
- IMF BLOG. COVID-19: Without Help, Low-Income Developing Countries Risk a Lost Decade. Available online: https://www.imf.org/en/Blogs/Articles/2020/08/27/blog-covid-19-without-help-low-income-developing-countries-risk-a-lost-decade (accessed on 6 June 2023).
- Memon Medical Institute Hospital. Access to Primary Healthcare in Pakistan. Available online: https://mmi.edu.pk/blog/access-to-primary-health-care-in-pakistan/ (accessed on 16 May 2023).
- The World Bank. Rural Population (% of Total Population)-Pakistan. Available online: https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS?locations=PK (accessed on 21 April 2023).
- Kurji, Z.; Premani, Z.S.; Mithani, Y. Analysis of The Health Care System of Pakistan: Lessons Learnt and Way Forward. J. Ayub. Med. Coll. Abbottabad. 2016, 28, 601–604. [Google Scholar] [PubMed]
- Usman, A.; Baig, A.; Amjad, A.; Amjad, U. Reformative Measures for Basic Health Units in Pakistan. Iran J. Public Health 2015, 44, 1158–1159. [Google Scholar] [PubMed]
- Khan, M.M.; Alanazi, T.M.; Albraikan, A.A.; Almalki, F.A. IoT-Based Health Monitoring System Development and Analysis. Secur. Commun. Netw. 2022, 2022, 9639195. [Google Scholar] [CrossRef]
- Rafa, N.S.; Azmal, B.B.; Dhruba, A.R.; Khan, M.M.; Alanazi, T.M.; Almalki, F.A.; AlOmeir, O. IoT-Based Remote Health Monitoring System Employing Smart Sensors for Asthma Patients during COVID-19 Pandemic. Wirel. Commun. Mob. Comput. 2022, 2022, 6870358. [Google Scholar] [CrossRef]
- Babar, E.T.R.; Rahman, M.U. A Smart, Low Cost, Wearable Technology for Remote Patient Monitoring. IEEE Sens. J. 2021, 21, 21947–21955. [Google Scholar] [CrossRef]
- Islam, M.M.; Rahaman, A.; Islam, M.R. Development of Smart Healthcare Monitoring System in IoT Environment. SN Comput. Sci. 2020, 1, 185. [Google Scholar] [CrossRef] [PubMed]
- Hadis, N.S.M.; Amirnazarullah, M.N.; Jafri, M.M.; Abdullah, S. IoT Based Patient Monitoring System using Sensors to Detect, Analyse and Monitor Two Primary Vital Signs. J. Phys. Conf. Ser. 2020, 1535, 12004. [Google Scholar] [CrossRef]
- Al Bassam, N.; Hussain, S.A.; Al Qaraghuli, A.; Khan, J.; Sumesh, E.P.; Lavanya, V. IoT based wearable device to monitor the signs of quarantined remote patients of COVID-19. Inform. Med. Unlocked 2021, 24, 100588. [Google Scholar] [CrossRef] [PubMed]
- Hameed, K.; Bajwa, I.S.; Ramzan, S.; Anwar, W.; Khan, A. An Intelligent IoT Based Healthcare System Using Fuzzy Neural Networks. Sci. Program. 2020, 2020, 8836927. [Google Scholar] [CrossRef]
- Chen, Z.; Khan, S.; Abbas, M.; Nazir, S.; Ullah, K. Enhancing Healthcare through Detection and Prevention of COVID-19 Using Internet of Things and Mobile Application. Mob. Inf. Syst. 2021, 2021, 5291685. [Google Scholar] [CrossRef]
- Anan, S.R.; Hossain, M.A.; Milky, M.Z.; Khan, M.M.; Masud, M.; Aljahdali, S. Research and Development of an IoT-Based Remote Asthma Patient Monitoring System. J. Healthc. Eng. 2021, 2021, 2192913. [Google Scholar] [CrossRef] [PubMed]
- Krichen, M. A Survey on Formal Verification and Validation Techniques for Internet of Things. Appl. Sci. 2023, 13, 8122. [Google Scholar] [CrossRef]
- Alsharif, M.H.; Alsharif, Y.H.; Chaudhry, S.A.; Albreem, M.A.; Jahid, A.; Hwang, E. Artificial intelligence technology for diagnosing COVID-19 cases: A review of substantial issues. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9226–9233. [Google Scholar] [CrossRef] [PubMed]
- Alsharif, M.H.; Alsharif, Y.H.; Yahya, K.; Alomari, O.A.; Albreem, M.A.; Jahid, A. Deep learning applications to combat the dissemination of COVID-19 disease: A review. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 11455–11460. [Google Scholar] [CrossRef] [PubMed]
- Thakur, N.; Han, C.Y. An Intelligent Ubiquitous Activity Aware Framework for Smart Home. In Human Interaction, Emerging Technologies and Future Applications III; Springer: Cham, Switzerland, 2021; pp. 296–302. [Google Scholar]
- Wang, J.; Cheng, H. Human Posture Recognition Based On Convolutional Neural Network. In Proceedings of the 2020 4th International Conference on Electronic Information Technology and Computer Engineering, Xiamen, China, 6–8 November 2020; pp. 475–480. [Google Scholar] [CrossRef]
- Baig, M.J.A.; Iqbal, M.T.; Jamil, M.; Khan, J. A Low-Cost, Open-Source Peer-to-Peer Energy Trading System for a Remote Community Using the Internet-of-Things, Blockchain, and Hypertext Transfer Protocol. Energies 2022, 15, 4862. [Google Scholar] [CrossRef]
- ESP32-Datasheet. Available online: https://www.espressif.com/sites/default/files/documentation/esp32-wroom-32_datasheet_en.pdf (accessed on 1 June 2023).
- Biswas, S.B.; Iqbal, M.T. Solar Water Pumping System Control Using a Low Cost ESP32 Microcontroller. In Proceedings of the 2018 IEEE Canadian Conference on Electrical & Computer Engineering (CCECE), Quebec, QC, Canada, 13–16 May 2018; pp. 1–5. [Google Scholar] [CrossRef]
- Dataversity. Data Topics. A Brief History of Internet of Things. Available online: https://www.dataversity.net/brief-history-internet-things/# (accessed on 6 June 2023).
- Darshan, K.R.; Anandakumar, K.R. A comprehensive review on usage of Internet of Things (IoT) in healthcare system. In Proceedings of the 2015 International Conference on Emerging Research in Electronics, Computer Science and Technology (ICERECT), Mandya, India, 17–19 December 2015; pp. 132–136. [Google Scholar] [CrossRef]
- Sethi, P.; Sarangi, S.R. Internet of Things: Architectures, Protocols, and Applications. J. Electr. Comput. Eng. 2017, 2017, 9324035. [Google Scholar] [CrossRef]
- Shammar, E.A.; Zahary, A.T. The Internet of Things (IoT): A survey of techniques, operating systems, and trends. Libr. Hi Tech 2020, 38, 5–66. [Google Scholar] [CrossRef]
- Krishnamoorthy, S.; Dua, A.; Gupta, S. Role of emerging technologies in future IoT-driven Healthcare 4.0 technologies: A survey, current challenges and future directions. J. Ambient. Intell. Hum. Comput. 2023, 14, 361–407. [Google Scholar] [CrossRef]
- Max30100. Pulse Oximeter and Heart-Rate Sensor IC. Available online: https://www.analog.com/media/en/technical-documentation/data-sheets/max30100.pdf (accessed on 6 June 2023).
- DHT11Humidity and Temperature Sensor. Available online: https://www.mouser.com/datasheet/2/758/DHT11-Technical-Data-Sheet-Translated-Version-1143054.pdf (accessed on 11 May 2023).
- BN-220 GPS Module + Antenna DataSheet. Available online: http://files.banggood.com/2016/11/BN-220%20GPS+Antenna%20datasheet.pdf (accessed on 11 May 2023).
- ESP32-DHT-Webserver. Available online: https://github.com/Enjoy-Mechatronics/ESP32-DHT-Webserver/blob/main/ESP32-DHT-Webserver.ino (accessed on 30 April 2023).
- Arduino-Max30100. Available online: https://github.com/oxullo/Arduino-MAX30100 (accessed on 13 April 2023).
- TinyGPSPlus. Available online: https://github.com/mikalhart/TinyGPSPlus (accessed on 11 April 2023).
- Time. Available online: https://github.com/PaulStoffregen/Time (accessed on 11 April 2023).
- Centers for Disease Control and Prevention. Definition of Symptoms for Reportable Illnesses. Available online: https://www.cdc.gov/quarantine/air/reporting-deaths-illness/definitions-symptoms-reportable-illnesses.html (accessed on 3 June 2023).
- Mekruksavanich, S.; Jitpattanakul, A. LSTM Networks Using Smartphone Data for Sensor-Based Human Activity Recognition in Smart Homes. Sensors 2021, 21, 1636. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).