Abstract
Objective: The aim of this systematic review was to evaluate the effectiveness and safety of various laser systems for debonding ceramic orthodontic brackets compared to conventional mechanical removal methods. The primary outcomes assessed included enamel damage, pulp temperature changes, adhesive remnant index (ARI), and shear bond strength (SBS). Materials and Methods: A systematic search was conducted in November 2024 across the PubMed, Scopus, and Web of Science (WoS) databases following PRISMA guidelines. The initial search yielded 453 records, of which 41 studies met the inclusion criteria for qualitative and quantitative analysis. The risk of bias was assessed using a standardized scoring system, and only studies with accessible full texts were included. Results: The review highlighted significant heterogeneity in laser parameters, measurement protocols, and study methodologies. Among the evaluated lasers, CO2 and Er:YAG were the most frequently studied and demonstrated high efficacy in debonding ceramic brackets while maintaining enamel integrity. Sixteen studies assessing SBS reported a reduction from baseline values of 13–23 MPa to clinically acceptable ranges of 7–12 MPa following laser application. ARI was analyzed in 25 studies, with laser-treated groups exhibiting higher scores (2–3), indicating safer debonding with more adhesive remaining on the tooth surface, thereby reducing enamel damage. Pulpal temperature increases were examined in 23 studies, revealing that most laser types, when used within optimal parameters, did not exceed the 5.5 °C threshold considered safe for pulpal health. However, diode and Tm:YAP lasers showed potential risks of overheating in some studies. Conclusions: Laser-assisted debonding of ceramic orthodontic brackets is an effective and safe technique when applied with appropriate laser parameters. CO2 and Er:YAG lasers were the most effective in reducing SBS while preserving enamel integrity. However, variations in laser settings, study methodologies, and the predominance of in vitro studies limit the ability to establish standardized clinical guidelines. Further randomized controlled trials (RCTs) are necessary to develop evidence-based protocols for safe and efficient laser-assisted bracket removal in orthodontic practice.
1. Introduction
The utilization of ceramic brackets in orthodontic treatment has gained significant popularity due to their superior esthetics and biocompatibility [1]. The bracket system serves as the foundation of fixed orthodontic therapy, with ceramic brackets becoming an increasingly preferred choice among clinicians. Bonding these brackets to teeth necessitates a precise procedure involving composite resin materials, following the conditioning of the enamel surface through acid etching and the application of specific adhesive systems. These brackets are engineered to remain bonded throughout the entire orthodontic treatment, typically lasting two to three years. However, the debonding of these brackets presents a critical clinical challenge. Ceramic brackets exhibit higher bond strength compared to metal brackets and are additionally more brittle and susceptible to fracture, thereby increasing the risk of enamel damage during their removal [2,3].
Over the years, several methods have been developed for the debonding of ceramic brackets, including mechanical debonding (using specialized pliers), electrothermal debonding, chemical debonding, and ultrasonic debonding [2,4,5,6]. Currently, mechanical debonding is the most commonly employed technique, wherein brackets are typically removed using specialized pliers [4]. Despite its widespread use, this conventional approach raises several clinical concerns related to both efficiency and safety. Studies have reported varying degrees of enamel damage during the mechanical debonding process [2,7]. A significant challenge in debonding is managing adhesive residues that remain on the tooth surface after bracket removal. The mechanical removal of these residues often necessitates the use of rotating instruments, which can compromise the integrity of the enamel structure [7,8,9]. Additionally, patients may experience pain and discomfort when ceramic brackets are removed using mechanical methods [10]. Ultrasonic debonding presents an alternative approach, as it reduces the adhesive bond strength of the brackets, thereby enhancing the safety of the procedure. However, this method generally requires a longer procedure time, which may be inconvenient for patients [4,5]. Chemical debonding has also been explored; however, it does not significantly reduce shear bond strength (SBS) [3]. Electrothermal debonding has been investigated as another alternative, demonstrating safety by significantly lowering SBS levels without causing damage to the enamel or pulp [6].
In response to these challenges, researchers are investigating novel debonding methods, with laser technology emerging as a promising alternative for bracket removal. Current studies focus on identifying optimal laser parameters that can effectively debond brackets while minimizing potential damage to the enamel surface. Various laser systems and settings are being evaluated to establish the most efficient and safe protocols for ceramic bracket removal [11]. Laser energy facilitates the removal of adhesive resin from the tooth surface through three primary mechanisms: thermal softening, thermal ablation, and photoablation [2]. Specifically, laser technology provides an effective method for orthodontic bracket removal through its thermal softening mechanism [12]. The laser energy is converted into heat, causing the adhesive material to soften and weaken, thereby allowing the bracket to be naturally released from the tooth surface [2,13,14,15,16] (see Figure 1).
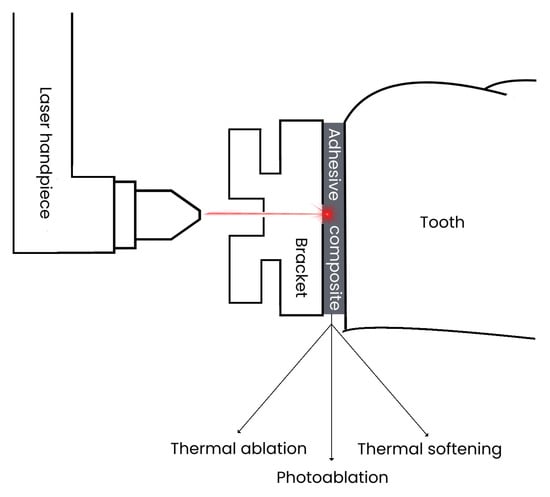
Figure 1.
Concept describing the mechanism of debonding using lasers.
The effective removal of orthodontic brackets using lasers necessitates the maintenance of several critical factors, including the preservation of enamel integrity, thermal regulation within physiological limits, and the minimization of residual adhesive material, as assessed by the adhesive remnant index (ARI) [2,17,18,19,20]. Despite its effectiveness, laser debonding presents limitations related to heat generation within the tooth structure. An increase in temperature of 5.5 °C can cause irreversible damage to the pulp tissue [2,21,22,23]. Furthermore, a temperature rise of 6 °C may damage the periodontal ligament [24], and an increase of up to 10 °C can result in bone damage [25,26]. Therefore, precise calibration of laser parameters—such as wavelength, power output, and exposure duration—is essential for achieving optimal bracket removal while safeguarding both the enamel surface and the deeper dental tissues from potential thermal or structural damage [2,27].
The aim of this systematic review is to evaluate the effectiveness of different laser wavelengths in debonding orthodontic ceramic brackets compared to traditional methods, with particular emphasis on identifying parameters that minimize enamel damage while maintaining clinical efficiency. Upon analyzing relevant studies on the use of lasers for ceramic bracket debonding, it became evident that the absence of a comprehensive systematic review in this area represents a significant opportunity to consolidate existing evidence. This review seeks to provide clinicians with evidence-based recommendations for the implementation of laser-assisted debonding techniques.
2. Materials and Methods
2.1. Focused Question
The systematic review followed the PICO framework [28] as follows: In the case of orthodontic ceramic bracket debonding (population), will the use of lasers (investigated condition) be more effective (outcome) in comparison to conventional methods (comparison condition)?
2.2. Protocol
The selection process for the articles included in the systematic review was carefully outlined following the PRISMA flow diagram [29] (see Figure 2). The systematic review was registered on the Open Science Framework under the following link: https://osf.io/sh2xw/ (accessed on 18 February 2025).
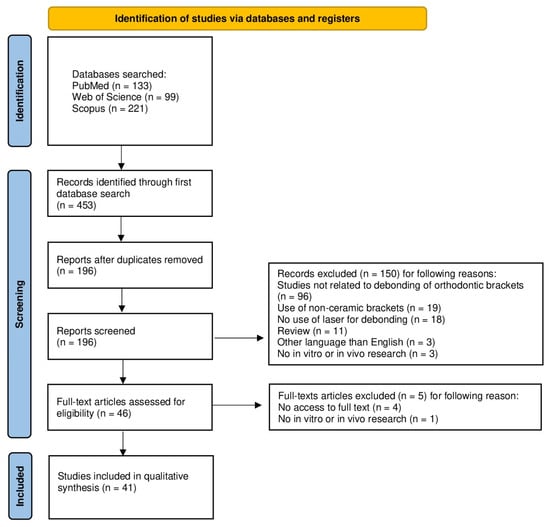
Figure 2.
The PRISMA 2020 flow diagram.
2.3. Eligibility Criteria
The researchers agreed to include only the articles that met the following criteria [30,31,32,33,34,35,36,37]:
- •
- Laser debonding;
- •
- Use of ceramic brackets;
- •
- Use of all types of lasers;
- •
- In vitro and in vivo studies;
- •
- Studies published in English;
- •
- Full-text availability.
The exclusion criteria the reviewers agreed upon were as follows [30,31,32,33,34,35,36,37]:
- •
- Use of metal brackets;
- •
- Use of forceps or ultrasound to debond brackets;
- •
- Review articles;
- •
- Duplicated publications.
No restrictions were applied with regard to the year of publication.
2.4. Information Sources, Search Strategy, and Study Selection
In November 2024, the PubMed, Scopus, and Web of Science (WoS) databases were searched for articles that met the specified inclusion criteria. To identify studies on laser debonding of ceramic orthodontic brackets, the search was refined using specific keywords. For PubMed, we used (orthodontic [Title/Abstract]) AND (brackets [Title/Abstract]) AND (laser [Title/Abstract]) AND (removal [Title/Abstract]); (orthodontic [Title/Abstract]) AND (brackets [Title/Abstract]) AND (laser [Title/Abstract]) AND (debonding [Title/Abstract]). For WoS, we used AB = (orthodontic AND brackets AND laser AND removal); AB = (orthodontic AND brackets AND laser AND debonding). For Scopus, we used TITLE-ABS-KEY (orthodontic) AND TITLE-ABS-KEY (brackets) AND TITLE-ABS-KEY (laser) AND TITLE-ABS-KEY (removal); TITLE-ABS-KEY (orthodontic) AND TITLE-ABS-KEY (brackets) AND TITLE-ABS-KEY (laser) AND TITLE-ABS-KEY (debonding). All searches adhered to the predefined eligibility criteria and only articles with accessible full-text versions were included.
2.5. Data Collection and Data Items
Five reviewers (J.K., A.K., K.W., M.M. and S.K.) meticulously selected the articles that met the inclusion criteria. The extracted data were then entered into a standardized Excel file.
2.6. Assessing Risk of Bias in Individual Studies
In the preliminary phase of study selection, the authors independently reviewed the titles and abstracts of each study to minimize the risk of reviewer bias. They assessed the level of agreement among reviewers using Cohen’s κ test [38]. Any disagreements regarding the inclusion or exclusion of studies were resolved through discussion.
2.7. Quality Assessment
Two independent evaluators (J.M. and M.D.) assessed the procedural quality of each study included in the analysis. The evaluation criteria encompassed randomization, a minimum group size of 10 samples, the presence of a control group, sample size calculation, and a detailed description of laser parameters and the debonding protocol. Studies were scored on a scale of 0 to 6 points, with higher scores indicating better study quality. The risk of bias was classified as follows: 0–2 points indicated a high risk, 3–4 points a moderate risk, and 5–6 points a low risk. Any discrepancies in scoring were resolved through discussion until a consensus was reached [30,31,32,33,34,35,36,37].
3. Results
3.1. Study Selection
The initial search of the electronic databases yielded 453 records. After removing 257 duplicates, 196 unique records remained for abstract screening. During this phase, 150 articles were excluded for the following reasons: 96 studies were unrelated to the debonding of orthodontic brackets, 19 used brackets made of materials other than ceramic, 18 did not utilize lasers for debonding, 11 were review articles, 3 were published in languages other than English, and 3 did not involve in vitro or in vivo research. This left 46 articles for full-text review. Of these, five were excluded: one was a theoretical study without in vitro or in vivo research, and access to four publications was unavailable. Consequently, 41 articles were selected for both qualitative and quantitative analyses (see Figure 2).
3.2. General Characteristics of the Included Studies
The studies included in this systematic review exhibited heterogeneity in the types of lasers used for debonding ceramic orthodontic brackets, the parameters assessed, and the outcomes related to enamel and pulp. The primary objective of most studies was to evaluate the efficacy of various lasers, including CO2 [39,40,41,42,43,44,45,46,47,48,49], Tm:YAP [50,51,52,53], Nd:YAG [12,44,54,55], Er:YAG [3,13,56,57,58,59,60,61,62,63,64,65,66,67,68], Er,Cr:YSGG [56,60,63,69,70], and diode lasers [3,53,71,72,73,74,75] with different wavelengths. The studies primarily focused on changes in pulp temperature [13,39,40,41,43,45,46,47,50,51,52,53,55,56,57,59,65,66,70,71,74,75,76], shear bond strength [3,39,40,42,43,47,48,49,50,54,55,60,62,63,66,67,68,73,75], and adhesive residues remaining after the procedure [3,13,39,40,41,42,43,44,47,48,49,54,60,61,62,64,65,66,67,68,69,70,72,73,74,75] (see Supplementary Table S1).
3.2.1. CO2 Laser Debonding
Among the authors who utilized the CO2 laser, all unanimously agreed that it is an effective and safe method for debonding ceramic brackets [39,40,41,42,43,44,45,46,47,48,49]. Additionally, three studies concluded that its use significantly reduces the risk of enamel surface damage [44,47,49]. Several researchers highlighted the importance of the adhesive material used [40,43,48]. Arima et al. [40] and Saito et al. [43] incorporated thermally expanded microcapsules into a conventional composite, and both concluded that this modification yields the best results for debonding with a CO2 laser. However, while Saito et al. [43] found no difference in the adhesive remnant index (ARI) value, Arima et al. [39], who tested different proportions, reported improved ARI results with a 25% microcapsule content. Mimura et al. [48] compared a material containing BIS-GMA resin to MMA resin without filler, finding significantly better results with the MMA resin. A decrease in shear bond strength (SBS) was observed only by Macri et al. [40].
3.2.2. Er:YAG (Erbium–Yttrium, Aluminum, Garnet) Laser Debonding
The use of the Er:YAG laser has also been shown to be effective, with authors consistently agreeing on its efficacy and safety for debonding ceramic brackets [3,13,56,57,58,59,60,61,62,63,64,65,66,67,68]. However, several researchers emphasize the importance of laser parameters, demonstrating consistent findings [57,64,65,67]. Hamadah et al. [64] identified a pulse duration of 100 to 300 milliseconds as optimal. Nalbantgil et al. [65], utilizing a pulse duration of 300 milliseconds, further recommended a power setting of 4 W, an exposure time of 6 s, and the use of a scanning mode for optimal results. Yilanci et al. [57], applying exposure times of 4–6 s, observed that while longer exposure increases temperature, it remains safe within this duration. Oztoprak et al. [67] confirmed that employing a scanning mode significantly reduces shear bond strength (SBS), facilitating safer debonding.
3.2.3. Diode Laser Debonding
The use of diode lasers for debonding has not received as much enthusiasm from researchers as CO2 or Er:YAG lasers. Four publications report positive outcomes, stating that diode lasers shorten working time and reduce the risk of enamel damage [71,72,73,74]. Notably, three of these studies used a laser with a 445 nm wavelength, with Steffen Stein as the lead author in each case [71,72,73]. Other studies, however, present varying results. Feldon et al. [75] observed a significant decrease in shear bond strength (SBS) only when using monocrystalline brackets. Nalbantgil et al. [65], who also studied monocrystalline brackets and compared different lasers, concluded that the Er:YAG laser is more effective and safer than the 980 nm diode laser. Dostalová et al. [53] found that the 808 nm diode laser could heat the tooth surface to as high as 114 °C without causing bracket detachment, raising concerns about potential thermal effects on dental tissues.
3.2.4. Er,Cr:YSGG (Erbium, Chromium–Yttrium, Scandium, Gallium, Garnet) Laser Debonding
Authors comparing different laser types concluded that the Er,Cr:YSGG laser is equally as effective and safe as the Er:YAG laser [56,60,63]. However, Hoteit et al. [63] cautioned that improper parameter settings for both lasers could lead to enamel damage, though they did not specify the power and exposure time used in their studies. Rao et al. [69] determined that power settings between 4.5 and 6 W are completely safe for debonding. Abdulaziz et al. [70], using a power setting of 4 W, observed that operating in scanning mode resulted in a smaller temperature increase, further enhancing the safety of the procedure.
3.2.5. Nd:YAG (Neodymium–Yttrium, Aluminum, Garnet) Laser Debonding
The Nd:YAG laser was used by only four researchers, yet all reached the same conclusion: it is a fast and painless method for the patient. Its application reduces both shear bond strength (SBS) and the adhesive remnant index (ARI) while minimizing the risk of enamel damage. Hayakawa et al. [55] investigated the debonding process using various types of adhesives and brackets. Their findings indicate that the Nd:YAG laser is effective regardless of the adhesive used, although monocrystalline brackets are more easily debonded.
3.2.6. Tm:YAP (Thulium–Yttrium, Aluminum, Perovskite) Laser Debonding
The use of the Tm:YAP laser warrants special attention due to the significant variation in its effects depending on the applied parameters. Dostalová et al. [52] studied its performance in 2011 at a power range of 1–2 W and found that irradiated brackets were removed with most of the adhesive, making it a useful tool for debonding. However, in a follow-up study in 2012, they observed that while shear bond strength (SBS) decreases at 1 W, using 4 W power leads to a significant increase in SBS [51]. Demirkan et al. [50] provided a detailed analysis of temperature changes associated with Tm:YAP laser use. They found that a safe temperature increase was achieved with 2.5–3 W power under the following conditions: 7 s at 3 W in scanning mode, 7 s at 2.5 W, and 10 s at 3 W in non-scanning mode. Dostalová et al. [53] further investigated the laser’s thermal effects and concluded that irradiation at 1–2 W for more than 60 s or without proper cooling can cause irreversible changes in the dental pulp.
3.3. Main Study Outcomes
The main outcomes evaluated in the studies included shear bond strength (SBS), assessed by 16 research groups [3,39,40,42,43,47,48,49,60,62,63,66,67,68,73,75]. Twenty-five studies assessed ARI, confirming that laser-assisted debonding shifts adhesive failure from the enamel–adhesive interface toward the bracket–adhesive interface, reducing enamel damage risk [3,13,39,40,41,42,43,44,48,49,55,60,61,62,64,65,66,67,68,69,70,72,73,74,75]. Temperature increase was evaluated in twenty-one studies, with all findings confirming that laser use remains within the 5.5 °C safety threshold, ensuring pulp vitality [13,39,40,41,43,45,46,47,48,50,51,52,56,57,59,65,66,70,71,74,76]. CO2 and Nd:YAG lasers exhibited the highest temperature increases, while Er:YAG and Er,Cr:YSGG lasers showed the lowest thermal effects, making them preferable for temperature-sensitive applications.
Various laser types were used, including CO2 [39,40,41,42,43,44,45,46,47,48,49], five researchers used an Er,Cr:YSGG laser [56,60,63,69,70], twelve an Er:YAG laser [13,57,58,59,60,61,62,64,65,66,67,68], three a Nd:YAG laser [12,54,55], two a fiber laser [50,76], seven a diode laser [3,53,71,72,73,74,75], and three researchers used a YAP laser [51,52,53], with Er:YAG and Er,Cr:YSGG lasers emerging as the most effective options.
The studies included different bracket materials, ceramic [13,43,46,51,52,53,56,59,63,64,75], monocrystalline [3,12,41,47,55,57,58,70,75], polycrystalline [12,40,41,42,44,45,48,49,50,54,55,61,62,65,66,67,68,71,72,73,74,76], and zirconia brackets [39], and demonstrated that monocrystalline and zirconia brackets require higher debonding forces (see Table 1).

Table 1.
Detailed characteristics of studies.
3.4. Quality Assessment
Among the articles included in the review, twelve studies [3,39,41,47,55,56,62,66,67,70,72,73] were rated as high quality, achieving scores of between 5 and 6 out of 6. Twenty-four studies [12,13,42,43,45,48,49,50,51,52,53,56,58,59,60,63,64,65,68,69,71,74,75,76] were identified as having a moderate risk of bias with scores ranging from 3 to 4. Five of the studies [44,46,54,57,61] included in this review were classified as low quality (see Table 2).

Table 2.
Quality assessment.
4. Discussion
The objective of this systematic review was to evaluate the effectiveness and safety of laser-assisted debonding of ceramic orthodontic brackets. The lasers investigated in the included studies were the CO2 laser [39,40,41,42,43,44,45,46,47,48,49], Er,Cr:YSGG laser [56,60,63,69,70], Er:YAG laser [3,13,56,57,58,59,60,61,62,63,64,65,66,67,68], Nd:YAG laser [12,44,54,55], fiber laser [50,76], diode laser [3,53,71,72,73,74,75], and Tm:YAP laser [50,51,52,53]. The findings suggest that laser-assisted debonding generally leaves more adhesive residue on the tooth surface compared to conventional debonding methods [3,41,48,49,67,68,72,73]. However, laser irradiation effectively and safely reduces shear bond strength (SBS), provided that appropriate parameter settings—such as laser power, exposure time, and irradiation technique—are utilized [3,39,40,42,43,47,48,49,60,62,63,66,67,68,72,75]. The increase in pulp temperature during laser irradiation varies based on the type of laser, power output, exposure duration, and irradiation method employed [13,39,40,41,43,45,46,47,50,51,52,53,55,56,57,59,65,66,70,71,74,75,76]. These findings emphasize the importance of optimizing laser parameters to achieve efficient debonding while minimizing the risk of thermal damage to dental tissues.
Laser debonding of orthodontic brackets poses a potential risk of thermal damage to the dental pulp [2]. A temperature increase of no more than 5.5 °C is generally considered safe and unlikely to cause irreversible pulp damage [66]. Therefore, selecting an appropriate laser type and optimizing its operational parameters are crucial for ensuring a safe debonding procedure. Of the 41 studies analyzed, 23 specifically evaluated the temperature increase during laser-assisted debonding of ceramic brackets [13,39,40,41,43,45,46,47,50,51,52,53,55,56,57,59,65,66,70,71,74,75,76], while 18 studies did not include temperature measurements [3,12,42,44,48,49,54,58,60,61,62,63,64,67,68,69,72,73]. The results indicate that, in most cases, the use of CO2, Er:YAG, diode, Er,Cr:YSGG, Nd:YAG, Tm:YAP, Tm:fiber, and ytterbium fiber lasers did not cause a pulp temperature increase exceeding the 5.5 °C threshold, suggesting their relative safety for debonding procedures [13,39,40,41,43,45,46,50,51,52,55,57,59,65,66,70,71,74,75,76]. However, temperature elevation was directly correlated with increased laser power. While most tested lasers remained within the safe range, one study reported pulp-damaging temperatures when using a diode laser and a Tm:YAP laser [53]. For CO2 lasers, the mode of irradiation significantly influenced temperature rise. Irradiation in the pulse mode at 5–10 W for 3–5 s [40] and at 188 W for 5 s [41] resulted in a lower temperature increase than in the continuous wave mode at 7 W for 6 s [39]. Additionally, in the same study, when a CO2 laser was set to 3 W, the temperature increase was lower in the super pulse mode (+2.1 °C) than in the normal pulse continuous wave mode (+2.7 °C) [46]. Abdulaziz et al. [70] reported that using a CO2 laser at 4 W in the scanning mode resulted in a lower temperature increase. Similarly, Demirkan et al. [50] found that temperature elevation was reduced in the scanning mode, but only under specific conditions: 2.5 W with a 10 s exposure and 3 W with a 7 s exposure. These findings highlight the importance of optimizing laser parameters, particularly power settings, exposure duration, and irradiation mode, to mitigate thermal risks while ensuring effective bracket debonding.
Reducing shear bond strength (SBS) between the tooth and the ceramic orthodontic bracket is a critical factor in achieving safe and efficient debonding while minimizing the risk of enamel damage. An analysis of 41 published studies revealed that 16 studies specifically evaluated SBS during laser-assisted debonding of ceramic brackets [3,39,40,42,43,47,48,49,60,62,63,66,67,68,73,75], whereas 25 studies did not include SBS measurements [12,13,41,44,45,46,50,51,52,53,54,55,56,57,58,59,61,64,65,69,70,71,72,74,76]. The findings demonstrated that laser exposure effectively reduces SBS compared to conventional debonding methods. For CO2 lasers, optimal parameters included a power setting of 5–10 W with an exposure duration of 3–6 s in a continuous wave mode [39,40,42,43,47,48,49]. In contrast, the Er:YAG laser yielded the best results at a power of 3–4 W with an exposure duration of 6–9 s, particularly when applied using a scanning motion [62,66,67,68]. Studies reported that laser application reduced SBS from baseline values of 13–23 MPa to 7–12 MPa, with higher power settings and longer exposure durations (within safe limits) leading to greater SBS reductions [40,49,62,66,67,68]. Most studies concluded that the reduced SBS values remained within clinically acceptable ranges (5–10 MPa) for safe bracket removal while mitigating the risk of enamel damage [40,42,62,66,67,68]. Furthermore, the application of a scanning motion proved to be more effective than static irradiation across different laser types, ensuring a more uniform energy distribution and reducing the risk of localized overheating [62,66,67]. These findings emphasize the importance of optimizing laser parameters to achieve efficient debonding while preserving enamel integrity.
The adhesive remnant index (ARI) is a crucial parameter that quantifies the amount of adhesive residue remaining on the tooth surface after bracket debonding, playing a key role in assessing the effectiveness and safety of different debonding techniques [2]. Among the 41 analyzed studies, 25 specifically evaluated ARI [3,13,39,40,41,42,43,44,47,48,49,60,61,62,64,65,66,67,68,69,70,72,73,74,75], while 16 did not include ARI measurements [12,45,46,50,51,52,53,54,55,56,57,58,59,63,71,76]. Most studies employed a standardized 4-point ARI scale, where Score 0 indicated no adhesive remaining on the tooth surface and Score 3 represented complete adhesive retention. A consistent trend emerged across laser types, with laser-treated groups exhibiting a higher frequency of Scores 2 and 3 [41,48,67,68,72,73], suggesting more adhesive remained on the tooth surface compared to control groups, which showed a higher prevalence of Scores 0 and 1 [3,41,49]. Studies on CO2 [41,48,49], Er:YAG [61,62,64,66,67,68], diode [3], and Nd:YAG [54] lasers confirmed that bond failure predominantly occurred at the bracket–adhesive interface rather than the enamel–adhesive interface, reducing the risk of enamel damage. In contrast, conventional debonding methods showed a higher occurrence of Scores 0 and 1 [41,49,66,67,68,69,70], indicating bond failure often occurred at the enamel–adhesive interface, increasing the potential for enamel microfractures. Several studies [3,13,41,42,49,67,68] concluded that the higher ARI scores associated with laser debonding offer clinical benefits, as they reduce enamel damage risk, improve debonding safety by shifting failure to the bracket–adhesive interface, and enhance tooth surface preservation by minimizing the need for aggressive adhesive removal. The consistency of these findings suggests that laser-assisted debonding provides a safer and more protective alternative to conventional mechanical methods, making it a valuable tool in contemporary orthodontic practice.
The reviewed research on laser-assisted debonding of ceramic brackets demonstrates significant heterogeneity in methodology and measurement protocols across studies, posing challenges in drawing definitive clinical conclusions. One of the primary limitations is the predominance of in vitro studies over clinical trials, with only a single in vivo investigation available [58]. Additionally, variability in the type of teeth used for experimentation introduces further inconsistency, as the majority of studies (28) utilized human teeth, whereas 7 studies used bovine teeth, and 2 studies incorporated both types. The lack of uniformity in laser settings, application techniques, and measurement protocols for shear bond strength (SBS), adhesive remnant index (ARI), and temperature assessment further complicates direct comparisons across studies. The diversity in research approaches and the absence of standardized protocols significantly limit the ability to formulate universal clinical recommendations. These limitations underscore the urgent need for more extensive, well-designed randomized clinical trials (RCTs) with larger sample sizes and standardized methodologies to ensure reproducibility and clinical applicability. Future studies should focus on establishing evidence-based guidelines for laser parameters, application techniques, and safety thresholds to optimize debonding efficiency while minimizing risks. To facilitate the integration of laser-assisted debonding into routine orthodontic practice, further investigations should aim to develop a standardized protocol that ensures both effectiveness and patient safety.
5. Conclusions
The systematic review of 41 studies on laser-assisted ceramic bracket removal has demonstrated promising effectiveness across multiple laser types, particularly CO2 and Er:YAG lasers, which were the most frequently studied and reported as safe and efficient for debonding. The majority of studies confirmed that laser-assisted techniques provide a reliable alternative to conventional mechanical methods while minimizing the risk of enamel damage. Shear bond strength (SBS) was evaluated in 16 studies, revealing a significant reduction from baseline values of 13–23 MPa to clinically acceptable ranges of 7–12 MPa post-laser application, facilitating safer bracket removal. Additionally, 25 studies assessed the adhesive remnant index (ARI), with laser-treated groups consistently exhibiting higher ARI scores (2–3), indicating that bond failure primarily occurred at the bracket–adhesive interface rather than the enamel–adhesive interface, thereby reducing the risk of enamel microfractures compared to conventional methods. Temperature monitoring, conducted in 23 studies, confirmed that carefully optimized laser parameters can maintain pulpal temperature increases within safe limits, preventing irreversible thermal damage. However, despite these positive findings, precise laser parameter settings remain critical for ensuring both efficiency and safety, particularly in preventing excessive temperature elevation that could compromise pulpal health. Given the heterogeneity in methodologies and the predominance of in vitro studies, further randomized clinical trials (RCTs) with standardized protocols are essential to establish evidence-based guidelines for optimal laser parameters and application techniques. This will facilitate the safe and effective integration of laser-assisted debonding into routine orthodontic practice while maximizing patient safety and treatment outcomes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jfb16040123/s1, Table S1. General characteristics of studies.
Author Contributions
Conceptualization, M.M., J.M. and M.D.; methodology, S.K.; software, M.M.; validation, J.M.; formal analysis, M.M.; investigation, M.M., A.K., S.K., J.K. and K.W.; resources, M.M.; data curation, M.M., A.K., S.K., J.K. and K.W.; writing—original draft preparation, M.M., A.K., S.K., J.K. and K.W.; writing—review and editing, J.Z.Z., J.M. and M.M.; visualization, J.Z.Z. and J.K.; supervision, J.M.; project administration, J.M. and M.D.; funding acquisition, M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financed by a subsidy from Wroclaw Medical University.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data supporting the findings of this study are available within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Russell, J.S. Current Products and Practice. J. Orthod. 2005, 32, 146–163. [Google Scholar] [CrossRef] [PubMed]
- Woś, P.; Kiryk, S.; Dyl, T.; Kiryk, J.; Horodniczy, T.; Szablińska, M.; Dubowik, M.A.; Dobrzyński, W.; Mikulewicz, M.; Matys, J.; et al. Laser Applications in Metal Orthodontic Bracket Debonding: A Systematic Review. Appl. Sci. 2025, 15, 927. [Google Scholar] [CrossRef]
- Khalil, A.S.; Tamish, N.M.; Elkalza, A.R. Assessment of Chemical, Ultrasonic, Diode Laser, and Er:YAG Laser Application on Debonding of Ceramic Brackets. BMC Oral Health 2022, 22, 79. [Google Scholar] [CrossRef] [PubMed]
- Dhannawat, P.K.; Gilani, R.; Shrivastav, S.S.; Kamble, R.H.; Murarka, S.P.; Rathi, S.S.; Vishnani, R. Debonding Techniques—A Review. J. Evol. Med. Dent. Sci. 2021, 10, 3430–3435. [Google Scholar] [CrossRef]
- Subramani, K.; Bollu, P. Debonding of Orthodontic Ceramic Brackets: A Comprehensive Review of the Literature—Part 1. IP Indian J. Orthod. Dentofac. Res. 2020, 6, 109–113. [Google Scholar] [CrossRef]
- Subramani, K.; Bollu, P. Debonding of Orthodontic Ceramic Brackets: A Comprehensive Review of the Literature—Part 2. IP Indian J. Orthod. Dentofac. Res. 2020, 6, 114–119. [Google Scholar] [CrossRef]
- Suliman, S.N.; Trojan, T.M.; Tantbirojn, D.; Versluis, A. Enamel Loss Following Ceramic Bracket Debonding: A Quantitative Analysis in Vitro. Angle Orthod. 2015, 85, 651–656. [Google Scholar] [CrossRef]
- Grocholewicz, K. Effect of Orthodontic Debonding and Adhesive Removal on the Enamel—Current Knowledge and Future Perspectives—A Systematic Review. Med. Sci. Monit. 2014, 20, 1991–2001. [Google Scholar] [CrossRef]
- Vidor, M.M.; Felix, R.P.; Marchioro, E.M.; Hahn, L. Enamel Surface Evaluation after Bracket Debonding and Different Resin Removal Methods. Dental Press J. Orthod. 2015, 20, 61–67. [Google Scholar] [CrossRef]
- Nakada, N.; Uchida, Y.; Inaba, M.; Kaetsu, R.; Shimizu, N.; Namura, Y.; Motoyoshi, M. Pain and Removal Force Associated with Bracket Debonding: A Clinical Study. J. Appl. Oral Sci. 2021, 29, e20200879. [Google Scholar] [CrossRef]
- Ajwa, N.; Alfayez, H.; Al-Oqab, H.; Melibary, R.; Alzamil, Y. The Effect of Erbium-Doped Yttrium Aluminum Garnet Laser in Debonding of Orthodontic Brackets: A Systematic Review of the Literature. Photobiomodul. Photomed. Laser Surg. 2021, 39, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Tocchio, R.M.; Williams, P.T.; Mayer, F.J.; Standing, K.G. Laser Debonding of Ceramic Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Leśniak, K.; Matys, J.; Żmuda-Stawowiak, D.; Mroczka, K.; Dominiak, M.; Brugnera Junior, A.; Gruber, R.; Romanos, G.E.; Sculean, A. Er:YAG Laser for Metal and Ceramic Bracket Debonding: An In Vitro Study on Intrapulpal Temperature, SEM, and EDS Analysis. Photomed. Laser Surg. 2018, 36, 595–600. [Google Scholar] [CrossRef]
- Mosaddad, S.A.; Abduo, J.; Zakizade, M.; Tebyaniyan, H.; Hussain, A. The Effect of Various Lasers on the Bond Strength Between Orthodontic Brackets and Dental Ceramics: A Systematic Review and Meta-Analysis. Photobiomodul. Photomed. Laser Surg. 2024, 42, 20–48. [Google Scholar] [CrossRef]
- Azzeh, E.; Feldon, P.J. Laser Debonding of Ceramic Brackets: A Comprehensive Review. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 79–83. [Google Scholar] [CrossRef]
- Mahmoud, E.; Pacurar, M.; Bechir, E.S.; Maris, M.; Olteanu, C.; Dascalu, I.T.; Moldovan, M. Comparison of Shear Bond Strength and Adhesive Remnant Index of Brackets Bonded with Two Types of Orthodontic Adhesives. Mater. Plast. 2017, 54, 141–144. [Google Scholar] [CrossRef]
- Gupta, M.; David, S.A.; Nishad, A.; Ramanna, P.K.; Bhagvandas, S.C. In Vitro Analysis of Shear Bond Strength and Adhesive Remnant Index of Stainless Steel Brackets with Different Adhesive Systems to Enamel. J. Contemp. Dent. Pract. 2018, 19, 1047–1051. [Google Scholar] [CrossRef]
- Kunizhev, B.I.; Torshkhoeva, Z.S.; Zhelikhazhev, R.N.; Starov, A.V. Destruction of Polymers under the Action of Laser Radiation. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1083, 012040. [Google Scholar] [CrossRef]
- Kiryk, J.; Matys, J.; Nikodem, A.; Burzyńska, K.; Grzech-Leśniak, K.; Dominiak, M.; Dobrzyński, M. The Effect of Er:YAG Laser on a Shear Bond Strength Value of Orthodontic Brackets to Enamel—A Preliminary Study. Materials 2021, 14, 2093. [Google Scholar] [CrossRef]
- Guzman, U.A.; Jerrold, L.; Vig, P.S.; Abdelkarim, A. Comparison of Shear Bond Strength and Adhesive Remnant Index between Precoated and Conventionally Bonded Orthodontic Brackets. Prog. Orthod. 2013, 14, 39. [Google Scholar] [CrossRef]
- Mesaroș, A.; Mesaroș, M.; Buduru, S. Orthodontic Bracket Removal Using LASER-Technology—A Short Systematic Literature Review of the Past 30 Years. Materials 2022, 15, 548. [Google Scholar] [CrossRef] [PubMed]
- Zach, L.; Cohen, G. Pulp Response to Externally Applied Heat. Oral Surg. Oral Med. Oral Pathol. 1965, 19, 515–530. [Google Scholar] [CrossRef] [PubMed]
- Nalbantgil, D.; Tozlu, M.; Oztoprak, M.O. Pulpal Thermal Changes Following Er-YAG Laser Debonding of Ceramic Brackets. Sci. World J. 2014, 2014, 1–4. [Google Scholar] [CrossRef]
- Sauk, J.J.; Norris, K.; Foster, R.A.; Moehring, J.M.; Somerman, M.J. Expression of Heat Stress Proteins by Human Periodontal Ligament Cells. J. Oral Pathol. Med. 1988, 17, 496–498. [Google Scholar] [CrossRef]
- Eriksson, A.R.; Albrektsson, T. Temperature Threshold Levels for Heat-Induced Bone Tissue Injury: A Vital-Microscopic Study in the Rabbit. J. Prosthet. Dent. 1983, 50, 101–107. [Google Scholar] [CrossRef]
- Gibas-Stanek, M.; Pełka, P.; Pihut, M. What Is the Safest Method of Orthodontic Debonding- a Systematic Review of the Literature. Folia Med. Cracov. 2023, 30, 133–156. [Google Scholar] [CrossRef]
- Ozcan, M.; Finnema, K.; Ybema, A. Evaluation of Failure Characteristics and Bond Strength after Ceramic and Polycarbonate Bracket Debonding: Effect of Bracket Base Silanization. Eur. J. Orthod. 2008, 30, 176–182. [Google Scholar] [CrossRef]
- Huang, X.; Lin, J.; Demner-Fushman, D. Evaluation of PICO as a Knowledge Representation for Clinical Questions. AMIA Annu. Symp. Proc. 2006, 2006, 359–363. [Google Scholar]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Struzik, N.; Wiśniewska, K.; Piszko, P.J.; Piszko, A.; Kiryk, J.; Matys, J.; Dobrzyński, M. SEM Studies Assessing the Efficacy of Laser Treatment for Primary Teeth: A Systematic Review. Appl. Sci. 2024, 14, 1107. [Google Scholar] [CrossRef]
- Kiryk, J.; Kiryk, S.; Kensy, J.; Świenc, W.; Palka, B.; Zimoląg-Dydak, M.; Dobrzyński, W.; Matys, J.; Dobrzyński, M. Effectiveness of Laser-Assisted Teeth Bleaching: A Systematic Review. Appl. Sci. 2024, 14, 9219. [Google Scholar] [CrossRef]
- Piszko, P.J.; Piszko, A.; Kiryk, J.; Lubojański, A.; Dobrzyński, W.; Wiglusz, R.J.; Matys, J.; Dobrzyński, M. The Influence of Fluoride Gels on the Physicochemical Properties of Tooth Tissues and Dental Materials—A Systematic Review. Gels 2024, 10, 98. [Google Scholar] [CrossRef] [PubMed]
- Struzik, N.; Kensy, J.; Piszko, P.J.; Kiryk, J.; Wiśniewska, K.; Kiryk, S.; Korjat, Ł.; Horodniczy, T.; Sobierajska, P.; Matys, J.; et al. Contamination in Bone Substitute Materials: A Systematic Review. Appl. Sci. 2024, 14, 8266. [Google Scholar] [CrossRef]
- Piszko, P.J.; Piszko, A.; Kiryk, S.; Kiryk, J.; Horodniczy, T.; Struzik, N.; Wiśniewska, K.; Matys, J.; Dobrzyński, M. Bone Regeneration Capabilities of Scaffolds Containing Chitosan and Nanometric Hydroxyapatite—Systematic Review Based on In Vivo Examinations. Biomimetics 2024, 9, 503. [Google Scholar] [CrossRef]
- Rygas, J.; Matys, J.; Wawrzyńska, M.; Szymonowicz, M.; Dobrzyński, M. The Use of Graphene Oxide in Orthodontics—A Systematic Review. J. Funct. Biomater. 2023, 14, 500. [Google Scholar] [CrossRef]
- Kowalski, J.; Rygas, J.; Homa, K.; Dobrzyński, W.; Wiglusz, R.J.; Matys, J.; Dobrzyński, M. Antibacterial Activity of Endodontic Gutta-Percha—A Systematic Review. Appl. Sci. 2023, 14, 388. [Google Scholar] [CrossRef]
- Kensy, J.; Dobrzyński, M.; Wiench, R.; Grzech-Leśniak, K.; Matys, J. Fibroblasts Adhesion to Laser-Modified Titanium Surfaces—A Systematic Review. Materials 2021, 14, 7305. [Google Scholar] [CrossRef]
- Watson, P.F.; Petrie, A. Method Agreement Analysis: A Review of Correct Methodology. Theriogenology 2010, 73, 1167–1179. [Google Scholar] [CrossRef]
- Arima, S.; Namura, Y.; Tamura, T.; Shimizu, N. Easy Debonding of Ceramic Brackets Bonded with a Light-Cured Orthodontic Adhesive Containing Microcapsules with a CO2 Laser. Photomed. Laser Surg. 2018, 36, 162–168. [Google Scholar] [CrossRef]
- Macri, R.T.; de Lima, F.A.; Bachmann, L.; Galo, R.; Romano, F.L.; Borsatto, M.C.; Matsumoto, M.A.N. CO2 Laser as Auxiliary in the Debonding of Ceramic Brackets. Lasers Med. Sci. 2015, 30, 1835–1841. [Google Scholar] [CrossRef]
- Ahrari, F.; Heravi, F.; Fekrazad, R.; Farzanegan, F.; Nakhaei, S. Does Ultra-Pulse CO2 Laser Reduce the Risk of Enamel Damage during Debonding of Ceramic Brackets? Lasers Med. Sci. 2012, 27, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Matos, D.S.; Küchler, E.C.; Borsatto, M.C.; Matsumoto, M.A.N.; Marques, F.V.; Romano, F.L. CO2 Laser Irradiation for Debonding Ceramic Orthodontic Brackets. Braz. Dent. J. 2021, 32, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Saito, A.; Namura, Y.; Isokawa, K.; Shimizu, N. CO2 Laser Debonding of a Ceramic Bracket Bonded with Orthodontic Adhesive Containing Thermal Expansion Microcapsules. Lasers Med. Sci. 2015, 30, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Strobl, K.; Bahns, T.L.; Wiliham, L.; Bishara, S.E.; Stwalley, W.C. Laser-Aided Debonding of Orthodontic Ceramic Brackets. Am. J. Orthod. Dentofac. Orthop. 1992, 101, 152–158. [Google Scholar] [CrossRef]
- Ma, T.; Marangoni, R.D.; Flint, W. In Vitro Comparison of Debonding Force and Intrapulpal Temperature Changes during Ceramic Orthodontic Bracket Removal Using a Carbon Dioxide Laser. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 203–210. [Google Scholar] [CrossRef]
- Obata, A. Super Pulse CO2 Laser for Bracket Bonding and Debonding. Eur. J. Orthod. 1999, 21, 193–198. [Google Scholar] [CrossRef]
- Iijima, M.; Yasuda, Y.; Muguruma, T.; Mizoguchi, I. Effects of CO2 Laser Debonding of a Ceramic Bracket on the Mechanical Properties of Enamel. Angle Orthod. 2010, 80, 1029–1035. [Google Scholar] [CrossRef]
- Mimura, H.; Deguchi, T.; Obata, A.; Yamagishi, T.; Ito, M. Comparison of Different Bonding Materials for Laser Debonding. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 267–273. [Google Scholar] [CrossRef]
- Tehranchi, A.; Fekrazad, R.; Zafar, M.; Eslami, B.; Kalhori, K.A.M.; Gutknecht, N. Evaluation of the Effects of CO2 Laser on Debonding of Orthodontics Porcelain Brackets vs. the Conventional Method. Lasers Med. Sci. 2011, 26, 563–567. [Google Scholar] [CrossRef]
- Demirkan, I.; Sarp, A.S.K.; Gülsoy, M. Ceramic Bracket Debonding with Tm:Fiber Laser. J. Biomed. Opt. 2016, 21, 065007. [Google Scholar] [CrossRef]
- Dostalová, T.; Jelinková, H.; Šulc, J.; Němec, M.; Fibrich, M.; Jelínek, M.; Michalík, P.; Bučková, M. Bond Strengths Evaluation of Laser Ceramic Bracket Debonding. Laser Phys. 2012, 22, 1395–1400. [Google Scholar] [CrossRef]
- Dostalova, T.; Jelinkova, H.; Sulc, J.; Nemec, M.; Jelinek, M.; Fibrich, M.; Michalik, P.; Miyagi, M.; Seydlova, M. Ceramic Bracket Debonding by Tm:YAP Laser Irradiation. Photomed. Laser Surg. 2011, 29, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Dostálová, T.; Jelínková, H.; Šulc, J.; Koranda, P.; Nemec, M.; Racek, J.; Miyagi, M. Laser Radiation Bracket Debonding; Rechmann, P., Fried, D., Eds.; SPIE: Bellingham, WA, USA, 2008; p. 684304. [Google Scholar]
- Han, X.; Liu, X.; Bai, D.; Meng, Y.; Huang, L. Nd:YAG Laser-Aided Ceramic Brackets Debonding: Effects on Shear Bond Strength and Enamel Surface. Appl. Surf Sci. 2008, 255, 613–615. [Google Scholar] [CrossRef]
- Hayakawa, K. Nd: YAG Laser for Debonding Ceramic Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 638–647. [Google Scholar] [CrossRef]
- Downarowicz, P.; Noszczyk, P.; Mikulewicz, M.; Nowak, R. Thermal Effect of Er:YAG and Er,Cr:YSGG Used for Debonding Ceramic and Metal Orthodontic Brackets: An Experimental Analysis. Adv. Clin. Exp. Med. 2020, 29, 557–563. [Google Scholar] [CrossRef]
- Yilanci, H.; Yildirim, Z.B.; Ramoglu, S.I. Intrapulpal Temperature Increase During Er:YAG Laser-Aided Debonding of Ceramic Brackets. Photomed. Laser Surg. 2017, 35, 217–222. [Google Scholar] [CrossRef]
- Mocuta, D.-E.; Miron, M.I.; Lungeanu, D.; Mateas, M.; Ogodescu, E.; Todea, C.D. Laser Er:YAG-Assisted Debonding May Be a Viable Alternative to the Conventional Method for Monocrystalline Ceramic Brackets. Int. J. Environ. Res. Public Health 2022, 19, 14564. [Google Scholar] [CrossRef]
- Dostalova, T.; Jelinkova, H.; Remes, M.; Šulc, J.; Němec, M. The Use of the Er:YAG Laser for Bracket Debonding and Its Effect on Enamel Damage. Photomed. Laser Surg. 2016, 34, 394–399. [Google Scholar] [CrossRef]
- Mirhashemi, A.H.; Hossaini, S.M.H.; Etemadi, A.; Kharazifard, M.J.; Bahador, A.; Soudi, A. Effect of Er:YAG and Er,Cr:YSGG Lasers on Ceramic Bracket Debonding from Composite Blocks. Front. Dent. 2019, 16, 88. [Google Scholar] [CrossRef]
- Mundethu, A.R.; Gutknecht, N.; Franzen, R. Rapid Debonding of Polycrystalline Ceramic Orthodontic Brackets with an Er:YAG Laser: An in Vitro Study. Lasers Med. Sci. 2014, 29, 1551–1556. [Google Scholar] [CrossRef] [PubMed]
- Tozlu, M.; Oztoprak, M.O.; Arun, T. Comparison of Shear Bond Strengths of Ceramic Brackets after Different Time Lags between Lasing and Debonding. Lasers Med. Sci. 2012, 27, 1151–1155. [Google Scholar] [CrossRef]
- Hoteit, M.; Nammour, S.; Zeinoun, T. Evaluation of Enamel Topography after Debonding Orthodontic Ceramic Brackets by Different Er,Cr:YSGG and Er:YAG Lasers Settings. Dent. J. 2020, 8, 6. [Google Scholar] [CrossRef] [PubMed]
- Hamadah, O.; Bachir, W.; Zamzam, M.K. Thermal Effect of Er:YAG Laser Pulse Durations on Teeth During Ceramic Bracket Debonding. Dent. Med. Probl. 2016, 53, 352–357. [Google Scholar] [CrossRef]
- Nalbantgil, D.; Tozlu, M.; Oztoprak, M.O. Comparison of Different Energy Levels of Er:YAG Laser Regarding Intrapulpal Temperature Change During Safe Ceramic Bracket Removal. Photomed. Laser Surg. 2018, 36, 209–213. [Google Scholar] [CrossRef]
- Nalbantgil, D.; Oztoprak, M.O.; Tozlu, M.; Arun, T. Effects of Different Application Durations of ER:YAG Laser on Intrapulpal Temperature Change during Debonding. Lasers Med. Sci. 2011, 26, 735–740. [Google Scholar] [CrossRef]
- Oztoprak, M.O.; Nalbantgil, D.; Erdem, A.S.; Tozlu, M.; Arun, T. Debonding of Ceramic Brackets by a New Scanning Laser Method. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 195–200. [Google Scholar] [CrossRef]
- Alakuş Sabuncuoğlu, F.; Erşahan, Ş.; Ertürk, E. Debonding of Ceramic Brackets by Er:YAG Laser. J. Istanb. Univ. Fac. Dent. 2016, 50, 24. [Google Scholar] [CrossRef]
- Rao, A.; Deenadayalan, P.; Deepak, C.; Dilipkumar, D.; Angrish, N.; Shetty, S.S. Effect of ER, CR: YSGG Laser Debonding on Enamel Surface Changes in Stainless Steel and Ceramic Brackets—An in Vitro Study. J. Orthod. Sci. 2023, 12, 7. [Google Scholar] [CrossRef]
- Abdulaziz, A.; El-Kholy, M.M.; Bushra, S.S.; Ali, S.M.; Shehab, K.A. Performance of Two Laser Motion Modes versus Conventional Orthodontic Ceramic Brackets Debonding Technique on Enamel Surface Topography. Lasers Med. Sci. 2024, 39, 156. [Google Scholar] [CrossRef]
- Stein, S.; Wenzler, J.; Hellak, A.; Schauseil, M.; Korbmacher-Steiner, H.; Braun, A. Intrapulpal Temperature Increases Caused by 445-Nm Diode Laser-Assisted Debonding of Self-Ligating Ceramic Brackets During Simulated Pulpal Fluid Circulation. Photomed. Laser Surg. 2018, 36, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Stein, S.; Kleye, A.; Schauseil, M.; Hellak, A.; Korbmacher-Steiner, H.; Braun, A. 445-Nm Diode Laser-Assisted Debonding of Self-Ligating Ceramic Brackets. Biomed. Eng. Biomed. Tech. 2017, 62, 513–520. [Google Scholar] [CrossRef]
- Stein, S.; Hellak, A.; Schauseil, M.; Korbmacher-Steiner, H.; Braun, A. Effects of 445-Nm Diode Laser-Assisted Debonding of Self-Ligating Ceramic Brackets on Shear Bond Strength. Photomed. Laser Surg. 2018, 36, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Yassaei, S.; Soleimanian, A.; Nik, Z.E. Effects of Diode Laser Debonding of Ceramic Brackets on Enamel Surface and Pulpal Temperature. J. Contemp. Dent. Pract. 2015, 16, 270–274. [Google Scholar] [CrossRef]
- Feldon, P.J.; Murray, P.E.; Burch, J.G.; Meister, M.; Freedman, M.A. Diode Laser Debonding of Ceramic Brackets. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 458–462. [Google Scholar] [CrossRef]
- Sarp, A.S.K.; Gülsoy, M. Ceramic Bracket Debonding with Ytterbium Fiber Laser. Lasers Med. Sci. 2011, 26, 577–584. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).