Abstract
Little has been studied regarding the repeated usage of healing abutments and their effects on the distortion of dental implant-healing abutment hex surfaces. Additionally, implant manufacturers do not provide specific guidelines on how many times a healing abutment can be used before discarding. Therefore, we evaluated the effect of repeated screwing-unscrewing of implant-healing abutment on the healing abutment hex surface and screw head. A total of 12 Biomate implants with 4 mm diameter and 13 mm length were inserted into a synthetic bone block. The standard healing abutments of 3 mm diameter and 4 mm length were screwed onto each implant using a torque ratchet at a final torque of 30 Ncm. Immediately, the abutments were unscrewed at 30 Ncm. Then, screwing-unscrewing was repeated for 4, 8, 16, 24, 32, 40, 80, 160, 320, and 400 times and the healing abutments were scanned under the scanning electron microscope for any distortion. Distortion was graded as 0, 1, 2, and 3. Data were analyzed using SPSS 24.0. Descriptive statistics were calculated. One-way ANOVA with post hoc using Tukey’s HSD test was performed to analyze the difference in distortion at different screwing-unscrewing times. A significant level was selected at p-value = 0.05. It was found that distortion healing abutments screws were seen after 32 times screwing and unscrewing. There was a significant difference in the distortion (p-value < 0.05) after 24 times of repeated usage of healing abutment and at 160, 320, and 400 times. No surface distortions were observed at the healing abutment screw head at 4, 8, 16, 24, 32, 40, 80, 160, 320, and 400 cycles of screwing-unscrewing. It can be concluded that repeated screwing and unscrewing of the implant-healing abutments causes damage to the healing abutment hex surface. The distortion of healing abutments screws was seen after 32 times screwing and unscrewing. No surface distortions were observed on the healing abutment screw head until 400 times of screwing and unscrewing. Hence, the clinician should be cautious while using the healing abutments repeatedly.
1. Introduction
Dental implants with digital technologies are widely used for the prosthetic rehabilitation of a missing tooth [1]. A typical dental implant consists of a body, which gets integrated with the native bone, and an abutment, which connects to the implant body and holds the tooth superstructure. Healing abutments and cover screws are interim devices used for special purposes [2].
Healing abutments are temporary components placed on the implant body during the healing period and aid in providing healthy peri-implant mucosa to support the future tooth prosthesis. Implant components are usually manufactured from titanium or its alloys, although newer materials are being tried [3]. The mechanized material is suggested to be a principal factor in increasing the execution of the healing abutment [4,5].
The screw design of the healing abutment and its physical properties vary greatly between manufacturers. The differences in screw design and physical property among healing abutments of different manufacturers may be attributed to the external diameter, thread depth, precision of taper, components, and poor tooling of the healing abutment. These may cause significant differences in complications especially screw loosening [6,7].
Poor connection between healing abutment screw and implant internal hex connection may cause implant-related complications, such as implant-crown dislodgement. Although the interface between the healing abutment screw and implant internal hex connection is important, no studies have been carried out on the biomechanical integrity of the healing abutment screw and implant internal hex connection. Hence, we evaluated the distortion of hex threads of a used healing abutment microscopically [8].
Repeated use of healing abutment may lead to plastic deformation due to repetitive preloads during tightening and retightening. This plastic deformation might cause screw loosening and accidental removal of the abutment in the patient’s oral cavity or might cause micro gaps between the implant-abutment interface [9]. The peri-implant dimensions, as evident from histologic studies, are significantly influenced by the micro gaps at the implant-abutment junction and its location in relation to the alveolar crest, which ultimately affects the peri-implant bone loss [10]. As reported by literature, the mechanism behind this was due to mechanical and biological problems. Biological factors include the formation of bacterial reservoirs near the implant-abutment interface. The mechanical problem of the micro gap results in the micro-movements and possible loosening or fracture of screw-retained abutments [11,12].
Decontamination of implant parts, especially used healing abutments, is important and is achievable through procedures such as autoclave, NOC, air polishing, electrolysis, etc. [13,14,15]. An effective method for decontamination of used healing abutment can be performed by electrolysis by placing the contaminated healing abutments on a carbon cathode and applying the electric current of 1 A at a constant 10 V in 7.5% sodium bicarbonate [14]. This method can be useful in the clinical management of peri-implant infections.
The reusability of healing abutments has often been considered debatable owing to the lack of universal consensus or guidelines. In addition, the implant manufacturers have not provided any recommendations for the repeated usage of their healing abutments, although there is an effect of screwing-unscrewing of healing abutment on the healing abutment hex surface and screw head [16,17]. Hence, the present study was conducted to assess the effect of screwing-unscrewing of implant-healing abutment on the implant hex surface and screw head. The null hypothesis proposes that there is no effect of screwing-unscrewing of healing abutment on the implant hex surface and screw head.
2. Materials and Methods
2.1. Materials
This study used dental implants and healing abutments, bone block, dental implant torque ratchet (Biomate Medical Devices Technology Co., Ltd., Kaohsiung, Taiwan), and SEM (ProSciTech Pty Ltd., Townsville, Australia). The characteristics of the dental implant parts are summarized in Table 1. The mechanical properties of the implant, healing abutment, and the screwdriver are shown in Table 2.

Table 1.
Characteristics of the dental implant used in this study.

Table 2.
The mechanical properties of the dental implant, healing abutment, and screwdriver [18,19,20].
2.2. Implant Insertion
In this study, 12 Biomate implants were used. The sample size calculation was conducted following previous studies in which the sample size ranged from 10 to 15 [21,22]. Implants of size 4 mm in diameter and 14 mm in length were inserted into the synthetic bone block. Three bone blocks were used in our study. Four implants were placed in each bone block at a distance of 5 mm. All the implants were placed equicrestally as per the standard procedure [23]. Copious irrigation was maintained throughout the procedure. Physiodispenser was set at a torque of 40 Newtons and speed of 800 rpm and used to place all the implants as recommendations from previous studies [24,25].
2.3. Placement of Healing Abutment
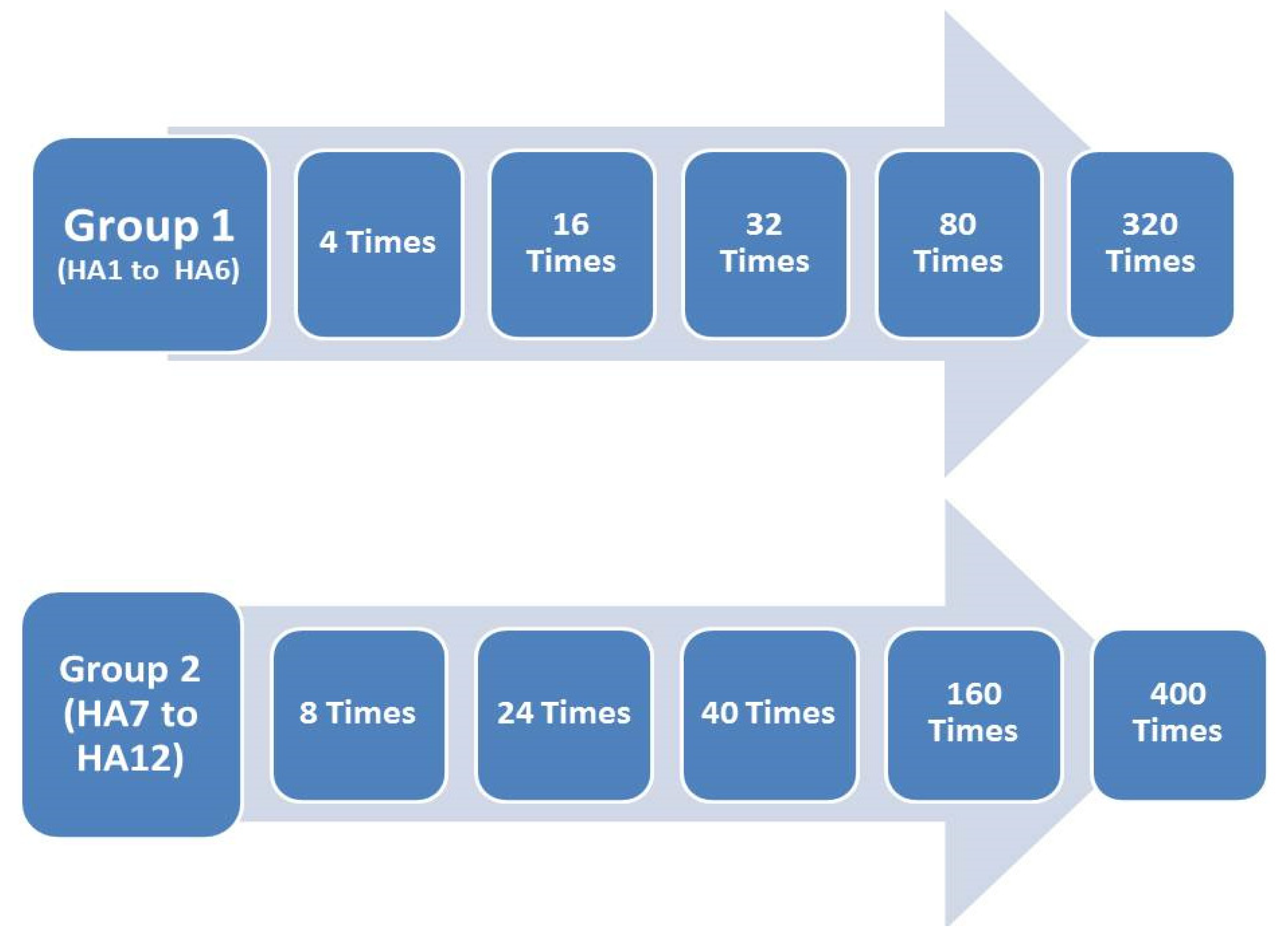
The standard healing abutment (HA) of 3 mm diameter and 4 mm length was used in our study. The 12 healing abutments were divided into two groups; the first group (HA 1 to HA 6) was screwed-unscrewed 4, 16, 32, 80, and 320 times (Figure 1). The second group (HA7 to HA12) was screwed-unscrewed for 8, 24, 40, 160, and 400 times. A torque ratchet at a final torque of 30 Ncm was used for all samples. Then, the abutments were unscrewed, and the procedure was repeated.
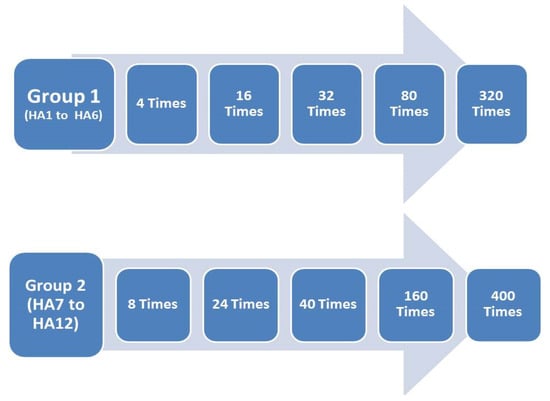
Figure 1.
Study groups of screwing-unscrewing used in this study.
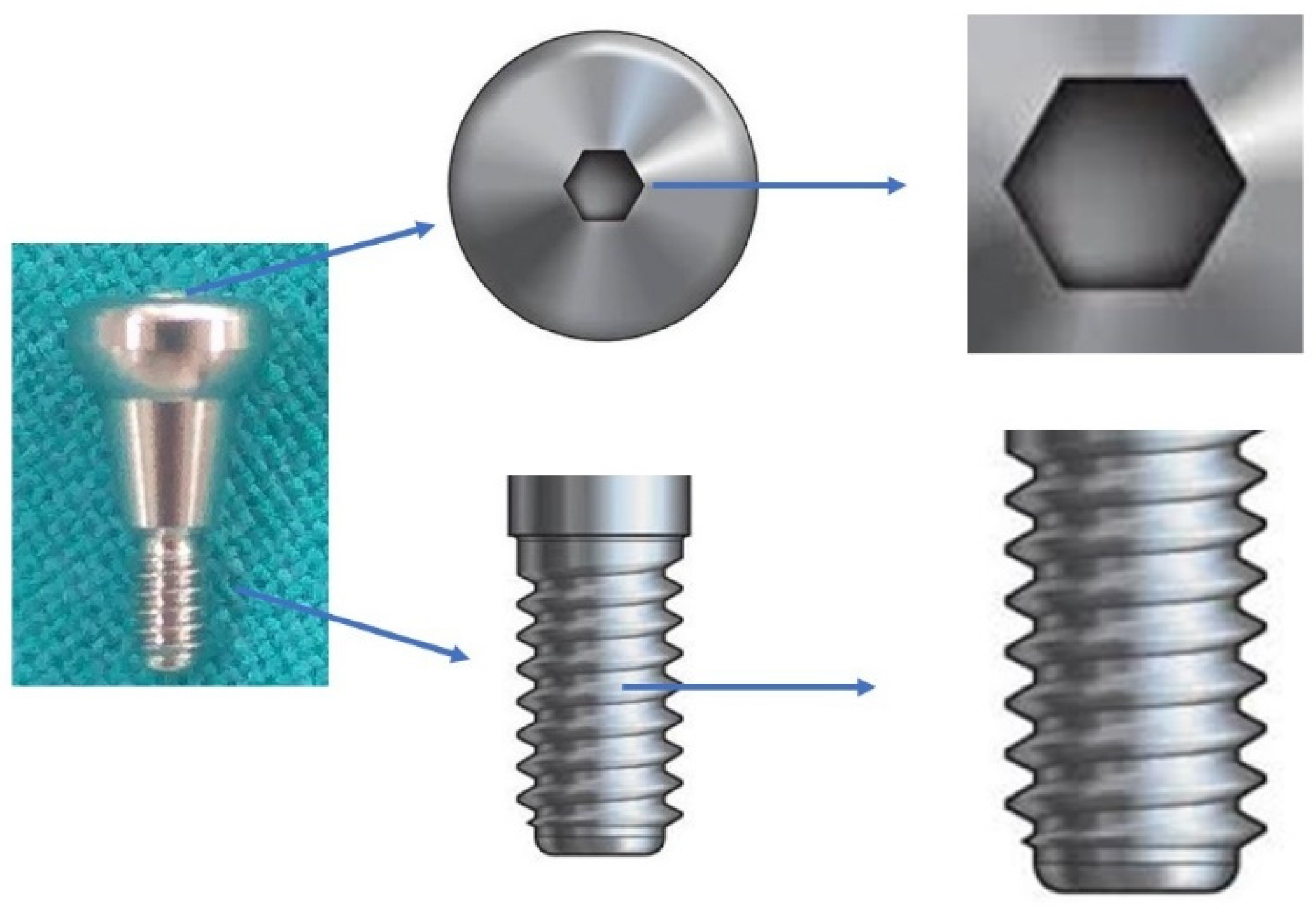
One-sided grooves were created on the healing abutment by an ai-rotor handpiece using straight diamond bur for placement, orientation, and identification during the microscopic procedure. Each healing abutment was sent for the SEM evaluation after the aforementioned times of screwing and unscrewing. Two parts of the healing abutments were evaluated under the SEM; first, the connecting screw head of the healing abutment, and second, the screw thread of the healing abutments. The external surface of the healing abutment screw consisting of thread for connection to the corresponding internal hex of the dental implant was hypothesized to deform after repeated loading and unloading. The hollow portion over the superior surface of the screw wherein the screwdriver gets embedded to tighten or loosen the screw from the implant (Figure 2).
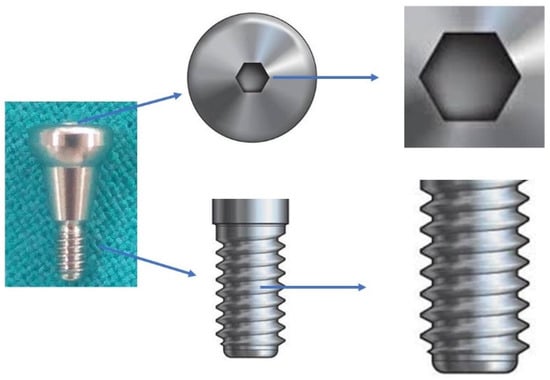
Figure 2.
Healing abutment hex surface and screw head.
2.4. Scanning Electron Microscope (SEM)
All the 12 healing abutments were examined using the SEM after repeated screwing and unscrewing. The healing abutments were again scanned after 4, 8, 16, 24, 32, 40, 80, 160, 320, and 400 insertion and removal cycles. Abutment screws were positioned on separate SEM pin-type mounts using conductive adhesive carbon tabs.
The healing abutments were gold-sputtered prior to SEM procedures to make the samples more electroconductive (Figure 3). The hex driver-healing abutment hex interface and screw thread of each healing abutment were analyzed under the SEM, and images were obtained at lower magnifications such that the focus area of each abutment could be visualized to obtain an accurate measurement of the surface distortion [25,26].

Figure 3.
Sample preparation for the scanning electron microscope (SEM).
2.5. Distortion Measurements
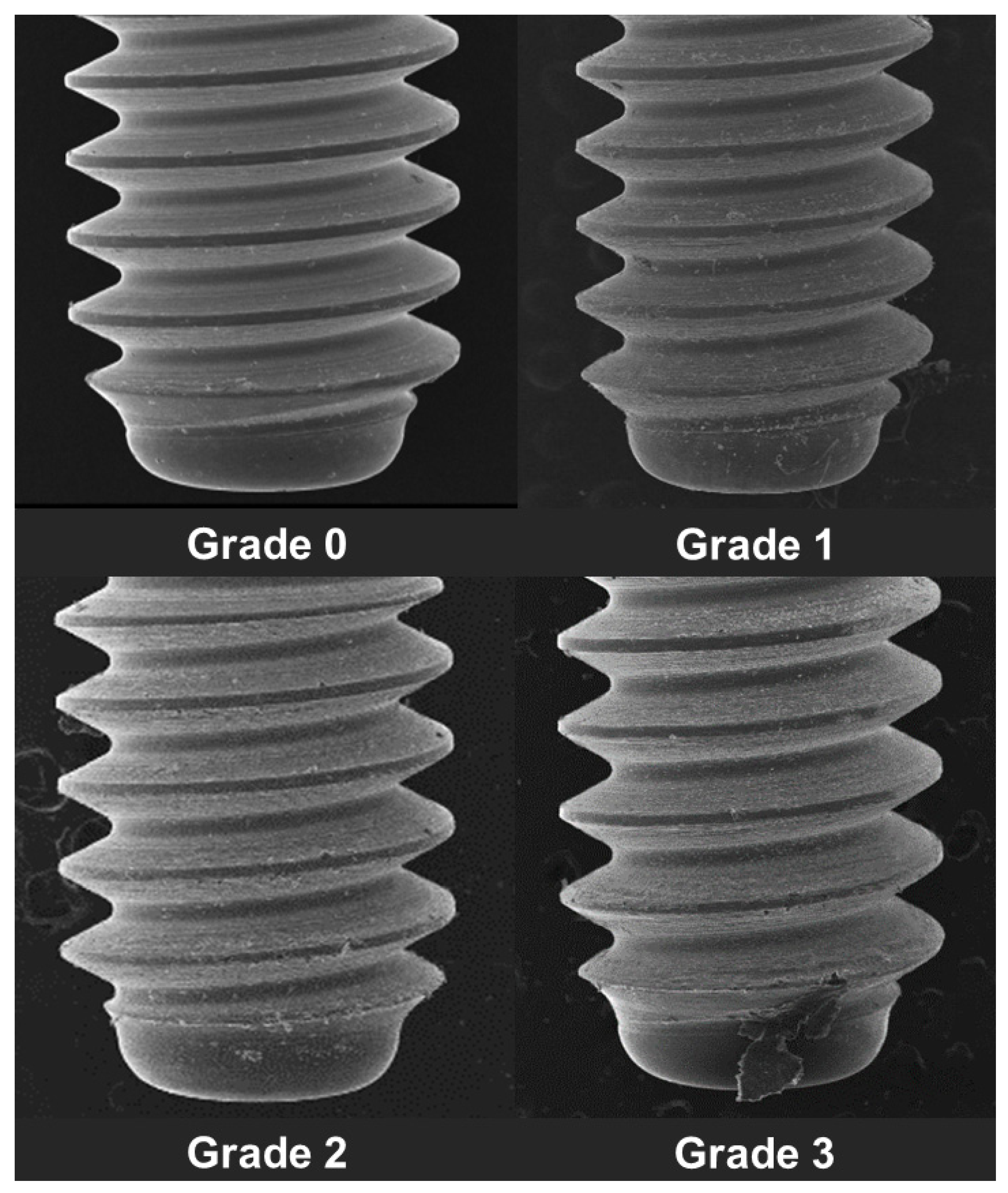
The surface distortion of the implant-healing abutment screw (hex thread) was determined under the SEM by using the following criteria using an ordinal scale (Figure 4) [27,28].
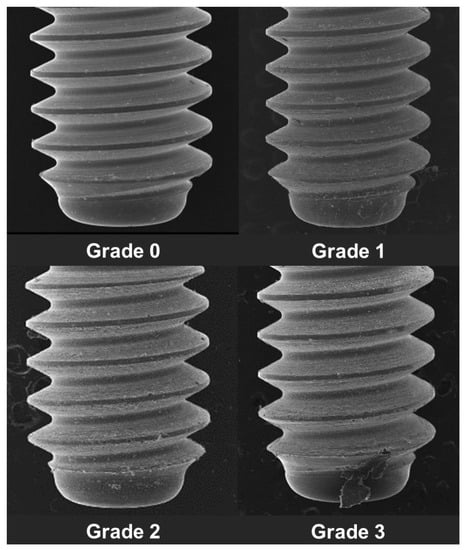
Figure 4.
Grading of implant-healing abutment hex surface distortion.
Grade 0: Thread surface intact with no visible surface irregularity.
Grade 1: Mild surface irregularities with pitting or slight cracking on the thread surface.
Grade 2: Moderate surface irregularities with deformed thread crests with pitting and slight cracking on the thread surface.
Grade 3: Severe surface irregularities with advanced deformation of thread crests.
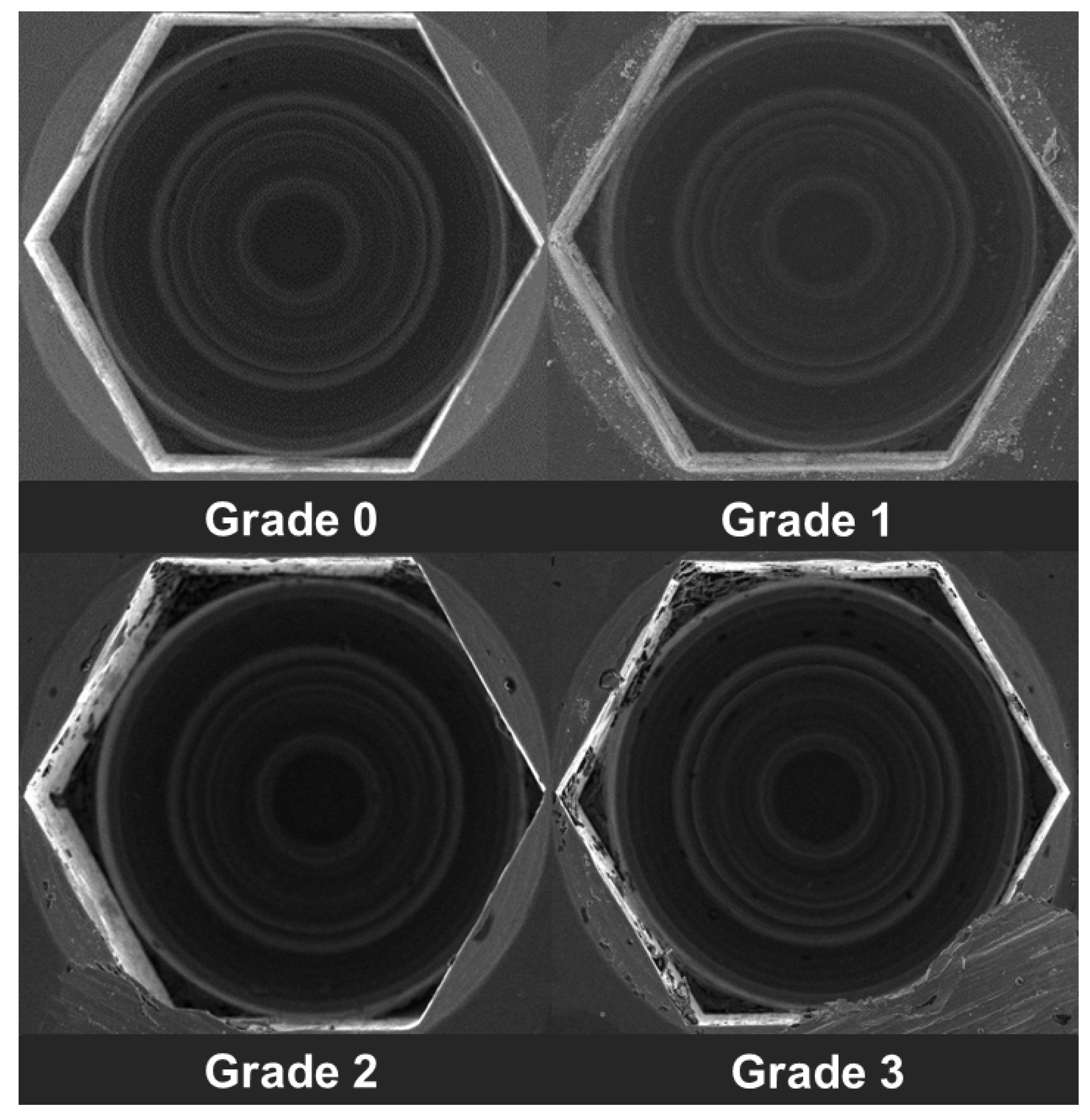
The implant-healing abutment screw head distortion was determined under SEM were determined by using the following criteria using an ordinal scale (Figure 5) [27,28].
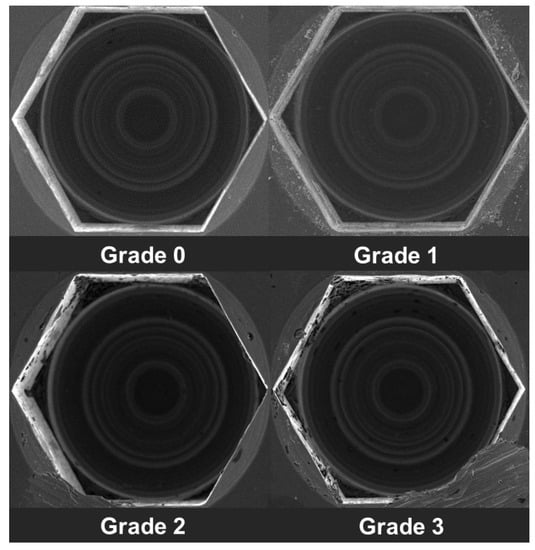
Figure 5.
Grading of implant-healing abutment screw head distortion.
Grade 0: Screw head intact with no visible surface irregularity.
Grade 1: Mild surface irregularities with pitting or slight cracking on the screw head.
Grade 2: Moderate surface irregularities with deformed screw head with pitting and slight cracking.
Grade 3: Severe surface irregularities with advanced deformation of the screw head.
2.6. Statistics Analysis
Data were analyzed using SPSS 24.0 (SPSS, Chicago, IL, USA). Descriptive statistics were calculated. One-way ANOVA with post hoc using Tukey’s HSD test was performed to analyze the difference in distortion at different screwing-unscrewing times. Significance level was selected at p-value = 0.05. Only one researcher performed all the research procedures. Then, in the end, all data were verified by random measurements, and data were found valid.
3. Result
3.1. Healing Abutment Screw Thread
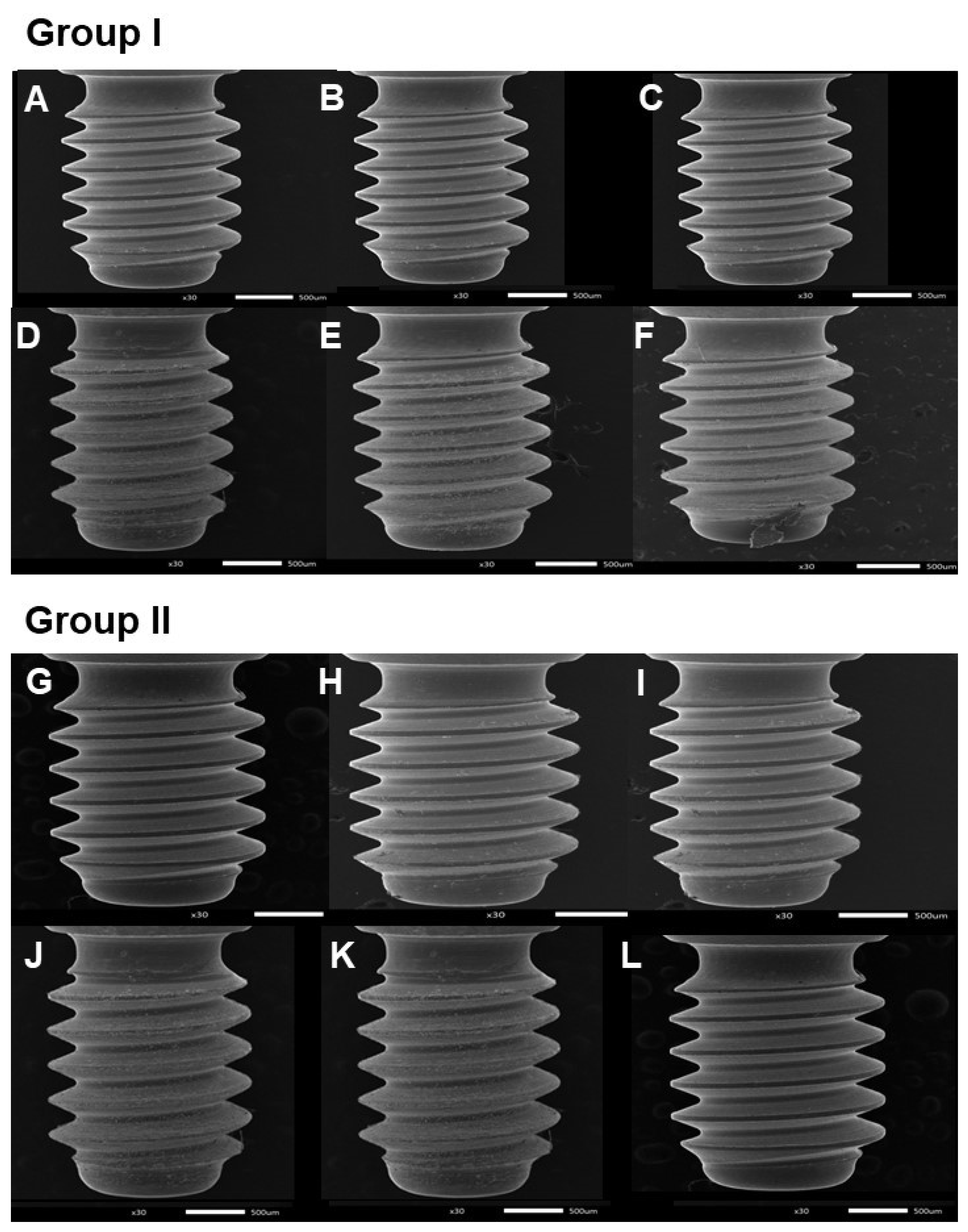
No surface distortions occurred at the healing abutment screw threads up to 16 cycles of screwing-unscrewing (Figure 6). However, after 24, 32, and 40 repeated cycles, mild surface irregularities with pitting or slight cracking on the thread surface of the healing abutment.
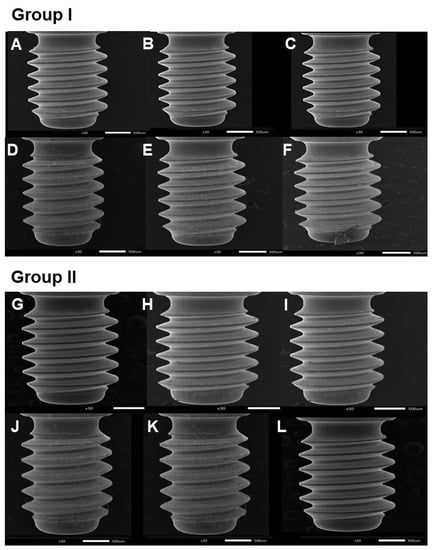
Figure 6.
Scanning electron microscope (SEM) images of healing abutment screw. Group I; (A) = before screwing-unscrewing, (B) = after 4 times of screwing-unscrewing, (C) = after 16 times of screwing-unscrewing, (D) = after 32 times of screwing-unscrewing, (E) = after 80 times of screwing-unscrewing, (F) = after 320 times of screwing-unscrewing. Group II; (G) = before screwing-unscrewing, (H) = after 8 times of screwing-unscrewing, (I) = after 24 times of screwing-unscrewing, (J) = after 40 times of screwing-unscrewing, (K) = after 160 times of screwing-unscrewing, and (L) = after 400 times of screwing-unscrewing.
The descriptive statistics of surface distortions of the healing abutments after the specific cycles of screwing-unscrewing are shown in Table 3. It was found that distortion healing abutments screws were seen after 32 screwing-unscrewing times.

Table 3.
Descriptive statistics of the mean scores of surface distortions of the healing abutments screw threads after the specific cycles of screwing-unscrewing.
Multiple comparisons (Table 4 and Table 5) show that there was a significant difference in the distortion (p-value < 0.05) after 24 times of repeated usage of the healing abutment.

Table 4.
Multiple comparisons of the surface distortions of the healing abutments screw threads after screwing-unscrewing in Group I (4, 16, 32, 80, 320).

Table 5.
Multiple comparisons of the surface distortions of the healing abutments screw threads after screwing-unscrewing in Group II (8, 24, 40, 160, 400).
3.2. Healing Abutment Screw Head
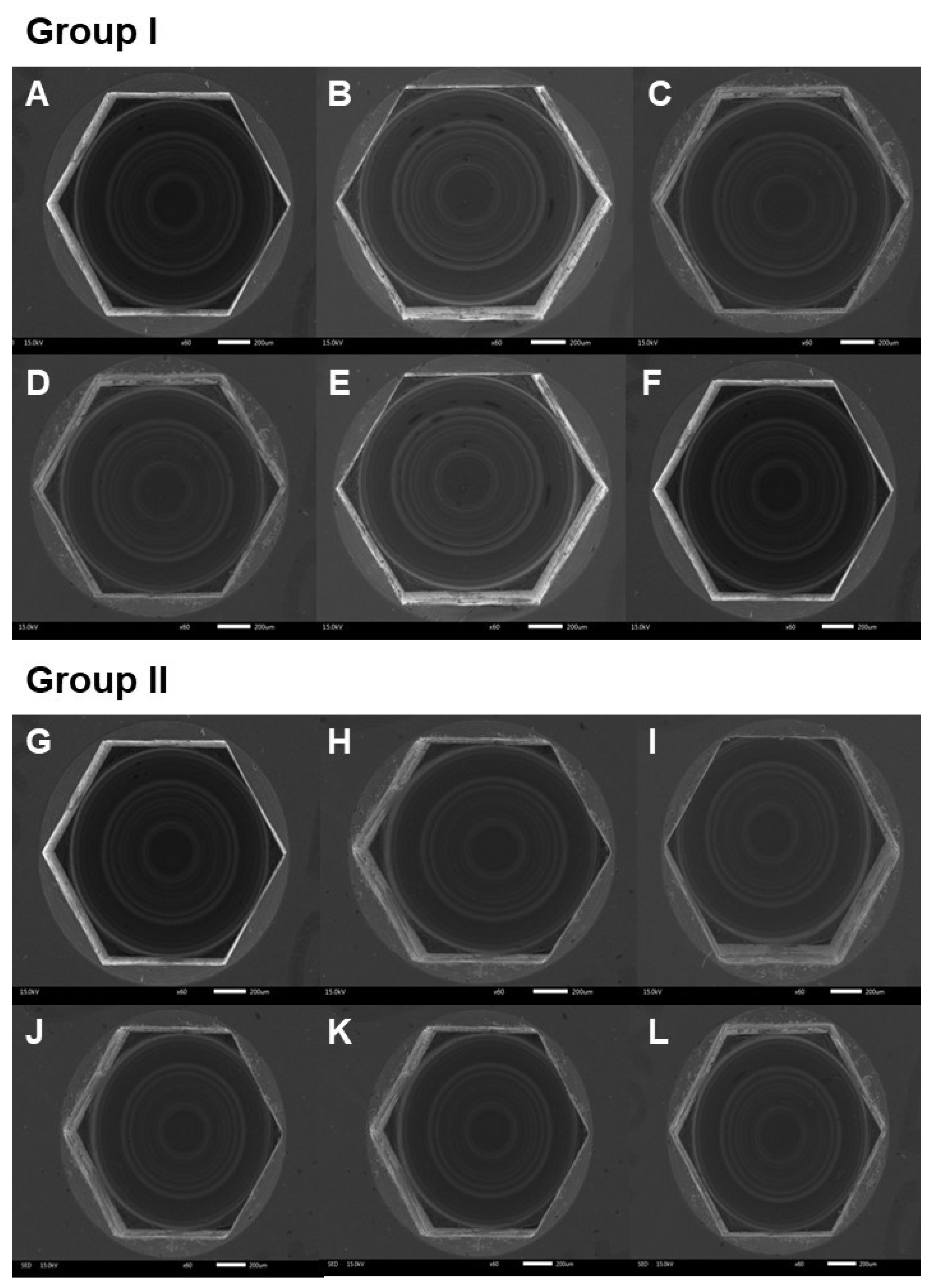
No surface distortions were observed at the healing abutment screw head at 4, 8, 16, 24, 32, 40, 80, 160, 320, and 400 cycles of screwing-unscrewing (Figure 7).
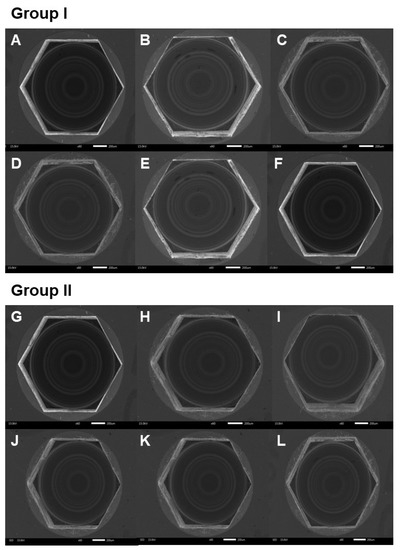
Figure 7.
Scanning electron microscope (SEM) images of healing abutment screw head. Group I; (A) = before screwing-unscrewing, (B) = after 4 times of screwing-unscrewing, (C) = after 16 times of screwing-unscrewing, (D) = after 32 times of screwing-unscrewing, (E) = after 80 times of screwing-unscrewing, (F) = after 320 times of screwing-unscrewing. Group II; (G) = before screwing-unscrewing, (H) = after 8 times of screwing-unscrewing, (I) = after 24 times of screwing-unscrewing, (J) = after 40 times of screwing-unscrewing, (K) = after 160 times of screwing-unscrewing, and (L) = after 400 times of screwing-unscrewing.
4. Discussion
We aimed to examine if repetitive screwing and unscrewing could affect the surface characteristics of the healing abutment. This is the first study to investigate the same to the best of our knowledge. The null hypothesis is rejected, and there are some surface changes following the screwing-unscrewing of healing abutment on the implant hex surface and screw head. Various methods to measure the surface wear are the 2D surface profilometry [29,30], SEM [31,32], 3D images superimposition using computer software [33,34], wear volume calculation using 3D images from focus variation microscopy [30] and wear particle characterization [35]. Stress distribution analysis can be performed from the finite element (FE) study [36]. However, in our study, 3D image superimposition was not a suitable method as the 3D scan images using Trios 3 (3Shape Dental Systems, Copenhagen, Denmark) were not of adequate quality due to the small size of the healing abutment hex, and the 3D scan cannot capture the hex threads. This is similar to the case of the light profilometer. Due to the hex thread shape, contact profilometers were also not suitable. Finally, wear volume and wear particle characterization were also not suitable due to the implant-healing abutment connection. Hence, we used SEM to analyze the wear of the healing abutment hex.
From this study, the microscopic pictographs confirmed this at higher resolution taken after recurring cycles, in which we observed thread and hex driver insertion surface distortion of healing abutments. We also found that the abutment removal torque gradually lowed than the insertion torque with increased repetitive screw unscrew cycles. These results could be explained based on the behavior of prosthesis abutment and hence would be discussed accordingly henceforth.
The friction helps in the retention of the restoration, contributes the joint stability, and resists screw loosening. Increasing screw insertion cycles decreases the friction between the screw and internal threads of the implant. We observed that after 24, 32, and 40 times repeated cycling of loosening and tightening of healing abutment causes mild surface irregularities with pitting or slight cracking on the thread surface of healing abutment occurring in all the tested healing abutments. This has been confirmed by SEM analysis that increasing screw closure cycles caused changes in the surface of the screw. The clinical implications of the screwing and unscrewing are shown in Table 6. It is not recommended to use the same healing abutment after 8–10 patients.

Table 6.
The clinical implications of the times of screwing and unscrewing in patients.
Our findings were in concordance with the results of Delben et al. [16], Carsdosa et al. [17], and Arshad et al. [23], who observed screw loosening and reduced torque after cyclic mechanical retightening. This could be due to the mechanical galling of metal surfaces due to their repetitive adherence to each other.
Another factor responsible could be the brittleness of titanium screws due to the body-centric cubic crystal structure making them more vulnerable to distortion [17]. Our findings further confirm those of Weiss et al. [25], Ricciardi Coppedê et al. [26], and Kim et al. [27], who also demonstrated that frequent mechanical retightening causes retention loss of stability torque.
Assunção et al. [37] studied the maintenance of tightening torque in various retention screw types of implant crowns and found that all screws exhibited a reduction in the detorque. The Ti screw showed the highest torque, whereas the gold-coated screw and the Ti screw with TiAlN coating showed the lowest torque. Similarly, Pardal-Peláez and Montero [38] studied the preload loss of the abutment screws in internal and external connections of dental implants, and they mentioned that internal connection with morse taper resisted cyclic loading of screw loosening.
The coefficient of friction among two metals is maintained by their intrinsic metallurgic properties and the mechanized process, which determines their geometric design and surface texture, which might be the reason previous studies observed differences in pre-facture torque value of abutments from different brands and within the same brand, and different shipments as well [24,25].
In a clinical setting, surface distortion could lead to the formation of micro gaps, causing microleakage of bacterial substrates or accidental slippage of the abutment in the oral cavity, which might lead to its aspiration [39,40].
The mechanical properties of the implant and the screwdriver (Table 2) can affect the distortion of the healing abutment due to the friction while screwing and unscrewing the healing abutment. In our study, the implants and healing abutments have similar mechanical properties as they were made from similar materials (titanium grade 4), whereas the mechanical properties of the screwdriver were lower mechanical as they were made from stainless steel. Hence, we assumed that the implant and screwdriver have no or very less effect on the distortion of the healing abutment hex and screw head.
This study can be extended to study the wear by advanced imaging methods in the future. In addition, the type of stress distribution can be studied using the FE study. The in vitro study design of the present study is one of its potential limitations as it could not simulate the exact biologic surroundings of the oral cavity. Thus, the findings should be validated in a clinical condition. The decontamination (autoclaving) of the healing abutments is performed in between repeated use [13], but we did not do the decontamination as this study is an in vitro study. Moreover, it has been shown that in SEM analysis, there were no detectable differences in the surface of Ti healing abutments the following decontamination using autoclaving, chemicals, or air polishing. In addition, only a single implant brand has been tested in our study, which could not justify the behavior of other implant systems. Finally, in this study, multiple screw insertion cycles and constant friction were not assumed. We could not perform this study in more samples due to the limitations of the research budget and time. In further studies, proper design, the passive fit of the prosthesis, and the correct patient selection are vital, controlling and treating the possible para functions and occlusal overloads.
5. Conclusions
Within the limitation of this study, it can be concluded that repeated screwing and unscrewing of the implant-healing abutments causes damage to the healing abutment hex surface. The distortion of healing abutments screws was seen after 32 times screwing and unscrewing. No surface distortions were observed on the healing abutment screw head until 400 times of screwing and unscrewing. Hence, the clinician should be cautious while using the healing abutments repeatedly.
Author Contributions
Conceptualization, N.W.; methodology, C.P., B.P.B., A.R., N.W. and D.R.; software, C.P., B.P.B., A.R. and D.R.; validation, B.P.B. and D.R.; formal analysis, C.P., B.P.B. and D.R.; investigation, C.P.; resources, C.P. and D.R.; data curation, B.P.B., A.R. and D.R.; writing—original draft preparation, C.P.; writing—review and editing, B.P.B. and D.R.; visualization, C.P. and D.R.; supervision, B.P.B., A.R., N.W. and D.R.; project administration, D.R.; funding acquisition, N.W. and D.R. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by Walailak University International College of Dentistry Research Fund, award number 07/2564.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank Pokpong Amornvit for the research consultation and the ideas for this research study. We would also like to acknowledge Biomate Medical Devices Technology Co. for the support for this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Amornvit, P.; Rokaya, D.; Bajracharya, S.; Keawcharoen, K.; Supavanich, W. Management of obstructive sleep apnea with implant retained mandibular advancement device. World J. Dent. 2014, 5, 184–189. [Google Scholar] [CrossRef]
- Cochran, D.L.; Morton, D.; Weber, H.P. Consensus statements and recommended clinical procedures regarding loading protocols for endosseous dental implants. Int. J. Oral Maxillofac. Implant. 2004, 19, 109–113. [Google Scholar]
- Suphangul, S.; Rokaya, D.; Kanchanasobhana, C.; Rungsiyakull, P.; Chaijareenont, P. Peek biomaterial in long-term provisional implant restorations: A review. J. Funct. Biomater. 2022, 13, 33. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.T.; Buser, D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int. J. Oral Maxillofac. Implant. 2009, 24, 186–217. [Google Scholar]
- Cakan, U.; Delilbasi, C.; Er, S.; Kivanc, M. Is it safe to reuse dental implant healing abutments sterilized and serviced by dealers of dental implant manufacturers? An in vitro sterility analysis. Implant. Dent. 2015, 24, 174–179. [Google Scholar] [CrossRef]
- Wadhwani, C.; Schonnenbaum, T.R.; Audia, F.; Chung, K.H. In-vitro study of the contamination remaining on used healing abutments after cleaning and sterilizing in dental practice. Clin. Implant Dent. Relat. Res. 2016, 18, 1069–1074. [Google Scholar] [CrossRef]
- Stacchi, C.; Berton, F.; Porrelli, D.; Lombardi, T. Reuse of implant healing abutments: Comparative evaluation of the efficacy of two cleaning procedures. Int. J. Prosthodont. 2018, 31, 161–162. [Google Scholar] [CrossRef]
- Park, I.S.; Won, S.; Bae, T.; Song, K.; Park, C.; Eom, T.; Jeong, C. Fatigue characteristics of five types of implant-abutment joint designs. Met. Mater. Int. 2008, 14, 133–138. [Google Scholar] [CrossRef]
- Jorge, J.R.; Barao, V.A.; Delben, J.A.; Assuncao, W.G. The role of implant/abutment system on torque maintenance of retention screws and vertical misfit of implant-supported crowns before and after mechanical cycling. Int. J. Oral Maxillofac. Implant. 2013, 28, 415–422. [Google Scholar] [CrossRef]
- Binon, P.P. The effect of implant/abutment hexagonal misfit on screw joint stability. Int. J. Prosthodont. 1996, 9, 149–160. [Google Scholar]
- Lopes, P.A.; Carreiro, A.F.P.; Nascimento, R.M.; Vahey, B.R.; Henriques, B.; Souza, J.C.M. Physicochemical and microscopic characterization of implant-abutment joints. Eur. J. Dent. 2018, 12, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Tzenakis, G.K.; Nagy, W.W.; Fournelle, R.A.; Dhuru, V.B. The effect of repeated torque and salivary contamination on the preload of slotted gold implant prosthetic screws. J. Prosthet. Dent. 2002, 88, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Chew, M.; Tompkins, G.; Tawse-Smith, A.; Waddell, J.N.; Ma, S. Reusing titanium healing abutments: Comparison of two decontamination methods. Int. J. Prosthodont. 2018, 31, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Kyaw, T.T.; Hanawa, T.; Kasugai, S. Investigation of different electrochemical cleaning methods on contaminated healing abutments in vitro: An approach for metal surface decontamination. Int. J. Implant Dent. 2020, 6, 64. [Google Scholar] [CrossRef] [PubMed]
- Rokaya, D.; Srimaneepong, V.; Wisitrasameewon, W.; Humagain, M.; Thunyakitpisal, P. Peri-implantitis update: Risk indicators, diagnosis, and treatment. Eur. J. Dent. 2020, 14, 672–682. [Google Scholar] [CrossRef]
- Delben, J.A.; Gomes, E.A.; Barão, V.A.; Assunção, W.G. Evaluation of the effect of retightening and mechanical cycling on preload maintenance of retention screws. Int. J. Oral Maxillofac. Implant. 2011, 26, 251–256. [Google Scholar]
- Cardoso, M.; Torres, M.F.; Lourenço, E.J.; de Moraes Telles, D.; Rodrigues, R.C.; Ribeiro, R.F. Torque removal evaluation of prosthetic screws after tightening and loosening cycles: An in vitro study. Clin. Oral Implant. Res. 2012, 23, 475–480. [Google Scholar] [CrossRef]
- Masa, R.; Braunitzer, G. Titanium and its alloys in dental implantology. Implants 2017, 18, 6–10. [Google Scholar]
- Nicholson, J.W. Titanium alloys for dental implants: A review. Prosthesis 2020, 2, 100–116. [Google Scholar] [CrossRef]
- Liu, X.; Chen, S.; Tsoi, J.; Matinlinna, J. Binary titanium alloys as dental implant materials—A review. Regen. Biomater. 2017, 4, 315–323. [Google Scholar] [CrossRef]
- Monjo, M.; Petzold, C.; Ramis, J.M.; Lyngstadaas, S.P.; Ellingsen, J.E. In vitro osteogenic properties of two dental implant surfaces. Int. J. Biomater. 2012, 2012, 181024. [Google Scholar] [CrossRef] [PubMed]
- Laino, L.; La Noce, M.; Fiorillo, L.; Cervino, G.; Nucci, L.; Russo, D.; Herford, A.S.; Crimi, S.; Bianchi, A.; Biondi, A.; et al. Dental pulp stem cells on implant surface: An in vitro study. BioMed Res. Int. 2021, 2021, 3582342. [Google Scholar] [CrossRef]
- Arshad, M.; Mahgoli, H.; Payaminia, L. Effect of repeated screw joint closing and opening cycles and cyclic loading on abutment screw removal torque and screw thread morphology: Scanning electron microscopy evaluation. Int. J. Oral Maxillofac. Implant. 2018, 33, 31–40. [Google Scholar] [CrossRef]
- Mlikota, M.; Schmauder, S. On the critical resolved shear stress and its importance in the fatigue performance of steels and other metals with different crystallographic structures. Metals 2018, 8, 883. [Google Scholar] [CrossRef]
- Weiss, E.I.; Kozak, D.; Gross, M.D. Effect of repeated closures on opening torque values in seven abutment-implant systems. J. Prosthet. Dent. 2000, 84, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Ricciardi Coppedê, A.; de Mattos Mda, G.; Rodrigues, R.C.; Ribeiro, R.F. Effect of repeated torque/mechanical loading cycles on two different abutment types in implants with internal tapered connections: An in vitro study. Clin. Oral Implant. Res. 2009, 20, 624–632. [Google Scholar] [CrossRef]
- Kim, K.S.; Lim, Y.J. Axial displacements and removal torque changes of five different implant-abutment connections under static vertical loading. Materials 2020, 13, 699. [Google Scholar] [CrossRef] [PubMed]
- Byrne, D.; Jacobs, S.; O’Connell, B.; Houston, F.; Claffey, N. Preloads generated with repeated tightening in three types of screws used in dental implant assemblies. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2006, 15, 164–171. [Google Scholar] [CrossRef]
- Roux, S.L.; Boher, C.; Penazzi, L.; Dessain, C.; Tavernier, B. A methodology and new criteria to quantify the adhesive and abrasive wear damage on a die radius using white light profilometry. Tribol. Int. 2012, 52, 40–49. [Google Scholar] [CrossRef][Green Version]
- Hatos, I.; Hargitai, H.; Solecki, L. Study of 2d and 3d methods for worn surface analysis of tool materials. Acta Tech. Jaurinensis 2015, 8, 165–178. [Google Scholar] [CrossRef]
- Subha, N.; Sikri, V.K. Comparative evaluation of surface changes in four ni-ti instruments with successive uses—An sem study. J. Conserv. Dent. 2011, 14, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, S.; Howes, M.A.H.; Johari, O. A scanning electron microscopic study of wear surfaces. J. Miner. Met. Mater. Soc. 1970, 22, 49–60. [Google Scholar] [CrossRef]
- Anh, J.W.; Park, J.M.; Chun, Y.S.; Kim, M.; Kim, M. A comparison of the precision of three-dimensional images acquired by 2 digital intraoral scanners: Effects of tooth irregularity and scanning direction. Korean J. Orthod. 2016, 46, 3–12. [Google Scholar] [CrossRef]
- Torfeh, T.; Hammoud, R.; Perkins, G.; McGarry, M.; Aouadi, S.; Celik, A.; Hwang, K.P.; Stancanello, J.; Petric, P.; Al-Hammadi, N. Characterization of 3d geometric distortion of magnetic resonance imaging scanners commissioned for radiation therapy planning. Magn. Reson. Imaging 2016, 34, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, P.; Stachowiak, G.W. Characterization of surface topography of wear particles by sem stereoscopy. Wear 1997, 206, 39–52. [Google Scholar] [CrossRef]
- Amornvit, P.; Rokaya, D.; Keawcharoen, K.; Thongpulsawasdi, N. Stress distribution in implant retained finger prosthesis: A finite element study. J. Clin. Diagn. Res. 2013, 7, 2851–2854. [Google Scholar] [CrossRef]
- Assunção, W.G.; Delben, J.A.; Tabata, L.F.; Barão, V.A.; Gomes, E.A.; Garcia, I.R., Jr. Preload evaluation of different screws in external hexagon joint. Implant Dent. 2012, 21, 46–50. [Google Scholar] [CrossRef]
- Pardal-Peláez, B.; Montero, J. Preload loss of abutment screws after dynamic fatigue in single implant-supported restorations. A systematic review. J. Clin. Exp. Dent. 2017, 9, e1355–e1361. [Google Scholar] [CrossRef]
- Bernardes, S.R.; da Gloria Chiarello de Mattos, M.; Hobkirk, J.; Ribeiro, R.F. Loss of preload in screwed implant joints as a function of time and tightening/untightening sequences. Int. J. Oral Maxillofac. Implant. 2014, 29, 89–96. [Google Scholar] [CrossRef]
- Kim, A.; Ahn, K.M. Endoscopic removal of an aspirated healing abutment and screwdriver under conscious sedation. Implant Dent. 2014, 23, 250–252. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).