Abstract
Cardiovascular diseases are the leading cause of death worldwide. Aging and/or metabolic stress directly impact the cardiovascular system. Over the last few years, the contributions of altered nicotinamide adenine dinucleotide (NAD+) metabolism to aging and other pathological conditions closely related to cardiovascular diseases have been intensively investigated. NAD+ bioavailability decreases with age and cardiometabolic conditions in several mammalian tissues. Compelling data suggest that declining tissue NAD+ is commonly related to mitochondrial dysfunction and might be considered as a therapeutic target. Thus, NAD+ replenishment by either genetic or natural dietary NAD+-increasing strategies has been recently demonstrated to be effective for improving the pathophysiology of cardiac and vascular health in different experimental models, as well as human health, to a lesser extent. Here, we review and discuss recent experimental evidence illustrating that increasing NAD+ bioavailability, particularly by the use of natural NAD+ precursors, may offer hope for new therapeutic strategies to prevent and treat cardiovascular diseases.
1. Introduction
Cardiovascular diseases are the leading cause of death worldwide according to the World Health Organization. Aging is a primary risk factor for many cardiovascular diseases. With the progressively aging population, the elevated prevalence of cardiovascular diseases undermines human health and longevity [1].
Mitochondrial dysfunction is a hallmark of metabolic decline during aging [2]. Nicotinamide adenine dinucleotide (NAD+) bioavailability decreases with age in a number of mammalian tissues, and evidence suggests that failing mitochondrial function is related to this decline [3,4]. Beyond aging, altered NAD+ metabolism levels have also been reported in obesity, diabetes mellitus, fatty liver disease, and hypertension [5]. NAD+ depletion is observed in several cardiovascular pathologies, including atherosclerosis, ischemia-reperfusion injury, cardiomyopathy, and heart failure (HF), which has prompted studies exploring its pathophysiological role in cardiovascular diseases [6]. In this regard, NAD+ decline prevention may represent an innovative therapeutic target in the management of cardiovascular diseases [7]. Accordingly, many studies have revealed that dietary administration of NAD+ precursors, such as tryptophan, nicotinic acid (NA, also termed niacin), nicotinamide (NAM), and nicotinamide riboside (NR), and its phosphorylated form, nicotinamide mononucleotide (NMN), efficiently raises the tissue NAD+ content in rodents and humans [8,9]. In particular, NAM, NMN, and NR administration has been reported to prevent obesity and improve glucose tolerance in mice [10,11,12,13,14] and favorably influenced fatty liver by reducing oxidative stress and inflammation in aged, diet-induced obese mice [15]. Conceivably, NAD+ precursors may protect the cardiovascular system [6,16].
NA is a vitamin B3 form that has been widely used in clinical practice to reduce the atherothrombotic cardiovascular risk by decreasing plasma triglycerides and increasing plasma high-density lipoprotein (HDL) cholesterol (HDL-C) [17]. NA interacts with the GPR109A receptor in immune cells, thereby blunting immune activation and protecting against inflammatory cell infiltration in age-related diseases [18]. Recent studies suggest that many physiological effects of NA on cardiovascular protection can be at least partly explained on the basis of its role as an NAD+ precursor [19]. However, a major problem with NA administration is adverse effects, which range from cutaneous flushing to effects linked to muscle, liver, and gastrointestinal toxicity [20]. Moreover, early reports supporting secondary cardiovascular preventive effects of NA were not confirmed by more recent, large prospective trials including 29,087 patients, the AIM-HIGH [21] and the HPS2-THRIVE [22], which were prematurely stopped due to a lack of efficacy in patients that were taking statins in the context of secondary prevention. Thus, these results do not, therefore, necessarily apply to primary cardiovascular prevention, but not such type of novel NA clinical trial seems to be planned at this point. In a recent study [23], NA also ameliorated wound healing and cardiac function after myocardial infarction via DP1-mediated M2 macrophage polarization and timely resolution of inflammation, thus suggesting that DP1 inhibition, as the agent used together with NA in the abovementioned large clinical trials, may attenuate the cardiovascular benefits of NA.
The potential benefits of other forms of vitamin B3 have also been studied, albeit more experimentally than at the clinical level. NAM, an amide vitamin B3 form, does not interact with the GPR109A receptor and is apparently free of NA-induced adverse side effects [7,8]. Treatment with both NAM and NA improved aneurysms in an experimental mouse model through GPR109A receptor-independent activity against this disease [24]. Unlike NA, NAM does not show strong lipid-lowering effects [19] but exerts antioxidant and anti-inflammatory effects [15,25]. Interestingly, NAM administration protected against beta pancreatic cell damage and loss and, thus, delayed the onset of diabetes mellitus type 1 in experimental models [26]. Although this effect was not reproduced in the ENDIT clinical trial [27], NAM administration at a dose of 1.2 g/m2 did not cause adverse effects (including flushing) similar to those attributed to NA. Recent data from our own group show that NAM prevents inflammation and atherosclerosis in experimental animals [25]. Similarly, some other related compounds, such as NR [28], NMN [9], and N-methylated NAM (me-NAM) [29,30], seem to protect against vascular damage.
Some evidence indicates that NAM or other related compounds that act as a source of NAD+ might be of interest in the context of cardiomyopathy and heart failure (HF) [31].
Thus, this comprehensive review provides updated, critically revised information on the potential therapeutic effects of boosting NAD+ metabolism in animal models of cardiovascular diseases and its potential translation into clinical practice. In particular, we mainly focus on the role of NAD+-increasing strategies based on the use of NAD+ precursors. Other determinants of NAD+ metabolism also lead to NAD+ elevations; however, owing to space limitations, genetically modified mouse models are not extensively discussed in this review. Furthermore, although various pharmacological strategies have also been reported to boost NAD+ levels, including the use of activators and inhibitors of NAD+ biosynthesis, we focus on the therapeutic potential of direct natural NAD+ precursors in cardiovascular health.
2. Preferential Physiological Sources of NAD+
NAD+ is an essential cofactor in all living cells [32]. Abundant amounts of this metabolite are found in different cellular compartments, including mitochondria, cytoplasm, and nuclei. NAD+ plays a key physiological role in modulating many biological processes and cellular metabolism pathways, including glycolysis, fatty acid β-oxidation, and the tricarboxylic acid cycle [33,34]. NAD+ exists in two forms—the oxidized form (NAD+) and the reduced form (NADH). The latter is generated by NAD+ accepting high-energy electrons from glycolytic and tricarboxylic acid intermediates and acts as a primary electron donor in ATP production by feeding electrons into complex I of the electron transport chain to drive mitochondrial oxidative phosphorylation [35].
2.1. NAD+ Sources
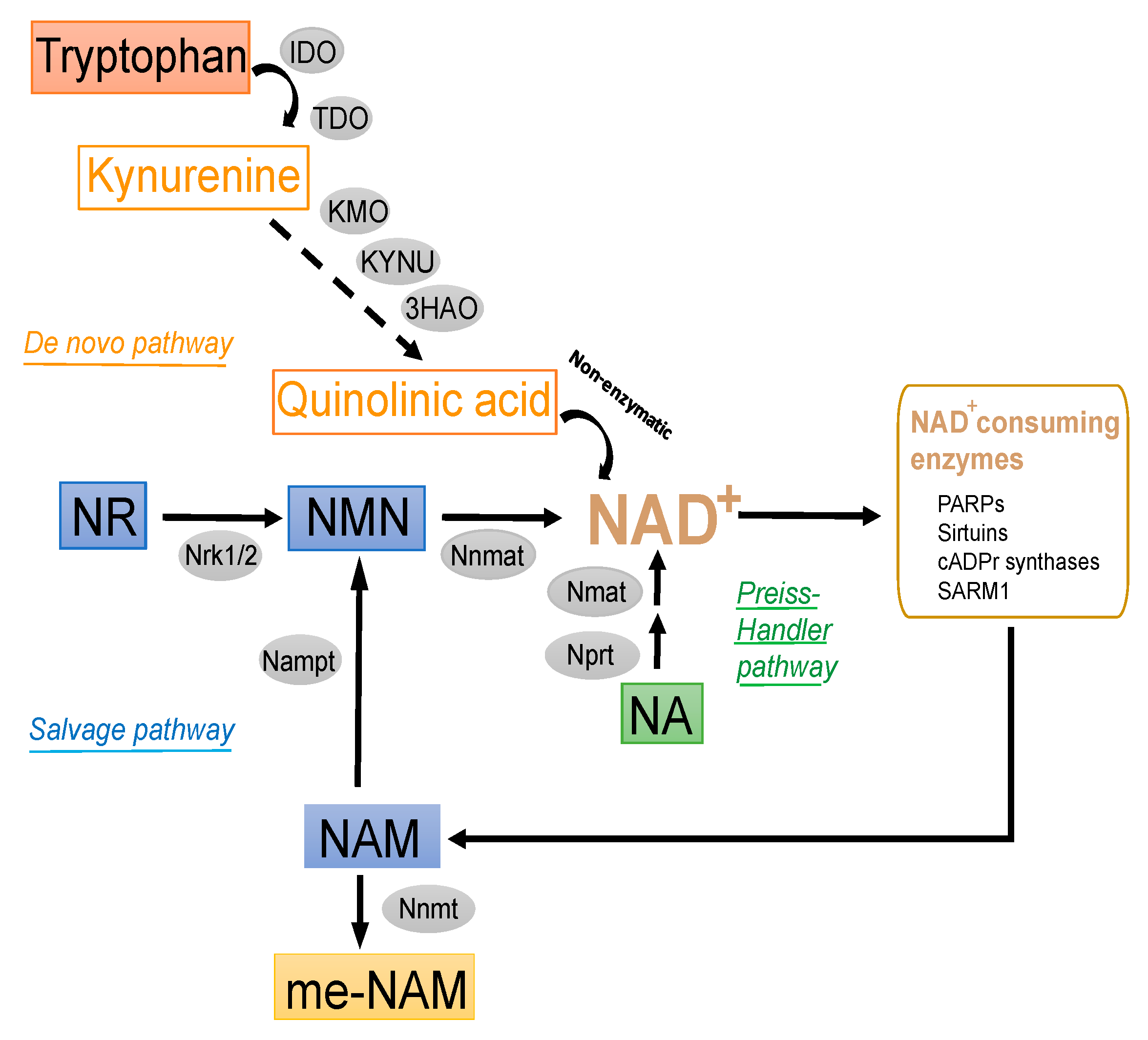
Because NAD+-dependent signaling reactions (protein deacetylation by sirtuins, intracellular calcium signaling, and mono-/poly-ADP-ribosylation) involve degradation of the dinucleotide, a constant supply of this molecule is required to reach cellular homeostasis. NAD+ precursors are commonly ingested from dietary sources. Intracellular NAD+ can be technically produced through distinct metabolic pathways (Figure 1): (i) the de novo pathway from tryptophan, (ii) the salvage synthesis pathway from NAM and NR, and (iii) the Preiss-Handler pathway from NA [32,36]. Additionally, intermediate molecules from these NAD+ biosynthetic pathways, such as NMN, can also be direct substrates for NAD+ synthesis [33].
Figure 1.
NAD+ precursor metabolism and NAD+-consuming enzymes. Tryptophan, NA, NAM, and NR can be used by different pathways to obtain NAD+. NAD+ formation can be obtained de novo from tryptophan. The first step relies in the conversion of tryptophan to N-formylkynurenine by either indoleamine 2,3-dioxygenase (IDO) or tryptophan 2,3-dioxygenase (TDO). N-formylkynurenine can be converted into quinolinic acid and NAD+ thereafter. NAD+ synthesis from NA is initiated by the NA phosphoribosyltransferase (NPRT), which uses phosphoribosyl pyrophosphate (PRPP) to form NAMN prior to NAD+ synthesis (Preiss-Handler pathway). Finally, the synthesis of NAD+ can be also possible using NAM or NR via the Salvage pathway. This pathway just needs 2 steps for each precursor. NAM is converted by the rate-limiting nicotinamide phosphoribosyltransferase (NAMPT) to form NMN, also using PRPP as a co-substrate. NMN can be also formed by NR phosphorylation through the action of NR kinases (NRK1-2). Finally, the conversion of NMN to NAD+ is eventually catalyzed by cellular NMN adenylyl transferase (NMNAT1-3) enzymes. Abbreviations used were: 3HAO: 3-hydroxyanthranilate 3,4-dioxygenase; IDO: indoleamine 2,3-dioxygenase; KMO: kynureine monooxygenase; KYNU: kynureinase; NAD: nicotinamide adenine dinucleotide; NA: nicotinic acid; NAM: nicotinamide; NMN: nicotinamide mononucleotide; Nampt: nicotinamide phosphoribosyltransferase; Nnmat: nicotinamide mononucleotide adenylyltransferase; NR: nicotinamide riboside; Nrk1/2: NR kinase 1, 2; Nmat: nicotinate mononucleotide adenyltransferase; Nprt: nicotinate phosphoribosyl-transferase; Nnmt: nicotinamide methyltransferase; TDO: tryptophan 2,3-dioxygenase.
2.1.1. De Novo Synthesis Pathway
The kynurenine pathway drives de novo synthesis of NAD+ from the essential amino acid tryptophan [37] (Figure 1). This metabolic pathway is the dominant route of metabolism for absorbed tryptophan [38], accounting for more than 95% of daily metabolized tryptophan. However, tryptophan is considered an inefficient source of NAD+, as it requires 8 enzymatic reactions and, thus, has lower therapeutic value than other precursors, including NAM, NR, and NMN [39]. Therefore, these last molecules can be considered much more physiologically preferred NAD+ precursors than tryptophan [40]. Although the potential function of the kynurenine pathway of tryptophan metabolism to produce NAD+ has received little attention, emerging evidence suggests potential interplay between this pathway and cardiovascular disease [37,41]. In line with this, the kynurenine pathway has been recently regarded as a potential source of NAD+ in macrophages [42].
2.1.2. Salvage Pathway
NMN is a major intermediate of NAD+ (Figure 1). The salvage synthesis of NMN from NAM is catalyzed by nicotinamide phosphoribosyltransferase (NAMPT), whereas the synthesis of NMN from NR is catalyzed by intracellular NR kinases (NRK1 and NRK2) [43]. Finally, NMN may be subsequently transformed into NAD+ by different subcellular forms of adenylyltransferases (NMNAT1-3) [44].
2.1.3. Other Modulators of Intracellular NAD+ Pools
In addition to these enzymes, others may also influence the tissue abundance of NAD+ (Figure 1). Specifically, nicotinamide N-methyltransferase (NNMT) catalyzes the N-methylation reaction of NAM and other analogous molecules using S-adenosyl methionine (SAM) as a donor of methyl groups [45] and produces me-NAM and S-adenosyl homocysteine (SAH) [39,40]. Recent reports suggest that NNMT may also act as a determinant of tissue NAD+ pools in vivo [43]. Interestingly, the subproduct me-NAM has been reported to exert anti-inflammatory, antioxidant, and antidiabetic effects in different experimental models [46,47,48,49,50].
2.2. Administration and Bioavailability of NAD+ Precursors
L-tryptophan can be safely supplemented in the diet [51]. This amino acid can be added directly to feedstuff and dissolved into drinking water [38]. As indicated previously, its availability is primarily governed by the kynurenine pathway, which may contribute to NAM production under dietary deficiency of this vitamin form [38].
NAM is highly soluble in water and is considered a safe food supplement in animal nutrition and the predominant circulating form of vitamin B3 in vivo [52]. Its safety margin is at least ten times the dietary requirements and use levels, and it can be administered orally by feeding or drinking (tap water) routes with similar bioequivalence rates. Oral NAM can be absorbed in the stomach and the small intestine either through passive diffusion or by Na+-dependent carrier-mediated facilitated transport mechanisms [52], with passive diffusion predominating at pharmacological doses. Similarly, NA absorption into the intestinal mucosa follows the same transport mechanisms as NAM. NA can be further metabolized via NA mononucleotide (NAMN) to form the NA analog of NAD+ through the Preiss-Handler pathway (Figure 1). NAD+ can then be enzymatically cleaved into NAM in the intestinal mucosa and then the liver. The latter tissues contain elevated amounts of NAD+-consuming enzymes, such as NAD+ glycohydrolase, that allow NAM synthesis from NAD+. NAM can be subsequently transported to tissues for the synthesis of NAD+ or its phosphorylated form (NADP+). The principal excretory product is the methylated, water-soluble metabolite me-NAM (Subsection: Other modulators of intracellular NAD+ pools) or some of its oxidation products [53].
NR has a good bioavailability [54]. Unlike NA and NAM, dietary NR cell uptake is mediated by a specific nucleoside transporter [55], where it is transformed into NAD+ through a distinct, two-step biosynthetic pathway.
In contrast to that of NR, the bioavailability of NMN is rather limited [56]. Indeed, extracellular sources of NMN do not efficiently cross the endothelial membrane and require previous dephosphorylation by CD73 (ecto-5′-nucleotidase) to generate NR or must be extracellularly metabolized to NAM by CD38 [57]. Interestingly, a specific NMN transporter (i.e., Slc12a8) exists in murine small intestinal epithelium [58]. This transporter is predominantly expressed in the small intestine and in white adipose tissue and the liver to a lesser extent. However, whether Slc12a8 can also be expressed by cells of the vasculature or cardiomyocytes remains to be determined. NMN can also be obtained from NAM by extracellular NAMPT (eNAMPT, also termed visfatin). In endothelial cells, this conversion process requires the participation of phosphoribosyl-1-pyrophosphate (PRPP) [8]. Finally, extracellular NAD+ can be directly transported into cardiomyocytes through connexin 43 (i.e., Cx43) channels [59]. Taken together, these findings suggest that intracellular transport of NAD+ and NMN may be cell-specific and rely on different transporters.
2.3. NAD+-Consuming Enzymes as Determinants of the NAD+ Content
In the last two decades, beyond its important contribution to intermediate metabolism, NAD+ has also been shown to influence multiple signaling pathways (reviewed in detail in ref. [8]). Indeed, NAD+ can also be used by different protein regulators, including NAD+-dependent histone deacetylases (also termed sirtuins), which regulate the cellular mitohormetic response and, thus, favorably influence energy metabolism (reviewed in detail in ref. [33]). Moreover, several families of ADP-ribose synthesizing enzymes—mono-(ADP-ribose) polymerases (MARPs) and poly-(ADP-ribose) polymerases (PARPs)—also require NAD+ to specifically catalyze mono-/poly-ADP-ribosylation reactions of target proteins [60]. These enzymes are generally considered DNA damage sensors because of their participation in DNA repair, replication and transcription and the chromatin structure, among other functions [33,34,61,62,63,64]. Other enzymes, such as NAD+-dependent glycohydrolases (i.e., CD38 and CD157) involved in calcium signaling [65,66] and regulation of the cell cycle [66,67,68], use NAD+ to produce the second messenger cyclic-ADP-ribose and ADP-ribosyl cyclase-produced glycoproteins [69].
3. In Vitro Cardioprotective Effects of NAD+ Sources
Experimental evidence suggests that oxidative stress and inflammation are mechanistically interconnected in driving cardiac and vascular diseases, and both may contribute to disease progression [70]. Increased vascular reactive oxygen species can react with cellular molecules and organelles, which become dysfunctional, leading to inflammation and endothelial dysfunction with devastating consequences on the vasculature and cardiac tissue. Moreover, impaired vascular reactive oxygen species homeostasis and inflammation may be reciprocally exacerbated, thereby resulting in a vicious and chronic cycle.
Current applications for successful control of enhanced oxidative stress and inflammation for the management of such complex chronic diseases are still elusive, partly due to the extensive diversity of oxidative stress pathways and inflammatory cells that can either be cardioprotective or cause cardiac damage. In this context, we next focus on relevant recent research evidence to examine some cardioprotective properties shown by vitamin B3 forms or intermediates in appropriate cell models of disease.
3.1. Ex Vivo Properties of NAD+ Precursors Relevant to Cardiovascular Diseases
Reactive oxygen species, including the superoxide anion (O2•−) and the nitric oxide radical (NO•), are critical bioreactive signaling molecules that may influence both cellular homeostasis and disease. Under physiological conditions, the intracellular pool of such reactive oxygen species is controlled by an intricate array of antioxidant defense systems that include superoxide dismutases, catalase, the glutathione peroxidase/reductase system, and the peroxiredoxin/thioredoxin system [71]. Under pathological conditions, elevated reactive oxygen species can overwhelm cellular antioxidant defenses, impair reactive oxygen species scavenging and, therefore, lead to cardiac dysfunction [72,73,74,75,76].
In addition to the enzymatic antioxidant systems, certain molecules (identified as antioxidants) may serve as direct metabolic scavengers of electrons from reactive radicals and, thus, confer direct protection to biomolecules from oxidative damage by virtue of their chemical ability to accept/donate electrons. In particular, NAM may directly function as an O2•− radical scavenger and inhibit the generation of free radicals (e.g., O2•−, NO•, and HCLO•) [77] and prevent protein and lipid oxidation in vitro [78]. Importantly, this scavenging ability may paradoxically enable some vitamins with recognized antioxidant properties to function as pro-oxidants under certain circumstances [79,80,81]. Notably and in contrast to other vitamins with antioxidant abilities, such as vitamins A and C, vitamin B3 (NA) did not induce oxidative damage in vitro at physiologically relevant concentrations [82].
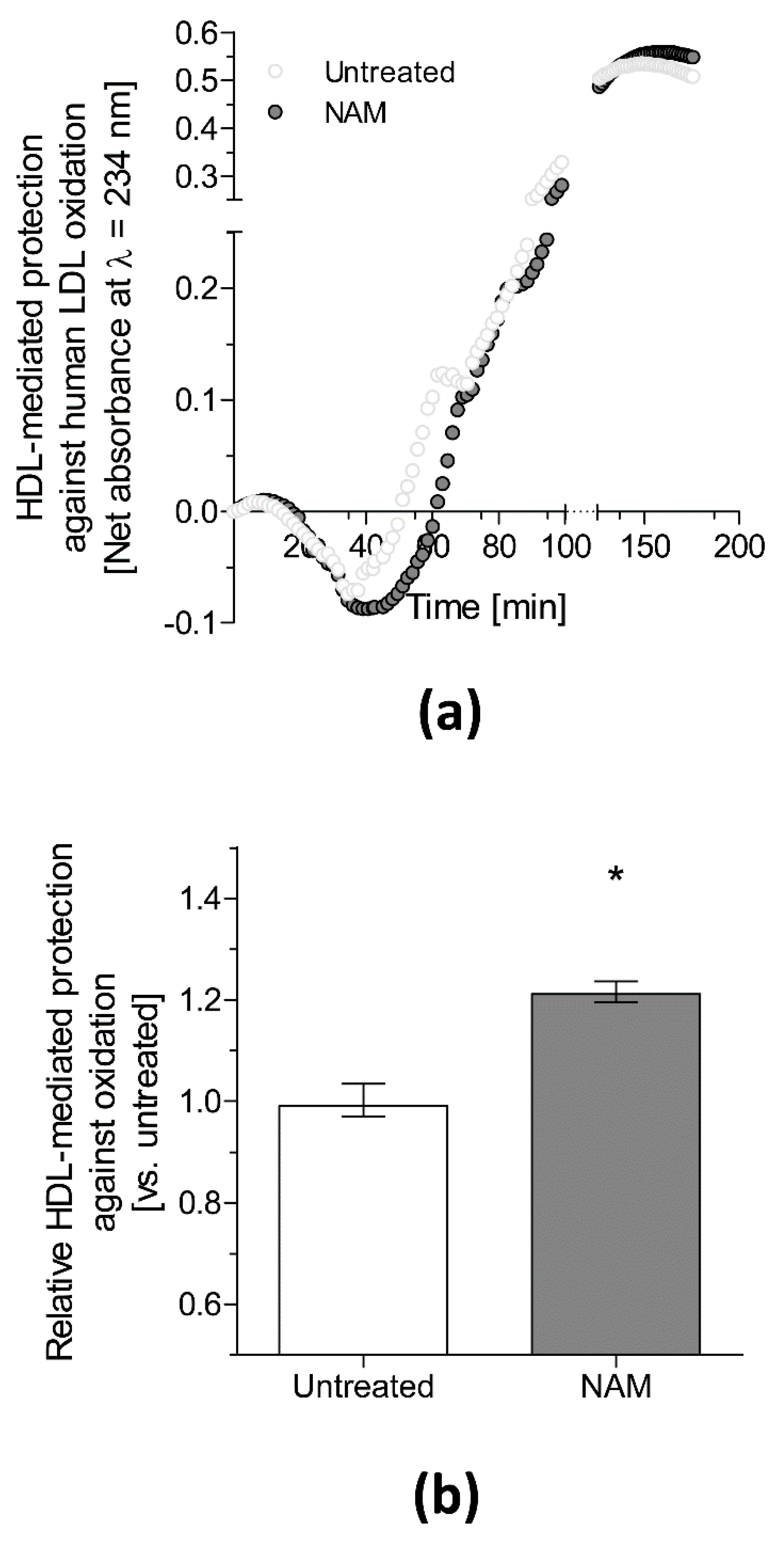
Both the resistance to oxidation of non-HDL and the antioxidant properties of HDL are two of the most important antiatherogenic metrics of lipoproteins ex vivo [83]. We recently reported that isolated plasma non-HDL from mice lacking apolipoprotein (Apo)E (Apoe−/−) treated with NAM was less susceptible to oxidation ex vivo than that from untreated mice [25]. Notably, incubation of human low-density lipoprotein (LDL) with NAM produced a direct inhibitory effect on lipid peroxidation during an analysis of the oxidation kinetics of exposed lipoproteins [25]. However, the effect of NAM on the HDL antioxidant capacity of Apoe−/− mice could not be evaluated in the latter study due to the limited circulating HDL moieties in this mouse model. Instead, the effect was directly assessed using HDL isolated from wild-type mice on the same genetic background as the Apoe−/− mice. Consistently, our data revealed that HDL isolated from the plasma of NAM-treated mice was more protective against LDL oxidation ex vivo than HDL isolated from untreated mice (Julve et al., 2021, unpublished data, Figure 2), suggesting enhanced atheroprotection by HDL from NAM-treated mice.
Figure 2.
Effect of NAM manipulation on antioxidant ex vivo protection conferred by plasma isolated HDL. (a) Representative diene formation curves of human LDL incubated with mouse HDL isolated from untreated and NAM-treated wildtype C57BL/6J mice in the presence of 2.5 μM CuSO4 at 37 °C. The final oxidation kinetics of the LDL+HDL mixture was shown after subtracting the kinetics of HDL incubated without LDL. (b) HDL antioxidant activity against LDL oxidative modification. Methods used can be found in greater detail in reference [84]. Data were expressed as relative lag phase to LDL oxidized in the presence of HDL isolated from Untreated mice (arbitrary unit = 1). Data were expressed as the median ± interquartile range (n = 4–5 independent pools per group). Differences between the mean values were determined using a nonparametric Mann–Whitney test. * indicates significant differences versus untreated mice (p < 0.05). Abbreviations used were NAM, NAM-treated mice using 1% NAM dissolved in tap water [85] (Julve et al., 2021, unpublished data).
3.2. Cellular Effects of NAD+-Increasing Strategies Relevant to Cardiovascular Diseases
Compelling experimental evidence suggests a favorable influence of NAD+-restoring strategies on the main cellular mechanisms involved in cardiovascular cell damage.
3.2.1. Oxidation
NAM protects vascular cells against oxidation [78]. This antioxidant property has also been reported for other vitamin B3 derivatives, such as NR [86] and NMN [9], probably suggesting common mechanistic pathways among such different NAD+ precursor intermediates.
The maintenance of intracellular pools of NAD+ is an important vasoprotective mechanism in arterial endothelial cells [86,87]. Consistently, NAD+ depletion is commonly related to age-related vascular dysfunction [88]. Aged endothelial cells exposed to NMN were protected against oxidative stress in a SIRT1-dependent fashion [89]. Similarly, NR-mediated restoration of NAD+ contents in the lung and heart protected against oxidative stress and apoptosis in tissues from an animal model of sepsis [86]. NR exposure prevents reactive oxygen species production and apoptosis in endothelial cells induced by conditioned medium collected from LPS-treated macrophages [86], further supporting the beneficial vascular effects of NR. NR is also protective against alcohol-induced oxidative stress and inflammation in cultured macrophages [90]. Importantly, NR effects occurred via NAD+/SIRT1 signaling [86,90].
More recently, NAD+ depletion in lipopolysaccharide (LPS)-mediated activated macrophages was accompanied by reactive oxygen species-mediated DNA damage and by activation of PARP, an NAD+-consuming enzyme [91]. In this study, the salvage pathway was induced upon NAD+ depletion, as revealed by increased NAMPT expression allowing the maintenance of intracellular pools of NAD+ sufficient for fueling glyceraldehyde-3-phosphate dehydrogenase activity and Warburg metabolism, which is critical for LPS-mediated activation of macrophages [92]. Interestingly, reduced intracellular NAD+ and increased NAMPT expression developed rapidly after inflammatory activation together with DNA damage caused by reactive oxygen species [91].
3.2.2. Inflammation
Insufficient NAD+ leads to vascular inflammation [93]. Accumulating data strongly suggest the contribution of NAD+/SIRT1 signaling to inflammation.
The anti-inflammatory effects of NAM were first described in vitro in multiple immune cell types frequently involved in chronic inflammatory processes, such as atherosclerosis [94,95,96,97,98,99,100,101,102], including activated circulating monocytes and tissue immune cells (i.e., resident macrophages), which are the first inflammatory responders and are ultimately involved in the resolution of inflammation. Notably, NAM can promote the differentiation of monocytes toward macrophages with attenuated inflammatory characteristics, i.e., with strongly reduced proinflammatory features [94]. NA administration may also shift macrophages to M2 polarization in vitro [23]. Similar anti-inflammatory actions in activated macrophages have been reported for NR [90].
Mitochondria play an important role in innate immunity and chronic inflammation [103]. Dysfunctional mitochondria can contribute to the pathophysiology of cardiovascular diseases [104]. Indeed, blockade of de novo synthesis by NAD+ using genetic or pharmacological approaches depleted NAD+ stores, suppressed mitochondrial NAD+-dependent signaling and respiration, and impaired phagocytosis and inflammation resolution [42]. This suggests a critical role for intracellular NAD+ pools in the regulation of macrophage immune function in resting and in aged and immune-challenged macrophages.
Elevated systemic inflammation has been causally linked to mitochondrial dysfunction of peripheral blood mononuclear cells (PBMCs) in subjects with HF, whereas NR-mediated NAD+ elevations improved mitochondrial respiration and attenuated proinflammatory activation of PBMCs isolated from treated volunteers with HF [105].
3.2.3. Apoptosis
Apoptosis may precede cell death and fibrosis and, thus, drive cardiac and vascular dysfunction. Excess reactive oxygen species may damage intracellular proteins, lipids, and DNA and induce apoptotic cell death [106,107]. Under ischemic/hypoxic conditions, NAD+ metabolism is significantly inhibited in myocardial cells and accompanied by reduced cell viability due to enhanced apoptosis [108,109]. Conceivably, strategies to increase NAD+ metabolism may enable cardiomyocytes to evade apoptosis. Supporting this notion, NAM exposure to primary cardiomyocytes and the H9C2 cell line conferred protection against hypoxia-induced apoptosis [108,109,110]. The attenuation of apoptosis alleviated oxidative stress and improved mitochondrial stress in NAM-treated cells [108,109]. Notably, NAM-mediated protection from apoptosis was linked to upregulation of autophagy-related proteins and accompanied by concomitant attenuation of the mTOR pathway in another study [110].
Cardiomyocyte mitochondrial dysfunction and mitochondrial DNA instability are increasingly believed to be important features of the progression of various forms of cardiac disease [111]. Under these circumstances, mitochondrial DNA repair mechanisms are commensurately induced, including PARP activity [112]. Elevations in cellular PARP activity may drain cellular NAD+ reserves [113] and lead to mitochondrial dysfunction and, thus, impaired cardiac function. Conversely, NR-mediated restoration of NAD+ pools improved the mitochondrial unfolded protein response and mitochondrial health in cultured cardiomyocytes subjected to mitochondrial stress conditions [114]. The latter finding suggests that NAM not only confers direct cellular protection against oxidation to vascular cells but also prevents cellular apoptosis during free radical exposure and blocks inflammatory vascular cell activation [115] by preventing membrane phosphatidylserine exposure [116], which is an apoptotic inducer [117]. In line with this assertion, NAD+ depletion is linked to macrophage apoptosis [118], whereas its repletion with NAD+ precursors (NA and NAM) protects cells against apoptosis [86,119].
3.2.4. Mitochondrial Stress
Cellular NAD+ depletion may occur upon increased mitochondrial DNA damage due to prolonged PARP action [113], an NAD+-consuming enzyme involved in mitochondrial DNA repair, which may cause inhibition of other NAD+-dependent proteins, especially sirtuins.
NAM pretreatment attenuated mitochondrial stress and protected hypoxic primary rat cardiomyocytes against cell necrosis and apoptosis [108]. In this study, NAM increased the intracellular ATP content in mitochondria, further revealing that NAM protected cardiomyocytes from hypoxia-mediated mitochondrial damage. Importantly, NAM-mediated favorable effects were accompanied by activation of the AMPK pathway [108]. By increasing the intracellular NAD+ content, NAM can also increase the protein abundance of superoxide dismutase and catalase and induce intracellular energy production [109], thus reducing the abundance of mitochondrial reactive oxygen species and preventing the loss of mitochondrial membrane potential.
3.2.5. Autophagy
Autophagy is a cellular process that recycles components of the cytoplasm of cells and plays a key role in tissue remodeling. As previously mentioned, NAM supplementation protected chronic hypoxic myocardial cells against hypoxia-induced apoptosis and increased the protein abundance of autophagy-related proteins by attenuating mTOR pathways [110].
NR exposure promoted autolysosome generation in neonatal and adult mouse cardiomyocytes exposed to doxorubicin (DOX) [120]. In particular, NR can attenuate autophagic flux blockade, autolysosome accumulation, and oxidative stress in DOX-treated cardiomyocytes. Notably, inhibition of lysosomal acidification or SIRT1 abrogated such NR-mediated protective effects during DOX-induced cardiotoxicity, thereby suggesting that NR enhances autolysosome clearance via NAD+/SIRT1 signaling to prevent DOX-induced cardiotoxicity.
3.2.6. Fibrosis
Organ fibrosis is characterized by excess deposition of extracellular matrix proteins. Administration of NA, NAM, and NR attenuates experimental liver fibrosis [14,121,122,123,124], potentially indicating that an insufficient NAD+ supply may underlie organ fibrosis. Similar favorable effects could be conceivably suggested for NAD+-increasing interventions aiming to directly combat myocardial fibrosis. Although such interventions have not yet been explored, this strategy may warrant further investigation.
4. In Vivo Cardiovascular Effects of NAD+-Boosting Strategies: Lessons from Animal Models
4.1. Atherosclerosis
Immune cell infiltration and activation are a characteristic finding in chronic inflammation processes, such as atherosclerosis [125]. Macrophages and vascular smooth muscle cells are regulated through a coordinated pivotal program during the development of atherosclerotic lesions [126,127]. Regulation of the cholesterol balance in these cell types is critical in atherogenic processes, and the accumulation of LDL-derived cholesterol in foam cells leads to chronic inflammatory responses in the subendothelial arterial intima [128]. The interaction of LDL with proteoglycans initiates LDL retention in the intima, facilitating LDL modifications and increasing their nonregulated uptake by macrophages [129]. In contrast, HDL stimulates cholesterol efflux from macrophages, the first step of the reverse cholesterol transport pathway, which is mechanistically linked to the anti-inflammatory and immunosuppressive functions of HDL [126].
The first evidence that NA administration reduced atherosclerosis was reported in rabbits [130,131,132,133] and minipigs [134] (Table 1). The antiatherogenic effect of NA was also confirmed in humans [135,136]. Originally, these antiatherogenic effects were mainly attributed to the ability of NA to reduce serum LDL cholesterol (LDL-C) and triglycerides while increasing HDL-C levels. However, these antiatherogenic effects did not always correlate with NA-mediated hypolipidemic effects [130,134]. The development of genetically engineered mice permitted us to evaluate the potential of NA to prevent massive atherosclerosis in different mouse models of hyperlipidemia and investigate the potential atheroprotective mechanisms. NA had a strong lipid-independent antiatherogenic effect on LDL receptor-deficient (Ldlr−/−) mice, which was mainly mediated by its receptor GPR109A on bone marrow–derived cells [137]. GPR109A activation by NA enhanced ATP binding cassette (ABC) G1-dependent macrophage cholesterol efflux to HDL, inhibited MCP-1–induced macrophage recruitment into the peritoneal cavity, and impaired macrophage homing into atherosclerotic lesions [137]. Furthermore, NA administration in Apoe−/− mice also reduced advanced lesion progression and plaque inflammation independent of plasma lipoprotein levels, rendering advanced atherosclerotic lesions more stable [138]. In line with these findings, an independent study also showed that both Ldlr−/− and Apoe−/− mice treated with NA had significantly lowered aortic cholesterol levels, although this study also reported an NA-mediated hypolipidemic effect [139]. However, these findings were not reproduced in another study conducted in Apoe−/− mice [140], likely because the researchers used a low-fat diet combined with an insufficient NA dose and a short treatment period. On the other hand, Apoe3Leiden transgenic mice overexpressing human cholesteryl ester transfer protein (CETP) treated with NA also showed reduced atherosclerosis development concomitant with enhanced very-low density lipoprotein clearance and low CETP activity resulting in higher HDL-C [141]. In this study, NA also reduced monocyte adhesion and macrophage homing into atherosclerotic lesions but promoted macrophage-to-feces reverse cholesterol transport [141], thereby emphasizing that multiple mechanisms may explain the antiatherogenic effects of NA in vivo.
Other vitamin B3 intermediates, such as NMN and NR, reversed age-related endothelial dysfunction and reduced oxidative stress [15,28]. Although their mechanism of action in atherosclerosis prevention has not been directly evaluated in vivo, the effects of these intermediates can be at least partly explained by their ability to effectively increase the tissue content of NAD+ and, thus, restore SIRT1 activity (reviewed in reference [8]). Supporting this assertion, a host of studies in genetically engineered atherosclerotic mice suggest a protective role of SIRT1, although this effect was mainly related to its expression in vascular cells (reviewed in Reference [142]). However, the potential involvement of a SIRT1-mediated mechanism was reflected only by the upregulation of some aortic targets of liver X receptor (LXR) [143]. Supporting this notion, our group has demonstrated that the gene expression of Abca1 and Abcg1 was upregulated in aortic tissue from Apoe−/− mice and in cultured macrophages exposed to NAM, although only marginally [25]. In the latter study, dietary NAM supplementation prevented aortic atherosclerosis in Apoe−/− mice, which was related to an improvement in the susceptibility of ApoB-containing lipoproteins to oxidation and to upregulation of aortic IL-10 and downregulation of TNFα, suggesting a switch toward anti-inflammatory macrophages [25]. Rather surprisingly, these antiatherogenic effects were accompanied by higher levels of plasma ApoB-containing lipoproteins and impaired macrophage-specific reverse cholesterol transport in vivo [25,144]. Overall, these findings support that NAM-mediated anti-inflammatory effects may prevail in atherogenesis. In line with these findings, me-NAM administration, a major endogenous metabolite of NAM (Section 2), also prevents atherosclerotic plaque progression and inflammation in double Ldlr−/−/Apoe−/− mice [29]. In this study, me-NAM improved endothelial function [29], as was also reported in an independent study conducted in Apoe−/− mice [30].
NAMPT is the rate-limiting enzyme in the NAD+ salvage pathway. However, different studies investigating the effects of NAMPT in atherosclerosis in vivo found conflicting results depending on the localization of NAMPT. Administration of the NAMPT inhibitor FK866 reduced inflammation in atherosclerotic plaques after carotid cast implantation in Apoe−/− mice by reducing CXCL1-mediated activities on neutrophils and improving plaque vulnerability parameters [145]. Additionally, liver-specific deficiency of NAMPT increased plasma HDL-C levels and reduced aortic atherosclerosis, including macrophage homing [146]. These effects were closely related to upregulation of LXR target genes and a consequently enhanced macrophage-to-feces reverse cholesterol transport rate in vivo [146]. Conversely, NAMPT overexpression aggravated atherosclerotic inflammation and enhanced atherosclerosis development in Apoe−/− mice [147]. In contrast, hematopoietic overexpression of human NAMPT attenuated the plaque burden and stabilized lesions in Ldlr−/− mice [148], likely suggesting tissue-specific and possibly species-specific differences to explain such apparently divergent findings. Notably, these effects were found only after modulating intracellular levels of NAMPT and were associated with macrophage resistance to apoptosis, attenuating monocyte intravasation and migration in response to chemotactic signals, thereby skewing monocyte differentiation and macrophage polarization toward an anti-inflammatory M2 phenotype [148].
Finally, NAD+ is also a substrate for poly(ADP-ribose) polymerase, also known as PARP (Section 2). PARP activity leads to NAD+ and ATP depletion after various types of DNA damage [149]. Both PARP pharmacological inhibition and gene deletion reduced plaque sizes in Apoe−/− mice concomitant with reduced macrophage homing in two independent studies [150,151]. In particular, PARP inhibition increased plaque stability without improving the lipoprotein profile. Consistently, PARP inhibition also reduced traits of plaque disruption in a separate study conducted in Apoe−/− mice [152], mainly by decreasing oxidative DNA damage and iNOS-associated protein nitration. In two of these studies, Parp gene deletion protected against oxidant-induced foam cell death [150,152], which may be related to preserved intracellular NAD+ and ATP pools. Moreover, pharmacological inhibition of PARP action also promoted atherosclerotic plaque regression in this mouse model of atherosclerosis by modulating most of these key antiatherogenic factors [153]. Consistent with these findings, a recent report confirmed the in vivo antiatherogenic effects of PARP inhibition in rabbits [154], which were likely due to its ability to improve endothelial function by preserving NAD+ levels.
4.2. Ischemic-Infarcted Myocardium or Ischemia-Reperfusion
Myocardial infarction is a common major cardiovascular event that originates from myocardial ischemia in the presence/absence of reperfusion [155]. The term ischemia encompasses a broad range of clinical hypoxia scenarios ranging from angina to permanent occlusion. Although reperfusion intervention is clinically mandatory to treat ischemic injury, the associated cardiac damage caused by this intervention should not be overlooked.
The loss of several dinucleotide species, including NAD+, NADH, NADP+, and NADPH, has been shown in myocardial tissue after ligature of the coronary artery branch [156] in dogs. In the corresponding study, NAD+ decline was accompanied by increased activity of NAD+ glycohydrolase, an NAD+-consuming enzyme (Section 2), which has been reported in response to acute experimental acute infarction [157]. Notably, irreversible postischemic injury occurred when NAD+ depletion was approximately 60–70% [158]. Therefore, NAD+ stabilization appears to be critical for the recovery of mitochondrial and cardiac function. NAD+ mainly acts by reducing oxidative stress and cell death [159]. Importantly, cardiac-specific overexpression of NAMPT increased NAD+ levels in the heart and reduced the size of myocardial infarction in response to prolonged ischemia/reperfusion in mice [160]. In this context, NAD+ supplementation also protected hearts from ischemia/reperfusion injury in mice [161], Bama miniature pigs [162], and rats [159,163] (Table 1). Furthermore, cardiac hypoxia-ischemia injury can be relieved in mice treated with NMN supplementation [164]. NMN also protected against ischemia/reperfusion injury in aged rats [165]. NMN replenished heart NAD+ levels but reduced oxidative stress and mitochondrial ROS levels. Another study also suggested that NRK-2 alleviates ischemia-induced HF through P38 signaling [166]. Finally, NR was also shown to be effective in improving vascular function. NR improved endothelium-dependent relaxation of isolated rat mesenteric arteries in an ischemia-reperfusion model [167]. Overall, these studies strongly suggested that NAD+ and its precursors improve alterations following ischemia/reperfusion injury in vivo.
4.3. Cardiomyopathy and Heart Failure (HF)
Cardiomyopathy is one of many causes of HF. Its prevalence continues to rise over time, especially with aging.
Dilated cardiomyopathy is characterized by dilatation of the left and right ventricles, leading to systolic dysfunction and a reduced ejection fraction [168]. Susceptibility to dilated cardiomyopathy has been predominantly explained by genetic mechanisms, and, in Western societies, this cardiac condition is the principal indication for heart transplantation.
Various studies have explored HF and NAD+ levels in vivo. Cellular NAD+ is a key regulator of metabolism and bioenergetics, and failure of cardiomyocyte bioenergetics is a critical hallmark of HF. Interestingly, previous studies suggest that mitochondrial dysfunction and metabolic remodeling in HF are associated with an imbalance in the intracellular ratio of NADH to oxidized NAD+ or the NADH/NAD ratio [169,170]. Therefore, controlling intracellular NAD+ levels may improve myocardial bioenergetics and cardiac function. In fact, in a recent paper, normalization of NADH/NAD through supplementation with NAD+ precursors was shown to be associated with cardiac function improvement in an HF mouse model [171]. Specifically, the authors studied the impact of NAD+ precursor supplementation in food (NR) in two different mouse models of dilated cardiomyopathy and found stable myocardial NAD+ levels in the failing heart. Diguet et al. [171] proposed that the benefit observed in their study was due to improved energy metabolism rather than altered protein acetylation. However, previous studies found that NAD+ availability was associated with increased protein acetylation in the failing myocardium, which was attributable to impaired NAD+-dependent protein deacetylation by sirtuins, especially SIRT3 [172,173,174,175]. Another study reported oral supplementation of NR to treat cardiomyopathy caused by laminin A/C gene (Lmna) mutations (LMNA cardiomyopathy) in mice. Mutant mice suffered from dilated cardiomyopathy [176]. The NAD+ salvage pathway has been shown to be altered in the hearts of mice and humans carrying Lmna mutations, leading to alteration of PARP-1, which is an NAD+ cosubstrate enzyme [177]. Oral administration of NR to LmnaH222P/H222P mice resulted in an improvement in the NAD+ cellular content, an increase in PARylation of cardiac proteins, and an improvement in left ventricular structure and function [177]. However, NAM supplementation to LmnaH222P/H222P mice did not change NAD+ contents in the liver or heart or cardiac left ventricular function [177].
In general, approximately half of subjects with HF present with a reduced ejection fraction (HFrEF), and the other half present with a preserved ejection fraction (HEpEF) [178], which is important to emphasize because these presentations reflect different but not entirely distinct pathogenic mechanisms, and their treatments may also be different. For example, mitochondrial dysfunction and metabolic remodeling are known to play important roles in HFrEF, but little is known about the mechanisms of mitochondrial dysfunction in HFpEF. In the myocardium of an HFpEF mouse model, mitochondrial fatty acid oxidation has recently been observed to be impaired and to be associated with hyperacetylation of key enzymes along the pathway. SIRT3 downregulation and NAD+ deficiency secondary to an impaired NAD+ salvage pathway are the main contributors to mitochondrial fatty acid oxidation according to the authors of Reference [179]. Interestingly, supplementation with NAD+ or a direct activator of NAD+ biosynthesis in HFpEF mice with NR ameliorated the HFpEF phenotype by improving mitochondrial function and pathological cardiac remodeling [179].
In the setting of aging, the role of NAD+ has been explored by Tannous et al., who demonstrated that a lack of NRK2 does not influence the NAD+ level in the myocardium in young adults [180]. However, NRK2 expression is required to support the maintenance of NAD+ levels in 24-month-old mouse hearts. At this late stage, the major biosynthetic pathways are repressed, and, in the absence of myocardial NRK2, NAD+ levels fall by 50% [180]. Moreover, Nmrk2-deficient mice, which develop a progressive DCM-like phenotype with aging, are viable but develop progressive cardiac dysfunction and eccentric cardiac remodeling associated with an alteration in laminin deposition in the extracellular matrix starting at 4 months, followed by cardiac fibrosis and structural defects in the adult myocardium [180]. Consistent with these findings, another study suggested that feeding aging mice with NR improved mitochondrial function and preservation of stem cell function, which may contribute to the extended lifespan of NR-treated mice [11]. Additionally, iron overload and iron deficiency have been associated with cardiomyopathy and HF. Inactivation of transferrin receptor (Tfr1) in mice was associated with cardiomegaly, poor cardiac function, failure of mitochondrial respiration and mortality in the second week of life. Interestingly, the lifespan of Tfr1-deficient mice was prolonged by treatment with NR [181]. However, the benefit and safety of NAD+ precursor supplementation require further elucidation. For instance, in another study with a high-dose NR supplementation in a cardiomyocyte mutUNG1 mouse model, which is a mouse model with myocardial mitochondrial DNA damage, sirtuin activity was inhibited rather than increased due to intracellular NAM accumulation, while the addition of NR failed to improve cardiac function [182]. Thus, the authors suggested that high doses of NR should be used with caution, especially when cardiomyopathic symptoms are caused by mitochondrial dysfunction and mitochondrial DNA instability.
As stated above (Section 2), NAMPT, a rate-limiting enzyme in the NAD+ salvage pathway, plays an important role in controlling the level of NAD+. In another mouse model of HF, Byun et al. demonstrated that pressure overload-induced HF is exacerbated in both systemic Nampt-deficient mice and mice with cardiac-specific Nampt overexpression. Unexpectedly, both loss- and gain-of-function models exhibited reduced protein acetylation, suppression of metabolic genes, and mitochondrial energetic dysfunction. Therefore, endogenous NAMPT plays a protective role under pressure overload conditions, but cardiac-specific Nampt overexpression is detrimental rather than therapeutic. The authors suggested that these deleterious effects in NAMPT transgenic mice may be partially due to SIRT1 and suppression of the gene expression of key metabolic targets [183].
Another pathophysiological process promoting HF progression is cardiac fibrosis, which is characterized by increasing ventricular stiffness and a reduced cardiac pumping capacity. In a mouse model of isoproterenol-induced cardiac fibrosis, Wu et al. demonstrated that NMN treatment attenuates cardiac fibrosis in vivo and fibroblast activation in vitro by suppressing oxidative stress and SMAD3 acetylation in an NAD+/SIRT1-dependent fashion [184].
Diabetic cardiomyopathy is another major cause of HF. Subjects with diabetic cardiomyopathy have adverse structural remodeling due to enhanced cardiac hypertrophy and fibrosis, resulting in characteristic cardiac dysfunction. The prevalence of diabetic cardiomyopathy is increasing in parallel with the increase in diabetes mellitus. Accordingly, epidemiological studies show a positive correlation of hyperglycemia with an increase in HF in subjects with either type 1 or type 2 diabetes mellitus. Notably, the manifestation of these conditions is independent of atherosclerotic cardiovascular disease and hypertension [185,186,187]. Additionally, hyperglycemia has been shown to be associated with a reduced NAD+ content, a decreased NAD+/NADH ratio, and promoted protein hyperacetylation and mitochondrial dysfunction in diabetic organs [188,189,190,191,192,193,194]; thus, NAD+ restoration is of therapeutic importance. More recently, NAD+ redox imbalance has been shown to alter protein acetylation and phosphorylation in two different mouse models of diabetic cardiomyopathy [195]. Specifically, an NAD+ redox imbalance in mice with cardiac-specific knockout of complex I subunit Ndufs4 (cKO) hearts causes systolic and diastolic dysfunction due to cardiomyocyte dysfunction. Moreover, diabetic cKO hearts presented increased acetylation of superoxide dismutase 2, protein oxidation, troponin I S150 phosphorylation and impaired energetics. Importantly, all these effects were normalized when cardiac NAD+ levels were elevated using Nampt transgenic mice (diabetic cKO-NAMPT mice), suggesting a beneficial effect of exploiting NAD+ metabolism for diabetic cardiomyopathy. Consistent with this finding, restoration of cardiac NAD+ with NMN supplementation in the myocardium of genetically deficient mice with cardiac-specific expression of Kruppel-like factor 4 (Klf4) (CMK4KO) protected against pressure overload-induced HF induced by transverse aortic constriction [194]. Notably, CMK4KO mice are more prone to pressure overload-induced HF caused by transverse aortic constriction [196,197]. KLF4 belongs to a larger family of zinc-finger transcription factors that regulate critical cellular processes, such as cell survival, apoptosis, and metabolism. Some members of the KLF family influence several cell types belonging to the cardiovascular system [198]. Specifically, KLF4 is a critical regulator of cardiac mitochondrial homeostasis [197]. Conceivably, its cardiac deficiency was associated with cardiac NAD+ deficiency and mitochondrial protein hyperacetylation coupled with reduced SIRT3 in the hearts of mice [198]. Notably, cardiac NAD+ replenishment with NMN supplementation successfully protected these mice from cardiac disease by positively influencing mitochondrial health and oxidative stress and preventing cardiac cell death in treated mice.
Cardiac hypertrophy is also a common feature in many cardiovascular diseases [199]. Although cardiac hypertrophy may develop as a benign, adaptive response to either physiological or pathological situations, chronic cardiac stimulation can cause cardiac hypertrophy, remodeling and dysfunction and eventually lead to HF [200]. Enhanced inflammation via activation of the nucleotide-binding and leucine-rich repeat pyrin domains protein 3 (NLRP3) inflammasome and concomitant secretion of cytokines contributes to the progression of cardiac hypertrophy [201]. Therefore, cardiac hypertrophy inhibition has been considered a possible target for novel therapies. In this context, a recent study demonstrated that NR administration favorably influenced cardiac hypertrophy and dysfunction induced by transverse aortic constriction (TAC) surgery in a mouse model by directly inhibiting myocardial NLRP3 inflammasome activation [202]. Notably, this NR-mediated NAD+ rise in myocardial tissue elevated SIRT3 activity, which resulted in MnSOD deacetylation and TAC-induced myocardial oxidative stress alleviation.
4.4. Cardiotoxicity
Cardiotoxicity can occur during cancer treatment and can reduce quality of life and increase the risk of death from cardiac-related causes [203,204]. This condition can appear within days, months, or years after chemotherapy, even after disease remission, which is the case, for example, for doxorubicin (DOX), a drug widely used in chemotherapy for the treatment of several malignancies. Nonetheless, the dose-dependent cardiotoxic effects of DOX, which include increased cardiomyocyte death via apoptosis [205,206], necroptosis [207] and ferroptosis [208], left ventricular dysfunction, dilated cardiomyopathy, and congestive HF in severe cases [209], limit its use in clinical practice; therefore, intensive research to attenuate such adverse effects is currently underway. Importantly, oxidative stress is commonly increased upon DOX treatment and underlies cardiotoxicity. In this context, NAM administration to DOX-treated rats successfully reversed signs of cardiac tissue injury revealed by elevated serum cardiotoxicity molecules and conduction and histopathological abnormalities [210]. Consistently, NR also reduced cardiac injury and myocardial dysfunction in DOX-treated mice by restoring NAD+ levels [120].
4.5. Aortic Aneurysm: Vascular Disease
Aortic diseases can be extremely life-threatening and include a variety of clinical entities, the most frequent of which is aortic aneurysm. Aortic aneurysm (AA) refers to progressive localized dilatation and weakening of the aorta, which can occur in the chest, thorax (thoracic aneurysm, TAA) or abdomen (abdominal aortic aneurysm, AAA). Although differences can be found in the pathobiology between TAA and AAA, both are characterized by local chronic inflammation of the aortic wall, apoptosis of smooth muscle cells in the aortic media layer and fragmentation of the extracellular matrix of the aorta at the site of the aneurysm. Increased local expression of proinflammatory cytokines, extracellular matrix degradation, microcalcification, and oxidative stress are biological processes contributing to degeneration of the aorta [211].
The risk factors for developing aortic aneurysms are age, sex, smoking, high blood pressure, peripheral artery disease, genetic disorders (individuals with Marfan, Ehlers–Danlos, Loeys–Dietz, or Turner syndrome can develop TAA), a family history of aneurysmal diseases, inflammatory diseases of the blood vessels (vasculitis), and aortic valve abnormalities. No effective drug therapy is currently available for AA, and 70% of small AAs grow to a size requiring surgical repair before fatal aortic rupture occurs [211]. Accordingly, identifying targets for the development of drug therapies that can effectively limit AA growth and rupture has attracted strong interest.
The sequential pathophysiology of aneurysm formation is unclear, but vascular smooth muscle cells (VSMCs) are known to play a central role in vascular cell vitality and, thus, matrix integrity. NAMPT is expressed in cultured SMCs, and its content and activity decline during advanced smooth muscle cells (SMC) aging [212,213,214]. Knockdown of Nampt in VSMCs has been shown to increase VSMC apoptosis, which has an important influence on AA development [215], whereas overexpression of Nampt can enhance VSMC survival [212], thereby suggesting a potential contribution of the salvage pathway to NAD+ synthesis in this cell type. Although controversial, some reports show that the NAMPT-NAD+ axis control system may favorably influence SMC contractile function [216,217,218].
NAMPT is expressed in periaortic adipose tissue [219], and altering NAD+ metabolism through the diet has been found to suppress age-related aortic dysfunction [220]. Watson and colleagues showed that the aortas of patients with thoracic aortic aneurysms had lower levels of NAMPT than nondilated aortas and correspondingly increased DNA strand breakage in SMCs [217]. They generated mice with homozygous deficiency of NAMPT in SMCs and found that loss of NAMPT rendered the aorta susceptible to aortic dilation and rupture and that their SMCs were more prone to senescence and DNA damage. Finally, they found that the NAMPT promoter was hypermethylated in the aortic media of aortopathy patients, suggesting epigenetically repressed NAMPT production. Together, the results uncovered an endogenous NAD+-fueling system in the aortic media that protects against DNA damage and premature SMC senescence.
The pharmacologic potential of NR in TAAs associated with genetic disorders has been investigated [221]. Using a mouse model with specific deletion of mitochondrial transcription factor A (Tfam) in VSMCs, Tfam-deficient VSMCs were observed to acquire a senescent and proinflammatory phenotype together with impairment in their contractile function [221]. These mice develop aortic aneurysms, medial degeneration, and lethal dissections, and NR supplementation rapidly raised TFAM levels, improved mitochondrial metabolism, and normalized aortic function and diameter in the Marfan mouse model of TAA.
NA inhibits vascular inflammation by decreasing oxidative stress and inhibiting monocyte/macrophage inflammatory responses and inflammatory cytokine production, which are key events in the pathogenesis of AAA [222,223]. Accordingly, NA may of particular interest for the prevention and treatment of aortic aneurysms [224,225].
In this regard, a previous study using two distinct animal models of AAA reported that NA inhibited AAA formation in conjunction with reduced aortic immune cell infiltration, inflammation, and matrix degradation [24]. The beneficial effects of NA are independent of GPR109A signaling, similar to NAM, and likely mediated through NAD+ production leading to SIRT1 activation. These results suggest that boosting NAD+ levels and SIRT1 activity by supplementation with NAM or related biomolecules may represent a promising therapeutic strategy for AAA treatment and prevention [24].
The role of SIRT1 in vascular homeostasis and diseases in mammals has been well documented [226,227,228]. Enhancing NAD+ biosynthesis with NAD+ precursors, such as NMN and NR, increases the activity of SIRT1 [10,12,229,230], improving mitochondrial dysfunction in different pathologies [33,231,232]. Notably, supplementation with NMN restored arterial SIRT1 activity and reversed age-associated arterial dysfunction and oxidative stress in the aortas of aged mice, which was associated with partial normalization of structural proteins in the arterial wall [9]. Additionally, acute NMN incubation in isolated aortas increased NAD+ threefold, supporting the promising potential of NMN supplementation for the treatment of arterial aging [9]. This is consistent with previous reports showing that NMN increases NAD+ in cultured vascular endothelial cells [233] and normalizes the ratio of NAD+/NADH in aortic tissue [234].
Downregulation of SIRT1 might also be mechanistically linked to AAA pathogenesis. Compared with those in adjacent control sections, SIRT1 expression and activity are significantly decreased in human AAA lesions [235]. In Apoe−/− mice infused with Ang II using pumps to induce hypertension (a recognized animal model of aneurysm), the incidence of AAA and the mortality rate were markedly reduced in VSMC-specific, Sirt1 transgenic mice [235]. Even without Apoe deficiency, an increase in both the prevalence and mortality of AAAs was found in VSMC-specific Sirt1 deficient mice compared with wild-type mice. Similar data were obtained in a calcium chloride–induced mouse AAA model in independent studies [235]. The underlying mechanism involves attenuation of vascular senescence by SIRT1 via modulation of the p53/p21 pathway. Moreover, macrophage-specific Sirt1 expression was reported to contribute to AAA protection [236]. Reducing calorie intake protected against AAA formation in Apoe−/− mice by upregulating the expression and activity of SIRT1 in VSMCs [237], and specific knockout of VSMC-derived Sirt1 abolished the prevention of AAA by caloric restriction [235].
In addition to AAAs, SIRT1 is also important in the prevention of TAA. VSMC-specific Sirt1 deficient mice did not influence the incidence of TAA but increased the fatality rate in mice. Moreover, VSMC-specific Sirt1 overexpression markedly blocked TAA development mainly through epigenetic downregulation of MMP-2 [238].
These findings provide evidence that SIRT1 reduction links vascular senescence through vascular inflammation to AAAs and that SIRT1 in VSMCs is a promising therapeutic target for the prevention of life-threatening aortic diseases.
Finally, CD38, another NAD+-consuming enzyme, is a key modulator of NAD+ metabolism and influences cell signaling, aging, and tumor biology, suggesting a role for this enzyme as a target with promising therapeutic potential. CD38 was found to be highly expressed in aortic aneurysm tissue, and circulating CD38 was positively correlated with peak wall stress values, but the mechanisms by which CD38 was involved in AAA remain unclear [239].
4.6. Hypertension
Hypertension, also known as high or increased blood pressure, is a condition in which blood vessels are subjected to persistently elevated pressure, eventually causing health problems, such as heart disease [240]. The pathogenesis of essential hypertension is complex and likely multifactorial, involving genetic factors, activation of neurohormonal systems, such as the sympathetic nervous system and renin-angiotensin-aldosterone system, obesity, and increased dietary salt intake. This entity involves the interaction of multiple organs and numerous mechanisms, with the kidney playing a central role, as it is both the contributing and the target organ of the hypertensive processes. In accordance with most major guidelines, a subject with hypertension is defined by a systolic blood pressure (SBP) ≥ 140 mm Hg and/or a diastolic blood pressure (DBP) ≥ 90 mm Hg on repeated examination [241].
Studies exploring NAD+ and hypertension relationships in vivo have shown that endothelial dysfunction by SIRT impairment is involved in vascular homeostasis and cardiovascular disease and is related to hypertension [242]. Several studies in hypertensive mice described that, under the pathological stress of hypertension, endothelial-specific deletion of Sirt6 further exacerbated endothelial dysfunction and cardiorenal injuries, indicating the importance of SIRT6 in maintaining endothelial functions and preventing hypertension and its complications by ensuring endothelial function [242,243]. Inhibition of angiotensin II-activated TGF-β by SIRT1 has been described to contribute to the improvement of vascular remodeling (including reduced vascular inflammation and collagen synthesis) in the aortas of transgenic mice, resulting in a decreased SBP [244]. Other in vivo studies have also demonstrated the vasorelaxing capacity of NAM through inhibition of ADP ribosyl cyclase (a mediator of renal vasoconstriction in vivo through the Ca2+ signaling pathway) [245,246,247] (Table 1). In a previous study performed in spontaneously hypertensive rats receiving NADH, a lower SPB in treated rats versus nontreated rats was observed after 60 days of treatment [248]. In an in vivo study in rats with renal mass reduction, long-term NA supplementation ameliorated hypertension and partially reversed the upregulation of oxidative, inflammatory, and profibrotic mediators in the remnant kidney [249]. NAM has also been used to treat preeclampsia (high blood pressure and proteinuria in pregnant women) in a reduced uterine perfusion pressure mouse model, which was found to be effective in improving and preventing hypertension, fetal growth restriction and premature birth [250]. In a similar study involving 2 mouse models of preeclampsia, the authors concluded that NAM decreased blood pressure and endotheliosis in the mothers, probably by inhibiting ADP ribosyl cyclase, and also prevented fetal growth restriction, probably by normalizing fetal ATP synthesis via the nucleotide salvage pathway [251]. The same group also reported that a pharmacological dose of NAM normalized blood pressure in mice with impaired eNOS function either pharmacologically or genetically by suppressing inflammation and had partial benefits on kidney damage induced by L-NAME [252]. A previous work carried out in C57BL/6J mice demonstrated that upregulation of monocyte-derived extracellular NAMPT contributed to preservation of myocardial NAD+ levels and functional compensation against pressure overload, which is crucial to avoid HF [253]. In a recent study regarding HF with a HFpEF, oral supplementation of NAD+ precursors, such as NAM, in Dahl salt-sensitive rats, improved hypertension and diastolic dysfunction, and these effects were mediated partly through alleviated systemic comorbidities, enhanced myocardial bioenergetics and ameliorated cardiomyocyte passive stiffness, and calcium-dependent active relaxation [31].
Nonetheless, most authors conclude that the mechanisms underlying the observed effects explaining how NAD+ precursors reduce blood pressure are still unclear. NAD+-consuming enzymes, ADP ribosyl cyclase and SIRTs, and the anti-inflammatory effects of NAD+ have been hypothesized to contribute to blood pressure reduction; however, this assertion requires further research [6].

Table 1.
In vivo evidence for NAD+-increasing strategies in different animal models of different cardiovascular pathologies.
Table 1.
In vivo evidence for NAD+-increasing strategies in different animal models of different cardiovascular pathologies.
| Form of Suppl. B3 | Animal Model | Dose and Route of Administration | Duration | Outcome | Reference |
|---|---|---|---|---|---|
| Atherosclerosis | |||||
| NA | Ldlr−/− mice | Dietary supplementation of NA (0.3% w/w) in a high-fat diet containing 21% butter fat and 1.5% cholesterol | 10 weeks | Reduced aortic atherosclerotic plaque area | [137] |
| NA | Apoe−/− mice | Dietary supplementation NA (0.5% w/w) in a regular chow diet | 27 weeks | Reduced atherosclerotic lesions within the innominate artery | [138] |
| NA | Apoe−/− mice and Ldlr−/− mice | Dietary supplementation of NA (3% w/w) in a high-fat diet containing 21% of fat and 0.2% cholesterol | 8 weeks | Reduced aortic cholesterol and whole atherosclerotic plaque area | [139] |
| NA | Apoe−/− mice | Dietary supplementation NA (0.5% w/w) in a regular chow diet containing 0.2% cholesterol | 14 weeks | No changes in aortic root atherosclerotic area | [140] |
| NA | Apoe*3Leiden transgenic mice expressing human CETP | Dietary supplementation NA (0.1% w/w) in high fat diet containing 15% cacao butter and 0.1% cholesterol | 18 weeks | Reduced aortic root atherosclerotic area | [141] |
| NA and pentaerythritoltetran NA | Rabbit | Dietary supplementation of NA or pentaerythritoltetran NA (0.5% w/w) in a cholesterol-containing (1%) diet | 71 days | Only pentaerythritoltetran NA reduced the lipid infiltrated area of the aorta | [132] |
| NA and pentaerythritoltetran NA | Rabbit | Dietary supplementation of NA or pentaerythritoltetran NA (0.5% w/w) in a cholesterol- and coconut oil- containing (1% and 3%, respectively) diet | 81 days | Both drugs reduced the lipid infiltrated area of the aorta | [132] |
| Pentaerythritoltetran NA | Rabbit | Dietary supplementation of pentaerythritoltetran NA (0.5% w/w) in a coconut oil- containing (8% and 15%) diet | 120 and 160 days | Reduced lipid infiltration in the aorta | [131] |
| Pentaerythritoltetran NA | Rabbit | Dietary supplementation of pentaerythritoltetran NA (0.75% w/w) in a coconut oil- containing (3%) diet. The concentration of cholesterol in the diet was adjusted for each rabbit andt the animals attained a mean plasma cholesterol level of about 6 mg/mL | 160 days | Reduced aortic cholesterol | [130] |
| NA and Pentaerythritoltetran NA | Mini-pigs | Dietary supplementation of NA or pentaerythritoltetran NA (0.25–0.75% w/w) in egg yolk- and cholesterol- (11 and 0.5–0.75%, respectively) containing diet | 12–19 months | Reduced lipid infiltration in the aorta | [134] |
| Me-NAM and NA | Double Ldlr−/−/Apoe−/− mice | Administration of me-NAM or NA (0.1 g/kg/day) in the drinking water together a regular chow diet | 4 weeks | Both drugs reduced aortic root atherosclerotic area | [29] |
| NAM | Apoe−/− mice | Administration of NAM (0.25 and 1% w/v equivalent to 0.5 and 1.9 g/kg/day, respectively) in the drinking water together a high-fat diet containing 21% of fat and 0.2% cholesterol | 4 weeks | Reduced aortic root atherosclerotic area | [25] |
| me-NAM | Apoe−/− mice | Dietary supplementation of me-NAM (0.0057 and 0.017% w/w) in a high-fat diet containing 21% of fat and 0.2% cholesterol | 8 weeks | Reduced aortic root atherosclerotic area | [30] |
| Cardiotoxicity | |||||
| NAM | Sprague Dawley male rats treated with DOX (5 mg/kg, i.p.) once/week for four consecutive weeks | Oral dose of NAM (600 mg/kg by oral gavage). | 28 consecutive days | Amelioration of cardiotoxic serum cardiotoxicity indices, conduction and histopathological abnormalities | [210] |
| NR | Male mice (aged 2 months) were injected with a single dose of DOX (20 mg/kg, i.p.) | 0, 100, 300, or 500 mg/kg (i.p.) given 30 min prior DOX injection | 5 days | Reduced cardiac injury and myocardial dysfunction | [120] |
| Myocardial ischemia/reperfusion injury | |||||
| NAD+ | Male Wistar rats | 10–20 mg/kg intravenous (i.v) (approximately 85% reduction of the infarct at the dosage of 20 mg/kg) | A single dose immendiately before ischemia The rats were sacrificed 6 and 24 h after reperfusion. | Reduced the infarct size after ischemia/reperfusion Attenuated apoptotic damage and enhancing the antioxidant capacity | [159] |
| NAD+ | C57BL/6 wild-type mice | i.p. administration of 0.2 g/kg NAD | 1 dose before myocardial injury | Reduced myocardial infarct size after ischemia/reperfusion | [161] |
| NAD+ | Bama miniature pigs (a swine model of ischemia/reperfusion injury) | 20 mg/kg NAD+ or saline, i.v. | Before reperfusion | Dysinflammation, less cardiac fibrosis, and better ventricular compliance; reduced myocardial necrosis, and promoted cardiac function recovery | [162] |
| NAD+ | Specific-pathogen-free male Sprague-Dawley rats | 10 mg/kg i.p. | 14 days | Attenuation the depression of cardiac function in the isolated rat hearts after ischemia-reperfusion | [163] |
| NMN | C57BL/6 wild-type mice | administration of 0.5 g/kg i.p. | 30 min before ischemia and repetitive administration just before and during reperfusion | Reduced the infarct size after ischemia/reperfusion | [164] |
| NR | Male Wistar rats | i.v. infusion of 50 mg/kg NR | NR infusion for 5 min before and 15 min after the beginning of reperfusion | Restoration of small intestine microcirculation after mesenteric ischaemia/reperfusion; improved small intestine mucosa damage. | [167] |
| Cardiomyopathy | |||||
| NR soft pellets | Srfh−/− and Sf/Sf control littermates | Chow diet or NR-supplemented with 400 mg/Kg of body weight/day | 50 days | Protection against cardiac dysfunction (measure LVEF and FS, dilatation and thinning of the LV wall) | [171] |
| NR soft pellets or in water | LmnaH222P/H222P and wild-type mice | Chow diet or NR-supplemented with 400 mg/kg of body weight/day | 16 days | Increased NAD+ content in liver and heart and partially restore the left ventricular function and increase survival | [177] |
| NR soft pellets or in water | LmnaH222P/H222P mice and wild-type mice | For post-symptomatic treatment, LmnaH222P/H222P mice received 400 mg/kg per day orally by gavage | 9 weeks | Stable left ventricular dimensions and fractional shortening | [177] |
| NAM | LmnaH222P/H222P and wild-type mice | Received 500 mg/kg i.p. | every other day during 9 weeks | Treatment with NAM is not efficient to restore the cardiac NAD+ content and cardiac function | [177] |
| NR | C57BL/6 CD or HFD+L-NAME (HFpEF mice model) | 400 mg/kg body weight/d | 5 day per week for 4 weeks | Improved mitochondrial function, ameliorates cardiac hypertrophy, attenuates diastolic dysfunction, improves exercise capacity, and reduces lung capacity | [179] |
| NR medium and high dose | MutUNG1 mice and control littermates | CD, NR-supplemented with 400 mg/kg (medium dose) or 1,000 mg/kg (high dose) | 2 weeks | NR high dose: inhibits SIRT3 activity due to an enhance levels of NAM and promotes mitochondrial dysfunction. Reduction of NAD+ levels in cardiac tissue and loss of mitochondrial deacetylation | [182] |
| NMN | Myh6-Cre:Klf4 fl/fl mice, designated CM-K4KO (C57BL/6J background) | 500 mg/kg/day i.p. | 5 days | NMN protected the mutant mice from pressure overload-induced HF | [194] |
| NR | Mouse model of cardiac hypertrophy established using Transverse aortic constriction surgery (C57BL/6J background) | 400 mg/kg/day (daily oral gavage) | 8 weeks | NR alleviated from cardiac hypertrophy and dysfunction | [202] |
| Aortic Aneurysm | |||||
| NR | Marfan Syndrome mouse model Fbn1c1039g/+ | i.p. injections 1,000 mg/kg every second day | 28 days | Elevation of TFAM levels, improvement of mitochondrial metabolism, and normalization of aortic function and diameter | [221] |
| NA NAM | Apoe−/− mice infused with Ang II and C57BL/6J mouse CaCl2 induced AAA | Drinking water supplemented with NA 0.3% w/v, NAM 0.1% or 0.4% w/v | 2 days prior AAA induction to the end of the study | Protection against AAA formation mediated through NAD+ repletion that lead to SIRT1 activation | [24] |
| Me-NAM | Apoe−/− mice | Dietary supplementation of me-NAM (0.0057 and 0.017% w/w) in a high-fat diet containing 21% of fat and 0.2% cholesterol | 8 weeks | Reduced aortic root atherosclerotic area | [30] |
| Hypertension | |||||
| NA | Male Sprague-Dawley rats | NA dissolved in the drinking water (50 mg/kg/day) | 12 weeks | Ameliorated hypertension and partial reversal of upregulation of oxidative, inflammatory, and profibrotic mediators in the remnant kidney | [249] |
| NAD+ | Sirt1 transgenic and C57BL/6J mice | Incubation of NAD+ in whole aorta homogenates to measure SIRT1 deacetylase activity | 80 min | Improvement of vascular remodeling in the aortas of transgenic mice resulting in a decreased SBP | [244] |
| NADH | Spontaneously hypertensive male rats | 5 mg administered in single tablets daily | 60 days | Lower SPB in treated rats vs. non-treated ones | [248] |
| β-NAD+ and NAM | Sea urchin egg | Incubation in the medium, Various concentrations of β-NAD+ (0–4 mM) and nicotinamide (0–5 mM) | 90 min | vasorelaxation by inhibition of ADP ribosyl cyclase | [245] |
| β-NAD+ β-NADH NGD+ NGD and NAM | Male New Zeland white rabbit | Incubation in smooth muscle homogenates of pulmonary arteries β-NAD+ (2.5 mM) β-NADH (25 mM) NGD+ (250 µM) NGD+ (250 µM) + NAM (10 mM) | 60 min | Vasorelaxation by inhibition of ADP ribosyl cyclase | [247] |
| NAM | Sprague-Dawley rats, wild-type C57BL/6 mice, and CD38/mice on a C57BL6 background | Injection of 6 mg/kg/min in the renal artery | 3 min before and 5 min following endothelin-1 or sarafotoxin-6c injection | Vasorelaxation by inhibition of ADP ribosyl cyclase | [246] |
| NAM | Dahl salt-sensitive rats | 40 mM oral supplementation in the drinking water | 5 weeks | improved diastolic dysfunction | [31] |
| NAM | RUPP mice | Daily oral gavage (500 mg/kg/day) | In between 14.5 and 18.5 days postcoitus | Improving and preventing hypertension, fetal growth restriction, and premature birth | [250] |
| NAM | 1-Non-pregnant female C57BL/6J 2-Pregnant female ICR 3-Asb4−/− females | Daily oral gavage (500 mg/kg/day) | In between 12.5 and 18.5 days postcoitus | Improving and preventing hypertension, proteinuria, miscarriage, and premature birth in preeclampsia | [251] |
| NAM | 1-C57BL/6J male mice 2-Renin-transgenic male mice 3-eNOS-null female and male mice | NAM dissolved in the drinking water (500 mg/kg/day) L-NAME: 50 mg/kg/day in drinking water L-NAME + NAM same dose as above in drinking water | 60 days | Normalized blood pressure in mice with impaired eNOS function via suppressing inflammation | [252] |
| NMN | C57BL/6J mice | i.p. injection of NMN (500 mg/kg) | twice a day during 7 consecutive days | Preservation of myocardial NAD+ levels and functional compensation against pressure overload | [253] |
5. NAD+-Increasing Strategies in Human Heart Health: From Bench to Bed
Clinical interest in NAD+-increasing strategies is growing. The use of these compounds offers exciting new biological insights and therapeutic opportunities. However, the results from clinical trials investigating the impact of vitamin B3 intermediate-based therapies on combatting cardiovascular diseases are still scarce (see ongoing clinical trials in Table 2). Thus, we next discuss current research focusing on the impact of NAD+ precursors on the cardiovascular system.
5.1. NA
Historically, NA was one of the first drugs used to treat atherogenic hyperlipidemia by virtue of its contribution to reducing LDL cholesterol levels and increasing HDL-C levels [254] (Section 1). The AIM-HIGH trial did not demonstrate a potential benefit of using NA to reduce cardiovascular events in patients with atherosclerotic cardiovascular disease and optimally controlled LDL cholesterol levels by statin therapy [255]. The potential of NA as an NAD+ source has been elusive in former clinical trials [19], and its clinical use has been progressively reduced mainly due to its adverse side effects, such as flushing [20], despite the generation of new formulations, i.e., a currently used PGD2 receptor subtype 1 (DP1) blocker developed with the purpose of decreasing NA side effects [256].
Pellagra is a systemic disease resulting from severe vitamin B3 deficiency. Although symptomatic cardiac involvement is rather infrequent in subjects with pellagra, a recent case of pellagra in a female child was reported to present signs of dilated cardiomyopathy, as revealed by echocardiography. Notably, NA replacement positively influenced cardiac dysfunction [257].
5.2. NAM
The clinical use of NAM may also have benefits in the treatment of clinical myocarditis. This condition refers to heart inflammation that can be caused by infectious (viral)-related mechanisms [258] and displays signs similar to those of other causes of inflamed hearts, including cardiac amyloidosis and hypertrophic cardiomyopathy [259,260]. Previous data in the middle of the 20th century demonstrated that NA was effective in the treatment of myocarditis diagnosed on the basis of abnormal electrocardiograms [261,262].
The latter data might be of particular clinical interest in the context of the COVID-19 pandemic. Indeed, myocarditis is one of the clinical findings observed in subjects with SARS-CoV-2 infection [263], and a positive effect of NAM or any other NAD+ precursor could be hypothesized to prevent this adverse cardiac outcome of COVID-19. Notably, SARS-CoV-2 has been recently reported to directly infect cardiomyocytes of patients with COVID-19 myocarditis but not cardiac macrophages, fibroblasts, or endothelial cells [264]. Similar results have also been found in vitro using iPSC-human derived cardiomyocytes [265]. Interestingly, NAD+ depletion may occur secondarily to the activities induced by NAD+-consuming enzymes, i.e., SIRT1 and PARP, which are directly involved in the activation of intracellular immune defenses upon SARS-CoV-2 infection. These data might suggest that NAD+ depletion is critical in the pathogenesis of viral myocarditis and that administration of NAD+ precursors may serve as a promising therapy. Consistently, vitamin B3 intermediates may be effective in promoting innate and adaptive responses to SARS-CoV-2 infection [266,267,268]. In particular, NAM treatment has been effective for reducing adverse disease outcomes of COVID-19 syndrome in other systems apart from the respiratory system in infected subjects, including the renal system [269]. Therefore, NAM and other NAD+ precursors, i.e., NR, can be hypothesized to contribute to NAD+ replenishment and attenuate myocardial damage. In this context, a recent clinical trial aimed to assess whether NR administration would affect the clinical course of the disease; however, myocardial structure or function was not considered an outcome measure (https://clinicaltrials.gov/ct2/show/NCT04407390, accessed on 20 October 2021).
NAD+ elevation using NAM is currently under investigation to assess its influence on myocardial injury in patients undergoing on-pump cardiac surgery (https://clinicaltrials.gov/ct2/show/NCT04750616, accessed on 20 October 2021) (Table 2).
5.3. NR
Because NR may be a more suitable NAD+ precursor than NA and NAM [270], the first clinical trials used NR to assess its pharmacokinetics in humans. Clinical trials involving NR supplementation have shown that orally administered NR is well tolerated with no adverse events [54,271]. Single doses of 100, 300 and 1000 mg of NR produced dose-dependent increases in the blood NAD+ metabolome [54].
Diabetic cardiomyopathy, a risk factor for HF, may occur even in well-controlled asymptomatic diabetic patients [272]. Because exogenous administration of NAD+ improves the mitochondrial NAD+ pool and cardiac function [175], its supplementation either directly or indirectly using NAD+ precursors has been proposed to contribute to increasing the mitochondrial NAD+ pool and mitochondrial homeostasis and in turn benefit myocardial health. However, the potential use of such therapies in obese and diabetic hearts requires further investigation [272].
Oral NR administration attenuated proinflammatory activation of PBMCs in 4 of 19 patients with HF [105]. This observation is consistent with findings following 6-week oral NR administration (1000 mg per day) in healthy middle-aged and older humans, which revealed that such treatment reduced SBP and aortic stiffness, two major independent risk factors for incident cardiovascular events and disease with advancing age [270]. However, these observations have not yet been reproduced in other studies and are being addressed in a currently ongoing clinical trial (https://clinicaltrials.gov/ct2/show/NCT03821623, accessed on 20 October 2021). As mentioned previously, in a long-term human cohort study involving patients with HF with HFpEF, high dietary intake of naturally occurring NAD+ precursors was associated with lower blood pressure and a reduced risk of cardiac mortality, suggesting a potential role of NAD+ precursors in treating diastolic dysfunction and HFpEF in humans [31].
Other therapeutic approaches have already been approved; for instance, a phase II clinical trial to assess the efficiency of NR for HF treatment is expected to start soon (https://anr.fr/Project-ANR-17-CE17-0015, accessed on 20 October 2021). Interestingly, an interventional clinical trial with 30 participants with systolic HF is underway to determine the safety and tolerability of NR (https://clinicaltrials.gov/ct2/show/NCT03423342, accessed on 20 October 2021) (Table 2), although no results have been published yet. Another interventional randomized placebo-controlled trial with NR treatment in elective left ventricular assist device surgery has been scheduled to demonstrate whether subjects randomized to receive NR will have higher myocardial NAD+ levels, improved mitochondrial function, restored gene expression, and reduced inflammatory responses compared to participants randomized to the placebo group (https://clinicaltrials.gov/ct2/show/NCT04528004, accessed on 20 October 2021) (Table 2).
5.4. NMN
A recent study performed in 48 young middle-aged recreationally trained runners supplemented with NMN for 6 weeks revealed that exercise training combined with NMN further elevated the ventilatory threshold in amateur runners, most likely due to enhanced O2 utilization of skeletal muscle rather than cardiac muscle [273]. Although cardiac function was not analyzed in this study, recent data in aged Drosophila demonstrated that exercise training can improve lipotoxic cardiomyopathy induced by a high-fat diet [274,275]. Because activation of the cardiac NMNAT/NAD+/SIR2/FOXO and NMNAT/NAD+/SIR2/PGC-1α pathways was identified to mediate the beneficial effects of endurance training in this animal model, NMN administration can be hypothesized to further potentiate exercise resistance to high-fat diet-induced cardiomyopathy. Further investigation is warranted to directly address the potential positive influence of NMN on heart health in future clinical trials.

Table 2.
Current clinical trials of NAD+-increasing strategies to combat cardiovascular diseases.
Table 2.
Current clinical trials of NAD+-increasing strategies to combat cardiovascular diseases.
| Interventions | Aimed Cardiovascular-Related Outcomes | Study Start Date | Finish Date | Time Frame | Dosage | NCT |
|---|---|---|---|---|---|---|
| NA | Change in the mean severity of proximal stenosis | Jan 1984 | Aug 1989 | 2.5 years | NA was started at 125 mg twice a day and gradually increased to 500 mg four times a day (with meals and at bedtime) at one month and 1 g four times a day at two months. If the LDL cholesterol level did not fall below 3.1 mmol per liter (120 mg per deciliter) after three months, the dose of niacin was increased to 1.5 g (three tablets) four times a day, but no further | NCT00000512 |
| NA | Change in minimal diameter of coronary artery lesions | Dec 1986 | Nov 1992 | Not available | Not available | NCT00000461 |
| NA | Change in proximal obstructive disease | Sep 1994 | Aug 1999 | 2.5 years | Not available | NCT00000553 |
| NA | Change in plaque morphology | Jan 2000 | Sep 2005 | 12 months | NA 20 mg daily | NCT00307307 |
| NA | Changes in carotid plaque composition | Jun 2001 | Apr 2019 | 40 months | NA 2000 mg daily | NCT00715273 |
| NA | Inflammation and clot formation and blood vessel health | Jun 2002 | Nov 2005 | 16 weeks | NA 1500 mg daily | NCT00590629 |
| NA | Endothelial function | Jun 2003 | Jun 2005 | 16 weeks | NA 1.5 g daily | NCT01921010 |
| NA | Changes in aortic and carotid plaque architecture and composition | Sep 2003 | Dec 2008 | 18 months | NA extended release 0.5 to 3.0 g daily | NCT00127218 |
| NA | Change in superficial femoral artery wall volume | Apr 2004 | Dec 2021 | 24 months | NA 1500 mg daily | NCT00687076 |
| NA | Brachial artery flow mediated dilation | Sep 2005 | Aug 2008 | 3 months | NA extended release 1500 mg daily | NCT00150722 |
| NA | Relative effect on flow-mediated dilatation of radial artery | Mar 2006 | Jun 2009 | 6 months | NA extended-release | NCT00298909 |
| NA | Endothelial function by high resolution echography in response to nitric agent | Jun 2007 | May 2009 | 3 months | Not available | NCT00855257 |
| NA | Mean plaque lipid composition in carotid arteries | Mar 2008 | Feb 2015 | 24 months | NA extended-release 1500 mg or 2000 mg daily | NCT01178320 |
| NA | Composite score of plaque inflammation/stability, plaque instability protein composite score, total cholesterol, and free cholesterol | Apr 2009 | Oct 2010 | 12 weeks | NA extended-release tablet 2 g daily | NCT00804843 |
| NA | Endothelial dependant dilatation of the arterial wall | Sep 2010 | Oct 2011 | 12 weeks | NA 2000 mg/40 mg | NCT01126073 |
| NA | Change in percent atheroma volume by intravascular ultrasonography | Oct 2010 | Nov 2015 | 12 months | NA extended release 1500–2000 mg daily | NCT01221402 |
| NA | Change from baseline in arterial fluorodeoxyglucose uptake | Mar 2012 | Jan 2013 | 12 weeks | NA titrated to 6000 mg daily | NCT02003638 |
| NA | Changes in protein or lipid composition of any lipoprotein fraction and changes in vascular compliance | Mar 2015 | Jun 2019 | 14 weeks | NA extended release 2000 mg/day | NCT02322203 |
| NAM | Number of participants with adverse events (early onset Preeclampsia) | Aug 2014 | Nov 2018 | 48 h | Either 500 mg or 1000 mg by mouth each morning until delivery or 14 days, whichever occurs first | NCT02213094 |
| NAM | NAD+ augmentation in cardiac surgery associated myocardial injury trial. Troponin T (area under the curve) | Feb 2021 | Sep 2021 | From baseline to three days after surgery | 3 g on the day of surgery and post-surgical days one and two | NCT04750616 |
| NR | Mean IL-1beta release From peripheral blood mononuclear cells during refeeding after 24 h fast | Jun 2016 | Aug 2018 | 4 weeks | Either NR at 1000 mg/day or placebo for one week, followed by a washout period of 2–3 weeks, then a crossover to placebo or NR at 1000 mg/day for one additional week. The end point was analyzed at end of each treatment. | NCT02812238 |
| NR | Bioavailability (pharmacokinetics), safety (blood pressure, pulse, etc.) and impact on mitochondrial disease symptoms * | Dec 2017 | Dec 2019 | 24 h (bioavailability and safety) and 4 weeks (mitochondrial characteristics) | not defined (open-label experimental medicine study; all subjects will receive the same dosage of the supplement) | NCT03432871 |
| NR | Number of participants without heart failure linked inflammation in patients with stable, systolic heart failure | Jun 2018 | Oct 2020 | 12 weeks | Starting at 500 mg daily (250 mg BID) be increased at two weekly intervals by 250 mg/dose (BID) (500 mg/day) to a final dose of 1000 mg PO BID (2000 mg/day) | NCT03565328 |
| NR | Incidence of treatment-emergent adverse events (safety and tolerability), whereby the main aim was to assess the preoperative effect of NR supplementation in patients undergoing elective left ventricular assist device (LVAD) implantation | Nov 2018 | Sep 2020 | Up to 14 days | Dose Escalation: Day 1: 250 mg (1 capsule) twice daily (total daily intake = 500 mg) Day 2: 500 mg (2 capsules) twice daily Day 3: 1000 mg (4 capsules) twice daily (total daily intake = 2000 mg) Dose Maintenance: Day 4: 1000 mg (4 capsules) twice daily Day 5–14 as applicable through Day Before Surgery: 1000 mg (4 capsules) twice daily(total daily intake = 1000 mg) | NCT03727646 |
| NR | Exploratory endpoint: effect of NR on left ventricular diastolic and systolic function | May 2019 | Jun 2019 | 12 weeks | The initial dose will be 1 capsule twice daily, followed by weekly up-titration by 1 capsule/dose to a final dose of 4 capsules (1000 mg) twice daily at the end of week 4; participants will be continued on the final dose up to the final follow up visit (week 12) | NCT03423342 |
| NR | Carotid-femoral pulse wave velocity (primary) and systolic and diastolic blood pressure (secondary) | Nov 2019 | Sep 2014 | 3 months | 500 mg by mouth twice | NCT04040959 |
| NR | Systolic blood pressure | May 2019 | Dec 2023 | 3 months | 500 mg of the vitamin B3-precursor, nicotinamide riboside (NIAGEN) twice per day (1000 mg per day total) | NCT03821623 |
| NR | Between-group comparisons of myocardial NAD(H) levels, myocardial mitochondrial morphology, myocardial mitochondrial respiratory function, myocardial protein acetylation, myocardial gene expression by RNA-seq and the myocardial epigenome by ATAC-seq, inflammatory markers in myocardium | Sep 2020 | Aug 2024 | Up to 14 days | Dose Escalation: Day 1: 250 mg (1 capsule) twice daily (total daily intake = 500 mg) Day 2: 500 mg (2 capsules) twice daily Day 3: 1000 mg (4 capsules) twice daily (total daily intake = 2000 mg) Dose Maintenance: Day 4: 1000 mg (4 capsules) twice daily Day 5–14 as applicable through Day Before Surgery: 1000 mg (4 capsules) twice daily(total daily intake = 1000 mg) | NCT04528004 |
| NR | Change in Systolic blood pressure (primary), and change in arterial stiffness (secondary) | Jul 2020 | May 2022 | 6 week | 1000 mg/day | NCT04112043 |
| NMN | Effect of NMN on flow mediated dilation and brachial-ankle pulse wave velocity | Jun 2021 | Jul 2022 | 2 months | NMN10,000 WRIGHT LIFE® + lifestyle modification | NCT04903210 |
| NR | Vasodilatory Reserve (Percent change in systemic vascular resistance at baseline vs. exhaustion) and Kansas City Cardiomyopathy Questionnaire Overall Summary Score (Assess the impact of our interventions on quality of life) | Oct 2021 | Sep 2026 | 6 days | Potassium Nitrate (KNO3) 6 mmol three times daily + Propionyl-L-Carnitine (PLC) 1000 mg twice daily + NR 300 mg three times daily | NCT04913805 |
* studies were focused in mitochondrial diseases, including myopathies, in skeletal, not cardiac, muscle. Abbreviations were used: NAD: nicotinamide adenine dinucleotide; NA: nicotinic acid; NAM: nicotinamide; NMN: nicotinamide mononucleotide; NR: nicotinamide riboside; NCT, clinical trial identifier (ClinicalTrials.gov).
6. Concluding Remarks
In addition to the long time since the discovery of NAD+, a huge number of studies have been performed, although more work is required to fully understand its role in human diseases. Compelling evidence suggests that NAD+ homeostasis is required for normal cardiovascular function. Numerous studies suggest that declining NAD+ concomitant with mitochondrial dysfunction is a common trait in myocardial and cardiovascular diseases. Over the last few decades, the contribution of NAD+ precursor supplementation to increasing NAD+ levels and improving cardiovascular function in multiple preclinical animal models of several cardiovascular pathologies has attracted therapeutic interest [276]. Furthermore, except for NA, which causes some adverse clinical outcomes, vitamin B3 intermediates have been demonstrated to be safe and to have promising beneficial effects in combating cardiovascular diseases in vivo. Additional basic and translational research is needed to better understand the underlying mechanisms and consequences for cardiac and vascular structure and function. From a translational perspective and despite considerable current efforts, many questions remain in relation to the use of NAD+ precursors, including administration, optimal and safe doses, and the distribution of NAD+ in different tissues, to achieve the desired therapeutic efficacy. Recent and ongoing clinical trials are predominantly investigating NR, followed by NAM and then NMN, while NA is studied the least. Whether these NAD+-increasing therapies will favorably influence cardiovascular outcomes remains to be determined.
Author Contributions
Conceptualization and design, N.R., M.C. (Mercedes Camacho), J.C.E.-G., F.B.-V., and J.J.; writing—original draft preparation, N.R., M.C. (Mercedes Camacho), M.T., F.B.-V., and J.J.; writing—review and editing, N.R., M.C. (Mercedes Camacho), E.M.G.D.-A., M.C. (Marina Canyelles), S.B., N.A., K.A.M.-L., D.M., J.C.E.-G., F.B.-V., and J.J.; supervision, F.B.-V. and J.J.; funding acquisition, N.R., J.C.E.-G., F.B.-V., and J.J.; J.C.E.-G., F.B.-V. and J.J. are co-corresponding authors. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III (Madrid, Spain) grant FIS PI17/00232 (to J.J.), PI18/00164 (to F.B.-V.), FEDER “Una manera de hacer Europa”, and by Fundació La Marató de TV3 2016 (303/C/2016) (201602.30.31) (to N.A. and J.J.) E.M.G.D.-A. was recipient of The National Program of Foreign Postgraduate Scholarships “DON CARLOS ANTONIO LOPEZ” (BECAL) (BCAL04-451-3824321) by Ministerio de Educación (Republic of Paraguay). J.J. was recipient of a Miguel Servet Type 2 contract (CPII18/00004; ISCIII). This work was also funded by the Agencia Estatal de Investigación (AEI/10.13039/501100011033) within the Subprograma Ramón y Cajal (RYC-201722879) to NR. CIBER de Diabetes y Enfermedades Metabólicas Asociadas (CIBERDEM) is a project of Instituto de Salud Carlos III. J.J. is member of Red de Investigación en “Enfermedades Metabólicas y Cáncer” (RED2018-102799-T), Ministerio de Economía y Competitividad (MINECO), Madrid, Spain. Institut de Recerca de l’Hospital de la Santa Creu i Sant Pau is accredited by the Generalitat de Catalunya as Centre de Recerca de Catalunya (CERCA).
Acknowledgments
We thank Julia Niño for her exhaustive language review and David Santos for his technical support in generating data shown in Figure 2.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fajemiroye, J.O.; da Cunha, L.C.; Saavedra-Rodriguez, R.; Rodrigues, K.L.; Naves, L.M.; Mourao, A.A.; da Silva, E.F.; Williams, N.E.E.; Martins, J.L.R.; Sousa, R.B.; et al. Aging-Induced Biological Changes and Cardiovascular Diseases. Biomed. Res. Int. 2018, 2018, 7156435. [Google Scholar] [CrossRef] [Green Version]
- Srivastava, S. The Mitochondrial Basis of Aging and Age-Related Disorders. Genes 2017, 8, 398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prolla, T.A.; Denu, J.M. NAD+ deficiency in age-related mitochondrial dysfunction. Cell Metab. 2014, 19, 178–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schultz, M.B.; Sinclair, D.A. Why NAD(+) Declines during Aging: It’s Destroyed. Cell Metab. 2016, 23, 965–966. [Google Scholar] [CrossRef] [Green Version]
- Okabe, K.; Yaku, K.; Tobe, K.; Nakagawa, T. Implications of altered NAD metabolism in metabolic disorders. J. Biomed. Sci. 2019, 26, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, Q.; Zuo, W.; Liu, Y.; Wu, K.; Liu, Q. NAD(+) and cardiovascular diseases. Clin. Chim. Acta 2021, 515, 104–110. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, Y.; Sun, A.; Je, G. The effects of nicotinamide adenine dinucleotide in cardiovascular diseases: Molecular mechanisms, roles and therapeutic potential. Genes Dis. 2021, in press. [Google Scholar] [CrossRef]
- Yoshino, J.; Baur, J.A.; Imai, S.I. NAD(+) Intermediates: The Biology and Therapeutic Potential of NMN and NR. Cell Metab. 2018, 27, 513–528. [Google Scholar] [CrossRef] [Green Version]
- de Picciotto, N.E.; Gano, L.B.; Johnson, L.C.; Martens, C.R.; Sindler, A.L.; Mills, K.F.; Imai, S.; Seals, D.R. Nicotinamide mononucleotide supplementation reverses vascular dysfunction and oxidative stress with aging in mice. Aging Cell 2016, 15, 522–530. [Google Scholar] [CrossRef]
- Yoshino, J.; Mills, K.F.; Yoon, M.J.; Imai, S. Nicotinamide mononucleotide, a key NAD(+) intermediate, treats the pathophysiology of diet- and age-induced diabetes in mice. Cell Metab. 2011, 14, 528–536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, H.; Ryu, D.; Wu, Y.; Gariani, K.; Wang, X.; Luan, P.; D’Amico, D.; Ropelle, E.R.; Lutolf, M.P.; Aebersold, R.; et al. NAD(+) repletion improves mitochondrial and stem cell function and enhances life span in mice. Science 2016, 352, 1436–1443. [Google Scholar] [CrossRef] [Green Version]
- Canto, C.; Houtkooper, R.H.; Pirinen, E.; Youn, D.Y.; Oosterveer, M.H.; Cen, Y.; Fernandez-Marcos, P.J.; Yamamoto, H.; Andreux, P.A.; Cettour-Rose, P.; et al. The NAD(+) precursor nicotinamide riboside enhances oxidative metabolism and protects against high-fat diet-induced obesity. Cell Metab. 2012, 15, 838–847. [Google Scholar] [CrossRef] [Green Version]
- Mills, K.F.; Yoshida, S.; Stein, L.R.; Grozio, A.; Kubota, S.; Sasaki, Y.; Redpath, P.; Migaud, M.E.; Apte, R.S.; Uchida, K.; et al. Long-Term Administration of Nicotinamide Mononucleotide Mitigates Age-Associated Physiological Decline in Mice. Cell Metab. 2016, 24, 795–806. [Google Scholar] [CrossRef] [Green Version]
- Mendez-Lara, K.A.; Rodriguez-Millan, E.; Sebastian, D.; Blanco-Soto, R.; Camacho, M.; Nan, M.N.; Diarte-Anazco, E.M.G.; Mato, E.; Lope-Piedrafita, S.; Roglans, N.; et al. Nicotinamide Protects Against Diet-Induced Body Weight Gain, Increases Energy Expenditure, and Induces White Adipose Tissue Beiging. Mol. Nutr. Food Res. 2021, 65, e2100111. [Google Scholar] [CrossRef]
- Mitchell, S.J.; Bernier, M.; Aon, M.A.; Cortassa, S.; Kim, E.Y.; Fang, E.F.; Palacios, H.H.; Ali, A.; Navas-Enamorado, I.; Di Francesco, A.; et al. Nicotinamide Improves Aspects of Healthspan, but Not Lifespan, in Mice. Cell Metab. 2018, 27, 667–676.e4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajman, L.; Chwalek, K.; Sinclair, D.A. Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence. Cell Metab. 2018, 27, 529–547. [Google Scholar] [CrossRef] [Green Version]
- Masana, L.; Cabre, A.; Heras, M.; Amigo, N.; Correig, X.; Martinez-Hervas, S.; Real, J.T.; Ascaso, J.F.; Quesada, H.; Julve, J.; et al. Remarkable quantitative and qualitative differences in HDL after niacin or fenofibrate therapy in type 2 diabetic patients. Atherosclerosis 2015, 238, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Lukasova, M.; Hanson, J.; Tunaru, S.; Offermanns, S. Nicotinic acid (niacin): New lipid-independent mechanisms of action and therapeutic potentials. Trends Pharmacol. Sci. 2011, 32, 700–707. [Google Scholar] [CrossRef]
- Romani, M.; Hofer, D.C.; Katsyuba, E.; Auwerx, J. Niacin: An old lipid drug in a new NAD(+) dress. J. Lipid Res. 2019, 60, 741–746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, T.J.; Boden, W.E.; Desvigne-Nickens, P.; Fleg, J.L.; Kashyap, M.L.; McBride, R.; Probstfield, J.L. Safety profile of extended-release niacin in the AIM-HIGH trial. N. Engl. J. Med. 2014, 371, 288–290. [Google Scholar] [CrossRef] [Green Version]
- Investigators, A.-H.; Boden, W.E.; Probstfield, J.L.; Anderson, T.; Chaitman, B.R.; Desvignes-Nickens, P.; Koprowicz, K.; McBride, R.; Teo, K.; Weintraub, W. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N. Engl. J. Med. 2011, 365, 2255–2267. [Google Scholar] [CrossRef] [Green Version]
- HPS2-THRIVE Collaborative Group. HPS2-THRIVE randomi.ized placebo-controlled trial in 25,673 high-risk patients of ER niacin/laropiprant: Trial design, pre-specified muscle and liver outcomes, and reasons for stopping study treatment. Eur. Heart J. 2013, 34, 1279–1291. [Google Scholar] [CrossRef] [PubMed]
- Kong, D.; Li, J.; Shen, Y.; Liu, G.; Zuo, S.; Tao, B.; Ji, Y.; Lu, A.; Lazarus, M.; Breyer, R.M.; et al. Niacin Promotes Cardiac Healing after Myocardial Infarction through Activation of the Myeloid Prostaglandin D2 Receptor Subtype 1. J. Pharmacol. Exp. Ther. 2017, 360, 435–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horimatsu, T.; Blomkalns, A.L.; Ogbi, M.; Moses, M.; Kim, D.; Patel, S.; Gilreath, N.; Reid, L.; Benson, T.W.; Pye, J.; et al. Niacin protects against abdominal aortic aneurysm formation via GPR109A independent mechanisms: Role of NAD+/nicotinamide. Cardiovasc. Res. 2020, 116, 2226–2238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mendez-Lara, K.A.; Letelier, N.; Farre, N.; Diarte-Anazco, E.M.G.; Nieto-Nicolau, N.; Rodriguez-Millan, E.; Santos, D.; Pallares, V.; Escola-Gil, J.C.; Vazquez Del Olmo, T.; et al. Nicotinamide Prevents Apolipoprotein B-Containing Lipoprotein Oxidation, Inflammation and Atherosclerosis in Apolipoprotein E-Deficient Mice. Antioxidants 2020, 9, 1162. [Google Scholar] [CrossRef]
- Elliott, R.B.; Pilcher, C.C.; Stewart, A.; Fergusson, D.; McGregor, M.A. The use of nicotinamide in the prevention of type 1 diabetes. Ann. N. Y. Acad. Sci. 1993, 696, 333–341. [Google Scholar] [CrossRef]
- Gale, E.A.; Bingley, P.J.; Emmett, C.L.; Collier, T. European Nicotinamide Diabetes Intervention Trial (ENDIT): A randomised controlled trial of intervention before the onset of type 1 diabetes. Lancet 2004, 363, 925–931. [Google Scholar] [CrossRef]
- Hawrylyshyn, K.M. Nicotinamide Riboside Delivery Generates NAD+ Reserves to Protect Vascular Cells against Oxidative Damage; The University of Western Ontario: London, ON, USA, 2015. [Google Scholar]
- Mateuszuk, L.; Jasztal, A.; Maslak, E.; Gasior-Glogowska, M.; Baranska, M.; Sitek, B.; Kostogrys, R.; Zakrzewska, A.; Kij, A.; Walczak, M.; et al. Antiatherosclerotic Effects of 1-Methylnicotinamide in Apolipoprotein E/Low-Density Lipoprotein Receptor-Deficient Mice: A Comparison with Nicotinic Acid. J. Pharmacol. Exp. Ther. 2016, 356, 514–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, N.; Wang, M.; Song, J.; Liu, Y.; Chen, H.; Mu, D.; Xia, M. N-methylnicotinamide protects against endothelial dysfunction and attenuates atherogenesis in apolipoprotein E-deficient mice. Mol. Nutr. Food Res. 2016, 60, 1625–1636. [Google Scholar] [CrossRef]
- Abdellatif, M.; Trummer-Herbst, V.; Koser, F.; Durand, S.; Adao, R.; Vasques-Novoa, F.; Freundt, J.K.; Voglhuber, J.; Pricolo, M.R.; Kasa, M.; et al. Nicotinamide for the treatment of heart failure with preserved ejection fraction. Sci. Transl. Med. 2021, 13. [Google Scholar] [CrossRef]
- Bogan, K.L.; Brenner, C. Nicotinic acid, nicotinamide, and nicotinamide riboside: A molecular evaluation of NAD+ precursor vitamins in human nutrition. Annu. Rev. Nutr. 2008, 28, 115–130. [Google Scholar] [CrossRef] [Green Version]
- Canto, C.; Menzies, K.J.; Auwerx, J. NAD(+) Metabolism and the Control of Energy Homeostasis: A Balancing Act between Mitochondria and the Nucleus. Cell Metab. 2015, 22, 31–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magni, G.; Amici, A.; Emanuelli, M.; Orsomando, G.; Raffaelli, N.; Ruggieri, S. Enzymology of NAD+ homeostasis in man. Cell. Mol. Life Sci. 2004, 61, 19–34. [Google Scholar] [CrossRef]
- Houtkooper, R.H.; Canto, C.; Wanders, R.J.; Auwerx, J. The secret life of NAD+: An old metabolite controlling new metabolic signaling pathways. Endocr. Rev. 2010, 31, 194–223. [Google Scholar] [CrossRef] [Green Version]
- Chi, Y.; Sauve, A.A. Nicotinamide riboside, a trace nutrient in foods, is a vitamin B3 with effects on energy metabolism and neuroprotection. Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 657–661. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, R.; Forteza, M.J.; Ketelhuth, D.F.J. The interplay between cytokines and the Kynurenine pathway in inflammation and atherosclerosis. Cytokine 2019, 122, 154148. [Google Scholar] [CrossRef]
- Bender, D.A. Biochemistry of tryptophan in health and disease. Mol. Aspects Med. 1983, 6, 101–197. [Google Scholar] [CrossRef]
- Bieganowski, P.; Brenner, C. Discoveries of nicotinamide riboside as a nutrient and conserved NRK genes establish a Preiss-Handler independent route to NAD+ in fungi and humans. Cell 2004, 117, 495–502. [Google Scholar] [CrossRef] [Green Version]
- Sauve, A.A. NAD+ and vitamin B3: From metabolism to therapies. J. Pharmacol. Exp. Ther. 2008, 324, 883–893. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polyzos, K.A.; Ketelhuth, D.F. The role of the kynurenine pathway of tryptophan metabolism in cardiovascular disease. An emerging field. Hamostaseologie 2015, 35, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Minhas, P.S.; Liu, L.; Moon, P.K.; Joshi, A.U.; Dove, C.; Mhatre, S.; Contrepois, K.; Wang, Q.; Lee, B.A.; Coronado, M.; et al. Macrophage de novo NAD(+) synthesis specifies immune function in aging and inflammation. Nat. Immunol. 2019, 20, 50–63. [Google Scholar] [CrossRef]
- Kraus, D.; Yang, Q.; Kong, D.; Banks, A.S.; Zhang, L.; Rodgers, J.T.; Pirinen, E.; Pulinilkunnil, T.C.; Gong, F.; Wang, Y.C.; et al. Nicotinamide N-methyltransferase knockdown protects against diet-induced obesity. Nature 2014, 508, 258–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Felici, R.; Lapucci, A.; Ramazzotti, M.; Chiarugi, A. Insight into molecular and functional properties of NMNAT3 reveals new hints of NAD homeostasis within human mitochondria. PLoS ONE 2013, 8, e76938. [Google Scholar] [CrossRef]
- Weinshilboum, R. Methyltransferase pharmacogenetics. Pharmacol. Ther. 1989, 43, 77–90. [Google Scholar] [CrossRef]
- Bartus, M.; Lomnicka, M.; Kostogrys, R.B.; Kazmierczak, P.; Watala, C.; Slominska, E.M.; Smolenski, R.T.; Pisulewski, P.M.; Adamus, J.; Gebicki, J.; et al. 1-Methylnicotinamide (MNA) prevents endothelial dysfunction in hypertriglyceridemic and diabetic rats. Pharmacol. Rep. 2008, 60, 127–138. [Google Scholar]
- Chlopicki, S.; Swies, J.; Mogielnicki, A.; Buczko, W.; Bartus, M.; Lomnicka, M.; Adamus, J.; Gebicki, J. 1-Methylnicotinamide (MNA), a primary metabolite of nicotinamide, exerts anti-thrombotic activity mediated by a cyclooxygenase-2/prostacyclin pathway. Br. J. Pharmacol. 2007, 152, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Mateuszuk, L.; Khomich, T.I.; Slominska, E.; Gajda, M.; Wojcik, L.; Lomnicka, M.; Gwozdz, P.; Chlopicki, S. Activation of nicotinamide N-methyltrasferase and increased formation of 1-methylnicotinamide (MNA) in atherosclerosis. Pharmacol. Rep. 2009, 61, 76–85. [Google Scholar] [CrossRef] [Green Version]
- Sternak, M.; Khomich, T.I.; Jakubowski, A.; Szafarz, M.; Szczepanski, W.; Bialas, M.; Stojak, M.; Szymura-Oleksiak, J.; Chlopicki, S. Nicotinamide N-methyltransferase (NNMT) and 1-methylnicotinamide (MNA) in experimental hepatitis induced by concanavalin A in the mouse. Pharmacol. Rep. 2010, 62, 483–493. [Google Scholar] [CrossRef]
- Watala, C.; Kazmierczak, P.; Dobaczewski, M.; Przygodzki, T.; Bartus, M.; Lomnicka, M.; Slominska, E.M.; Durackova, Z.; Chlopicki, S. Anti-diabetic effects of 1-methylnicotinamide (MNA) in streptozocin-induced diabetes in rats. Pharmacol. Rep. 2009, 61, 86–98. [Google Scholar] [CrossRef]
- Fernstrom, J.D. A Perspective on the Safety of Supplemental Tryptophan Based on Its Metabolic Fates. J. Nutr. 2016, 146, 2601S–2608S. [Google Scholar] [CrossRef] [Green Version]
- EFSA. Scientific Opinion on the safety and efficacy of niacin (nicotinamide) as a feed additivefor all animal species based on a dossier submitted by EUROPE-ASIA Import Export GmbH. EFSA J. 2012, 10, 2789. [Google Scholar]
- McDowell, L.R. Vitamins in Animal and Human Nutrition, 2nd ed.; Wiley-Blackwell: Oxford, UK, 2000; p. 816. [Google Scholar]
- Trammell, S.A.; Schmidt, M.S.; Weidemann, B.J.; Redpath, P.; Jaksch, F.; Dellinger, R.W.; Li, Z.; Abel, E.D.; Migaud, M.E.; Brenner, C. Nicotinamide riboside is uniquely and orally bioavailable in mice and humans. Nat. Commun. 2016, 7, 12948. [Google Scholar] [CrossRef]
- Belenky, P.A.; Moga, T.G.; Brenner, C. Saccharomyces cerevisiae YOR071C encodes the high affinity nicotinamide riboside transporter Nrt1. J. Biol. Chem. 2008, 283, 8075–8079. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grozio, A.; Sociali, G.; Sturla, L.; Caffa, I.; Soncini, D.; Salis, A.; Raffaelli, N.; De Flora, A.; Nencioni, A.; Bruzzone, S. CD73 protein as a source of extracellular precursors for sustained NAD+ biosynthesis in FK866-treated tumor cells. J. Biol. Chem. 2013, 288, 25938–25949. [Google Scholar] [CrossRef] [Green Version]
- Hogan, K.A.; Chini, C.C.S.; Chini, E.N. The Multi-faceted Ecto-enzyme CD38: Roles in Immunomodulation, Cancer, Aging, and Metabolic Diseases. Front. Immunol. 2019, 10, 1187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grozio, A.; Mills, K.F.; Yoshino, J.; Bruzzone, S.; Sociali, G.; Tokizane, K.; Lei, H.C.; Cunningham, R.; Sasaki, Y.; Migaud, M.E.; et al. Slc12a8 is a nicotinamide mononucleotide transporter. Nat. Metab. 2019, 1, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Bruzzone, S.; Guida, L.; Zocchi, E.; Franco, L.; De Flora, A. Connexin 43 hemi channels mediate Ca2+-regulated transmembrane NAD+ fluxes in intact cells. FASEB J. 2001, 15, 10–12. [Google Scholar] [CrossRef]
- Ferrero, E.; Lo Buono, N.; Horenstein, A.L.; Funaro, A.; Malavasi, F. The ADP-ribosyl cyclases--the current evolutionary state of the ARCs. Front. Biosci. (Landmark Ed.) 2014, 19, 986–1002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwer, B.; Verdin, E. Conserved metabolic regulatory functions of sirtuins. Cell Metab. 2008, 7, 104–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, B.A.; Kraus, W.L. New insights into the molecular and cellular functions of poly(ADP-ribose) and PARPs. Nat. Rev. Mol. Cell Biol. 2012, 13, 411–424. [Google Scholar] [CrossRef]
- Belenky, P.; Bogan, K.L.; Brenner, C. NAD+ metabolism in health and disease. Trends Biochem. Sci. 2007, 32, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Canto, C.; Sauve, A.A.; Bai, P. Crosstalk between poly(ADP-ribose) polymerase and sirtuin enzymes. Mol. Aspects Med. 2013, 34, 1168–1201. [Google Scholar] [CrossRef] [Green Version]
- Clapham, D.E. Calcium signaling. Cell 2007, 131, 1047–1058. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.C. Physiological functions of cyclic ADP-ribose and NAADP as calcium messengers. Annu. Rev. Pharmacol. Toxicol. 2001, 41, 317–345. [Google Scholar] [CrossRef]
- Zocchi, E.; Daga, A.; Usai, C.; Franco, L.; Guida, L.; Bruzzone, S.; Costa, A.; Marchetti, C.; De Flora, A. Expression of CD38 increases intracellular calcium concentration and reduces doubling time in HeLa and 3T3 cells. J. Biol. Chem. 1998, 273, 8017–8024. [Google Scholar] [CrossRef] [Green Version]
- Ortolan, E.; Vacca, P.; Capobianco, A.; Armando, E.; Crivellin, F.; Horenstein, A.; Malavasi, F. CD157, the Janus of CD38 but with a unique personality. Cell Biochem. Funct. 2002, 20, 309–322. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C. Cyclic ADP-ribose and nicotinic acid adenine dinucleotide phosphate (NAADP) as messengers for calcium mobilization. J. Biol. Chem. 2012, 287, 31633–31640. [Google Scholar] [CrossRef] [Green Version]
- Steven, S.; Frenis, K.; Oelze, M.; Kalinovic, S.; Kuntic, M.; Bayo Jimenez, M.T.; Vujacic-Mirski, K.; Helmstadter, J.; Kroller-Schon, S.; Munzel, T.; et al. Vascular Inflammation and Oxidative Stress: Major Triggers for Cardiovascular Disease. Oxid. Med. Cell. Longev. 2019, 2019, 7092151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Betteridge, D.J. What is oxidative stress? Metabolism 2000, 49, 3–8. [Google Scholar] [CrossRef]
- Li, Y.; Huang, T.T.; Carlson, E.J.; Melov, S.; Ursell, P.C.; Olson, J.L.; Noble, L.J.; Yoshimura, M.P.; Berger, C.; Chan, P.H.; et al. Dilated cardiomyopathy and neonatal lethality in mutant mice lacking manganese superoxide dismutase. Nat. Genet. 1995, 11, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Ardanaz, N.; Yang, X.P.; Cifuentes, M.E.; Haurani, M.J.; Jackson, K.W.; Liao, T.D.; Carretero, O.A.; Pagano, P.J. Lack of glutathione peroxidase 1 accelerates cardiac-specific hypertrophy and dysfunction in angiotensin II hypertension. Hypertension 2010, 55, 116–123. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.; Chua, C.C.; Gao, J.; Chua, K.W.; Ho, Y.S.; Hamdy, R.C.; Chua, B.H. Prevention of ischemia/reperfusion-induced cardiac apoptosis and injury by melatonin is independent of glutathione peroxdiase 1. J. Pineal Res. 2009, 46, 235–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, C.; Zhang, H.; Qiao, Z.; Wang, Y.; Zhang, P.; Yang, D. Loss of thioredoxin 2 alters mitochondrial respiratory function and induces cardiomyocyte hypertrophy. Exp. Cell Res. 2018, 372, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Zhou, H.J.; Zhang, H.; Huang, Y.; Hinojosa-Kirschenbaum, F.; Fan, P.; Yao, L.; Belardinelli, L.; Tellides, G.; Giordano, F.J.; et al. Thioredoxin-2 inhibits mitochondrial reactive oxygen species generation and apoptosis stress kinase-1 activity to maintain cardiac function. Circulation 2015, 131, 1082–1097. [Google Scholar] [CrossRef] [Green Version]
- Ogata, S.; Takeuchi, M.; Teradaira, S.; Yamamoto, N.; Iwata, K.; Okumura, K.; Taguchi, H. Radical scavenging activities of niacin-related compounds. Biosci. Biotechnol. Biochem. 2002, 66, 641–645. [Google Scholar] [CrossRef] [PubMed]
- Kamat, J.P.; Devasagayam, T.P. Nicotinamide (vitamin B3) as an effective antioxidant against oxidative damage in rat brain mitochondria. Redox. Rep. 1999, 4, 179–184. [Google Scholar] [CrossRef] [Green Version]
- Osiecki, M.; Ghanavi, P.; Atkinson, K.; Nielsen, L.K.; Doran, M.R. The ascorbic acid paradox. Biochem. Biophys. Res. Commun. 2010, 400, 466–470. [Google Scholar] [CrossRef] [PubMed]
- Palozza, P.; Calviello, G.; Serini, S.; Maggiano, N.; Lanza, P.; Ranelletti, F.O.; Bartoli, G.M. beta-carotene at high concentrations induces apoptosis by enhancing oxy-radical production in human adenocarcinoma cells. Free Radic. Biol. Med. 2001, 30, 1000–1007. [Google Scholar] [CrossRef]
- Bergstrom, T.; Bergman, J.; Moller, L. Vitamin A and C compounds permitted in supplements differ in their abilities to affect cell viability, DNA and the DNA nucleoside deoxyguanosine. Mutagenesis 2011, 26, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Bergstrom, T.; Ersson, C.; Bergman, J.; Moller, L. Vitamins at physiological levels cause oxidation to the DNA nucleoside deoxyguanosine and to DNA--alone or in synergism with metals. Mutagenesis 2012, 27, 511–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Escola-Gil, J.C.; Rotllan, N.; Julve, J.; Blanco-Vaca, F. In vivo macrophage-specific RCT and antioxidant and antiinflammatory HDL activity measurements: New tools for predicting HDL atheroprotection. Atherosclerosis 2009, 206, 321–327. [Google Scholar] [CrossRef]
- Mendez-Lara, K.A.; Santos, D.; Farre, N.; Ruiz-Nogales, S.; Leanez, S.; Sanchez-Quesada, J.L.; Zapico, E.; Lerma, E.; Escola-Gil, J.C.; Blanco-Vaca, F.; et al. Administration of CORM-2 inhibits diabetic neuropathy but does not reduce dyslipidemia in diabetic mice. PLoS ONE 2018, 13, e0204841. [Google Scholar] [CrossRef] [Green Version]
- Elliott, R.B.; Chase, H.P. Prevention or delay of type 1 (insulin-dependent) diabetes mellitus in children using nicotinamide. Diabetologia 1991, 34, 362–365. [Google Scholar] [CrossRef] [Green Version]
- Hong, G.; Zheng, D.; Zhang, L.; Ni, R.; Wang, G.; Fan, G.C.; Lu, Z.; Peng, T. Administration of nicotinamide riboside prevents oxidative stress and organ injury in sepsis. Free Radic. Biol. Med. 2018, 123, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Mateuszuk, L.; Campagna, R.; Kutryb-Zajac, B.; Kus, K.; Slominska, E.M.; Smolenski, R.T.; Chlopicki, S. Reversal of endothelial dysfunction by nicotinamide mononucleotide via extracellular conversion to nicotinamide riboside. Biochem. Pharmacol. 2020, 178, 114019. [Google Scholar] [CrossRef]
- Gomes, A.P.; Price, N.L.; Ling, A.J.; Moslehi, J.J.; Montgomery, M.K.; Rajman, L.; White, J.P.; Teodoro, J.S.; Wrann, C.D.; Hubbard, B.P.; et al. Declining NAD(+) induces a pseudohypoxic state disrupting nuclear-mitochondrial communication during aging. Cell 2013, 155, 1624–1638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiss, T.; Giles, C.B.; Tarantini, S.; Yabluchanskiy, A.; Balasubramanian, P.; Gautam, T.; Csipo, T.; Nyul-Toth, A.; Lipecz, A.; Szabo, C.; et al. Nicotinamide mononucleotide (NMN) supplementation promotes anti-aging miRNA expression profile in the aorta of aged mice, predicting epigenetic rejuvenation and anti-atherogenic effects. Geroscience 2019, 41, 419–439. [Google Scholar] [CrossRef]
- Kang, H.; Park, Y.K.; Lee, J.Y. Nicotinamide riboside, an NAD(+) precursor, attenuates inflammation and oxidative stress by activating sirtuin 1 in alcohol-stimulated macrophages. Lab. Invest. 2021, 101, 1225–1237. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.M.; Castoldi, A.; Sanin, D.E.; Flachsmann, L.J.; Field, C.S.; Puleston, D.J.; Kyle, R.L.; Patterson, A.E.; Hassler, F.; Buescher, J.M.; et al. Inflammatory macrophage dependence on NAD(+) salvage is a consequence of reactive oxygen species-mediated DNA damage. Nat. Immunol. 2019, 20, 420–432. [Google Scholar] [CrossRef] [PubMed]
- Langston, P.K.; Shibata, M.; Horng, T. Metabolism Supports Macrophage Activation. Front. Immunol. 2017, 8, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiss, T.; Nyul-Toth, A.; Balasubramanian, P.; Tarantini, S.; Ahire, C.; Yabluchanskiy, A.; Csipo, T.; Farkas, E.; Wren, J.D.; Garman, L.; et al. Nicotinamide mononucleotide (NMN) supplementation promotes neurovascular rejuvenation in aged mice: Transcriptional footprint of SIRT1 activation, mitochondrial protection, anti-inflammatory, and anti-apoptotic effects. Geroscience 2020, 42, 527–546. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.; Schilling, E.; Grahnert, A.; Kolling, V.; Dorow, J.; Ceglarek, U.; Sack, U.; Hauschildt, S. Nicotinamide: A vitamin able to shift macrophage differentiation toward macrophages with restricted inflammatory features. Innate Immun. 2015, 21, 813–826. [Google Scholar] [CrossRef]
- Hiromatsu, Y.; Sato, M.; Tanaka, K.; Ishisaka, N.; Kamachi, J.; Nonaka, K. Inhibitory effects of nicotinamide on intercellular adhesion molecule-1 expression on cultured human thyroid cells. Immunology 1993, 80, 330–332. [Google Scholar]
- Hiromatsu, Y.; Sato, M.; Yamada, K.; Nonaka, K. Inhibitory effects of nicotinamide on recombinant human interferon-gamma-induced intercellular adhesion molecule-1 (ICAM-1) and HLA-DR antigen expression on cultured human endothelial cells. Immunol. Lett. 1992, 31, 35–39. [Google Scholar] [CrossRef]
- Biedron, R.; Ciszek, M.; Tokarczyk, M.; Bobek, M.; Kurnyta, M.; Slominska, E.M.; Smolenski, R.T.; Marcinkiewicz, J. 1-Methylnicotinamide and nicotinamide: Two related anti-inflammatory agents that differentially affect the functions of activated macrophages. Arch. Immunol. Ther. Exp. (Warsz) 2008, 56, 127–134. [Google Scholar] [CrossRef] [Green Version]
- Fukuzawa, M.; Satoh, J.; Muto, G.; Muto, Y.; Nishimura, S.; Miyaguchi, S.; Qiang, X.L.; Toyota, T. Inhibitory effect of nicotinamide on in vitro and in vivo production of tumor necrosis factor-alpha. Immunol. Lett. 1997, 59, 7–11. [Google Scholar] [CrossRef]
- Ungerstedt, J.S.; Heimersson, K.; Soderstrom, T.; Hansson, M. Nicotinamide inhibits endotoxin-induced monocyte tissue factor expression. J. Thromb. Haemost. 2003, 1, 2554–2560. [Google Scholar] [CrossRef] [Green Version]
- Ungerstedt, J.S.; Blomback, M.; Soderstrom, T. Nicotinamide is a potent inhibitor of proinflammatory cytokines. Clin. Exp. Immunol. 2003, 131, 48–52. [Google Scholar] [CrossRef]
- Grange, P.A.; Raingeaud, J.; Calvez, V.; Dupin, N. Nicotinamide inhibits Propionibacterium acnes-induced IL-8 production in keratinocytes through the NF-kappaB and MAPK pathways. J. Dermatol. Sci. 2009, 56, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Lappas, M.; Permezel, M. The anti-inflammatory and antioxidative effects of nicotinamide, a vitamin B(3) derivative, are elicited by FoxO3 in human gestational tissues: Implications for preterm birth. J. Nutr. Biochem. 2011, 22, 1195–1201. [Google Scholar] [CrossRef] [PubMed]
- Sack, M.N. Mitochondrial fidelity and metabolic agility control immune cell fate and function. J. Clin. Invest. 2018, 128, 3651–3661. [Google Scholar] [CrossRef]
- Kirkman, D.L.; Robinson, A.T.; Rossman, M.J.; Seals, D.R.; Edwards, D.G. Mitochondrial contributions to vascular endothelial dysfunction, arterial stiffness, and cardiovascular diseases. Am. J. Physiol. Heart Circ. Physiol. 2021, 320, H2080–H2100. [Google Scholar] [CrossRef]
- Zhou, B.; Wang, D.D.; Qiu, Y.; Airhart, S.; Liu, Y.; Stempien-Otero, A.; O’Brien, K.D.; Tian, R. Boosting NAD level suppresses inflammatory activation of PBMCs in heart failure. J. Clin. Invest. 2020, 130, 6054–6063. [Google Scholar] [CrossRef] [PubMed]
- Lenaz, G. Role of mitochondria in oxidative stress and ageing. Biochim. Biophys. Acta 1998, 1366, 53–67. [Google Scholar] [CrossRef] [Green Version]
- Wang, X. The expanding role of mitochondria in apoptosis. Genes Dev. 2001, 15, 2922–2933. [Google Scholar] [PubMed]
- Lai, Y.F.; Wang, L.; Liu, W.Y. Nicotinamide pretreatment alleviates mitochondrial stress and protects hypoxic myocardial cells via AMPK pathway. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 1797–1806. [Google Scholar] [PubMed]
- Tong, D.L.; Zhang, D.X.; Xiang, F.; Teng, M.; Jiang, X.P.; Hou, J.M.; Zhang, Q.; Huang, Y.S. Nicotinamide pretreatment protects cardiomyocytes against hypoxia-induced cell death by improving mitochondrial stress. Pharmacology 2012, 90, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Zhu, L.; Ruan, Z.B.; Wang, M.X.; Ren, Y.; Lu, W. Nicotinamide protects chronic hypoxic myocardial cells through regulating mTOR pathway and inducing autophagy. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 5503–5511. [Google Scholar]
- Unno, K.; Isobe, S.; Izawa, H.; Cheng, X.W.; Kobayashi, M.; Hirashiki, A.; Yamada, T.; Harada, K.; Ohshima, S.; Noda, A.; et al. Relation of functional and morphological changes in mitochondria to myocardial contractile and relaxation reserves in asymptomatic to mildly symptomatic patients with hypertrophic cardiomyopathy. Eur. Heart J. 2009, 30, 1853–1862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ren, J.; Pulakat, L.; Whaley-Connell, A.; Sowers, J.R. Mitochondrial biogenesis in the metabolic syndrome and cardiovascular disease. J. Mol. Med. 2010, 88, 993–1001. [Google Scholar] [CrossRef] [Green Version]
- Karamanlidis, G.; Lee, C.F.; Garcia-Menendez, L.; Kolwicz, S.C., Jr.; Suthammarak, W.; Gong, G.; Sedensky, M.M.; Morgan, P.G.; Wang, W.; Tian, R. Mitochondrial complex I deficiency increases protein acetylation and accelerates heart failure. Cell Metab. 2013, 18, 239–250. [Google Scholar] [CrossRef] [Green Version]
- Smyrnias, I.; Gray, S.P.; Okonko, D.O.; Sawyer, G.; Zoccarato, A.; Catibog, N.; Lopez, B.; Gonzalez, A.; Ravassa, S.; Diez, J.; et al. Cardioprotective Effect of the Mitochondrial Unfolded Protein Response During Chronic Pressure Overload. J. Am. Coll. Cardiol. 2019, 73, 1795–1806. [Google Scholar] [CrossRef] [PubMed]
- Chong, Z.Z.; Lin, S.H.; Maiese, K. The NAD+ precursor nicotinamide governs neuronal survival during oxidative stress through protein kinase B coupled to FOXO3a and mitochondrial membrane potential. J. Cereb. Blood Flow Metab. 2004, 24, 728–743. [Google Scholar] [CrossRef] [Green Version]
- Maiese, K. New Insights for nicotinamide: Metabolic disease, autophagy, and mTOR. Front. Biosci. 2020, 25, 1925–1973. [Google Scholar] [CrossRef] [PubMed]
- Marino, G.; Kroemer, G. Mechanisms of apoptotic phosphatidylserine exposure. Cell Res. 2013, 23, 1247–1248. [Google Scholar] [CrossRef] [Green Version]
- Pajuelo, D.; Gonzalez-Juarbe, N.; Tak, U.; Sun, J.; Orihuela, C.J.; Niederweis, M. NAD(+) Depletion Triggers Macrophage Necroptosis, a Cell Death Pathway Exploited by Mycobacterium tuberculosis. Cell Rep. 2018, 24, 429–440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crowley, C.L.; Payne, C.M.; Bernstein, H.; Bernstein, C.; Roe, D. The NAD+ precursors, nicotinic acid and nicotinamide protect cells against apoptosis induced by a multiple stress inducer, deoxycholate. Cell Death Differ. 2000, 7, 314–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, D.; Zhang, Y.; Zheng, M.; Cao, T.; Wang, G.; Zhang, L.; Ni, R.; Brockman, J.; Zhong, H.; Fan, G.C.; et al. Nicotinamide riboside promotes autolysosome clearance in preventing doxorubicin-induced cardiotoxicity. Clin. Sci. 2019, 133, 1505–1521. [Google Scholar] [CrossRef]
- Pham, T.X.; Bae, M.; Kim, M.B.; Lee, Y.; Hu, S.; Kang, H.; Park, Y.K.; Lee, J.Y. Nicotinamide riboside, an NAD+ precursor, attenuates the development of liver fibrosis in a diet-induced mouse model of liver fibrosis. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 2451–2463. [Google Scholar] [CrossRef] [PubMed]
- Traister, A.; Breitman, I.; Bar-Lev, E.; Zvibel, I.; Harel, A.; Halpern, Z.; Oren, R. Nicotinamide induces apoptosis and reduces collagen I and pro-inflammatory cytokines expression in rat hepatic stellate cells. Scand. J. Gastroenterol. 2005, 40, 1226–1234. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Lee, K.B.; Park, S.Y.; Jang, J.J. Nicotinamide inhibits hepatic fibrosis by suppressing DNA synthesis and enhancing apoptosis of hepatic stellate cells. Virchows Arch. 2011, 458, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Arauz, J.; Rivera-Espinoza, Y.; Shibayama, M.; Favari, L.; Flores-Beltran, R.E.; Muriel, P. Nicotinic acid prevents experimental liver fibrosis by attenuating the prooxidant process. Int. Immunopharmacol. 2015, 28, 244–251. [Google Scholar] [CrossRef]
- Wolf, D.; Ley, K. Immunity and Inflammation in Atherosclerosis. Circ. Res. 2019, 124, 315–327. [Google Scholar] [CrossRef] [PubMed]
- Mallat, Z. Macrophages. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 2509–2519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feil, S.; Fehrenbacher, B.; Lukowski, R.; Essmann, F.; Schulze-Osthoff, K.; Schaller, M.; Feil, R. Transdifferentiation of vascular smooth muscle cells to macrophage-like cells during atherogenesis. Circ. Res. 2014, 115, 662–667. [Google Scholar] [CrossRef]
- Sorci-Thomas, M.G.; Thomas, M.J. Microdomains, Inflammation, and Atherosclerosis. Circ. Res. 2016, 118, 679–691. [Google Scholar] [CrossRef] [Green Version]
- Williams, K.J.; Tabas, I. The response-to-retention hypothesis of early atherogenesis. Arterioscler. Thromb. Vasc. Biol. 1995, 15, 551–561. [Google Scholar] [CrossRef] [Green Version]
- Brattsand, R.; Petersen, H.; Lundholm, L. Action of niceritrol (pentaerythritoltetranicotinate) on lipid accumulation in aortas of cholesterol-fed rabbits independent of contemporary reduction of serum lipids. Atherosclerosis 1974, 20, 469–479. [Google Scholar] [CrossRef]
- Brattsand, R. The effect of niceritrol (pentaerythritoltetranicotinate) and clofibrate upon hyperlipemia and atherosclerosis induced in rabbits by cholesterol-free semisynthetic diets. Atherosclerosis 1974, 20, 453–467. [Google Scholar] [CrossRef]
- Brattsand, R.; Lundholm, L. The effect of nicotinic acid and pentaerythritolteranicotinate upon experimental atherosclerosis in the rabbit. Atherosclerosis 1971, 14, 91–105. [Google Scholar] [CrossRef]
- Brattsand, R. Actions of vitamins A and E and some nicotinic acid derivatives on plasma lipids and on lipid infiltration of aorta in cholesterol-fed rabbits. Atherosclerosis 1975, 22, 47–61. [Google Scholar] [CrossRef]
- Lundholm, L.; Jacobsson, L.; Brattsand, R.; Magnusson, O. Influence of nicotinic acid, niceritrol and beta-pyridylcarbinol on experimental hyperlipidemia and atherosclerosis in mini-pigs. Atherosclerosis 1978, 29, 217–239. [Google Scholar] [CrossRef]
- Ost, C.R.; Stenson, S. Regression of peripheral atherosclerosis during therapy with high doses of nicotinic acid. Scand. J. Clin. Lab. Invest. Suppl. 1967, 99, 241–245. [Google Scholar]
- Lee, J.M.; Robson, M.D.; Yu, L.M.; Shirodaria, C.C.; Cunnington, C.; Kylintireas, I.; Digby, J.E.; Bannister, T.; Handa, A.; Wiesmann, F.; et al. Effects of high-dose modified-release nicotinic acid on atherosclerosis and vascular function: A randomized, placebo-controlled, magnetic resonance imaging study. J. Am. Coll. Cardiol. 2009, 54, 1787–1794. [Google Scholar] [CrossRef] [PubMed]
- Lukasova, M.; Malaval, C.; Gille, A.; Kero, J.; Offermanns, S. Nicotinic acid inhibits progression of atherosclerosis in mice through its receptor GPR109A expressed by immune cells. J. Clin. Invest. 2011, 121, 1163–1173. [Google Scholar] [CrossRef] [Green Version]
- Holzhauser, E.; Albrecht, C.; Zhou, Q.; Buttler, A.; Preusch, M.R.; Blessing, E.; Katus, H.A.; Bea, F. Nicotinic acid has anti-atherogenic and anti-inflammatory properties on advanced atherosclerotic lesions independent of its lipid-modifying capabilities. J. Cardiovasc. Pharmacol. 2011, 57, 447–454. [Google Scholar] [CrossRef]
- Strack, A.M.; Carballo-Jane, E.; Wang, S.P.; Xue, J.; Ping, X.; McNamara, L.A.; Thankappan, A.; Price, O.; Wolff, M.; Wu, T.J.; et al. Nicotinic acid and DP1 blockade: Studies in mouse models of atherosclerosis. J. Lipid Res. 2013, 54, 177–188. [Google Scholar] [CrossRef] [Green Version]
- Declercq, V.; Yeganeh, B.; Moshtaghi-Kashanian, G.R.; Khademi, H.; Bahadori, B.; Moghadasian, M.H. Paradoxical effects of fenofibrate and nicotinic acid in apo E-deficient mice. J. Cardiovasc. Pharmacol. 2005, 46, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Kuhnast, S.; Louwe, M.C.; Heemskerk, M.M.; Pieterman, E.J.; van Klinken, J.B.; van den Berg, S.A.; Smit, J.W.; Havekes, L.M.; Rensen, P.C.; van der Hoorn, J.W.; et al. Niacin Reduces Atherosclerosis Development in APOE*3Leiden.CETP Mice Mainly by Reducing NonHDL-Cholesterol. PLoS ONE 2013, 8, e66467. [Google Scholar] [CrossRef] [Green Version]
- Kane, A.E.; Sinclair, D.A. Sirtuins and NAD(+) in the Development and Treatment of Metabolic and Cardiovascular Diseases. Circ. Res. 2018, 123, 868–885. [Google Scholar] [CrossRef]
- Li, X.; Zhang, S.; Blander, G.; Tse, J.G.; Krieger, M.; Guarente, L. SIRT1 deacetylates and positively regulates the nuclear receptor LXR. Mol. Cell 2007, 28, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Mendez-Lara, K.A.; Santos, D.; Farre, N.; Nan, M.N.; Pallares, V.; Perez-Perez, A.; Alonso, N.; Escola-Gil, J.C.; Blanco-Vaca, F.; Julve, J. Vitamin B3 impairs reverse cholesterol transport in Apolipoprotein E-deficient mice. Clin. Investig. Arterioscler. 2019, 31, 251–260. [Google Scholar] [PubMed]
- Nencioni, A.; da Silva, R.F.; Fraga-Silva, R.A.; Steffens, S.; Fabre, M.; Bauer, I.; Caffa, I.; Magnone, M.; Sociali, G.; Quercioli, A.; et al. Nicotinamide phosphoribosyltransferase inhibition reduces intraplaque CXCL1 production and associated neutrophil infiltration in atherosclerotic mice. Thromb. Haemost. 2014, 111, 308–322. [Google Scholar]
- Li, S.; Wang, C.; Li, K.; Li, L.; Tian, M.; Xie, J.; Yang, M.; Jia, Y.; He, J.; Gao, L.; et al. NAMPT knockdown attenuates atherosclerosis and promotes reverse cholesterol transport in ApoE KO mice with high-fat-induced insulin resistance. Sci. Rep. 2016, 6, 26746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kong, Y.Y.; Li, G.Q.; Zhang, W.J.; Hua, X.; Zhou, C.C.; Xu, T.Y.; Li, Z.Y.; Wang, P.; Miao, C.Y. Nicotinamide phosphoribosyltransferase aggravates inflammation and promotes atherosclerosis in ApoE knockout mice. Acta Pharmacol. Sin. 2019, 40, 1184–1192. [Google Scholar] [CrossRef]
- Bermudez, B.; Dahl, T.B.; Medina, I.; Groeneweg, M.; Holm, S.; Montserrat-de la Paz, S.; Rousch, M.; Otten, J.; Herias, V.; Varela, L.M.; et al. Leukocyte Overexpression of Intracellular NAMPT Attenuates Atherosclerosis by Regulating PPARgamma-Dependent Monocyte Differentiation and Function. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 1157–1167. [Google Scholar] [CrossRef] [Green Version]
- Xu, S.; Bai, P.; Little, P.J.; Liu, P. Poly(ADP-ribose) polymerase 1 (PARP1) in atherosclerosis: From molecular mechanisms to therapeutic implications. Med. Res. Rev. 2014, 34, 644–675. [Google Scholar] [CrossRef]
- Oumouna-Benachour, K.; Hans, C.P.; Suzuki, Y.; Naura, A.; Datta, R.; Belmadani, S.; Fallon, K.; Woods, C.; Boulares, A.H. Poly(ADP-ribose) polymerase inhibition reduces atherosclerotic plaque size and promotes factors of plaque stability in apolipoprotein E-deficient mice: Effects on macrophage recruitment, nuclear factor-kappaB nuclear translocation, and foam cell death. Circulation 2007, 115, 2442–2450. [Google Scholar] [CrossRef] [Green Version]
- von Lukowicz, T.; Hassa, P.O.; Lohmann, C.; Boren, J.; Braunersreuther, V.; Mach, F.; Odermatt, B.; Gersbach, M.; Camici, G.G.; Stahli, B.E.; et al. PARP1 is required for adhesion molecule expression in atherogenesis. Cardiovasc. Res. 2008, 78, 158–166. [Google Scholar] [CrossRef]
- Hans, C.P.; Zerfaoui, M.; Naura, A.S.; Catling, A.; Boulares, A.H. Differential effects of PARP inhibition on vascular cell survival and ACAT-1 expression favouring atherosclerotic plaque stability. Cardiovasc. Res. 2008, 78, 429–439. [Google Scholar] [CrossRef]
- Hans, C.P.; Zerfaoui, M.; Naura, A.S.; Troxclair, D.; Strong, J.P.; Matrougui, K.; Boulares, A.H. Thieno[2,3-c]isoquinolin-5-one, a potent poly(ADP-ribose) polymerase inhibitor, promotes atherosclerotic plaque regression in high-fat diet-fed apolipoprotein E-deficient mice: Effects on inflammatory markers and lipid content. J. Pharmacol. Exp. Ther. 2009, 329, 150–158. [Google Scholar] [CrossRef] [Green Version]
- Zha, S.; Wang, F.; Li, Z.; Ma, Z.; Yang, L.; Liu, F. PJ34, a PARP1 inhibitor, promotes endothelial repair in a rabbit model of high fat diet-induced atherosclerosis. Cell Cycle 2019, 18, 2099–2109. [Google Scholar] [CrossRef]
- Lindsey, M.L.; Bolli, R.; Canty, J.M., Jr.; Du, X.J.; Frangogiannis, N.G.; Frantz, S.; Gourdie, R.G.; Holmes, J.W.; Jones, S.P.; Kloner, R.A.; et al. Guidelines for experimental models of myocardial ischemia and infarction. Am. J. Physiol. Heart Circ. Physiol. 2018, 314, H812–H838. [Google Scholar] [CrossRef] [PubMed]
- Nunez, R.; Calva, E.; Marsh, M. Nicotinamide adenine dinucleotide degradation in infarcted cardiac muscle. Recent Adv. Stud. Cardiac Struct. Metab. 1975, 10, 241–250. [Google Scholar]
- Nunez, R.; Calva, E.; Marsch, M.; Briones, E.; Lopez-Soriano, F. NAD glycohydrolase activity in hearts with acute experimental infarction. Am. J. Physiol. 1976, 231, 1173–1177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, H.H.; Schaper, J.; Puschmann, S.; Nienaber, C.; Kreuzer, H.; Schaper, W. Loss of canine myocardial nicotinamide adenine dinucleotides determines the transition from reversible to irreversible ischemic damage of myocardial cells. Basic Res. Cardiol. 1981, 76, 612–621. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, B.; Fu, X.; Guan, S.; Han, W.; Zhang, J.; Gan, Q.; Fang, W.; Ying, W.; Qu, X. Exogenous NAD(+) administration significantly protects against myocardial ischemia/reperfusion injury in rat model. Am. J. Transl. Res. 2016, 8, 3342–3350. [Google Scholar] [PubMed]
- Hsu, C.P.; Oka, S.; Shao, D.; Hariharan, N.; Sadoshima, J. Nicotinamide phosphoribosyltransferase regulates cell survival through NAD+ synthesis in cardiac myocytes. Circ. Res. 2009, 105, 481–491. [Google Scholar] [CrossRef] [Green Version]
- Guan, X.H.; Liu, X.H.; Hong, X.; Zhao, N.; Xiao, Y.F.; Wang, L.F.; Tang, L.; Jiang, K.; Qian, Y.S.; Deng, K.Y.; et al. CD38 Deficiency Protects the Heart from Ischemia/Reperfusion Injury through Activating SIRT1/FOXOs-Mediated Antioxidative Stress Pathway. Oxid. Med. Cell. Longev. 2016, 2016, 7410257. [Google Scholar] [CrossRef] [Green Version]
- Zhai, X.; Han, W.; Wang, M.; Guan, S.; Qu, X. Exogenous supplemental NAD+ protect myocardium against myocardial ischemic/reperfusion injury in swine model. Am. J. Transl. Res. 2019, 11, 6066–6074. [Google Scholar] [PubMed]
- Liu, L.; Wang, Q.; Zhao, B.; Wu, Q.; Wang, P. Exogenous nicotinamide adenine dinucleotide administration alleviates ischemia/reperfusion-induced oxidative injury in isolated rat hearts via Sirt5-SDH-succinate pathway. Eur. J. Pharmacol. 2019, 858, 172520. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Byun, J.; Zhai, P.; Ikeda, Y.; Oka, S.; Sadoshima, J. Nicotinamide mononucleotide, an intermediate of NAD+ synthesis, protects the heart from ischemia and reperfusion. PLoS ONE 2014, 9, e98972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosseini, L.; Vafaee, M.S.; Badalzadeh, R. Melatonin and Nicotinamide Mononucleotide Attenuate Myocardial Ischemia/Reperfusion Injury via Modulation of Mitochondrial Function and Hemodynamic Parameters in Aged Rats. J. Cardiovasc. Pharmacol. Ther. 2020, 25, 240–250. [Google Scholar] [CrossRef]
- Ahmad, F.; Tomar, D.; Aryal, A.C.S.; Elmoselhi, A.B.; Thomas, M.; Elrod, J.W.; Tilley, D.G.; Force, T. Nicotinamide riboside kinase-2 alleviates ischemia-induced heart failure through P38 signaling. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165609. [Google Scholar] [CrossRef] [PubMed]
- Toropova, Y.G.; Pechnikova, N.A.; Zelinskaya, I.A.; Zhuravsky, S.G.; Kornyushin, O.V.; Gonchar, A.I.; Ivkin, D.Y.; Leonova, Y.V.; Karev, V.E.; Karabak, I.A. Nicotinamide riboside has protective effects in a rat model of mesenteric ischaemia-reperfusion. Int. J. Exp. Pathol. 2018, 99, 304–311. [Google Scholar] [CrossRef]
- Pinto, Y.M.; Elliott, P.M.; Arbustini, E.; Adler, Y.; Anastasakis, A.; Bohm, M.; Duboc, D.; Gimeno, J.; de Groote, P.; Imazio, M.; et al. Proposal for a revised definition of dilated cardiomyopathy, hypokinetic non-dilated cardiomyopathy, and its implications for clinical practice: A position statement of the ESC working group on myocardial and pericardial diseases. Eur. Heart J. 2016, 37, 1850–1858. [Google Scholar] [CrossRef] [Green Version]
- Ussher, J.R.; Jaswal, J.S.; Lopaschuk, G.D. Pyridine nucleotide regulation of cardiac intermediary metabolism. Circ. Res. 2012, 111, 628–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, C.F.; Tian, R. Mitochondrion as a Target for Heart Failure Therapy- Role of Protein Lysine Acetylation. Circ. J. 2015, 79, 1863–1870. [Google Scholar] [CrossRef] [Green Version]
- Diguet, N.; Trammell, S.A.J.; Tannous, C.; Deloux, R.; Piquereau, J.; Mougenot, N.; Gouge, A.; Gressette, M.; Manoury, B.; Blanc, J.; et al. Nicotinamide Riboside Preserves Cardiac Function in a Mouse Model of Dilated Cardiomyopathy. Circulation 2018, 137, 2256–2273. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.F.; Chavez, J.D.; Garcia-Menendez, L.; Choi, Y.; Roe, N.D.; Chiao, Y.A.; Edgar, J.S.; Goo, Y.A.; Goodlett, D.R.; Bruce, J.E.; et al. Normalization of NAD+ Redox Balance as a Therapy for Heart Failure. Circulation 2016, 134, 883–894. [Google Scholar] [CrossRef] [Green Version]
- Martin, A.S.; Abraham, D.M.; Hershberger, K.A.; Bhatt, D.P.; Mao, L.; Cui, H.; Liu, J.; Liu, X.; Muehlbauer, M.J.; Grimsrud, P.A.; et al. Nicotinamide mononucleotide requires SIRT3 to improve cardiac function and bioenergetics in a Friedreich’s ataxia cardiomyopathy model. JCI Insight 2017, 2, e93885. [Google Scholar] [CrossRef] [Green Version]
- Horton, J.L.; Martin, O.J.; Lai, L.; Riley, N.M.; Richards, A.L.; Vega, R.B.; Leone, T.C.; Pagliarini, D.J.; Muoio, D.M.; Bedi, K.C., Jr.; et al. Mitochondrial protein hyperacetylation in the failing heart. JCI Insight 2016, 2, e84897. [Google Scholar] [CrossRef]
- Pillai, V.B.; Sundaresan, N.R.; Kim, G.; Gupta, M.; Rajamohan, S.B.; Pillai, J.B.; Samant, S.; Ravindra, P.V.; Isbatan, A.; Gupta, M.P. Exogenous NAD blocks cardiac hypertrophic response via activation of the SIRT3-LKB1-AMP-activated kinase pathway. J. Biol. Chem. 2010, 285, 3133–3144. [Google Scholar] [CrossRef] [Green Version]
- Fatkin, D.; MacRae, C.; Sasaki, T.; Wolff, M.R.; Porcu, M.; Frenneaux, M.; Atherton, J.; Vidaillet, H.J., Jr.; Spudich, S.; De Girolami, U.; et al. Missense mutations in the rod domain of the lamin A/C gene as causes of dilated cardiomyopathy and conduction-system disease. N. Engl. J. Med. 1999, 341, 1715–1724. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vignier, N.; Chatzifrangkeskou, M.; Morales Rodriguez, B.; Mericskay, M.; Mougenot, N.; Wahbi, K.; Bonne, G.; Muchir, A. Rescue of biosynthesis of nicotinamide adenine dinucleotide protects the heart in cardiomyopathy caused by lamin A/C gene mutation. Hum. Mol. Genet. 2018, 27, 3870–3880. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef]
- Tong, D.; Schiattarella, G.G.; Jiang, N.; Altamirano, F.; Szweda, P.A.; Elnwasany, A.; Lee, D.I.; Yoo, H.; Kass, D.A.; Szweda, L.I.; et al. NAD(+) Repletion Reverses Heart Failure With Preserved Ejection Fraction. Circ. Res. 2021, 128, 1629–1641. [Google Scholar] [CrossRef]
- Tannous, C.; Deloux, R.; Karoui, A.; Mougenot, N.; Burkin, D.; Blanc, J.; Coletti, D.; Lavery, G.; Li, Z.; Mericskay, M. NMRK2 Gene Is Upregulated in Dilated Cardiomyopathy and Required for Cardiac Function and NAD Levels during Aging. Int. J. Mol. Sci. 2021, 22, 3534. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Barrientos, T.; Mao, L.; Rockman, H.A.; Sauve, A.A.; Andrews, N.C. Lethal Cardiomyopathy in Mice Lacking Transferrin Receptor in the Heart. Cell Rep. 2015, 13, 533–545. [Google Scholar] [CrossRef] [Green Version]
- Lauritzen, K.H.; Olsen, M.B.; Ahmed, M.S.; Yang, K.; Rinholm, J.E.; Bergersen, L.H.; Esbensen, Q.Y.; Sverkeli, L.J.; Ziegler, M.; Attramadal, H.; et al. Instability in NAD(+) metabolism leads to impaired cardiac mitochondrial function and communication. Elife 2021, 10, e59828. [Google Scholar] [CrossRef] [PubMed]
- Byun, J.; Oka, S.I.; Imai, N.; Huang, C.Y.; Ralda, G.; Zhai, P.; Ikeda, Y.; Ikeda, S.; Sadoshima, J. Both gain and loss of Nampt function promote pressure overload-induced heart failure. Am. J. Physiol. Heart Circ. Physiol. 2019, 317, H711–H725. [Google Scholar] [CrossRef]
- Wu, K.; Li, B.; Lin, Q.; Xu, W.; Zuo, W.; Li, J.; Liu, N.; Tu, T.; Zhang, B.; Xiao, Y.; et al. Nicotinamide mononucleotide attenuates isoproterenol-induced cardiac fibrosis by regulating oxidative stress and Smad3 acetylation. Life Sci. 2021, 274, 119299. [Google Scholar] [CrossRef]
- Francis, G.S. Diabetic cardiomyopathy: Fact or fiction? Heart 2001, 85, 247–248. [Google Scholar] [CrossRef] [Green Version]
- Picano, E. Diabetic cardiomyopathy. the importance of being earliest. J. Am. Coll. Cardiol. 2003, 42, 454–457. [Google Scholar] [CrossRef] [Green Version]
- Avogaro, A.; Vigili de Kreutzenberg, S.; Negut, C.; Tiengo, A.; Scognamiglio, R. Diabetic cardiomyopathy: A metabolic perspective. Am. J. Cardiol. 2004, 93, 13A–16A. [Google Scholar] [CrossRef] [PubMed]
- Trammell, S.A.; Weidemann, B.J.; Chadda, A.; Yorek, M.S.; Holmes, A.; Coppey, L.J.; Obrosov, A.; Kardon, R.H.; Yorek, M.A.; Brenner, C. Nicotinamide Riboside Opposes Type 2 Diabetes and Neuropathy in Mice. Sci. Rep. 2016, 6, 26933. [Google Scholar] [CrossRef] [Green Version]
- Ido, Y.; Kilo, C.; Williamson, J.R. Cytosolic NADH/NAD+, free radicals, and vascular dysfunction in early diabetes mellitus. Diabetologia 1997, 40 (Suppl. 2), S115–S117. [Google Scholar] [CrossRef] [Green Version]
- Williamson, J.R.; Chang, K.; Frangos, M.; Hasan, K.S.; Ido, Y.; Kawamura, T.; Nyengaard, J.R.; van den Enden, M.; Kilo, C.; Tilton, R.G. Hyperglycemic pseudohypoxia and diabetic complications. Diabetes 1993, 42, 801–813. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Jin, Z.; Zheng, H.; Yan, L.J. Sources and implications of NADH/NAD(+) redox imbalance in diabetes and its complications. Diabetes Metab. Syndr. Obes. 2016, 9, 145–153. [Google Scholar]
- Berthiaume, J.M.; Hsiung, C.H.; Austin, A.B.; McBrayer, S.P.; Depuydt, M.M.; Chandler, M.P.; Miyagi, M.; Rosca, M.G. Methylene blue decreases mitochondrial lysine acetylation in the diabetic heart. Mol. Cell. Biochem. 2017, 432, 7–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vazquez, E.J.; Berthiaume, J.M.; Kamath, V.; Achike, O.; Buchanan, E.; Montano, M.M.; Chandler, M.P.; Miyagi, M.; Rosca, M.G. Mitochondrial complex I defect and increased fatty acid oxidation enhance protein lysine acetylation in the diabetic heart. Cardiovasc. Res. 2015, 107, 453–465. [Google Scholar] [CrossRef] [Green Version]
- Zhang, R.; Shen, Y.; Zhou, L.; Sangwung, P.; Fujioka, H.; Zhang, L.; Liao, X. Short-term administration of Nicotinamide Mononucleotide preserves cardiac mitochondrial homeostasis and prevents heart failure. J. Mol. Cell. Cardiol. 2017, 112, 64–73. [Google Scholar] [CrossRef]
- Chiao, Y.A.; Chakraborty, A.D.; Light, C.M.; Tian, R.; Sadoshima, J.; Shi, X.; Gu, H.; Lee, C.F. NAD(+) Redox Imbalance in the Heart Exacerbates Diabetic Cardiomyopathy. Circ. Heart Fail. 2021, 14, e008170. [Google Scholar] [CrossRef] [PubMed]
- Liao, X.; Haldar, S.M.; Lu, Y.; Jeyaraj, D.; Paruchuri, K.; Nahori, M.; Cui, Y.; Kaestner, K.H.; Jain, M.K. Kruppel-like factor 4 regulates pressure-induced cardiac hypertrophy. J. Mol. Cell. Cardiol. 2010, 49, 334–338. [Google Scholar] [CrossRef] [Green Version]
- Liao, X.; Zhang, R.; Lu, Y.; Prosdocimo, D.A.; Sangwung, P.; Zhang, L.; Zhou, G.; Anand, P.; Lai, L.; Leone, T.C.; et al. Kruppel-like factor 4 is critical for transcriptional control of cardiac mitochondrial homeostasis. J. Clin. Invest. 2015, 125, 3461–3476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McConnell, B.B.; Yang, V.W. Mammalian Kruppel-like factors in health and diseases. Physiol. Rev. 2010, 90, 1337–1381. [Google Scholar] [CrossRef] [PubMed]
- Zeitz, M.J.; Smyth, J.W. Translating Translation to Mechanisms of Cardiac Hypertrophy. J. Cardiovasc. Dev. Dis. 2020, 7, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, M.; Sadoshima, J. Mechanisms of physiological and pathological cardiac hypertrophy. Nat. Rev. Cardiol. 2018, 15, 387–407. [Google Scholar] [CrossRef] [PubMed]
- Samak, M.; Fatullayev, J.; Sabashnikov, A.; Zeriouh, M.; Schmack, B.; Farag, M.; Popov, A.F.; Dohmen, P.M.; Choi, Y.H.; Wahlers, T.; et al. Cardiac Hypertrophy: An Introduction to Molecular and Cellular Basis. Med. Sci. Monit. Basic Res. 2016, 22, 75–79. [Google Scholar] [CrossRef] [Green Version]
- Ma, S.; Feng, J.; Lin, X.; Liu, J.; Tang, Y.; Nie, S.; Gong, J.; Wang, L. Nicotinamide Riboside Alleviates Cardiac Dysfunction and Remodeling in Pressure Overload Cardiac Hypertrophy. Oxid. Med. Cell. Longev. 2021, 2021, 5546867. [Google Scholar] [CrossRef]
- Lyon, A.R.; Dent, S.; Stanway, S.; Earl, H.; Brezden-Masley, C.; Cohen-Solal, A.; Tocchetti, C.G.; Moslehi, J.J.; Groarke, J.D.; Bergler-Klein, J.; et al. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: A position statement and new risk assessment tools from the Cardio-Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio-Oncology Society. Eur. J. Heart Fail. 2020, 22, 1945–1960. [Google Scholar]
- Battisti, N.M.L.; Andres, M.S.; Lee, K.A.; Ramalingam, S.; Nash, T.; Mappouridou, S.; Senthivel, N.; Asavisanu, K.; Obeid, M.; Tripodaki, E.S.; et al. Incidence of cardiotoxicity and validation of the Heart Failure Association-International Cardio-Oncology Society risk stratification tool in patients treated with trastuzumab for HER2-positive early breast cancer. Breast Cancer Res. Treat. 2021, 188, 149–163. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zheng, D.; Wei, M.; Ma, J.; Yu, Y.; Chen, R.; Lacefield, J.C.; Xu, H.; Peng, T. Over-expression of calpastatin aggravates cardiotoxicity induced by doxorubicin. Cardiovasc. Res. 2013, 98, 381–390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, J.; Wang, Y.; Zheng, D.; Wei, M.; Xu, H.; Peng, T. Rac1 signalling mediates doxorubicin-induced cardiotoxicity through both reactive oxygen species-dependent and -independent pathways. Cardiovasc. Res. 2013, 97, 77–87. [Google Scholar] [CrossRef] [Green Version]
- Zhang, T.; Zhang, Y.; Cui, M.; Jin, L.; Wang, Y.; Lv, F.; Liu, Y.; Zheng, W.; Shang, H.; Zhang, J.; et al. CaMKII is a RIP3 substrate mediating ischemia- and oxidative stress-induced myocardial necroptosis. Nat. Med. 2016, 22, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Wang, H.; Han, D.; Xie, E.; Yang, X.; Wei, J.; Gu, S.; Gao, F.; Zhu, N.; Yin, X.; et al. Ferroptosis as a target for protection against cardiomyopathy. Proc. Natl. Acad. Sci. USA 2019, 116, 2672–2680. [Google Scholar] [CrossRef] [Green Version]
- Armenian, S.H.; Lacchetti, C.; Barac, A.; Carver, J.; Constine, L.S.; Denduluri, N.; Dent, S.; Douglas, P.S.; Durand, J.B.; Ewer, M.; et al. Prevention and Monitoring of Cardiac Dysfunction in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. 2017, 35, 893–911. [Google Scholar] [CrossRef]
- Awad, H.H.; El-Derany, M.O.; Mantawy, E.M.; Michel, H.E.; El-Naa, M.M.; Salah El-Din, R.A.; El-Brairy, A.I.; El-Demerdash, E. Comparative study on beneficial effects of vitamins B and D in attenuating doxorubicin induced cardiotoxicity in rats: Emphasis on calcium homeostasis. Biomed. Pharmacother. 2021, 140, 111679. [Google Scholar] [CrossRef]
- Kuivaniemi, H.; Platsoucas, C.D.; Tilson, M.D., 3rd. Aortic aneurysms: An immune disease with a strong genetic component. Circulation 2008, 117, 242–252. [Google Scholar] [CrossRef] [Green Version]
- van der Veer, E.; Nong, Z.; O’Neil, C.; Urquhart, B.; Freeman, D.; Pickering, J.G. Pre-B-cell colony-enhancing factor regulates NAD+-dependent protein deacetylase activity and promotes vascular smooth muscle cell maturation. Circ. Res. 2005, 97, 25–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Veer, E.; Ho, C.; O’Neil, C.; Barbosa, N.; Scott, R.; Cregan, S.P.; Pickering, J.G. Extension of human cell lifespan by nicotinamide phosphoribosyltransferase. J. Biol. Chem. 2007, 282, 10841–10845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, H.; van der Veer, E.; Frontini, M.J.; Thibert, V.; O’Neil, C.; Watson, A.; Szasz, P.; Chu, M.W.; Pickering, J.G. Intrinsic directionality of migrating vascular smooth muscle cells is regulated by NAD(+) biosynthesis. J. Cell Sci. 2012, 125, 5770–5780. [Google Scholar] [CrossRef] [Green Version]
- Golledge, J.; Muller, J.; Daugherty, A.; Norman, P. Abdominal aortic aneurysm: Pathogenesis and implications for management. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 2605–2613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, P.; Li, W.L.; Liu, J.M.; Miao, C.Y. NAMPT and NAMPT-controlled NAD Metabolism in Vascular Repair. J. Cardiovasc. Pharmacol. 2016, 67, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Watson, A.; Nong, Z.; Yin, H.; O’Neil, C.; Fox, S.; Balint, B.; Guo, L.; Leo, O.; Chu, M.W.A.; Gros, R.; et al. Nicotinamide Phosphoribosyltransferase in Smooth Muscle Cells Maintains Genome Integrity, Resists Aortic Medial Degeneration, and Is Suppressed in Human Thoracic Aortic Aneurysm Disease. Circ. Res. 2017, 120, 1889–1902. [Google Scholar] [CrossRef] [PubMed]
- McCrudden, C.M.; O’Rourke, M.G.; Cherry, K.E.; Yuen, H.F.; O’Rourke, D.; Babur, M.; Telfer, B.A.; Thomas, H.D.; Keane, P.; Nambirajan, T.; et al. Vasoactivity of rucaparib, a PARP-1 inhibitor, is a complex process that involves myosin light chain kinase, P2 receptors, and PARP itself. PLoS ONE 2015, 10, e0118187. [Google Scholar] [CrossRef] [Green Version]
- Wang, P.; Xu, T.Y.; Guan, Y.F.; Su, D.F.; Fan, G.R.; Miao, C.Y. Perivascular adipose tissue-derived visfatin is a vascular smooth muscle cell growth factor: Role of nicotinamide mononucleotide. Cardiovasc. Res. 2009, 81, 370–380. [Google Scholar] [CrossRef] [Green Version]
- Howard, D.P.; Banerjee, A.; Fairhead, J.F.; Perkins, J.; Silver, L.E.; Rothwell, P.M. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford Vascular Study. Circulation 2013, 127, 2031–2037. [Google Scholar] [CrossRef] [Green Version]
- Oller, J.; Gabande-Rodriguez, E.; Ruiz-Rodriguez, M.J.; Desdin-Mico, G.; Aranda, J.F.; Rodrigues-Diez, R.; Ballesteros-Martinez, C.; Blanco, E.M.; Roldan-Montero, R.; Acuna, P.; et al. Extracellular Tuning of Mitochondrial Respiration Leads to Aortic Aneurysm. Circulation 2021, 143, 2091–2109. [Google Scholar] [CrossRef] [PubMed]
- Ganji, S.H.; Qin, S.; Zhang, L.; Kamanna, V.S.; Kashyap, M.L. Niacin inhibits vascular oxidative stress, redox-sensitive genes, and monocyte adhesion to human aortic endothelial cells. Atherosclerosis 2009, 202, 68–75. [Google Scholar] [CrossRef]
- Digby, J.E.; Martinez, F.; Jefferson, A.; Ruparelia, N.; Chai, J.; Wamil, M.; Greaves, D.R.; Choudhury, R.P. Anti-inflammatory effects of nicotinic acid in human monocytes are mediated by GPR109A dependent mechanisms. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 669–676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guzik, B.; Sagan, A.; Ludew, D.; Mrowiecki, W.; Chwala, M.; Bujak-Gizycka, B.; Filip, G.; Grudzien, G.; Kapelak, B.; Zmudka, K.; et al. Mechanisms of oxidative stress in human aortic aneurysms--association with clinical risk factors for atherosclerosis and disease severity. Int. J. Cardiol. 2013, 168, 2389–2396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miyake, T.; Morishita, R. Pharmacological treatment of abdominal aortic aneurysm. Cardiovasc. Res. 2009, 83, 436–443. [Google Scholar] [CrossRef] [Green Version]
- Lavu, S.; Boss, O.; Elliott, P.J.; Lambert, P.D. Sirtuins--novel therapeutic targets to treat age-associated diseases. Nat. Rev. Drug Discov. 2008, 7, 841–853. [Google Scholar] [CrossRef] [PubMed]
- Pillarisetti, S. A review of Sirt1 and Sirt1 modulators in cardiovascular and metabolic diseases. Recent Pat. Cardiovasc. Drug Discov. 2008, 3, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Potente, M.; Dimmeler, S. Emerging roles of SIRT1 in vascular endothelial homeostasis. Cell Cycle 2008, 7, 2117–2122. [Google Scholar] [CrossRef]
- Imai, S. A possibility of nutriceuticals as an anti-aging intervention: Activation of sirtuins by promoting mammalian NAD biosynthesis. Pharmacol. Res. 2010, 62, 42–47. [Google Scholar] [CrossRef] [Green Version]
- Satoh, A.; Stein, L.; Imai, S. The role of mammalian sirtuins in the regulation of metabolism, aging, and longevity. Handb. Exp. Pharmacol. 2011, 206, 125–162. [Google Scholar] [PubMed] [Green Version]
- Verdin, E. NAD(+) in aging, metabolism, and neurodegeneration. Science 2015, 350, 1208–1213. [Google Scholar] [CrossRef]
- Cerutti, R.; Pirinen, E.; Lamperti, C.; Marchet, S.; Sauve, A.A.; Li, W.; Leoni, V.; Schon, E.A.; Dantzer, F.; Auwerx, J.; et al. NAD(+)-dependent activation of Sirt1 corrects the phenotype in a mouse model of mitochondrial disease. Cell Metab. 2014, 19, 1042–1049. [Google Scholar] [CrossRef] [Green Version]
- Hughes-Large, J.M.; Pang, D.K.; Robson, D.L.; Chan, P.; Toma, J.; Borradaile, N.M. Niacin receptor activation improves human microvascular endothelial cell angiogenic function during lipotoxicity. Atherosclerosis 2014, 237, 696–704. [Google Scholar] [CrossRef]
- Marcu, R.; Kotha, S.; Zhi, Z.; Qin, W.; Neeley, C.K.; Wang, R.K.; Zheng, Y.; Hawkins, B.J. The mitochondrial permeability transition pore regulates endothelial bioenergetics and angiogenesis. Circ. Res. 2015, 116, 1336–1345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, H.Z.; Wang, F.; Gao, P.; Pei, J.F.; Liu, Y.; Xu, T.T.; Tang, X.; Fu, W.Y.; Lu, J.; Yan, Y.F.; et al. Age-Associated Sirtuin 1 Reduction in Vascular Smooth Muscle Links Vascular Senescence and Inflammation to Abdominal Aortic Aneurysm. Circ. Res. 2016, 119, 1076–1088. [Google Scholar] [CrossRef]
- Zhang, Z.; Xu, J.; Liu, Y.; Wang, T.; Pei, J.; Cheng, L.; Hao, D.; Zhao, X.; Chen, H.Z.; Liu, D.P. Mouse macrophage specific knockout of SIRT1 influences macrophage polarization and promotes angiotensin II-induced abdominal aortic aneurysm formation. J. Genet. Genom. 2018, 45, 25–32. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, T.T.; Zhang, R.; Fu, W.Y.; Wang, X.; Wang, F.; Gao, P.; Ding, Y.N.; Xie, Y.; Hao, D.L.; et al. Calorie restriction protects against experimental abdominal aortic aneurysms in mice. J. Exp. Med. 2016, 213, 2473–2488. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Tu, Y.; Gao, Y.; Chen, H.; Liu, J.; Zheng, J. Smooth Muscle Sirtuin 1 Blocks Thoracic Aortic Aneurysm/Dissection Development in Mice. Cardiovasc. Drugs Ther. 2020, 34, 641–650. [Google Scholar] [CrossRef]
- Sanchez-Infantes, D.; Nus, M.; Navas-Madronal, M.; Fite, J.; Perez, B.; Barros-Membrilla, A.J.; Soto, B.; Martinez-Gonzalez, J.; Camacho, M.; Rodriguez, C.; et al. Oxidative Stress and Inflammatory Markers in Abdominal Aortic Aneurysm. Antioxidants 2021, 10, 602. [Google Scholar] [CrossRef]
- Oparil, S.; Acelajado, M.C.; Bakris, G.L.; Berlowitz, D.R.; Cifkova, R.; Dominiczak, A.F.; Grassi, G.; Jordan, J.; Poulter, N.R.; Rodgers, A.; et al. Hypertension. Nat. Rev. Dis. Primers 2018, 4, 18014. [Google Scholar] [CrossRef] [Green Version]
- Kjeldsen, S.E.; Narkiewicz, K.; Burnier, M.; Oparil, S. 2018 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension. Blood Press 2018, 27, 313. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wang, Z.; Wu, J.; Liu, M.; Li, M.; Sun, Y.; Huang, W.; Li, Y.; Zhang, Y.; Tang, W.; et al. Endothelial SIRT6 Is Vital to Prevent Hypertension and Associated Cardiorenal Injury Through Targeting Nkx3.2-GATA5 Signaling. Circ. Res. 2019, 124, 1448–1461. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Liu, H.; Zhu, S.; Woodson, M.; Liu, R.; Tilton, R.G.; Miller, J.D.; Zhang, W. Sirt6 deficiency results in progression of glomerular injury in the kidney. Aging 2017, 9, 1069–1083. [Google Scholar] [CrossRef] [Green Version]
- Gao, P.; Xu, T.T.; Lu, J.; Li, L.; Xu, J.; Hao, D.L.; Chen, H.Z.; Liu, D.P. Overexpression of SIRT1 in vascular smooth muscle cells attenuates angiotensin II-induced vascular remodeling and hypertension in mice. J. Mol. Med. 2014, 92, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Sethi, J.K.; Empson, R.M.; Galione, A. Nicotinamide inhibits cyclic ADP-ribose-mediated calcium signalling in sea urchin eggs. Biochem. J. 1996, 319 Pt. 2, 613–617. [Google Scholar] [CrossRef] [Green Version]
- Thai, T.L.; Arendshorst, W.J. ADP-ribosyl cyclase and ryanodine receptors mediate endothelin ETA and ETB receptor-induced renal vasoconstriction in vivo. Am. J. Physiol. Renal Physiol. 2008, 295, F360–F368. [Google Scholar] [CrossRef] [Green Version]
- Wilson, H.L.; Dipp, M.; Thomas, J.M.; Lad, C.; Galione, A.; Evans, A.M. Adp-ribosyl cyclase and cyclic ADP-ribose hydrolase act as a redox sensor. a primary role for cyclic ADP-ribose in hypoxic pulmonary vasoconstriction. J. Biol. Chem. 2001, 276, 11180–11188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bushehri, N.; Jarrell, S.T.; Lieberman, S.; Mirdamadi-Zonozi, N.; Birkmayer, G.; Preuss, H.G. Oral reduced B-nicotinamide adenine dinucleotide (NADH) affects blood pressure, lipid peroxidation, and lipid profile in hypertensive rats (SHR). Geriatr. Nephrol. Urol. 1998, 8, 95–100. [Google Scholar] [CrossRef]
- Cho, K.H.; Kim, H.J.; Rodriguez-Iturbe, B.; Vaziri, N.D. Niacin ameliorates oxidative stress, inflammation, proteinuria, and hypertension in rats with chronic renal failure. Am. J. Physiol. Renal Physiol. 2009, 297, F106–F113. [Google Scholar] [CrossRef] [Green Version]
- Fushima, T.; Sekimoto, A.; Oe, Y.; Sato, E.; Ito, S.; Sato, H.; Takahashi, N. Nicotinamide ameliorates a preeclampsia-like condition in mice with reduced uterine perfusion pressure. Am. J. Physiol. Renal Physiol. 2017, 312, F366–F372. [Google Scholar] [CrossRef] [Green Version]
- Li, F.; Fushima, T.; Oyanagi, G.; Townley-Tilson, H.W.; Sato, E.; Nakada, H.; Oe, Y.; Hagaman, J.R.; Wilder, J.; Li, M.; et al. Nicotinamide benefits both mothers and pups in two contrasting mouse models of preeclampsia. Proc. Natl. Acad. Sci. USA 2016, 113, 13450–13455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huynh, P.K.; Wilder, J.; Hiller, S.; Hagaman, J.; Takahashi, N.; Maeda-Smithies, N.; Li, F. Beneficial effects of nicotinamide on hypertensive mice with impaired endothelial nitric oxide function. J. Exp. Nephrol. 2020, 1, 1–8. [Google Scholar]
- Yano, M.; Akazawa, H.; Oka, T.; Yabumoto, C.; Kudo-Sakamoto, Y.; Kamo, T.; Shimizu, Y.; Yagi, H.; Naito, A.T.; Lee, J.K.; et al. Monocyte-derived extracellular Nampt-dependent biosynthesis of NAD(+) protects the heart against pressure overload. Sci. Rep. 2015, 5, 15857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altschul, R.; Hoffer, A.; Stephen, J.D. Influence of nicotinic acid on serum cholesterol in man. Arch. Biochem. Biophys. 1955, 54, 558–559. [Google Scholar] [CrossRef]
- Investigators, A.-H. The role of niacin in raising high-density lipoprotein cholesterol to reduce cardiovascular events in patients with atherosclerotic cardiovascular disease and optimally treated low-density lipoprotein cholesterol: Baseline characteristics of study participants. The Atherothrombosis Intervention in Metabolic syndrome with low HDL/high triglycerides: Impact on Global Health outcomes (AIM-HIGH) trial. Am. Heart J. 2011, 161, 538–543. [Google Scholar]
- Markel, A. The resurgence of niacin: From nicotinic acid to niaspan/laropiprant. Isr. Med. Assoc. J. 2011, 13, 368–374. [Google Scholar]
- Halder, P.; Bera, D.; Majumder, B.; Venkatraman, D.; Bhandari, M. Dilated cardiomyopathy in a case of pellagra: A extremely rare but treatable entity. Indian J. Med. Res. Pharm. Sci. 2015, 2, 24–27. [Google Scholar]
- Misner, D.L.; Kauss, M.A.; Singh, J.; Uppal, H.; Bruening-Wright, A.; Liederer, B.M.; Lin, T.; McCray, B.; La, N.; Nguyen, T.; et al. Cardiotoxicity Associated with Nicotinamide Phosphoribosyltransferase Inhibitors in Rodents and in Rat and Human-Derived Cells Lines. Cardiovasc. Toxicol. 2017, 17, 307–318. [Google Scholar] [CrossRef]
- Rahman, J.E.; Helou, E.F.; Gelzer-Bell, R.; Thompson, R.E.; Kuo, C.; Rodriguez, E.R.; Hare, J.M.; Baughman, K.L.; Kasper, E.K. Noninvasive diagnosis of biopsy-proven cardiac amyloidosis. J. Am. Coll. Cardiol. 2004, 43, 410–415. [Google Scholar] [CrossRef] [Green Version]
- Frustaci, A.; Verardo, R.; Caldarulo, M.; Acconcia, M.C.; Russo, M.A.; Chimenti, C. Myocarditis in hypertrophic cardiomyopathy patients presenting acute clinical deterioration. Eur. Heart J. 2007, 28, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Rachmilewitz, M.; Braun, K. Electrocardiographic changes in typhoid fever and their reversibility following niacin treatment. Am. Heart J. 1948, 36, 284–294. [Google Scholar] [CrossRef]
- Fine, I.; Brainerd, H.; Sokolow, M. Myocarditis in acute infectious diseases; a clinical and electrocardiographic study. Circulation 1950, 2, 859–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clerkin, K.J.; Fried, J.A.; Raikhelkar, J.; Sayer, G.; Griffin, J.M.; Masoumi, A.; Jain, S.S.; Burkhoff, D.; Kumaraiah, D.; Rabbani, L.; et al. COVID-19 and Cardiovascular Disease. Circulation 2020, 141, 1648–1655. [Google Scholar] [CrossRef] [Green Version]
- Bailey, A.L.; Dmytrenko, O.; Greenberg, L.; Bredemeyer, A.L.; Ma, P.; Liu, J.; Penna, V.; Winkler, E.S.; Sviben, S.; Brooks, E.; et al. SARS-CoV-2 Infects Human Engineered Heart Tissues and Models COVID-19 Myocarditis. JACC Basic Transl. Sci. 2021, 6, 331–345. [Google Scholar] [CrossRef] [PubMed]
- Perez-Bermejo, J.A.; Kang, S.; Rockwood, S.J.; Simoneau, C.R.; Joy, D.A.; Silva, A.C.; Ramadoss, G.N.; Flanigan, W.R.; Fozouni, P.; Li, H.; et al. SARS-CoV-2 infection of human iPSC-derived cardiac cells reflects cytopathic features in hearts of patients with COVID-19. Sci. Transl. Med. 2021, 13. [Google Scholar] [CrossRef]
- Badawy, A.A. Immunotherapy of COVID-19 with poly (ADP-ribose) polymerase inhibitors: Starting with nicotinamide. Biosci. Rep. 2020, 40, BSR20202856. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.; Wentzel, A.R.; Richards, G.A. COVID-19: NAD(+) deficiency may predispose the aged, obese and type2 diabetics to mortality through its effect on SIRT1 activity. Med. Hypotheses 2020, 144, 110044. [Google Scholar] [CrossRef] [PubMed]
- Omran, H.M.; Almaliki, M.S. Influence of NAD+ as an ageing-related immunomodulator on COVID 19 infection: A hypothesis. J. Infect. Public Health 2020, 13, 1196–1201. [Google Scholar] [CrossRef] [PubMed]
- Raines, N.H.; Ganatra, S.; Nissaisorakarn, P.; Pandit, A.; Morales, A.; Asnani, A.; Sadrolashrafi, M.; Maheshwari, R.; Patel, R.; Bang, V.; et al. Niacinamide May Be Associated with Improved Outcomes in COVID-19-Related Acute Kidney Injury: An Observational Study. Kidney360 2021, 2, 33–41. [Google Scholar] [CrossRef]
- Martens, C.R.; Denman, B.A.; Mazzo, M.R.; Armstrong, M.L.; Reisdorph, N.; McQueen, M.B.; Chonchol, M.; Seals, D.R. Chronic nicotinamide riboside supplementation is well-tolerated and elevates NAD(+) in healthy middle-aged and older adults. Nat. Commun. 2018, 9, 1286. [Google Scholar] [CrossRef]
- Airhart, S.E.; Shireman, L.M.; Risler, L.J.; Anderson, G.D.; Nagana Gowda, G.A.; Raftery, D.; Tian, R.; Shen, D.D.; O’Brien, K.D. An open-label, non-randomized study of the pharmacokinetics of the nutritional supplement nicotinamide riboside (NR) and its effects on blood NAD+ levels in healthy volunteers. PLoS ONE 2017, 12, e0186459. [Google Scholar] [CrossRef]
- Berthiaume, J.M.; Kurdys, J.G.; Muntean, D.M.; Rosca, M.G. Mitochondrial NAD(+)/NADH Redox State and Diabetic Cardiomyopathy. Antioxid. Redox. Signal. 2019, 30, 375–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liao, B.; Zhao, Y.; Wang, D.; Zhang, X.; Hao, X.; Hu, M. Nicotinamide mononucleotide supplementation enhances aerobic capacity in amateur runners: A randomized, double-blind study. J. Int. Soc. Sports Nutr. 2021, 18, 54. [Google Scholar] [CrossRef] [PubMed]
- Wen, D.T.; Zheng, L.; Lu, K.; Hou, W.Q. Activation of cardiac Nmnat/NAD+/SIR2 pathways mediates endurance exercise resistance to lipotoxic cardiomyopathy in aging Drosophila. J. Exp. Biol. 2021, 224, jeb242425. [Google Scholar] [CrossRef] [PubMed]
- Wen, D.T.; Zheng, L.; Li, J.X.; Cheng, D.; Liu, Y.; Lu, K.; Hou, W.Q. Endurance exercise resistance to lipotoxic cardiomyopathy is associated with cardiac NAD(+)/dSIR2/PGC-1alpha pathway activation in old Drosophila. Biol. Open 2019, 8, bio044719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hershberger, K.A.; Martin, A.S.; Hirschey, M.D. Role of NAD(+) and mitochondrial sirtuins in cardiac and renal diseases. Nat. Rev. Nephrol. 2017, 13, 213–225. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).