Abstract
Based on the relationship between the posterior clinoid process and the basilar artery (BA) apex it may be difficult to obtain proximal control of the BA using temporary clips. Endovascular BA temporary balloon occlusion (TBO) can reduce aneurysm sac pressure, facilitate dissection/clipping, and finally lower the risk of intraoperative rupture. We present our experience with TBO during aneurysm clipping of posterior circulation aneurysms within the setting of a hybrid operating room (hOR). We report one case each of a basilar tip, posterior cerebral artery, and superior cerebellar artery aneurysm that underwent surgical occlusion under TBO within an hOR. Surgical exposure of the BA was achieved with a pterional approach and selective anterior and posterior clinoidectomy. Intraoperative digital subtraction angiography (iDSA) was performed prior, during, and after aneurysm occlusion. Two patients presented with subarachnoid hemorrhage and one patient presented with an unruptured aneurysm. The intraluminal balloon was inserted through the femoral artery and inflated in the BA after craniotomy to allow further dissection of the parent vessel and branches needed for the preparation of the aneurysm neck. No complications during balloon inflation and aneurysm dissection occurred. Intraoperative aneurysm rupture prior to clipping did not occur. The duration of TBO varied between 9 and 11 min. Small neck aneurysm remnants were present in two cases (BA and PCA). Two patients recovered well with a GOS 5 after surgery and one patient died due to complications unrelated to surgery. Intraoperative TBO within the hOR is a feasible and safe procedure with no additional morbidity when using a standardized protocol and setting. No relevant side effects or intraoperative complications were present in this series. In addition, iDSA in an hOR facilitates the evaluation of the surgical result and 3D reconstructions provide documentation of potential aneurysm remnants for future follow-up.
1. Introduction
Aneurysms of the posterior circulation, such as the basilar artery (BA), present a particular surgical challenge [1,2]. They represent 5–8% of all intracranial aneurysms and more than 50% of those in the posterior circulation [3,4]. Posterior circulation aneurysms are known to have a higher risk of rupture [5]. According to recently published scores such as PHASES [6] or UIATS [7], preventive endovascular or surgical methods can be performed in patients at risk, to minimize the chance of aneurysm rupture. The difficulties of microsurgical clipping are mainly caused by anatomical conditions and a demanding approach [8]. Surgical complexity varies according to size, shape, and localization of the aneurysm, degree of intraoperative brain swelling, and the microsurgical experience of the surgeon [9]. Moreover, standard clipping could fail due to insufficient proximal control and lead to incomplete occlusion or intraoperative aneurysm rupture [10]. Nevertheless, microsurgical clipping is still more accessible worldwide, especially in developing countries [11].
The ISAT (International Subarachnoid Aneurysm Trial) reported a higher rupture rate for basilar apex aneurysm in correlation with aneurysm size [12]. Increased morbidity and mortality, and worse clinical outcome was also reported after surgical clipping compared to endovascular coiling of a posterior circulation aneurysm [12]. These findings initiated the use of endovascular treatment for a basilar apex region aneurysm [13]. The fact that fewer neurosurgeons are performing microsurgical clipping of basilar apex aneurysm supports the trend for treating basilar artery aneurysms endovascularly rather than surgically [14]. The safety of endovascular occlusion of BA aneurysms has been proven, although long-term sustainability and efficacy remain unclear [13,14,15,16,17].
Up to 50% recanalization and regrowth of a coiled aneurysm has been reported [17,18,19,20]. The annual risk of bleeding in a partially coiled or recanalized aneurysm is reported to range from 2.1–15% [17,18,21,22,23]. This is relatively high and similar to rates for an unruptured aneurysm [5,24,25,26,27,28,29].
The exact location of the aneurysm is the key factor when deciding which surgical approach to take. The prevention of any injury to the brainstem and its perforators is crucial [30]. Different approaches to BA aneurysms have been described including the pterional approach introduced by G. Yasargil [31], the subtemporal approach pioneered by C. Drake [32], as well as lateral supraorbital [33], orbitozygomatic [34,35], modified presigmoid [36], transpetrosal [37] or transzygomatic transcavernous approaches, [13] and many others [38,39].
Various methods of temporary vessel occlusion or local blood flow interruption have been applied to facilitate a microsurgical approach to a large aneurysm in a narrow and deep location. Also, adenosine-induced cardiac arrest [40], hypothermic circulatory arrest [41], temporary clip placement [42], and temporary balloon occlusion [43] have been described. The relationship between the posterior clinoid process and the BA apex may limit the access for temporary clips [39]. An endovascular technique using balloon inflation in the parent vessel of the aneurysm can achieve proximal and distal control during surgery and, therefore, eliminate the need for temporary clipping [43]. Intraoperative temporary balloon occlusion (TBO) of the parent vessel might lower the risk of intraoperative rupture, reduce pressure in the aneurysm sac, and facilitate dissection and microsurgical clipping. The aim of this study is to describe the technical issues, setup, and experience of intraoperative TBO during surgical occlusion of complex posterior circulation aneurysms within the hybrid operating room (hOR).
2. Materials and Methods
We report three cases of intracranial aneurysms of the posterior circulation that underwent clipping with the concurrent use of TBO in our department between 2013 and 2016. The first patient suffered subarachnoid hemorrhage (SAH) after the rupture of a basilar tip aneurysm (16 × 16 × 15 mm). Endovascular occlusion was not indicated due to the risk of occlusion of the posterior cerebral artery (PCA) and the superior cerebellar artery (SCA). The second case presented with a ruptured, partially thrombosed BA aneurysm (11 × 8 × 8 mm) with secondary wall hematoma and no SAH. As in the previous case, endovascular occlusion was considered not possible due to the risk of SCA occlusion caused by duplicate origin from the aneurysm fundus. The third patient had an incidental right proximal PCA (P1) aneurysm (4 × 5 × 5 mm). Endovascular treatment was scheduled, but 3D digital cerebral angiography (DSA) showed the SCA originating from the aneurysm sac and the treatment strategy was changed to surgery occlusion. Complex anatomical vascular findings were considered for the decision to choose a combined endovascular and microsurgical procedure within the (hOR) in these three cases (Table 1).

Table 1.
Demographic characteristics, clinical findings, aneurysm description, and outcome parameters.
The technical aspects of performed combined approaches in the hOR have been described by our group in an earlier publication [44]. The main unit consists of a 360° radiolucent carbon fiber table (Alphamaquet 1150, Maquet AG, Switzerland) that is coupled with the C-arm angiography system (Allura Xper FD20, Philips, Netherlands). A radiolucent head holder and pins are required for optimal acquisition of angiograms and intraoperative CT scans (Mayfield, Integra GmbH, Ratingen, Germany). A 7-Fr sheath is placed in the right or left femoral artery in preparation for intraoperative endovascular balloon occlusion and control DSA. All cases underwent an intraoperative DSA (iDSA) and CT (iCT) scan before they were transferred to the intensive care unit.
2.1. Illustrative Cases
The surgical approach and endovascular techniques were similar in all three cases.
2.1.1. Surgical Procedure
After the positioning of the patient′s head in a carbon clamp in the hOR, a right fronto-temporal craniotomy and selective extradural anterior clinoidectomy were performed. The proximal Sylvian fissure was opened, and the chiasmatic cistern incised, followed by dissection of the optic and oculomotor nerve, and carotid artery. Once the posterior clinoid process was exposed, a posterior clinoidectomy was completed with a 2 mm drill. The afterward visible BA, PCA′s, SCA′s, and aneurysm were inspected. After craniotomy, the first iDSA was performed by cannulation of the right femoral artery with a 7-Fr sheath and inserting a 5F diagnostic catheter in one of the vertebral arteries. The first iDSA showed the previously identified aneurysm and in Case 1 a progression of the dissecting basilar tip aneurysm with a new bleb. The diagnostic catheter was exchanged for a soft guiding catheter (Neuron 6F 058, Penumbra, Alameda CA, USA). An ASCENT® 4 × 7 balloon (DePuy Synthes) and was then placed in the middle or distal segment of the BA and inflated under fluoroscopy to interrupt blood flow. The dual lumen design of the ASCENT balloon allows the distal flushing of the occluded vessel by saline. In the meantime, the BA or PCA aneurysm neck, which was significantly softened, as well as PCA and SCA branches were further dissected. The aneurysms were occluded in a microtechnical fashion with straight standard titanium 790-Yasargil-Clips (Aesculap, Tübingen, Germany) under visualization of both SCA branches. The balloon was deflated after 9, 10, and 11 min of TBO. An iDSA and intraoperative 3D-angiography in Case 1 showed complete occlusion of the BA aneurysm with patent PCA and SCA branches (Figure 1). The iDSA in Cases 2 and 3, revealed a small remnant at the aneurysm neck to preserve the SCA exit, no sign of aneurysm perfusion, and patent PCA and SCA branches (Figure 2 and Figure 3). The dura was sutured, the bone flap fixed, and the wound sutured using a standard multilayered technique. The iCT scan documented no hemorrhage or midline shift.
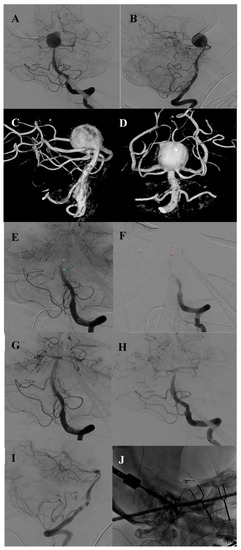
Figure 1.
Case 1. Preoperative ap and lateral DSA of the basilar tip aneurysm (A,B). Preoperative 3D angiography of the basilar aneurysm presenting the bilateral origin of the PCA and SCA from the aneurysm base (C,D). Intraoperative angiography showing the endovascular placement of the balloon and occlusion of the basilar artery (E,F). Intraoperative DSA after clipping and closure of the balloon showing complete occlusion of the aneurysm in ap and lateral view with all branches open (G–I). Intraoperative picture of the opened skull, placed fish hooks, spatula and clip (J).
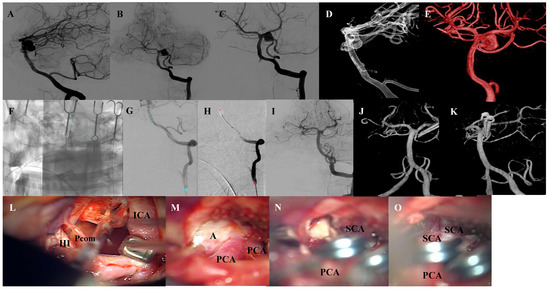
Figure 2.
Case 2. Preoperative DSA ap and lateral projections of the left side dissecting basilar artery aneurysm (A–C). Preoperative 3D-DSA of the basilar aneurysm, presenting the ampullary exit of the left double-laid SCA from the aneurysm fundus (D,E). Intraoperative DSA showing the endovascular placement of the balloon and occlusion of the basilar artery through balloon inflation (F,G). Intraoperative angiography after clipping and deflation of the balloon demonstrating occlusion of the aneurysm in the ap and lateral view (H,I). Intraoperative 3D angiography in the ap and lateral view, showing a small remnant at the neck of the aneurysm to preserve the SCA exit (J). Microsurgical view showing the aneurysm approach with mobilization of the ICA with hook retractor (K), BA aneurysm (L), and situs after clipping with patency of all branches and parent vessel (M–O). Abbreviations: DSA = digital subtraction angiography, SCA = superior cerebellar artery, ICA= internal carotid artery, BA= basilar artery, III = oculomotor nerve, PCA = posterior cerebral artery, A = aneurysm, Pcom = posterior communicating artery.
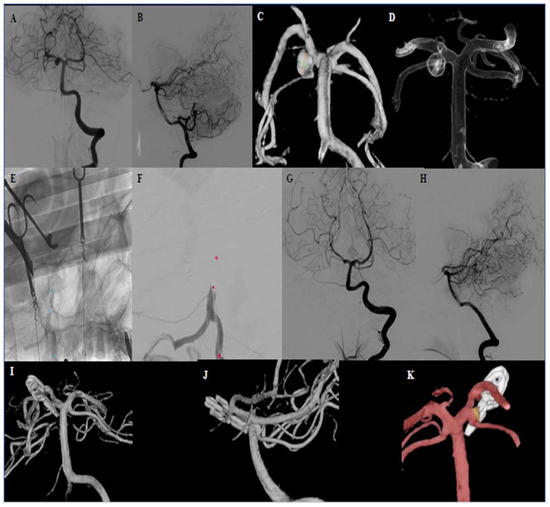
Figure 3.
Case 3. Preoperative DSA ap and lateral projections of the proximal right side PCA aneurysm (P1 branch) (A,B). Preoperative 3D-DSA of the PCA aneurysm, showing the right SCA leaving the P1 segment from the aneurysm sidewall (C,D). Intraoperative DSA presenting the placement of the balloon and occlusion of the BA after balloon inflation (E,F). Intraoperative angiography after clipping and balloon removal demonstrating occlusion of the aneurysm and patency of the BA and PCA (G–I). Intraoperative 3D-DSA showing a small remnant at the aneurysm neck to preserve the patency of the SCA (J,K). Abbreviations: DSA = digital subtraction angiography, PCA = posterior cerebral artery, SCA = superior cerebellar artery.
Case 1
History
This 53-year-old patient presented with a SAH after a sudden loss of consciousness at home. The patient was intubated upon admission with a Glasgow Coma Scale (GCS) score of 3. The CT scan showed a SAH caused by a ruptured basilar tip aneurysm (Fisher grade IV). A DSA was performed after the patient improved to a GCS of 10 following two days of conservative treatment and CSF drainage after ventriculostomy. A basilar tip aneurysm (16 × 16 × 15 mm) with the PCA and SCA bilaterally arising from the aneurysm base was identified. Indication for surgical occlusion was decided after interdisciplinary case discussion. The surgical procedure in the hOR had to be postponed for six days due to severe vasospasms in the posterior circulation.
Postoperative Course
Further course on the ICU was unsuccessful. Consciousness persisted at a low level of GCS 5 due to severe vasospasm and the deterioration of cerebral perfusion on CT was observed within 48 h after surgery. Despite of endovascular spasmolysis with Nimodipine was performed no clinical improvement could be observed. During the next days, the general condition of the patient deteriorated due to pneumonia and respiratory failure leading to death eight days after surgery.
Case 2
History
A 44-year-old patient was admitted to the emergency room with a thunderclap headache, neck pain, vomiting, and paresthesia in the right arm. The patient had a GCS score of 15 without meningism or any neurological deficits. Further investigations (CT, CTA, and DSA) excluded an SAH but showed a dissecting, partially thrombosed BA aneurysm (11 × 8 × 8 mm) with a secondary wall hematoma. Cerebral angiography revealed a duplicate origin of the SCA out of the aneurysm fundus. Treatment options were discussed in the interdisciplinary neurovascular board. In principal, endovascular occlusion by coiling or stent-assisted coiling was considered—with a high risk of SCA occlusion and secondary cerebellar ischemia. Therefore, the group decided to recommend microsurgical aneurysm clipping under endovascular TBO in the hOR.
Postoperative Course
The patient was hospitalized for one more week. During this time, the patient suffered an epileptic seizure. Apart from this, the patient could be rapidly mobilized with a GCS score of 15 and no new neurological deficits.
Case 3
History
After the occurrence of vertigo, this 48-year-old patient underwent an MRI scan which revealed an incidental right PCA aneurysm. The patient was referred to our Institution, and the history and clinical examination excluded any episodes of headache, epileptic seizure, or neurological deficits. Further aneurysm imaging with DSA showed a saccular right BA aneurysm at the origin of the P1 segment of the PCA (4 × 5 × 5 mm). The pre-interventional 3D-DSA depicted the origin of the SCA directly arising from the aneurysm fundus, as well as a hypoplastic bilateral posterior communicating artery. After the case discussion with the neurovascular board, surgical occlusion with TBO in the hOR was recommended.
Postoperative Course
Postoperatively, the patient presented with a GCS score of 15, discrete ptosis, anisocoria, and double vision. A further CT scan confirmed otherwise regular findings (the ophthalmological symptoms were mainly caused by an impairment of oculomotor nerve function). The oculomotor nerve dysfunction had resolved by itself by the three-month follow up.
3. Results
All cases underwent combined surgical and endovascular procedures in our hOR. After craniotomy and dissection of the parent vessel and aneurysm the intraluminal balloon was inserted through the femoral artery and inflated in the BA. In all three cases, intraoperative TBO was successfully performed without complications. No aneurysm rupture prior to clipping, or any other intra- or postoperative problems (necessary clip repositioning, parent vessel or branch occlusion, thromboembolic event, or re-bleeding) occurred. The mean duration of TBO was 10 min (Table 2). Upon inflation of the balloon, the intraluminal pressure releases and the aneurysm softens rapidly, which gives the surgeon more space and flexibility to explore the aneurysm and vessels branching out of the aneurysm base. Intraoperative DSA following clipping confirmed complete aneurysm occlusion with patent parent and branch vessels. In two cases, a small remnant at the aneurysm neck was visible in the intraoperative 3D angiography, which was necessary to preserve the branch origin. Two patients showed good postoperative recovery with GOS 5 and one patient died due to severe vasospasm and pneumonia.

Table 2.
Details of the intraoperative balloon occlusion procedure, clipping, and iDSA findings.
4. Discussion
The findings of this technical note support the fact that TBO is a feasible, safe, and reliable method for the clipping of posterior aneurysms that are technically demanding and complex due to size or anatomy. In our institution, TBO with a combined endovascular and surgical approach is also used for giant and complex recurrent middle cerebral artery (MCA) or anterior communicating artery aneurysms. In cases with a ruptured MCA aneurysm and surrounding hematoma, endovascular TBO facilitated clipping following hematoma evacuation and prevented an intraoperative rupture of fragile high-risk aneurysms.
In the case of intraoperative rupture, TBO could effectively control acute bleeding and increase the safety and accuracy of clip placement. In one case report with the intraoperative rupture of a paraclinoid aneurysm, TBO provided a salvage procedure for adequate hemostasis with additional intraluminal support to preserve the parent artery during clip placement [43].
In our opinion, microsurgery should still be viewed as a valuable option in the management of posterior circulation aneurysms. Various authors have reported good radiological and clinical outcomes for BA clipping with or without additional bypass [33,45,46,47,48,49,50,51]. Overall, the most common complications in this location are perforator and branch ischemia-related events and cranial nerve deficits, often involving oculomotor nerve palsies [47,52,53,54]. One case of transient oculomotor nerve palsy occurred in our series.
The angiographic obliteration rate of posterior circulation aneurysm has been reported with a range from 91.9–98.1% [8,29,45,55]. However, other reports also cited 11.5% transient and 7.8% permanent neurological deteriorations [45].
Circumferential exposure of the aneurysm, including branches and perforators, is necessary prior to a safe and efficacious clip application. Dissection and visualization of where they exit the aneurysm can be very demanding. Various methods have been described to support the surgeon during the clip application. Additional endovascular assistance can help prospective vascular neurosurgeons to become more confident and proficient in these cases. Temporary parent vessel occlusion seems to be a safe procedure. Interestingly, a study with a mean follow-up of 53 months showed that a temporary artery occlusion time (mean 16.1 min) had no effect on overall long-term clinical outcomes [56].
The “gold standard” for proximal vessel control is a temporary clip application, which is not always feasible, especially in areas with limited access [57]. Proximal parent vessel ligation [58] can be considered for treating giant aneurysms. Transient asystole with adenosine [40,59,60], deep hypothermic circulatory arrest [61], or rapid ventricular pacing [62] are other techniques also described in the literature but have higher risk profiles for side effects such as atrial or ventricular fibrillation, arrhythmias, and prolonged hypotension [62]. In addition, the risk of stroke can increase after a circulatory arrest, and the resulting need for a multidisciplinary team of surgeons and technologists is logistically challenging and expensive [63]. Perioperative morbidity and mortality for circulatory arrest has been described as ranging from 8.3–17% [41,61]. The risk of side effects of these different techniques has to be weighed against the significant chance of intraoperative aneurysm rupture, incomplete clipping, or unintended branch occlusion due to poor visualization.
In comparison, TBO presents a simple, fast, and inexpensive technique with no need for special anesthesiological monitoring or training and can be performed at any time in every center with endovascular expertise. Although temporary clipping will remain the routinely used technique, TBO may be more accurate for complex and large aneurysms, especially in the posterior circulation and to prevent premature rupture. In posterior circulation aneurysm clipping, proximal control with temporary clipping is often not possible due to the complex anatomy, skull base proximity, and location near the brain stem and cranial nerves [64]. The temporary clip itself may hinder the placement of the permanent one due to the limited surgical corridor [65]. In these cases, TBO can provide a reliable alternative. Proximal control with TBO can be achieved before craniotomy with minimal obstruction of the surgical field and less brain retraction.
Possible side effects of TBO and temporary clipping include wall injury of the parent vessel or thromboembolic events causing postoperative ischemic deficits. MacDonald et al. compared the degree of acute endothelial injury after temporary vessel occlusion with external clipping and endovascular balloon occlusion in a pig model [66]. The results revealed that vessel injury worsened with time and was more prevalent adjacent to the clip; as compared to the widespread pattern with TBO [66]. There is the concern of a higher risk of ischemic complications with balloon occlusion in perforator-rich vessels like MCA and BA, but neither MCA nor BA TBO interventions at our institution led to perforator infarctions.
The TBO technique was first described in 1986 by Kinjo et al. [67], by Shucart et al. in 1990 [68], and in many other case series since then. More recently, another group has reported on the use of TBO in the hybrid OR [69]. Table 3 provides an overview of the literature to-date.

Table 3.
Overview of all aneurysm cases including clipping with TBO in the literature. Information includes aneurysm characteristics, TBO duration, additional techniques, aneurysm occlusion status and complications. All posterior circulation aneurysms and complications related to TBO are listed in bold type.
Most series included large or giant paraclinoid ICA aneurysms occluded with clip ligation after balloon catheter placement in the ICA [69,70,71]. Intra-luminal pressure was decreased through the additional placement of a temporary clip distal to the aneurysm on the posterior communicating artery to reduce collateral blood flow, as well as the application of the retrograde decompression-suction method in the ICA [69,71,72]. In these series, endovascular TBO eliminated the need for cervical ICA dissection [68,69]. A review of the literature found a total of 188 aneurysms clipped with TBO. The largest series, published by Fulkerson et al [73]. included 63 ophthalmic artery aneurysms. The description of TBO in posterior circulation aneurysms, however, is less common with a total of only 20 cases. Bailes et al. published the first series of TBO use in multiple basilar artery aneurysms [74]. Apart from the recent study, eight other series have used TBO only for successful clipping [64,65,68,70,74,75,76,77]. Balloon placement in the aneurysm orifice or neck has only been described in two case series [65,77] and was otherwise performed in the proximal parent vessel. TBO duration ranged from 1.5–3 min for each balloon inflation and a total maximum of 50 min [43,63,64,65,68,71,75,77,78,79,80,81].
The overall reported complication rate for TBO is very low at 1.7–3.7% [72]. TBO procedure-related thromboembolic events occurred in five patients (2.6%). This risk is increased in cases with pronounced vessel wall sclerosis or prolonged temporary occlusion. One intraoperative balloon rupture and balloon exchange led to a thrombus in the M1 segment, with subsequent intraoperative embolectomy and postoperative transient hemiparesis. Symptoms such as dysphasia and hemiparesis were transient in all other cases except one major MCA infarct, which lead to the death of the patient [71,80,81,82]. Further TBO-related complications included: ICA intima dissection with ICA occlusion at the neck requiring medical treatment only (recovery was complete after four days) [81], as well as increases in vasospasms due to mechanical wall stimulation with transient hemiparesis [77].
Thromboembolic events may be reduced by limiting TBO duration and using double-lumen balloon systems that allow for maintaining continuous heparinized saline catheter flush. In thrombosed aneurysms or patients with severe atherosclerosis, the risk for thromboembolism might be increased. No complications occurred in our series that had a mean TBO time of 10 min. Several series suggested multiple short inflation times of 1.5–5 min to reduce thromboembolic event rate [63,65,78]. Some studies used a preoperative TBO test [83] to investigate the capacity of collateral support. In view of the short TBO time in our series, it is questionable if this is needed. The advantage of performing a TBO procedure in the hybrid OR is that control angiography is possible immediately after clip placement. We performed 2D and 3D intraoperative angiography in the hybrid OR and confirmed aneurysm occlusion in all cases. This standardized protocol can achieve better outcomes [84,85].
The main limitation of our study is the small sample size, as we chose to report on posterior circulation aneurysms only.
5. Conclusions
Intraoperative endovascular TBO is a feasible, safe, and valuable procedure for surgical treatment of complex posterior circulation aneurysm undergoing clipping. In addition, intraoperative DSA and 3D-DSA in the hOR was confirmed as a valuable tool for the evaluation of aneurysm occlusion and possible aneurysm remnants.
Author Contributions
J.F., J.C.K., J.F., L.R. methodology; Software, L.R., M.D.; Validation, J.F., L.R., J.C.K., Y.Y. and M.D.; Formal analysis, J.F.; Writing—original draft preparation, J.C.K., J.F.; Writing—review and editing, J.F., S.M.; Supervision, J.F., L.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Batjer, H.H.; Samson, D.S. Retrograde suction decompression of giant paraclinoidal aneurysms. Technical note. J. Neurosurg. 1990, 73, 305–306. [Google Scholar] [CrossRef] [PubMed]
- Batjer, H.H.; Kopitnik, T.A.; Giller, C.A.; Samson, D.S. Surgery for paraclinoidal carotid artery aneurysms. J. Neurosurg. 1994, 80, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Vlak, M.H.; Rinkel, G.J.; Greebe, P.; van der Bom, J.G.; Algra, A. Trigger factors for rupture of intracranial aneurysms in relation to patient and aneurysm characteristics. J. Neurol. 2012, 259, 1298–1302. [Google Scholar] [CrossRef]
- Brisman, J.L.; Song, J.K.; Newell, D.W. Cerebral aneurysms. N. Engl. J. Med. 2006, 355, 928–939. [Google Scholar] [CrossRef] [PubMed]
- Molyneux, A.J.; Kerr, R.S.; Yu, L.M.; Clarke, M.; Sneade, M.; Yarnold, J.A.; Sandercock, P.; International Subarachnoid Aneurysm Trial Collaborative Group. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 2005, 366, 809–817. [Google Scholar] [PubMed]
- Greving, J.P.; Wermer, M.J.; Brown, R.D., Jr.; Morita, A.; Juvela, S.; Yonekura, M.; Ishibashi, T.; Torner, J.C.; Nakayama, T.; Rinkel, G.J.; et al. Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: A pooled analysis of six prospective cohort studies. Lancet Neurol. 2014, 13, 59–66. [Google Scholar] [CrossRef]
- Etminan, N.; Brown, R.D., Jr.; Beseoglu, K.; Juvela, S.; Raymond, J.; Morita, A.; Torner, J.C.; Derdeyn, C.P.; Raabe, A.; Mocco, J.; et al. The unruptured intracranial aneurysm treatment score: A multidisciplinary consensus. Neurology 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Nanda, A.; Sonig, A.; Banerjee, A.D.; Javalkar, V.K. Microsurgical management of basilar artery apex aneurysms: A single surgeon’s experience from Louisiana State University, Shreveport. World Neurosurg. 2014, 82, 118–129. [Google Scholar] [CrossRef]
- Hernesniemi, J.; Goehre, F. Approaches to upper basilar artery aneurysms. World Neurosurg. 2014, 82, 1001–1002. [Google Scholar] [CrossRef]
- Batjer, H.; Samson, D. Intraoperative aneurysmal rupture: Incidence, outcome, and suggestions for surgical management. Neurosurgery 1986, 18, 701–707. [Google Scholar] [CrossRef]
- Molyneux, A.; Kerr, R.; Stratton, I.; Sandercock, P.; Clarke, M.; Shrimpton, J.; Holman, R.; International Subarachnoid Aneurysm Trial Collaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised trial. Lancet 2002, 360, 1267–1274. [Google Scholar] [CrossRef]
- Ogilvy, C.S.; Hoh, B.L.; Singer, R.J.; Putman, C.M. Clinical and radiographic outcome in the management of posterior circulation aneurysms by use of direct surgical or endovascular techniques. Neurosurgery 2002, 51, 14–21; discussion 21–22. [Google Scholar] [CrossRef] [PubMed]
- Krisht, A.F.; Bikmaz, K.; Kadri, P.A.; Partington, S. Outcome of Surgical Clipping of 40 Complex Basilar Aneurysms Using the Transcavernous Route: Paper 34. Neurosurgery 2006, 58, 407. [Google Scholar] [CrossRef]
- Eskridge, J.M.; Song, J.K. Endovascular embolization of 150 basilar tip aneurysms with Guglielmi detachable coils: Results of the Food and Drug Administration multicenter clinical trial. J. Neurosurg. 1998, 89, 81–86. [Google Scholar] [CrossRef]
- Bavinzski, G.; Killer, M.; Gruber, A.; Reinprecht, A.; Gross, C.E.; Richling, B. Treatment of basilar artery bifurcation aneurysms by using Guglielmi detachable coils: A 6-year experience. J. Neurosurg. 1999, 90, 843–852. [Google Scholar] [CrossRef]
- Tateshima, S.; Murayama, Y.; Gobin, Y.P.; Duckwiler, G.R.; Guglielmi, G.; Vinuela, F. Endovascular treatment of basilar tip aneurysms using Guglielmi detachable coils: Anatomic and clinical outcomes in 73 patients from a single institution. Neurosurgery 2000, 47, 1332–1339; discussion 1339–1342. [Google Scholar] [CrossRef]
- Henkes, H.; Fischer, S.; Mariushi, W.; Weber, W.; Liebig, T.; Miloslavski, E.; Brew, S.; Kuhne, D. Angiographic and clinical results in 316 coil-treated basilar artery bifurcation aneurysms. J. Neurosurg. 2005, 103, 990–999. [Google Scholar] [CrossRef]
- Owen, C.M.; Montemurro, N.; Lawton, M.T. Microsurgical Management of Residual and Recurrent Aneurysms After Coiling and Clipping: An Experience With 97 Patients. Neurosurgery 2015, 62 (Suppl. 1), 92–102. [Google Scholar] [CrossRef]
- Spetzler, R.F.; McDougall, C.G.; Zabramski, J.M.; Albuquerque, F.C.; Hills, N.K.; Russin, J.J.; Partovi, S.; Nakaji, P.; Wallace, R.C. The Barrow Ruptured Aneurysm Trial: 6-year results. J. Neurosurg. 2015, 123, 609–617. [Google Scholar] [CrossRef]
- Ferns, S.P.; Sprengers, M.E.; van Rooij, W.J.; Rinkel, G.J.; van Rijn, J.C.; Bipat, S.; Sluzewski, M.; Majoie, C.B. Coiling of intracranial aneurysms: A systematic review on initial occlusion and reopening and retreatment rates. Stroke 2009, 40, e523–e529. [Google Scholar] [CrossRef]
- van Eijck, M.; Bechan, R.S.; Sluzewski, M.; Peluso, J.P.; Roks, G.; van Rooij, W.J. Clinical and Imaging Follow-Up of Patients with Coiled Basilar Tip Aneurysms Up to 20 Years. AJNR Am. J. Neuroradiol. 2015, 36, 2108–2113. [Google Scholar] [CrossRef] [PubMed]
- Molyneux, A.J.; Kerr, R.S.; Birks, J.; Ramzi, N.; Yarnold, J.; Sneade, M.; Rischmiller, J.; Collaborators, I. Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): Long-term follow-up. Lancet Neurol. 2009, 8, 427–433. [Google Scholar] [CrossRef]
- Ferns, S.P.; Sprengers, M.E.; van Rooij, W.J.; van Zwam, W.H.; de Kort, G.A.; Velthuis, B.K.; Schaafsma, J.D.; van den Berg, R.; Sluzewski, M.; Brouwer, P.A.; et al. Late reopening of adequately coiled intracranial aneurysms: Frequency and risk factors in 400 patients with 440 aneurysms. Stroke 2011, 42, 1331–1337. [Google Scholar] [CrossRef] [PubMed]
- Juvela, S.; Porras, M.; Heiskanen, O. Natural history of unruptured intracranial aneurysms: A long-term follow-up study. J. Neurosurg. 1993, 79, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Juvela, S.; Porras, M.; Poussa, K. Natural history of unruptured intracranial aneurysms: Probability of and risk factors for aneurysm rupture. J. Neurosurg. 2000, 93, 379–387. [Google Scholar] [CrossRef]
- Wiebers, D.O.; Whisnant, J.P.; Huston, J., III; Meissner, I.; Brown, R.D., Jr.; Piepgras, D.G.; Forbes, G.S.; Thielen, K.; Nichols, D.; O’Fallon, W.M.; et al. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003, 362, 103–110. [Google Scholar] [CrossRef]
- Molyneux, A.J.; Birks, J.; Clarke, A.; Sneade, M.; Kerr, R.S. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT). Lancet 2015, 385, 691–697. [Google Scholar] [CrossRef]
- Investigators, U.J.; Morita, A.; Kirino, T.; Hashi, K.; Aoki, N.; Fukuhara, S.; Hashimoto, N.; Nakayama, T.; Sakai, M.; Teramoto, A.; et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N. Engl. J. Med. 2012, 366, 2474–2482. [Google Scholar] [CrossRef]
- Sekhar, L.N.; Tariq, F.; Morton, R.P.; Ghodke, B.; Hallam, D.K.; Barber, J.; Kim, L.J. Basilar tip aneurysms: A microsurgical and endovascular contemporary series of 100 patients. Neurosurgery 2013, 72, 284–298; discussion 298–299. [Google Scholar] [CrossRef]
- Hernesniemi, J.; Korja, M. At the apex of cerebrovascular surgery--basilar tip aneurysms. World Neurosurg. 2014, 82, 37–39. [Google Scholar] [CrossRef]
- Yasargil, M.G.; Antic, J.; Laciga, R.; Jain, K.K.; Hodosh, R.M.; Smith, R.D. Microsurgical pterional approach to aneurysms of the basilar bifurcation. Surg. Neurol. 1976, 6, 83–91. [Google Scholar] [PubMed]
- Drake, C.G. Bleeding aneurysms of the basilar artery. Direct surgical management in four cases. J. Neurosurg. 1961, 18, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Tjahjadi, M.; Kivelev, J.; Serrone, J.C.; Maekawa, H.; Kerro, O.; Jahromi, B.R.; Lehto, H.; Niemela, M.; Hernesniemi, J.A. Factors Determining Surgical Approaches to Basilar Bifurcation Aneurysms and Its Surgical Outcomes. Neurosurgery 2016, 78, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Day, J.D.; Fukushima, T.; Giannotta, S.L. Cranial base approaches to posterior circulation aneurysms. J. Neurosurg. 1997, 87, 544–554. [Google Scholar] [CrossRef]
- Hsu, F.P.; Clatterbuck, R.E.; Spetzler, R.F. Orbitozygomatic approach to basilar apex aneurysms. Neurosurgery 2005, 56 (Suppl. 1), 172–177. [Google Scholar] [CrossRef]
- Gonzalez, L.F.; Amin-Hanjani, S.; Bambakidis, N.C.; Spetzler, R.F. Skull base approaches to the basilar artery. Neurosurg. Focus 2005, 19, E3. [Google Scholar] [CrossRef]
- Kawase, T.; Toya, S.; Shiobara, R.; Mine, T. Transpetrosal approach for aneurysms of the lower basilar artery. J. Neurosurg. 1985, 63, 857–861. [Google Scholar] [CrossRef]
- Kato, Y.; Sano, H.; Behari, S.; Kumar, S.; Nagahisa, S.; Iwata, S.; Kanno, T. Surgical clipping of basilar aneurysms: Relationship between the different approaches and the surgical corridors. Minim. Invasive Neurosurg. MIN 2002, 45, 142–145. [Google Scholar] [CrossRef]
- Spiessberger, A.; Strange, F.; Fandino, J.; Marbacher, S. Microsurgical Clipping of Basilar Apex Aneurysms: A Systematic Historical Review of Approaches and their Results. World Neurosurg. 2018, 114, 305–316. [Google Scholar] [CrossRef]
- Groff, M.W.; Adams, D.C.; Kahn, R.A.; Kumbar, U.M.; Yang, B.Y.; Bederson, J.B. Adenosine-induced transient asystole for management of a basilar artery aneurysm. Case report. J. Neurosurg. 1999, 91, 687–690. [Google Scholar] [CrossRef]
- Lawton, M.T.; Raudzens, P.A.; Zabramski, J.M.; Spetzler, R.F. Hypothermic circulatory arrest in neurovascular surgery: Evolving indications and predictors of patient outcome. Neurosurgery 1998, 43, 10–20; discussion 20–21. [Google Scholar] [CrossRef]
- Samson, D.; Batjer, H.H.; Bowman, G.; Mootz, L.; Krippner, W.J., Jr.; Meyer, Y.J.; Allen, B.C. A clinical study of the parameters and effects of temporary arterial occlusion in the management of intracranial aneurysms. Neurosurgery 1994, 34, 22–28; discussion 28–29. [Google Scholar] [PubMed]
- Elhammady, M.S.; Nakaji, P.; Farhat, H.; Morcos, J.J.; Aziz-Sultan, M.A. Balloon-assisted clipping of a large paraclinoidal aneurysm: A salvage procedure. Neurosurgery 2009, 65, E1210–E1211; discussion E1211. [Google Scholar] [CrossRef] [PubMed]
- Fandino, J.; Taussky, P.; Marbacher, S.; Muroi, C.; Diepers, M.; Fathi, A.R.; Remonda, L. The concept of a hybrid operating room: Applications in cerebrovascular surgery. Acta Neurochir. Suppl. 2013, 115, 113–117. [Google Scholar] [PubMed]
- Sanai, N.; Tarapore, P.; Lee, A.C.; Lawton, M.T. The current role of microsurgery for posterior circulation aneurysms: A selective approach in the endovascular era. Neurosurgery 2008, 62, 1236–1249; discussion 1249–1253. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.T.; Abla, A.A.; Rutledge, W.C.; Benet, A.; Zador, Z.; Rayz, V.L.; Saloner, D.; Halbach, V.V. Bypass Surgery for the Treatment of Dolichoectatic Basilar Trunk Aneurysms: A Work in Progress. Neurosurgery 2016, 79, 83–99. [Google Scholar] [CrossRef]
- Basma, J.; Ryttlefors, M.; Latini, F.; Pravdenkova, S.; Krisht, A. Mobilization of the transcavernous oculomotor nerve during basilar aneurysm surgery: Biomechanical bases for better outcome. Neurosurgery 2014, 10 (Suppl. 1), 106–114; discussion 114–115. [Google Scholar] [CrossRef]
- Shi, X.; Qian, H.; Singh, K.C.; Zhang, Y.; Zhou, Z.; Sun, Y.; Liu, F. Surgical management of vertebral and basilar artery aneurysms: A single center experience in 41 patients. Acta Neurochir. (Wien) 2013, 155, 1087–1093. [Google Scholar] [CrossRef]
- Yanagisawa, T.; Kinouchi, H.; Sasajima, T.; Shimizu, H. Long-Term Follow-Up for a Giant Basilar Trunk Aneurysm Surgically Treated by Proximal Occlusion and External Carotid Artery to Posterior Cerebral Artery Bypass Using a Saphenous Vein Graft. J. Stroke Cerebrovasc. Dis. 2016, 25, e212–e213. [Google Scholar] [CrossRef]
- Indo, M.; Oya, S.; Matsui, T. Ruptured Basilar Tip Aneurysm in a Patient with Bilateral Internal Carotid Artery Occlusion Successfully Treated with Bilateral Superficial Temporal Artery-Middle Cerebral Artery Anastomoses: Case Report. World Neurosurg. 2016, 86, 512.e5–512.e8. [Google Scholar] [CrossRef]
- Kai, Y.; Hamada, J.; Morioka, M.; Yano, S.; Hamasaki, K.; Ushio, Y. Successful treatment of a ruptured dissecting basilar artery aneurysm. Case report. J. Neurosurg. 2004, 100, 1072–1075. [Google Scholar] [CrossRef] [PubMed]
- Krisht, A.F.; Krayenbuhl, N.; Sercl, D.; Bikmaz, K.; Kadri, P.A. Results of microsurgical clipping of 50 high complexity basilar apex aneurysms. Neurosurgery 2007, 60, 242–250; discussion 250–252. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Kobayashi, S.; Hongo, K.; Tada, T.; Nagashima, H.; Kakizawa, Y. Intentional body clipping of wide-necked basilar artery bifurcation aneurysms. J. Neurosurg. 2000, 93, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Matsukawa, H.; Tanikawa, R.; Kamiyama, H.; Tsuboi, T.; Noda, K.; Ota, N.; Miyata, S.; Tokuda, S. Localization in the Interpeduncular Cistern as Risk Factors for the Thalamoperforators’ Ischemia, Poor Outcome, and Oculomotor Nerve Palsy in Patients with Complex Unruptured Basilar Apex Aneurysm Treated with Neck Clipping. World Neurosurg. 2015, 84, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Mooney, M.A.; Kalani, M.Y.; Nakaji, P.; Albuquerque, F.C.; McDougall, C.G.; Spetzler, R.F.; Zabramski, J.M. Long-term Patient Outcomes After Microsurgical Treatment of Blister-Like Aneurysms of the Basilar Artery. Neurosurgery 2015, 11 (Suppl. 3), 387–393. [Google Scholar] [CrossRef]
- Griessenauer, C.J.; Poston, T.L.; Shoja, M.M.; Mortazavi, M.M.; Falola, M.; Tubbs, R.S.; Fisher, W.S., III. The impact of temporary artery occlusion during intracranial aneurysm surgery on long-term clinical outcome: Part I. Patients with subarachnoid hemorrhage. World Neurosurg. 2014, 82, 140–148. [Google Scholar] [CrossRef]
- Taylor, C.L.; Selman, W.R.; Kiefer, S.P.; Ratcheson, R.A. Temporary vessel occlusion during intracranial aneurysm repair. Neurosurgery 1996, 39, 893–905; discussion 905–906. [Google Scholar]
- Steinberg, G.K.; Drake, C.G.; Peerless, S.J. Deliberate basilar or vertebral artery occlusion in the treatment of intracranial aneurysms. Immediate results and long-term outcome in 201 patients. J. Neurosurg. 1993, 79, 161–173. [Google Scholar] [CrossRef]
- Al-Mousa, A.; Bose, G.; Hunt, K.; Toma, A.K. Adenosine-assisted neurovascular surgery: Initial case series and review of literature. Neurosurg. Rev. 2019, 42, 15–22. [Google Scholar] [CrossRef]
- Desai, V.R.; Rosas, A.L.; Britz, G.W. Adenosine to facilitate the clipping of cerebral aneurysms: Literature review. Stroke Vasc. Neurol. 2017, 2, 204–209. [Google Scholar] [CrossRef]
- Mack, W.J.; Ducruet, A.F.; Angevine, P.D.; Komotar, R.J.; Shrebnick, D.B.; Edwards, N.M.; Smith, C.R.; Heyer, E.J.; Monyero, L.; Connolly, E.S., Jr.; et al. Deep hypothermic circulatory arrest for complex cerebral aneurysms: Lessons learned. Neurosurgery 2007, 60, 815–827. [Google Scholar] [CrossRef] [PubMed]
- Konczalla, J.; Platz, J.; Fichtlscherer, S.; Mutlak, H.; Strouhal, U.; Seifert, V. Rapid ventricular pacing for clip reconstruction of complex unruptured intracranial aneurysms: Results of an interdisciplinary prospective trial. J. Neurosurg. 2018, 128, 1741–1752. [Google Scholar] [CrossRef] [PubMed]
- Skrap, M.; Petralia, B.; Toniato, G. Temporary balloon occlusion during the surgical treatment of giant paraclinoid and vertebrobasilar aneurysms. Acta Neurochir. (Wien) 2010, 152, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Mizoi, K.; Yoshimoto, T.; Takahashi, A.; Ogawa, A. Direct clipping of basilar trunk aneurysms using temporary balloon occlusion. J. Neurosurg. 1994, 80, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Thorell, W.; Rasmussen, P.; Perl, J.; Masaryk, T.; Mayberg, M. Balloon-assisted microvascular clipping of paraclinoid aneurysms. Technical note. J. Neurosurg. 2004, 100, 713–716. [Google Scholar] [CrossRef]
- MacDonald, J.D.; Gyorke, A.; Jacobs, J.M.; Mohammad, S.F.; Sunderland, P.M.; Reichman, M.V. Acute phase vascular endothelial injury: A comparison of temporary arterial occlusion using an endovascular occlusive balloon catheter versus a temporary aneurysm clip in a pig model. Neurosurgery 1994, 34, 876–881; discussion 881. [Google Scholar] [CrossRef]
- Kinjo, T.; Mizoi, K.; Takahashi, A.; Yoshimoto, T.; Suzuki, J. A successfully treated case of giant basilar artery aneurysm utilizing balloon catheter occlusion and brain protective substances. No Shinkei Geka 1986, 14 (Suppl. 3), 397–402. [Google Scholar]
- Shucart, W.A.; Kwan, E.S.; Heilman, C.B. Temporary balloon occlusion of a proximal vessel as an aid to clipping aneurysms of the basilar and paraclinoid internal carotid arteries: Technical note. Neurosurgery 1990, 27, 116–119. [Google Scholar] [CrossRef]
- Xu, F.; Huang, L.; Xu, B.; Gu, Y.; Leng, B. Endovascular Retrograde Suction Decompression-Assisted Clipping of Large Paraclinoid Aneurysm in Hybrid Operating Room: 2-Dimensional Operative Video. World Neurosurg. 2018, 114, 178. [Google Scholar] [CrossRef]
- Ricci, G.; Ricci, A.; Gallucci, M.; Zotta, D.; Scogna, A.; Costagliola, C.; Galzio, R.J. Combined endovascular and microsurgical approach in the treatment of giant paraclinoid and vertebrobasilar aneurysms. J. Neurosurg. Sci. 2005, 49, 1–6. [Google Scholar]
- Ng, P.Y.; Huddle, D.; Gunel, M.; Awad, I.A. Intraoperative endovascular treatment as an adjunct to microsurgical clipping of paraclinoid aneurysms. J. Neurosurg. 2000, 93, 554–560. [Google Scholar] [CrossRef] [PubMed]
- Albert, F.K.; Forsting, M.; Aschoff, A.; Krieger, D.; Kunze, S. Clipping of proximal paraclinoid aneurysms with support of the balloon-catheter "trapping-evacuation" technique. Technical note. Acta Neurochir. (Wien) 1993, 125, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Fulkerson, D.H.; Horner, T.G.; Payner, T.D.; Leipzig, T.J.; Scott, J.A.; Denardo, A.J.; Redelman, K.; Goodman, J.M. Endovascular retrograde suction decompression as an adjunct to surgical treatment of ophthalmic aneurysms: Analysis of risks and clinical outcomes. Neurosurgery 2009, 64 (Suppl. 3), ons107–ons111; discussion ons111–ons112. [Google Scholar] [CrossRef] [PubMed]
- Bailes, J.E.; Deeb, Z.L.; Wilson, J.A.; Jungreis, C.A.; Horton, J.A. Intraoperative angiography and temporary balloon occlusion of the basilar artery as an adjunct to surgical clipping: Technical note. Neurosurgery 1992, 30, 949–953. [Google Scholar]
- Petralia, B.; Skrap, M. Temporary Balloon Occlusion during Giant Aneurysm Surgery. A Technical Description. Interv. Neuroradiol. 2006, 12, 245–250. [Google Scholar] [CrossRef]
- Hacein-Bey, L.; Connolly, E.S., Jr.; Mayer, S.A.; Young, W.L.; Pile-Spellman, J.; Solomon, R.A. Complex intracranial aneurysms: Combined operative and endovascular approaches. Neurosurgery 1998, 43, 1304–1312; discussion 1312–1313. [Google Scholar]
- Steiger, H.J.; Lins, F.; Mayer, T.; Schmid-Elsaesser, R.; Stummer, W.; Turowski, B. Temporary aneurysm orifice balloon occlusion as an alternative to retrograde suction decompression for giant paraclinoid internal carotid artery aneurysms: Technical note. Neurosurgery 2005, 56 (Suppl. 2), E442. [Google Scholar] [CrossRef]
- Scott, J.A.; Horner, T.G.; Leipzig, T.J. Retrograde suction decompression of an ophthalmic artery aneurysm using balloon occlusion. Technical note. J. Neurosurg. 1991, 75, 146–147. [Google Scholar] [CrossRef]
- Hoh, D.J.; Larsen, D.W.; Elder, J.B.; Kim, P.E.; Giannotta, S.L.; Liu, C.Y. Novel use of an endovascular embolectomy device for retrograde suction decompression-assisted clip ligation of a large paraclinoid aneurysm: Technical case report. Neurosurgery 2008, 62 (Suppl. 2), ONSE412–ONSE413; discussion ONSE413–ONSE414. [Google Scholar] [CrossRef] [PubMed]
- Fahlbusch, R.; Nimsky, C.; Huk, W. Open surgery of giant paraclinoid aneurysms improved by intraoperative angiography and endovascular retrograde suction decompression. Acta Neurochir. (Wien) 1997, 139, 1026–1032. [Google Scholar] [CrossRef]
- Arnautovic, K.I.; Al-Mefty, O.; Angtuaco, E. A combined microsurgical skull-base and endovascular approach to giant and large paraclinoid aneurysms. Surg. Neurol. 1998, 50, 504–518; discussion 518–520. [Google Scholar] [CrossRef]
- Mizoi, K.; Takahashi, A.; Yoshimoto, T.; Fujiwara, S.; Koshu, K. Combined endovascular and neurosurgical approach for paraclinoid internal carotid artery aneurysms. Neurosurgery 1993, 33, 986–992. [Google Scholar] [PubMed]
- Capo, G.; Vescovi, M.C.; Toniato, G.; Petralia, B.; Gavrilovic, V.; Skrap, M. Giant vertebral aneurysm: A case report detailing successful treatment with combined stenting and surgery. Surg. Neurol. Int. 2018, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- Marbacher, S.; Kienzler, J.C.; Mendelowitsch, I.; D’Alonzo, D.; Andereggen, L.; Diepers, M.; Remonda, L.; Fandino, J. Comparison of Intra- and Postoperative 3-Dimensional Digital Subtraction Angiography in Evaluation of the Surgical Result After Intracranial Aneurysm Treatment. Neurosurgery 2019, nyz487. [Google Scholar] [CrossRef] [PubMed]
- Marbacher, S.; Mendelowitsch, I.; Gruter, B.E.; Diepers, M.; Remonda, L.; Fandino, J. Comparison of 3D intraoperative digital subtraction angiography and intraoperative indocyanine green video angiography during intracranial aneurysm surgery. J. Neurosurg. 2018, 131, 64–71. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).