Abstract
This study evaluated the push-out bond strength (PBS) and failure modes of fiber posts cemented with silane-containing self-adhesive resin cement (SARC) compared with conventional SARC and universal adhesive strategies, considering the effects of root section and aging. Ninety single-rooted human premolars were equally assigned to three cementation protocols: silane-containing SARC (PANAVIA SA Cement Universal), conventional SARC (RelyX Universal), and universal adhesive plus SARC (Scotchbond Universal Plus + RelyX Universal). Each group was divided into two aging subgroups: 24 h water storage and thermal cycling (10,000 cycles between 5 °C and 55 °C, 30 s dwell time; n = 15). After root canal treatment and post space preparation, glass fiber posts were cemented, and each root was sectioned to obtain six slices. PBS was measured using a push-out test, and failure modes were examined under stereomicroscopy. Data were analyzed using three-way ANOVA, post hoc tests, Spearman’s correlation, and logistic regression (α = 0.05). Cement type, root section, and aging significantly influenced PBS (p < 0.001). PBS decreased from coronal to apical sections, and thermal cycling reduced PBS in all groups. The universal adhesive plus SARC achieved the highest PBS, while conventional SARC had the lowest PBS. Cementdentin adhesive failures (FM2) predominated overall, with proportions varying between 43% and 90%, and higher PBS values were associated with fewer FM2 failures. The combination of a universal adhesive with SARC provided superior bonding compared to simplified protocols. Although silane-containing SARC improved bonding relative to conventional SARC, durable adhesion to radicular dentin remains challenging, particularly in apical regions.
1. Introduction
The restoration of severely compromised endodontically treated teeth frequently requires the placement of intraradicular posts to provide adequate retention and support for the coronal restoration [1]. The success of post-retained restorations largely depends on the quality of adhesion achieved at the postcementdentin interface, which represents one of the most challenging bonding scenarios in adhesive dentistry due to the complex intraradicular environment characterized by limited light access, moisture control difficulties, and altered dentin substrate properties [2]. The imperfectly bonded dentinadhesive interface is susceptible to hydrolytic degradation and bacterial and enzyme attack, severely jeopardizing longevity of restorations [3]. Microgaps that develop along the post-cementdentin interface may allow the penetration of oral fluids and bacteria. Such bacterial microleakage has been associated with secondary infection, inflammatory reactions in the periapical tissues, and long-term failure of endodontically treated teeth, particularly when adhesive sealing is inadequate. Therefore, improving the integrity of the adhesive interface is essential for minimizing bacterial ingress and enhancing the longevity of fiber post restorations. The incorporation of functional monomers in dental adhesive systems promotes chemical interaction with dental substrates, resulting in higher adhesion forces when compared to micromechanical adhesion only [4], and among these functional monomers, 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) has emerged as a cornerstone in modern adhesive dentistry. The 10-MDP monomer has the capacity to produce an acid-base-resistant zone on the adhesive interface, which increases the response to acid-base challenges [4], and the adhesion established by these systems is stable over time [5].
The clinical application of adhesive systems has evolved toward simplified protocols that reduce technique sensitivity while maintaining reliable bonding performance. Self-adhesive resin cements (SARCs) combine easy application of conventional luting materials with improved mechanical properties and bonding capability of resin cements [6], as they contain functional acidic monomers that simultaneously condition and prime the tooth substrate, eliminating the need for separate pretreatment steps [7]. The role of silane coupling agents in fiber post bonding has been extensively debated in the literature, as surface treatments of glass fiber posts can enhance bonding performance, with silane application being one of the most investigated approaches [8]. However, conflicting evidence exists regarding the necessity of silanization when using SARCs, since recent systematic reviews indicate that silane application alone may not always provide significant improvements in bond strength when SARCs are used [8]. Some studies suggest that the bond strength of SARCs was significantly higher compared to conventional cements, even without post-surface treatments [9,10]. The effectiveness of silane treatment appears to be influenced by multiple factors, including the composition of the cement system, post-surface characteristics, and the specific silane formulation employed [9].
Universal adhesive systems have gained considerable attention due to their versatility in application modes and simplified clinical protocols, as these systems can be applied in both etch-and-rinse and self-etch modes, providing clinicians with flexibility while maintaining reliable bonding performance [11]. Recent studies demonstrate that universal adhesives can achieve comparable bond strengths to dentin regardless of the application mode, though etch-and-rinse strategies may provide slight advantages in certain clinical scenarios [12]. Contemporary adhesive dentistry has advanced significantly, with universal adhesive systems showing improved long-term clinical performance in various applications, and recent clinical evidence suggests favorable long-term performance of universal adhesives, with clinical trials demonstrating reliable retention rates and acceptable marginal adaptation over extended follow-up periods [13,14,15]. Five-year clinical evaluations have shown that universal adhesives can maintain stable bonding performance when applied following appropriate protocols [16].
The long-term stability of postcementdentin bonds is critically important for clinical success, since aging studies consistently demonstrate that thermal cycling significantly affects bond strength values, though the magnitude of degradation varies considerably among different cement systems [17]. Recent investigations have shown that SARCs may be particularly susceptible to degradation over time, with some studies reporting significant decreases in bond strength after aging protocols [18,19], and the resistance of resindentin bonds to thermal-aging degradation appears to be material-dependent, with 10-MDP-containing systems generally showing superior durability [4]. In vitro thermal cycling remains an indispensable method for initial screening of dental materials, typically involving alternating temperature exposure between 5 °C and 55 °C to simulate thermal stress encountered in the oral environment [17,20].
A significant advancement in adhesive cementation has been the development of silane-containing SARCs. PANAVIA SA Cement Universal (Kuraray Noritake, Tokyo, Japan) represents a recent development as an SARC containing an integrated silane coupling agent (LCSi monomer) combined with the established 10-MDP functional monomer, and this dual functionality potentially eliminates the complexity associated with separate silane application while maintaining the chemical bonding advantages of both 10-MDP and silane coupling mechanisms. Research has demonstrated that incorporating silane in a 10-MDP-based SARC combines efficient silane-coupling ability at ceramic surfaces with effective bonding ability to dentin [21], which represents a recent advancement in cement technology, offering simplified clinical procedures with the potential for effective bonding.
Despite the promising characteristics of silane-containing SARCs, limited research has specifically evaluated their performance in intraradicular post cementation compared to conventional approaches, and the formulation of PANAVIA SA Cement Universal, combining both 10-MDP and integrated silane coupling agent (LCSi monomer) in a single-component system, represents a development in SARC formulation that warrants systematic evaluation. Furthermore, the comparative performance of this integrated approach versus the traditional combination of universal adhesive systems with conventional SARCs has not been thoroughly investigated in the context of fiber post bonding [1]. Understanding the relative merits of these different adhesive strategies is crucial for evidence-based clinical decision-making, particularly given the complexity of the intraradicular bonding environment and the long-term loading conditions that post-retained restorations must withstand.
Although self-adhesive resin cements (SARCs) are widely used in restorative dentistry, the performance of a silane-containing SARC in intraradicular post cementation has not yet been systematically compared with a universal adhesive + SARC strategy under both immediate and thermally aged conditions across coronalmiddleapical root sections. In addition, the association between push-out bond strength and failure mode patterns has rarely been modeled using multivariable approaches. This study specifically addresses these gaps by combining a three-factor design with failure-mode-oriented logistic regression. Therefore, the aim of this in vitro study was to evaluate and compare the push-out bond strength and failure modes of fiber posts cemented with three different adhesive approaches: a silane-containing SARC, a conventional SARC, and a universal adhesive system combined with conventional SARC. The evaluation was conducted across different root canal sections (coronal, middle, and apical) under both immediate and thermally aged conditions to simulate clinical service conditions. It was hypothesized that there would be no significant differences in push-out bond strength or failure mode distribution between the three cementation systems tested, and that root canal section and thermal cycling aging would not significantly influence bonding performance.
2. Materials and Methods
2.1. Study Design
This laboratory study was prepared in accordance with the Preferred Reporting Items for Laboratory studies in Endodontology (PRILE) 2021 guidelines, and the PRILE 2021 flowchart was followed (Figure 1). The study was conducted in accordance with the Declaration of Helsinki and its subsequent revisions, and ethical approval was obtained from the Clinical Research Ethics Committee of Altinbas University (2022/146). Patient consent forms were completed for all tooth donors. A total of 90 single-rooted human premolars were used, equally distributed among three cementation protocols (n = 30 per protocol). Within each protocol, teeth were assigned to two aging conditions (24 h and thermal cycling; 10,000 cycles; n = 15 per subgroup). Each tooth provided three root sections (coronal, middle, and apical), with two slices obtained per section, yielding six slices per tooth and 540 slices in total. These factors resulted in 18 experimental cells (3 × 3 × 2).
Figure 1.
PRILE 2021 flowchart.
An a priori power analysis was conducted using G*Power (version 3.1; Heinrich Heine University, Düsseldorf, Germany) for a fixed-effects three-way ANOVA (3 × 3 × 2 design) to detect medium main effects (f = 0.25) with α = 0.05 and power (1-β) = 0.80 [22]. The analysis indicated a minimum of n = 15 teeth per aging subgroup within each Cement Type × Root Section cell. This matched the experimental allocation and ensured adequate power, corresponding to 30 slices per cell (15 teeth × 2 slices per section).
2.2. Specimen Selection and Preparation
Single-rooted human premolars with similar root dimensions extracted for periodontal or orthodontic reasons were collected with informed consent under institutional review board approval. To minimize anatomical variability and ensure standardization, teeth were selected based on comparable root length, diameter, and morphology. The inclusion criteria were a single straight root canal, a fully formed apex, absence of caries, root cracks, or previous endodontic treatment. Extracted teeth were disinfected in 0.5% chloramine-T (Sigma-Aldrich, St. Louis, MO, USA) solution for 24 h and then stored in distilled water at 4 °C for no longer than six months until sample preparation. The crowns were sectioned perpendicular to the long axis 2 mm coronal to the cemento-enamel junction using a low-speed diamond disc (IsoMet High Speed Pro; Buehler, Lake Bluff, IL, USA) under water cooling, and root length was standardized to 16 mm.
2.3. Endodontic Treatment and Post Space Preparation
Root canal preparation was performed using the ProTaper Universal rotary file system (Dentsply Sirona, Ballaigues, Switzerland) up to size F3 with Dentsply X-smart IQ endodontic motor (Dentsply Sirona, Ballaigues, Switzerland). Canals were irrigated with 2 mL of 2.5% sodium hypochlorite (NaOCl) between each instrument, followed by final irrigation with 17% EDTA for 1 min and 5 mL of 2.5% NaOCl. After drying with sterile paper points, canals were obturated with gutta-percha and AH Plus sealer (Dentsply Sirona, Ballaigues, Switzerland) using the lateral condensation technique, and access cavities were sealed with temporary restoration (Cavit; 3M ESPE/Solventum, St. Paul, MN, USA). All specimens were stored in distilled water at 37 °C, which provides 100% humidity and prevents dehydration of dentin during the experimental period. Following one week of storage in distilled water at 37 °C to allow complete sealer polymerization and minimize sealer-cement interference, post spaces were prepared using a standardized protocol [23]. Gutta-percha was removed with heated Peeso reamers, leaving 5 mm of apical filling material, and post space preparation was completed with a fiber post drill system (Glassix; Nordin, Chailly, Switzerland) to a depth of 10 mm and diameter of 1.4 mm. Final irrigation was performed with 2.5% NaOCl, followed by distilled water, and canals were dried with paper points.
2.4. Experimental Groups and Cementation Protocol
Specimens were randomly assigned to three cement groups with equal distribution (n = 30 teeth per group), based on their adhesive approach and chemical composition.
- Silane-containing SARC group: PANAVIA SA Cement Universal (Kuraray Noritake, Tokyo, Japan), a dual-cure SARC with integrated silane coupling agent, applied according to the manufacturer’s instructions without requiring separate primer or adhesive application.
- SARC group: RelyX Universal (3M ESPE/Solventum, St. Paul, MN, USA), a conventional, dual-cure SARC applied in self-adhesive mode without separate primer or adhesive components.
- Universal adhesive + SARC group: A universal adhesive (Scotchbond Universal Plus; 3M ESPE/Solventum, St. Paul, MN, USA) was applied in self-etch mode for 20 s with gentle agitation, air-thinned for 5 s, light-cured for 10 s, followed by RelyX Universal application.
Glass fiber posts (Glassix size 1.35; Nordin, Chailly, Switzerland) were cleaned with 70% ethanol and air-dried, while post spaces were also cleaned with 70% ethanol using microbrush applicators. Luting agents were applied to both post surfaces and canal walls using appropriate delivery systems, and posts were inserted slowly to full depth with gentle finger pressure and maintained under consistent seating pressure for 5 min. Excess cement was carefully removed, and light-curing was performed from the coronal aspect for 40 s using an LED curing unit (1000 mW/cm2; Valo Grand; Ultradent, South Jordan, UT, USA).
Within each cementation protocol group (30 teeth), specimens were split into two aging conditions: 24 h (n = 15 teeth) and thermal cycling (n = 15 teeth). After the initial 24 h distilled water storage at 37 °C, the thermal cycling group underwent 10,000 cycles alternating between 5 °C and 55 °C with a 30 s dwell time in each bath and a 10 s transfer time between baths using an automated thermal cycling machine (Esetron, Ankara, Turkey), simulating approximately one year of clinical service and assessing the durability of the postcementdentin interface under thermal stress. All aging procedures were performed while the teeth remained as whole specimens. Samples in the immediate group were stored in distilled water for 24 h, whereas specimens in the thermal cycling group underwent the thermal cycling protocol. Aging was completed before any sectioning was performed. After aging, each specimen was embedded in acrylic resin (Imicryl, Konya, Turkey) to stabilize it during sectioning.
2.5. Push-Out Bond Strength Testing
Specimens were embedded in acrylic resin and serially sectioned perpendicular to the long axis using a precision cutting machine (IsoMet High Speed Pro; Buehler, Lake Bluff, IL, USA) under water cooling, producing six 2 mm thick slices per tooth (two per root section: coronal, middle, and apical). Sectioning was performed with a precision low-speed diamond saw under continuous water cooling to minimize vibration and mechanical stresses during slice preparation, as recommended in push-out testing methodologies. Push-out tests were performed using a universal testing machine (Esetron, Ankara, Turkey) with a 1 kN load cell. Specimens were positioned on a custom-made stainless-steel fixture with a central hole larger than the post diameter to allow free extrusion, and loading was applied in the apical-to-coronal direction using cylindrical steel plungers of appropriate diameter (1.2 mm for coronal, 1.0 mm for middle, 0.8 mm for apical sections) at a crosshead speed of 0.5 mm/min until post segment dislodgment occurred. The specimenpunch alignment and mounting configuration are illustrated in Figure 2. Push-out bond strength was calculated by dividing the maximum failure load in Newtons by the bonded surface area in square millimeters, determined using the cylindrical surface area formula (π × post diameter × slice thickness). To ensure accuracy, post diameters were measured at both the coronal and apical surfaces of each slice with a digital caliper (±0.01 mm), and values were averaged for the final calculation.
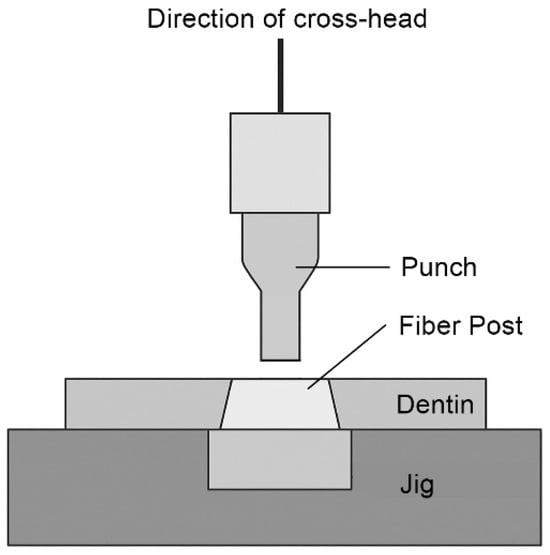
Figure 2.
The specimenpunch alignment and mounting configuration.
All fractured specimens were examined under a stereomicroscope (SMZ745T; Nikon, Tokyo, Japan) at 40× magnification to determine the predominant failure mode, and each specimen was classified into one of five categories: adhesive failure at the postcement interface (FM1), adhesive failure at the cementdentin interface (FM2), mixed failure involving both interfaces (FM3), cohesive failure within the cement (FM4), or cohesive failure within dentin (FM5).
2.6. Statistical Analysis
All statistical analyses were performed using R software (version 4.5.1; R Foundation for Statistical Computing, Vienna, Austria). Descriptive statistics (mean, standard deviation, 95% confidence intervals, and sample size) were calculated for each group, and a three-way ANOVA was conducted to assess the effects of cement type, root section, and aging condition (Immediate vs. Thermal Cycling) on push-out bond strength, including their two-way and three-way interactions. Effect size estimates (η2 and partial η2) were additionally reported. Post hoc multiple comparisons were performed with Tukey’s HSD test and presented with compact letter displays (CLD). Failure mode distributions were analyzed descriptively and illustrated as stacked bar charts. To explore the relationship between bond strength and failure mode, Spearman’s rank correlation was first applied as a non-parametric measure of association, followed by binary logistic regression with cementdentin adhesive failure (FM2) as the dependent outcome. Both crude and adjusted models were fitted, with the latter including cement type, root section, and aging as covariates, and odds ratios (OR) with 95% confidence intervals were reported. Complementary chi-square analysis compared FM2 prevalence across bond strength quartiles, and a significance level of α = 0.05 was adopted for all statistical tests.
3. Results
3.1. Push-Out Bond Strength (PBS) Evaluation
The three-way ANOVA (Table 1) demonstrated that cement type, root section, and aging condition each exert a statistically significant effect on push-out bond strength (p < 0.001). All interaction terms were non-significant (p > 0.05) and had negligible effect sizes (η2 < 0.01), confirming that the factors acted independently (Table 1). Effect size analysis revealed that the root section was the dominant factor (η2 = 0.475, partial η2 = 0.606), explaining the largest proportion of variance in bond strength. This was followed by cement type (η2 = 0.173, partial η2 = 0.359) and aging (η2 = 0.039, partial η2 = 0.112), both of which also showed meaningful contributions.

Table 1.
Three-way ANOVA results with effect size estimates (η2 and partial η2) for push-out bond strength (MPa).
Descriptive statistics of bond strength values are presented in Table 2. Across both aging conditions, bond strength consistently decreased from the coronal to the apical sections. Among the cement systems, the universal adhesive + SARC group exhibited the highest bond strength values, followed by the silane-containing SARC group, while the SARC group presented the lowest. Aging had a clear effect in all groups, as thermal cycling significantly reduced bond strength compared with the immediate condition (p < 0.05 for all subgroups). Pairwise analyses indicated that in the immediate condition, coronal sections bonded with the universal adhesive + SARC group and the silane-containing SARC group formed the highest-performing groups, whereas under thermal cycling conditions, coronal samples from the universal adhesive + SARC group retained the top performance, while apical samples from the SARC group represented the lowest. All analyses were conducted at the slice level (n = 540 slices), derived from 90 teeth as described in the methodology.

Table 2.
Descriptive statistics (mean, standard deviation, minimum, maximum, and sample size) of push-out bond strength (MPa) for different cement types, root sections, and aging conditions.
3.2. Failure Mode Distribution
Figure 3 illustrates the distribution of failure modes by cement type, root section, and aging condition. Cementdentin adhesive failures (FM2) were overall the most frequent, although proportions varied substantially between groups, ranging from approximately 43% to more than 90%. Postcement adhesive failures (FM1) were more frequent in the universal adhesive + SARC group, while mixed failures (FM3) appeared only in coronal sections of the silane-containing SARC group and the universal adhesive + SARC group. No cohesive failures (FM4 or FM5) were observed. The overall trends were similar between immediate and thermal cycling conditions, suggesting that aging did not substantially alter failure mode proportions.
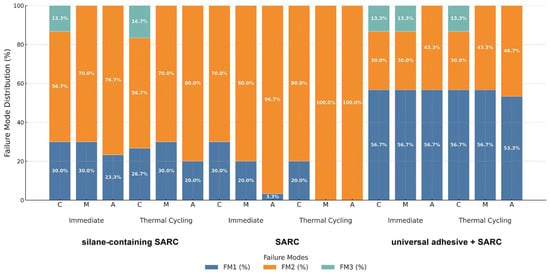
Figure 3.
Failure mode distribution of fiber postcementdentin specimens according to cement type, root section, and aging condition. Bars represent the percentage of each failure mode (FM1: adhesive at postcement interface, FM2: adhesive at cementdentin interface, FM3: mixed failure, FM4: cohesive within cement, FM5: cohesive within dentin). Data are presented separately for Immediate and Thermal Cycling conditions within each cement group (silane-containing SARC, SARC, universal adhesive + SARC). Percentage values are shown within the bars. FM4 and FM5 were not observed in any group. Failure modes are summarized as A (adhesive failures: FM1+FM2), M (mixed failure: FM3), and C (cohesive failures: FM4+FM5). Small discrepancies in total percentages are attributable to rounding.
3.3. Correlation and Regression Analysis
Spearman’s correlation revealed a significant negative association between bond strength and failure mode (ρ = −0.421, p < 0.001), indicating that higher bond strength values were associated with a reduced probability of cementdentin adhesive failures (FM2). Logistic regression analysis confirmed this relationship (Table 3). In the crude model, bond strength significantly decreased the odds of FM2 (OR = 0.600; 95% CI: 0.5480.657; p < 0.001). In the adjusted model, which included cement type, root section, and aging, bond strength remained a strong independent predictor (Adjusted OR = 0.369; 95% CI: 0.3050.448; p < 0.001). FM2 failures were markedly less frequent in middle and apical sections compared to coronal sections, and under thermal cycling compared to immediate conditions. Moreover, the universal adhesive + SARC group exhibited significantly lower odds of FM2 compared with the silane-containing SARC group. Complementary chi-square analysis supported these findings, demonstrating that FM2 prevalence decreased monotonically across increasing bond strength quartiles (Q1: lowest 25% vs. Q4: highest 25%; χ2 = 165.85, df = 3, p < 0.001).

Table 3.
Logistic regression analysis of the association between bond strength and cementdentin adhesive failure (FM2).
4. Discussion
The present study was designed to evaluate and compare the push-out bond strength and failure modes of fiber posts cemented with three different adhesive approaches: silane-containing SARC group, SARC group, and universal adhesive + SARC group. This investigation addresses a critical gap in current endodontic literature regarding the performance of innovative silane-incorporated SARCs in intraradicular post cementation. The results of this investigation led to the rejection of both null hypotheses. Significant differences were observed between the three cementation systems in terms of push-out bond strength (p < 0.001), with the universal adhesive + SARC group demonstrating superior performance, followed by the silane-containing SARC group, and the SARC group showing the lowest values. Additionally, root canal section and thermal cycling aging significantly influenced bonding performance regardless of the cementation system used (p < 0.001).
The superior performance of the universal adhesive + SARC group can be attributed to the synergistic effect of dual bonding mechanisms. Recent studies have demonstrated that universal adhesive systems achieve enhanced bonding effectiveness through the incorporation of functional monomers, particularly 10-MDP, which forms stable chemical bonds with tooth substrates [24]. The etch-and-rinse capability of Scotchbond Universal Plus creates micromechanical retention through dentin demineralization, while simultaneously providing chemical adhesion through 10-MDP-calcium salt formation [25]. This dual approach appears particularly advantageous in the challenging intraradicular environment where moisture control and light access are limited. Contemporary evidence supports the clinical efficacy of universal adhesive systems, with evaluations demonstrating stable bonding performance when applied following appropriate protocols [26]. The versatility of these systems in both etch-and-rinse and self-etch modes provides clinicians with procedural flexibility while maintaining reliable bonding effectiveness [16].
The silane-containing SARC group represents an advancement in SARC formulation by integrating both 10-MDP functional monomer and LCSi silane coupling agent within a single-component system [27,28]. The intermediate performance observed in this study reflects the dual functionality of this material. The 10-MDP monomer provides chemical bonding to dentin through phosphatecalcium interactions, while the proprietary LCSi monomer theoretically enhances bonding to silica-based substrates without requiring separate silanization procedures. Recent clinical evaluations have reported favorable performance of the silane-containing SARC group, with laboratory data confirming high initial shear bond strength values to dentin and various substrates. However, the present findings suggest that in the specific context of fiber post cementation, the integrated approach may not fully compensate for the bonding efficiency achieved through separate adhesive application. This observation aligns with recent systematic reviews indicating that while silane-containing SARCs offer procedural simplification, their bonding performance may vary depending on substrate characteristics and clinical application [28].
The relatively lower performance of the SARC group when used without adhesive pretreatment indicates the limitations inherent in conventional SARC formulations. Despite containing functional acidic monomers designed to simultaneously condition and prime tooth substrates, these materials may achieve suboptimal bonding in challenging clinical scenarios such as intraradicular post space [6]. The acidic monomers in SARCs create a more aggressive initial pH, which may compromise long-term bond stability through incomplete neutralization and persistent acidity at the interface [25].
The pronounced influence of root canal section on bond strength (η2 = 0.475) represents the most significant finding of this investigation. The consistent decrease in bond strength from coronal to apical sections can be attributed to several anatomical and morphological factors. Dentinal tubule density and diameter vary significantly along the root length, with coronal dentin exhibiting larger tubules (approximately 4.32 μm) compared to middle (3.74 μm) and apical regions (1.73 μm) [29]. This morphological variation directly impacts the available surface area for micromechanical retention and chemical bonding mechanisms [29]. Furthermore, the decreased number of dentinal tubules per unit area in the apical region, combined with increased mineralization and potential tubular sclerosis, creates less favorable conditions for adhesive infiltration and polymerization [17]. Consequently, the observed regional variations in bond strength have important clinical implications for post cementation protocols. While the 5 mm apical seal remains paramount for endodontic success, the reduced bonding effectiveness in the apical third suggests that reliance on bonding for post retention should be concentrated in the coronal and middle portions of the root canal. This finding is consistent with current clinical recommendations advocating for post length optimization primarily in the coronal two-thirds of the root canal space.
Thermal cycling significantly reduced bond strength across all experimental groups (p < 0.001), with the magnitude of degradation varying among cement systems. This finding aligns with extensive literature demonstrating that resindentin bonds are susceptible to hydrolytic degradation over time, particularly when subjected to thermal stress [3]. The alternating temperature exposure between 5 °C and 55 °C simulates thermal stress encountered in the oral environment, leading to differential thermal expansion between materials and potential interfacial stress concentration. Recent investigations have identified that SARCs may be particularly vulnerable to aging-related degradation, with significant bond strength decreases reported after thermal cycling protocols [24]. The resistance to thermal-aging degradation appears to be material-dependent, with 10-MDP-containing systems generally demonstrating superior durability compared to systems lacking this functional monomer [26]. Moreover, the observed bond strength reduction following thermal cycling raises important considerations for long-term clinical success. While immediate bond strength values may appear adequate, the progressive deterioration under simulated aging conditions suggests the need for conservative treatment planning and long-term monitoring. The differential aging response among cement systems indicates that material selection should consider not only immediate bonding performance but also anticipated durability under clinical loading conditions.
The effect of aging and specimen preparation on push-out bond strength tests has been a subject of methodological scrutiny. Research indicates that the height of disk specimens significantly affects push-out bond strength results [30], with studies demonstrating that thermal cycling protocols can impact bond strength values differently depending on the adhesive system used [31]. Recent investigations combining fiber post cementation with thermal aging protocols have shown that applying aging procedures to intact restored roots prior to sectioning yields reliable retention values across different resin cement systems [6]. Studies investigating thermal cycling effects on self-adhesive resin cements found that factors such as cement type and thermal cycling significantly influence bond strengths, though some cement systems show increased bond strength after thermal challenge [32]. Furthermore, methodological evaluations have demonstrated that combined thermal and mechanical aging methods provide more clinically relevant bond strength assessments than water storage alone [31]. In the present work, thermal cycling was applied to the whole restored specimens before sectioning and slice preparation for push-out testing, consistent with these practices. This methodological choice helps minimize risks related to acrylic embedding, dehydration, or mechanical stresses during sectioning, thus supporting the validity of the bond-strength measurements under thermal cycling conditions.
The predominance of cementdentin adhesive failures (FM2) was overall the most frequent, with proportions ranging from approximately 43% to more than 90% depending on the group. This variation identifies the cementdentin interface as the critical weak link in the postcementdentin complex. This finding is consistent with numerous studies demonstrating that radicular dentin presents unique challenges for adhesive bonding, including altered surface characteristics following endodontic treatment, limited access for moisture control, and reduced light penetration for optimal polymerization [33]. The negative correlation between bond strength and FM2 prevalence (ρ = −0.421, p < 0.001) indicates that improved bonding performance is associated with a higher proportion of mixed failures and postcement interface failures, which represent less critical failure patterns compared with cementdentin adhesive failures (FM2). Higher bond strength values were correlated with increased prevalence of mixed failures and postcement interface failures, suggesting more balanced stress distribution within the adhesive complex. Additionally, thermal cycling did not substantially alter failure mode distributions, suggesting that while bond strength values decreased, the fundamental failure mechanisms remained consistent. This observation indicates that thermal aging primarily weakens existing interfaces rather than altering the predominant failure pathways. The stability of failure patterns across aging conditions supports the validity of immediate testing protocols for predicting long-term failure modes, although quantitative bond strength assessment requires aging simulation.
The findings of this study provide useful evidence to guide clinical material selection in fiber post cementation. The superior performance of the universal adhesive + SARC group supports a multi-step approach when optimal bonding is critical. While this approach requires additional procedural steps compared to simplified self-adhesive protocols, the enhanced bonding effectiveness may justify the increased complexity in cases where post retention is primarily dependent on adhesive mechanisms. The intermediate performance of the silane-containing SARC group suggests that integrated silane-containing SARCs may represent a reasonable compromise between procedural simplicity and bonding effectiveness. This finding is particularly relevant for clinical scenarios where simplified protocols are advantageous, such as in cases with limited time constraints or when multiple posts require cementation. Furthermore, the pronounced influence of root canal section on bonding effectiveness has direct implications for post design and cementation protocols. Clinical techniques should prioritize optimal adhesive application and polymerization in the coronal and middle thirds of the post space, where bonding conditions are most favorable. The use of appropriate light-conducting systems or dual-cure formulations becomes particularly critical in the apical regions where light access is limited [34]. Additionally, the thermal cycling results emphasize the importance of proper post space preparation, moisture control, and complete polymerization to optimize long-term bond durability.
This in vitro investigation has several limitations. It used extracted human premolars under controlled laboratory conditions; although clinically relevant, in vitro thermal cycling may not fully reproduce intraoral loading and environmental challenges. The 24 h testing protocol and push-out test methodology may also differ from actual clinical scenarios. Future research should focus on long-term clinical trials to validate these findings, investigate the molecular mechanisms of integrated silane-containing cements, and evaluate the influence of different irrigation protocols on bonding effectiveness. Advanced analytical techniques such as micro-CT analysis and confocal microscopy could provide deeper insights into cementdentin interface characteristics and failure mechanisms.
5. Conclusions
Within the limitations of this in vitro study, the universal adhesive + SARC group demonstrated superior push-out bond strength compared to the silane-containing SARC group and the SARC group, indicating that multi-step adhesive protocols remain advantageous for optimal bonding in intraradicular post cementation. Bond strength consistently decreased from coronal to apical sections across all cement systems, with the root canal section representing the most influential factor affecting bonding performance (η2 = 0.475). All cement systems demonstrated significant bond strength reduction following thermal cycling, emphasizing the importance of long-term durability considerations in material selection and clinical technique. Cementdentin interface failures predominated across all groups, identifying this interface as the critical weak link requiring continued research and clinical attention. The integration of silane coupling agents in SARCs (silane-containing SARC group) may offer a viable alternative to conventional approaches, providing a balance between procedural simplicity and bonding effectiveness. These findings contribute to the evidence base supporting informed clinical decision-making in fiber post-cementation and highlight the importance of meticulous techniques and appropriate material selection to improve long-term outcomes.
Author Contributions
Conceptualization—S.S.; design—S.S.; data collection—R.T., S.S. analysis/interpretation—S.S., V.I., Z.H.K.; literature research—R.T., S.S., V.I., Z.H.K.; writing manuscript—R.T., S.S., V.I., Z.H.K.; critical review—S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All procedures conducted in this research, which included human participants, were in accordance with the Helsinki Declaration, 1964. Approval for the trial was granted by the Altinbas University Clinical Research Ethics Committee (2022/09/20-146).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Patthanawijit, L.; Yanpiset, K.; Saikaew, P.; Jantarat, J. Fiber post cemented using different adhesive strategies to root canal dentin obturated with calcium silicate-based sealer. BMC Oral Health 2024, 24, 1290. [Google Scholar] [CrossRef] [PubMed]
- de Morais, D.C.; Butler, S.; Santos, M.J.M.C. Current Insights on Fiber Posts: A Narrative Review of Laboratory and Clinical Studies. Dent. J. 2023, 11, 236. [Google Scholar] [CrossRef] [PubMed]
- Mokeem, L.S.; Garcia, I.M.; Melo, M.A. Degradation and failure phenomena at the dentin bonding interface. Biomedicines 2023, 11, 1256. [Google Scholar] [CrossRef] [PubMed]
- Carrilho, E.; Cardoso, M.; Marques Ferreira, M.; Marto, C.M.; Paula, A.; Coelho, A.S. 10-MDP based dental adhesives: Adhesive interface characterization and adhesive stability-A systematic review. Materials 2019, 12, 790. [Google Scholar] [CrossRef]
- Hidari, T.; Takamizawa, T.; Imai, A.; Hirokane, E.; Ishii, R.; Tsujimoto, A.; Suzuki, T.; Miyazaki, M. Role of the functional monomer 10-methacryloyloxydecyl dihydrogen phosphate in dentin bond durability of universal adhesives in etch-&-rinse mode. Dent. Mater. J. 2020, 39, 616–623. [Google Scholar] [CrossRef]
- Baena, E.; Escribano, N.; Fuentes, V.; Reche, I.; Ceballos, L. Aging effect on push-out bond strength of six resin cements: An in vitro study. Materials 2025, 18, 1371. [Google Scholar] [CrossRef]
- Turp, V.; Sen, D.; Tuncelli, B.; Ozcan, M. Adhesion of 10-MDP containing resin cements to dentin with and without the etch-and-rinse technique. J. Adv. Prosthodont. 2013, 5, 226–233. [Google Scholar] [CrossRef]
- Jacob, S.E.; Zubair, S.M.; Thomas, M.S.; Jathanna, V.; Shenoy, R. Effect of surface treatment on the dislocation resistance of prefabricated esthetic fiber posts bonded with self-adhesive resin cement: A systematic review and meta-analysis. J. Conserv. Dent. 2021, 24, 113–123. [Google Scholar] [CrossRef]
- Dos Santos, L.R.; Lima, D.M.; Carvalho, E.M.; Rodrigues, V.P.; Alves, C.M.C. Effect of glass fiber post surface treatment on bond strength of a self-adhesive resin aement: An “in vitro” study. Int. J. Dent. 2021, 2021, 8856657. [Google Scholar]
- Santander-Rengifo, F.M.; Castillo-Andamayo, D.E.; Tay, L.Y.; López-Gurreonero, C.; Cornejo-Pinto, A.; Cervantes-Ganoza, L.A.; Cayo-Rojas, C.F. Bond strength and failure mode of Gglass fiber posts with different surface treatments prior to silanization: An in vitro comparative study. J. Int. Soc. Prev. Community Dent. 2022, 13, 42–53. [Google Scholar] [CrossRef]
- Oskoee, S.S.; Bahari, M.; Kimyai, S.; Asgary, S.; Katebi, K. Push-out bond strength of fiber posts to intraradicular dentin using multimode adhesive system. J. Endod. 2016, 42, 1794–1798. [Google Scholar] [CrossRef]
- Tang, C.; Mercelis, B.; Ahmed, M.H.; Yoshihara, K.; Peumans, M.; Van Meerbeek, B. Adhesive performance assessment of universal adhesives and universal adhesive/composite cement combinations. J. Adhes. Dent. 2023, 25, 241–256. [Google Scholar] [PubMed]
- Ñaupari-Villasante, R.; Carpio-Salvatierra, B.; Matos, T.P.; de Freitas, A.; Aliaga-Galvez, R.; Gutiérrez, M.F.; Binz-Ordonez, M.C.; Reis, A.; Loguercio, A.D. Six-year clinical evaluation of a copper-containing universal adhesive in non-carious cervical lesions: A split-mouth double-blind randomized clinical trial. J. Dent. 2025, 153, 105532. [Google Scholar] [CrossRef] [PubMed]
- de Paris Matos, T.; Perdigão, J.; de Paula, E.; Coppla, F.; Hass, V.; Scheffer, R.F.; Reis, A.; Loguercio, A.D. Five-year clinical evaluation of a universal adhesive: A randomized double-blind trial. Dent. Mater. 2020, 36, 1474–1485. [Google Scholar] [CrossRef] [PubMed]
- Oz, F.D.; Ozturk, C.; Soleimani, R.; Gurgan, S. Sixty-month follow up of three different universal adhesives used with a highly-filled flowable resin composite in the restoration of non-carious cervical lesion. Clin. Oral Investig. 2022, 26, 5377–5387. [Google Scholar] [CrossRef]
- Ñaupari-Villasante, R.; Matos, T.P.; de Albuquerque, E.G.; Warol, F.; Tardem, C.; Calazans, F.S.; Poubel, L.A.; Reis, A.; Barceleiro, M.O.; Loguercio, A.D. Five-year clinical evaluation of universal adhesive applied following different bonding techniques: A randomized multicenter clinical trial. Dent. Mater. 2023, 39, 586–594. [Google Scholar] [CrossRef]
- Breschi, L.; Mazzoni, A.; Ruggeri, A.; Cadenaro, M.; Di Lenarda, R.; De Stefano Dorigo, E. Dental adhesion review: Aging and stability of the bonded interface. Dent. Mater. 2008, 24, 90–101. [Google Scholar] [CrossRef]
- Marchesi, G.; Mazzoni, A.; Turco, G.; Cadenaro, M.; Ferrari, M.; Di Lenarda, R.; Breschi, L. Aging affects the adhesive interface of posts luted with self-adhesive cements: A 1-year study. J. Adhes. Dent. 2013, 15, 173–180. [Google Scholar]
- Şişmanoğlu, S.; Turunç-Oğuzman, R. Microshear bond strength of contemporary self-adhesive resin cements to CAD/CAM restorative materials: Effect of surface treatment and aging. J. Adhes. Sci. Tech. 2020, 34, 2484–2498. [Google Scholar] [CrossRef]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Takahashi, S.; Zhou, J.; Wurihan; Shimomura, N.; Kataoka, Y.; Watanabe, C.; Shibata, Y.; Funatsu, T.; Gao, P.; Miyazaki, T. High-resolution mechanical mapping of the adhesive-dentin interface: The effect of co-monomers in 10-methacryloyloxydecyl dihydrogen phosphate. J. Mech. Behav. Biomed. Mater. 2021, 117, 104389. [Google Scholar] [CrossRef] [PubMed]
- Shahrokhi, A.M.; Shahrokhi, A.A.; Asghari, R.; Badiee, M.; Seyedan, K. Push-out bond strength of fiber-reinforced post using various post space irrigation treatments. Int. J. Dent. 2024, 2024, 8647515. [Google Scholar] [CrossRef] [PubMed]
- Başer Can, E.D.; Barut, G.; Işık, V.; Algül, E.; Yaprak, G.; Can, E. Push-out bond strength of fiber posts to irradiated and non-irradiated intraradicular dentin. Clin. Oral Investig. 2022, 26, 7057–7069. [Google Scholar] [CrossRef] [PubMed]
- Brkanović, S.; Sever, E.K.; Vukelja, J.; Ivica, A.; Miletić, I.; Krmek, S.J. Comparison of different universal adhesive systems on dentin bond strength. Materials 2023, 16, 1530. [Google Scholar] [CrossRef]
- Ren, Z.; Wang, R.; Zhu, M. Comparative evaluation of bonding performance between universal and self-etch adhesives: In vitro study. Heliyon 2024, 10, e35226. [Google Scholar] [CrossRef]
- Hardan, L.; Bourgi, R.; Cuevas-Suárez, C.E.; Devoto, W.; Zarow, M.; Monteiro, P.; Jakubowicz, N.; Zoghbi, A.E.; Skaba, D.; Mancino, D.; et al. Effect of different application modalities on the bonding performance of adhesive systems to dentin: A systematic review and meta-analysis. Cells 2023, 12, 190. [Google Scholar] [CrossRef]
- Vidal, C.M.P.; Teixeira, E.C.; Armstrong, S.R.; Qian, F. Comparison of adhesion performance of a self-curing and a light-curing universal adhesive to various dental substrates and CAD/CAM materials. J. Adhes. Dent. 2024, 26, 31–40. [Google Scholar]
- Calheiros-Lobo, M.J.; Vieira, T.; Carbas, R.; da Silva, L.F.M.; Pinho, T. Effectiveness of self-adhesive resin luting cement in CAD-CAM blocks-A systematic review and meta-analysis. Materials 2023, 16, 2996. [Google Scholar] [CrossRef]
- Lo Giudice, G.; Cutroneo, G.; Centofanti, A.; Artemisia, A.; Bramanti, E.; Militi, A.; Rizzo, G.; Favaloro, A.; Irrera, A.; Lo Giudice, R.; et al. Dentin morphology of root canal surface: A quantitative evaluation based on a scanning electronic microscopy study. Biomed. Res. Int. 2015, 2015, 164065. [Google Scholar] [CrossRef]
- Bitter, K.; Priehn, K.; Martus, P.; Kielbassa, A.M. In vitro evaluation of push-out bond strengths of various luting agents to tooth-colored posts. J. Prosthet. Dent. 2006, 95, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Chaves, F.; de Medeiros, A.T.; Borges, B.C.D.; Mianirdi, M.C.A.J.; Catelan, A.; Aguiar, F.H.B. Influence of aging methods on push-out bond strength of adhesive systems to dentin cavities. Appl. Adhes. Sci. 2017, 5, 1. [Google Scholar] [CrossRef]
- Mazzitelli, C.; Monticelli, F.; Toledano, M.; Ferrari, M.; Osorio, R. Effect of thermal cycling on the bond strength of self-adhesive cements to fiber posts. Clin. Oral Investig. 2012, 16, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, H.; Krithikadatta, J.; Shrivastava, D.; Onazi, M.A.A.; Algarni, H.A.; Munaga, S.; Hamza, M.O.; Saad Al-Fridy, T.; Teja, K.V.; Janani, K.; et al. Systematic review fracture resistance of endodontically treated posterior teeth restored with fiber reinforced composites—A systematic review. BMC Oral Health 2023, 23, 566. [Google Scholar] [CrossRef]
- Faraoni-Romano, J.J.; Turssi, C.P.; Serra, M.C. Effect of a 10% carbamide peroxide on wear resistance of enamel and dentine: In situ study. J. Dent. 2009, 37, 273–278. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.