Abstract
Iterative decision making is deeply embedded in the design process of healthcare facilities. A significant body of literature and practices, most notably Evidence-based Design, explicitly seeks to better inform decisions as a key pathway to achieving improved outcomes. The objective of this systematic review is to explore multiple dimensions of decision making in the healthcare design literature, including interprofessional stakeholder engagement, decision flow elements, and multidisciplinary methodologies aimed at improving decision quality during healthcare facility design processes. This review offers a comprehensive review of 114 papers from the Web of Science, CINAHL, MEDLINE, and Art and Architecture Source. Decisions made during healthcare facility design processes are characterized as complex, highly interdependent, and difficult to reverse with significant implications for human and operational outcomes. The published literature emphasizes decision support generated from ex ante or ex post research. Despite numerous references to the importance of decision making, there are considerable gaps in the study of interprofessional group decision-making dynamics. The adoption and application of decision analysis tools and integrated decision flows are emerging. This review synthesizes current perspectives and methods aimed at improving decision making during the design of healthcare facilities and proposes a potential framework for future investigations of design decision quality.
1. Introduction
Globally, the vulnerabilities of healthcare facilities have been revealed to be a result of regional conflicts [], SARS-CoV-2 and other diseases [,], extreme weather [], climate change, and other challenges [,], while opportunities have arisen with rapid shifts in clinical practice and care delivery [,]. Healthcare facility quality evaluations in developed and developing countries identify multifaceted elements associated with quality, linking stakeholder satisfaction/well-being, hospital management, building maintenance, and healthcare policy with improving facility quality []. Prepared and resilient healthcare facilities are essential to the delivery of all levels of care irrespective of location []. It is in this context that the complexity and critical impact of decision making (DM) during the design of healthcare facilities are situated. Sequential and iterative decision making is deeply embedded in the design process of healthcare facilities. Healthcare facility design (HCFD) refers to activities conducted to design a new or renovated building or building space, generally undertaken in phases that may begin with establishing the project vision; determining building and room organization, shape, and capacity; developing operational and clinical systems; and continuing through a detailed design of materials, furnishings, and equipment. The complexity of designing healthcare environments emerges from the critical interdependencies between the physical environment, clinical pathways, operational efficiency, and the needs and values of healthcare teams and the patients and families who seek care. In design, decision making and decision support are most often considered in the context of option development and selection; however, there are also behavioral challenges in team decision making during design, as presented in the literature. As the environment in which a multitude of encounters and interactions occur, facilities are an integral part of a healthcare system. The physical environment influences almost every touchpoint in that system. In healthcare settings, the alignment between people, care, the environment, and outcomes is paramount to supporting quality inputs and outcomes. Healthcare facilities are more than a “backdrop” to care []; they shape workflows and influence the cognitive, emotional, and physical states of those who occupy them. Well-designed facilities are a strategic advantage, conferring competitive advantage and contributing to important health benefits and operational performance [,]. Healthcare has been described as a complex and adaptive system of systems [], and healthcare facilities are among the most complex to design []. This complexity in healthcare facility design can be attributed to the presence of multiple stakeholders; multiple, and sometimes competing, priorities; significant contingencies among care pathways and the support systems for patient care; considerable uncertainties regarding volumes and emerging clinical directions; evolving regulatory environments; and shifting strategic needs, to name some. The decisions made by design teams, over what can be years of planning, shape these environments in significant ways.
This review explores multiple dimensions of the HCFD process from early planning to detailed design, focusing on decision-making methods and associated processes. HCFD encompasses planning and decisions related to the shape, size, layout, configuration, and interior design (equipment and/or materials) as well as the associated operational aspects of a new or existing healthcare facility. These decisions are made by interprofessional teams and can be of a strategic or tactical nature, complex under uncertainty, and with long-term impacts. Facility typologies include hospital, residential, and outpatient facilities. The HCFD process is often represented as consisting of four overlapping phases that proceed in a linear nature beginning with programming and planning or pre-design and proceeding through schematic design, design development, and construction. In practice, the HCFD process is highly iterative and rarely linear. During pre-design capacity planning and programming, interprofessional project teams establish the project scope, vision, and guiding principles together with processes for stakeholder leadership, engagement, and participation. Early phases may focus on problem framing and establishing values that influence later decisions. During the early phases of design, teams decide on the types and number of key planning units or resources such as the number and size of exam rooms, inpatient hospital rooms, blood draw stations, check-in kiosks, or operating rooms. High-level building organization is most often determined in pre-design. Transitioning to the schematic design (SD) phase, key decision problems focus on spatial or layout planning. Teams design and test concepts that will determine the size, layout, and spatial organization of buildings, departments, and rooms, refining decisions conceptualized during pre-design. Key room and department adjacencies and operational flows are developed during schematic design. Stakeholder input typically expands in schematic design to include interprofessional, front-line team members and, at times, patients and family members. In SD, option generation, ranking, and analysis often dominate decision making. In design development (DD), material choices, such as those for flooring types, wall coverings, and furniture, and equipment decisions, such as those regarding ventilation or mobile documentation computers, are made. During DD, selection-type decision problems are often prominent, as are those regarding room organization. Equipment and supply placement, wayfinding, and people and material flows are additional decision contexts or problems that intersect with those previously mentioned. For this review, the focus is limited to the pre-design to design development phases. Figure 1 shows a simplified HCFD process with example key decisions in each phase.
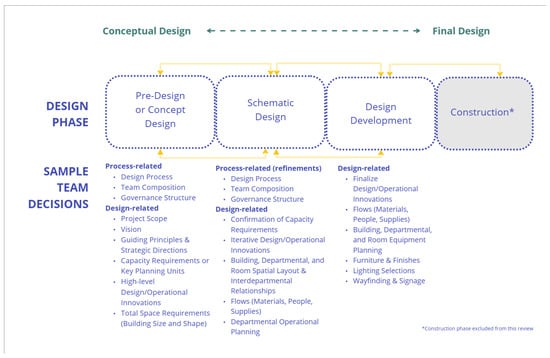
Figure 1.
Simplified HCFD process with example decisions.
A considerable amount of design research has established strong correlations between healthcare environments and important outcomes related to patient and staff safety, well-being, comfort, stress levels, recovery times, and timeliness of care. This is true of many different healthcare spaces such as surgical suites, emergency departments, and inpatient rooms, as well as clinical workspaces, family amenity spaces, exam rooms, consultation rooms, and many other specialized settings. Decisions that guide the design of healthcare facilities are rarely trivial, and they have been likened to medical interventions whose facilitators carry a moral obligation to bring a rigorous approach to decision making []. It has been acknowledged that complexity in decision making is present during architectural design projects of all sizes and scopes [,,]. As such, informed decision making has become an increasingly critical cornerstone of healthcare design practice. A significant body of HCFD literature and practices, most notably Evidence-based Design (EBD), has the stated objective of contributing to more informed decisions as a key pathway to achieving improved outcomes. Conventional decision making in architectural design has been described as a process that focuses more on compositional elements than on multi-criteria approaches to structuring and making decisions []. Simon and Hu [] characterize the traditional design approach as deterministic problem solving, a loosely structured, open-ended activity that includes problem definition, representation, performance evaluation, and decision making. Many factors intervene that prompt rework or reversals [] along the way. Some examples include changing strategic priorities, significant changes in leadership or project team membership, and financial or budgetary concerns. Decisions regarding the designed attributes of healthcare environments or facilities are made, solutions generated, options compared, and decisions made again in a highly dynamic, interdependent system with a diversity of interprofessional stakeholders [,].
The practice of EBD emerged over 20 years ago as an effort to demonstrate the importance of design for health outcomes and to support design decision making with credible research. EBD acknowledges the complexity of healthcare design, the need for improving design outcomes, and the important role of decision making. In the past 10 years, novel tools, frameworks, and concepts from the disciplines of systems science, systems engineering, operations research, and management sciences have been introduced into healthcare facility design. Discrete event simulation (DES) and Lean methods, in particular, have become accepted, validated methods for guiding healthcare design practice and research []. Such tools and processes, together with reliable evidence, have been proposed to address over-reliance on heuristics, anecdotal information [,] or best practices []. It has been noted that healthcare management teams have adopted decision analysis and decision science methodologies as the industry has become increasingly complex and the focus on efficient use of resources has grown [], but this is not necessarily true for HCFD. Much research has been devoted to seeking and enhancing evidence-based decision support, including the introduction of more rigorous ex ante or ex post methods for creating, testing, and choosing design options. This is well captured in the statement “With the availability of scientific evidence, decision-making processes about facility design and operation can be transformed from an intuitive process to an evidence-informed and analytical one” ([], p 44). This prompts further exploration; that is, what else, in addition to evidence and analytics, might drive better decisions or improve decision quality?
Designing facilities has been described as a process of “multiple explorations, discussions, evaluations, and decision making” ([], p. 44). Authors have pointed out the limited applications of decision-making strategies [] and decision-making models [] in design practice and hinted at the potential benefits. It has been proposed that the integration of ex ante techniques from other industries and disciplines that allow for a systematic assessment of complex and interdependent design decisions and iteration/optimization during design [,] offers the opportunity to improve decision making. Structured decision analysis tools and concepts such as Multi-criteria Decision Making (MCDM), decision quality, and value-based decision making are relatively less known in the healthcare design literature, with the exception of applications in healthcare facility location problems [] and limited applications in layout planning. As Kim and Augenbrow ([], p. 306) note, “Quantitative decision analysis methodology… needs to be more integrated than ‘spreadsheets’.”
Artificial intelligence (AI)-based methods have been identified as emerging techniques in healthcare design for generating healthcare design options more quickly while accounting for multiple variables, and they are expected to grow in the future []. In 2024, The American College of Healthcare Architects launched a think tank to explore how AI (machine learning, deep learning, large language models, and generative AI) will shape and influence health design and planning, as well as healthcare itself []. Their report highlights AI as a support for learning and decision making, as well as a driver of changes to healthcare pathways and service models that will influence design, while also highlighting concerns regarding transparency in algorithmic decision making []. While not specific to the built environment, others point to the ethical challenges of AI as it relates to stakeholder, and particularly patient, health co-design opportunities [] or call for human-centered design to address bias in AI-enabled design [].
While considerable importance is given to supporting good decisions in HCFD (at least as an ideal), integrated or holistic frameworks for understanding decision-making processes, governance, group composition, methodologies, and what constitutes decision quality have not been well researched or developed. The dynamics of interprofessional clinical decision making have been studied in healthcare settings [,] and in specialized environments such as intensive care units [], as well as in the construction industry []. Empirical studies of the governance structures of HCFD interprofessional design teams, how stakeholder values are established, their decision flows, the modes of decision making adopted, stakeholder satisfaction with the decision process, and other behavioral decision-making considerations are limited. Decision making is rarely considered from a holistic or systems perspective. Structured decision making, decision analysis, behavioral decision-making concepts, and decision science have made limited in-roads into the HCFD process. This systematic review addresses these gaps in three ways: first by exploring decision-making concepts, methodologies, and flow elements applied to HCFD DM; second, by identifying existing methodologies and frameworks applied to improve decision quality in HCFD; and finally, by providing a synthesis of the current literature related to interprofessional healthcare design team decision-making processes. A potential framework for future empirical investigations of design decision making with respect to decision quality is proposed.
1.1. Decision Analysis, Behavioral Decision Making, and Related Areas of Inquiry
Structured decision analysis (DA) can be conceptualized as both a paradigm and a set of tools that allow decision makers to build of a model of a decision as a basis for understanding and guiding a process that includes the framing of the decision to be made, stakeholder performance criteria, generating and innovating on options, and analyzing options against criteria [,]. DA can be considered as a discipline and area of inquiry falling under the umbrella of operations research/operations management (OR/OM). OR/OM has itself been described as an approach to problem solving and decision making. It has wide existing and potential applications, including HCFD, and utilizes mathematical and computation modeling, optimization techniques, and statistical methods. DA was first developed by Ron Howard and Howard Raiffa in the 1960s, with contributions from Ralph Keeney and others. This approach was introduced to apply the principles of decision theory directly to practice and to incorporate measures of probability into decision making. DA is intended to help people “think hard and systematically about some important real problems” ([], p. vii). It seeks to integrate and structure scientific, quantifiable insights and subjective and experiential insights in a process that contributes to better decisions and thereby improves the probability of better outcomes. Two aspects are worth noting. First, DA does not assume that group decision making is fully based on objective findings (if such a thing exists) such as those emerging from an experimental simulation model or cost model. Second, DA posits that it is a logical fallacy to judge the quality of a decision based on the outcome, sometimes called “resulting”. Many factors influence outcomes such as factors unknown at the time of the decision or the occurrence of improbable events. Outcomes are distinct from process, that is, the quality of the decision inputs and decision taken. In Making Hard Decisions, Clemen notes, “although decision analysis cannot improve your luck, it can help you understand better the problems you face and thus make better decisions” ([], p. 3). Other fields of empirical and practice-based research have made important contributions to DA and its evolution in practice. The importance of values in decision making emerged from the research of Ralph Keeney. Keeney emphasized the importance of the clear articulation of decision makers’ values and value-focused decision making, particularly as it relates to the generation of innovative and hidden alternatives []. The role of individual and group decision making can be found in the domain of behavioral decision science research and Behavioral Operational Research (BOR). BOR acknowledges the importance of supporting the teams involved in these problems/decision/methods and is based on the premise that behavior and cognition, biases, and external forces influence people and influence process, and success relies on both people and process []. Pioneered by the research of Tversky, Kahneman, and others, the field of behavioral decision making or judgment and decision making accounts for the role of prior experience, biases, and insensitivity to sample size, predictability, and the prior probability of outcomes in decision making that contribute to errors []. Later works by these authors explored the determinants of choice and how the framing of a decision influences preferences []. Yet another strand of research related to how people make decisions emerges from human factors. Naturalistic Decision Making (NDM) seeks to gain insight into how people make decisions in practice, given the constraints they face in their decision context and environment. NDM is considered divergent from utility-based or more analytical approaches to DM. Naturalistic and laboratory approaches to understanding human decision making have been identified as complementary, with the former providing greater validity and the latter incorporating the controls needed to establish causality []. A recent development in the behavioral arena is Cognitive Engineering and DM (CEDM) which integrates different threads of decision-making theory, research, and practice to reconcile the disconnect often seen between behavior and objective analysis in decision making and considers the system in which groups make decisions []. This is a large body of work of which only a small portion has been described here. While gaps exist in behavioral DM research in the context of design, theory and methods relating to choice architecture, nudging, decision bias and advocacy, framing, decision-making styles, and other behavioral insights may hold relevance to understanding, and improving, how interprofessional healthcare design teams can engage in quality decision-making flows.
1.2. What Defines the Quality of a Decision?
Decision quality concepts can be found in diverse domains such as pharmaceuticals, land management, and medical decision making. One such framework is the Decision Quality Chain (DQC), first proposed by Matheson [] and elaborated by Spetzler, Winter, and Meyer []. The DQC was built on the foundations of decision theory and decision analysis and expanded to incorporate research related to behavioral decision science research emerging in the mid-2010s. The DQC model describes six distinct dimensions of decision making, conceptualized as an interlinked chain, each of which are critical to achieving quality decisions. These six dimensions of decision quality are “a Helpful Frame, Clear Values, Creative Alternatives, Useful Information, Sound Reasoning, and Commitment to Action” ([], p. 12). The developers of the DQC argue that without structured approaches, bias impedes quality decisions. Groups tend to rely on “advocacy” whereby people champion options rather than considering the options in relation to each other. Without a guiding framework, uncertainty is not accounted for, evidence to the contrary of beliefs is ignored, and important decisions are made quickly with impatience. The DQC has since been revised to integrate, as described by David Matheson, “the head and the heart” of decision making []. In this way, both the decision makers and the methods of DA are considered. For example, framing is extended to include perspectives and the role of meaning in the decision context. Decision quality has also been defined in terms of multiple criteria related to both decision outcomes and decision processes, including the consideration of decision support, evidence, and the level of consensus []. It is also noted that decision quality is a challenging concept as the success of outcomes is difficult for decision makers to separate from the quality of the decision []. In the design literature, references to certain dimensions of decision flows and the DQC can be found, although the framework of understanding does not refer to decision quality per se. At least one paper has defined the concept of design quality in terms of requiring a considerable understanding of stakeholder values and needs []. Another discusses methods to assess quality in design process []. Decision-related challenges in the HCFD literature and practice are mostly framed in terms of poor or unintended outcomes, the presence of complexity and considerable interdependence in design, a lack of relevant or reliable information, the presence of stakeholder biases, rework due to poor decisions, dissatisfaction with the process, and missing or underutilized stakeholders.
1.3. Objectives of This Review
The objective of this review is to synthesize how decision making has been characterized in the HCFD literature, what is known about healthcare design team decision-making-related dynamics, and the methodologies and tools that have been applied to improve decision making. To this end, this review includes the following areas of exploration:
- Identify trends and areas of focus with respect to HCFD DM, including the types of decision problems that arise during design and the methods and approaches that have been proposed to improve decision quality.
- Examine how HCFD decision-making processes are described and what challenges and approaches have been discussed, including group processes and dynamics as well as decision-making tools and methodologies.
- Identify knowledge gaps with respect to group decision-making processes and interprofessional dynamics.
- Identify opportunities for future research related to a better understanding of decision flows and improved decision quality.
2. Methods
This review follows the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline for reporting systematic reviews. Accordingly, the search strategy comprised the following steps: the establishment of objectives for this review; the development of keyword search terms; and literature identification through a database search, screening, and review. Figure 2 provides an overview of the identification, screening, and inclusion/exclusion method applied.
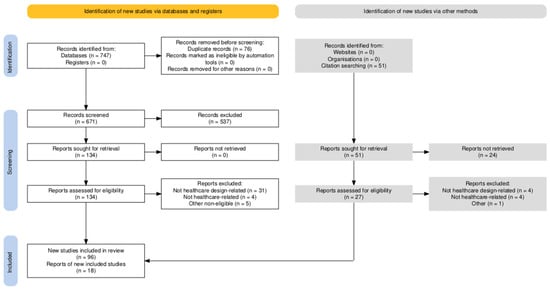
Figure 2.
PRISMA search flow diagram [].
2.1. Identification
A broad search strategy was employed to capture the decision contexts; key decision types; and the decision support tools, processes, and systems applied during the planning, schematic design, and design development phases of healthcare facility design. No generative AI or natural language processing methods were applied by the authors during screening or synthesis.
A keyword search was undertaken using four databases: Web of Science, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medical Literature Analysis and Retrieval System (MEDLINE), and Art and Architecture Source. These were chosen due to the multi- and interdisciplinary nature of HCFD, which draws on the disciplines of healthcare and medicine, architecture/design, systems engineering, environmental psychology, human factors/ergonomics, and healthcare management science, among others. The search encompassed peer-reviewed articles and reports published between January of 2013 and February 2024 using the following sample search keywords:
- ((ALL = (“healthcare design”)) OR ALL = (“healthcare design”)) AND ALL = (“decision”).
- ((ALL = (“facility design”)) OR ALL = (“healthcare”)) AND ALL = (“decision”).
- ((ALL = (“healthcare”)) OR ALL = (“facility design”)) AND ALL = (“design process”).
The initial search yielded a total of 747 articles for all databases, and after removing duplicates, 671 unique articles remained. During the full-text eligibility screening process, a manual bibliographic review was conducted and resulted in the identification of 51 additional articles. After removing duplicates, together, these sources resulted in a total of 717 articles available for screening.
2.2. Screening and Inclusion
Unique articles were initially screened according to the following exclusion and eligibility criteria:
- Exclusion Criteria:
- Conference papers to limit scope to peer-reviewed journals.
- No specific references to HCFD decision making or process.
- Papers focused on facility location problems.
- Non-English-language articles.
- Eligibility Criteria:
- Published between 1 January 2013 and 15 February 2024.
- English-language articles.
- Related to healthcare facility planning and/or design, defined as activities related to the shape, sizing, layout, or configuration and interior design (equipment and/or materials) and associated operational aspects of a new or existing healthcare facility, including hospital, residential, and outpatient facilities.
- Containing specific references to decision making or decision support.
Following the initial screening, 185 articles were retrieved, and the full text was reviewed in detail. Additional articles were excluded if they did not focus on HCFD, did not reference decision making directly or indirectly, or met the other exclusion criteria noted above. Of the 161 articles retrieved and fully screened, 114 papers were deemed relevant and included in this review. Screening was conducted by the first author, and no automation tools were utilized.
2.3. Coding and Thematic Analysis
Articles were coded in MS Excel according to the area(s) of focus (method or stakeholder-focused), relevant design phase, decision problem type, healthcare setting, decision flow element, and methods applied. The healthcare setting and decision context categories are based on the Facility Guidelines Institute categories for healthcare settings, which serve as the most widely applied design guidelines and requirements for HCFD in the US. [,]. Area of focus categories were developed during the detailed review and were refined and collapsed over the reading and synthesis process. The literature was categorized into two broad categories: decision support or evidence and decision-making process. The literature was also mapped according to the elements of decision flows as described by Clemen [] and the DQC as formulated by Spetzler et al. []. The decision support tools, methods, and frameworks proposed or discussed in each article were likewise identified in the context of specific HCFD decision problems or contexts. A conceptual map of the literature can be seen in Figure 3.
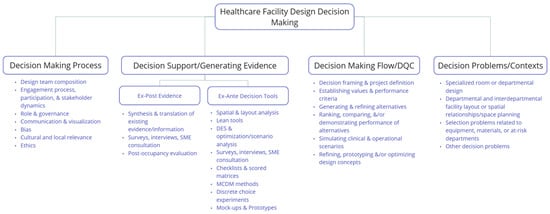
Figure 3.
HCFD decision-making literature concept map.
3. Results
3.1. Trends
Across the period of January 2013 through February 2024, the number of identified papers with a focus on HCFD decision making steadily grew from 2013 to 2021, doubling from 2019 and 2020 and then dropping off after 2021. The reason for this trend is not evident. The identified articles appear in a total of 57 unique journals, representing a wide range of journals from single and multidisciplinary domains. Approximately one-third of articles (38 of the 114 articles) were published in Health Environments Research and Development (HERD), which is the primary peer-reviewed publication for research focused on the HCFD field. Overall, 57% of articles appear in journals specific to architecture, architectural engineering, design research, or facility design; 14% published in nursing, healthcare, and medicine journals; 7% in healthcare management science; and the remaining in systems engineering, informatics, human factors, sustainability, and other discipline-focused journals. This diversity provides evidence of the multidisciplinary nature of the HCFD process. No articles identified in this search appeared in journals focused on decision analysis or decision science. A 2022 systematic review of health decision analysis trends and emerging topics did not identify literature related to healthcare facilities or design [].
For included papers which have a country-level focus, there is a high representation of the HCFD experiences in North America (35) and Western Europe (21), followed by East Asia and Pacific (17) and Latin America and the Caribbean (12). Many fewer studies focused on HCFD in the Middle East and North Africa (5), Eastern Europe and Central Asia (3), and South Asia (2), and none were within Sub-Saharan Africa. Within these regional categories, 30 countries are represented, the 3 most frequent countries being the USA (35), Canada (9), and China (7). A total of 12 papers include reviews or articles with multi-country representation, while 11 did not specify any country focus. Table A1, Table A2 and Table A3 in Appendix A list the country of focus or author for studies focused on the most frequent decision problems.
The literature considering decision making during HCFD was broadly categorized into two primary areas of focus: decision support, encompassing decision analysis and evidence for decision making, and decision process, with an emphasis on stakeholder dynamics and the design process. Decision analysis tools include methods such as MCDM techniques, DES, or the Delphi technique. The role of high-quality evidence in improving decisions (and, by extension, outcomes) is prominent in the HCFD literature, which includes studies that establish causal and correlational relationships between design elements and outcomes of interest. Included under the category of evidence are papers focused on synthesizing and communicating evidence to stakeholders and ex ante and post-occupancy and other ex post design research. Over the period of 2013 to 2024, the number of papers applying decision support tools and methods grew faster than that of papers applying evidence alone. The number of papers specifically mentioning decision making peaked in 2020 and 2021. This increase in the application of decision support tools may be due to the increase in the application of systems engineering, Lean, and management science techniques to healthcare design []. The proportion of articles only focused on decision process, that is, assessing the role of the composition of design teams, interdisciplinary group work, and integrated decision support frameworks, is smaller compared to that of decision support, but these articles have received some attention.
A slight upward trend in papers considering multiple aspects of decision making, rather than an exclusive focus on evidence, tools, or process, is observed in this set of papers over time. Figure 4 provides a breakdown of the literature by the area of focus over the entire period.
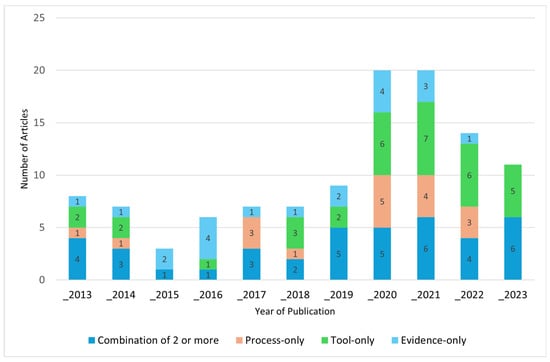
Figure 4.
Trends in area of focus by year of publication, 2013–2023 (n = 112; 2024 excluded due to partial year).
3.2. Decisions and Decision Making in HCFD
Decisions made during HCFD are characterized in the literature as complex, highly interdependent, uncertain, costly, difficult to reverse, dynamic, iterative, and critical for important human and operational outcomes. The importance of decisions related to attributes of a new or renovated healthcare facility is widely acknowledged in the papers included in this review. Design decisions are linked to the quality of the outcomes, alignment between design and operational objectives, cost, facility maintenance, and stakeholder buy-in as relates to design innovation linked to changes in clinical or operational pathways, as well as carrying ethical responsibilities [,]. As noted by Kailin and Oakland ([], p. 15), “the design of a health care facility fundamentally affects all aspects of care”. One factor behind this acknowledgement is the substantial body of literature that has demonstrated the associations between the built environment and significant human and organizational outcomes. Some argue, however, that these effects are often underestimated by healthcare leadership [,], with considerable implications for design decisions and outcomes. Design decisions, it is argued, require a focus on user-centered, measurable outcomes and emerging evidence, a focus often lacking in projects []. There are other factors at play here as well. Investments in new facilities involve considerable financial and reputational costs [], many of which are irreversible or, at a minimum, challenging to reverse []. Questions of permanence or reversibility are relevant, for example, for decisions related to furniture versus room size or number []. Given the long timelines associated with building projects (seven years on average), early decisions have important downstream effects [,]. Teams are also subject to turnover in leadership, which has been associated with rework, changes in vision or design strategies, delays, and increased cost []. The volume of decisions is great, and decisions present themselves in a continuous stream []. Unintended or negative outcomes have been attributed to a lack of sufficient attention to early project stage framing and analysis []. Decisions made during the pre-design phase, where performance and functional criteria are established and translated into design concepts, greatly influence options and the analysis of the options [,]. Early design is often conceptual and initiates conversations among key stakeholders regarding requirements, vision, and innovation []. As conceptual and schematic design proceed, the continuing influence of early decisions and the relative flexibility of alternatives [,] can circumscribe alternatives and decision options. Safety and costs are among the important outcomes [] that are tied to early decisions. Cost [,] and post-occupancy maintenance implications [,,] are attributed to a lack of systematic decision making. Decision reversals or changes made later in the design process have considerable financial and schedule-related costs associated with them, and even the effects of these may not be evident until years later []. Some of these reversals are due to new information, others to changes in team composition or leadership []. The complex regulatory and competitive landscape, fast-evolving clinical practices [], shifting patient demographics and preferences [,], increasing demand for performance-based environments, and long timelines all contribute to considerable uncertainty [].
This appreciation for the complexity and interdependencies inherent in the delivery of healthcare and, by extension, the design of healthcare facilities is a common theme in the literature [,,,,,,,,,,,,,,,,,,,]. Authors posit that the presence of complexity of care in a healthcare facility contributes to complexity in decision making, thereby requiring more systematic and advanced analytical methods [,]. The presence of uncertainty, subjectivity [], and difficult-to-resolve trade-offs [,] are features of complexity that can constitute considerable challenges to effective and quality decision making. The physical spaces (departments, rooms, etc.) and flow elements (layout and patient care pathways) within a healthcare facility are highly interdependent []. Thus healthcare facilities are characterized as complex systems []. This interconnectedness between the physical environment and work design, particularly in the context of transformative facility projects, contributes to complexity [,]. Health systems are also characterized by the presence of non-linear relationships, constraints on adaptability, and dependence on earlier states []. During design, the iterative process that flows from the identification of functional needs to concept ideation, cost evaluation, performance testing against performance metrics, feedback loops, and re-design adds to complexity []. Moreover, design teams and decisions involve diverse, interprofessional stakeholders with different, often competing, needs and preferences [,]. It is noted that this complexity is not sufficiently addressed by existing methods, particularly with reference to accounting trade-offs [].
3.3. Decision Making in the Context of HCFD Frameworks
As noted, the conventional conceptualization of the HCFD process is linear and iterative—beginning with pre-design programming and proceeding through concept design, schematic design (SD), design development (DD), construction, and occupancy—however iterative loops are common. While key decisions often signal the subsequent phase of design, decisions are often revisited and revised over the course of the project. Phases are often distinguished by the project schedule and typically end with a design document which is agreed upon. These documents become more detailed and much more costly to change as design progresses.
Among the most common processes or frameworks that guide design (or portions of design) over these phases are EBD-based, Lean-led design (or process-led design), and participatory design. The boundaries of these frameworks are quite fluid, and many of the same approaches and methods are applied among them. The tools, methods, and philosophies of human factors, systems engineering, MCDM, OR, design thinking, and healthcare management science are likewise interwoven among them. Whatever conceptual umbrella one is standing under, the emphasis on decision support and the challenges associated with quality decision making emerges time and again in the literature. Conventional, cross-disciplinary, and hybrid methods emerging from the disciplines of decision analysis, EBD, MCDM, architectural systems, systems engineering, and human factors are proposed by multiple authors as a means to improve design decision-making flow.
EBD advocates a continuous, informed approach to design decisions, defined as a “deliberate attempt to base building decisions on the best available research” []. EBD has been referred to as “a decision-making tool during design” ([], p. 18). While EBD is an integrated process that is inclusive of a broad engagement process with stakeholders and decision makers [], building a knowledge base or generating evidence linking design attributes to outcomes [] is its most common application. EBD incorporates a range of interdisciplinary ex post and ex ante methods in support of decisions. In EBD, and HCFD more broadly, evidence is often an umbrella term for decision-making inputs. Evidence can take the form of experimental or quasi-experimental and mixed methods ex post design or post-occupancy research studies [] and best practices or benchmarking, expert-driven inputs, and/or ex ante-generated evidence/insights derived from modeling, prototyping, stakeholder preference elicitation, and other computational or participatory methodologies. Under this large and expanding umbrella fall diverse permutations of processes and tools that are explicitly referred to as EBD-based approaches, including the emergence of newer methods such as DES, design thinking, MCDM, and systems thinking. Conventional design research mixed methods approaches that apply literature reviews, the Delphi process, subject matter expert consultation, surveys, experimental and quasi-experimental studies, case studies, and post-occupancy evaluation also fall under the EBD umbrella.
Lean-led design is described as a process that is inclusive of stakeholders and, in particular, of the end-users of facilities in development [] with an emphasis on inputs that include building trust and shared decision making. Lean design has also been defined as a “systematic approach” to designing healthcare facilities that leads with understanding process as well as user-defined needs and performance expectations ([], p 18). Depending on the organization, this can be a departure from more conventional architectural design in that end-users take an active role in project definition and problem framing, along with a focus on understanding and explicitly mapping existing processes. Lean-led design adapts the Lean participatory ethos together with Lean tools and methods from manufacturing settings. Some features of the Lean approach include engaging with multidisciplinary stakeholders; establishing clear and measurable design criteria; Kaizen collaborative planning, concept development, and evaluation; ranking options using matrices; establishing a “big room” or dedicated space to meet and share progress visually; and using retrospective and prospective techniques to assess progress and changes. An additional contribution of Lean is a renewed emphasis on the relationships between flows, operational efficiencies, satisfaction, and design. While EBD and conventional HCFD have incorporated concepts of flows (and continue to integrate Lean methodologies), Lean concepts have been a driver behind process-led approaches to design, which has also driven movement towards more multidisciplinary and interprofessional user groups.
The Participatory Design Process (PDP) emerged as an alternative to so-called expert-driven planning and shares engagement and collaboration with stakeholders with Lean and EBD as an imperative. Here, process is an important input, including governance structures and group composition. PDP and other co-design approaches have been identified as having their roots in the work of Arnstein’s foundational work on hierarchies of participation [] and make a distinction between the role of the stakeholder as a source of information and the stakeholder as a full partner []. While there is a considerable overlap and cross-fertilization of ideas among these frameworks or approaches, EBD, in practice at least, is primarily concerned with how evidence is generated, how it influences concept development, and how it is used in evaluation, whereas the PDP is more fully focused on creating a process whereby participation is engendered, co-design emerges, and decision-making modes are made more transparent.
3.4. Decision Flows and Decision Quality in HCFD
Within the disciplines of decision theory and decision analysis, structured decision analysis flow is described as a multi-step, iterative process that includes identifying the decision problem or frame; establishing stakeholder values and objectives as well as trade-offs and constraints; modeling the problem, uncertainties, and preferences and measuring the consequences of options or alternatives (often in probabilities); choosing an option; performing a sensitivity analysis; and undertaking an additional analysis if needed before moving to implementation []. In the HCFD literature, aspects of DM flow have been explored in part but rarely in a holistic or connected manner. In the design process, the terms project definition and scope, rather than decision framing, are often used to describe the problem or opportunity that initiates DM flow. Schönbeck et al. ([], p. 5) explicitly reference defining the decision problem as the “first step in decision-making analyses.” Chbaly & Brunet [] draw attention to the importance of structured frameworks for early project definition and scope (i.e., what problems are we solving) through the application of Lean-led approaches that define functional needs over budget and code requirements.
Figure 5 illustrates the set and intersection sizes for 114 papers categorized according to the six DQC [] dimensions using an Upset Plot []. This figure illustrates the absence of the consideration of integrated decision flow elements within the literature. The greatest number of papers are categorized as concerned with generating/utilizing useful information (set size of 54), reflecting the widespread practice of EBD. Information in HCFD decision making is most often conceived of as evidence—usually in the form of a systematic literature review, design research conducted post-occupancy or as pre/post-comparisons in similar environments, or ex ante research to test design performance. Guidelines or standards are extrapolated from ex post research as well as from expert or stakeholder input, taking the form of checklists against which options are compared. The ability of diverse stakeholders to effectively apply research findings from other settings into their unique environment during HCFD has been challenging [,]. Methods for enhancing the quality, integration, and translation of evidence to inform the adoption of existing designs or the generation of new design alternatives are widely emphasized [,,,,,,,,,].
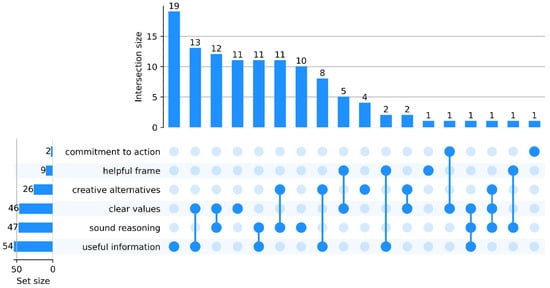
Figure 5.
Upset Plot illustrating Decision Quality Chain [] dimension set and intersection sizes.
Establishing clear values is also commonly addressed (set size of 46). Defining values in HCFD DM often takes the form of establishing project-wide guiding principles and measures of success that are synthesized and agreed upon in consultative processes with differing levels of participation and decision-making modes. Guiding principles are referred to as “benchmarks of guidance in consistent decision making” ([], p. 7).Values and trade-offs may be described as “design imperatives” or open goals that can be used to generate creative options ([], p. 379). Some argue that needs are often elicited in a rushed manner and compiled together with regulatory and other requirements, thereby effectively losing the voice of the client, leading to rework and miscommunication []. In this way, a lack of clear objectives impedes both the generation of creative solutions and their ranking or comparison []. Several authors propose methods to identify and/or prioritize stakeholder values and objectives/performance criteria to guide option development and the comparison of options [,,,,,] and to determine therapeutic design goals [,].
Generating high-performing, innovative alternative design concepts while accounting for multiple criteria and functional needs emerged as an important theme. In this review, at least four means of generating new design options emerged: (1) borrowing or innovating concepts emerging from design research in similar environments (usually conducted post-occupancy or as pre/post-comparisons) which are generated by architectural teams and refined over time; (2) ex ante studies conducted during the design process such as DES, which, while not generative per se, do result in the generation of new or refined alternatives; (3) the prototyping of mock-up design concepts which, in turn, generate new ideas and concepts; and (4) computationally generated design alternatives. The use of genetic programming was noted in one paper []. Alfredson Larsen et al. [] discuss the importance of openness and flexibility in concept generation in the context of a study of front-end planning for a new hospital, noting the challenges associated with path dependency, avoiding concepts that are not simply variations on a theme but, in fact, creative alternatives to a decision problem which the authors link back to clear objectives and values. The authors further note that “early lock-in” on preferred concepts hinders creative solutions []. The predominant approach to generating alternative designs is often extrapolating from research and/or stakeholder input to provide best practices and choosing or adapting designed environment attributes that have been demonstrated to be strongly associated with specific outcomes of interest. Alfonsi et al. ([], p. 137) call this process of research informing new designs as a “virtuous cycle” leading to improved decisions based on knowledge.
The number of studies focused on the sound reasoning and analysis of options was relatively high as well (set size of 47). In HCFD, it might be more accurate to consider this element of decision flow as optimization, gaining insights, or perhaps prototyping. A considerable proportion of the HCFD literature identified in this review is concerned with analyzing alternative design options through systematic, data-driven, and objective methods. Exploring or proposing mock-up and physical simulations to more effectively visualize, prototype, and communicate the performance of design options under consideration with multiple stakeholder groups is identified by multiple authors as a beneficial approach to assessing performance and refining design concepts. Without effective visualization, either physical or virtual, decision making can be particularly challenging for non-designers [,]. Physical mock-up simulations, both low and high fidelity, address a challenge in design decisions that may not emerge as important in strategic or other realms of decision making, that is, providing direct experience with, and invitation to alter, decision alternatives. Virtual mock-ups provide more flexibility to evaluate multiple options and variations of design compared to physical mock-ups, but they may be more time-consuming and costly []. Augmented reality may also decrease the time required in evaluating options as compared to physical mock-ups []. Related stakeholder-engaged approaches includes Simulation-based Clinical Systems Testing (SbCST) [], which involves a facilitated workflow simulation, and Summarize, Anchor, Facilitate, Explore, Elicit (SAFEE), which is a useability test that allows stakeholders to interact with design options and provide feedback in the form of direct communication and alignment to work as done []. Mock-ups can help avoid costly rework post-construction or late in design [] and increase confidence in team decisions.
In terms of intersecting dimensions, the most common intersections are useful information with clear values (13 papers) and clear values with sound reasoning (12 papers), reflecting the importance of stakeholder engagement in design and possibly the growing influence of Lean and systems engineering methods in design. The intersection of useful information with sound reasoning or sound reasoning with creative alternatives was present in 22 papers. Seeking or creating new information, generating alternatives, comparing, and optimizing alternatives are often intersecting activities during design. This overlap may be attributed to the fact that design follows an iterative, looping path whereby alternatives are generated, evaluated, and refined or optimized in a non-linear fashion. Just two papers incorporate more than two decision quality elements. Commitment to action receives limited attention in this HCFD literature set reporting that Lean-led approaches contribute to new design innovation adoption [], noting that structures and inclusive group analyses of options lead to innovation [], and reporting that stakeholders who are more engaged in decision-making processes adapt quicker to, and experience greater satisfaction with new facilities [].
3.5. Stakeholder Roles and Participation in HCFD Decision Making and Design Process
There are many stakeholders engaged in the design of a healthcare facility, and they participate in various ways and bring perspectives from their training, discipline, and job role(s). Interprofessional design teams might consist of the architectural and engineering team; front-line and administrative or managerial staff from facilities, operations, security, admitting, clinical, finance and strategic, or environmental services; and patient experience departments. The teams are diverse and typically change over time, and they can include physicians from multiple specialties, nurses at all levels and specialties, respiratory therapists, physical therapists, pharmacists, supply chain managers, radiologists, patient advocates, patients, families, and community members, among others. There are ample references to the existence of multiple stakeholders and the interplay between design teams and structured or unstructured decision-making processes. The involvement of many different stakeholders in a healthcare design project is acknowledged, and authors have discussed the utility of MCDM to provide a “platform” for the plurality of stakeholder views and needs []. Trudel et al. [] highlight the need to improve focus and consensus-building among teams. With respect to the role and participation of stakeholders in the design process and decision making, team composition, collaboration, shared decision making, team roles, levels of participation, transparency, bias, subjectivity, and governance have been explored across EBD-, Lean-, and PDP-focused papers.
The roles of subjectivity, bias, the presence of objective evidence, and team dynamics are also noted as considerable challenges to effective decision making during facility design processes. The need for access to more rigorous evidence and methods to support design decision making and the translation of that evidence into practical options are commonly described as a response to subjective or biased decision making. The pitfalls associated with decisions made based on past experience, so-called “gut instincts”, or best practice, rather than systematic evaluation, are described by others as a contributor to sub-optimal choices [,]. One survey of design team stakeholders involved in an EBD process described decision making as “80% function and 20% culture”, whereby the difficult task of synthesizing evidence together with team dynamics led to lower-quality decisions ([], p. 7). Examples of these dynamics can be seen in influential team members who resist or support certain design features based on their own biases [], political machinations [], competitive rather than collaborative work [], or the inclusion of key stakeholders late in the process [,,]. In one study, however, it was reported that resistance to more evidence-based or systematic analysis was found to be due in part to the corresponding lower value placed on experience and knowledge gained from practice [].
In the literature with a PDP focus, facility design is described as a “social and situated practice” ([], p. 99) that relies on thoughtful team composition and attention to team dynamics. Some have argued that the uniqueness of design context elevates the importance of stakeholder participation []. One author attributes this lack of focus on the roles of patients, staff, visitors, and other end-users of healthcare facilities in decision making to concerns by leadership regarding time and resource requirements, as well as uncertainty related to the benefits of alternative approaches to decision making []. Because design teams are by nature interprofessional, it is noted that multiple forms and methods are needed to develop a shared language and understanding of disciplinary differences []. There is general agreement that a collaborative decision style can bring different perspectives and a wider breadth of expert knowledge, which allows for co-ownership and adds value to the process [,]. Shared collaborative decision making during the planning and design phases of healthcare environments between representatives from healthcare, the construction sector, and architecture based on evidence and the perspectives of end-users has been noted as a critical factor to success []. The question of trust, or the lack thereof, between design teams and stakeholders is raised [], which uncovers a lack of mutual understanding and processes for evaluation or making decisions. Multidisciplinary and consensus-based guideline development has been a mainstay for code development, such as that issued by the Facility Guidelines Institute []. During the design process, however, the level of involvement and the structure of collaboration are still under debate. Perkins et al. ([], p. 380) note, “… People will be more involved in and satisfied with their workplace and care environment if they understand the reasons for, and consequences of, design decisions”. One study of Lean-led design user groups concludes that too much involvement and siloed discussions could have an adverse effect on success []. A follow-on study by the same author [] notes that the development of a collective identity for the stakeholder team facilitated cross-departmental and cross-functional understanding and supported consensus-building around decision options. Other authors echo the importance of awareness among stakeholders of the impact of decisions on diverse constituents []. The complexity of the facility project may also play a role, with the need for communication and interaction to clarify needs and perspectives increasing with the complexity of the facility []. The greater time commitment required for wider and more participatory decision making is also acknowledged []. Riejula et al. [] acknowledge the adjustment challenges for design team members who balance clinical responsibilities with project-based design team process, whereby stakeholders drop out of processes and leave decision making to management. Due to the wide participation of diverse stakeholders, some may drop in and out of the process for other reasons, which may contribute to contingency logic, whereby solutions and problems may become reshuffled and misunderstood [].
Related to collaborative or shared decision making is the consideration of the governance structures that define the role of stakeholders in decisions. In three papers assessing participation in design team and processes, Carthey [,,] finds that a clear understanding of roles and the degree of input into decisions are critical to success and group satisfaction. Additional cross-cutting challenges described in the literature include miscommunication between teams and stakeholders, which is directly associated with avoidable rework and re-design efforts, particularly given the visual and three-dimensional character of design [,]. Hierarchies of decision-making input (spoken and unspoken) and individual influence play out in many decisions []. The levels of satisfaction with decisions have been found to be unequal across different stakeholder groups []. Team composition and the full and early involvement of key stakeholders such as nurses [,] and patients are also identified as a challenge and opportunity for higher-quality decisions.
Suggested improvements to interprofessional group decision making include governance structures, analytic methods, structured decision support and frameworks, and widening group participation. MCDM methods [] and participatory design process have been proposed to improve group decisions []. With regard to consensus-building and participation, Taylor et al. [] note the importance of discovering critical and potentially contentious issues early. Several papers identify a beneficial role for structured decision-making frameworks and methodologies in HCFD, both in terms of the design process and facility performance. Colman et al. [] propose an Simulation-based Hospital Design (SbHDT) process that provides a structure for the effective engagement of stakeholders. Irizarry et al. [] note that Building Information Management (BIM)-driven decision support systems have the potential to improve productivity and project success. Access to information in a form and content that stakeholders can use to interpret design options and consequences is considered an important contributor to satisfaction with process and outcomes []. Creating a “superordinate identity” ([], p. 123) for teams and the facilitation of discussions that take into account group dynamics have been identified as important inputs to quality decision making []. Ensuring that stakeholders are aware of their role as well as the extent and limitations of their input into decisions is important to satisfaction with the process as well [,]. Collaboration and consideration given to both evidence and the experiences of the group, documenting decisions, and a focus on outcomes for different constituent groups have likewise been identified as important inputs [,]. Moreover, successful engagement in the design process is linked to buy-in for changes and to employee engagement/organizational culture more generally, particularly where new models of care are proposed in facility re-design [,,]. With respect to the communication of spatial relationships and built environment options, tools such as BIM-augmented reality [] and augmented reality [] are all suggested and validated approaches. Greater design literacy can contribute to more engaged and meaningful decision making by stakeholders []. With respect to stakeholders and the design process, Carthey [] calls for a more explicit focus on how group dynamics and composition can support quality decisions. With respect to decision-making modes, consensus-driven approaches are a theme, whereas less detailed attention has been given to the study of modes or models such as those where team recommendations are used/leadership decides, voting is conducted, or leaders decide and inform stakeholders, for example.
Tools such as project charters and terms of reference have been proposed as being supportive for decision-making teams []. A study applying a Kaizen approach to project vision in a Lean-led approach noted that participants reported that the process supported framing, option comparison, and consensus-building for decisions []. Access to better, more reliable information on design strategies and the cost of those strategies is described as essential to successful, quality decision making. Zadeh et al. [] present a framework that combines EBD together with “value-driven decision-making” with the objective of facilitating communication among stakeholders and establishing a “common analytical language” to inform decision making with respect to specific interventions. This four-step process is primarily information-driven rather than decision-making-driven. The synthesis, translation, and communication of evidence (ex post or ex ante) regarding design options or alternatives are identified as considerable challenges. Harris et al. [] present a multi-step protocol to identify, summarize, and assess the quality of research and connect research to user-defined concerns using an EBD-translator but do not comment on its application vis-a-vis team dynamics.
Elf et al. [] highlight the importance of shared group decision making, noting that many projects fail to define stakeholder requirement, do not involve all important parties, do not establish clear communication structures, and/or do not allocate sufficient time to this critical pre-design activity. Instead, projects adopt a solutions-focused approach which leads to downstream challenges. They propose a holistic approach to understanding needs. Lorusso et al. [] note the importance of clarifying the team and the decision support structure early in the design process but do not elaborate further on this point.
A number of authors have addressed questions related to who is involved in decision making (team composition) and at what level of participation [,,,,,,,,,,,,,,,,,,]. Others have focused on clarifying governance structures and stakeholder roles [,], as well as stakeholder perceptions of design process [], improving information flows for collaboration [], communicating design options, and consensus-building methods []. Included in these discussions are analyses of existing, novel, or hybrid design process frameworks or approaches such as participatory design, change management, the Delphi process, EBD, BIM, and Lean design. Several papers have addressed the need to increase the awareness and integration of cultural and local considerations during design processes and solutions [,,]. It is assumed that structured decision making and stakeholder engagement require slowing down the decision process in spite of the perceived cost as it comes with benefits for DM quality and stakeholder satisfaction []. Yet, some estimate that planning costs may represent less than 6% of the total building cost []. A summary of key challenges with respect to HCFD DM can be found in Table 1.

Table 1.
Summary of Decision-making Challenges in HCFD.
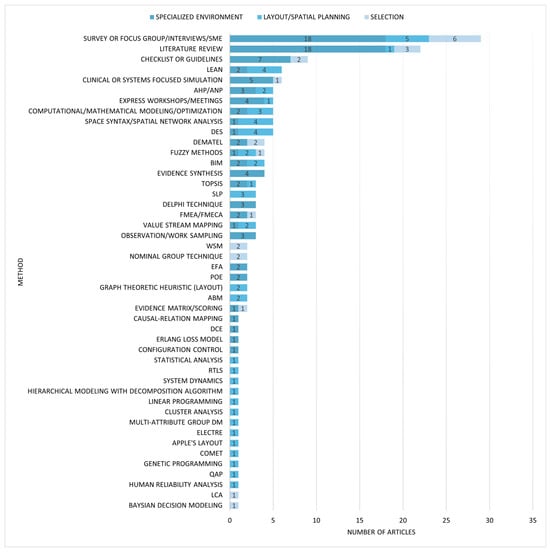
3.6. What Types of Decision Problems Arise During Design, and What Methods and Approaches Have Been Proposed and Studied to Improve Decision Quality?
Three primary design decision problems/contexts can be identified in the literature reviewed here: the design of specialized environments with multiple attributes, building layout or spatial planning problems, and point-in-time selection problems for elements such as equipment or materials. Other decision problems included those related to the wayfinding navigation process [,], signage and wayfinding cues [], and performance assessment []. Cost-related decision problems were explored using target value design with BIM [], Cost–Benefit Analysis (CBA) with BIM [], EBD/value-driven design [], and the collection and ranking of cost drivers []. This section looks at each of the three primary decision contexts in turn, both in terms of challenges and opportunities as well as potential methods for improving decision quality. The most common settings in which these decision problems are explored are Medical Hospital Facilities (including five children’s hospitals), comprising approximately half (53%) of articles. Most of the remaining articles were focused on healthcare facilities with no sub-settings identified (43%). Very few articles focused on outpatient settings, rehabilitation, or behavioral and mental health hospitals (six total). For papers that were focused on the Medical Hospital Facility sub-setting, 24 of the 60 papers concern the design of inpatient care areas, with 10 of these specifically concerned with patient room design. Also considered within the Hospital Facilities category are Diagnostic and Treatment departments (Imaging, Emergency Department, and Surgery) which comprised 13 of the 60 in that sub-setting. Figure 6 shows the counts of articles by healthcare facility setting and medical healthcare facility sub-setting.
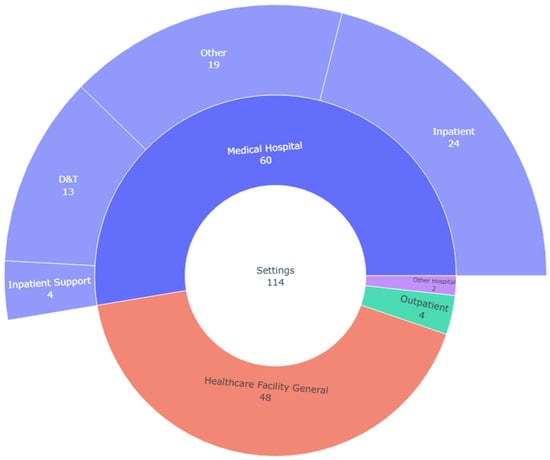
Figure 6.
Included articles by healthcare setting and sub-setting (n = 114).
Layout or spatial planning and the design of specialized patient care environments emerged as the two most common design-specific decision problems for this set of papers. Specialized environment design problems include planning and designing the shape and placement of functional elements in patient rooms, operating suites, and emergency departments, as examples. Decision making related to the design of specialized environments such as patient rooms or operating suites (primarily within hospital settings) was the focus for approximately one-third of all papers reviewed (33%). For the purposes of this paper, the design of specialized spaces is defined as rooms or departmental design that encompass multiple attributes such as equipment, placement, materials, and/or room layout. Layout-related design decision problems (17 papers) relate to decisions as associated with generating, optimizing, prototyping, and choosing among departmental and interdepartmental layouts (also referred to as healthcare facility layout problems or space planning selection-type problems). Point-in-time selection-type decision problems (9 papers) focus on choosing among alternative materials or finishes [], equipment, or departments in need of renovation. Decisions related to improved flows and functionality are a cross-cutting concern throughout many papers.
3.6.1. Decision Problem Focus Area 1: Specialized Room or Departmental Design
Healthcare facilities provide environments for many varied clinical practices as well as administrative, operational, and supportive functions. Specialized spaces require considerable effort and time to design, are functionally critical, and involve spaces that are repeated multiple times in one building. A new inpatient tower design, for example, may repeat an inpatient room upwards of 100 to 400 times. Other specialized spaces such as operating rooms or imaging rooms may be fewer in number and are highly technical. These specialized spaces are care environments where interdisciplinary teams deliver patient care activities. Therefore, group decisions often require building consensus and negotiating trade-offs with a diversity of stakeholders. In the identified literature, the tools and methods applied to the design decisioning process focus on understanding needs and values; building consensus around needs and expected outcomes; aligning design to existing and new workflows through process mapping, visualization, and prototyping; and decision modeling. Figure 7 summarizes the methodologies applied to each type of decision problem. Table A1 provides a summary of articles by settings, methods, country, and decision quality dimensions.
In the context of decision support related to specialized environments, one approach is to develop guidelines based on stakeholder input to guide the generation and evaluation of design concepts. The Delphi technique has been applied in several instances as a method for clarifying therapeutic goals and designing guidelines based on expert opinion for children’s hospitals [], while other studies have adopted mixed method approaches that combine interviews and surveys to establish preferences to guide future decisions [,,,], conduct a review of previous projects [], or evaluate inpatient room designs []. Wang et al. [] apply a Hybrid Multiple-Attribute Decision-Making Model to inform the design of an occupational therapy space that combines Exploratory Factor Analysis, and Decision-Making Trial and Evaluation Laboratory (DEMATEL) Analytic Network Process (DANP) to elicit and prioritize design attribute preferences. Other approaches to informing decision making in specialized environments begin with a literature review and stakeholder consultations and then use prototyping and mock-ups to test performance and refine design options related to outcomes such as infectious disease mitigation [].
Piatkowski et al. [] describe a process for designing an inpatient room, whereby a design advisory council provided input on multiple patient room configurations and used augmented reality modeling, together with spatial heat maps that determine room configuration based on a risk evaluation. The active involvement of the expert group in experiencing and conducting simulation care in the rooms included a discussion of benefits and trade-offs followed by a statistical analysis of surveys to identify important risk mitigation design elements. The relevance of mock-ups and simulations in the evaluation and refinement of specialized environments is described in papers concerning the design of nurse team stations [], a specialized Simulation-based Hospital Design Testing (SbHDT) instrument for children’s hospitals [], and an operating room evaluation toolkit to structure input []. Virtual reality has likewise been applied to evaluate specialized environments such as medication rooms to support stakeholder decisions []. In another study describing the design process for inpatient rooms, van Oel et al. [] engaged patients and clinicians in a Discrete Choice Experiment (DCE) to guide room design decisions. The authors report the benefits of DCE include engaging with larger stakeholder populations and the use of visualization of combined multiple elements results in different choices than when room elements are presented one by one. Novin et al. [] developed a computational model to evaluate multiple patient room designs based on predicting patient movement to address trade-offs and inform decisions effectively but did not comment on stakeholder experience. Lean-led Exploration Loops (LELs) are described as an effective method for supporting decision making in both the programming and schematic phases of design. Johnson et al. [] proposed the use of LELs, a process that organizes express workshops where stakeholders capture flows and subsequently use process maps to generate insights that will assist them in the decision process for the design of operating rooms. Additional multi-step decision support systems for improving design decisions include the application of an Erlang loss model and analytical model for an admission lounge []. Lean approaches are also combined with DES to model design options with operational scenarios to test performance on key indicators for emergency departments []. In summary, while conventional ex post approaches such as original research studies and literature reviews with or without expert input still dominate decision support for specialized environments, more structured ex ante approaches to prototyping as well as more recent hybrid ex ante approaches that integrate computational models, MCDM, LELs, DES, and DCE are emerging methodologies.
3.6.2. Decision Problem Focus Area 2: Departmental and Interdepartmental Facility Layout or Spatial Relationships/Space Planning
Layout planning refers to the size, orientation, adjacencies, and organization of rooms and connectors within a healthcare facility building or department. It refers to the complex process of optimizing flows and connections among spaces which directly influence the efficiency of care processes, communications, visibility and surveillance, occupant satisfaction and comfort, and safety []. Layout has important implications for stress, treatment delays, workload, co-awareness, and error []. Space planning or layout planning takes place during the master planning, early design, and/or schematic design phases where spatial relationships, scale, and form are determined, and floor plans generated []. Layout problems are highly context-dependent given multiple operational approaches and building forms. As layout is most often determined during the space planning or schematic design phase, these approaches are most often applied during these phases. Generative techniques and the application of machine learning and bio-inspired algorithms for layout planning in the context of decision making in HCFD are still nascent.
Two recent systematic reviews [,] have synthesized the literature related to layout decision contexts in HCFD. A third review [] discusses layout problems in healthcare design in some detail. The most recent of these three (covering the period 1965 to 2022) focuses on spatial decision support for healthcare facility layouts [], classifying the literature according to the decision problem and context and methods applied and summarizing decision problems as well as indicators and quality criteria used to assess them. The authors narrow in on papers that have applied spatial network analysis and simulation modeling (DES, Agent-based Modeling (ABM), and Random Walk Simulation (RWS)) to layout problems and provide a useful overview of hospital typologies; graph theory and network analysis; and the use of Geographic Information System (GIS), BIM, OR, and human factors/ergonomics-derived methods []. The authors identify key challenges to optimal layouts, such as addressing overcrowding, long wait times, limited visibility, non-intuitive wayfinding, inconvenient distances between care processes and departments, and infection movement, and synthesize the research with respect to these challenges []. They also propose a “Hospital Design Support System” akin to a transport planning support system as a reliable and transparent decision support mechanism that can predict the impact of the alternatives under consideration [].
An earlier 54-year systematic review of layout planning in HCFD (1965 to 2018) by Benitez et al. [] synthesizes research into two categories of approaches: concepts and guidelines developed based primarily on architectural benchmarks and/or EBD studies, and tools and techniques such as Systematic Layout Process (SLP), Quadratic Assignment Problem (QAP), DES/hybrid DES, Lean, and MCDM or Subject Matter Expert (SME)-based methodologies. That review also summarizes settings, as well as performance criteria such as cost, flows of people and materials, safety and ventilation, staff communication, quality of care, and facility flexibility of use/adaptation. Halawa et al. [] offer a systematic, cross-disciplinary review of the HCFD literature (2008 to 2018) and include a discussion of approaches to layout modeling and performance optimization as one of the primary categories of the literature. Halawa et al. [] acknowledge that the complexity of generating optimal layouts in a healthcare setting implies the need for multiple approaches. The authors conclude with opportunities to apply interdisciplinary systems engineering approaches such as AI, ex ante studies that incorporate variability and are more robust, specialized optimization models, simulation–optimization, and Lean methods.
In the present review, multiple hybrid and integrated methods from the disciplines of architecture and design as well as operations research, systems engineering, and human factors were applied to decisions related to hospital-wide, departmental, or room-specific layout decision problems. See Table A2 for a summary of the approaches applied to facility layout or planning decisions by facility setting, country, and DQC dimension. Performance criteria for layout decisions among the papers in this review included safety or infection risk [,], reducing multiple classes of waste from a Lean perspective [,], minimizing transportation distances [], minimizing walking distances [,], optimizing resource capacity [], ensuring sustainability [], improving occupant satisfaction and functional performance [,,], optimizing departmental closeness or adjacency and determining the allocation of square footage to a department based on expected occupancy [], team communication, the visibility of patients and situational awareness [,], and cost []. Additional criteria introduced by Parsia and Sorooshian [] are the avoidance of the unnecessary traffic of people or materials and clearly separating areas of higher and lower noise levels or tolerance.
The diversity of methods identified in this review reflects the complexity of layout decisions given the highly interdependent nature of care pathways and workflow, subjective and objectively measured performance criteria, multiple stakeholder interests, and the multidisciplinary nature of HCFD. It may also suggest the improvisational, early-stage adoption of new methods from non-design disciplines. Methods include hybrid combinations of DES [,] and ABM [], systems-focused simulation [], Lean techniques [,], SLP, BIM collision detection techniques [], Failure Modes and Effects Analysis (FMEA) [], linear programming, quadratic and genetic programming [], space syntax analysis [,], real-time information systems (RTLS) [], entropy with graph heuristic theory [], hierarchical modeling systems with decomposition algorithms [], the nominal group technique [], Analytic Hierarchy Process (AHP) [], multi-attribute group decision making, and other MCDM methodologies [,,,,,,,,]. Elements in conventional facility layout problem approaches, such as eliciting stakeholder preferences and performance criteria, ranking criteria and establishing optimization objectives and constraints, generating layout options, and ranking their performance, were applied in some form in most papers in this category.
Due to the interactions between the built environment and important human-focused outcomes, methods that can predict behavioral implications are combined with techniques that demonstrate the flow or operational consequences of options. Cai and Jia [] demonstrate the application of the DES process supported by real-time location systems and space syntax analysis in three decision settings: a surgical suite, emergency department, and clinic. These contexts include operational, volumetric, resource, and behavior performance metrics. Space syntax analysis allows for a comparison of multiple layout options to provide quantifiable measures of visibility and navigability based on widely accepted theories related to the effects of layout on people’s behavior []. Cai and Jia [] provide a structured simulation process that begins with the establishment of simulation objectives, data analysis, process mapping through modeling with included “what if” sensitivity analyses, and application to planning decisions. The authors note that the combination of operational (DES) and behavioral space syntax methods provide more comprehensive decision-making information. Morgareidge et al. [] use DES modeling at two different points in planning—first during master planning to decide among options for a relocated emergency department based on operating cost comparisons, and later, during SD, space syntax analysis with DES was applied to plan a pod design to meet expected utilization scenarios and measure visibility and privacy improvements.
Lean principles have also been integrated into layout problem approaches using systems dynamics with DES to optimize layouts with respect to resources and infection flows []. Fogliatto et al. [] also propose a Lean-oriented method that combines extensive workflow analyses to reduce waste with SLP to generate options and the AHP to rank options with respect to multiple criteria. Li et al. [] provide a systematic decision support method which integrates the flow of resources, for example, and optimizes adjacencies between highly related departments. This hybrid approach incorporates multi-objective optimization and BIM with ABM to measure performance for both operational and occupant satisfaction criteria.
Simulation methods for layout analysis and decision support are not limited to computational approaches. Systems-focused simulations which involve the physical simulation of clinical or care processes combined with FMEA have also been proposed to engage with teams to assess the implications of various options for new patient and public corridors to connect existing buildings []. Vimal et al. [] propose a hybrid application of Elimination and Choice Expressing Reality (ELECTRE) and Apple’s layout procedure to assess and select a preferred layout concept. A multistakeholder survey was conducted to establish selection criteria based on higher mean importance scores, and Apple’s layout procedure was applied to map multiple flows (patients, staff, and materials) and determine space needs. Interdepartmental relationship scores were also calculated. The ELECTRE method was then applied to rank multiple options. Helber et al. [] propose a hierarchical modeling system and decomposition algorithm to determine important adjacencies and generate layout options to address the computational complexity involved in the planning of very large hospital environments, noting the approach as supportive of other design option development methods.
Multi-objective layout optimization is proposed by Gülsün et al. [] using a comparative solution approach that models the problem using a quadratic assignment problem and applied genetic algorithm to find the optimal solution. Criteria include walking distances, satisfaction, and closeness relationships. Gai and Ji [] propose a novel integrated, multi-attribute group decision-making (MAGDM) method, whereby reasonable layout concepts are generated using special linear programming and quantitative (cost) and qualitative (expert stakeholder evaluation) values scored using intuitionistic fuzzy sets and weighted using the Technique for Order Preference by Similarity to Ideal Solution (TOPSIS) method. Quantitative and qualitative criteria are synthesized, and options are ranked. Jia et al. [] provide a detailed description and identify limitations in the application of spatial network analysis, RWS, ABM and DES to layout planning and suggest stakeholder-driven use cases for an ex ante integrated spatial decision support system. Benitez et al. [] propose a micro/macro approach, utilizing a novel antecedent cluster analysis of radiologist workflow to establish optimal working cells with the input of SMEs (so-called micro-level planning), followed by SLP (macro-level planning) to plan the layout of the department. Lin and Wang [] apply a three-part process to generate and assess layout options for an operating theater. Systematic layout planning is used to develop concept schemes, and human reliability analysis was conducted to elicit and prioritize software, hardware, environment, and people, followed by a fuzzy AHP to compare the performance of alternative layouts. Applying another hybrid multi-step MCDM methodology, Parsia and Sorooshian [] utilize a hybrid weighted sum method together with Expanded DEMATEL to assess the risks of nosocomial infection transmission associated with spatial relationships that influence the flows between departments. Hassanain et al. [] propose the use of TOPSIS with a reallocation algorithm that identified code-deficient departments and was used to generate re-designed, higher-performing operating suite options. Another study which places high emphasis on flow and operations applies DES to address overcrowding in an emergency department []. Layout and clinical pathways associated with multiple flow scenarios (use of corridors for patient care or alternative holding areas for admitted patients) are evaluated iteratively using DES with input from SMEs. The application of systems engineering and MCDM techniques is more widely represented in facility layout problems compared to specialized environment contexts, including many novel and hybrid approaches.
3.6.3. Decision Problem Focus Area 3: Point-in-Time Selection of Materials, Equipment, or Departments
Typically occurring during the design development phase, choices related to interior finishes, materials, and equipment are safety-critical decisions [] as they directly and indirectly affect patient and staff outcomes related to falls, infection transmission rates, air quality, and comfort, among others. Identifying departments in need of renovation is a related selection problem, albeit one that is on-going and continuous, reflecting changes in care or the emergence of new risks. A small number (9) of papers focused on specific selection decisions related to equipment [,,], materials [,,], or departmental renovation [,]. Figure 7 provides a summary of the methods applied to selection-type decisions. Kim and Augenbroe [] propose a decision model which allows for a multi-criteria comparison of patient isolation room ventilation strategies and their projected impact on energy use, contamination risk, interruptions in care, and thermal comfort. Developed to support facility management decision making, the authors elicit priorities based on stakeholder surveys and calculate equivalent utilities. They note a distinction between assessing performance and utility for a given set of alternatives and apply significance testing on the performance values of decision alternatives. The authors emphasize the practical application of decision tools, including “fast track” assessments as well as the need for integrated quantitative DA methods that can account for both uncertainty and variability. Platt and Chen [] propose a Prevention through Design Environment Material Integrative Control instrument to assist design teams to both analyze and select interior building materials with the lowest potential for infection transmission using the concept of resilience outcomes. A proof-of-concept analysis was conducted on multiple flooring materials. This computational design tool applies a fuzzy hierarchical resilience framework (robustness, recovery, grace extensibility, and sustained adaptability). Two fuzzy inference methods, Sugeno Zeroth Order and Adaptive Neuro-Fuzzy Infection Systems, are used to map performance indicators. Sánchez-Barroso [] propose a bottom-up multi-case Life Cycle Impact Assessment using the ReCiPe method whereby emissions and resource use are translated into environmental impact scores to support decision making related to investments in shielding materials for X-ray rooms. Comparing eight alternative shielding materials, this method generates scores to select from alternative options. In a different type of selection decision problem, a two-step hybrid DEMATEL-Weighted Sum Method (WSM)—MCDM methodology is applied to select departments at the highest risk for nosocomial infection transmission based on inter-relationships and then rank them according to stakeholder-identified criteria []. A nominal group technique is used to gather input from multiple stakeholder groups whose recommendations and criteria were weighted by the major decision-making group. This technique is proposed to simplify the selection of departments for removal/revision in the context of renovation efforts with less time and effort. A Hospital Environmental Appraisal Thermal comfort (HEAT) EBD tool is proposed by Alotaibi et al. [] that elicits preferences by means of a stakeholder survey, validated by a literature review, and provides a scoring system to evaluate alternative thermal comfort strategies. Lenfestey et al. [] apply grounded theory to elicit stakeholder preferences and expert knowledge related to infection mitigation as relates to the choices of materials, flooring, and heating/ventilation/air conditioning systems as well as human behavior to inform future design decisions. See Table A3 for a summary of articles by setting, method, country, and DQC dimensions.
4. Discussion
The need to improve and enhance decision making and decision support during the design of healthcare facilities is widely acknowledged in the HCFD literature. HCFD is characterized by complex decisions made within complex processes and environments with multiple stakeholders. This complexity is attributed to the complex and dynamic nature of the healthcare systems, the involvement of interprofessional stakeholders with varied perspectives and roles in care processes, and high levels of uncertainty. Additional factors influencing decisions include the large, often irreversible, capital outlays required; increasing pressure to innovate and to demonstrate performance and improve efficiency and outcomes; risk aversion within healthcare; long timelines; team turnover in leadership and stakeholders; and the knowledge that decision reversals are costly in terms of schedule, financial impact, and stakeholder trust. Despite numerous references to the importance of decision making, there are considerable gaps in the study of interprofessional group decision-making dynamics. The adoption and application of decision analysis tools and integrated decision flows are in the early stages, most often applied to layout and selection decision problems. Decision quality in the context of HCFD is absent from research. Specific references to holistic or multi-step decision-making or analysis flow, as compared with emphasis on one aspect of that flow, are rare.
Evidence, encompassing ex post and ex ante research and analysis for decision support, is given heavy emphasis in the literature. Within the HCFD literature, there is wide reference to support for informed and evidence-based decision making. Yet, familiar and well-known methods for informed decision making such as EBD in its most broad definition still face challenges in practice. This difficulty has been attributed to an over-reliance on subjective decision making, the limited application of computational or structured decision methods, a preference for qualitative methods, challenges related to communications, and team dynamics. These factors are not unique to EBD. Tension between so-called objective or systematic methods and the qualitative or experiential aspects of decision making is present throughout the literature. Within the EBD literature, the focus is primarily on how evidence is used to design better environments. In the OR/OM research related to healthcare design, the emphasis is on tools and methods for quantifying the benefits of one layout or design strategy over another. However, much of the literature stops there and does not explicitly discuss the decision-making process. There appears to be an assumption that evidence and information will drive better decisions. This suggests the need for integrative or holistic approaches which go beyond tools for decision support and the need to consider a systems approach that considers the decision-making environment and the interdependence between process and people. Standalone and hybrid methods from the disciplines and frameworks of systems engineering, Lean, and healthcare management together with design research and architectural approaches to generating, optimizing, and analyzing design options continue to emerge. One area where the crossover between industries is evident is in facility layout planning techniques and healthcare facility layout problems (HFLPs), as researchers apply tools such as QAP with SLP or QAP with genetic programming to the healthcare facility domain. MCDM methods such as TOPSIS, AHP, ELECTRE, and others are primarily used as decision support methods for layout planning and selection-type problems. This literature review suggests that the crossover and diffusion of these methods are still in an early phase, with experimentation being conducted by early adopters or so-called crossover researchers (systems engineers interested in healthcare design). DES, by comparison, is becoming more common in concurrent HCFD and operational planning, particularly in decisions related to layout and specialized environments. Mock-ups and clinical simulation (physical, virtual, and augmented reality) are conventional architectural approaches typically used to compare and refine design options related to specialized environments. These too have begun to integrate hybrid approaches from other disciplines which include FMEA, Lean, the Delphi method, space syntax, and DCE. DA methods such as tornado diagrams, decision trees, relevance diagrams, flying bar charts, and influence diagrams are absent from this literature set. Option comparison, on the other hand, has received considerable attention in the literature, often combined with optimization, option refinement, or prototyping. Given the iterative and stacking nature of design, the distinctions between option generation, optimization, testing, and prototyping are blurred.
The challenges associated with the interprofessional nature of healthcare design teams are also highlighted in the HCFD literature including team composition, roles, governance, bias, and cultural norms. Design teams encounter challenges of buy-in, commitment, and the clarification of roles. The presence of interprofessional teams with varying needs and preferences, the role of change management in decision buy-in and commitment, the lack of clear roles and governance, and difficulty in translating research into analysis effectively are also acknowledged hurdles to quality decision making. A problem specific to facility design is that of visualizing, communicating, and analyzing three-dimensional options with stakeholders. Authors point to the benefits of participatory design that emphasizes engagement, buy-in, and commitment and the importance of the early engagement of key stakeholders, particularly nurses and patients. Creating supraordinate team identities has likewise been proposed to improve decision making. The interplay between decision support, decision processes, and team dynamics in these articles is often implicit but not well understood or studied in a systematic way. Perceived time constraints or familiarity/trust in processes that engage substantially with stakeholders continues to be a barrier for all these methods. There are limited studies that can demonstrate the benefits of participatory or decision-maker-focused approaches. Even where structured and standalone methods for decision support have been proposed and validated during HCFD, the general emphasis is on improving evidence-based or unbiased objective information or analysis with less attention to the role of behavioral dynamics. As Power et al. ([], p. 120) note, “Decision support builders and data scientists must consider … knowledge and belief, social factors and technical capabilities when developing cognitive, analytical, and decision support systems”.
The knowledge gaps related to HCFD DM suggest a forward-looking interdisciplinary research agenda encompassing two key areas of exploration with potential contributions to decision theory, its application to interprofessional group decision making, and an understanding of design decision quality. First, there is a gap in the empirical understanding of how interprofessional design teams make decisions in practice that could inform a theoretical framework. The literature suggests that decision flows in HCFD involve aspects unique to the context of design. A better understanding of those flows and the elements that contribute to quality facility design-specific decisions could advance decision making in the industry. This would represent a shift from the current emphasis on decision outcomes and shed additional light on decision-making dynamics and decision quality. Potential benefits of applying and adapting approaches and frameworks from the behavioral sciences, BOR, CEDM, and organizational studies may exist. Future research might include the exploration of the dynamics of how teams are assembled and organized to design options, evaluate those options, and make decisions. The second area of exploration would be to consider novel applications of structured decision analysis methods or other relevant decision support approaches in design [], particularly as projects continue to be more complex and dynamic and standards for decision quality increase. With the further expected influence of AI in healthcare and generative AI in architecture and the resulting transformation of planning and design processes, the awareness and exploration of potential AI-enabled innovations on decision making are warranted.
A potential relationships-oriented framework for HCFD decision quality to guide future investigation is proposed in Figure 8. This framework builds on the decision quality dimensions described by Spetzler et al. [] and further developed by SmartOrg [], reframing the dimensions in terms of their interactions and inter-relationships and their contributions to decision quality as well as considering the role of design decision-making inputs in reaching decision quality. A seventh dimension, Testing/Prototyping, is added to the original six in the Spetzler/SmartOrg DQC. In this conceptual frame, four decision-making inputs include decision methods (tools—supportive, augmented, autonomous), design methods (participatory design, Lean, EBD, etc.), decision makers (human or digital), and decision modes (consensus, consultation, etc.). This systems approach explicitly considers the role of interprofessional stakeholder processes, governance, and DM modes and represents a potentially fruitful direction for future research. Due to the lack of empirically derived design-specific DQ frameworks or decision-making flows, future research might also contribute to novel frameworks of theoretical or practical utility. Questions related to whether decision quality is process-agnostic or how satisfaction with the decision process intersects with decision quality have yet to be explored. Other areas of inquiry include additional studies of the relationships between decision analysis methodology and decision quality and the interactions among process, method, and other decision flows.
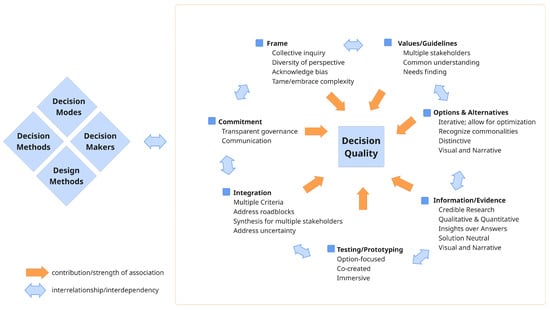
Figure 8.
A proposed relationship framework for HCFD decision making and decision quality. Builds on DQC originally developed by Spetzler et al. [] and SmartOrg [].
The limitations of this systematic review relate to the relative absence of decision quality concepts in the HCFD literature, and therefore relevant papers may have been overlooked if the language used in those papers did not specifically reference decision making. The exploration of non-healthcare design is warranted, as preliminary searches showed a number of innovations related to human decision making in design [], sequential decision making [], and computation frameworks for influencers [] and others. The categorization of the literature related to DQC elements had limitations due to DQC terms being used differently in the healthcare facility design domain. An additional limitation of this study is the unbalanced regional and country-level representation and acknowledgement that 37% of included papers with a specific country-level focus are from the USA. Databases such as the Web of Science have been shown to have less representation from countries in the Global South []. To expand this work to include wider global innovations and perspectives on HCFD DM, future research should be expanded to include additional sources such as African Journals Online or the Directory of Open Access Journals (DOAJ) and others []. The exclusion of conference papers and the gray literature may have limited the inclusion of novel or emerging methods or contributed to fewer non-USA- or European-based studies. New areas of exploration could be informed by research in non-design disciplines related to how team member mental models relate to decision making [,] and teamwork among interprofessional design teams. Several papers identified while conducting this research are related to software design processes and architectural processes more generally [,,] and may indicate utility in expanding search terms.
5. Conclusions
There is a wide acknowledgement of the importance of decision making during HCFD. The relationships between decision support, decision makers, and decision quality during HCFD, however, are not well understood. Evidence and rigorous methods are but one element in enhancing decisions. The contributions of systems engineering and OR/OM approaches to HCFD option development, comparison, and testing have been increasingly demonstrated and adopted in practice. Behavioral decision-making concepts are less evident. The development of integrative decision-making tools and processes and decision quality concepts specific to HCFD is proposed as an opportunity to further enhance the benefits to healthcare organizations, patients, and healthcare teams through high-quality healthcare facilities.
Author Contributions
Conceptualization, A.B.M.G. and S.S.L.; methodology, A.B.M.G.; software, A.B.M.G.; formal analysis, A.B.M.G.; investigation, A.B.M.G.; data curation, A.B.M.G.; writing—original draft preparation, A.B.M.G.; writing—review and editing, A.B.M.G. and S.S.L.; visualization, A.B.M.G.; supervision, S.S.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ABM | Agent-based Modeling |
| AHP | Analytic Hierarchy Process |
| AI | Artificial Intelligence |
| BIM | Building Information Management |
| BOR | Behavioral Operations Research |
| CBA | Cost-Benefit Analysis |
| CEDM | Cognitive Engineering and Decision Making |
| COMET | Characteristic Objects Method |
| DA | Decision Analysis |
| DCE | Discrete Choice Experiment |
| DANP | DEMATEL Analytic Network Process |
| DES | Discrete Event Simulation |
| DM | Decision Making |
| DQ | Decision Quality |
| DQC | Decision Quality Chain |
| EBD | Evidence-based Design |
| EFA | Exploratory Factor Analysis |
| ELECTRE | Elimination and Choice Expressing Reality |
| FMEA | Failure Mode and Effects Analysis |
| HCFD | Healthcare Facility Design |
| HFLP | Healthcare Facility Layout Problem |
| LEL | Lean Exploration Loops |
| MCDM | Multi-criteria Decision Making |
| NDM | Naturalistic Decision Making |
| OR/OM | Operations Research/Operations Management |
| PDP | Participatory Design Process |
| POE | Post-occupancy Evaluation |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| QAP | Quadratic Assignment Problem |
| SSA | Space Syntax Analysis |
| SLP | Systematic Layout Planning |
| SMEs | Subject Matter Experts |
| SRF | Simon Roy Figueras Method |
| TOPSIS | Technique for Order Preference by Similarity to Ideal Solution |
| WSM | Weighted Sum Method |
Appendix A

Table A1.
Settings, methods, country, and DQC dimensions [] for specialized environments decision problems.
Table A1.
Settings, methods, country, and DQC dimensions [] for specialized environments decision problems.
| Specialized Environments Decision Problems | DQC Dimensions | |||||||
|---|---|---|---|---|---|---|---|---|
| Setting | Method(s) (Citation) | Country * | Clear Values | Helpful Frame | Creative Alts. | Useful Info. | Sound Reasoning | Commit. to Action |
| Behavioral and Mental Health Hospital | Literature review [] | INTER (AUS) | ✓ | ✓ | ||||
| Children’s Hospital | Delphi technique [] | IND | ✓ | ✓ | ||||
| Children’s Hospital | Simulation-based Hospital Design Testing (SbHDT) & mock-ups, FMEA [] | USA | ✓ | ✓ | ||||
| Children’s Hospital | SAFEE/SbHDT & mock-ups [] | USA | ✓ | ✓ | ||||
| Children’s Outdoor Therapy Spaces | Delphi technique (fuzzy), survey, EFA, DANP [] | CHN | ✓ | |||||
| Community Health Center | Causal relation mapping, survey, AHP, TOPSIS [] | USA | ✓ | |||||
| Healthcare Design (generally) | Physical mock-ups & clinical simulation [] | USA | ✓ | ✓ | ||||
| Healthcare Design (generally) | Literature review & synthesis [] | N/S (USA) | ✓ | |||||
| Hospital Admissions Lounge | Erlang loss model, survey [] | NLD | ✓ | ✓ | ||||
| Hospital Elevator Maintenance | Literature review, survey, checklist [] | SAU | ✓ | |||||
| Hospital Emergency Department | Mixed methods (interviews & surveys) [] | USA | ✓ | |||||
| Hospital Emergency Department | Lean thinking with DES [] | CAN | ✓ | |||||
| Hospital Infection Mitigation | Mock-ups SME engagement [] | SWE | ✓ | ✓ | ||||
| Hospital Infection Mitigation | Literature review, SME consultation [] | USA | ✓ | |||||
| Hospital Infection Mitigation | Literature review, survey, ANP, DEMATEL, EFA [] | CHN | ✓ | ✓ | ||||
| Hospital Inpatient Room | BIM collision-detection method [] | CHN | ✓ | |||||
| Hospital Inpatient Room | Computational modeling [] | USA | ✓ | ✓ | ||||
| Hospital Inpatient Room | Design advisory council, augmented reality, & heat mapping [] | USA | ✓ | ✓ | ||||
| Hospital Inpatient Room | Literature review [] | INTER (USA) | ✓ | |||||
| Hospital Inpatient Room | Discrete choice experiment, survey [] | NLD | ✓ | ✓ | ||||
| Hospital Inpatient Room | Literature review [] | INTER (USA) | ✓ | ✓ | ||||
| Hospital Inpatient Room | Mixed methods (interviews & surveys) [] | USA | ✓ | ✓ | ||||
| Hospital Inpatient Room | Literature review, stakeholder SME consultation [] | USA | ✓ | ✓ | ||||
| Hospital Intensive Care Unit | Delphi technique; PSSI [] | CAN | ✓ | ✓ | ||||
| Hospital Intensive Care Unit | Observation/work mapping [] | CAN | ✓ | ✓ | ||||
| Hospital Medication Room | VR mock-ups [] | USA | ✓ | ✓ | ||||
| Hospital Operating Room | OR evaluation toolkits, including clinical simulation/mock-up [] | USA | ✓ | ✓ | ||||
| Hospital Operating Room | Lean Exploration Loops (process mapping & stakeholder workshops) [] | USA | ✓ | ✓ | ||||
| Hospital Radiology and Imaging | Case studies, BIM [] | SWE | ✓ | ✓ | ||||
| Hospital Temperature and Lighting Controls | Construction document review & literature synthesis [] | USA | ✓ | |||||
| Inpatient Room - Patient Falls Mitigation | Literature review [] | INTER (USA/GBR) | ✓ | |||||
| Inpatient Room - Patient Privacy and Comfort | Construction document review & literature synthesis [] | USA | ✓ | ✓ | ||||
| Inpatient Unit Team or Nurse Stations | Literature review, survey, synthesis [] | USA | ✓ | ✓ | ||||
| Occupant health | Literature review & synthesis [] | N/S (USA) | ✓ | |||||
| Oncology Inpatient unit | POE, survey [] | USA | ✓ | |||||
| Outpatient Breast Care Center | Literature review, survey, checklist [] | INTER (USA) | ✓ | ✓ | ||||
| Outpatient Supervised consumption | Surveys [] | CAN | ✓ | ✓ | ||||
| Rehabilitation Hospital | Mixed methods (interviews & surveys) [] | AUS | ✓ | ✓ | ||||
* Country abbreviations ([] AUS:, Australia; BRA, Brazil; CAN, Canada; CHN, China; EGY, Egypt; GER, Germany; GRB, Great Britian; IND, India; IRN, Iran; ITA, Italy; NLD, The Netherlands; SAU, Saudi Arabia; SWE, Sweden; TUR, Turkey; USA, United States of America; INTER, international scope (author country); N/S, not specified (author country).

Table A2.
Settings, methods, country, and DQC dimensions [] for layout/spatial planning decision problems.
Table A2.
Settings, methods, country, and DQC dimensions [] for layout/spatial planning decision problems.
| Layout/Spatial Decision Problems | DQC Dimensions | |||||||
|---|---|---|---|---|---|---|---|---|
| Setting | Method(s) & Citation | Country * | Clear Values | Helpful Frame | Creative Alt. | Useful Info. | Sound Reasoning | Commit. to Action |
| HCFD (generally) | Multi-objective QAP, genetic programming [] | TUR | ✓ | ✓ | ||||
| HCFD (generally) | DES, RTLS & SSA [] | USA | ✓ | ✓ | ||||
| HCFD (generally) | Integrated multi-attribute group decision making (MAGDM) [] | CHN | ✓ | ✓ | ||||
| HCFD (generally) | SSA [] | INTER (EGY/ USA) | ✓ | ✓ | ||||
| Hospital Emergency Department | Fuzzy TOPSIS and Graph Heuristic Theories [] | EGY | ✓ | ✓ | ||||
| Hospital Emergency Department | Survey & Checklist [] | USA | ✓ | ✓ | ||||
| Hospital Emergency Department | DES & SSA [] | USA | ✓ | ✓ | ||||
| Hospital Facilities | MCDM Hospital Design Support System with Simulation [] | INTER (NLD) | ✓ | |||||
| Hospital Facilities | Entropy & Graph Heuristics Theory [] | EGY | ✓ | ✓ | ||||
| Hospital Facilities | Hybrid MCDM: ELECTRE/Apple’s Layout Procedure [] | IND | ✓ | ✓ | ||||
| Hospital Facilities | Hierarchical modeling with decomposition algorithm [] | GER | ✓ | ✓ | ||||
| Hospital Intensive Care Unit | Lean principles; systems dynamics [] | ITA | ✓ | |||||
| Hospital Medical/Surgical Unit | Multi-objective optimization & simulation [] | CHN | ✓ | ✓ | ||||
| Hospital Radiology and Imaging Dept | SLP with cluster analysis [] | BRA | ✓ | ✓ | ||||
| Hospital Sterilization Unit | Integrated SLP, MCDM, with Lean techniques [] | BRA | ✓ | ✓ | ✓ | |||
| Hospital Surgery Unit | SHELL; Fuzzy AHP [] | CHN | ✓ | |||||
| Hospital Surgery Unit | Lean Exploration Loops [] | USA | ✓ | ✓ | ✓ | |||
* Country abbreviations []: AUS, Australia; BRA, Brazil; CAN, Canada; CHN, China; EGY, Egypt; GER, Germany; GRB, Great Britian; IND, India; IRN, Iran; ITA, Italy; NLD, The Netherlands; SAU, Saudi Arabia; SWE, Sweden; TUR, Turkey; USA, United States of America; INTER, international scope (author country); N/S, not specified (author country).

Table A3.
Settings, methods, country, and DQC [] dimensions for point-in-time selection-type decision problems.
Table A3.
Settings, methods, country, and DQC [] dimensions for point-in-time selection-type decision problems.
| Selection Decision Problems (Equipment, Materials, Departments) | DQC Dimensions | |||||||
|---|---|---|---|---|---|---|---|---|
| Setting | Method(s) (Citation) | Country * | Clear Values | Helpful Frame | Creative Alts. | Useful Info. | Sound Reasoning | Commit. to Action |
| Healthcare Facility Design (generally) | Survey, Nominal Group Technique, DEMATEL, WSM [] | IRN | ✓ | ✓ | ||||
| Healthcare Floor Finishes | Weighted checklist based on literature review, survey [] | USA | ✓ | ✓ | ||||
| Healthcare Infection Mitigation Materials | Mixed methods (literature review & surveys) [] | USA | ✓ | ✓ | ||||
| Healthcare Interior Materials Selection | Design Environment Material Integrative Control (PtD-EMIC) instrument [] | USA | ✓ | |||||
| Hospital Corridor Connector | Systems focused Simulation with FMEA [] | CAN | ✓ | |||||
| Hospital Indoor Air Quality Selection | Hospital Environmental Appraisal Thermal comfort (HEAT) tool [] | N/S (SAU) | ✓ | ✓ | ||||
| Hospital Infection Mitigation | Algorithm and integrated MCDM techniques []) | IRN | ✓ | ✓ | ||||
| Hospital Radiology room shielding alternatives | LCA [] | ESP | ✓ | ✓ | ||||
| Hospital Ventilation systems | Survey, Bayesian decision modeling [] | USA | ✓ | ✓ | ||||
* Country abbreviations []: AUS, Australia; BRA, Brazil; CAN, Canada; CHN, China; EGY, Egypt; GER, Germany; GRB, Great Britian; IND, India; IRN, Iran; ITA, Italy; NLD, The Netherlands; SAU, Saudi Arabia; SWE, Sweden; TUR, Turkey; USA, United States of America; INTER, international scope (author country); N/S, not specified (author country).
References
- Badri, R.; Dawood, I. The Implications of the Sudan War on Healthcare Workers and Facilities: A Health System Tragedy. Confl. Health 2024, 18, 22. [Google Scholar] [CrossRef]
- Filip, R.; Gheorghita Puscaselu, R.; Anchidin-Norocel, L.; Dimian, M.; Savage, W.K. Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J. Pers. Med. 2022, 12, 1295. [Google Scholar] [CrossRef] [PubMed]
- Kaye, A.D.; Okeagu, C.N.; Pham, A.D.; Silva, R.A.; Hurley, J.J.; Arron, B.L.; Sarfraz, N.; Lee, H.N.; Ghali, G.E.; Gamble, J.W.; et al. Economic Impact of COVID-19 Pandemic on Healthcare Facilities and Systems: International Perspectives. Best Pract. Res. Clin. Anaesthesiol. 2021, 35, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, H.; Kirsch, T.; O’Neil, D.; Anderson, S. The Resilience of Health Care Systems Following Major Disruptive Events: Current Practice and a Path Forward. Reliab. Eng. Syst. Saf. 2023, 235, 109264. [Google Scholar] [CrossRef]
- Sharma, M.; Akhter, M.S.; Roy, S.; Srejon, R. Future Issues in Global Health: Challenges and Conundrums. Int. J. Environ. Res. Public Health 2025, 22, 325. [Google Scholar] [CrossRef]
- Alabi, A.S.; Alabi, O.A.; Adebakin, T.E.; Alayande, B.T. Revisiting Literature on Building Quality of Healthcare Facilities between Developed and Developing Countries: Scoping Review. Int. J. Build. Pathol. Adapt. 2025; ahead-of-print. [Google Scholar] [CrossRef]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing Healthcare: The Role of Artificial Intelligence in Clinical Practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Lee, D. Opportunities and Challenges for Contactless Healthcare Services in the Post-COVID-19 Era. Technol. Forecast. Soc. Change 2021, 167, 120712. [Google Scholar] [CrossRef]
- Joseph, A.; Mihandoust, S.; Wingler, D.; Machry, H.; Allison, D.; Reeves, S. Comparing User Perceptions of Surgical Environments: Simulations in a High-Fidelity Physical Mock-up Versus a Postoccupancy Evaluation. HERD-Health Environ. Res. Des. J. 2022, 15, 116–133. [Google Scholar] [CrossRef]
- Reijula, J.; Ruohomaki, V.; Lahtinen, M.; Reijula, K. Participatory Facility Design Challenges in Two University Hospitals. Intell. Build. Int. 2020, 12, 3–16. [Google Scholar] [CrossRef]
- Wanigarathna, N.; Jones, K.; Bell, A.; Kapogiannis, G. Building Information Modelling to Support Maintenance Management of Healthcare Built Assets. Facilities 2019, 37, 415–434. [Google Scholar] [CrossRef]
- Taylor, E.; Card, A.J.; Piatkowski, M. Single-Occupancy Patient Rooms: A Systematic Review of the Literature Since 2006. HERD Health Environ. Res. Des. J. 2018, 11, 85–100. [Google Scholar] [CrossRef]
- Sharma, V.; Caldas, C.; Mulva, S. Identification and Prioritization of Factors Affecting the Overall Project Cost of Healthcare Facilities. J. Contruction Eng. Manag. 2020, 146, 04019106. [Google Scholar] [CrossRef]
- Anderson, D.C.; Teti, S.L.; Hercules, W.J.; Deemer, D.A. The Bioethics of Built Space: Health Care Architecture as a Medical Intervention. Hastings Cent. Rep. 2022, 52, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Brambilla, A.; Lindahl, G.; Dell’Ovo, M.; Capolongo, S. Validation of a Multiple Criteria Tool for Healthcare Facilities Quality Evaluation. Facilities 2020, 39, 434–447. [Google Scholar] [CrossRef]
- Halawa, F.; Madathil, S.C.; Gittler, A.; Khasawneh, M.T. Advancing Evidence-Based Healthcare Facility Design: A Systematic Literature Review. Health Care Manag. Sci. 2020, 23, 453–480. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.; Hu, M. Value by Design—Systematic Design Decision Making in the Architectural Design Process. In Proceedings of the Architecture of Complexity: Design, Systems, Society and Environment, Salt Lake City, UT, USA, 14–17 June 2017; ITAC: Salt Lake City, UT, USA, 2017. [Google Scholar]
- Elango, M.; Devadas, M.D. Multi-Criteria Analysis of the Design Decisions In Architectural Design Process during the Pre-Design Stage. Int. J. Eng. Technol. 2014, 6, 1033–1046. [Google Scholar]
- Shoemaker, L.K.; Kazley, A.S.; White, A. Making the Case for Evidence-Based Design in Healthcare: A Descriptive Case Study of Organizational Decision Making. HERD-Health Environ. Res. Des. J. 2010, 4, 56–88. [Google Scholar] [CrossRef]
- Perkins, N. Including Patients, Staff and Visitors in the Design of the Psychiatric Milieu Notes from the Field. Facilities 2013, 31, 379–390. [Google Scholar] [CrossRef]
- Morgareidge, D.; Cai, H.; Jia, J. Performance-Driven Design with the Support of Digital Tools: Applying Discrete Event Simulation and Space Syntax on the Design of the Emergency Department. Front. Archit. Res. 2014, 3, 250–264. [Google Scholar] [CrossRef]
- Zadeh, R.; Sadatsafavi, H.; Xue, R. Evidence-Based and Value-Based Decision Making about Healthcare Design: An Economic Evaluation of the Safety and Quality Outcomes. HERD Health Environ. Res. Des. J. 2015, 8, 58–76. [Google Scholar] [CrossRef]
- Piatkowski, M.; Taylor, E.; Wong, B.; Taylor, D.; Foreman, K.B.; Merryweather, A. Designing a Patient Room as a Fall Protection Strategy: The Perspectives of Healthcare Design Experts. Int. J. Environ. Res. Public Health 2021, 18, 8769. [Google Scholar] [CrossRef] [PubMed]
- Cumpat, M. Building Quality Decision Making in Healthcare; Dinu, V., Ed.; Alexandru Ioan Cuza University: Iași, Romania, 2019; pp. 261–267. [Google Scholar]
- Viryasiri, T.; Laovisutthichai, V.; Sangnin, K.; Dhanakoses, K.; Roopkaew, P.; Viryasiri, P. Hospital Design Principles Implementation: Reflections from Practitioners in Thailand. J. Asian Archit. Build. Eng. 2023, 23, 43–56. [Google Scholar] [CrossRef]
- Parsia, Y.; Sorooshian, S. Minimization of Nosocomial Infections Risks by a Decision Algorithm for Upgrading of Healthcare Facilities. J. Infect. Public Health 2020, 13, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Jia, Z.; Nourian, P.; Luscuere, P.; Wagenaar, C. Spatial Decision Support Systems for Hospital Layout Design: A Review. J. Build. Eng. 2023, 67, 106042. [Google Scholar] [CrossRef]
- Ahmadi-Javid, A.; Seyedi, P.; Syam, S.S. A Survey of Healthcare Facility Location. Comput. Oper. Res. 2017, 79, 223–263. [Google Scholar] [CrossRef]
- Kim, S.; Augenbroe, G. Decision Support for Choosing Ventilation Operation Strategy in Hospital Isolation Rooms: A Multi-Criterion Assessment under Uncertainty. Build. Environ. 2013, 60, 305–318. [Google Scholar] [CrossRef]
- ACHA. AI & Its Impact to Health Facility Design & Planning; American College of Healthcare Architects: Cary, NC, USA, 2024; p. 21. [Google Scholar]
- Donia, J.; Shaw, J.A. Co-Design and Ethical Artificial Intelligence for Health: An Agenda for Critical Research and Practice. Big Data Soc. 2021, 8, 20539517211065248. [Google Scholar] [CrossRef]
- Chen, Y.; Clayton, E.W.; Novak, L.L.; Anders, S.; Malin, B. Human-Centered Design to Address Biases in Artificial Intelligence. J. Med. Internet Res. 2023, 25, e43251. [Google Scholar] [CrossRef]
- Alexanian, J.A.; Kitto, S.; Rak, K.J.; Reeves, S. Beyond the Team: Understanding Interprofessional Work in Two North American ICUs. Crit. Care Med. 2015, 43, 1880–1886. [Google Scholar] [CrossRef]
- Bouchez, T.; Cagnon, C.; Hamouche, G.; Majdoub, M.; Charlet, J.; Schuers, M. Interprofessional Clinical Decision-making Process in Health: A Scoping Review. J. Adv. Nurs. 2024, 80, 884–907. [Google Scholar] [CrossRef]
- Ervin, J.N.; Kahn, J.M.; Cohen, T.R.; Weingart, L.R. Teamwork in the Intensive Care Unit. Am. Psychol. 2018, 73, 468–477. [Google Scholar] [CrossRef] [PubMed]
- Manyathi, R.; Terblanche, R. Team Dynamics and Its Effect on the Design Process Within the Construction Industry. In Advances in Engineering Management, Innovation, and Sustainability; Rotimi, J.O.B., Shahzad, W.M., Sutrisna, M., Kahandawa, R., Eds.; Springer Nature: Cham, Switzerland, 2024; pp. 37–50. [Google Scholar]
- Clemen, R.T. Making Hard Decisions: An Introduction to Decision Analysis, 2nd ed.; Duxbury Press: Belmont, CA, USA, 1996; ISBN 0-534-26034-9. [Google Scholar]
- Howard, R.A. The Foundations of Decision Analysis. IEEE Trans. Syst. Sci. Cybern. 1968, 4, 211–219. [Google Scholar] [CrossRef]
- Keeney, R.L.; Raiffa, H. Preface to First Edition. In Decisions with Multiple Objectives: Preferences and Value Trade-Offs; Cambridge University Press: Cambridge, UK, 1993; pp. xv–xx. [Google Scholar]
- Keeney, R.L. Value-Focused Thinking a Path to Creative Decisionmaking; Harvard University Press: Cambridge, MA, USA, 1992; ISBN 0-674-03940-8. [Google Scholar]
- Petropoulos, F.; Laporte, G.; Aktas, E.; Alumur, S.A.; Archetti, C.; Ayhan, H.; Battarra, M.; Bennell, J.A.; Bourjolly, J.-M.; Boylan, J.E.; et al. Operational Research: Methods and Applications. J. Oper. Res. Soc. 2024, 75, 423–617. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Judgment under Uncertainty: Heuristics and Biases. Science 1974, 185, 1124–1131. [Google Scholar] [CrossRef]
- Kahneman, D.; Tversky, A. (Eds.) Choices, Values, and Frames; Cambridge University Press: Cambridge, MA, USA, 2000; ISBN 978-0-521-62749-8. [Google Scholar]
- Markman, A.B. Combining the Strengths of Naturalistic and Laboratory Decision-Making Research to Create Integrative Theories of Choice. J. Appl. Res. Mem. Cogn. 2018, 7, 1–10. [Google Scholar] [CrossRef]
- Gonzalez, C.; Meyer, J. Integrating Trends in Decision-Making Research. J. Cogn. Eng. Decis. Mak. 2016, 10, 120–122. [Google Scholar] [CrossRef]
- Matheson, J.E. Decision Analysis = Decision Engineering. In INFORMS TutORials in Operations Research; Institute for Operations Research and the Management Sciences (INFORMS): Catonsville, MA, USA, 2014; pp. 195–212. ISBN 1-877640-21-2. [Google Scholar]
- Spetzler, C.; Winter, H.; Meyer, J. Decision Quality: Value Creation from Better Business Decisions; John Wiley & Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- SmartOrg Decision Quality 2.0 Worksheet. Available online: https://smartorg.com/gbs-decision-quality-2-worksheet/ (accessed on 14 March 2025).
- Adya, M.; Phillips-Wren, G. Stressed Decision Makers and Use of Decision Aids: A Literature Review and Conceptual Model. Inf. Technol. People 2020, 33, 710–754. [Google Scholar] [CrossRef]
- Arvai, J.; Froschauer, A. Good Decisions, Bad Decisions: The Interaction of Process and Outcome in Evaluations of Decision Quality. J. Risk Res. 2010, 13, 845–859. [Google Scholar] [CrossRef]
- Anåker, A.; Heylighen, A.; Nordin, S.; Elf, M. Design Quality in the Context of Healthcare Environments: A Scoping Review. HERD Health Environ. Res. Des. J. 2017, 10, 136–150. [Google Scholar] [CrossRef]
- Donato, V.; Lo Turco, M.; Bocconcino, M.M. BIM-QA/QC in the Architectural Design Process. Archit. Eng. Des. Manag. 2018, 14, 239–254. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R Package and Shiny App for Producing PRISMA 2020-Compliant Flow Diagrams, with Interactivity for Optimised Digital Transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef] [PubMed]
- The Facility Guidelines Institute. Guidelines for Design and Construction of Hospitals; The Facility Guidelines Institute: Florence, MA, USA, 2022. [Google Scholar]
- The Facility Guidelines Institute. Guidelines for Design and Construction of Outpatient Facilities; The Facility Guidelines Institute: Florence, MA, USA, 2018. [Google Scholar]
- Long, E.F.; Montibeller, G.; Zhuang, J. Health Decision Analysis: Evolution, Trends, and Emerging Topics. Decis. Anal. 2022, 19, 255–264. [Google Scholar] [CrossRef]
- Lincourt, J. A Place for Empathy: Ethics Involving Architectural Designs in Healthcare. HEC Forum 2002, 14, 86. [Google Scholar] [CrossRef]
- Kaelin, K.; Okland, K. Buildings, Barriers, and Breakthroughs: Bridging Gaps in the Health Care Enterprise. Nurs. Adm. Q. 2018, 42, 15–25. [Google Scholar] [CrossRef]
- Elf, M.; Fröst, P.; Lindahl, G.; Wijk, H. Shared Decision Making in Designing New Healthcare Environments—Time to Begin Improving Quality. BMC Health Serv. Res. 2015, 15, 114. [Google Scholar] [CrossRef]
- Taylor, E.; Hignett, S. The SCOPE of Hospital Falls: A Systematic Mixed Studies Review. HERD Health Environ. Res. Des. J. 2016, 9, 86–109. [Google Scholar] [CrossRef]
- Alassafi, H.; Al-Gahtani, K.; Almohsen, A.; Alfalah, G. The Causal Factors of Elevator Maintenance: A Perspective from Saudi Arabia Healthcare Facility Management. Buildings 2022, 12, 532. [Google Scholar] [CrossRef]
- Reno, K.; Okland, K.; Finis, N.; LaMantia, G.; Call, R.; Cardon, K.; Gerber, D.; Zeigler, J. Lessons Learned: Clinicians’ Post-Occupancy Perspective of Facility Design Involvement. HERD Health Environ. Res. Des. J. 2014, 7, 127–139. [Google Scholar] [CrossRef] [PubMed]
- Schouten, H.; Heusinkveld, S.; van der Kam, W.; Benders, J. Implementing Lean-Led Hospital Design; Lessons Gained at a Pioneer. J. Health Organ. Manag. 2020, 35, 1–16. [Google Scholar] [CrossRef]
- Colman, N.; Edmond, M.; Dalpiaz, A.; Walter, S.; Miller, D.; Hebbar, K. Designing for Patient Safety and Efficiency: Simulation-Based Hospital Design Testing. HERD Health Environ. Res. Des. J. 2020, 13, 68–80. [Google Scholar] [CrossRef]
- Ban, Q.; Lyu, M.; Gao, W.; Chen, Y.; Yao, J. Study on Collision Detection Techniques for the Informed Design of Natural Views in Healthcare Environments. HERD Health Environ. Res. Des. J. 2022, 15, 229–245. [Google Scholar] [CrossRef] [PubMed]
- Kevdzija, M. “Everything Looks the Same”: Wayfinding Behaviour and Experiences of Stroke Inpatients in Rehabilitation Clinics. Int. J. Qual. Stud. Health Well-Being 2022, 17, 2087273. [Google Scholar] [CrossRef]
- Dixit, M.; Singh, S.; Lavy, S.; Yan, W.; Pariafsai, F.; Ostadalimakhmalbaf, M. Floor Finish Selection in the Design of Healthcare Facilities: A Survey of Facility Managers. Facilities 2019, 37, 571–599. [Google Scholar] [CrossRef]
- Hassanain, A.A.; Eldosoky, M.A.A.; Soliman, A.M. Healthcare Facilities Redesign Using Multicriteria Decision-Making: Fuzzy TOPSIS and Graph Heuristic Theories. J. Healthc. Eng. 2023, 2023, 9648510. [Google Scholar] [CrossRef]
- Dinulescu, R.; Dobrin, C. Applying the Fuzzy Analytical Hierarchy Process for Classifying and Prioritizing Healthcare Quality Attributes. Manag. Mark.-Chall. Knowl. Soc. 2022, 17, 15–40. [Google Scholar] [CrossRef]
- Alfredsen Larsen, A.S.; Karlsen, A.T.; Andersen, B. Hospital Project Front-End Planning: Current Practice and Discovered Challenges. Proj. Leadersh. Soc. 2020, 1, 100004. [Google Scholar] [CrossRef]
- Brambilla, A.; Sun, T.; Elshazly, W.; Ghazy, A.; Barach, P.; Lindahl, G.; Capolongo, S. Flexibility during the COVID-19 Pandemic Response: Healthcare Facility Assessment Tools for Resilient Evaluation. Int. J. Environ. Res. Public Health 2021, 18, 11478. [Google Scholar] [CrossRef]
- Demirdoegen, G.; Isik, Z.; Arayici, Y. Determination of Business Intelligence and Analytics-Based Healthcare Facility Management Key Performance Indicators. Appl. Sci. 2022, 12, 651. [Google Scholar] [CrossRef]
- Fréchette, J.; Lavoie-Tremblay, M.; Aubry, M.; Kilpatrick, K.; Bitzas, V. Major Hospital Transformations: An Integrative Review and Implications for Nursing. J. Nurs. Educ. Pract. 2020, 10, 46. [Google Scholar] [CrossRef]
- Irizarry, J.; Gheisari, M.; Williams, G.; Roper, K. Ambient Intelligence Environments for Accessing Building Information A Healthcare Facility Management Scenario. Facilities 2014, 32, 120–138. [Google Scholar] [CrossRef]
- Li, Y.; Liao, P.; Song, Y.; Chi, H. A Systematic Decision-Support Approach for Healthcare Facility Layout Design Integrating Resource Flow and Space Adjacency Optimization with Simulation-Based Performance Evaluation. J. Build. Eng. 2023, 77, 107465. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Chen, Y.-P.; Yien, H.-W.; Huang, C.-Y.; Su, Y.-C. Integrated BIM, Game Engine and VR Technologies for Healthcare Design: A Case Study in Cancer Hospital. Adv. Eng. Inform. 2018, 36, 130–145. [Google Scholar] [CrossRef]
- Parsia, Y.; Sorooshian, S. A Decision-Making Algorithm for Rearchitecting of Healthcare Facilities to Minimize Nosocomial Infections Risks. Int. J. Environ. Res. Public Health 2020, 17, 855. [Google Scholar] [CrossRef]
- Pouyan, A.; Ghanbaran, A.; Shakibamanesh, A. Evaluating Building Wayfinding Performance in Healthcare Environment: A Novel Hybrid Decision-Making Model. Archit. Sci. Rev. 2023, 66, 443–467. [Google Scholar] [CrossRef]
- Romano, E.; Falegnami, A.; Cagliano, A.; Rafele, C. Lean ICU Layout Re-Design: A Simulation-Based Approach. Informatics 2022, 9, 35. [Google Scholar] [CrossRef]
- Saad, D.A.; Gharib, F.; El-Said, M. Simulation of Design Changes Impact in Healthcare Construction Projects Using System Dynamics. Can. J. Civ. Eng. 2021, 48, 554–569. [Google Scholar] [CrossRef]
- Schönbeck, P.; Löfsjögård, M.; Ansell, A. A Decision Support System for Hospital Configurations in Construction Projects. Buildings 2022, 12, 1569. [Google Scholar] [CrossRef]
- Shultz, J.; Jha, R. Using Virtual Reality (VR) Mock-Ups for Evidence-Based Healthcare Facility Design Decisions. Int. J. Environ. Res. Public Health 2021, 18, 11250. [Google Scholar] [CrossRef]
- Stichler, J.F. Using Consultants in the Design, Construction, and Occupancy of New Healthcare Facilities. J. Nurs. Adm. 2015, 45, 537–539. [Google Scholar] [CrossRef]
- Ahmed, R.; Nasiri, F.; Zayed, T. A Novel Neutrosophic-Based Machine Learning Approach for Maintenance Prioritization in Healthcare Facilities. J. Build. Eng. 2021, 42, 102480. [Google Scholar] [CrossRef]
- Pati, D. Improving Precision and Confidence of Research Application Through Mediator and Moderator Models. HERD Health Environ. Res. Des. J. 2020, 13, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Bueno, C.; Pereira, L.; Fabricio, M. Early Design BIM-Based Target Value Design for Public Facilities: An Application to a Healthcare Facility Case. Int. J. Archit. Comput. 2023, 22, 540–558. [Google Scholar] [CrossRef]
- Carthey, J. Participatory Design, Project Clients, and Healthcare User Groups. HERD Health Environ. Res. Des. J. 2021, 14, 96–108. [Google Scholar] [CrossRef]
- Chbaly, H. The Challenges and Advantages of Implementing a Lean-Led Design Approach. Architecture 2022, 2, 157–174. [Google Scholar] [CrossRef]
- Alotaibi, B.S.; Codinhoto, R.; Albadra, D.; Lo, S. Combined Multi-Attribute Inpatient Thermal Comfort Requirements in Hospitals: A Designer’s Assessment Method. J. Build. Eng. 2021, 42, 103039. [Google Scholar] [CrossRef]
- The Center for Health Design About EBD. Available online: http://www.healthdesign.org/certification-outreach/edac/about-ebd (accessed on 16 June 2025).
- Harris, D.; Baker, E.; Svacina, J.; Funderburk, L. A Systematic Approach to Evidence-Based Design for Measurable Health and Wellness Outcomes: Curating and Translating Evidence to Practice. HERD Health Environ. Res. Des. J. 2024, 17, 17–29. [Google Scholar] [CrossRef]
- Pati, D.; Pati, S. Methodological Issues in Conducting Post-Occupancy Evaluations to Support Design Decisions. HERD Health Environ. Res. Des. J. 2013, 6, 157–163. [Google Scholar] [CrossRef]
- Chbaly, H.; Forgues, D.; Ben Rajeb, S. Towards a Framework for Promoting Communication during Project Definition. Sustainability 2021, 13, 9861. [Google Scholar] [CrossRef]
- Grunden, N.; Hagood, C. Lean-Led Hospital Design: Creating the Efficient Hospital of the Future; CRC Press: Boca Raton, FL, USA, 2012; ISBN 978-1-4665-5835-9. [Google Scholar]
- Arnstein, S.R. A Ladder of Citizen Participation. J. Am. Inst. Plan. 1969, 35, 216–224. [Google Scholar] [CrossRef]
- Chbaly, H.; Brunet, M. Enhancing Healthcare Project Definition with Lean-Led Design. Sustainability 2022, 14, 1588. [Google Scholar] [CrossRef]
- Lex, A.; Gehlenborg, N.; Strobelt, H.; Vuillemot, R.; Pfister, H. UpSet: Visualization of Intersecting Sets. IEEE Trans. Vis. Comput. Graph. 2014, 20, 1983–1992. [Google Scholar] [CrossRef]
- Novin, R.S.; Taylor, E.; Hermans, T.; Merryweather, A. Development of a Novel Computational Model for Evaluating Fall Risk in Patient Room Design. HERD Health Environ. Res. Des. J. 2021, 14, 350–367. [Google Scholar] [CrossRef]
- Quan, X.; Joseph, A.; Nanda, U. Developing Evidence-Based Tools for Designing and Evaluating Hospital Inpatient Rooms. J. Inter. Des. 2017, 42, 19–38. [Google Scholar] [CrossRef]
- Davidson, J.E. Organizing the Evidence for Healthcare Design Projects. HERD Health Environ. Res. Des. J. 2017, 10, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Devlin, A.S. Wayfinding in Healthcare Facilities: Contributions from Environmental Psychology. Behav. Sci. 2014, 4, 423–436. [Google Scholar] [CrossRef] [PubMed]
- Durham, J.; Kenyon, A. Decentralized Nurse Stations: A Methodology for Using Research to Guide Design Decisions. HERD Health Environ. Res. Des. J. 2019, 12, 8–21. [Google Scholar] [CrossRef]
- Pati, D.; Valipoor, S.; Lorusso, L.; Mihandoust, S.; Jamshidi, S.; Rane, A.; Kazem-Zadeh, M. The Impact of the Built Environment on Patient Falls in Hospital Rooms: An Integrative Review. J. Patient Saf. 2021, 17, 273–281. [Google Scholar] [CrossRef]
- Stichler, J.F. A Conceptual Model for Healthcare Facility Design. J. Nurs. Adm. 2014, 44, 321–325. [Google Scholar] [CrossRef][Green Version]
- Trudel, C.; Cobb, S.; Momtahan, K.; Brintnell, J.; Mitchell, A. Developing Tacit Knowledge of Complex Systems: The Value of Early Empirical Inquiry in Healthcare Design. Technol. Innov. Manag. Rev. 2016, 6, 28–38. [Google Scholar] [CrossRef]
- Zimring, C.; Denham, M.E.; Jacob, J.T.; Kamerow, D.B.; Lenfestey, N.; Hall, K.K.; Kasali, A.; Cowan, D.Z.; Steinberg, J.P. The Role of Facility Design in Preventing Healthcare-Associated Infection: Interventions, Conclusions, and Research Needs. HERD Health Environ. Res. Des. J. 2013, 7, 127–139. [Google Scholar] [CrossRef]
- Brittin, J.; Araz, O.; Frerichs, L.; Elijah-Barnwell, S.; Huang, T. Methodology to Integrate Complex-Systems Thinking and Multi-Criteria Decision Analysis in Health-Oriented Planning and Application to a Health-Care Example. J. Archit. Plan. Res. 2017, 34, 192–215. [Google Scholar]
- Devlin, A.S.; Andrade, C.C.; Carvalho, D. Qualities of Inpatient Hospital Rooms: Patients’ Perspectives. HERD Health Environ. Res. Des. J. 2016, 9, 190–211. [Google Scholar] [CrossRef]
- Watson, T.; Strike, C.; Kolla, G.; Penn, R.; Jairam, J.; Hopkins, S.; Luce, J.; Degani, N.; Millson, P.; Bayoumi, A. Design Considerations for Supervised Consumption Facilities (SCFs): Preferences for Facilities Where People Can Inject and Smoke Drugs. Int. J. Drug Policy 2013, 24, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Babbu, A.; Haque, M. A Framework for the Design of Pediatric Healthcare Environment Using the Delphi Technique. Ain Shams Eng. J. 2023, 14, 101975. [Google Scholar] [CrossRef]
- Wang, G.; Wang, R.; Liu, T.; Zhuo, Y.; Shen, K. Application of Hybrid Multiple Attribute Decision-Making Model to Explore the Design Strategies of Children’s Facilities in Neighborhood Open Spaces Based on Sensory Integration Theory. J. Healthc. Eng. 2021, 2021, 5556172. [Google Scholar] [CrossRef]
- Gülsün, B.; Miç, P.; Edali, M. Comparative Solution Approach with Quadratic and Genetic Programming to Multi-Objective Healthcare Facility Location Problem. Sigma J. Eng. Nat. Sci. 2022, 40, 63–78. [Google Scholar] [CrossRef]
- Alfonsi, E.; Capolongo, S.; Buffoli, M. Evidence Based Design and Healthcare: An Unconventional Approach to Hospital Design. Ann. Ig. Med. Prev. E Comunita 2014, 26, 137–143. [Google Scholar] [CrossRef]
- Colman, N.; Dalpiaz, A.; Walter, S.; Chambers, M.S.; Hebbar, K.B. SAFEE: A Debriefing Tool to Identify Latent Conditions in Simulation-Based Hospital Design Testing. Adv. Simul. 2020, 5, 14. [Google Scholar] [CrossRef]
- Slosberg, M.; Nejati, A.; Evans, J.; Nanda, U. Transitioning to a New Facility: The Crucial Role of Employee Engagement. J. Healthc. Manag. 2018, 63, 63. [Google Scholar] [CrossRef]
- Brittin, J.; Okland, K.; Rogers, J.L.; Rich, R.K.; Bazuin, D.; Harper, K.; Roy, L. From Competition to Collaboration: How a Multi-Firm Research Coalition Is Realizing Rigorous Facility Evaluation at Parkland Hospital. HERD Health Environ. Res. Des. J. 2020, 13, 32–45. [Google Scholar] [CrossRef]
- Dubé, M.; Martel, J.; Kumagai, J.; Suddes, M.; Cullen, J.; Laberge, J. Applying Human Factors and Systems Simulation Methods to Inform a Multimillion-Dollar Healthcare Decision. HERD Health Environ. Res. Des. J. 2024, 17, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Mohammadpour, A.; Anumba, C.; Messner, J. Retrofitting of Healthcare Facilities: Case Study Approach. J. Archit. Eng. 2017, 23, 05017003. [Google Scholar] [CrossRef]
- Lenfestey, N.; Denham, M.; Hall, K.; Kamerow, D. Expert Opinions on the Role of Facility Design in the Acquisition and Prevention of Healthcare-Associated Infections. HERD Health Environ. Res. Des. J. 2013, 7, 31–45. [Google Scholar] [CrossRef]
- Carthey, J. Interdisciplinary User Groups and the Design of Healthcare Facilities. HERD Health Environ. Res. Des. J. 2020, 13, 114–128. [Google Scholar] [CrossRef] [PubMed]
- Guidance for Designing Health and Residential Care Facilities That Respond and Adapt to Emergency Conditions; Facilities Guidelines Institute: Florence, MA, USA, 2021; p. 679.
- Keys, Y. Chief Nursing Officers’ Perspectives on Hospital-Based Building or Remodeling Projects. J. Nurs. Adm. 2019, 49, 556–560. [Google Scholar] [CrossRef]
- Samset, K.; Christensen, T. Ex Ante Project Evaluation and the Complexity of Early Decision-Making. Public Organ. Rev. 2017, 17, 1–17. [Google Scholar] [CrossRef]
- Carthey, J. User Group Consultation: Design Quality and Project Success. HERD-Health Environ. Res. Des. J. 2020, 13, 143–169. [Google Scholar] [CrossRef]
- Damurski, L.; Pluta, J.; Maier, K.; Andersen, H. Stakeholders in the Local Service Centre: Who Should Be Involved in the Planning Process? Insights from Poland, Czech Republic and Denmark. Bull. Geogr.-Sicio-Econ. Ser. 2019, 43, 91–106. [Google Scholar] [CrossRef]
- Campion, N.; Thiel, C.L.; Focareta, J.; Bilec, M.M. Understanding Green Building Design and Healthcare Outcomes: Evidence-Based Design Analysis of an Oncology Unit. J. Archit. Eng. 2016, 22, 04016009. [Google Scholar] [CrossRef]
- Lorusso, L.; Allied, A.; Lee, J.; Worden, E. Design Thinking for Healthcare: Transliterating the Creative Problem-Solving Method Into Architectural Practice. HERD Health Environ. Res. Des. J. 2021, 14, 16–29. [Google Scholar] [CrossRef]
- Gregory, D.D.; Stichler, J.F.; Zborowsky, T. Adapting and Creating Healing Environments: Lessons Nurses Have Learned From the COVID-19 Pandemic. Nurse Lead. 2022, 20, 201–207. [Google Scholar] [CrossRef]
- Holmdahl, T.; Lanbeck, P. Design for the Post-Antibiotic Era: Experiences from a New Building for Infectious Diseases in Malmo, Sweden. HERD Health Environ. Res. Des. J. 2013, 6, 27–52. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.; Mazur, L.M.; Chadwick, J.; Pooya, P.; Amos, A.; McCreery, J. Integrating Lean Exploration Loops Into Healthcare Facility Design: Schematic Phase. HERD Health Environ. Res. Des. J. 2017, 10, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Mazur, L.M.; Johnson, K.; Pooya, P.; Chadwick, J.; McCreery, J. Integrating Lean Exploration Loops Into Healthcare Facility Design: Programming Phase. HERD Health Environ. Res. Des. J. 2017, 10, 116–130. [Google Scholar] [CrossRef] [PubMed]
- Taylor, E. We Agree, Don’t We? The Delphi Method for Health Environments Research. HERD Health Environ. Res. Des. J. 2020, 13, 11–23. [Google Scholar] [CrossRef]
- Crocker, S. A Call for Intersectional Healthcare Design Research. HERD Health Environ. Res. Des. J. 2021, 14, 273–277. [Google Scholar] [CrossRef]
- Reijula, J.; Kouri, J.; Aalto, L.; Miettunen, R.; Reijula, K. Healthcare Facility Design Development in Kuopio University Hospital. Intell. Build. Int. 2017, 9, 137–147. [Google Scholar] [CrossRef]
- Guo, W.; He, Y. Optimized Wayfinding Signage Positioning in Hospital Built Environment through Medical Data and Flows Simulations. Buildings 2022, 12, 1426. [Google Scholar] [CrossRef]
- Omar, F.; Fateh, M.; Godawatte, G. Critical Success Factors (CFSs) Implementation Cost-Benefit Analysis (CBA) Into Building Information Modelling (BIM) Application Through Malaysian Government Healthcare Projects. Int. J. Sustain. Constr. Eng. Technol. 2023, 14, 67–76. [Google Scholar] [CrossRef]
- Bosch, S.J.; Valipoor, S.; Alakshendra, A.; De Portu, G.; Mohammadigorji, S.; Rittenbacher, D.; Black, K.; Calienes, E. Coping and Caregiving: Leveraging Environmental Design to Moderate Stress Among Healthcare Workers in the Emergency Department Setting. HERD Health Environ. Res. Des. J. 2023, 16, 261–277. [Google Scholar] [CrossRef]
- Connellan, K.; Gaardboe, M.; Riggs, D.; Due, C.; Reinschmidt, A.; Mustillo, L. Stressed Spaces: Mental Health and Architecture. HERD Health Environ. Res. Des. J. 2013, 6, 127–168. [Google Scholar] [CrossRef] [PubMed]
- Lipson-Smith, R.; Zeeman, H.; Muns, L.; Jeddi, F.; Simondson, J.; Bernhardt, J. The Role of the Physical Environment in Stroke Recovery: Evidence-Based Design Principles from a Mixed-Methods Multiple Case Study. PLoS ONE 2023, 18, e0280690. [Google Scholar] [CrossRef] [PubMed]
- Bingham, E.; Whitaker, D.; Farnsworth, C.; Smith, J. Evidence-Based Design in Hospital Renovation Projects: Design Implementation for Patient Privacy and Comfort. J. Archit. Eng. 2022, 28, 04022002. [Google Scholar] [CrossRef]
- Durham, J.; Kenyon, A. Mock-Ups: Using Experiential Simulation Models in the Healthcare Design Process. HERD Health Environ. Res. Des. J. 2019, 12, 11–20. [Google Scholar] [CrossRef]
- Bayramzadeh, S.; Joseph, A.; Allison, D.; Shultz, J.; Abernathy, J. Using an Integrative Mock-up Simulation Approach for Evidence-Based Evaluation of Operating Room Design Prototypes. Appl. Ergon. 2018, 70, 288–299. [Google Scholar] [CrossRef]
- van Oel, C.J.; Mlihi, M.; Freeke, A. Design Models for Single Patient Rooms Tested for Patient Preferences. HERD Health Environ. Res. Des. J. 2021, 14, 31–46. [Google Scholar] [CrossRef]
- Veneklaas, W.; Leeftink, A.; van Boekel, P.; Hans, E. On the Design, Implementation, and Feasibility of Hospital Admission Services: The Admission Lounge Case. OMEGA-Int. J. Manag. Sci. 2021, 100, 102308. [Google Scholar] [CrossRef]
- Gabriel, G.T.; Campos, A.T.; Magacho, A.d.L.; Segismondi, L.C.; Vilela, F.F.; de Queiroz, J.A.; Montevechi, J.A.B. Lean Thinking by Integrating with Discrete Event Simulation and Design of Experiments: An Emergency Department Expansion. PeerJ Comput. Sci. 2020, 6, e284. [Google Scholar] [CrossRef]
- Benitez, G.B.; Da Silveira, G.J.C.; Fogliatto, F.S. Layout Planning in Healthcare Facilities: A Systematic Review. HERD Health Environ. Res. Des. 2019, 12, 31–44. [Google Scholar] [CrossRef]
- Defining the Architect’s Basic Services. Available online: https://www.aia.org/resource-center/defining-the-architects-basic-services (accessed on 30 August 2024).
- Fogliatto, F.S.; Tortorella, G.L.; Anzanello, M.J.; Tonetto, L.M. Lean-Oriented Layout Design of a Health Care Facility. Qual. Manag. Health Care 2019, 28, 25–32. [Google Scholar] [CrossRef]
- Helber, S.; Böhme, D.; Oucherif, F.; Lagershausen, S.; Kasper, S. A Hierarchical Facility Layout Planning Approach for Large and Complex Hospitals. Flex. Serv. Manuf. J. 2016, 28, 5–29. [Google Scholar] [CrossRef]
- Cai, H.; Jia, J. Using Discrete Event Simulation (DES) To Support Performance-Driven Healthcare Design. HERD Health Environ. Res. Des. J. 2019, 12, 89–106. [Google Scholar] [CrossRef] [PubMed]
- Vimal, K.; Kandasamy, J.; Nadeem, S.; Kumar, A.; Saparauskas, J.; Garza-Reyes, J.; Trinkuniene, E. Developing a Strategic Sustainable Facility Plan for a Hospital Layout Using ELECTRE and Apple’s Procedure. Int. J. Strateg. Prop. Manag. 2021, 25, 17–33. [Google Scholar] [CrossRef]
- Benitez, G.B.; Fogliatto, F.S.; Cardoso, R.B.; Torres, F.S.; Faccin, C.S.; Dora, J.M. Systematic Layout Planning of a Radiology Reporting Area to Optimize Radiologists’ Performance. J. Digit. Imaging 2018, 31, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Hassanain, A.A.; Eldosoky, M.; Soliman, A. Evaluating Building Performance in Healthcare Facilities Using Entropy and Graph Heuristic Theories. Sci. Rep. 2022, 12, 8973. [Google Scholar] [CrossRef]
- Sadek, A.; Shepley, M. Space Syntax Analysis: Tools for Augmenting the Precision of Healthcare Facility Spatial Analysis. HERD Health Environ. Res. Des. J. 2016, 10, 114–129. [Google Scholar] [CrossRef]
- Gai, L.; Ji, J. An Integrated Method to Solve the Healthcare Facility Layout Problem under Area Constraints. J. Comb. Optim. 2019, 37, 95–113. [Google Scholar] [CrossRef]
- Lin, Q.; Wang, D. Facility Layout Planning with SHELL and Fuzzy AHP Method Based on Human Reliability for Operating Theatre. J. Healthc. Eng. 2019, 2019, 8563528. [Google Scholar] [CrossRef]
- Valipoor, S.; Hatami, M.; Hakimjavadi, H.; Akçalı, E.; Swan, W.A.; Portu, G.D. Data-Driven Design Strategies to Address Crowding and Boarding in an Emergency Department: A Discrete-Event Simulation Study. HERD Health Environ. Res. Des. J. 2021, 14, 161–177. [Google Scholar] [CrossRef]
- Platt, L.; Chen, X. A Computational Approach to Estimating Healthcare Contact Surface Material Resilience. HERD Health Environ. Res. Des. J. 2023, 16, 268–283. [Google Scholar] [CrossRef]
- Sánchez-Barroso, G.; Botejara-Antúnez, M.; García-Sanz-Calcedo, J.; Zamora-Polo, F. A Life Cycle Analysis of Ionizing Radiation Shielding Construction Systems in Healthcare Buildings. J. Build. Eng. 2021, 41, 102387. [Google Scholar] [CrossRef]
- Power, D.J.; Cyphert, D.; Roth, R.M. Analytics, Bias, and Evidence: The Quest for Rational Decision Making. J. Decis. Syst. 2019, 28, 120–137. [Google Scholar] [CrossRef]
- Roth, A.; Rosenzweig, E. Advancing Empirical Science in Operations Management Research: A Clarion Call to Action. Manuf. Serv. Oper. Manag. 2020, 22, 179–190. [Google Scholar] [CrossRef]
- Vermillion, S.D.; Malak, R.J.; Smallman, R.; Becker, B.; Sferra, M.; Fields, S. An Investigation on Using Serious Gaming to Study Human Decision-Making in Engineering Contexts. Des. Sci. 2017, 3, e15. [Google Scholar] [CrossRef]
- Rahman, M.H.; Yuan, S.; Xie, C.; Sha, Z. Predicting Human Design Decisions with Deep Recurrent Neural Network Combining Static and Dynamic Data. Des. Sci. 2020, 6, e15. [Google Scholar] [CrossRef]
- Singh, H.; Cascini, G.; McComb, C. Idea Selection in Design Teams: A Computational Framework and Insights in the Presence of Influencers. Des. Sci. 2022, 8, e23. [Google Scholar] [CrossRef]
- Rucavado Rojas, D.; Postigo, J.C. The Cycle of Underrepresentation: Structural and Institutional Factors Limiting the Representation of Global South Authors and Knowledge in the IPCC. Clim. Change 2025, 178, 19. [Google Scholar] [CrossRef]
- Crow, R. LibGuides: Systematic Reviews for the Social Sciences: Location of Studies. Available online: https://bristol.libguides.com/sys-reviews-soc-sci/location-of-studies (accessed on 24 June 2025).
- Casakin, H.; Badke-Schaub, P. Mental Models and Creativity in Engineering and Architectural Design Teams. In Design Computing and Cognition ’14; Gero, J.S., Hanna, S., Eds.; Springer International Publishing: Cham, Switzerland, 2015; pp. 155–171. [Google Scholar]
- Casakin, H.; Badke-Schaub, P. Sharedness of Team Mental Models in the Course of Design-Related Interaction between Architects and Clients. Des. Sci. 2017, 3, e14. [Google Scholar] [CrossRef]
- Bakht, M.; El-Diraby, T.E. Synthesis of Decision-Making Research in Construction. J. Constr. Eng. Manag. 2015, 141, 04015027. [Google Scholar] [CrossRef]
- Chachere, J.M.; Haymaker, J.R. Framework for Measuring the Rationale Clarity of AEC Design Decisions. J. Archit. Eng. 2011, 17, 86–96. [Google Scholar] [CrossRef]
- Guo, K.L. DECIDE: A Decision-Making Model for More Effective Decision Making by Health Care Managers. Health Care Manag. 2020, 39, 133. [Google Scholar] [CrossRef] [PubMed]
- Xiong, L.; Sheng, G.; Fan, Z.; Yang, H.; Hwang, F.; Zhu, B. Environmental Design Strategies to Decrease the Risk of Nosocomial Infection in Medical Buildings Using a Hybrid MCDM Model. J. Healthc. Eng. 2021, 2021, 5534607. [Google Scholar] [CrossRef] [PubMed]
- Dubé, M.; Shultz, J.; Barnes, S.; Pascal, B.; Kaba, A. Goals, Recommendations, and the How-To Strategies for Developing and Facilitating Patient Safety and System Integration Simulations. HERD Health Environ. Res. Des. J. 2020, 13, 94–105. [Google Scholar] [CrossRef] [PubMed]
- Bingham, E.; Whitaker, D.; Christofferson, J.; Weidman, J. Evidence-Based Design in Hospital Renovation Projects: A Study of Design Implementation for User Controls. HERD 2020, 13, 133–142. [Google Scholar] [CrossRef]
- Guevara, D. Specialty Space: Breast Care Centers. HERD Health Environ. Res. Des. 2021, 14, 358–373. [Google Scholar] [CrossRef]
- ISO. ISO 3166-1; Codes for the Representation of Names of Countries and Their Subdivisions—Part 1: Country Code. ISO: Geneva, Switzerland, 2020. Available online: https://www.iso.org/iso-3166-country-codes.html (accessed on 7 July 2025).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).