Abstract
Background. Exercise stress test (EST) has been scarcely investigated in patients with arrhythmic myocarditis. Objectives. To report the results of EST late after myocarditis with arrhythmic vs. nonarrhythmic presentation. Methods. We enrolled consecutive adult patients with EST performed at least six months after acute myocarditis was diagnosed using gold-standard techniques. Patients with ventricular arrhythmia (VA) at presentation were compared with the nonarrhythmic group. Adverse events occurring during follow-up after EST included cardiac death, disease-related rehospitalization, malignant VA, and proven active myocarditis. Results. The study cohort was composed of 128 patients (age 41 ± 9 y, 70% males) undergoing EST after myocarditis. Of them, 64 (50%) had arrhythmic presentation. EST was performed after 15 ± 4 months from initial diagnosis, and was conducted on betablockers in 75 cases (59%). During EST, VA were more common in the arrhythmic group (43 vs. 4, p < 0.001), whereas signs and symptoms of ischemia were more prevalent in the nonarrhythmic one (6 vs. 1, p = 0.115). By 58-month mean follow-up, 52 patients (41%) experienced adverse events, with a greater prevalence among arrhythmic patients (39 vs. 13, p < 0.001). As documented both in the arrhythmic and nonarrhythmic subgroups, patients had greater prevalence of adverse events following a positive EST (40/54 vs. 12/74 with negative EST, p < 0.001). Electrocardiographic features of VA during EST correlated with the subsequent inflammatory restaging of myocarditis. Nonarrhythmic patients with uneventful EST both on- and off-treatment were free from subsequent adverse events. Conclusions. Late after the arrhythmic presentation of myocarditis, EST was frequently associated with recurrent VA. In both arrhythmic and nonarrhythmic myocarditis, EST abnormalities correlated with subsequent adverse outcomes.
1. Introduction
Exercise stress test (EST) is an informative diagnostic tool allowing assessment of both inducible myocardial ischemia and arrhythmia [1]. To date, however, EST is under-investigated in myocarditis, an inflammatory disease of the myocardium initiated by viral infections, toxic agents, or dysimmune processes and frequently affecting young and otherwise healthy subjects [2]. In fact, due to the potentially harmful effects of strenuous physical activity during the active inflammatory stage of the disease [3], EST is currently contraindicated in patients diagnosed with acute myocarditis [2,4]. On the other hand, EST is considered a safe and informative technique after myocarditis healing [2,4]. Consistently, international guideline documents agree in recommending the use of EST after six months from acute myocarditis before resuming competitive sport participation [4,5]. In this setting, the absence of arrhythmia and ischemia signs is needed to demonstrate safety during incremental physical activity [6]. Remarkably, the evidence currently supporting the role of EST in myocarditis focuses on the classic acute coronary syndrome (ACS)-like presentation of myocarditis, which is the most common and benign scenario [7,8,9]. Currently, there is a lack of consistent data about EST in the remaining clinical presentations, in particular in patients with ventricular arrhythmia (VA) at the time of diagnosis. The issue is demanding since VA associated with myocarditis may be life-threatening and have been described both during the acute and chronic phases of the disease [10].
The aim of our study is to compare the results of EST at late stage of arrhythmic vs. nonarrhythmic presentation of myocarditis.
2. Materials and Methods
2.1. Study Design
This study, observational and prospective, was performed at a referral center for the management of arrhythmic myocarditis. Following the local institutional review board approval, written informed consent was obtained from all participants (MYOCAR, 24/01/2018). From January 2013 to January 2021, we enrolled consecutive inhospital patients with myocarditis, undergoing EST late after clinical presentation. In detail, inclusion criteria were: (1) age ≥ 18 years; (2) acute clinical presentation with myocarditis diagnosed by gold standard techniques, namely cardiac magnetic resonance (CMR) and/or endomyocardial biopsy (EMB); (3) EST performed at least six months after myocarditis diagnosis.
Patients presenting with VA constituted the study group and were compared with controls without VA. For the purposes of the study, VA included ventricular fibrillation (VF), either sustained or nonsustained ventricular tachycardia (VT; NSVT), or ventricular ectopies (VE) of Lown’s grade ≥2 [11].
Exclusion criteria were: catheter ablation of VT performed before EST; EST not performed or contraindicated due to clinical instability; and loss to follow-up.
2.2. Myocarditis Diagnosis
EMB-proven active myocarditis was defined, as recommended [2], based on histological (inflammatory infiltrates and myocyte degeneration fulfilling the Dallas criteria), immunohistochemical (≥14 leucocytes/mm2 and CD3+ T-lymphocytes ≥7 cells/mm2), and molecular criteria (polymerase chain reaction, to identify or exclude viral etiology). EMB was performed by percutaneous right ventricular sampling under fluoroscopic and echocardiographic guidance [12]. CMR-proven myocarditis was defined by the standard and updated Lake Louise criteria (LLC) [13,14] in patients enrolled before and after 2016, respectively. In detail, CMR was performed on a 1.5 T scanner (Achieva dStream; Philips Medical Systems, Eindhoven, The Netherlands) equipped with a 32-channel phased-array coil. Myocardial edema was evaluated using black blood T2 short-tau inversion recovery (STIR) images. Modified Look-Locker inversion recovery sequences and gradient-(echo planar imaging) and spin-echo multi-echo sequences were used for T1 mapping and T2 mapping, respectively. Late gadolinium enhancement (LGE) images were acquired 10 min after gadolinium injection using 2D T1 weighted segmented inversion-recovery gradient-echo sequences, and analyzed on two orthogonal planes. The correct inversion time was determined using the Look-Locker technique. Extracellular volume (ECV) was obtained according to recommended standards [15].
2.3. Treatment and Follow-Up
Treatment for myocarditis was patient-tailored, including optimal medical treatment and cardiac device implant, based on international guideline recommendations [16,17] and the experience of the center [18]. Upon clinical indication, immunosuppressive therapy (IST) was applied to patients with virus-negative myocarditis [19]. In particular, IST use was driven by persistent symptomatic troponin release, left ventricular systolic dysfunction, and sustained or recurrent VA. For all patients, regular follow-up at a dedicated outpatient multidisciplinary facility [20] was obtained every three months by multimodal reassessment (blood exams including cardiac biomarkers, transthoracic echocardiogram, and 12-lead 24-h Holter ECG). To allow myocarditis restaging, either CMR or EMB was repeated during follow-up based on patient symptoms and clinical reassessment. In patients with implanted cardiac devices or contraindications to CMR, 18F-Fluorodeoxyglucose positron emission tomography (FDG-PET) scan was obtained instead [21].
2.4. EST
As per protocol and routine clinical practice, EST was performed at least six months after diagnosis of acute myocarditis. Judgement of clinical stability, including normalization of T-troponin, absence of episodes of sustained VT or VF over the last six months, and no worsening in left ventricular ejection fraction (LVEF), as compared to baseline assessment, was obtained before indicating EST. For patients receiving IST, treatment termination was an additional required condition.
EST was conducted in designed labs by personnel blinded to the study purposes, in compliance with the American College of Cardiology/American Heart Association guidelines [1]. The modified Bruce protocol [22] was applied. 12-lead ECG, heart rate, and blood pressure were closely monitored, symptoms constantly evaluated, and parameters such as maximal rate pressure product and metabolic equivalents (METs) of estimated exercise capacity systematically reported [22,23].
EST was terminated by the physician in patients with: (a) maximal test, defined as an increase in heart rate either to ≥85% of the maximum predicted value off betablockers, or to ≥75% of the threshold on betablockers; EST was otherwise defined as submaximal; (b) sustained VT/VF, symptomatic NSVT, or significant increase in VE burden on effort, including polymorphic or bi/trigeminal beats; (c) angina and/or ST-T changes, including ST depression of ≥2 mm read at 60 to 80 ms from the J point, or new-onset negative T waves in at least two consecutive leads. EST was deemed uninterpretable for ischemia in the presence of baseline left bundle branch block.
For all VA documented on EST, 12-lead morphology and cycle length regularity were assessed as previously described [24].
2.5. Endpoints
The study endpoints, evaluated for both the study and control groups, included: (1) occurrence of VA during EST; (2) documentation of signs and/or symptoms of ischemia (diagnostic ST-T changes; angina-like chest pain with subsequent documentation of T-troponin raise) during EST; (3) occurrence of adverse events, namely cardiac death, disease-related hospital readmissions, malignant VA (sustained VT, VF, appropriate ICD treatment), and active myocarditis proven either by EMB, CMR, or FDG-PET after EST until the end of study (1 June 2022).
2.6. Statistical Analysis
SPSS Version 20 (IBM Corp., Armonk, NY, USA) was used for analysis and graphic presentations. Continuous variables were expressed as mean and standard deviation, or as median and interquartile range (IQR), depending on the distribution of data. Accordingly, they were compared by parametric (unpaired Student T) or non-parametric (Mann-Whitney U) tests, respectively. Survival curves were generated by the Kaplan-Meier method and compared by the log-rank test. Confidence intervals (CI) were set at 95%. Where relevant, 2-sided p-values < 0.05 were considered as statistically significant.
3. Results
3.1. Study Population
The study population is composed of 128 consecutive patients (mean age 41 ± 9 years, males 70%) undergoing EST at least six months after myocarditis. Patient selection process and excluded cases are shown in Figure 1.
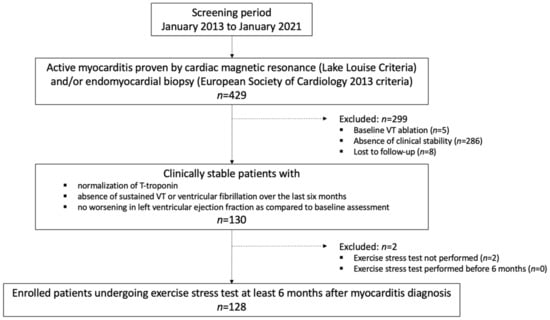
Figure 1.
Patient selection. The study flowchart is shown to highlight the selection of the 128 patients undergoing an exercise stress test. VT = ventricular tachycardia.
Of the 128 included patients, 64 (50%) presented with VA, namely VF/sustained VT in n = 32, NSVT in n = 18, and Lown’s grade ≥ 2 VE in n = 14 cases. Within the control group (n = 64), 34 (53%) had ACS-like clinical onset, while the remaining 30 (47%) presented with heart failure (HF). The cohort included up to 37 athletes (29%) who were previously eligible for agonistic sports practice. Overall, myocarditis was proven by CMR in 97 cases (76%, mainly nonarrhythmic), and by EMB in 116 (91%, mainly arrhythmic). Eighty-five patients (66%) had a diagnosis confirmed by both techniques. There were no cases of COVID-19-associated myocarditis. Patients were discharged from the hospital after 11 ± 4 days. Complete baseline characterization of the population and treatment strategies is shown in Table 1. Beta-blockers, antiarrhythmics, implantable cardioverter defibrillators, and immunosuppressants were all more commonly used in the arrhythmic group.

Table 1.
Baseline characteristics of population (n = 128).
3.2. EST Results
Complete data about EST are summarized in Table 2. EST was performed on average after 15 ± 4 months from the diagnosis of myocarditis, with a later timing for the arrhythmic group. In addition, patients presenting with VA more commonly were tested on beta-blockers and/or antiarrhythmics (59 vs. 20, respectively, p < 0.001), accounting for lower average exercise performance. Overall, five patients (4%) experienced malignant VA, all of them belonging to the arrhythmic group. The same group showed a significantly higher occurrence of any kind of VA (43 vs. 4 cases, respectively, p < 0.001). Conversely, signs and/or symptoms of myocardial ischemia were more commonly documented in the nonarrhythmic group (6 vs. 1 cases, respectively, p = 0.115). Representative examples of EST findings are shown in Figure 2. Case-by-case management based on EST results is shown in Table 3.

Table 2.
Exercise stress test.
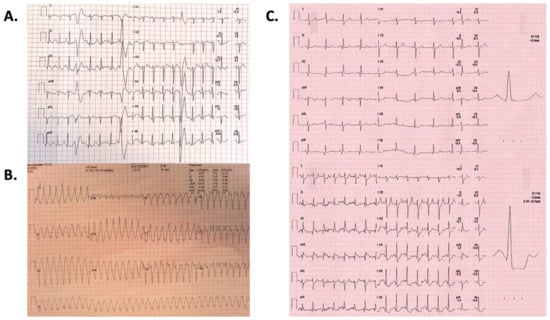
Figure 2.
Exercise stress test findings. Representative examples of remarkable findings on exercise stress tests are shown. (Panel (A)). Female patient, 32-year-old, with evidence of frequent polymorphic ventricular ectopies on the effort at exercise stress test performed 12 months after cardiac magnetic resonance-proven acute myocarditis presenting with nonsustained ventricular tachycardia and syncope. After the exercise stress test, he underwent an endomyocardial biopsy and subsequent immunosuppressive treatment for virus-negative lymphocytic myocarditis. (Panel (B)). Male patient, 44-year-old (P123, Table 3) with evidence of sustained monomorphic ventricular tachycardia causing syncope during an exercise stress test performed late after presentation with arrhythmic myocarditis. The subsequent workup is shown in Table 3. (Panel (C)). Male patient, 68-year-old (P37, Table 3) with exercise stress test showing dynamic ST segment depression in inferolateral leads with ST elevation in lead aVR (exercise peak, bottom; compared to baseline, top). He was asymptomatic for angina or dyspnea. After normal coronary angiography, he had both cardiac magnetic resonance and endomyocardial biopsy with a final diagnosis of chronically active myocarditis from parvovirus B19. Further details are reported in Table 3.

Table 3.
Management of patients with ischemia and malignant VA during exercise stress test.
3.3. Outcomes
After average follow-up of 58 months, 52 patients (41%) experienced adverse events, including cardiac death (n = 3), rehospitalization (n = 37), malignant VA (n = 23) and proven myocarditis (n = 10). The global occurrence of adverse events was 39 (61%) in the arrhythmic vs. 13 (20%) in the nonarrhythmic group (p < 0.001). Event details are shown in Table 4. Remarkably, adverse events occurred more frequently among patients with abnormal EST findings (40/54 vs. 12/74, p < 0.001). As shown by the Kaplan-Meier curves in Figure 3, this difference was observed in both the arrhythmic and nonarrhythmic groups.

Table 4.
Outcomes after exercise stress test.
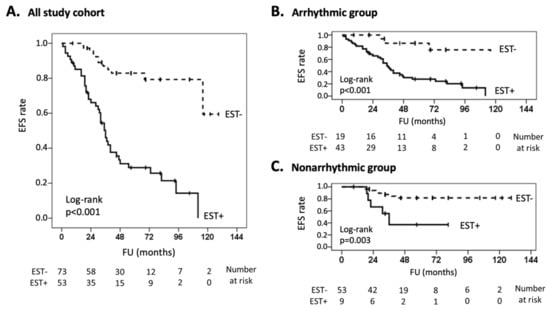
Figure 3.
Outcomes after exercise stress test. Kaplan-Meier curves are shown for the occurrence of adverse events after EST. Adverse events included cardiac death, disease-related hospital readmissions, malignant ventricular arrhythmia (sustained ventricular tachycardia, ventricular fibrillation, appropriate implantable cardioverter defibrillator treatment), and active myocarditis, proven by endomyocardial biopsy or myocardial imaging. For each graph, x-axis indicates follow-up months after EST, and y-axis indicates event-free survival. The continuous line refers to patients with EST positive for ventricular arrhythmia or ischemia (EST+), whereas the dashed line refers to patients with uneventful EST (EST-). Numbers at risk are reported below each chart. Curves are shown for the whole patient cohort (panel (A)) and arrhythmic and nonarrhythmic subgroups (panels (B,C), respectively). EFS = event-free survival; EST = exercise stress test; FU = follow-up.
Of 47 patients with VA documented during EST, 35 (74%) underwent myocarditis restaging either by CMR (n = 19), FDG-PET (n = 15), or EMB (n = 8): prevalence of polymorphic and/or irregular VA during EST were observed in patients with subsequent documentation of active myocarditis (6 of 7), whereas regular and monomorphic VA were more common among patients with no signs of active myocarditis (26 of 28, p < 0.001). Examples are shown in Figure 4.
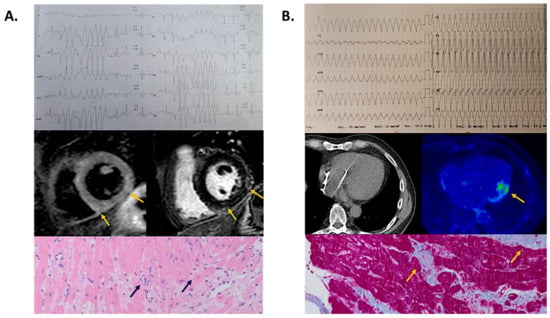
Figure 4.
Relationship between exercise stress test-induced ventricular arrhythmia and myocarditis staging. Representative examples of ventricular arrhythmia features on exercise stress test and subsequent myocarditis restaging are shown. (Panel (A)). Female patient, 40-year-old, with evidence of irregular nonsustained ventricular tachycardia immediately after exercise peak on stress test. She underwent cardiac magnetic resonance showing both T2 short-tau inversion recovery (mid panel, left) and late gadolinium enhancement sequences (mid panel, right) involving the subepicardial layer of the inferolateral left ventricular wall (arrows), fulfilling the Lake Louise criteria for active myocarditis. She underwent an endomyocardial biopsy showing multifocal lymphocytic inflammatory infiltrates (lower panel, arrows) confirming the diagnosis of chronically active virus-negative myocarditis, subsequently treated by immunosuppressants. (Panel (B)). Male patient, 66-year-old (P78, Table 3) with evidence of regular and monomorphic sustained ventricular tachycardia causing syncope during an exercise stress test performed late after presentation with arrhythmic myocarditis. Being an implantable cardioverter defibrillator carrier (mid panel, left), he underwent 18F-Fluorodeoxyglucose positron emission tomography (mid panel, right) with physiological glucose uptake in the mid-lateral left ventricular wall (arrow) and no signs of active myocarditis. Consistently, endomyocardial biopsy (lower panel) showed only replacement fibrosis (arrows) and no signs of persistent myocardial inflammation. He successfully underwent catheter ablation of monomorphic ventricular tachycardia (Table 3).
Among the 33 patients with uneventful EST on treatment, 16 (48%) had beta-blocker withdrawn (2/14 arrhythmic vs. 14/19 nonarrhythmic, p = 0.001) and subsequently underwent EST under off-treatment conditions: there were no cases of inducible ischemia and no major VA. Only two patients, those belonging to the arrhythmic group, required beta-blocker resumption, respectively, because of NSVT and frequent VE. Of the 27 athletes of the cohort, 12 cases (44%), all belonging to the nonarrhythmic group, were readmitted to competitive sports participation.
4. Discussion
4.1. Main Study Findings
We reported the results of EST late after myocarditis in a sizable cohort of patients with a balanced distribution between arrhythmic and nonarrhythmic presentations. We showed that: (1) the occurrence of VA during EST was more common in the arrhythmic presentation, whereas ischemic manifestations were more prevalent in the nonarrhythmic one; (2) in both arrhythmic and nonarrhythmic groups, adverse events occurred more frequently among patients with abnormal EST; (3) EST was an informative technique for the subsequent clinical management of patients with myocarditis.
4.2. EST after Myocarditis: Role of the Clinical Presentation
To the best of our knowledge, we provided the first report comparing the results of EST in patients with arrhythmic and nonarrhythmic myocarditis. Myocarditis was diagnosed by gold standard techniques [2,13,14] and followed at a dedicated outpatient clinic with multidisciplinary facilities [20]. Furthermore, in compliance with the current recommendations [4,5], EST was performed at least six months after acute myocarditis and provided a clinical judgment of stability for at least six months. In keeping with the current knowledge, EST was safe in the nonarrhythmic cohort, where malignant VA was never documented. As opposed, we documented a high prevalence of VA, including five cases of malignant ones, among patients with an arrhythmic presentation. Results are not unexpected, since VA may complicate both the active and the post-inflammatory stages of myocarditis [10,24]. Furthermore, evidence suggests that presentation with malignant VA predicts the subsequent occurrence of arrhythmic events in patients with myocarditis [25]. Our findings suggest that in patients with an arrhythmic presentation of myocarditis, EST should be requested with caution. Regarding inducible ischemia, we identified no patients with detectable abnormalities in epicardial coronary arteries (Table 3). Due to the subsequent diagnosis of chronically active myocarditis in most cases, the observed ST-T changes likely occurred secondary to structural heart disease-associated coronary microvascular dysfunction [26], as already demonstrated in patients with myocarditis secondary to viruses with endothelial tropism like parvovirus B19 [27].
4.3. Significance of EST
Figure 3 shows that the vast majority of adverse events during follow-up occurred in patients with abnormal findings at EST. To be noted, a number of known prognostic factors in patients with myocarditis, including male gender [28], LVEF [9], LGE [25], viral genomes [29], and wide QRS complex from left bundle branch block [30] displayed a balanced distribution between groups (Table 1). Also, relevant comorbidities [31,32,33] showed no major differences in arrhythmic vs. nonarrhythmic cases. However, a major difference between groups was found in medical treatment. In particular, beta-blockers and antiarrhythmic agents were largely more prevalent among the arrhythmic patients, who nevertheless experienced a greater rate of adverse events (Table 4).
Table 4 shows that the majority of adverse events occurred in patients with abnormal EST. However, multiple factors might have contributed to our findings. First, the majority of adverse events occurred in the arrhythmic group, which is already known for being associated with worse outcomes [6,7,25]. Second, a non-trivial subset of patients with abnormal EST (7 of 35, 20%) received a diagnosis of active myocarditis following the subsequent disease restaging: this observation suggests that adverse prognostic significance may be carried out by active myocardial inflammation, as previously reported [34]. Beyond any prognostic significance, EST remains an informative technique in daily clinical practice since the new documentation of VA may help identify high-risk patients who warrant treatment upgrade and close follow-up.
4.4. Additional Clinical Implications of EST
Our study was notable for a number of additional findings that may guide the clinical decision-making in patients undergoing EST late after myocarditis. First, the features of VA at 12-lead ECG may be a useful tool to identify the inflammatory stage of myocarditis. Previously, polymorphic and irregular VA was shown to be associated with active-phase myocarditis, whereas monomorphic and regular ones suggested post-inflammatory scar-related VA [24]. This distinction has been proven to turn into relevant differences in treatment strategies, ranging from immunosuppression for the former condition [35] and catheter ablation for the latter one [34]. Overall, the results of the current study are in keeping with this observation (Figure 4) and suggest that persistently active myocarditis could be suspected even in clinically-stable patients who show polymorphic and irregular VA on EST performed late after the acute presentation.
A second relevant point is that a normal EST may guide the withdrawal of medical treatment. In our experience, all nonischemic patients had uneventful EST even later, under off-treatment conditions. Most importantly, all of them had no adverse events during follow-up. These data suggest that, at least in patients with nonarrhythmic presentation and no alternative indications (i.e., heart failure), beta-blockers may be safely interrupted after uneventful EST. These findings are relevant, in particular for young patients requesting readmission to competitive sports participation [4,5], who constituted a non-neglectable subset of our cohort (29%). As opposed, an arrhythmic presentation may constitute a limitation for the subsequent readmission to sports practice. Our data are meant to be preliminary and deserve confirmation by larger, multicenter studies.
4.5. Study Limitations
Our study was single-center and took place at a referral center for arrhythmic myocarditis [18]. This may have led to an overestimation of the prevalence of VA as compared to the classic ACS-like and HF presentations of myocarditis [3]. Considerable overlap between acute and chronically active myocarditis, as well as improved diagnostic yield of modern CMR following the introduction of parametric mapping, constitute additional biases. Continuous electrical monitoring by cardiac devices in many patients allowed greater sensitivity for arrhythmia detection as compared with the classic approach based on repeated Holter ECG [36,37]. Due to the limited sample size, the statistical model allowing assessment of the independent prognostic value for EST was prevented.
5. Conclusions
In this study, we showed that EST, performed late after the clinical onset of myocarditis, is more commonly associated with VA in patients with arrhythmic presentation compared to nonarrhythmic ones. Furthermore, we showed that EST abnormalities are associated with adverse outcomes during subsequent follow-ups in both arrhythmic and nonarrhythmic groups. These preliminary findings suggest that EST should be requested and performed with caution in patients with myocarditis, in particular following the arrhythmic presentation. Confirmatory evidence by larger studies is needed.
Author Contributions
Conceptualization, G.P. and P.M.; methodology, S.G., M.S., C.C., D.V., G.D.L., A.P., A.V., S.R., G.C., M.D.G. and E.B.; software, G.P.; validation, L.G., L.D., C.B., A.E., S.S., P.D.B. and P.M.; formal analysis, G.P., S.S. and A.V.; investigation, G.P., S.G., M.S., C.C., D.V., G.D.L., A.P., A.V., S.R., G.C., M.D.G., E.B., L.G., L.D., C.B., A.E., S.S., P.D.B. and P.M.; resources, L.G., L.D., C.B., A.E., S.S., P.D.B. and P.M.; data curation, G.P., S.G., M.S., C.C., D.V., G.D.L., A.P., A.V., S.R., G.C., M.D.G., E.B. and S.S.; writing—original draft preparation, G.P.; writing—review and editing, S.G., M.S., C.C., D.V., G.D.L., A.P., A.V., S.R., G.C., M.D.G., E.B., L.G., L.D., C.B., A.E., S.S., P.D.B. and P.M.; visualization, S.G., M.S., C.C., D.V., G.D.L., A.P., A.V., S.R., G.C., M.D.G., E.B., L.G., L.D., C.B., A.E., S.S., P.D.B. and P.M.; supervision, L.G., L.D., C.B., A.E., S.S., P.D.B. and P.M.; project administration, P.D.B. and P.M.; funding acquisition, P.D.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of San Raffaele Hospital (MYOCAR, 24/01/2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data supporting the study findings will be made available upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
ACS = acute coronary syndrome; CMR = cardiac magnetic resonance; ECG = electrocardiogram; EMB = endomyocardial biopsy; EST = exercise stress test; FDG-PET = 18F-Fluorodeoxyglucose positron emission tomography; HF = heart failure; ICD = implantable cardioverter defibrillator; IST = immunosuppressive therapy; LGE = late gadolinium enhancement; LLC = Lake Louise criteria; LVEF = left ventricular ejection fraction; NSVT = nonsustained ventricular tachycardia; VA = ventricular arrhythmia; VE = ventricular ectopies; VF = ventricular fibrillation; VT = ventricular tachycardia.
References
- Gibbons, R.J.; Balady, G.J.; Bricker, J.T.; Chaitman, B.R.; Fletcher, G.F.; Froelicher, V.F. ACC/AHA 2002 Guideline Update for Exercise Testing: Summary Article A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation 2002, 106, 1883–1892. [Google Scholar] [CrossRef] [PubMed]
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648. [Google Scholar] [CrossRef] [PubMed]
- Hurwitz, B.; Issa, O. Management and Treatment of Myocarditis in Athletes. Curr. Treat Options Cardiovasc. Med. 2020, 22, 65. [Google Scholar] [CrossRef] [PubMed]
- Pelliccia, A.; Sharma, S.; Gati, S.; Bäck, M.; Börjesson, M.; Caselli, S.; Collet, J.-P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2020, 42, ehaa605. [Google Scholar] [CrossRef]
- Maron, B.J.; Udelson, J.E.; Bonow, R.O.; Nishimura, R.A.; Ackerman, M.J.; Estes, N.M.; Cooper, L.; Link, M.S.; Maron, M.S. Eligibility and Disqualification Recommendations for Competitive Athletes with Cardiovascular Abnormalities: Task Force 3: Hypertrophic Cardiomyopathy, Arrhythmogenic Right Ventricular Cardiomyopathy and Other Cardiomyopathies, and Myocarditis. A Scientific Statement from the American Heart Association and American College of Cardiology. Circulation 2015, 132, e273–e280. [Google Scholar] [CrossRef]
- Modica, G.; Bianco, M.; Sollazzo, F.; Di Murro, E.; Monti, R.; Cammarano, M.; Morra, L.; Nifosì, F.M.; Gervasi, S.F.; Manes Gravina, E.; et al. Myocarditis in Athletes Recovering from COVID-19: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4279. [Google Scholar] [CrossRef]
- Caforio, A.L.; Calabrese, F.; Angelini, A.; Tona, F.; Vinci, A.; Bottaro, S.; Ramondo, A.; Carturan, E.; Iliceto, S.; Thiene, G.; et al. A prospective study of biopsy-proven myocarditis: Prognostic relevance of clinical and aetiopathogenetic features at diagnosis. Eur. Heart J. 2007, 28, 1326–1333. [Google Scholar] [CrossRef]
- Anzini, M.; Merlo, M.; Sabbadini, G.; Barbati, G.; Finocchiaro, G.; Pinamonti, B.; Salvi, A.; Perkan, A.; Di Lenarda, A.; Bussani, R.; et al. Long-Term Evolution and Prognostic Stratification of Biopsy-Proven Active Myocarditis. Circulation 2013, 128, 2384–2394. [Google Scholar] [CrossRef]
- Ammirati, E.; Cipriani, M.; Moro, C.; Raineri, C.; Pini, D.; Sormani, P.; Mantovani, R.; Varrenti, M.; Pedrotti, P.; Conca, C.; et al. Clinical Presentation and Outcome in a Contemporary Cohort of Patients with Acute Myocarditis: Multicenter Lombardy Registry. Circulation 2018, 138, 1088–1099. [Google Scholar] [CrossRef]
- Peretto, G.; Sala, S.; Rizzo, S.; De Luca, G.; Campochiaro, C.; Sartorelli, S.; Benedetti, G.; Palmisano, A.; Esposito, A.; Tresoldi, M.; et al. Arrhythmias in myocarditis: State of the art. Heart Rhythm. 2019, 16, 793–801. [Google Scholar] [CrossRef]
- Lown, B.; Wolf, M. Approaches to sudden death from coronary heart disease. Circulation 1971, 44, 130–142. [Google Scholar] [CrossRef]
- Peretto, G.; Cappelletti, A.M.; Spoladore, R.; Slavich, M.; Rizzo, S.; Palmisano, A.; Esposito, A.; De Cobelli, F.; Margonato, A.; Basso, C.; et al. Right ventricular endomyocardial biopsy in patients with cardiac magnetic resonance showing left ventricular myocarditis. J. Cardiovasc. Med. 2021, 22, 560–566. [Google Scholar] [CrossRef]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; et al. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J. Am. Coll. Cardiol. 2009, 53, 1475–1487. [Google Scholar] [CrossRef]
- Ferreira, V.M.; Schulz-Menger, J.; Holmvang, G.; Kramer, C.M.; Carbone, I.; Sechtem, U.; Kindermann, I.; Gutberlet, M.; Cooper, L.T.; Liu, P.; et al. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations. J. Am. Coll. Cardiol. 2018, 72, 3158–3176. [Google Scholar] [CrossRef]
- Palmisano, A.; Benedetti, G.; Faletti, R.; Rancoita, P.M.V.; Gatti, M.; Peretto, G.; Sala, S.; Boccia, E.; Francone, M.; Galea, N.; et al. Early T1 Myocardial MRI Mapping: Value in Detecting Myocardial Hyperemia in Acute Myocarditis. Radiology 2020, 295, 316–325. [Google Scholar] [CrossRef]
- Priori, S.G.; Blomström-Lundqvist, C.; Mazzanti, A.; Blom, N.; Borggrefe, M.; Camm, J.; Van Veldhuisen, D.J. Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Europace 2015, 17, 1601–1687. [Google Scholar]
- Al-Khatib, S.M.; Stevenson, W.G.; Ackerman, M.J.; Bryant, W.J.; Callans, D.J.; Curtis, A.B.; Deal, B.J.; Dickfeld, T.; Field, M.E.; Fonarow, G.C.; et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Heart Rhythm 2018, 15, e190–e252. [Google Scholar] [CrossRef]
- Peretto, G.; Sala, S.; Della Bella, P. Diagnostic and therapeutic approach to myocarditis patients presenting with arrhythmias. G. Ital. Cardiol. 2020, 21, 187–194. [Google Scholar] [CrossRef]
- De Luca, G.; Campochiaro, C.; Sartorelli, S.; Peretto, G.; Dagna, L. Therapeutic strategies for virus-negative myocarditis: A comprehensive review. Eur. J. Intern. Med. 2020, 77, 9–17. [Google Scholar] [CrossRef]
- Peretto, G.; De Luca, G.; Campochiaro, C.; Palmisano, A.; Busnardo, E.; Sartorelli, S.; Barzaghi, F.; Cicalese, M.P.; Esposito, A.; Sala, S. Telemedicine in myocarditis: Evolution of a mutidisciplinary “Disease Unit” at the time of COVID-19 pandemic. Am. Heart J. 2020, 229, 121–126. [Google Scholar] [CrossRef]
- Peretto, G.; Busnardo, E.; Ferro, P.; Palmisano, A.; Vignale, D.; Esposito, A.; De Luca, G.; Campochiaro, C.; Sartorelli, S.; De Gaspari, M.; et al. Applications of FDG-PET scan in arrhythmic myocarditis. J. Am. Coll. Cardiol. Imaging 2022. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Bires, A.M.; Lawson, D.; Wasser, T.E.; Raber-Baer, D. Comparison of Bruce treadmill exercise test protocols: Is ramped Bruce equal or superior to standard bruce in producing clinically valid studies for patients presenting for evaluation of cardiac ischemia or arrhythmia with body mass index equal to or greater than 30? J. Nucl. Med. Technol. 2013, 41, 274–278. [Google Scholar] [PubMed]
- Kharabsheh, S.M.; Al-Sugair, A.; Al-Buraiki, J.; Farhan, J. Overview of Exercise Stress Testing. Ann. Saudi Med. 2006, 26, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Peretto, G.; Sala, S.; Rizzo, S.; Palmisano, A.; Esposito, A.; De Cobelli, F.; Campochiaro, C.; De Luca, G.; Foppoli, L.; Dagna, L.; et al. Ventricular Arrhythmias in Myocarditis: Characterization and Relationships with Myocardial Inflammation. J. Am. Coll. Cardiol. 2020, 75, 1046–1057. [Google Scholar] [CrossRef]
- Gentile, P.; Merlo, M.; Peretto, G.; Ammirati, E.; Sala, S.; Della Bella, P.; Aquaro, G.D.; Imazio, M.; Potena, L.; Campodonico, J.; et al. Post-discharge arrhythmic risk stratification of patients with acute myocarditis and life-threatening ventricular tachyarrhythmias. Eur. J. Heart Fail. 2021, 23, 2045–2054. [Google Scholar] [CrossRef]
- Camici, P.G.; d’Amati, G.; Rimoldi, O. Coronary microvascular dysfunction: Mechanisms and functional assessment. Nat. Rev. Cardiol. 2015, 12, 48–62. [Google Scholar] [CrossRef]
- Schmidt-Lucke, C.; Zobel, T.; Schrepfer, S.; Kuhl, U.; Wang, D.; Klingel, K.; Becher, P.M.; Fechner, H.; Pozzuto, T.; Van Linthout, S.; et al. Impaired Endothelial Regeneration Through Human Parvovirus B19-Infected Circulating Angiogenic Cells in Patients with Cardiomyopathy. J. Infect. Dis. 2015, 212, 1070–1081. [Google Scholar] [CrossRef]
- Peretto, G.; Sala, S.; Basso, C.; Della Bella, P. Programmed ventricular stimulation in patients with active vs previous arrhythmic myocarditis. J. Cardiovasc. Electrophysiol. 2020, 31, 692–701. [Google Scholar] [CrossRef]
- Schultheiss, H.-P.; Baumeier, C.; Aleshcheva, G.; Bock, C.-T.; Escher, F. Viral Myocarditis-From Pathophysiology to Treatment. J. Clin. Med. 2021, 10, 5240. [Google Scholar] [CrossRef]
- Ukena, C.; Mahfoud, F.; Kindermann, I.; Kandolf, R.; Kindermann, M.; Böhm, M. Prognostic electrocardiographic parameters in patients with suspected myocarditis. Eur. J. Heart Fail. 2011, 13, 398–405. [Google Scholar] [CrossRef]
- Peretto, G.; Basso, C.; Della Bella, P.; Sala, S. Thyroid dysfunction in adult patients with biopsy-proved myocarditis: Screening and characterization. Eur. J. Intern. Med. 2020, 71, 98–100. [Google Scholar] [CrossRef]
- Peretto, G.; Sala, S.; Camaschella, C. Iron deficiency in chronic myocarditis: Assessment and prognostic significance. Eur. J. Intern. Med. 2021, 89, 129–131. [Google Scholar] [CrossRef]
- Peretto, G.; Sala, S.; De Luca, G.; Campochiaro, C.; Sartorelli, S.; Cappelletti, A.M.; Rizzo, S.; Palmisano, A.; Esposito, A.; Margonato, A.; et al. Impact of systemic immune-mediated diseases on clinical features and prognosis of patients with biopsy-proved myocarditis. Int. J. Cardiol. 2019, 280, 110–116. [Google Scholar] [CrossRef]
- Peretto, G.; Sala, S.; Basso, C.; Rizzo, S.; Radinovic, A.; Frontera, A.; Limite, L.R.; Paglino, G.; Bisceglia, C.; De Luca, G.; et al. Inflammation as a Predictor of Recurrent Ventricular Tachycardia After Ablation in Patients with Myocarditis. J. Am. Coll. Cardiol. 2020, 76, 1644–1656. [Google Scholar] [CrossRef]
- Peretto, G.; Sala, S.; De Luca, G.; Marcolongo, R.; Campochiaro, C.; Sartorelli, S.; Tresoldi, M.; Foppoli, L.; Palmisano, A.; Esposito, A.; et al. Immunosuppressive therapy and risk stratification of patients with myocarditis presenting with ventricular arrhythmias. JACC Clin. Electrophysiol. 2020, 6, 1221–1234. [Google Scholar] [CrossRef]
- Cooper, L.T., Jr. Ventricular Arrhythmias and Sudden Cardiac Death in Lymphocytic Myocarditis. J. Am. Coll. Cardiol. 2020, 75, 1058–1060. [Google Scholar] [CrossRef]
- Peretto, G.; Mazzone, P.; Paglino, G.; Marzi, A.; Tsitsinakis, G.; Rizzo, S.; Basso, C.; Della Bella, P.; Sala, S. Continuous Electrical Monitoring in Patients with Arrhythmic Myocarditis: Insights from a Referral Center. J. Clin. Med. 2021, 10, 5142. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).