Abstract
Objective: This systematic review evaluated the effects of body weight strength training (BWST) on cognitive function and health-related quality of life (HRQoL) in apparently healthy older people compared with active/inactive control groups. Methods: A literature search was conducted in six databases: PubMed, Web of Science, Scopus, ScienceDirect, EBSCOhost, and PsycINFO. The PRISMA, TESTEX, RoB 2, and GRADEpro tools were used to assess the methodological quality and certainty of evidence. The protocol was registered in PROSPERO (code: CRD42024623038). Results: Among the 27,241 records, 9 randomized controlled trials involving 682 (85% women) apparently healthy older people were included. Compared with the active/inactive control groups, the BWST resulted in significant improvements in orientation to place, language, visuospatial ability, processing speed, attention, and short-term memory. Within-group improvements were observed in general cognitive function and health-related anxiety scores in both the BWST and active control groups. The calculation and set shifting improved only within the BWST group. Conclusions: The individual results of the RCTs suggest that BWST may have potential effects on cognitive function and HRQoL in apparently healthy older people. Nevertheless, the certainty of evidence was insufficient to support definitive recommendations. Therefore, further high-quality studies are needed to establish solid conclusions.
1. Introduction
Cognitive function refers to mental processes that enable humans to perceive, interpret, and interact with their environment, involving multiple cognitive domains, which are susceptible to decline with advancing age [,,], which may lead to changes in motor function and increased fall risk in physically inactive older people [,]. In contrast, meeting international physical activity recommendations, which suggest between 150 and 300 min of moderate-intensity physical activity or between 75 and 150 min of vigorous-intensity physical activity per week [], would lead toward a physically active and healthy lifestyle during aging [,]. Significant benefits in cognitive function, mainly in processing speed, memory, non-verbal reasoning, problem solving, orientation, short-term memory, and attention [,,,], and in core components of executive functions (i.e., working memory, inhibitory control, and cognitive flexibility) are observed in apparently healthy older people [], which are critical for functional independence in activities of daily living and improved health-related quality of life (HRQoL) [].
In this context, several physical activity strategies such as cardiorespiratory fitness [], strength training [,], mind–body training [] and multicomponent training [] have been shown to be effective non-pharmacological treatment interventions to counteract cognitive decline and improve mental health []. Their benefits are largely attributed to the modulation of neurotransmitter activity and the upregulation of neurotrophic factors, which promote synaptic plasticity, neuro-genesis, and cell survival []. A meta-analysis conducted by Gallardo-Gómez et al. [] revealed that low doses of strength training (529 metabolic equivalent task METs-min; 3 sessions of 40 min without considering warm-up and cool-down) per week could significantly improve cognitive function compared with other training methods in apparently healthy older people. Furthermore, minimal equipment strength training, such as that using elastic bands [,] or body weight exercises [], provides adaptable and accessible options, obtaining benefits mainly in muscle strength, which could be an important physical fitness marker in age-related cortical and subcortical neurodegeneration with implications in specific cognitive domains, such as spatial working memory, cognitive flexibility [], executive function and global cognitive function, in apparently healthy older people [].
Similarly, loss of muscle strength in the upper and lower body increases the probability of presenting a low HRQoL in apparently healthy older people []. This multidimensional concept closely related to general health status could directly benefit from strength training in older people []. A meta-analysis by Hart and Buck [] reported that after 8 weeks of strength training in older people, HRQoL improved in mental dimensions (including emotional role, mental health, vitality, and social function) and physical dimensions (such as body pain, general health, physical role, and physical function). Consequently, strength training—including body weight–based protocols—has proven effective in promoting physical, psychological, and social well-being in apparently healthy older people [,]. Despite this evidence, no systematic review has synthesized experimental studies (randomized or non-randomized controlled trials) evaluating the effects of body weight strength training (BWST) on cognitive function and HRQoL in apparently healthy older people. Addressing this gap could advance understanding in the fields of physical activity and health sciences while providing healthcare professionals with evidence-based guidance on the use of BWST. Therefore, this systematic review aimed to evaluate the available body of published peer-reviewed articles related to the effects of BWST on cognitive function and HRQoL in apparently healthy older people compared with active/inactive control groups.
2. Materials and Methods
2.1. Protocol and Registration
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines []. The review protocol was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO; ID code: CRD42024623038).
2.2. Eligibility Criteria
Studies were eligible if they were original, peer-reviewed articles published up to September 2025, without restrictions on language or publication date. Excluded records comprised conference abstracts, book chapters, editorials, letters, protocol registrations, reviews, case reports, and trials not meeting original research criteria. The Population, Intervention, Comparator, Outcome, and Study design (PICOS) framework guided study selection (Table 1).

Table 1.
Selection criteria used in the systematic review.
2.3. Information and Database Search Process
The literature search was conducted between November 2024 and September 2025 across six major databases: PubMed/MEDLINE, Web of Science (core collection), Scopus, ScienceDirect, EBSCOhost, and PsycINFO (American Psychological Association). Medical subject headings (MeSH) from the National Library of Medicine of the United States of America use free language terms related to BWST, cognitive function, HRQoL and older people. The search string used was as follows: (“body weight resistance training” OR “body-weight resistance training” OR “body weight” OR “body weight training” OR “calisthenics” OR “resistance training” OR “strength training” OR “high intensity interval training” OR “progressive resistance training” OR “aerobic interval training” OR “high-intensity interval training” OR “moderate-intensity continuous training”) AND (“cognition” OR “cognition functions” OR “executive functions” OR “executive control” OR “cognitive functioning” OR “cognitive control” OR “cognitive functions” OR “cognitive function” OR “memory” OR “cognitive abilities” OR “global cognition” OR “mental flexibility” OR “memory functioning” OR “executive function” OR “short-term memory” OR “long-term memory” OR “cognitive” OR “neurocognition” OR “neurocognitive” OR “neuro-cognition” OR “neuro-cognitive” OR “executive functioning” OR “brain” OR “brain function” OR “brain structure” OR “brain development” OR “cognitive performance” OR “language”) AND (“QoL” OR “HRQoL” OR “quality of life” OR “quality of life perception” OR “health related quality of life” OR “health-related quality of life” OR “mental health” OR “psychological health” OR “body image perception” OR “life satisfaction” OR “lifestyle” OR “healthy lifestyle” OR “psychological well-being” OR “emotional well-being” OR “health status” OR “health status indicators” OR “vitality”) AND (“elderly” OR “older adults” OR “older people” OR “older subject” OR “older participants” OR “aging” OR “ageing” OR “aged”). The lists of eligible and excluded studies were independently reviewed by two experts, both of whom hold doctorates in sports science and have peer-reviewed publications in journals indexed in the Journal Citation Reports® on physical activity or sports science. To avoid bias, the original search strategy was not provided to the reviewers. Following this step, on 11 September 2025, a search was conducted for errata and retractions related to the studies included in the same databases.
2.4. Study Selection and Data Collection Process
The studies were managed using Mendeley Reference Manager (version 1.19.8). Two reviewers (Á.L.C. and P.A.-S.) independently performed the literature search, removed duplicates, screened titles and abstracts, and assessed the full texts for eligibility. No discrepancies were found at this stage. The process was repeated for searches within reference lists and suggestions provided by external experts. The full texts of potentially eligible studies were subsequently reviewed, and the reasons for excluding those studies that did not meet the selection criteria were reported.
2.5. Methodological Quality Assessment
Study quality was appraised using the TESTEX scale, a 15-point instrument tailored for exercise interventions (5 points for methodological rigor and 10 points for reporting completeness) []. Two independent reviewers (Á.L.C. and P.A.-S.) performed the evaluations, while a third author (J.H.-M.) served as a referee for ambiguous situations, subsequently validated by another author (P.V.-B.).
2.6. Data Synthesis
Data synthesis consisted of systematically presenting the characteristics and results of the included studies. The variables included publication details (author, year, country), study characteristics (design, baseline health status, sample size, mean age), intervention and comparator information (exercise modality, training volume, intensity), data collection instruments for cognitive function and HRQoL, and main outcomes expressed as means and standard deviations.
2.7. Risk of Bias in Individual Studies
Risk of bias was independently evaluated by two reviewers (Á.L.C. and E.V.-C.) using the Cochrane RoB 2 tool as described in the Cochrane Handbook for Systematic Reviews of Interventions []. A third reviewer (J.H.-M.) resolved discrepancies. Assessed domains included: randomization process, deviations from intended interventions, missing outcome data, measurement of outcomes, and selective reporting. Each domain for every study was rated as “low risk,” “some concerns,” or “high risk,” and the overall distribution of risk judgments across domains was summarized graphically as percentages [].
2.8. Summary Measures for the Meta-Analysis
The study protocol called for a meta-analysis, the full details of which are available from PROSPERO, registration code: CRD4202462623038. Nevertheless, the limited number of RCTs and the heterogeneity of the instruments used to assess cognitive function and HRQoL made it difficult to perform a meta-analysis.
2.9. Certainty of Evidence
The overall certainty of evidence was evaluated using the GRADEpro (Grading of Recommendations, Assessment, Development, and Evaluation) framework, categorizing evidence levels as high, moderate, low, or very low []. Since only RCTs were included, the initial rating was high but could be downgraded when concerns arose regarding risk of bias, inconsistency, imprecision, indirectness, or potential publication bias. Two reviewers (Á.L.C. and E.V.C.) independently performed the assessments, and any disagreements were resolved through consensus with a third reviewer (J.H.M.).
3. Results
3.1. Study Selection
As illustrated in Figure 1, the initial search yielded 27,241 records. After duplicate removal and title/abstract/keyword screening, 25,618 records remained. Subsequent evaluation excluded 25,119 articles for not meeting the eligibility criteria, leaving 499. Consequently, three studies were excluded because the texts were not accessible (authors of inaccessible studies were contacted and asked for a copy of their manuscript, with an estimated maximum response time of 30 days). In the subsequent analysis phase, 109 strength training intervention studies involving implementation, 316 descriptive studies, 15 intervention studies involving unhealthy older people, 7 studies involving people under 60 years of age, 38 reviews, and 2 studies without a control group were excluded. After this process, nine studies met all the selection criteria [,,,,,,,,].
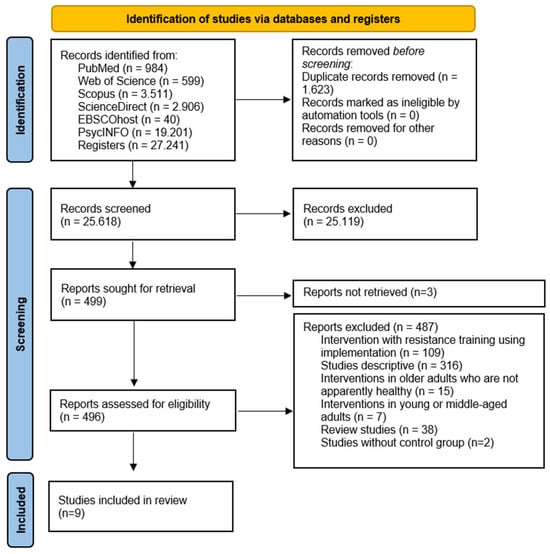
Figure 1.
Flowchart of the review process. Legends: Based on the PRISMA guidelines [].
3.2. Methodological Quality
All nine included trials were appraised using the TESTEX instrument (Table 2). All studies achieved a score equal to or above 60% on the scale, namely, 9/15 [,,,,], and 11/15 [,,,], representing at least 60% compliance with the methodological criteria. Therefore, no studies were excluded based on the TESTEX results.

Table 2.
Methodological quality assessment of the studies according to the TESTEX scale.
3.3. Risk of Bias Within Studies
One study was evaluated as having a minimal risk of bias [], while four studies exhibited certain issues [,,,]. Four studies were categorized as possessing a significant risk of bias [,,,]. This indicates a moderate risk of bias, as the majority of research presented certain problems, while one showed a high risk. Figure 2 and Figure 3 summarize the evaluations of bias risk.
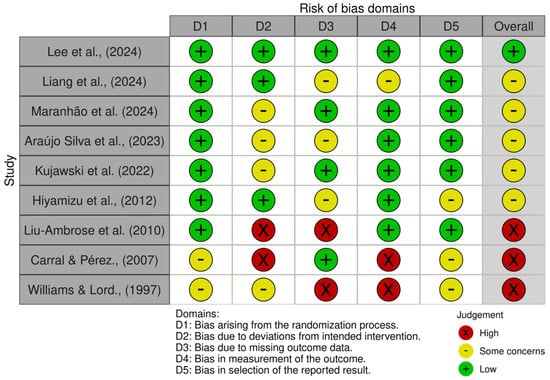
Figure 2.
Risk of bias tools: traffic lights chart [,,,,,,,,].
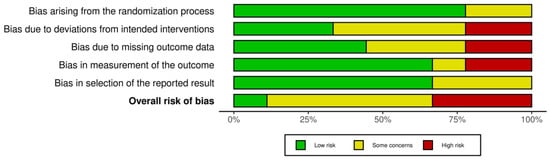
Figure 3.
Risk of bias tools: Summary chart by domain.
3.4. Study Characteristics
The variables analyzed in the nine selected studies are listed in Table 3. One study was conducted in South Korea [], one in the United Kingdom [], two in Brazil [,], one in Poland [], one in Japan [], one in Canada [], one in Spain [] and one in Australia []. All nine studies were RCTs [,,,,,,,,].

Table 3.
Studies report the effects of body weight strength training on cognitive function and health-related quality of life in apparently healthy older people.
3.5. Sample Characteristics
The nine studies presented 27 to 187 participants [,,,,,,,,]. Consequently, the cumulative sample size in all these studies involved 682 (85% female) apparently healthy older people with a mean age of 70 years [,,,,,,,,].
3.6. Dosing and Conducted Interventions
Intervention durations ranged from 5 to 42 weeks [,,,,,,,,], with 2 to 7 sessions per week of 10 to 60 min [,,,,,,,,]. The number of exercises ranged from 1 to 4 stimulating large muscle groups of the lower body, such as the quadriceps, abductors, hamstrings, and gastrocnemius [,,,,], 1 to 2 exercises stimulating upper body large muscle groups, such as the pectorals and deltoids, and one core exercise [,,,,]. Four studies did not report the number of exercises [,,,]. In addition, 4 studies reported the number of sets and repetitions, ranging from 2 to 3 sets of 8 to 12 repetitions, with a rest 1 min between each set [,,]. One study described the duration of the intervention as a function of time, specifying that each exercise was extended for 1 min with a 1 min rest between exercises []. Five studies did not report the number of sets and repetitions [,,,,]. On the other hand, one study reported that the intensity of the sessions was assessed via the Borg Perception of Exertion (RPE) scale and the resting heart rate [], whereas 8 studies did not provide this information [,,,,,,,].
Regarding the control groups, 3 studies included active control groups with BWST interventions lasting 12 weeks, ranging from 2 to 3 sessions of 20 to 60 min per week [,,]. Two studies reported 4 exercises for the lower body (sitting to stand, standing hip abduction, pelvic elevation and plantar flexion) and 3 exercises for the upper body (wall push-ups, supine abdominal and unilateral infra-abdominal), with 2 sets of 8 to 10 repetitions and a rest of 1 min between sets [,]. In the case of Hiyamizu et al. [], the control group performed 2 exercises for the lower body (sitting to stand and wall squats using 1 or 2 legs) and 1 exercise for the upper body (wall push-ups), without reporting the number of sets and repetitions. On the other hand, 3 studies reported active control groups using bodybuilding machines, the duration of the interventions ranged from 5 to 52 weeks, with 2 to 3 sessions per week [,,]. In addition, the number of exercises ranged from 2 to 6, stimulating large muscle groups of the lower body, such as quadriceps, hamstrings, gastrocnemius, and adductors, and 3 exercises stimulating large muscle groups of the upper body, such as biceps, triceps, deltoids, latissimus dorsi and pectorals, and 1 core exercise [,]. Only one study did not report the number of exercises []. Two studies reported the number of sets and repetitions, ranging from 2 to 4 sets of 6 to 15 repetitions [,]. Only one study reported a 45 s rest between each set []. Meanwhile, one study did not report the number of sets and repetitions []. In contrast, 3 studies reported inactive control groups without intervention and continued with their activities of daily living [,,].
3.7. Cognitive Function
The selected studies did not qualify for meta-analysis due to the heterogeneity of the assessments used to measure cognitive function. Nevertheless, individual results by Lee et al. [] reported improvements in orientation to place (p < 0.05), language, and visuospatial ability (p = 0.02) in favor of the BWST compared with the active control group, whereas attention and calculation only reported within-group improvements in the BWST (p = 0.04), as assessed by the Mini-Mental State Examination. Kujawski et al. [] observed improvements in visual information processing speed in favor of the BWST compared to the active control group (p = 0.02) and within-group improvements (p = 0.01), as assessed by the Simple Reaction Time, whereas set shifting only reported within-group improvements in the BWST (p = 0.04), as assessed by the Trail Making test. Hiyamizu et al. [] reported improvements in attention in favor of the BWST compared with the active control group (p = 0.04), as assessed by the Stroop test with a dual task. Carral and Pérez [] reported within-group improvements in the general cognitive function score in both the BWST (p = 0.03) and active control group (p = 0.02), as assessed by the Mini-Mental State Examination. Williams and Lord [] reported improvements in short-term memory in favor of the BWST (p = 0.02) compared with the inactive control group, as assessed by the Digit Span test of the Wechsler Adult Intelligence Scale-Revised. On the other hand, Maranhão et al. [] reported improvements in inhibitory control (p = 0.03) in favor of the active control group compared to the BWST as assessed by the Stroop test. Meanwhile, Liu-Ambrose et al. [] reported a decrease in selective attention and conflict resolution in the BWST compared to active control groups (p < 0.05) as assessed by the Stroop test.
3.8. Health-Related Quality of Life (HRQoL)
The selected studies did not qualify for meta-analysis because of the heterogeneity of the assessments used to measure HRQoL. However, Daniele de Araújo Silva et al. [] reported improvements in the dimensions of past, present, and future activities, social participation, intimacy, and general score of HRQoL in favor of the active control group compared to the BWST (p < 0.05), as assessed by the World Health Organization Quality of Life questionnaire for older people. On the other hand, Carral and Pérez [] reported within-group improvements in components related to HRQoL, specifically health-related anxiety, in both the BWST (p = 0.04) and in the active control group (p = 0.04), as assessed by the Health Orientation Scale. In contrast, Liang et al. [] did not observe significant differences between the BWST and the inactive control group in the dimensions of physical health (p = 0.28), mental health (p = 0.38), and general (p = 0.68) HRQoL scores, as assessed by the five-dimensional, five-level EuroQol questionnaire and the Short Form Health Survey-36.
3.9. Certainty of Evidence
The GRADE evaluation of the available trials indicated that, although the intervention demonstrated benefits in cognitive function and HRQoL, it was not possible to precisely estimate the relative effect. The certainty of evidence was rated as moderate, primarily limited by concerns about risk of bias, while consistency, applicability, and precision did not raise major concerns. Overall, these findings are considered clinically relevant and support the value of the intervention, yet they underscore the need for future studies with more rigorous designs to confirm and quantify its true effect (Table 4).

Table 4.
Methodological quality assessment via the GRADEpro tool.
3.10. Adherence and Adverse Events
The studies reported adherence rates of 100% [], 90% [], 72% [], 62% [] and 60% [,]. Three studies did not report with BWST [,,].
Regarding adverse events, only one study reported musculoskeletal complaints in 9.5% of participants and one fall without injury during the intervention with BWST []. Meanwhile, 6 studies reported adverse events unrelated to the intervention with BWST, including stroke, death, falls [] and other health problems [,,,,,]. Two studies reported no adverse events during the intervention with BWST [,]. On the other hand, the main reasons for dropping out were personal problems, health issues, failure to meet the minimum attendance requirements for training sessions, and withdrawal of informed consent [,,,,,,,]. Only one study reported that none of the participants dropped out of the intervention with BWST [].
4. Discussion
This systematic review aimed to evaluate the available body of published peer-reviewed articles related to the effects of BWST on cognitive function and HRQoL in apparently healthy older people compared with active/inactive control groups. After 27,241 records were reviewed, 9 RCTs involving 682 (85% women) older people were included. All selected studies scored 60% or higher on the TESTEX methodological scale. The heterogeneity observed in the assessments to measure cognitive function and HRQoL limited the possibility of performing a meta-analysis. Nevertheless, the results of the individual studies indicate that, compared with the active/inactive control groups, the BWST resulted in significant improvements in orientation to place, language, visuospatial ability, processing speed, attention, and short-term memory. Within-group improvements were observed in general cognitive function and health-related anxiety scores in both the BWST and active control groups. The calculation and set shifting improved only within the BWST group. In contrast, inhibitory control, the dimensions of past, present, and future activities, social participation, intimacy, and general HRQoL scores improved in the active control group.
4.1. Cognitive Function
The results of the studies analyzed reported moderate certainty of evidence with significant improvements in different areas of cognitive function in the BWST [,,,,]. These findings are consistent with the study by Sanchez-Lastra et al. [] reported that institutionalized older people improved their general cognitive function score (p = 0.008) and attention (p = 0.031) after 12 weeks of upper and lower body strength training. Similarly, the study by Coetsee and Terblanche [] in apparently healthy older people after 16 weeks physical training in three different modalities (strength, moderate continuous aerobic, and high-intensity aerobic interval), reported that the strength training group achieved greater within-group improvements in processing speed compared with the moderate continuous aerobic training group (15.05%, ES = 1.00 vs. 6.33%, ES = 0.69; p < 0.05), and greater within-group improvements in executive function compared to the high-intensity aerobic interval training group (48.43%, ES = 1.07 vs. 20.85%, ES = 0.45; p < 0.05), as assessed by the Stroop test. However, a meta-analysis by Xiong et al. [] in apparently healthy older people reported that aerobic training results in better executive function, specifically working memory (Hedge’s g = 0. 098, 95% CI = 0.017–0.178; p = 0.017, I2 = 0%), inhibitory control (Hedge’s g = 0.136; 95% CI = 0.053–0.218; p = 0.001, I2 = 0%), and cognitive flexibility (Hedge’s g = 0.566; 95% CI = 0.135–0.997; p = 0.010, I2 = 0%) compared with strength and mind–body training, results that were primarily assessed by the Digit Span test, N-back task, Task switching, Trail making test, Wisconsin card sorting test, and Stroop test. Both types of training are highly effective in improving cognitive function because of their ability to increase blood flow and the oxygen supply to brain tissue, preventing the neurodegenerative process associated with aging []. Strength training stands out for requiring a lower weekly exercise dose (529 METs-min; 3 sessions of 40 min of moderate intensity without considering warm-up and cool-down) to obtain clinically significant benefits in cognitive function compared with aerobic activities (758 METs-min; 4 sessions of 45 min of moderate intensity without considering warm-up and cool-down) [], thus aligning with the minimum international physical activity recommendations (600 METs-min) for healthy brain aging [,].
Furthermore, strength training combined with cognitive training (simultaneous dual-task training) in apparently healthy older people also yielded promising results. Hiyamizu et al. [] reported significant improvement in attentional cognitive function after 12 weeks of BWST combined with cognitive tasks of calculation, visual search and verbal fluency compared with the control group performing only BWST (p = 0.04). Similarly, Castano et al. [] reported that after 16 weeks of strength training combined with a verbal fluency cognitive task (2 sessions of 60 min per week), in which older people were required to mention aloud as many words as possible from a specific category (e.g., countries, colors, transportation) in each set of exercises, improved verbal fluency and short-term memory (p < 0.05). In contrast to the group that only performed conventional strength training without obtaining better results in these variables, according to the Scenery Picture Memory, semantic, and phonological tests []. These findings suggest that the BWST [,] combined with simultaneous cognitive training [], could induce changes in brain neuroplasticity mediated by brain-derived neurotrophic factor, leading to significant improvements in physical performance and cognitive function in apparently healthy older people [,,].
4.2. Health-Related Quality of Life (HRQoL)
The results of the studies analyzed reported moderate certainty of evidence with significant improvements in components associated with HRQoL [,]. Similarly, a study by Juesas et al. [] in apparently healthy older people reported that, compared to inactive control group, the strength training group had improvements in dimensions of social function (p < 0.001), mental health (p = 0.009), vitality (p < 0.001), and general health scores (p < 0.001) of HRQoL, as assessed the SF-36 questionnaire after 16 weeks of strength training intervention. Likewise, a meta-analysis by Khodadad Kashi et al. [] in apparently healthy older people reported that strength training improved in dimensions of physical function (SMD = 0.31, 95% CI = 0.04–0.57; p = 0.02), mental health (SMD = 0.44; 95% CI = 0.17–0.71; p = 0.001; I2 = 66%; p < 0.0001), body pain (SMD = −0.52; 95% CI = −0.87–−0.16; p = 0.004), general health (SMD = 0.43; 95% CI = 0.16–0.70; p = 0.002), and social function (SMD = 0.25; 95% CI = 0.07–0.42; p = 0.006) of HRQoL, results obtained mainly from the SF-36, SF-12, SF-8, WHOQOL-BREF, and WHOQOL-OLD assessments. In turn, reports improved upper (MD, 15.26 kg; 95% CI, 5.51–25.00; p = 0.002) and lower (MD, 48.46 kg; 95% CI, 6.53–90.39; p = 0.02) body muscle strength []. These results may be due to an association between HRQoL and physical fitness. Valdés-Badilla et al. [] noted that apparently healthy older people with low performance in lower (OR = 1.11; p = 0.001) and upper (OR = 1.07; p = 0.003) body muscle strength tests had an increased probability of having a low HRQoL in the physical function dimensions. Similarly, Haraldstad et al. [] reported that 12 weeks of strength training increases lower body muscle strength and upper body lean muscle mass, which are positively correlated with the physical function (p = 0.042) and social function (p = 0.021) dimensions of HRQoL, as assessed by the SF-12 questionnaire. However, Liang et al. [] reported nonsignificant effects on HRQoL after BWST intervention. This could be because the heterogeneity of the instruments used may not be sensitive enough to detect relevant changes in HRQoL after an intervention with BWST in apparently healthy older people. Nevertheless, unconventional physical activity strategies with minimal implementation demonstrate a mean adherence rate >80% and a small (d = 0.49) and moderate (d = 0.72) positive effect size on HRQoL in healthy middle-aged and older people []. Therefore, the BWST could be a cost-efficient alternative, allowing us to counteract risk factors associated with loss of muscle strength, anxiety and depressive symptoms and improving HRQoL in apparently healthy older people [,,].
On the other hand, certain active control groups achieved significant improvements in components of cognitive function and HRQoL compared to the BWST [,,]. These results should be taken with caution because they may be influenced by various factors such as the participants’ previous experience with strength training, which could yield minimal, non-significant benefits in cognitive function and HRQoL [,]. While BWST in these studies [,,] was not designed to achieve large gains in muscle strength, but rather to maintain the functional independence of older people, which could impact potentially significant improvements in cognitive function and HRQoL []. Furthermore, baseline values for cognitive function and HRQoL close to maximum limit the observation of significant room for improvement [,,,].
4.3. Limitations and Strengths
The main limitations of this systematic review include the following: (i) the small number of RCTs and the diversity of instruments used to assess cognitive function and HRQoL, which makes it difficult to perform a meta-analysis of the data; (ii) most of the instruments used to assess cognitive function were originally designed for the clinical diagnosis of cognitive disorders, rather than to assess normative performance []; (iii) reliance on self-reported measures may have influenced the observed effects, as their validation does not eliminate susceptibility to expectation or placebo biases, particularly in BWST interventions, potentially leading to an overestimation of perceived improvements; (iv) most RCTs included small samples composed predominantly of women and recruitment processes that may have attracted highly motivated participants expecting positive outcomes, introducing potential selection bias, reducing the certainty of evidence, and limiting the generalizability of the findings; (v) the HRQoL evidence is less consistent, as only three RCTs provided data and, in some cases, results favored the control group, limiting the strength of conclusions in this domain; (vi) individual results should be interpreted with caution, given that intervention intensity was not consistently reported, while exercise volume, intensity, and type varied considerably, making comparisons inconclusive; (vii) the optimal BWST dosage to maximize cognitive and HRQoL benefits remains unclear; (viii) adherence rates were relatively low in some trials (ranging from 62% to 72%), which may have affected internal validity; and (ix) heterogeneity in control group designs may have contributed to the insufficient certainty of evidence to establish definitive recommendations on BWST, as inactive controls in RCTs are less effective in accounting for placebo or expectation effects, particularly when combined with self-reported outcomes for cognitive function and HRQoL. On the other hand, the strengths of the studies included the following: (i) methodological quality above 60% in the reviewed studies; (ii) methodological procedures of the PRISMA, PROSPERO, TESTEX, RoB 2 and GRADE scales; (iii) use of a core collection of six generic databases (PubMed, Web of Science, Scopus, ScienceDirect, EBSCOhost, PsycINFO); and (iv) analysis of how BWST affects cognitive function and HRQoL in apparently healthy older people.
4.4. Practical Applications
The results of this systematic review suggest that BWST may have positive effects on cognitive function, especially in higher-level cognitive domains such as executive functions, and on HRQoL. According to the findings, a weekly frequency of 2–3 sessions of 20–60 min aligns with previous meta-analysis on the effects of strength training on cognitive function [], HRQoL [], and physical performance [] in apparently healthy older people. Moreover, BWST represents a promising intervention due to its accessibility and low economic cost, making it a viable and easily applicable strategy for physical activity and health professionals in community or home-based settings for apparently healthy older people [,].
4.5. Future Research Directions
It is recommended that upcoming RCTs incorporate more rigorous methodological designs and objective cognitive function assessments complementary to self-reported measures [,], as well as active control groups that minimize potential expectation or placebo biases to yield more accurate results []. Furthermore, greater adherence to BWST programs should be encouraged, which could be achieved through behavioral and motivational strategies such as individualized goal setting, the use of remote monitoring technologies (mobile applications or wearable devices) [], and the implementation of group-based programs that foster social interaction. Replication of findings in high-quality RCTs will contribute to consolidating the evidence on the effects of BWST on cognitive function and HRQoL in apparently healthy older people []. Finally, it is necessary to establish optimal dosage parameters for BWST interventions to ensure consistent benefits for cognitive function and HRQoL. In this regard, the Consensus on Exercise Reporting Template (CERT) provides a standardized framework comprising 16 essential elements that facilitate detailed descriptions of strength training principles, including frequency, intensity, time, and type of exercise implemented in RCTs [,].
5. Conclusions
The individual results of the RCTs suggest that BWST may have potential effects on cognitive function and HRQoL in apparently healthy older people. Nevertheless, the limited number of available RCTs and the observed methodological heterogeneity reduce the certainty of evidence, making it insufficient to support definitive recommendations. BWST appears to be a promising, feasible, and safe intervention for this population. Therefore, further high-quality studies are needed to establish robust conclusions and confirm the preliminary findings.
Author Contributions
Conceptualization, Á.L.C. and P.V.-B.; methodology, Á.L.C., P.A.-S., E.V.-C., J.H.-M. and P.V.-B.; software, Á.L.C., E.V.-C., J.H.-M. and P.V.-B.; validation, B.P.-F., F.C.-N., C.A.-H., T.H.-V., B.H.M.B. and P.V.-B.; formal analysis, Á.L.C., P.A.-S., E.V.-C., J.H.-M. and P.V.-B.; investigation, Á.L.C., P.A.-S., E.V.-C., J.H.-M. and P.V.-B.; resources, Á.L.C., P.A.-S., E.V.-C., J.H.-M. and P.V.-B.; data curation, Á.L.C., P.A.-S., E.V.-C., J.H.-M. and P.V.-B.; writing—original draft preparation, Á.L.C., B.P.-F., P.A.-S., E.V.-C., J.H.-M., F.C.-N., C.A.-H., C.S., T.H.-V., B.H.M.B. and P.V.-B.; writing—review and editing, Á.L.C., B.P.-F., P.A.-S., E.V.-C., J.H.-M., F.C.-N., C.A.-H., C.S., T.H.-V., B.H.M.B. and P.V.-B.; visualization, Á.L.C., B.P.-F., P.A.-S., E.V.-C., J.H.-M., F.C.-N., C.A.-H., C.S., T.H.-V., B.H.M.B. and P.V.-B.; supervision, P.V.-B.; project administration, Á.L.C., P.A.-S. and P.V.-B.; funding acquisition, Á.L.C., P.A.-S., C.S. and P.V.-B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets generated during and/or analyzed during the current review are available from the corresponding author upon reasonable request.
Acknowledgments
The author Á.L.C. acknowledges that his doctoral studies were funded by ANID-Subdirectorate of Human Capital/National Doctorate/2025-21251898.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- Son, J.J.; Arif, Y.; Okelberry, H.J.; Johnson, H.J.; Willett, M.P.; Wiesman, A.I.; Wilson, T.W. Aging modulates the impact of cognitive interference subtypes on dynamic connectivity across a distributed motor network. npj Aging 2024, 10, 54. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.S.; Singer, B.D.; Vaughan, D.E. Molecular and physiological manifestations and measurement of aging in humans. Aging Cell 2017, 16, 624–633. [Google Scholar] [CrossRef] [PubMed]
- Moini, J.; LoGalbo, A.; Ahangari, R. Cognitive functions. In Foundations of the Mind, Brain, and Behavioral Relationships; Moini, J., LoGalbo, A., Ahangari, R., Eds.; Academic Press: London, UK, 2024; pp. 211–228. ISBN 978-0-323-95975-9. [Google Scholar]
- Zhao, Y.; Li, Y.; Wang, L.; Song, Z.; Di, T.; Dong, X.; Song, X.; Han, X.; Zhao, Y.; Wang, B.; et al. Physical Activity and Cognition in Sedentary Older Adults: A Systematic Review and Meta-Analysis. J. Alzheimer’s Dis. 2022, 87, 957–968. [Google Scholar] [CrossRef]
- Kerminen, H.; Marzetti, E.; D’Angelo, E. Biological and Physical Performance Markers for Early Detection of Cognitive Impairment in Older Adults. J. Clin. Med. 2024, 13, 806. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Valdés-Badilla, P.A.; Gutiérrez-García, C.; Pérez-Gutiérrez, M.; Vargas-Vitoria, R.; López-Fuenzalida, A. Effects of Physical Activity Governmental Programs on Health Status in Independent Older Adults: A Systematic Review. J. Aging Phys. Act. 2019, 27, 265–275. [Google Scholar] [CrossRef]
- Vásquez-Carrasco, E.; Gómez, C.S.; Valdés-Badilla, P.; Hernandez-Martinez, J.; Villagrán-Silva, F.; Aravena-Sagardia, P.; Sandoval, C.; Miralles, P.M. Effectiveness of Combined Cognitive Stimulation and Physical Activity Interventions on Activities of Daily Living, Cognitive Function, and Physical Function in Older People with Mild Cognitive Impairment: A Systematic Review with Meta-Analysis. J. Clin. Med. 2025, 14, 2261. [Google Scholar] [CrossRef]
- Kujawski, S.; Kujawska, A.; Kozakiewicz, M.; Jakovljevic, D.G.; Stankiewicz, B.; Newton, J.L.; Kędziora-Kornatowska, K.; Zalewski, P. Effects of Sitting Callisthenic Balance and Resistance Exercise Programs on Cognitive Function in Older Participants. Int. J. Environ. Res. Public Health 2022, 19, 14925. [Google Scholar] [CrossRef]
- Coetsee, C.; Terblanche, E. The effect of three different exercise training modalities on cognitive and physical function in a healthy older population. Eur. Rev. Aging Phys. Act. 2017, 14, 13. [Google Scholar] [CrossRef]
- Erickson, K.I.; Hillman, C.; Stillman, C.M.; Ballard, R.M.; Bloodgood, B.; Conroy, D.E.; Macko, R.; Marquez, D.X.; Petruzzello, S.J.; Powell, K.E. Physical Activity, Cognition, and Brain Outcomes: A Review of the 2018 Physical Activity Guidelines. Med. Sci. Sport Exerc. 2019, 51, 1242–1251. [Google Scholar] [CrossRef] [PubMed]
- Castano, L.A.A.; de Lima, V.C.; Barbieri, J.F.; de Lucena, E.G.P.; Gáspari, A.F.; Arai, H.; Teixeira, C.V.L.; Coelho, H.J.; Uchida, M.C. Resistance Training Combined With Cognitive Training Increases Brain Derived Neurotrophic Factor and Improves Cognitive Function in Healthy Older Adults. Front. Psychol. 2022, 13, 870561. [Google Scholar] [CrossRef]
- Xiong, J.; Ye, M.; Wang, L.; Zheng, G. Effects of physical exercise on executive function in cognitively healthy older adults: A systematic review and meta-analysis of randomized controlled trials: Physical exercise for executive function. Int. J. Nurs. Stud. 2021, 114, 103810. [Google Scholar] [CrossRef]
- Xu, L.; Gu, H.; Cai, X.; Zhang, Y.; Hou, X.; Yu, J.; Sun, T. The Effects of Exercise for Cognitive Function in Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2023, 20, 1088. [Google Scholar] [CrossRef] [PubMed]
- Gallardo-Gómez, D.; del Pozo-Cruz, J.; Noetel, M.; Álvarez-Barbosa, F.; Alfonso-Rosa, R.M.; del Pozo Cruz, B. Optimal dose and type of exercise to improve cognitive function in older adults: A systematic review and bayesian model-based network meta-analysis of RCTs. Ageing Res. Rev. 2022, 76, 101591. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Ni, W.; Zhang, L.; Zhao, M.; Bai, X.; Zhang, S.; Ding, Y.; Yin, H.; Chen, L. Comparative efficacy of various exercise interventions on depression in older adults with mild cognitive impairment: A systematic review and network meta-analysis. Ageing Res. Rev. 2023, 91, 102071. [Google Scholar] [CrossRef]
- Yan, J.; Li, X.; Guo, X.; Lin, Y.; Wang, S.; Cao, Y.; Lin, H.; Dai, Y.; Ding, Y.; Liu, W. Effect of Multicomponent Exercise on Cognition, Physical Function and Activities of Daily Life in Older Adults With Dementia or Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2023, 104, 2092–2108. [Google Scholar] [CrossRef]
- Hernandez-Martinez, J.; Cid-Calfucura, I.; Chiguay, C.; Weinberger, M.; Delgado-Floody, P.; Muñoz-Vásquez, C.; Aristegui-Mondaca, J.; Levín-Catrilao, Á.; Herrera-Valenzuela, T.; Branco, B.H.M.; et al. Effects of elastic band training on body composition and physical performance in older people: A systematic review with meta-analysis. Exp. Gerontol. 2024, 196, 112553. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Lastra, M.A.; Varela, S.; Cancela, J.M.; Ayán, C. Upper versus Lower Body Resistance Exercise with Elastic Bands: Effects on Cognitive and Physical Function of Institutionalized Older Adults. Eur. Geriatr. Med. 2022, 13, 907–916. [Google Scholar] [CrossRef]
- Carral, J.M.C.; Pérez, C.A. Effects of High-Intensity Combined Training on Women over 65. Gerontology 2007, 53, 340–346. [Google Scholar] [CrossRef]
- Coca-Pulido, A.; Solis-Urra, P.; Fernandez-Gamez, B.; Olvera-Rojas, M.; Bellón, D.; Sclafani, A.; Toval, A.; Martín-Fuentes, I.; Bakker, E.A.; Fernández-Ortega, J.; et al. Fitness, Gray Matter Volume, and Executive Function in Cognitively Normal Older Adults: Cross-Sectional Findings From the AGUEDA Trial. Scand. J. Med. Sci. Sports 2024, 34, e14746. [Google Scholar] [CrossRef]
- Li, Z.; Peng, X.; Xiang, W.; Han, J.; Li, K. The effect of resistance training on cognitive function in the older adults: A systematic review of randomized clinical trials. Aging Clin. Exp. Res. 2018, 30, 1259–1273. [Google Scholar] [CrossRef]
- Valdés-Badilla, P.; Alarcón-Rivera, M.; Hernandez-Martinez, J.; Herrera-Valenzuela, T.; Branco, B.H.; Núñez-Espinosa, C.; Guzmán-Muñoz, E. Factors Associated with Poor Health-Related Quality of Life in Physically Active Older People. Int. J. Environ. Res. Public Health 2022, 19, 13799. [Google Scholar] [CrossRef]
- Khodadad Kashi, S.; Mirzazadeh, Z.S.; Saatchian, V. A Systematic Review and Meta-Analysis of Resistance Training on Quality of Life, Depression, Muscle Strength, and Functional Exercise Capacity in Older Adults Aged 60 Years or More. Biol. Res. Nurs. 2022, 25, 88–106. [Google Scholar] [CrossRef]
- Hart, P.D.; Buck, D.J. The effect of resistance training on health-related quality of life in older adults: Systematic review and meta-analysis. Health Promot Perspect 2019, 9, 1–12. [Google Scholar] [CrossRef]
- Daniele de Araújo Silva, J.; Cândido Mendes Maranhão, D.; Machado Ferreira Tenório de Oliveira, L.; Luiz Torres Pirauá, A. Comparison between the effects of virtual supervision and minimal supervision in a 12-week home-based physical exercise program on mental health and quality of life of older adults: Secondary analysis from a randomized clinical trial. Geriatr. Gerontol. Int. 2023, 23, 864–870. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) Approach to Healthy Ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef]
- Smart, N.A.; Waldron, M.; Ismail, H.; Giallauria, F.; Vigorito, C.; Cornelissen, V.; Dieberg, G. Validation of a New Tool for the Assessment of Study Quality and Reporting in Exercise Training Studies: TESTEX. Int. J. Evid. Based. Healthc. 2015, 13, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.X.; Machado, G.C. Clinimetrics: Grading of Recommendations, Assessment, Development and Evaluation (GRADE). J. Physiother. 2021, 67, 66. [Google Scholar] [CrossRef]
- Hiyamizu, M.; Morioka, S.; Shomoto, K.; Shimada, T. Effects of Dual Task Balance Training on Dual Task Performance in Elderly People: A Randomized Controlled Trial. Clin. Rehabil. 2012, 26, 58–67. [Google Scholar] [CrossRef]
- Williams, P.; Lord, S.R. Effects of group exercise on cognitive functioning and mood in older women. Aust. N. Z. J. Public Health 1997, 21, 45–52. [Google Scholar] [CrossRef]
- Lee, J.; Lim, B.-O.; Byeon, J.Y.; Seok, R. Effects of participation in an eight-week, online video body-weight resistance training on cognitive function and physical fitness in older adults: A randomized control trial. Geriatr. Nurs. 2024, 58, 98–103. [Google Scholar] [CrossRef]
- Liang, I.J.; Perkin, O.J.; Williams, S.; McGuigan, P.M.; Thompson, D.; Western, M.J. The Efficacy of 12-Week Progressive Home-Based Strength and Tai-Chi Exercise Snacking in Older Adults: A Mixed-Method Exploratory Randomised Control Trial. J. Frailty Aging 2024, 13, 572–581. [Google Scholar] [CrossRef]
- Maranhão, D.C.M.; de Araújo Silva, J.D.; Farah, B.Q.; Pirauá, N.B.B.; de Araújo, R.C.; Cavalcante, B.R.; Pirauá, A.L.T. Effects of 12-Weeks of Home-Based Exercise Training on Physical and Cognitive Function of Older Adults: Randomized Trial Comparing Virtual Versus Minimal Supervision in the Context of the Covid-19 Pandemic in Brazil. Can. Geriatr. J. 2024, 27, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Liu-Ambrose, T.; Nagamatsu, L.S.; Graf, P.; Beattie, B.L.; Ashe, M.C.; Handy, T.C. Resistance training and executive functions: A 12-month randomized controlled trial. Arch. Intern. Med. 2010, 170, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Herold, F.; Hamacher, D.; Schega, L.; Müller, N.G. Thinking While Moving or Moving While Thinking—Concepts of Motor-Cognitive Training for Cognitive Performance Enhancement. Front. Aging Neurosci. 2018, 10, 228. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Choi, J.-Y.; Moon, S.; Park, D.-H.; Kwak, H.-B.; Kang, J.-H. Roles of Myokines in Exercise-Induced Improvement of Neuropsychiatric Function. Pflug. Arch. 2019, 471, 491–505. [Google Scholar] [CrossRef]
- Juesas, A.; Saez-Berlanga, A.; Gene-Morales, J.; Jiménez-Martínez, P.; Alix-Fages, C.; Fernandez-Garrido, J.; Caballero, O.; Janicijevic, D.; Zarza, V.; Colado, J.C. Effects of High-Resistance Elastic Band Training and a Curcumin-Based Formulation on Neuro-Oxidative and Functional Health in Sedentary Older Adults. Healthcare 2025, 13, 1055. [Google Scholar] [CrossRef]
- Haraldstad, K.; Rohde, G.; Stea, T.H.; Lohne-Seiler, H.; Hetlelid, K.; Paulsen, G.; Berntsen, S. Changes in health-related quality of life in elderly men after 12 weeks of strength training. Eur. Rev. Aging Phys. Act. 2017, 14, 8. [Google Scholar] [CrossRef]
- Valdés Badilla, P.; Herrera-Valenzuela, T.; Guzmán-Muñoz, E.; Delgado Floody, P.; Núñez Espinosa, C.; Monsalves-Álvarez, M.; Andrade, D. Effects of olympic combat sports on health-related quality of life in middle-aged and older people: A systematic review. Front. Psychol. 2022, 12, 797537. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Gamez, B.; Solis-Urra, P.; Olvera-Rojas, M.; Molina-Hidalgo, C.; Fernández-Ortega, J.; Lara, C.P.; Coca-Pulido, A.; Bellón, D.; Sclafani, A.; Mora-Gonzalez, J.; et al. Resistance Exercise Program in Cognitively Normal Older Adults: CERT-Based Exercise Protocol of the AGUEDA Randomized Controlled Trial. J. Nutr. Health Aging 2023, 27, 885–893. [Google Scholar] [CrossRef] [PubMed]
- Hansford, H.J.; Wewege, M.A.; Cashin, A.G.; Hagstrom, A.D.; Clifford, B.K.; McAuley, J.H.; Jones, M.D. If exercise is medicine, why don’t we know the dose? An overview of systematic reviews assessing reporting quality of exercise interventions in health and disease. Br. J. Sports Med. 2022, 56, 692–700. [Google Scholar] [CrossRef] [PubMed]
- Vásquez-Carrasco, E.; Hernandez-Martinez, J.; Cid-Calfucura, I.; Guzmán-Muñoz, E.; Ruiz, C.; Baeza, C.; Márquez, M.J.; Herrera-Valenzuela, T.; Branco, B.H.; Carmine-Peña, E.; et al. Effects of Different Interventions Using Taekwondo, Boxing, and Elastic Band Training on Body Composition and Physical Function in Chilean Older Women: A Randomized Controlled Trial. Life 2025, 15, 1049. [Google Scholar] [CrossRef]
- Slade, S.C.; Dionne, C.E.; Underwood, M.; Buchbinder, R. Consensus on Exercise Reporting Template (CERT): Explanation and Elaboration Statement. Br. J. Sports Med. 2016, 50, 1428–1437. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).