Implications for Dietary Guideline Policy of a Cultural Adaptation of the US Dietary Guidelines for Women of Mexican Descent: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
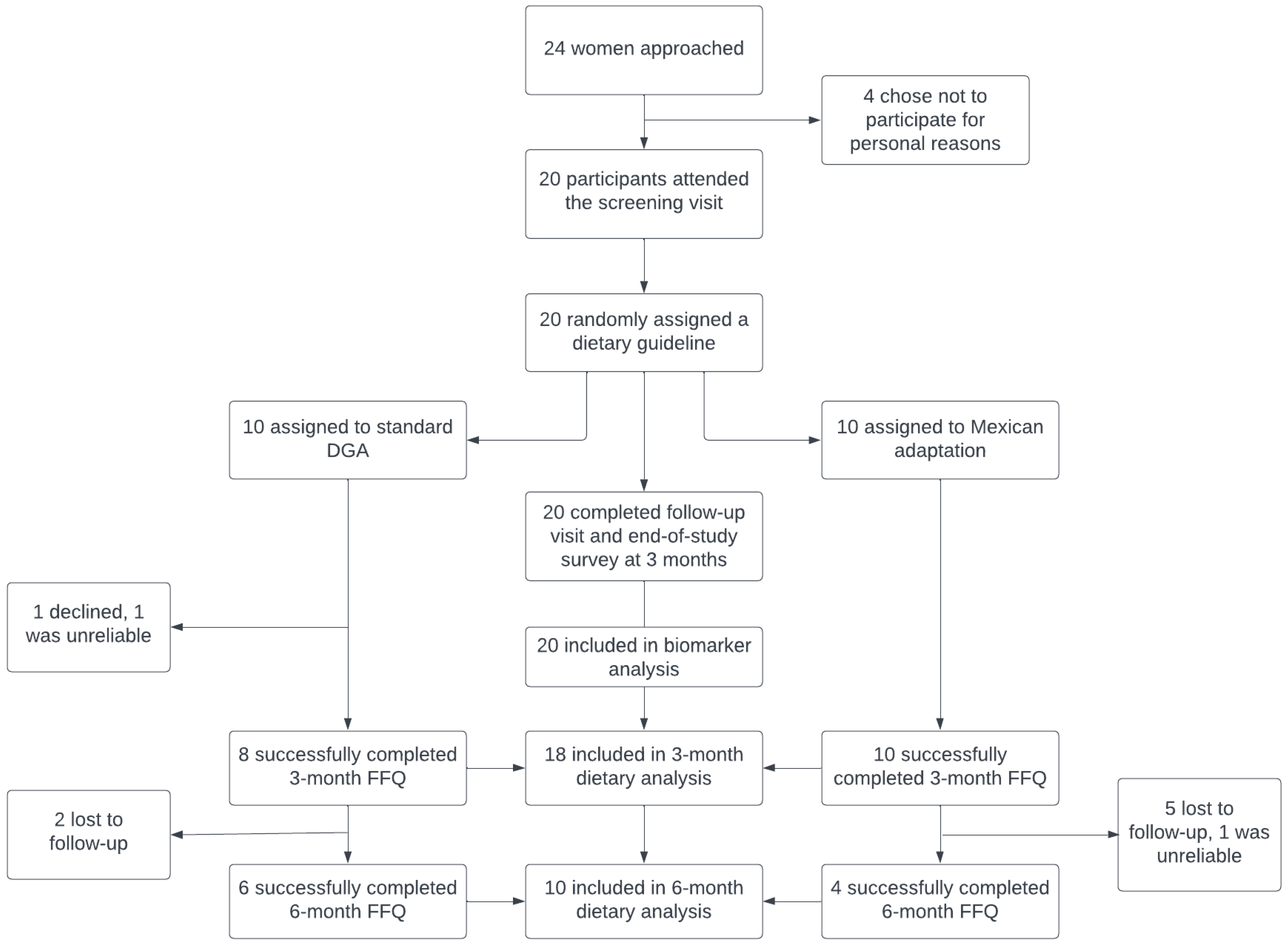
2.1. Participants
2.2. Data Collection
2.3. Quantitative Analysis Measures and Analysis
2.4. Qualitative Analysis: End-of-Study Survey
3. Results
End-of-Study Survey Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DGA | Dietary Guidelines for Americans |
| BMI | Body mass index |
| GEE | General estimating equation |
| EAR | Estimated average requirement |
| FFQ | Food Frequency Questionnaire |
| NDSR | Nutrition Data System for Research |
| hsCRP | High-sensitivity C-reactive protein |
| HDL | High-density lipoprotein |
| LDL | Low-density lipoprotein |
| VLDL | Very low-density lipoprotein |
| HOMA | Homeostatic Model Assessment |
| FFAs | Free fatty acids |
| CV | Coefficient of variation |
| SNAP | Supplemental Nutrition Assistance Program |
References
- FastStats—Health of Mexican American Population. Available online: https://www.cdc.gov/nchs/fastats/mexican-health.htm (accessed on 15 April 2021).
- Centers for Disease Control and Prevention. Diabetes Report Card 2019; Centers for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2020. Available online: https://stacks.cdc.gov/view/cdc/103877 (accessed on 9 March 2022).
- FastStats—Health of White Population. Available online: https://www.cdc.gov/nchs/fastats/white-health.htm (accessed on 15 April 2021).
- Office of Minority Health. Profile: Hispanic/Latino Americans. U.S. Department of Health & Human Services. 2021. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64 (accessed on 9 March 2022).
- Kaiser Family Foundation. Uninsured Rates for the Nonelderly by Race/Ethnicity. KFF. 2020. Available online: https://www.kff.org/uninsured/state-indicator/nonelderly-uninsured-rate-by-raceethnicity/ (accessed on 20 August 2021).
- Goldman, N.; Pebley, A.R.; Creighton, M.J.; Teruel, G.M.; Rubalcava, L.N.; Chung, C. The consequences of migration to the United States for short-term changes in the health of Mexican immigrants. Demography 2014, 51, 1159–1173. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, N. Acculturation, socioeconomic status, and health among hispanics. NAPA Bull. 2010, 34, 28–46. [Google Scholar] [CrossRef]
- Sofianou, A.; Fung, T.T.; Tucker, K.L. Differences in diet pattern adherence by nativity and duration of US residence in the Mexican-American population. J. Am. Diet. Assoc. 2011, 111, 1563–1569.e2. [Google Scholar] [CrossRef]
- Tapsell, L.C.; Neale, E.P.; Satija, A.; Hu, F.B. Foods, nutrients, and dietary patterns: Interconnections and implications for dietary guidelines. Adv. Nutr. 2016, 7, 445–454. [Google Scholar] [CrossRef]
- Eldeirawi, K.; Koenig, M.D.; Persky, V.; Chavez, N. Nativity and serum concentrations of antioxidants in Mexican American children: A cross-sectional study. Nutrients 2014, 6, 1598–1607. [Google Scholar] [CrossRef]
- Reyes-Ortiz, C.A.; Ju, H.; Inniss, A.; Eschbach, K.; Kuo, Y.-F.; Goodwin, J.S. Acculturation and serum nutrients thought to be involved with cancer prevention among Mexican American men in the United States. Cancer Control 2009, 16, 169–175. [Google Scholar] [CrossRef]
- Liu, J.; Zhu, X.; Fulda, K.G.; Chen, S.; Tao, M.-H. Comparison of Dietary Micronutrient Intakes by Body Weight Status among Mexican-American and Non-Hispanic Black Women Aged 19–39 Years: An Analysis of NHANES 2003–2014. Nutrients 2019, 11, 2846. [Google Scholar] [CrossRef] [PubMed]
- Pedroza-Tobías, A.; Hernández-Barrera, L.; López-Olmedo, N.; García-Guerra, A.; Rodríguez-Ramírez, S.; Ramírez-Silva, I.; Villalpando, S.; Carriquiry, A.; Rivera, J.A. Usual Vitamin Intakes by Mexican Populations. J. Nutr. 2016, 146, 1866S–1873S. [Google Scholar] [CrossRef]
- Wang, V.H.-C.; Foster, V.; Yi, S.S. Are recommended dietary patterns equitable? Public Health Nutr. 2022, 25, 464–470. [Google Scholar] [CrossRef] [PubMed]
- McClain, A.C.; Dickin, K.L.; Dollahite, J. Life course influences on food provisioning among low-income, Mexican-born mothers with young children at risk of food insecurity. Appetite 2019, 132, 8–17. [Google Scholar] [CrossRef]
- Méndez, R.; Goto, K.; Song, C.; Giampaoli, J.; Karnik, G.; Wylie, A. Cultural influence on mindful eating: Traditions and values as experienced by Mexican-American and non-Hispanic white parents of elementary-school children. Glob. Health Promot. 2020, 27, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, T.; Hudson, D.B.; Weber, K.; Pozehl, B.; Boeckner, L.; Wilhelm, S. Mexican American mothers’ eating and child feeding behaviors. Issues Compr. Pediatr. Nurs. 2012, 35, 4–23. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.J.; Brown, H.S.; Bastida, E. Cost-effectiveness of a community-based weight control intervention targeting a low-socioeconomic-status Mexican-origin population. Health Promot. Pract. 2015, 16, 101–108. [Google Scholar] [CrossRef]
- McEwen, M.M.; Pasvogel, A.; Murdaugh, C.; Hepworth, J. Effects of a Family-based Diabetes Intervention on Behavioral and Biological Outcomes for Mexican American Adults. Diabetes Educ. 2017, 43, 272–285. [Google Scholar] [CrossRef]
- Ayala, G.X.; Ibarra, L.; Horton, L.; Arredondo, E.M.; Slymen, D.J.; Engelberg, M.; Rock, C.L.; Hernandez, E.; Parada, H.; Elder, J.P. Evidence supporting a promotora-delivered entertainment education intervention for improving mothers’ dietary intake: The Entre Familia: Reflejos de Salud Study. J. Health Commun. 2015, 20, 165–176. [Google Scholar] [CrossRef]
- Rothschild, S.K.; Martin, M.A.; Swider, S.M.; Tumialán Lynas, C.M.; Janssen, I.; Avery, E.F.; Powell, L.H. Mexican American trial of community health workers: A randomized controlled trial of a community health worker intervention for Mexican Americans with type 2 diabetes mellitus. Am. J. Public Health 2014, 104, 1540–1548. [Google Scholar] [CrossRef]
- Ayala, G.X.; Elder, J.P.; Campbell, N.R.; Arredondo, E.; Baquero, B.; Crespo, N.C.; Slymen, D.J. Longitudinal Intervention Effects on Parenting of the Aventuras para Niños Study. Am. J. Prev. Med. 2010, 38, 154–162. [Google Scholar] [CrossRef]
- Lindberg, N.M.; Stevens, V.J.; Vega-López, S.; Kauffman, T.; Calderón, M.R.; Cervantes, M.A. A weight-loss intervention program designed for Mexican-American women: Cultural adaptations and results. J. Immigr. Minor. Health Cent. Minor. Public Health 2012, 14, 1030–1039. [Google Scholar] [CrossRef]
- Shea, M.; Cachelin, F.M.; Gutierrez, G.; Wang, S.; Phimphasone, P. Mexican American Women’s Perspectives on a Culturally Adapted Cognitive-Behavioral Therapy Guided Self-Help Program for Binge Eating. Psychol. Serv. 2016, 13, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, L.; Martinez, J.; Horowitz, M.; Lamp, C.; Johns, M.; Espinoza, D.; Byrnes, M.; Gomez, M.M.; Aguilera, A.; de la Torre, A. Adaptation of a Culturally Relevant Nutrition and Physical Activity Program for Low-Income, Mexican-Origin Parents with Young Children. Prev. Chronic Dis. 2015, 12, E72. [Google Scholar] [CrossRef]
- Santiago-Torres, M.; Kratz, M.; Lampe, J.W.; Tapsoba, J.D.D.; Breymeyer, K.L.; Levy, L.; Villaseñor, A.; Wang, C.-Y.; Song, X.; Neuhouser, M.L. Metabolic responses to a traditional Mexican diet compared with a commonly consumed US diet in women of Mexican descent: A randomized crossover feeding trial. Am. J. Clin. Nutr. 2016, 103, 366–374. [Google Scholar] [CrossRef]
- Evans, A.; Chow, S.; Jennings, R.; Dave, J.; Scoblick, K.; Sterba, K.R.; Loyo, J. Traditional foods and practices of Spanish-speaking Latina mothers influence the home food environment: Implications for future interventions. J. Am. Diet. Assoc. 2011, 111, 1031–1038. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Kaushal, N.; Waldfogel, J.; Wight, V. Food Insecurity and SNAP Participation in Mexican Immigrant Families: The Impact of the Outreach Initiative. BE J. Econ. Anal. Policy 2014, 14, 203–240. [Google Scholar] [CrossRef]
- Verde, L.; Kohler, L.N.; Muscogiuri, G.; Parra, O.; Klimentidis, Y.C.; Coletta, D.K.; Mandarino, L.J. Food insecurity and its associations with cardiometabolic health in Latino individuals of Mexican ancestry. Front. Nutr. 2024, 11, 1499504. [Google Scholar] [CrossRef]
- Boden, G. Obesity, insulin resistance and free fatty acids. Curr. Opin. Endocrinol. Diabetes Obes. 2011, 18, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Kimura, I.; Ichimura, A.; Ohue-Kitano, R.; Igarashi, M. Free fatty acid receptors in health and disease. Physiol. Rev. 2020, 100, 171–210. [Google Scholar] [CrossRef] [PubMed]
- Melse-Boonstra, A. Bioavailability of Micronutrients From Nutrient-Dense Whole Foods: Zooming in on Dairy, Vegetables, and Fruits. Front. Nutr. 2020, 7, 101. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.; Campbell, K.L.; Craig, J.C.; Tong, A.; Teixeira-Pinto, A.; Brown, M.A.; Howard, K.; Howell, M.; Khalid, R.; Sud, K.; et al. A text messaging intervention for dietary behaviors for people receiving maintenance hemodialysis: A feasibility study of KIDNEYTEXT. Am. J. Kidney Dis. 2021, 78, 85–95.e1. [Google Scholar] [CrossRef]
- Van Blarigan, E.L.; Kenfield, S.A.; Chan, J.M.; Van Loon, K.; Paciorek, A.; Zhang, L.; Chan, H.; Savoie, M.B.; Bocobo, A.G.; Liu, V.N.; et al. Feasibility and Acceptability of a Web-Based Dietary Intervention with Text Messages for Colorectal Cancer: A Randomized Pilot Trial. Cancer Epidemiol. Biomark. Prev. 2020, 29, 752–760. [Google Scholar] [CrossRef]
- Gustafson, A.; Jilcott Pitts, S.B.; McQuerry, K.; Babtunde, O.; Mullins, J. A Mentor-Led Text-Messaging Intervention Increases Intake of Fruits and Vegetables and Goal Setting for Healthier Dietary Consumption among Rural Adolescents in Kentucky and North Carolina, 2017. Nutrients 2019, 11, 593. [Google Scholar] [CrossRef] [PubMed]
| All | Standard DGA Arm | Mexican Adaptation Arm | |
|---|---|---|---|
| Age (years) * | 38.7 (8.6) | 41.1 (8.0) | 36.2 (8.9) |
| Weight (kg) * | 73.0 (19.4) | 77.5 (21.8) | 68.6 (16.5) |
| BMI (kg/m2) * | 29.9 (7.4) | 31.6 (7.5) | 28.3 (7.3) |
| Energy intake (kcal/d) * | 1685 (628) | 1742 (528) | 1627 (739) |
| BMI (kg/m2) † | |||
| ≥18.2–24.9 | 6 (30) | 2 (20) | 4 (40) |
| ≥25–29.9 | 6 (30) | 3 (30) | 3 (30) |
| ≥30.0 | 8 (40) | 5 (50) | 3 (30) |
| Education † | |||
| <12th grade | 4 (20) | 1 (10) | 3 (30) |
| 12th grade | 6 (30) | 2 (20) | 4 (40) |
| >12th grade | 10 (50) | 7 (70) | 3 (30) |
| Marital status † | |||
| Married | 17 (84) | 10 (100) | 7 (70) |
| Single | 3 (16) | 0 (0) | 3 (30) |
| Language † | |||
| Spanish | 15 (75) | 7 (70) | 8 (80) |
| English | 5 (25) | 3 (30) | 2 (20) |
| Occupation † | |||
| Full time | 8 (40) | 5 (50) | 3 (30) |
| Part time | 5 (25) | 2 (20) | 3 (30) |
| House spouse | 7 (35) | 3 (30) | 4 (40) |
| Biomarker | Standard DGA | Mexican Adaptation | p0 | p1 | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Mean Difference | Baseline | Follow-Up | Mean Difference | |||
| Cholesterol (mg/dL) | 203.78 (177.8, 233.56) | 192.88 (171.67, 216.70) | 10.9 | 171.49 (155.96, 188.56) | 164.06 (144.91, 185.73) | 7.43 | 0.4 | 0.09 |
| HDL (mg/dL) | 57.83 (48.9, 68.4) | 56.04 (46.51, 67.52) | 1.79 | 56.41 (49.78, 63.92) | 53.74 (46.31, 62.35) | 2.67 | 0.73 | 0.62 |
| LDL (mg/dL) | 116.78 (96.27, 141.67) | 108.85 (90.62, 130.74) | 7.93 | 93.83 (79.46, 110.8) | 86.97 (68.63, 110.21) | 6.86 | 0.64 | 0.38 |
| VLDL (mg/dL) | 23.25 (15.03, 35.99) | 20.30 (12.69, 32.49) | 2.95 | 18.2 (13.64, 24.27) | 18.95 (14.25, 25.18) | −0.75 | 0.49 | 0.25 |
| Triglycerides (mg/dL) | 115.48 (74.38, 179.31) | 101.80 (63.46, 163.30) | 13.68 | 90.96 (68.04, 121.61) | 94.35 (70.97, 125.44) | −3.39 | 0.55 | 0.3 |
| FFAs (mEq/L) | 0.50 (0.41, 0.62) | 0.37 (0.28, 0.47) | 0.13 | 0.41 (0.33, 0.50) | 0.45 (0.38, 0.52) | −0.04 | <0.01 | <0.01 |
| Glucose (mg/dL) | 103.43 (89.52, 119.5) | 104.47 (89.80, 121.53) | −1.04 | 95.09 (82.83, 109.15) | 97.22 (80.54, 117.36) | −2.13 | 0.43 | 0.37 |
| Insulin (µU/mL) | 7.79 (4.93, 12.32) | 8.10 (5.43, 12.09) | −0.31 | 8.10 (5.4, 12.16) | 7.98 (4.86, 13.09) | 0.12 | 0.9 | 0.85 |
| CRP (mg/dL) | 0.25 (0.10, 0.60) | 0.18 (0.06, 0.53) | 0.07 | 0.19 (0.09, 0.38) | 0.14 (0.07, 0.29) | 0.05 | 0.92 | 0.74 |
| HOMA-IR | 1.99 (1.11, 3.55) | 2.09 (1.24, 3.52) | −0.1 | 1.90 (1.14, 3.17) | 1.91 (1.02, 3.59) | −0.01 | 0.54 | 0.55 |
| Nutrient | Standard DGA a | Mexican Adaptation b | p1 | ||||
|---|---|---|---|---|---|---|---|
| Value at Baseline | 3-Month Follow-Up | Mean Difference | Value at Baseline | 3-Month Follow-Up | Mean Difference | ||
| Energy (kcal/d) | 1679 (1375, 2051) | 1160 (899, 1498) | 519 | 1496 (1104, 2027) | 1434 (1092, 1884) | 62 | 0.05 |
| Carbohydrates (%E/d) | 49.3% (44.7, 54.3) | 49.4% (45.7, 53.4) | −0.1 | 49.8% (45.1, 54.9) | 51% (47, 55.2) | −1.2 | |
| Carbohydrates (g/d) | 206.9 (161.8, 264.6) | 143.3 (109.7, 187.3) | 63.6 | 186.2 (135.8, 255.2) | 182.7 (142.3, 234.7) | 3.5 | 0.03 |
| Total fat (%E/d) | 34% (29.2, 39.7) | 33.1% (28.3, 38.6) | 0.9 | 32.9% (29.4, 36.8) | 33.4% (30.1, 37.1) | −0.5 | |
| Total fat (g/d) | 63.5 (52.1, 77.4) | 42.6 (30.8, 58.9) | 20.9 | 54.7 (38.5, 77.8) | 53.3 (38.2, 74.4) | 1.4 | 0.09 |
| Saturated fat (g/d) | 19.9 (16, 24.8) | 12.5 (9, 17.4) | 7.4 | 17.2 (11.4, 26) | 16.4 (12, 22.3) | 0.8 | 0.12 |
| Protein (%E/d) | 16.7% (15.6, 17.9) | 18.5% (16.2, 21.2) | −1.8 | 17.2% (15.6, 17.9) | 14.5% (12.1, 17.3) | 2.7 | |
| Protein (g/d) | 70.2 (57.3, 85.9) | 53.7 (44, 65.7) | 16.5 | 64.6 (48.1, 86.8) | 51.8 (38.2, 70.3) | 12.8 | 0.32 |
| Dietary fiber (g/d) | 21.2 (16.7, 26.9) | 14.5 (9.9, 21.2) | 6.7 | 20 (14.6, 27.2) | 19.5 (14.5, 26.3) | 0.5 | 0.08 |
| Fruit (servings/d) | 1.7 (1.1, 2.6) | 1.7 (1, 2.8) | 0 | 1.7 (1.3, 2.3) | 1.8 (1.1, 2.9) | −0.1 | 0.07 |
| Vegetable (servings/d) | 2.2 (1.3, 3.5) | 2 (1.2, 3.4) | 0.2 | 1.5 (0.9, 2.5) | 2.4 (1.7, 3.5) | −0.9 | 0.11 |
| Nutrient | Standard DGA a | Mexican Adaptation b | p1 | p2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Value at Baseline | 3-Month Follow-Up | 6-Month Follow-Up | Mean Difference 1 | Mean Difference 2 | Value at Baseline | 3-Month Follow-Up | 6-Month Follow-Up | Mean Difference 1 | Mean Difference 2 | |||
| Energy (kcal/d) | 1819 (1368, 2419) | 1143 (804, 1624) | 1194 (688, 2072) | 676 | 625 | 1829 (1047, 3193) | 1416 (868, 2310) | 983 (618, 1562) | 413 | 846 | 0.51 | <0.01 |
| Carbohydrate (%E/d) | 49.8% (41.8, 59.3) | 49.1% (45.6, 52.9) | 52% (45.4, 59.5) | 0.7 | −2.2 | 49.1% (47, 51.3) | 51.3% (49.5, 53.1) | 48.8% (38.7, 61.7) | −2.2 | 0.3 | ||
| Carbohydrate (g/d) | 226.5 (158.6, 323.5) | 140.3 (101.6, 193.9) | 155.1 (85.8, 280.5) | 86.2 | 71.4 | 224.5 (125.6, 401.5) | 181.5 (111.1, 296.6) | 119.9 (69.6, 206.6) | 43 | 104.6 | 0.39 | 0.02 |
| Total fat (%E/d) | 32.5% (24.9, 42.4) | 33.7% (28.4, 39.9) | 30.4% (24.9, 37) | −1.2 | 2.1 | 35.5% (33.6, 37.5) | 34.3% (30.3, 39) | 36.4% (28.4, 46.8) | 1.2 | −0.9 | ||
| Total fat (g)/d | 65.7 (46.5, 93) | 42.8 (26.5, 69.3) | 40.3 (23, 70.7) | 22.9 | 25.4 | 72.2 (41.8, 124.6) | 54 (32.2, 90.8) | 39.8 (23.4, 67.6) | 18.2 | 32.4 | 0.83 | 0.03 |
| Saturated fat (g/d) | 21 (14.5, 30.5) | 12.8 (7.9, 20.8) | 13.2 (7.4, 23.3) | 8.2 | 7.8 | 23.1 (12.3, 43.6) | 16.4 (9.3, 28.9) | 11.8 (6.7, 20.7) | 6.7 | 11.3 | 0.9 | 0.01 |
| Protein (%E/d) | 17.1% (15.3, 19.1) | 18.2% (15.1, 22) | 16.7% (14.2, 19.7) | −1.1 | 0.4 | 16.2% (15.3, 17.1) | 12.6% (7.1, 22.2) | 11.5% (10.5, 12.7) | 3.6 | 4.7 | ||
| Protein (g/d) | 77.9 (62.7, 96.7) | 52.1 (41.8, 64.8) | 55 (35, 86.5) | 25.8 | 22.9 | 73.9 (43.1, 126.7) | 44.4 (29.8, 66.2) | 37.8 (24.5, 58.2) | 29.5 | 36.1 | 0.48 | <0.01 |
| Dietary fiber (g/d) | 24.1 (14.5, 33.3) | 13.1 (8.5, 20.3) | 15.7 (9.1, 27.3) | 11 | 8.4 | 22.1 (10.1, 48) | 20.8 (12.5, 34.4) | 13.9 (8.6, 22.4) | 1.3 | 8.2 | 0.25 | 0.29 |
| Fruit (servings/d) | 1.6 (0.8, 3.4) | 1.5 (0.8, 2.9) | 1.3 (0.5, 3.6) | 0.1 | 0.3 | 2.1 (1.4, 3.3) | 2.1 (0.4, 9.9) | 1.6 (0.6, 4.1) | 0 | 0.5 | 0.08 | 0.71 |
| Vegetable (servings/d) | 2.1 (0.9, 5.3) | 1.7 (1, 3.1) | 2.2 (0.9, 5.6) | 0.4 | −0.1 | 1.4 (0.3, 7.1) | 2.2 (0.8, 5.7) | 1.5 (0.5, 4.5) | −0.8 | −0.1 | 0.32 | 0.49 |
| Question | Type of Question |
|---|---|
| Likert scale and open-ended question |
| Likert scale and open-ended question |
| Open-ended question |
| Open-ended question |
| Open-ended question |
| Open-ended question |
| Open-ended question |
| Open-ended question |
| Open-ended question |
| Open-ended question |
| Codes | Standard DGA Arm | Mexican Adaptation Arm |
|---|---|---|
| Ease of use | “It’s very simple, it gives you freedom to adapt the foods according to your needs […]” | “It wasn’t difficult since it’s the Mexican guide and it’s what I already consume the most […]” |
| Important or interesting topic | “This topic is very interesting to me and there’s a lot of very beneficial information concerning our eating habits and how to prepare and consume foods” | “This was a fun and engaging study, personally. It forged a connection back to my culture and history as a Latina.” |
| Perception of healthiness | “Seeing my plate with the portions and a variety of vegetables is very healthy.” | “It seems like a very important topic to me, and it helps us realize that small changes can help us make a big difference in preparing healthier meals without huge sacrifices.” |
| Variety | “All is perfect, like the variety” | Not reported |
| Intervention components (included nine codes: guide, recipes, study staff, calls, text, email, in-person guidance, all components, and others) | “How they explained how much you should eat of each group” “All of the information is useful, but for me visuals like the recipes are easier.” | “The guide is easy to understand, basic and to the point.” “All of the communications were useful (texts/phone calls/in-person conversations) I think 3–4 weeks was an appropriate time to be checking-in.” |
| Extrinsic facilitators: family values | “Continue as I am now because I know it’s healthy. For my children, cooking at home is important.” | “I eat a lot of traditional Mexican food already, especially with my family” |
| Codes | Standard DGA Arm | Mexican Adaptation Arm |
| Intrinsic barrier: lack of time | “Yes, my lack of time is always getting in the way. Exercise is difficult for me, finding the time.” | Not reported |
| Intrinsic barrier: challenge with specific dietary components | “I feel that dairy shouldn’t be pushed so much.” | “It was difficult to stop using lard, and with the recipes, the portions were difficult. The salt, I consume more salt. I know salt is bad, my doctor told me” |
| Other barriers (not included in the previous two codes) | “I liked the recipes, but I don’t always have the ingredients at home.” | “The guide was easy to understand, although I only make/eat traditional Mexican foods like pozole, menudo, etc. on special occasions.” |
| Extrinsic barrier: family pushback | “Yes, I had problems [in the form of] family pushing me to eat more meals at restaurants” | “Using more vegetables when cooking because I already eat vegetables. It’s difficult because my husband is more of a meat eater.” |
| Untimeliness of study materials | “Everything was good, but I would have liked to have received the recipes earlier at the beginning” | “Only complaint would be that it seemed we received some of the information too late, would have liked to have all materials at the beginning of the study.” |
| Codes | Standard DGA Arm | Mexican Adaptation Arm |
|---|---|---|
| Fruits and vegetables | “I realized I need to eat more veggies & fruits” | “Eating healthy, like fruits and vegetables” |
| Fats | “Avoiding red meats and fats (pork, beef)” | “Cooking with less fat because it is easier” |
| Sugar | “Cutting down on sugars, being more on top of my family’s sugar consumption” | “[…] tried to cut down on sugars, but it was a challenge” |
| Sugar-sweetened beverages | “No more soda, specifically Coca-Cola because of its sugar and caffeine content” | “Yes, switching from Coca-Cola to natural water” |
| Junk food/processed food (general) | “Tried to eat less junk food, smaller (decent) portions” | “No, just being more conscious to cut out more processed foods like potato chips, pizzas, fast food and cook more Mexican meals/dishes, which is the norm for me and my family anyway” |
| Water | Not mentioned | “Eating smaller portions and eating more fruits and vegetables and most of all, to drink a lot of water” |
| Salt/sodium | “Yes, follow a healthy eating pattern for my entire life and limit the consumption of sugars and saturated fats and sodium and also limit calorie consumption” | “The salt, I consume more salt. I know salt is bad, my doctor told me” |
| Meat | “That my stomach struggles to digest pork and beef” | “I got more ideas for how to cook meats and vegetables in meals” |
| Beans | “I’m eating a lot more beans than before, in the past I thought they made my [sic] gasy, but now I crave them. I used to burp a lot, now I don’t, not these past months.” | “Beans, they’re so good and dynamic, tostadas are a great vehicle for many other ingredients” |
| Flour | “Not eating white flour, I replaced it with whole wheat flour, or I avoided it” | “Reducing my flour [carb] intake and consuming more grains” |
| Others | “I tried to drink more pressed green juices, nothing added, just things like coconut water, turmeric.” | “I included more vegetables, nuts and eggs in my daily diet.” |
| Codes | Standard DGA Arm | Mexican Adaptation Arm |
|---|---|---|
| Useful information learned from the intervention | “How to put together meals or dishes and how to economize and buying foods with only $10, fresh or frozen, and the amount that it can yield.” | “Knowing that making small changes and eating healthier can prevent chronic illnesses” |
| Portion sizes | “Reading the quantities of each portion, like granola bars, the amount of sugar it has, fat, etc.” | “Thankful for teaching us to eat smaller portions” |
| Frequency | Not reported | “Eating pattern recommendations and keeping in mind to try to eat 1–2 servings of beans each day, vegetables, corn based (masa), fruits, and whole milk.” |
| Changes made during the intervention | “The change I made was to have protein for breakfast every day and to carry healthy snacks/or have them at hand” | “1. More salsa = more vitamin C & other nutrients 2. Meal planning and cooking more” |
| Continuation of changes post-intervention | “Eating less processed flour products, using less dressing” | “Continue incorporating vegetables to the meals I prepare” |
| Exercise | “Complimenting with exercise” | “With exercise, and to include more fruits and vegetables in my diet” |
| Suggestions | “Something that would help busy people like me eat better, guides, food recommendations” | “The recipes could have been more useful if handed out towards the beginning! I’m sad I didn’t get to use them. More emphasis on things we should eat less of. Would’ve liked seeing an on-line (log-in required) sort of method for completing food questionnaires, like a virtual food diary.” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garfias-Avila, N.; Wang, C.-Y.; Lampe, J.W.; Mendoza, J.A.; Tapsoba, J.D.D.; Alcalá, N.J.; Levy, L.; Neuhouser, M.L. Implications for Dietary Guideline Policy of a Cultural Adaptation of the US Dietary Guidelines for Women of Mexican Descent: A Pilot Study. Nutrients 2025, 17, 3578. https://doi.org/10.3390/nu17223578
Garfias-Avila N, Wang C-Y, Lampe JW, Mendoza JA, Tapsoba JDD, Alcalá NJ, Levy L, Neuhouser ML. Implications for Dietary Guideline Policy of a Cultural Adaptation of the US Dietary Guidelines for Women of Mexican Descent: A Pilot Study. Nutrients. 2025; 17(22):3578. https://doi.org/10.3390/nu17223578
Chicago/Turabian StyleGarfias-Avila, Norma, Ching-Yun Wang, Johanna W. Lampe, Jason A. Mendoza, Jean De Dieu Tapsoba, Norma J. Alcalá, Lisa Levy, and Marian L. Neuhouser. 2025. "Implications for Dietary Guideline Policy of a Cultural Adaptation of the US Dietary Guidelines for Women of Mexican Descent: A Pilot Study" Nutrients 17, no. 22: 3578. https://doi.org/10.3390/nu17223578
APA StyleGarfias-Avila, N., Wang, C.-Y., Lampe, J. W., Mendoza, J. A., Tapsoba, J. D. D., Alcalá, N. J., Levy, L., & Neuhouser, M. L. (2025). Implications for Dietary Guideline Policy of a Cultural Adaptation of the US Dietary Guidelines for Women of Mexican Descent: A Pilot Study. Nutrients, 17(22), 3578. https://doi.org/10.3390/nu17223578









