Effect of a Low Glycemic Index/Slow Digesting (LGI/SD) Carbohydrate Product on Maternal Glycemia and Neonatal Body Composition in Obese Pregnant Women: The NIGOHealth Randomized Clinical Trial
Abstract
1. Introduction
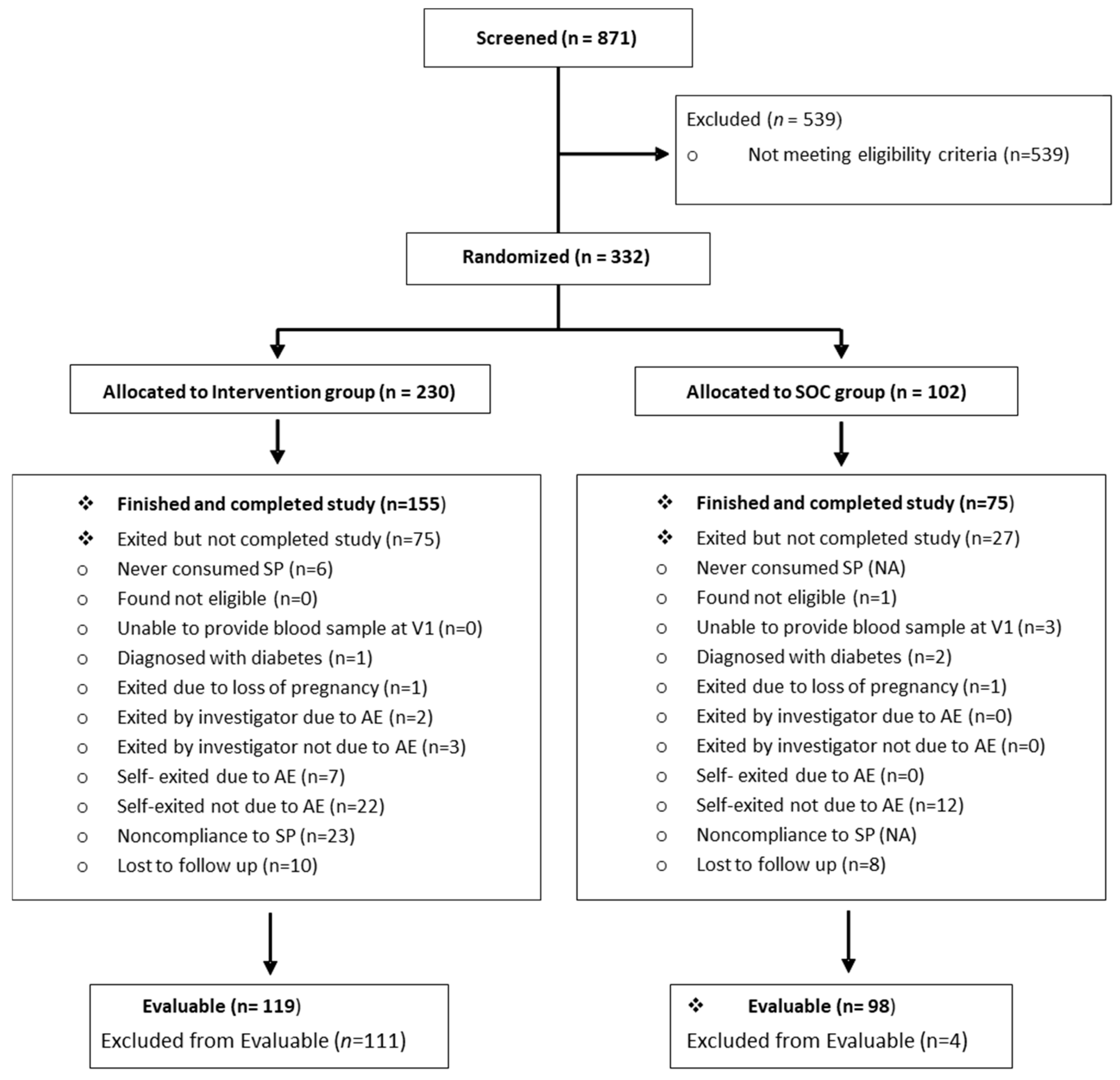
2. Materials and Methods
2.1. Study Overview
2.2. Study Protocol
2.2.1. Participants
2.2.2. Nutritional Intervention
2.2.3. Assessment of Outcomes
2.2.4. Statistical Analysis
- Subject did not provide OGTT data at Visit 2.
- The participants in the IG had <75% average intake of the SP between Visits 1–2, as determined by Product Intake Records.
- The participants in the IG had <50% intake of the SP in the 7 days prior to Visit 2, as determined by the Product Intake Records.
- The window between Visit 1 and Visit 2 was <10 weeks.
- The participant had a diabetes diagnosis at V1 from fasting glucose ≥ 126 mg/dL.
- The infant was born at <37+0 or >41+6 weeks gestation.
- The infant had a major congenital disease that would impact intrauterine growth, as determined by the study physician.
- Maternal subjects in the IG had <75% average intake of the SP between Visits 1–4, as determined by the Product Intake Records.
- The maternal participant was not Evaluable.
3. Results
3.1. Demographic and Other Baseline Characteristics
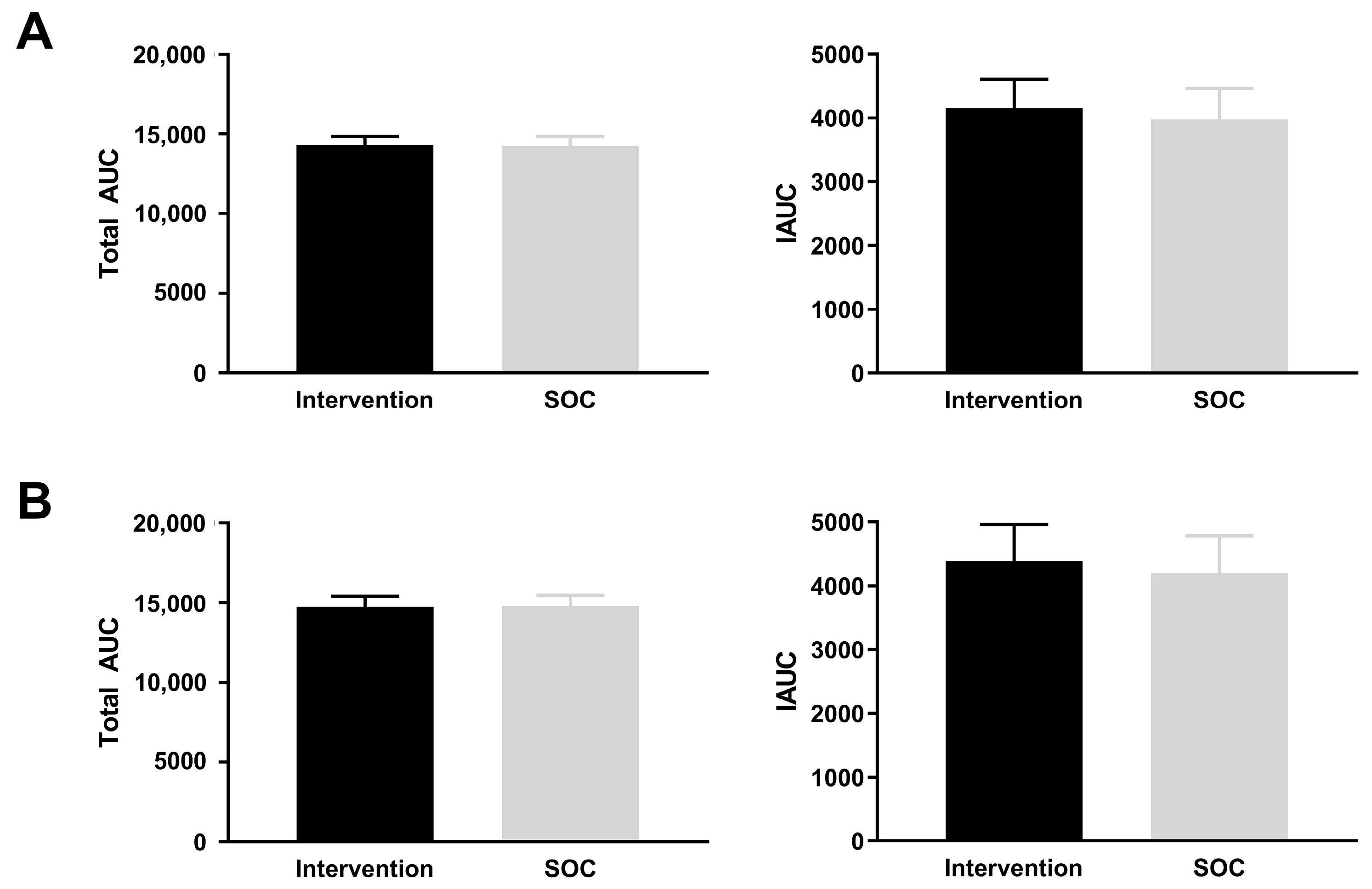
3.2. Main Outcome: AUC for Maternal Blood Glucose at 28 Weeks of Gestation
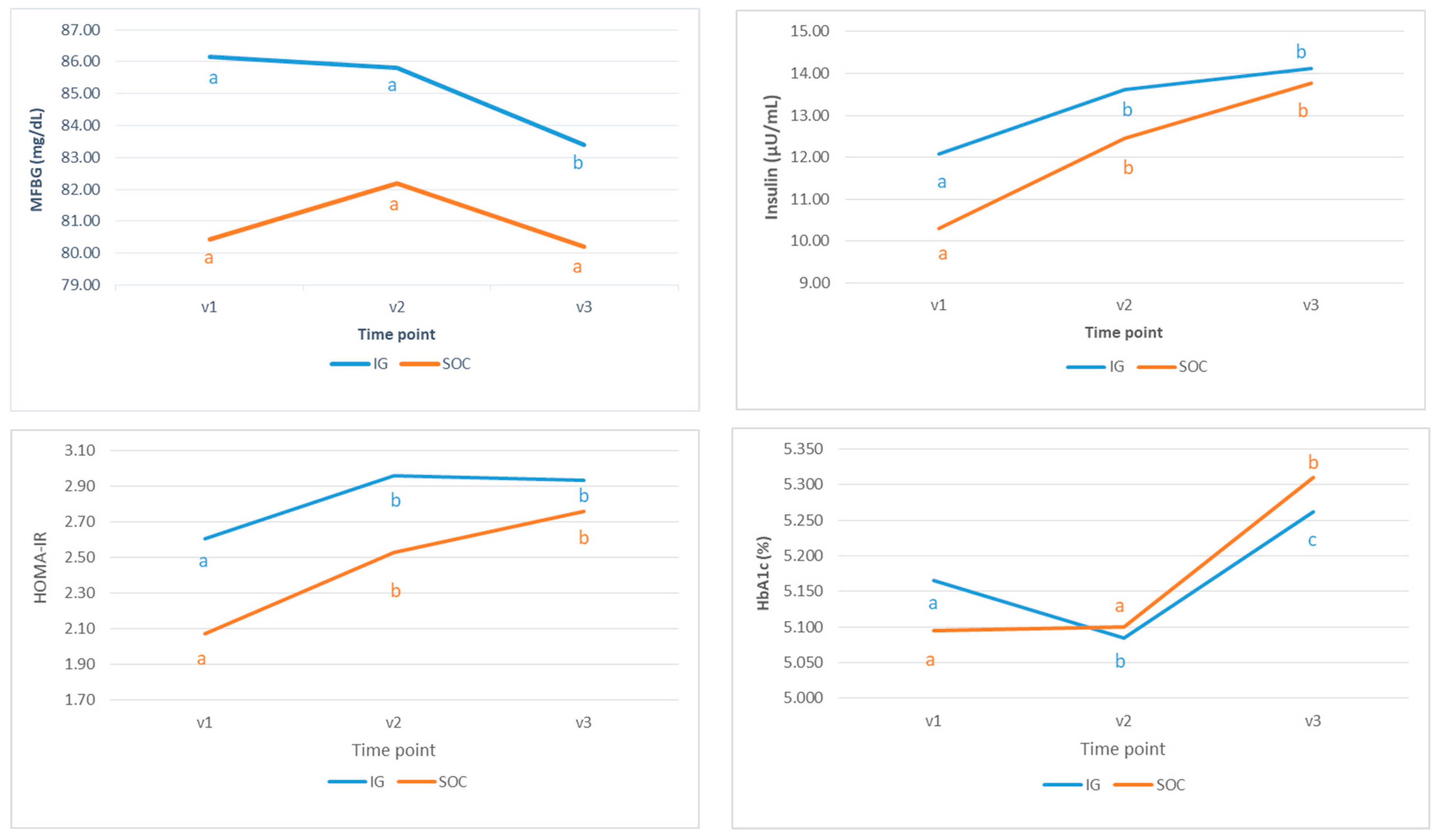
3.3. Secondary Variable: MFBG at 34+0–36+0 Weeks of Pregnancy
3.4. Secondary Variable: Neonatal Body Composition
3.5. Additional Analysis
3.6. Adverse Events (AEs)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gillman, M.W. Interrupting Intergenerational Cycles of Maternal Obesity. In Nestlé Nutrition Institute Workshop Series; Fewtrell, M.S., Haschke, F., Prescott, S.L., Eds.; S. Karger AG: Basel, Switzerland, 2016; Volume 85, pp. 59–69. ISBN 978-3-318-05642-6. [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC). Trends in Adult Body-Mass Index in 200 Countries from 1975 to 2014: A Pooled Analysis of 1698 Population-Based Measurement Studies with 19·2 Million Participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Xu, X.; Yan, Y. Estimated Global Overweight and Obesity Burden in Pregnant Women Based on Panel Data Model. PLoS ONE 2018, 13, e0202183. [Google Scholar] [CrossRef] [PubMed]
- Kent, L.; McGirr, M.; Eastwood, K.-A. Global Trends in Prevalence of Maternal Overweight and Obesity: A Systematic Review and Meta-Analysis of Routinely Collected Data Retrospective Cohorts. Int. J. Popul. Data Sci. 2024, 9, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- Devlieger, R.; Benhalima, K.; Damm, P.; Van Assche, A.; Mathieu, C.; Mahmood, T.; Dunne, F.; Bogaerts, A. Maternal Obesity in Europe: Where Do We Stand and How to Move Forward? Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 201, 203–208. [Google Scholar] [CrossRef]
- Catalano, P.M.; Shankar, K. Obesity and Pregnancy: Mechanisms of Short Term and Long Term Adverse Consequences for Mother and Child. BMJ 2017, 356, j1. [Google Scholar] [CrossRef]
- Catalano, P.M. The Impact of Gestational Diabetes and Maternal Obesity on the Mother and Her Offspring. J. Dev. Orig. Health Dis. 2010, 1, 208–215. [Google Scholar] [CrossRef]
- Friedman, J.E. Obesity and Gestational Diabetes Mellitus Pathways for Programming in Mouse, Monkey, and Man—Where Do We Go Next? The 2014 Norbert Freinkel Award Lecture. Diabetes Care 2015, 38, 1402–1411. [Google Scholar] [CrossRef]
- Alejandro, E.U.; Mamerto, T.P.; Chung, G.; Villavieja, A.; Gaus, N.L.; Morgan, E.; Pineda-Cortel, M.R.B. Gestational Diabetes Mellitus: A Harbinger of the Vicious Cycle of Diabetes. Int. J. Mol. Sci. 2020, 21, 5003. [Google Scholar] [CrossRef]
- Leoni, M.; Padilla, N.; Fabbri, A.; Della-Morte, D.; Ricordi, C.; Infante, M. Mechanisms of Insulin Resistance during Pregnancy. In Evolving Concepts in Insulin Resistance; Infante, M., Ed.; IntechOpen: London, UK, 2022; ISBN 978-1-80355-501-0. [Google Scholar]
- Poon, L.C.; Nguyen-Hoang, L.; Smith, G.N.; Bergman, L.; O’Brien, P.; Hod, M.; Okong, P.; Kapur, A.; Maxwell, C.V.; McIntyre, H.D.; et al. Hypertensive Disorders of Pregnancy and Long-term Cardiovascular Health: FIGO Best Practice Advice. Int. J. Gynecol. Obstet. 2023, 160, 22–34. [Google Scholar] [CrossRef]
- Brunner, K.; Linder, T.; Klaritsch, P.; Tura, A.; Windsperger, K.; Göbl, C. The Impact of Overweight and Obesity on Pregnancy: A Narrative Review of Physiological Consequences, Risks and Challenges in Prenatal Care, and Early Intervention Strategies. Curr. Diab. Rep. 2025, 25, 30. [Google Scholar] [CrossRef]
- Griffith, R.J.; Alsweiler, J.; Moore, A.E.; Brown, S.; Middleton, P.; Shepherd, E.; Crowther, C.A. Interventions to Prevent Women from Developing Gestational Diabetes Mellitus: An Overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2020, 2020, CD012394. [Google Scholar] [CrossRef]
- Prodan, N.C.; Schmidt, M.; Hoopmann, M.; Abele, H.; Kagan, K.O. Obesity in Prenatal Medicine: A Game Changer? Arch. Gynecol. Obstet. 2023, 309, 961–974. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, K.M.; Reynolds, R.M.; Prescott, S.L.; Nyirenda, M.; Jaddoe, V.W.; Eriksson, J.G.; Broekman, B.F. Influence of Maternal Obesity on the Long-Term Health of Offspring. Lancet Diabetes Endocrinol. 2017, 5, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.; Nilsson, I.A.K.; Gissler, M.; Lavebratt, C. Associations of Maternal Diabetes and Body Mass Index with Offspring Birth Weight and Prematurity. JAMA Pediatr. 2019, 173, 371. [Google Scholar] [CrossRef]
- Ornoy, A.; Reece, E.A.; Pavlinkova, G.; Kappen, C.; Miller, R.K. Effect of Maternal Diabetes on the Embryo, Fetus, and Children: Congenital Anomalies, Genetic and Epigenetic Changes and Developmental Outcomes. Birth Defects Res. Part C Embryo Today Rev. 2015, 105, 53–72. [Google Scholar] [CrossRef]
- Sheiner, E. Gestational Diabetes Mellitus: Long-Term Consequences for the Mother and Child Grand Challenge: How to Move on Towards Secondary Prevention? Front. Clin. Diabetes Healthc. 2020, 1, 546256. [Google Scholar] [CrossRef]
- Mustad, V.A.; Huynh, D.T.T.; López-Pedrosa, J.M.; Campoy, C.; Rueda, R. The Role of Dietary Carbohydrates in Gestational Diabetes. Nutrients 2020, 12, 385. [Google Scholar] [CrossRef]
- McGowan, C.A.; McAuliffe, F.M. The Influence of Maternal Glycaemia and Dietary Glycaemic Index on Pregnancy Outcome in Healthy Mothers. Br. J. Nutr. 2010, 104, 153–159. [Google Scholar] [CrossRef]
- Harmon, K.A.; Gerard, L.; Jensen, D.R.; Kealey, E.H.; Hernandez, T.L.; Reece, M.S.; Barbour, L.A.; Bessesen, D.H. Continuous Glucose Profiles in Obese and Normal-Weight Pregnant Women on a Controlled Diet. Diabetes Care 2011, 34, 2198–2204. [Google Scholar] [CrossRef]
- Geiker, N.R.; Magkos, F.; Zingenberg, H.; Svare, J.; Chabanova, E.; Thomsen, H.S.; Ritz, C.; Astrup, A. A High-Protein Low–Glycemic Index Diet Attenuates Gestational Weight Gain in Pregnant Women with Obesity: The “An Optimized Programming of Healthy Children” (APPROACH) Randomized Controlled Trial. Am. J. Clin. Nutr. 2022, 115, 970–979. [Google Scholar] [CrossRef]
- Goletzke, J.; De Haene, J.; Stotland, N.E.; Murphy, E.J.; Perez-Rodriguez, M.; King, J.C. Effect of a Low-Glycemic Load Diet Intervention on Maternal and Pregnancy Outcomes in Obese Pregnant Women. Nutrients 2021, 13, 748. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Han, S.; Chen, G.-C.; Li, Z.-N.; Silva-Zolezzi, I.; Parés, G.V.; Wang, Y.; Qin, L.-Q. Effects of Low-Glycemic-Index Diets in Pregnancy on Maternal and Newborn Outcomes in Pregnant Women: A Meta-Analysis of Randomized Controlled Trials. Eur. J. Nutr. 2018, 57, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Bruno, R.; Petrella, E.; Bertarini, V.; Pedrielli, G.; Neri, I.; Facchinetti, F. Adherence to a Lifestyle Programme in Overweight/Obese Pregnant Women and Effect on Gestational Diabetes Mellitus: A Randomized Controlled Trial. Matern. Child. Nutr. 2017, 13, e12333. [Google Scholar] [CrossRef] [PubMed]
- Poston, L.; Bell, R.; Croker, H.; Flynn, A.C.; Godfrey, K.M.; Goff, L.; Hayes, L.; Khazaezadeh, N.; Nelson, S.M.; Oteng-Ntim, E.; et al. Effect of a Behavioural Intervention in Obese Pregnant Women (the UPBEAT Study): A Multicentre, Randomised Controlled Trial. Lancet Diabetes Endocrinol. 2015, 3, 767–777. [Google Scholar] [CrossRef]
- Rhodes, E.T.; Pawlak, D.B.; Takoudes, T.C.; Ebbeling, C.B.; Feldman, H.A.; Lovesky, M.M.; Cooke, E.A.; Leidig, M.M.; Ludwig, D.S. Effects of a Low–Glycemic Load Diet in Overweight and Obese Pregnant Women: A Pilot Randomized Controlled Trial. Am. J. Clin. Nutr. 2010, 92, 1306–1315. [Google Scholar] [CrossRef]
- Deng, Y.; Yu, J.; Tao, A.; Liu, J.; Wang, Q.; Cao, Y.; Han, S.; Xu, X.; Yan, X.; Fang, X.; et al. Effect of Low-Glycemic Index Diet Advice on Pregnant Outcomes in Women with Elevated Risk of Gestational Diabetes Mellitus: A Meta-Analysis of Randomized Controlled Trails. Clin. Nutr. ESPEN 2023, 57, 501–509. [Google Scholar] [CrossRef]
- Calancie, L.; Brown, M.; Choi, W.; Caouette, J.; McCann, J.; Werner, E. A Systematic Review of Interventions in Early Pregnancy Among Pregnant Individuals at Risk for Hyperglycemia; INPLASY—International Platform of Registered Systematic Review and Meta-analysis Protocols: Middletown, DE, USA, 2024. [Google Scholar]
- Saros, L.; Hart, K.; Koivuniemi, E.; Egan, B.; Raats, M.; Laitinen, K. Micronutrient Supplement Recommendations in Pregnancy Vary across a Geographically Diverse Range of Countries: A Narrative Review. Nutr. Res. 2024, 123, 18–37. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis Model Assessment: Insulin Resistance and ?-Cell Function from Fasting Plasma Glucose and Insulin Concentrations in Man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef]
- Antuna-Puente, B.; Disse, E.; Rabasa-Lhoret, R.; Laville, M.; Capeau, J.; Bastard, J.-P. How Can We Measure Insulin Sensitivity/Resistance? Diabetes Metab. 2011, 37, 179–188. [Google Scholar] [CrossRef]
- Kirwan, J.P.; Huston-Presley, L.; Kalhan, S.C.; Catalano, P.M. Clinically Useful Estimates of Insulin Sensitivity During Pregnancy. Diabetes Care 2001, 24, 1602–1607. [Google Scholar] [CrossRef]
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International Association of Diabetes and Pregnancy Study Groups Recommendations on the Diagnosis and Classification of Hyperglycemia in Pregnancy. Diabetes Care 2010, 33, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Floch, J.-P.L.; Escuyer, P.; Baudin, E.; Baudon, D.; Perlemuter, L. Blood Glucose Area Under the Curve: Methodological Aspects. Diabetes Care 1990, 13, 172–175. [Google Scholar] [CrossRef] [PubMed]
- Coustan, D.R.; Lowe, L.P.; Metzger, B.E.; Dyer, A.R. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study: Paving the Way for New Diagnostic Criteria for Gestational Diabetes Mellitus. Am. J. Obstet. Gynecol. 2010, 202, 654.e1–654.e6. [Google Scholar] [CrossRef] [PubMed]
- Nathan, D.M.; Kuenen, J.; Borg, R.; Zheng, H.; Schoenfeld, D.; Heine, R.J.; for the A1c-Derived Average Glucose (ADAG) Study Group. Translating the A1C Assay Into Estimated Average Glucose Values. Diabetes Care 2008, 31, 1473–1478. [Google Scholar] [CrossRef]
- Cosson, E.; Carbillon, L.; Valensi, P. High Fasting Plasma Glucose during Early Pregnancy: A Review about Early Gestational Diabetes Mellitus. J. Diabetes Res. 2017, 2017, 8921712. [Google Scholar] [CrossRef]
- Simmons, D.; Immanuel, J.; Hague, W.M.; Teede, H.; Nolan, C.J.; Peek, M.J.; Flack, J.R.; McLean, M.; Wong, V.; Hibbert, E.; et al. Treatment of Gestational Diabetes Mellitus Diagnosed Early in Pregnancy. N. Engl. J. Med. 2023, 388, 2132–2144. [Google Scholar] [CrossRef]
- Sweeting, A.; Hannah, W.; Backman, H.; Catalano, P.; Feghali, M.; Herman, W.H.; Hivert, M.-F.; Immanuel, J.; Meek, C.; Oppermann, M.L.; et al. Epidemiology and Management of Gestational Diabetes. Lancet 2024, 404, 175–192. [Google Scholar] [CrossRef]
- Moses, R.G.; Luebcke, M.; Davis, W.S.; Coleman, K.J.; Tapsell, L.C.; Petocz, P.; Brand-Miller, J.C. Effect of a Low-Glycemic-Index Diet during Pregnancy on Obstetric Outcomes. Am. J. Clin. Nutr. 2006, 84, 807–812. [Google Scholar] [CrossRef]
- Yamamoto, J.M.; Kellett, J.E.; Balsells, M.; García-Patterson, A.; Hadar, E.; Solà, I.; Gich, I.; Van Der Beek, E.M.; Castañeda-Gutiérrez, E.; Heinonen, S.; et al. Gestational Diabetes Mellitus and Diet: A Systematic Review and Meta-Analysis of Randomized Controlled Trials Examining the Impact of Modified Dietary Interventions on Maternal Glucose Control and Neonatal Birth Weight. Diabetes Care 2018, 41, 1346–1361. [Google Scholar] [CrossRef]
- Clapp III, J.F. Maternal Carbohydrate Intake and Pregnancy Outcome. Proc. Nutr. Soc. 2002, 61, 45–50. [Google Scholar] [CrossRef]
- Markovic, T.P.; Muirhead, R.; Overs, S.; Ross, G.P.; Louie, J.C.Y.; Kizirian, N.; Denyer, G.; Petocz, P.; Hyett, J.; Brand-Miller, J.C. Randomized Controlled Trial Investigating the Effects of a Low–Glycemic Index Diet on Pregnancy Outcomes in Women at High Risk of Gestational Diabetes Mellitus: The GI Baby 3 Study. Diabetes Care 2016, 39, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J.M.; McGowan, C.A.; Mahony, R.; Foley, M.E.; McAuliffe, F.M. Low Glycaemic Index Diet in Pregnancy to Prevent Macrosomia (ROLO Study): Randomised Control Trial. BMJ 2012, 345, e5605. [Google Scholar] [CrossRef] [PubMed]
- Tanvig, M.; Wehberg, S.; Vinter, C.; Joergensen, J.; Ovesen, P.; Beck-Nielsen, H.; Jensen, D.; Christesen, H. Pregestational Body Mass Index Is Related to Neonatal Abdominal Circumference at Birth—A Danish Population-based Study. BJOG Int. J. Obstet. Gynaecol. 2013, 120, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Tanvig, M.; Vinter, C.A.; Jørgensen, J.S.; Wehberg, S.; Ovesen, P.G.; Beck-Nielsen, H.; Christesen, H.T.; Jensen, D.M. Effects of Lifestyle Intervention in Pregnancy and Anthropometrics at Birth on Offspring Metabolic Profile at 2.8 Years: Results from the Lifestyle in Pregnancy and Offspring (LiPO) Study. J. Clin. Endocrinol. Metab. 2015, 100, 175–183. [Google Scholar] [CrossRef]
- Koletzko, B.; Godfrey, K.M.; Poston, L.; Szajewska, H.; van Goudoever, J.B.; de Waard, M.; Brands, B.; Grivell, R.M.; Deussen, A.R.; Dodd, J.M.; et al. Nutrition During Pregnancy, Lactation and Early Childhood and Its Implications for Maternal and Long-Term Child Health: The Early Nutrition Project Recommendations. Ann. Nutr. Metab. 2019, 74, 93–106. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologist. Weight Gain during Pregnancy. Committee Opinion No. 548. Obstet Gynecol 2013, 121, 210–212. [Google Scholar] [CrossRef]
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.; Boyle, J.A.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; Rode, L.; et al. Association of Gestational Weight Gain With Maternal and Infant Outcomes: A Systematic Review and Meta-Analysis. JAMA 2017, 317, 2207. [Google Scholar] [CrossRef]
- Phelan, S.; Wing, R.R.; Brannen, A.; McHugh, A.; Hagobian, T.A.; Schaffner, A.; Jelalian, E.; Hart, C.N.; Scholl, T.O.; Munoz-Christian, K.; et al. Randomized Controlled Clinical Trial of Behavioral Lifestyle Intervention with Partial Meal Replacement to Reduce Excessive Gestational Weight Gain. Am. J. Clin. Nutr. 2018, 107, 183–194. [Google Scholar] [CrossRef]
- Koivusalo, S.B.; Rönö, K.; Klemetti, M.M.; Roine, R.P.; Lindström, J.; Erkkola, M.; Kaaja, R.J.; Pöyhönen-Alho, M.; Tiitinen, A.; Huvinen, E.; et al. Gestational Diabetes Mellitus Can Be Prevented by Lifestyle Intervention: The Finnish Gestational Diabetes Prevention Study (RADIEL). Diabetes Care 2016, 39, 24–30. [Google Scholar] [CrossRef]
- Dodd, J.M.; Turnbull, D.; McPhee, A.J.; Deussen, A.R.; Grivell, R.M.; Yelland, L.N.; Crowther, C.A.; Wittert, G.; Owens, J.A.; Robinson, J.S.; et al. Antenatal Lifestyle Advice for Women Who Are Overweight or Obese: LIMIT Randomised Trial. BMJ 2014, 348, g1285. [Google Scholar] [CrossRef]
- Facchinetti, F.; Vijai, V.; Petrella, E.; Gambigliani Zoccoli, S.; Pignatti, L.; Di Cerbo, L.; Neri, I. Food Glycemic Index Changes in Overweight/Obese Pregnant Women Enrolled in a Lifestyle Program: A Randomized Controlled Trial. Am. J. Obstet. Gynecol. MFM 2019, 1, 100030. [Google Scholar] [CrossRef] [PubMed]
- Dorise, B.; Byth, K.; McGee, T.; Wood, A.; Blumenthal, C. A Low Intensity Dietary Intervention for Reducing Excessive Gestational Weight Gain in an Overweight and Obese Pregnant Cohort. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2020, 25, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Daly, N.; Farren, M.; McKeating, A.; O’Kelly, R.; Stapleton, M.; Turner, M.J. A Medically Supervised Pregnancy Exercise Intervention in Obese Women: A Randomized Controlled Trial. Obstet. Gynecol. 2017, 130, 1001–1010. [Google Scholar] [CrossRef]
- Adamczak, L.; Mantaj, U.; Sibiak, R.; Gutaj, P.; Wender-Ozegowska, E. Physical Activity, Gestational Weight Gain in Obese Patients with Early Gestational Diabetes and the Perinatal Outcome—A Randomised–Controlled Trial. BMC Pregnancy Childbirth 2024, 24, 104. [Google Scholar] [CrossRef]
- Van Poppel, M.N.M.; Simmons, D.; Devlieger, R.; Van Assche, F.A.; Jans, G.; Galjaard, S.; Corcoy, R.; Adelantado, J.M.; Dunne, F.; Harreiter, J.; et al. A Reduction in Sedentary Behaviour in Obese Women during Pregnancy Reduces Neonatal Adiposity: The DALI Randomised Controlled Trial. Diabetologia 2019, 62, 915–925. [Google Scholar] [CrossRef]
- Vinter, C.A.; Jensen, D.M.; Ovesen, P.; Beck-Nielsen, H.; Jørgensen, J.S. The LiP (Lifestyle in Pregnancy) Study. Diabetes Care 2011, 34, 2502–2507. [Google Scholar] [CrossRef]
- Trak-Fellermeier, M.A.; Campos, M.; Meléndez, M.; Pomeroy, J.; Palacios, C.; Rivera-Viñas, J.; Méndez, K.; Febo, I.; Willett, W.; Gillman, M.W.; et al. PEARLS Randomized Lifestyle Trial in Pregnant Hispanic Women with Overweight/Obesity: Gestational Weight Gain and Offspring Birthweight. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 225–238. [Google Scholar] [CrossRef]
- Barquiel, B.; Calvo, M.; Moreno-Domínguez, Ó.; Martínez-Sánchez, N.; Muner, M.; Bedate, M.F.; Delgado, M.; López, S.; Hillman, N.; González, N.; et al. The PREDG Study: A Randomised Controlled Trial Testing Whether an Educational Intervention Can Prevent Gestational Weight Gain in Women with Obesity. Clin. Nutr. ESPEN 2023, 57, 266–271. [Google Scholar] [CrossRef]
- Goldstein, R.F.; Boyle, J.A.; Cooray, S.D.; Joham, A.E.; Fitz-Gerald, A.L.; Enticott, J.; Harrison, C.L.; Teede, H.J. Implementation Effectiveness of an Antenatal Lifestyle Intervention to Optimize Gestational Weight Gain in Women with Obesity. Obesity 2025, 33, 54–66. [Google Scholar] [CrossRef]
- Maitland, R.; Patel, N.; Barr, S.; Sherry, C.; Marriage, B.; Seed, P.; Garcia Fernandez, L.; Lopez Pedrosa, J.M.; Murphy, H.; Rueda, R.; et al. A Slow-Digesting, Low-Glycemic Load Nutritional Beverage Improves Glucose Tolerance in Obese Pregnant Women Without Gestational Diabetes. Diabetes Technol. Ther. 2018, 20, 672–680. [Google Scholar] [CrossRef]
- Rogozińska, E.; Zamora, J.; Marlin, N.; Betrán, A.P.; Astrup, A.; Bogaerts, A.; Cecatti, J.G.; Dodd, J.M.; Facchinetti, F.; Geiker, N.R.W.; et al. Gestational Weight Gain Outside the Institute of Medicine Recommendations and Adverse Pregnancy Outcomes: Analysis Using Individual Participant Data from Randomised Trials. BMC Pregnancy Childbirth 2019, 19, 322. [Google Scholar] [CrossRef] [PubMed]
| Assessment | Screening ≤ 14+6 Weeks | Visit 1/Baseline 15+0–16+6 Weeks | Visit 2 27+0–28+6 Weeks | Visit 3 34+0–36+0 Weeks | Visit 4 Parturition |
|---|---|---|---|---|---|
| Verify Eligibility | √ | √ | |||
| Informed consent(s) | √ | ||||
| Pre-pregnancy BMI | √ | ||||
| Subject medical and family history, demographic data | √ | ||||
| SP taste test | √ | ||||
| Socioeconomic information | √ | ||||
| Current medication(s)/supplement(s) | √ | √ | √ | √ | |
| Randomization | √ | ||||
| Anthropometry | √ | √ | √ | ||
| Pregnancy/maternal health | √ | √ | √ | ||
| Fetal ultrasounds | √ | √ | √ | ||
| QoL questionnaires (EQ-5D, IPAQ, EPDS, FFQ) | √ | √ | √ | ||
| Fasting blood samples 1 | √ | √ | √ | ||
| OGTT (75 g, 2 h) | √ | √ | |||
| GDM diagnosis | √ | ||||
| Distribution of SP, nutritional information, and Product Intake Records (IG only) | √ | √ | √ | ||
| Palatability questionnaire (IG only) | √ | √ | |||
| Delivery and newborn data | √ | ||||
| Infant PEA POD® and anthropometry | √ | ||||
| Umbilical cord blood 2 | √ | ||||
| Umbilical cord tissue | √ | ||||
| Placental tissue 2 | √ | ||||
| Adverse Events | √ | √ | √ | √ | |
| Maternal blood at delivery 1,2 | √ | ||||
| Colostrum sample | √ | ||||
| Infant meconium and buccal cheek swab | √ |
| Demographic and Lifestyle Parameters | IG (n = 230) | SOC (n = 102) | p | |
|---|---|---|---|---|
| Maternal Age | 31.43 ± 0.34 | 30.39 ± 0.56 | 0.10 | |
| Parity | 0 | 45.2% (104) | 45.1% (46) | 0.12 |
| 1 | 43.9% (101) | 36.3% (37) | ||
| >1 | 10.9% (25) | 18.6% (19) | ||
| Main Ethnicity | German | 0.9% (2) | 1% (1) | 0.82 |
| Spanish | 91.7% (211) | 90.2% (92) | ||
| South American | 2.6% (6) | 4% (4) | ||
| Arabic | 2.2% (5) | 3.9% (4) | ||
| African | 0.4% (1) | 0% (0) | ||
| Other | 2.2% (5) | 1% (1) | ||
| Current Job Situation | Going to school or college full-time | 3% (7) | 2% (2) | <0.001 |
| In paid employment or self-employed | 55% (127) | 40% (41) | ||
| On a government employment | 2% (4) | 8% (8) | ||
| Looking after home or family | 40% (92) | 46% (47) | ||
| Doing something else | 0% (0) | 4% (4) | ||
| Highest Educational Level | <High school/secondary school | 13% (29) | 20% (20) | 0.071 |
| High school equivalent | 12% (27) | 7% (7) | ||
| High school | 20% (47) | 15% (15) | ||
| Some college/Professional training | 28% (64) | 36% (37) | ||
| University: Diploma course/Degree | 22% (51) | 22% (22) | ||
| Postgraduate (Master, PhD.) | 5% (12) | 1% (1) | ||
| Total Years of Full-Time Education | 14.00 (12.00, 17.00) | 13.00 (10.00, 15.00) | 0.057 | |
| Smoking | Never | 55% (127) | 50% (51) | 0.63 |
| Ex-gave up before pregnancy | 20% (46) | 25% (26) | ||
| Ex gave up during pregnancy | 9% (20) | 7% (7) | ||
| Currently | 16% (37) | 18% (18) | ||
| Alcohol (per week) consumed pre-pregnancy | 0.00 (0.00, 1.00) | 0.00 (0.00, 1.00) | 0.74 | |
| Maternal parameters at Baseline/Visit 1 | ||||
| Weight (kg) | 91.99 ± 0.88 | 92.47 ± 1.16 | 0.75 | |
| Height (cm) | 1.63 ± 0.004 | 1.63 ± 0.006 | 0.73 | |
| BMI (kg/m2) | 34.47 ± 0.26 | 34.84 ± 0.39 | 0.47 | |
| BMI 30–34.99 (kg/m2) | 65.7% (151) | 61.8% (63) | 0.64 | |
| BMI 35–39.99 (kg/m2) | 25.7% (59) | 29.4% (30) | ||
| BMI ≥ 40 (kg/m2) | 8.7% (20) | 8.8% (9) | ||
| Triceps SF (mm) | 34.26 ± 0.47 | 33.19 ± 0.68 | 0.21 | |
| Biceps SF (mm) | 25.72 ± 0.46 | 25.25 ± 0.65 | 0.56 | |
| Subscapular SF (mm) | 35.80 ± 0.55 | 35.17 ± 0.99 | 0.55 | |
| Suprailiac SF (mm) | 41.90 ± 0.66 | 40.52 ± 1.14 | 0.27 | |
| Arm Diastolic Blood Pressure (mm Hg) | 62.20 ± 0.53 | 64.59 ± 0.76 | 0.012 | |
| Pulse (beats/min) | 85.85 ± 0.66 | 84.43 ± 1.01 | 0.24 | |
| Glucose (mg/dL) | 84.71 ± 0.60 | 80.45 ± 0.98 | <0.001 | |
| Cholesterol (mg/dL) | 203.68 ± 2.14 | 205.86 ± 3.52 | 0.58 | |
| Triglycerides (mg/dL) | 135.93 ± 2.84 | 139.47 ± 4.99 | 0.51 | |
| Hemoglobin A1c (%) | 5.140 ± 0.017 | 5.089 ± 0.025 | 0.097 | |
| Insulin (µU/mL) | 11.52 ± 0.36 | 10.29 ± 0.42 | 0.044 | |
| HOMA-IR | 2.446 ± 0.087 | 2.071 ± 0.094 | 0.010 | |
| AUC | 13,516.54 ± 210.53 | 13,073.08 ± 291.99 | 0.22 | |
| AAUC | 3415.00 ± 183.47 | 3453.08 ± 271.48 | 0.91 | |
| Visit | Variable | Evaluable | |||
|---|---|---|---|---|---|
| IG (n = 119) | SOC (n = 76) | p | p * | ||
| 2 | MFBG (mg/dL) | 85.82 ± 0.80 | 82.20 ± 0.96 | 0.05 | 0.48 |
| HOMA-IR | 2.96 ± 0.17 | 2.53 ± 0.12 | 0.072 | 0.91 | |
| Insulin (µU/mL) | 13.62 ± 0.65 | 12.46 ± 0.59 | 0.22 | 0.79 | |
| HbA1c (%) | 5.084 ± 0.026 | 5.100 ± 0.036 | 0.72 | 0.064 | |
| 3 | MFBG (mg/dL) | 83.39 ± 0.83 | 80.21 ± 0.95 | 0.015 | 0.13 |
| HOMA-IR | 2.94 ± 0.13 | 2.76 ± 0.16 | 0.39 | 0.49 | |
| Insulin (µU/mL) | 14.12 ± 0.56 | 13.73 ± 0.75 | 0.70 | 0.26 | |
| HbA1c (%) | 5.26 ± 0.03 | 5.31 ± 0.04 | 0.31 | 0.007 | |
| Variable * | IG | SOC | padj |
|---|---|---|---|
| MFBG (mg/dL) | −1.3845 ± 0.5057 | −0.1521 ± 0.6067 | 0.12 |
| Insulin (µU/mL) | 0.9927 ± 0.2662 | 1.7406 ± 0.3265 | 0.077 |
| HOMA-IR | 0.1609 ± 0.0640 | 0.3383 ± 0.0784 | 0.081 |
| HbA1c (%) | 0.0500 ± 0.0121 | 0.1093 ± 0.0154 | 0.0028 |
| Cohort | ITT | Evaluable | ||||||
|---|---|---|---|---|---|---|---|---|
| PEA POD® Parameters | IG (n = 77) | SOC (n = 49) | p | padj | IG (n = 35) | SOC (n = 47) | p | padj |
| Fat (%) | 9.70 ± 0.54 | 8.33 ± 0.57 | 0.098 | 0.14 | 9.71 ± 0.76 | 8.17 ± 0.58 | 0.11 | 0.22 |
| FM (kg) | 0.33 ± 0.02 | 0.27 ± 0.02 | 0.047 | 0.065 | 0.34 ± 0.03 | 0.26 ± 0.02 | 0.034 | 0.095 |
| FFM (%) | 90.31 ± 0.54 | 91.73 ± 0.57 | 0.085 | 0.12 | 90.29 ± 0.76 | 91.89 ± 0.59 | 0.094 | 0.20 |
| FFM (kg) | 2.876 ± 0.054 | 2.881 ± 0.051 | 0.96 | 0.98 | 2.95 ± 0.09 | 2.89 ± 0.05 | 0.53 | 0.82 |
| Body mass (kg) | 3.25 ± 0.05 | 3.15 ± 0.07 | 0.17 | 0.17 | 3.35 ± 0.08 | 3.15 ± 0.06 | 0.039 | 0.10 |
| Body Volume (L) | 3.11 ± 0.05 | 2.96 ± 0.07 | 0.056 | 0.068 | 3.20 ± 0.08 | 2.96 ± 0.07 | 0.023 | 0.078 |
| Body density (kg/L) | 1.047 ± 0.001 | 1.050 ± 0.001 | 0.056 | 0.087 | 1.047 ± 0.001 | 1.049 ± 0.001 | 0.12 | 0.26 |
| FM density (kg/L) | 0.8964 ± 0.0043 | 0.9007 ± 0.00 | 1 | - | 0.9007 ± 0.00 | 0.9007 ± 0.00 | 1 | - |
| FFM density (kg/L) | 1.090 ± 0.0003 | 1.065 ± 0.0001 | 0.57 | 0.63 | 1.065 ± 0.0005 | 1.065 ± 0.0001 | 0.41 | 0.50 |
| Body surface area (cm2) | 2223.88 ± 19.64 | 2182.80 ± 25.45 | 0.20 | 0.22 | 2262.58 ± 30.55 | 2186.35 ± 26.03 | 0.061 | 0.16 |
| Thoracic gas volume (L) | 0.144 ± 0.038 | 0.122 ± 0.019 | 0.67 | 0.55 | 0.191 ± 0.083 | 0.123 ± 0.020 | 0.37 | 0.27 |
| Anthropometry | IG (n = 144) | SOC (n = 71) | p | padj | IG (n = 72) | SOC (n = 65) | p | padj |
| Weight (g) | 3368.88 ± 36.78 | 3239.19 ± 58.35 | 0.053 | 0.10 | 3417.27 ± 50.54 | 3268.81 ± 56.48 | 0.051 | 0.18 |
| Length (cm) | 49.83 ± 0.20 | 49.33 ± 0.31 | 0.17 | 0.27 | 50.06 ± 0.25 | 49.50 ±0.29 | 0.15 | 0.60 |
| HC (cm) | 32.54 ± 0.16 | 31.86 ± 0.26 | 0.15 | 0.21 | 34.73 ± 0.23 | 31.88 ± 0.27 | 0.045 | 0.22 |
| AC (cm) | 32.54 ± 0.16 | 31.86 ± 0.26 | 0.021 | 0.021 | 32.73 ± 0.23 | 31.88 ± 0.27 | 0.017 | 0.074 |
| SF Biceps (mm) | 4.64 ± 0.12 | 4.90 ± 0.24 | 0.27 | 0.10 | 4.67 ± 0.18 | 4.88 ± 0.26 | 0.51 | 0.20 |
| SF Triceps (mm) | 5.41 ± 0.12 | 5.44 ± 0.21 | 0.91 | 0.59 | 5.34 ± 0.17 | 5.31 ± 0.20 | 0.91 | 0.61 |
| SF Subscapular (mm) | 5.03 ± 0.10 | 5.01 ± 0.17 | 0.94 | 0.69 | 4.95 ± 0.12 | 4.93 ± 0.17 | 0.91 | 0.56 |
| SF Suprailiac (mm) | 4.08 ± 0.09 | 3.97 ± 0.12 | 0.47 | 0.94 | 4.13 ± 0.12 | 3.94 ± 0.12 | 0.27 | 0.67 |
| Time Point | Variable | n | IG | n | SOC | p | |
|---|---|---|---|---|---|---|---|
| Mother | V2 | Total AUC | 49 | 14,339.39 ± 365.06 | 37 | 14,211.89 ± 399.09 | 0.17 |
| AAUC | 49 | 4484.69 ± 326.99 | 37 | 4410.81 ± 385.67 | 0.35 | ||
| MFBG (mg/dL) | 90 | 83.46 ± 0.82 | 72 | 81.58 ± 0.93 | 0.72 | ||
| Insulin (µU/mL) | 90 | 12.67 ± 0.56 | 72 | 12.37 ± 0.61 | 0.73 | ||
| HOMA-IR | 90 | 2.641 ± 0.135 | 72 | 2.490 ± 0.125 | 0.95 | ||
| HbA1c (%) | 84 | 5.06 ± 0.03 | 55 | 5.10 ± 0.04 | 0.022 | ||
| V3 | MFBG (mg/dL) | 86 | 81.74 ± 0.92 | 68 | 80.37 ± 0.98 | 0.49 | |
| Insulin (µU/mL) | 85 | 13.51 ± 0.60 | 68 | 13.88 ± 0.78 | 0.20 | ||
| HOMA-IR | 85 | 2.73 ± 0.13 | 67 | 2.79 ± 0.16 | 0.28 | ||
| HbA1c (%) | 78 | 5.24 ± 0.04 | 60 | 5.31 ± 0.04 | 0.003 | ||
| Neonate | PEA POD® | Fat (%) * | 26 | 9.54 ± 0.96 | 45 | 8.11 ± 0.61 | 0.27 |
| FM (kg) * | 26 | 0.33 ± 0.04 | 45 | 0.26 ± 0.02 | 0.11 | ||
| FFM (%) * | 26 | 90.46 ± 0.96 | 45 | 91.96 ± 0.61 | 0.24 | ||
| FFM (kg) * | 26 | 2.99 ± 0.055 | 45 | 2.89 ± 0.053 | 0.23 | ||
| Body mass (kg) * | 26 | 3.32 ± 0.09 | 45 | 3.15 ± 0.06 | 0.11 | ||
| Body Volume (L) * | 26 | 3.17 ± 0.09 | 45 | 2.96 ± 0.07 | 0.10 | ||
| Body density (kg/L) * | 26 | 1.047 ± 0.002 | 45 | 1.049 ± 0.001 | 0.29 | ||
| FM density (kg/L) * | 26 | 0.9007 ± 0.0000 | 45 | 0.9007 ± 0.0000 | - | ||
| FFM density (kg/L) * | 26 | 1.064 ± 0.001 | 45 | 1.065 ± 0.000 | 0.31 | ||
| Body surface area (cm2) * | 26 | 2253.75 ± 35.21 | 45 | 2187.16 ± 26.75 | 0.15 | ||
| Thoracic gas volume (L) * | 26 | 0.22 ± 0.11 | 45 | 0.12 ± 0.02 | 0.21 | ||
| Anthropometry | Weight (g) * | 52 | 3371.06 ± 62.61 | 64 | 3253.13 ± 56.32 | 0.17 | |
| Length (cm) * | 50 | 50.01 ± 0.29 | 63 | 49.51 ± 0.30 | 0.42 | ||
| HC (cm) * | 50 | 34.77 ± 0.40 | 63 | 34.01 ± 0.20 | 0.15 | ||
| AC (cm) * | 50 | 32.70 ± 0.26 | 60 | 31.84 ± 0.28 | 0.08 | ||
| SF Biceps (mm) * | 50 | 4.83 ± 0.22 | 61 | 4.93 ± 0.26 | 0.47 | ||
| SF Triceps (mm) * | 50 | 5.44 ± 0.20 | 61 | 5.32 ± 0.21 | 0.91 | ||
| SF Subscapular (mm) * | 50 | 5.01 ± 0.14 | 61 | 4.88 ± 0.17 | 0.87 | ||
| SF Suprailiac (mm) * | 49 | 4.28 ± 0.15 | 59 | 3.93 ± 0.13 | 0.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
G. Bermúdez, M.; García-Ricobaraza, M.; García-Santos, J.A.; Segura, M.T.; Puertas-Prieto, A.; Gallo-Vallejo, J.L.; Padilla-Vinuesa, C.; Koletzko, B.; Baggs, G.E.; Oliveros, E.; et al. Effect of a Low Glycemic Index/Slow Digesting (LGI/SD) Carbohydrate Product on Maternal Glycemia and Neonatal Body Composition in Obese Pregnant Women: The NIGOHealth Randomized Clinical Trial. Nutrients 2025, 17, 1942. https://doi.org/10.3390/nu17111942
G. Bermúdez M, García-Ricobaraza M, García-Santos JA, Segura MT, Puertas-Prieto A, Gallo-Vallejo JL, Padilla-Vinuesa C, Koletzko B, Baggs GE, Oliveros E, et al. Effect of a Low Glycemic Index/Slow Digesting (LGI/SD) Carbohydrate Product on Maternal Glycemia and Neonatal Body Composition in Obese Pregnant Women: The NIGOHealth Randomized Clinical Trial. Nutrients. 2025; 17(11):1942. https://doi.org/10.3390/nu17111942
Chicago/Turabian StyleG. Bermúdez, Mercedes, María García-Ricobaraza, José Antonio García-Santos, M. Teresa Segura, Alberto Puertas-Prieto, José Luis Gallo-Vallejo, Carmen Padilla-Vinuesa, Berthold Koletzko, Geraldine E. Baggs, Elena Oliveros, and et al. 2025. "Effect of a Low Glycemic Index/Slow Digesting (LGI/SD) Carbohydrate Product on Maternal Glycemia and Neonatal Body Composition in Obese Pregnant Women: The NIGOHealth Randomized Clinical Trial" Nutrients 17, no. 11: 1942. https://doi.org/10.3390/nu17111942
APA StyleG. Bermúdez, M., García-Ricobaraza, M., García-Santos, J. A., Segura, M. T., Puertas-Prieto, A., Gallo-Vallejo, J. L., Padilla-Vinuesa, C., Koletzko, B., Baggs, G. E., Oliveros, E., Rueda, R., & Campoy, C. (2025). Effect of a Low Glycemic Index/Slow Digesting (LGI/SD) Carbohydrate Product on Maternal Glycemia and Neonatal Body Composition in Obese Pregnant Women: The NIGOHealth Randomized Clinical Trial. Nutrients, 17(11), 1942. https://doi.org/10.3390/nu17111942









