Abstract
This study investigated trends within a custom Sports Nutrition Assessment for Consultation (SNAC) survey designed to identify nutrition-related risk factors among post-operative lower-extremity youth athletes. Athletes aged 8–18 years who completed the SNAC at a sports medicine institution after lower-extremity surgery were reviewed for associations between SNAC questions and age/sex differences. Of 477 patients (15.0 ± 2.0 years; 47.8% female), 319 (66.9%) answered ‘yes’ to at least one question and were identified for a consult, though 216 (64.3%) declined. The most frequent questions to prompt a consult were a desire to better understand nutrition for recovery (41.5%) and regularly skipping at least one meal a day (29.8%). Inter-question responses were often significantly related, especially regarding appetite changes, weight changes, and/or meal-skipping. While consult acceptance was not significantly different between sex/age, males were more likely to report a desire to better understand nutrition (p = 0.004) and a weight change (p = 0.019), and females were more likely to report struggling with dizziness/fatigue (p < 0.001). Additionally, older athletes reported an appetite change (p = 0.022), meal-skipping (p = 0.002), a desire to better understand nutrition (p < 0.001), a weight change (p < 0.001), and an effort/recommendation to change their body composition/weight (p = 0.005). These findings demonstrate a link between risky nutrition behaviors and physical detriments.
1. Introduction
In the United States, nearly 27 million youths aged 6 to 17 years participate in sports and athletic activities [1]. Across recent years, participation trends demonstrate that youth athletes compete on multiple teams, train year-round, and specialize in sports at an early age, creating a highly competitive and demanding athletic environment [1,2,3]. This high level of participation underscores the importance of addressing the unique nutritional needs of this population. In addition to the energy demand required of daily activity, training, and competition, the typical youth athlete faces a unique stage of development when their body also requires energy to meet the demands of growth [4]. It is known that adolescence is a period of heightened nutritional demands due to growth and athletic activities combined with the unhealthy eating patterns and risky behaviors that occur in competitive athletics and the nutrition knowledge gap of this population [5]. Specifically, behaviors of adolescent athletes may include skipping meals, restrictive eating, over-exercising, and increasing dehydration risk with restriction of fluid intake, use of diuretics and saunas, and/or wearing nonporous suits to drastically increase production of sweat [6,7]. Furthermore, adolescent athletes often utilize nutritional supplements with the intention of improving athletic performance [8]. Those who participate in sports that emphasize body composition as a direct predictor of performance, such as leanness in distance runners, gymnasts, and dancers, face an especially high occurrence of disordered eating behaviors and attitudes in addition to body dissatisfaction [4,5,6].
While these behaviors can negatively influence athletic performance, they become increasingly harmful to the developing athlete who has sustained an injury. An optimal, balanced diet is extremely important to an athlete’s recovery and rehabilitation. Specifically, the recent literature has emphasized the importance of high-quality proteins, fat, vitamins, antioxidants, minerals, and other supplements during exercise-based rehabilitation to support athletes’ anabolism [9]. The essential role of energy and macronutrients requirements has been extensively investigated, indicating that athletes in recovery require high consumptions of energy via adequate carbohydrates and proteins [10]. Nutrition plays a crucial role in fighting muscle atrophy and anabolic resistance, managing inflammation and providing the body with adequate energy to heal [5]. Thus, it is critical to work with an athlete on their eating attitudes and behaviors during post-injury recovery. Improving nutrition habits can support the healing process, physical therapy efforts, and performance for recovered athletes returning to sport [10]. Thus, a Sports Nutrition Assessment for Consultation (SNAC) survey designed for injured youth athletes facing recovery may facilitate appropriate and effective interventions to promote their healing and support their futures as competitive athletes.
Numerous articles have recently published nutrition recommendations for youth athletes postoperatively [10,11,12,13], recent work has investigated sex and age differences in objective, nutrition-related measures (i.e., BMI, body composition) immediately postoperative [14,15], and one recent article was found validating a postoperative nutrition assessment of energy intake for adolescent athletes [16], but to our knowledge, there is no evidence that addresses the overall population of youth athletes and their nutrition-related risk factors immediately following surgical treatment. This is likely because no validated tool is currently available to screen patients for nutrition-related risk factors (i.e., attitudes, behaviors, and experiences) as they face post-operative recovery beyond provider discretion. The purpose of this study was to investigate trends within the responses of a custom sports nutrition assessment in the interest of better identifying nutrition-related risk factors among a post-operative lower-extremity patient cohort. As each question of the SNAC was designed to identify a different potential risk factor in nutrition-specific behaviors, it is important for clinicians employing the SNAC in clinic to understand how certain risky behaviors relate to others. For example, if a patient has experienced a recent change in weight, they may have recently started skipping meals or perhaps they are also feeling dizzy or fatigued at practice. While these behaviors may be intuitively related, the current study aims to highlight evidence-based associations. Additional areas of interest were age- and sex-related differences in SNAC responses. It was hypothesized that the SNAC would identify relationships between nutrition-related risk factors in a post-operative youth athlete cohort and that age- and sex-related differences would exist. Specifically, nutrition-related behaviors, such as skipping meals or aiming to change body composition, were anticipated to be strongly associated with poor sport experiences, including a history of stress fractures or experiencing dizziness or fatigue during training. Additionally, it was hypothesized that older female athletes would report worse nutrition-related risk factors.
2. Methods
2.1. Participants
The current study received institutional review board approval with a waiver of informed consent before initiation of study procedures. Specifically, informed consent from patients was waived as all data collected and analyzed for the current study was captured as standard-of-care (i.e., the nutrition assessment is provided in clinic to all sports medicine patients post-operative). Thus, the current analysis was determined by the institutional review board to not expose patients to a greater than minimal risk and not adversely affect patients’ rights and welfare. A retrospective review of patients who underwent lower-extremity surgery at a single sports medicine treatment center was performed. Inclusion criteria were patients aged 8–18 years old, evaluated between 30 November 2021 and 19 January 2023 at their first post-operative clinic visit. No patients were excluded due to missing data.
2.2. Procedures
Patient-specific information was assessed through patient-reported electronic intake questionnaires that were administered at clinic visits as standard of care. Demographic variables were captured in addition to menstrual period dates for female respondents and specific SNAC responses.
An experienced sports medicine dietitian, in collaboration with other sports medicine medical staff, designed a custom sports nutrition assessment to identify potential nutrition-related risk factors immediately following surgery in a youth athlete population. The SNAC is a 9 to 14-question survey with ‘yes’ and ‘no’ response options (Table 1). The number of questions a participant receives depends on their sex, as females receive more questions than males regarding status of menarche. Each question of the SNAC investigates a different aspect of nutrition such as nutrition habits and preferences, fueling behaviors, goals, weight changes, and medical history of illnesses or symptoms related to under fueling. While most nutrition assessments in the recent literature focus on consumption (contents and frequency) [17,18] and/or nutritional knowledge [17,19,20,21], the primary goal in developing the SNAC was to identify risky behaviors, and/or experiences or feelings that may lead to risky behaviors, that may be mitigated through intervention via a consultation with a sports medicine dietitian. In addition to the influence of consumption- and knowledge-focused questionnaires, some questions are also based on a well-established nutrition risk screen developed for seniors [22] but have been adapted for the youth sport context.

Table 1.
Frequency (N, %) of responses to the Sports Nutrition Assessment for Consultation (SNAC).
At the first post-operative clinic visit, the SNAC was completed electronically either by the patient or a parent. Answering ‘yes’ to any of the SNAC questions prompted a question asking the patient/parent if they would like a consultation with a sports dietitian. Additionally, female patients who responded ‘yes’ to missing a menstrual cycle for 3 months or more and those female patients who were 15 years or older and said they had not yet started their menstrual cycle were also prompted with the consultation question. If the patient chose ‘no’ to consulting with the sports dietitian, they were prompted to select why they chose against the consultation.
2.3. Statistical Analysis
Descriptive statistics (means, standard deviations, and frequencies) were computed for each variable. Fisher’s exact tests were used to determine whether nonrandom associations existed between the binary variables collected. Comparisons included responses between SNAC questions and sex differences in response to the SNAC. For each comparative test between SNAC questions, odds ratios were also computed to quantify the strength of the association between positive responses for each question. Independent samples t-tests were performed to determine age-related differences across binary variables (sex, SNAC questions, response to a consultation). Significance level (α) was set to 0.05, and no data were missing from the standard eight nutrition questions. Statistical analysis was performed using SPSS (IBM Corp., Armonk, NY, USA, https://www.ibm.com/spss).
3. Results
In total, 477 patients (15.0 ± 2.0 years) completed the SNAC of which 228 (47.8%) were female. Of the female patients, 209 (92.5%) reported having had a period, and 17 (8.5%) reported having recently ‘gone longer than 3 months without a period’. Across all respondents, 319 (66.9%) answered ‘yes’ to at least one question on the SNAC, indicating a considerable proportion of patients exhibited a nutrition-related risk factor. The most common positive responses indicated a popular desire to better understand nutrition for recovery purposes (198, 41.5%), followed by whether the patient regularly skipped at least one meal a day (142, 29.8%; Table 1). In contrast, the majority of respondents indicated that they did not have a history of stress fractures (456, 95.6%), struggle with dizziness or fatigue during training (441, 92.5%), or have any food allergies or intolerances (434, 91.0%). Of the 336 (68.2%) that were asked about their interest in a sports dietitian consult, 216 (64.3%) declined, primarily reporting that they did not feel as though it applied to them (Table 2).

Table 2.
Frequency (N, %) of responses to a sports dietitian consult.
Furthermore, responses between questions were found to be significantly related (Table 3), especially for questions focusing on a change in appetite, change in weight, and/or skipping meals. Notably, minimal associations were identified with reporting a positive response to having food allergies/intolerances, a history of stress fractures, or a struggle with dizziness or fatigue during training. Specifically, respondents reporting a recent change in weight were 2.18 times more likely to report food allergies or intolerances (p = 0.042). Respondents reporting a history of stress fractures were 2.96 and 2.80 times more likely to indicate a desire to better understand nutrition for recovery purposes (p = 0.016) and a recent change in weight (p = 0.045), respectively. Respondents who indicated struggling with dizziness or fatigue during games, practices, or with exercise were 3.52 times more likely to report a recent change in appetite (p = 0.002), 2.89 times more likely to regularly skip at least one meal a day (p = 0.002), and 3.10 times more likely to be trying to or receiving a recommendation to change their body composition or weight (p = 0.003). Lastly, respondents were significantly more likely to express an interest in a consultation if they also indicated a desire to better understand nutrition (OR: 5.00, p < 0.001), experienced a recent change in weight (OR: 2.96, p < 0.001), or were trying to or received a recommendation to change their body composition or weight (OR: 1.65, p = 0.040).

Table 3.
Odds ratios per inter-question association for the Sports Nutrition Assessment for Consultation (SNAC) questions and consult inquiry.
3.1. Sex Comparison
A total of 149 females (65.4% of females) and 170 males (68.3% of males) were prompted about a potential consult (Table 2). While the frequency of positive responses to the consult inquiry was not significantly different between sexes (p = 0.422), males and females did significantly differ in their response to individual questions of the SNAC (Table 1 and Figure 1). Specifically, males were more likely to report that they wished they had a better understanding of their nutrition for their recovery (p = 0.004) and that they had experienced a recent change in their weight (p = 0.019). Alternatively, females were more likely to report struggling with dizziness or fatigue during training (p < 0.001).
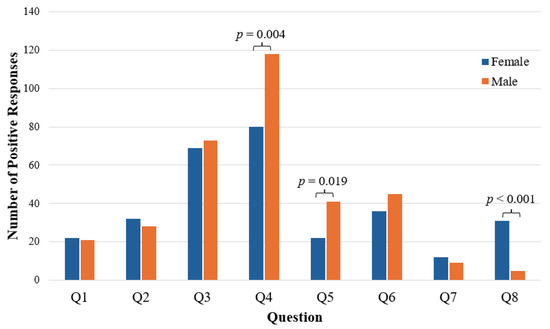
Figure 1.
Sex differences in SNAC responses.
3.2. Age Comparison
No significant difference in age was identified by sex (p = 0.292). However, female respondents who indicated having had a period were significantly older (Yes: 209, 15.2 ± 1.7 years; No: 17, 12.8 ± 1.7 years; p < 0.001). Regarding the SNAC responses, age-related differences were found among five of the eight questions (Table 4). Significantly older respondents reported a recent change in appetite (p = 0.022), regularly skipping at least one meal a day (p = 0.002), a desire to better understand nutrition for their recovery (p < 0.001), a recent change in weight (p < 0.001), and trying to or receiving a recommendation to change their body composition or weight (p = 0.005). However, it is important to note that the greatest mean difference in age was only 0.82 years.

Table 4.
Age differences by the Sports Nutrition Assessment for Consultation (SNAC) question.
4. Discussion
The purpose of the current study was to investigate trends among responses of a custom Sports Nutrition Assessment for Consultation (SNAC) survey created to indicate potential nutrition-related risk factors in a lower-extremity patient cohort post-operatively. While an emphasis on nutrition after sports surgery is addressed in the recent literature [14,15], the current study contains the only questionnaire created to identify specific habits which are risk factors for post-operative recovery to our knowledge. The identification of specific risk factors may assist in understanding which athletes are at risk of delayed recovery or reinjury. While post-operative weight, sex, age, and other risk factors are also valuable, some are non-modifiable and others may be directly reflective of a recent surgery (limited ability to eat, etc.). Conversely, the SNAC assesses modifiable risk factors which are likely more reflective of pre-surgical attitudes. The primary reasons patients were identified for a nutrition consult were that they (1) wished they better understood nutrition for recovery, (2) skipped at least one meal a day, or (3) were trying to or someone recommended they change their weight or body composition. These results support the recent literature investigating the lack of nutrition knowledge in adolescent athletes. A 2020 study found that young athletes lack key knowledge specifically related to Daily Recommended Intakes and supplements, or when they do have such knowledge, it comes from “unqualified or non-professional sources” [23]. This lack of knowledge has been further reported on in a review by Brown et al. (2021) [24], which emphasized that acquiring accurate food and nutrition knowledge could improve individuals’ ability to make healthy choices and build optimal dietary habits.
As 67% of athletes were identified for a consult but 64% declined, most often due to feeling as though it did not apply to them (57%), more responsibility rests with the clinician to coach proper post-operative nutrition. The feeling of athletes that the consult does not apply to them may be due to a belief that the athlete can handle their rehabilitation independently, potential embarrassment, or the determination that their positive response does not actually indicate poor nutrition. As clinicians, greater care to explain the normalcy of nutrition difficulties during rehabilitation may assuage some athlete concerns, and telehealth options may improve the burden on those concerned about time or cost. While some positive responses may indicate normal development, such as recent weight changes after a growth spurt, clinicians must look for responses which cannot be explained by a patient history and suggest further counseling. Athletes will benefit from meeting with a registered dietitian or receiving educational handouts/videos, if a dietitian is unavailable, to enable the athlete to optimize their nutrition in the way most needed for their return to sport. The SNAC has the potential to flag athletes struggling with disordered eating behaviors and indicate to a clinician which athletes put their current recovery at risk.
4.1. Weight Concerns
Young athletes feel pressure to meet certain standards set by sport culture, society, coaches, parents, teammates or themselves. The positive responses to questions regarding a “recent change in weight” (13%) and “trying to or someone recommended I change my body weight or body composition” (17%) indicate that young athletes are already regularly concerned with weight and body image. The past ten years have seen a rise in studies assessing social media [25,26] and other body image views [27,28,29] of children as parents and providers have witnessed the negative impact poor body image can have on athletic participation and mental wellness [30]. For example, Bird and Rushton (2020) stated that athletes, specifically those in weight-based or aesthetic sports, are at higher risk of feeling pressure to restrict their energy intake. While we traditionally associate these concerns with older athletes, studies have also found that childhood, specifically the preschool and elementary school age, is often the critical stage when body image attitudes develop [31]. In fact, one study found that 50% of children between the ages of 7 and 12 years old wished to be slimmer [32]. These findings are important for clinicians to understand as concerns about weight and body shape in the younger years could compromise psychological health throughout later stages of life and increase the individual’s risk for eating disorders, particularly during the vulnerable stage of recovery [32,33]. The current study primarily involved post-menarchal athletes, but future work may look at similar nutrition survey data in even younger athletes.
4.2. Appetite and Under Fueling
Responses regarding a recent change in appetite, recent change in weight, and skipping at least one meal a day were found to be significantly related with those experiencing weight changes having a 3.93 times greater odds of appetite changes and 2.27 times greater odds of skipping meals. Our findings suggest that the majority of young athletes surveyed in the current study have inconsistent eating patterns, often skipping meals (30%), which is similar to recent results published in other studies on child and adolescent eating habits [6,23,34]. Due to child and adolescent athletes’ higher energy and nutrient needs, making all meals and eating additional snacks throughout the day is necessary to support proper growth and development, prevent burnout, and protect against nutrition-related injuries [35,36]. However, adolescent eating patterns are often characterized by meal-skipping, frequent snacking, and a higher intake of fast food [4,8,24] which may lead to under fueling of important nutrients such as calcium, iron, magnesium, and iodine [37,38].
Though not intuitively surprising, respondents struggling with dizziness and fatigue were more likely to also report a recent change in appetite (3.52 times), skipping meals (2.89 times), and recommendations to change their body composition (3.10 times). Someone trying to change their weight (especially during the early recovery phase) might view skipping meals as a method for weight loss, which could lead to under fueling that materializes as dizziness and fatigue with activity. This is concerning as it can set up the athlete for poor physical therapy sessions, muscle atrophy, and delayed recovery. The relationship found between a reported history of stress fractures, a desire to better understand nutrition for recovery, and a reported recent change in weight likely represent a continuation of this same under fueling issue that, if not addressed, could delay an injured athlete’s recovery and return to sport.
4.3. Sex- and Age-Related Differences
Both sexes may benefit from a sports nutrition consult after injury as 65.4% of females and 68.3% of males were identified in this study, but the reasons for this consult may differ. Males were more likely to report a desire to better understand nutrition and a recent weight change, while females were more likely to report struggling with fatigue and dizziness with exercise. Females often tend to desire a “leaner silhouette”, while males often desire a “larger body” [33]. Clinical experience dictates that females’ desire to be thinner can often lead to complications of under fueling, such as dizziness and fatigue with exercise. This under fueling has been estimated at nearly 50% in female athletes aged 15–30 years [39,40]. Even when females meet traditional sports nutrition standards for essential ingredients, such standards tend to be based largely on male athlete needs and may not adequately guide female athletes to avoid the effects of low energy availability [40]. Additionally, while a portion of males desire to be thinner or “leaner”, many male youth athletes desire to be bigger and more muscular which can often lead to supplement use, confusion on the best ways to gain weight and build muscle, and a desire to learn more about nutrition—which was assessed on the SNAC. Though the SNAC did not assess the direction of weight change, it is possible that weight changes represent an outcome of this desire for education on strength building. Alternatively, it may be that male athletes are less accustomed to calorie restriction, and during the immediate post-operative period at which they were assessed, males found themselves with undesired weight gain and more interest in learning about how to address it from a dietitian.
The data did not demonstrate age-related differences when comparing sex, but age-related differences were demonstrated in five of the eight SNAC questions with older respondents more frequently reporting a recent appetite change, skipping meals, a desire to understand nutrition, a recent weight change, and trying or being recommended to change body composition or weight. Athletes at older ages are more likely to participate in club- or national-level sport, which may both introduce them to poor nutrition habits which they believe to maximize their performance and provide them with an opportunity to work with team-sponsored dietitians. Similarly, they could be more motivated than the young, recreational athlete to learn about nutrition and take steps to alter their body composition, leading to the higher frequency of positive SNAC responses observed. Even in the absence of competition-level differences, older adolescents undergo a period of physical and psychological transformation during puberty which includes developmental weight and body composition changes as well as more awareness of the perception of others [41], likely reflected in the SNAC. Still, among these significant differences, athletes with positive responses tended to be only about eight months older, and younger children are not exempt from these risks. Thoughts and attitudes around weight have been established in children as young as three years old [31], and girls between the ages of five and seven years old with weight concerns have been more likely to show dietary restraint and other disordered eating behaviors, independent of their individual Body Mass Index [42]. Clinicians should, therefore, address nutrition with all patients post-operatively, taking extra care with those at older ages. An understanding of an athlete’s goals in life and in sport assists the clinician in tailoring the rehabilitation process to each child and providing appropriate dietary recommendations which correspond to their current and desired level of performance.
4.4. Limitations
The current study has certain limitations that should be noted apart from standard limitations associated with patient-reported outcomes which may be subject to under-reporting but also reflect the most feasible method of patient nutrition screening. Given that this study was conducted on athletes with lower-extremity injuries post-operatively at a single sports medicine clinic, the results presented here may not be generalizable to patients with a different injury profile or at another time point of recovery. Although not statistically evaluated given the uneven distributions, differences between races, ethnicities, and sports should be explored further in future studies as the relevant literature has indicated that nutrition behaviors in the general youth may differ based on these factors. Specifically, Lytle et al. reported that poorer diet habits were more commonly observed in African American and Hispanic youth compared to Caucasian students [43], and Neumark-Sztainer et al. found that non-White (i.e., African American, Hispanic, Asian American, and Native American) youth reported notably different weight-related concerns/behaviors [44]. Similarly, among different sports, various nutrition-related risks have been reported. Klein et al. reported that collegiate-level individual sport athletes were more knowledgeable about hydrations and micronutrients than team sport athletes [45], and numerous reports have highlighted sport-specific risk factors related to nutrition [46,47,48], such as with youth runners [48,49,50]. Targeted interventions such as broad testing of athletes at different private and public schools in varying demographics could better support such populations.
Furthermore, the question investigating a recent change in appetite may have a relationship with the timeline of surgical intervention and potentially any pharmaceutical interventions administered post-operatively, which were not considered in the current analysis. Additionally, although this study did not investigate direction of weight gain and/or loss, future work could contribute to this knowledge gap by linking potential relationships between sex, age, and risk factors in nutrition to direction of weight change. A better understanding of these trends (e.g., females or younger athletes may drop considerable weight immediately post-operative compared to their male and/or older counterparts) would help clinicians be more proactive in providing nutrition education or interventions to counteract poor habits or a negative impact on recovery.
5. Conclusions
The long-term goal of this work is to provide the research and clinical community with a valid and reliable tool that will likely improve awareness of nutrition-related risk factors and intervention for youth athletes. There is an urgent need for early screening tools to facilitate prompt detection of disordered eating patterns as well as nutrition knowledge deficits and ensure timely management of risky nutritional behavior that could delay an athlete’s recovery. Overall, 67% of athletes were identified for a nutrition consultation under the criteria of this study. Interest in a nutrition consultation was strongly related to a desire to better understand nutrition, a recent weight change, and a recommendation to change body weight. The significant relationships within the SNAC questions demonstrate the links between nutritionally risky behavior and physical detriments due to under fueling, such as dizziness and/or stress fractures. Given a high overall decline rate toward interest in a sports dietitian consult, often citing that respondents felt it was not applicable to them, more responsibility is placed on the clinician to determine which responses indicate normal development and which responses require further conversation. Quick standard-of-care tools such as the SNAC may assist with screening patients, and clinicians should suggest that athletes who display risky nutrition behaviors meet with a registered dietitian to proactively reduce re-injury risk and improve overall wellness.
Author Contributions
Conceptualization, C.P. and S.U.; Methodology, C.P.; Formal Analysis, S.U.; Investigation, C.P., T.M. and J.D.; Resources, T.M., H.B.E. and P.L.W.; Data Curation, C.P. and S.U.; Writing—Original Draft Preparation, C.P. and J.J.M.; Writing—Review and Editing, T.M., J.D., J.J.M., H.B.E., P.L.W. and S.U.; Visualization, S.U.; Supervision, S.U.; Project Administration, S.U. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of University of Texas Southwestern (STU-2019-0701; 25 July 2022).
Informed Consent Statement
Informed consent from patients was waived as standard-of-care data collected during patient clinic visits were retrospectively reviewed.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request. The data are not publicly available due to ethical reasons.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Child and Adolescent Health Measurement Initiative. 2019 National Survey of Children’s Health (NSCH) Data Query; Resource Center for Child and Adolescent Health Supported by the U.S. Department of Health and Human Services, Maternal and Child Health Bureau (MCHB): Washington, DC, USA, 2019. [Google Scholar]
- Fabricant, P.D.; Robles, A.; Downey-Zayas, T.; Do, H.T.; Marx, R.G.; Widmann, R.F.; Green, D.W. Development and validation of a pediatric sports activity rating scale: The Hospital for Special Surgery Pediatric Functional Activity Brief Scale (HSS Pedi-FABS). Am. J. Sports Med. 2013, 41, 2421–2429. [Google Scholar] [CrossRef] [PubMed]
- Jayanthi, N.A.; LaBella, C.R.; Fischer, D.; Pasulka, J.; Dugas, L.R. Sports-specialized intensive training and the risk of injury in young athletes: A clinical case-control study. Am. J. Sports Med. 2015, 43, 794–801. [Google Scholar] [CrossRef] [PubMed]
- Desbrow, B. Youth Athlete Development and Nutrition. Sports Med. 2021, 51 (Suppl. S1), 3–12. [Google Scholar] [CrossRef] [PubMed]
- Huhmann, K. Menses Requires Energy: A Review of How Disordered Eating, Excessive Exercise, and High Stress Lead to Menstrual Irregularities. Clin. Ther. 2020, 42, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Kontele, I.; Vassilakou, T. Nutritional Risks among Adolescent Athletes with Disordered Eating. Children 2021, 8, 715. [Google Scholar] [CrossRef] [PubMed]
- Hannon, M.P.; Flueck, J.L.; Gremeaux, V.; Place, N.; Kayser, B.; Donnelly, C. Key Nutritional Considerations for Youth Winter Sports Athletes to Optimize Growth, Maturation and Sporting Development. Front. Sports Act. Living 2021, 3, 599118. [Google Scholar] [CrossRef] [PubMed]
- Wahl, R. Nutrition in the adolescent. Pediatr. Ann. 1999, 28, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, S.K.; Mantzorou, M.; Kondyli-Sarika, F.; Alexandropoulou, I.; Papathanasiou, J.; Voulgaridou, G.; Nikolaidis, P.T. The Key Role of Nutritional Elements on Sport Rehabilitation and the Effects of Nutrients Intake. Sports 2022, 10, 84. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, S.K. Rehabilitation Nutrition for Injury Recovery of Athletes: The Role of Macronutrient Intake. Nutrients 2020, 12, 2449. [Google Scholar] [CrossRef]
- Hirsch, K.R.; Wolfe, R.R.; Ferrando, A.A. Pre- and Post-Surgical Nutrition for Preservation of Muscle Mass, Strength, and Functionality Following Orthopedic Surgery. Nutrients 2021, 13, 1675. [Google Scholar] [CrossRef]
- Hoelscher, D.M.; Kirk, S.; Ritchie, L.; Cunningham-Sabo, L. Position of the Academy of Nutrition and Dietetics: Interventions for the prevention and treatment of pediatric overweight and obesity. J. Acad. Nutr. Diet. 2013, 113, 1375–1394. [Google Scholar] [CrossRef] [PubMed]
- Smith-Ryan, A.E.; Hirsch, K.R.; Saylor, H.E.; Gould, L.M.; Blue, M.N.M. Nutritional Considerations and Strategies to Facilitate Injury Recovery and Rehabilitation. J. Athl. Train. 2020, 55, 918–930. [Google Scholar] [CrossRef] [PubMed]
- Mackie, A.T.; Pascual-Leone, N.; Coxe, F.R.; Fabricant, P.D.; Doyle, S.M. No Postoperative Change in Body Mass Index Was Observed Among Adolescent Female Patients After Sports or Trauma Surgery. J. Pediatr. Orthop. Soc. N. Am. 2022, 4, 417. [Google Scholar] [CrossRef]
- Olson, T.; Devana, S.; Papanos, L.; Hame, S. Postoperative Body Composition in NCAA Division I Collegiate Athletes. J. Women’s Sports Med. 2023, 3, 22–29. [Google Scholar] [CrossRef]
- Belarde, C.; Barrack, M.; Gray, V.; Blaine, R. Evaluating the Concurrent Validity of a Web-Based Nutrition Screening Survey among Preadolescent Student Athletes; Department of Family and Consumer Sciences, California State University Long Beach: Long Beach, CA, USA, 2020. [Google Scholar]
- Sánchez-Díaz, S.; Yanci, J.; Raya-González, J.; Scanlan, A.T.; Castillo, D. A Comparison in Physical Fitness Attributes, Physical Activity Behaviors, Nutritional Habits, and Nutritional Knowledge Between Elite Male and Female Youth Basketball Players. Front. Psychol. 2021, 12, 685203. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Espino, K.; Fernández-Tena, C.; Lizarraga-Dallo, M.A.; Farran-Codina, A. Development and Validation of a Short Sport Nutrition Knowledge Questionnaire for Athletes. Nutrients 2020, 12, 3561. [Google Scholar] [CrossRef] [PubMed]
- Manore, M.M.; Patton-Lopez, M.M.; Meng, Y.; Wong, S.S. Sport Nutrition Knowledge, Behaviors and Beliefs of High School Soccer Players. Nutrients 2017, 9, 350. [Google Scholar] [CrossRef] [PubMed]
- Dvorak, T.E.; Jordan, K.C.; Dolan, S.H.; Wing-Gaia, S.L.; Manore, M.M.; Meyer, N.L. The Adolescent Sport Nutrition (SN) Knowledge Questionnaire: Validity and Reliability: 1459: Board #6 May 28 2:00 PM–3:30 PM. Med. Sci. Sports Exerc. 2008, 40, S218. [Google Scholar] [CrossRef]
- Rosi, A.; Ferraris, C.; Guglielmetti, M.; Meroni, E.; Charron, M.; Menta, R.; Manini, F.; Di Gioia, V.; Martini, D.; Erba, D. Validation of a General and Sports Nutrition Knowledge Questionnaire in Italian Early Adolescents. Nutrients 2020, 12, 3121. [Google Scholar] [CrossRef]
- Keller, H.H.; Goy, R.; Kane, S.L. Validity and reliability of SCREEN II (Seniors in the community: Risk evaluation for eating and nutrition, Version II). Eur. J. Clin. Nutr. 2005, 59, 1149–1157. [Google Scholar] [CrossRef]
- Bird, S.P.; Rushton, B.D. Nutritional knowledge of youth academy athletes. BMC Nutr. 2020, 6, 35. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.; Seabrook, J.A.; Stranges, S.; Clark, A.F.; Haines, J.; O’Connor, C.; Doherty, S.; Gilliland, J.A. Examining the Correlates of Adolescent Food and Nutrition Knowledge. Nutrients 2021, 13, 2044. [Google Scholar] [CrossRef] [PubMed]
- Dignard, N.A.L.; Jarry, J.L. The “Little Red Riding Hood effect”: Fitspiration is just as bad as thinspiration for women’s body satisfaction. Body Image 2021, 36, 201–213. [Google Scholar] [CrossRef] [PubMed]
- Prichard, I.; Kavanagh, E.; Mulgrew, K.E.; Lim, M.S.C.; Tiggemann, M. The effect of Instagram #fitspiration images on young women’s mood, body image, and exercise behaviour. Body Image 2020, 33, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Betz, D.E.; Sabik, N.J.; Ramsey, L.R. Ideal comparisons: Body ideals harm women’s body image through social comparison. Body Image 2019, 29, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, C.J.; Desmond, D. The effect of viewing fitness imagery on body dissatisfaction: Sex and physical activity differences. Psychol. Health Med. 2018, 23, 980–986. [Google Scholar] [CrossRef]
- Sundar, T.K.B.; Londal, K.; Lagerlov, P.; Glavin, K.; Helseth, S. Overweight adolescents’ views on physical activity—Experiences of participants in an internet-based intervention: A qualitative study. BMC Public Health 2018, 18, 448. [Google Scholar] [CrossRef]
- Corr, M.; McSharry, J.; Murtagh, E.M. Adolescent Girls’ Perceptions of Physical Activity: A Systematic Review of Qualitative Studies. Am. J. Health Promot. 2019, 33, 806–819. [Google Scholar] [CrossRef]
- Damiano, S.R.; McLean, S.A.; Nguyen, L.; Yager, Z.; Paxton, S.J. Do we cause harm? Understanding the impact of research with young children about their body image. Body Image 2020, 34, 59–66. [Google Scholar] [CrossRef]
- Mendo-Lazaro, S.; Polo-Del-Rio, M.I.; Amado-Alonso, D.; Iglesias-Gallego, D.; Leon-Del-Barco, B. Self-Concept in Childhood: The Role of Body Image and Sport Practice. Front. Psychol. 2017, 8, 853. [Google Scholar] [CrossRef]
- Neves, C.M.; Cipriani, F.M.; Meireles, J.F.F.; Morgado, F.; Ferreira, M.E.C. Body Image in Childhood: An Integrative Literature Review. Rev. Paul. Pediatr. 2017, 35, 331–339. [Google Scholar] [CrossRef]
- Melin, A.K.; Heikura, I.A.; Tenforde, A.; Mountjoy, M. Energy Availability in Athletics: Health, Performance, and Physique. Int. J. Sport. Nutr. Exerc. Metab. 2019, 29, 152–164. [Google Scholar] [CrossRef]
- Meyer, F.; O’Connor, H.; Shirreffs, S.M.; International Association of Athletics, F. Nutrition for the young athlete. J. Sports Sci. 2007, 25 (Suppl. S1), S73–S82. [Google Scholar] [CrossRef]
- Smith, J.W.; Holmes, M.E.; McAllister, M.J. Nutritional Considerations for Performance in Young Athletes. J. Sports Med. 2015, 2015, 734649. [Google Scholar] [CrossRef]
- Spronk, I.; Heaney, S.E.; Prvan, T.; O’Connor, H.T. Relationship Between General Nutrition Knowledge and Dietary Quality in Elite Athletes. Int. J. Sport. Nutr. Exerc. Metab. 2015, 25, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Foo, W.L.; Faghy, M.A.; Sparks, A.; Newbury, J.W.; Gough, L.A. The Effects of a Nutrition Education Intervention on Sports Nutrition Knowledge during a Competitive Season in Highly Trained Adolescent Swimmers. Nutrients 2021, 13, 2713. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, K.E.; Holtzman, B.; Cooper, K.M.; Flynn, E.F.; Bruinvels, G.; Tenforde, A.S.; Popp, K.L.; Simpkin, A.J.; Parziale, A.L. Low energy availability surrogates correlate with health and performance consequences of Relative Energy Deficiency in Sport. Br. J. Sports Med. 2019, 53, 628–633. [Google Scholar] [CrossRef] [PubMed]
- Holtzman, B.; Ackerman, K.E. Recommendations and Nutritional Considerations for Female Athletes: Health and Performance. Sports Med. 2021, 51 (Suppl. S1), 43–57. [Google Scholar] [CrossRef]
- Voelker, D.K.; Reel, J.J.; Greenleaf, C. Weight status and body image perceptions in adolescents: Current perspectives. Adolesc. Health Med. Ther. 2015, 6, 149–158. [Google Scholar] [CrossRef]
- Davison, K.K.; Markey, C.N.; Birch, L.L. A longitudinal examination of patterns in girls’ weight concerns and body dissatisfaction from ages 5 to 9 years. Int. J. Eat. Disord. 2003, 33, 320–332. [Google Scholar] [CrossRef]
- Lytle, L.; Himes, J.; Feldman, H.; Zive, M.; Dwyer, J.; Hoelscher, D.; Webber, L.; Yang, M. Nutrient intake over time in a multi-ethnic sample of youth. Public Health Nutr. 2002, 5, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Croll, J.; Story, M.; Hannan, P.J.; French, S.A.; Perry, C. Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: Findings from Project EAT. J. Psychosom. Res. 2002, 53, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Klein, D.J.; Eck, K.M.; Walker, A.J.; Pellegrino, J.K.; Freidenreich, D.J. Assessment of Sport Nutrition Knowledge, Dietary Practices, and Sources of Nutrition Information in NCAA Division III Collegiate Athletes. Nutrients 2021, 13, 2962. [Google Scholar] [CrossRef] [PubMed]
- North, M.; Kelly, A.; Ranchordas, M.; Cole, M. Nutritional Considerations in High Performance Youth Soccer: A Systematic Review. J. Sci. Sport Exerc. 2022, 4, 195–212. [Google Scholar] [CrossRef]
- Jakše, B.; Jakše, B.; Mis, N.F.; Jug, B.; Šajber, D.; Godnov, U.; Čuk, I. Nutritional Status and Cardiovascular Health in Female Adolescent Elite-Level Artistic Gymnasts and Swimmers: A Cross-Sectional Study of 31 Athletes. J. Nutr. Metab. 2021, 2021, 8810548. [Google Scholar] [CrossRef] [PubMed]
- Petrie, H.J.; Stover, E.A.; Horswill, C.A. Nutritional concerns for the child and adolescent competitor. Nutrition 2004, 20, 620–631. [Google Scholar] [CrossRef] [PubMed]
- Matt, S.A.; Barrack, M.T.; Gray, V.B.; Cotter, J.A.; Van Loan, M.D.; Rauh, M.J.; McGowan, R.; Nichols, J.F. Adolescent Endurance Runners Exhibit Suboptimal Energy Availability and Intakes of Key Nutrients. J. Am. Nutr. Assoc. 2022, 41, 551–558. [Google Scholar] [CrossRef]
- Nieves, J.W.; Melsop, K.; Curtis, M.; Kelsey, J.L.; Bachrach, L.K.; Greendale, G.; Sowers, M.F.; Sainani, K.L. Nutritional Factors That Influence Change in Bone Density and Stress Fracture Risk Among Young Female Cross-Country Runners. PM&R 2010, 2, 740–750. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).