Abstract
Despite evidence suggesting the importance of psychological resilience for successful aging, little is known about the relationship between diet quality and resilience at different ages. Our study aims to examine the association between diet quality and resilience across the stages of adulthood. Using Stanfords’ WELL for Life (WELL) survey data, we conducted a cross-sectional study of diet quality, resilience, sociodemographic, perceived stress, lifestyle, and mental health factors among 6171 Bay Area adults. Diet quality was measured by the WELL Diet Score, which ranges from 0–120. A higher score indicates a better diet quality. Linear regression analysis was used to evaluate the association between the WELL Diet Score and overall resilience and within the following age groups: early young (18–24), late young (25–34), middle (35–49), and late adulthood (≥50). To test whether these associations varied by age groups, an age group by resilience interaction term was also examined. In the fully adjusted model, the WELL Diet Score was positively and significantly associated with overall resilience (all ages (β = 1.2 ± sd: 0.2, p < 0.001)) and within each age group (early young (β = 1.1 ± sd: 0.3, p < 0.001); late young (β = 1.2 ± sd: 0.3, p < 0.001); middle (β = 0.9 ± sd: 0.3, p < 0.001); and late adulthood (β = 1.0 ± sd: 0.3, p < 0.001)). Young adults demonstrated the strongest associations between diet quality and resilience. However, there were no significant age-by-resilience interactions. Diet quality may be positively associated with resilience at all stages of adulthood. Further research is needed to determine whether assessing and addressing resilience could inform the development of more effective dietary interventions, particularly in young adults.
1. Introduction
Diet-related diseases, such as cardiovascular disease (CVD), are among the leading causes of death in the United States [1]. Despite the high prevalence of CVD, most Americans do not adhere to evidence-based dietary guidelines for chronic disease prevention [1,2]. As such, poor diet quality is the most prevalent CVD risk factor in US adults [3,4,5,6,7,8,9,10]. Although age is a well-established risk factor for CVD, it is less commonly recognized that diet quality tends to improve as we progress through subsequent phases of life (e.g., late young adulthood, 25–34 years; middle adulthood, 35–49 years; and late adulthood, 50+ years) [11,12,13]. Thus, enhancing diet quality in early adults is important for preventing and managing CVD risk factors throughout the life course [14,15,16].
High stress adversely affects dietary behaviors, promoting appetite and a preference for foods that are high in fat and sugar. Also, multilevel barriers have made it stressful for Americans to engage in healthy eating [17,18,19]. Over the past few decades, the food system has been flooded with aggressively marketed ultra-processed foods and sugar-sweetened drinks, making it psychologically taxing to engage in healthy eating [20,21,22,23,24]. Thus, identifying psychological assets that can serve as a stress buffer could be a key protective strategy to improving and sustaining a better diet quality, particularly in vulnerable populations [25,26].
Building psychological resilience—the perceived ability to bounce back from stress—may lead to better diet quality. Evidence suggests that psychological resilience (hereafter resilience) increases with age [27,28] and is positively linked to better diet quality in both young and older adults [29,30,31,32,33,34,35], although recent studies have focused on international populations. Compared with a younger person, it stands to reason that an older person may have accumulated more resources and developed greater abilities to cope with stress [36,37,38]. Moreover, behavioral interventions, including resilience training (e.g., meditation, mindful breathing, gratitude, and forgiveness exercises) have been shown to improve diet and diet-related outcomes in older adults [39,40,41,42]. However, definitions and measures of resilience vary in these studies, and evidence in young adults is limited, with even less known about the relationship between diet quality and resilience across adulthood.
To address this gap in the literature, our study aims to examine the relationship between diet quality and resilience while adjusting for perceived stress, sociodemographic, lifestyle, and mental health factors within the young, middle, and late adults enrolled in the Stanford WELL for Life (WELL) study. We hypothesize that resilience will show significant and positive associations with diet quality across age groups, as measured by the WELL Diet Score. Our study explored the link between age, resilience, and diet quality—an understanding that may inform the development of more effective dietary interventions to prevent disease (e.g., CVD) and promote health at varying stages of adulthood.
2. Methods
2.1. Study Design
Our study is a cross-sectional secondary analysis of Stanford WELL survey measures that assesses resilience, perceived stress, and diet-related behaviors. Since it was created within the Stanford Prevention Research Center (SPRC) in 2017, investigators have been using WELL to generate comprehensive scientific data to help define, understand, and improve well-being among people from diverse backgrounds [43]. The WELL study design, protocol, informed consent measures, recruitment, and survey measures have been published elsewhere [43,44,45,46]. Briefly, the WELL Survey consists of 76 items, spanning 10 domains of well-being. These domains include measures for stress and resilience, experiences of emotions (positive and negative feelings), lifestyle behaviors (physical activity and diet-related behaviors (used to calculate the WELL Diet Score)) as well as demographic and medical history (including self-reported height and weight, hypertension, depression). As of June 2021, 6171 women and men (18 years of age or older) have completed the survey. Participants provided informed consent and the study was approved by the Stanford University Institutional Review Board.
2.2. Measures
2.2.1. Main Outcome
Diet quality is measured by the WELL Diet Score. A detailed description of WELL Diet Score development was previously published [46]. Briefly, following the 2015 evidence-based dietary guidelines for chronic disease prevention, SPRC’s public health professionals developed the WELL Diet Survey (12 items). The WELL Diet Score was assessed by eliciting information regarding dietary intake and meal preparation behaviors.
The WELL Diet Score, ranging from 0–120, is the sum of 12 diet-related items that are rated from 1–10. Scoring criteria is based on the frequency of consumption, with 10 representing the maximum score. Such that, a higher total score indicates a better diet quality (and adherence to evidence-based guidelines). WELL Diet Score items included (1) vegetables, (2) fruits, (3) whole grains, (4) beans or lentils, (5) sugar-sweetened beverages (including 100% fruit juice) (reverse-scored), (6) red/processed meats (reverse-scored), (7) nuts and seeds, (8) high-sodium processed foods (reverse-scored), (9) sugar-sweetened baked goods or candy (reverse-scored), (10) fish, (11) preparing meals at home, and (12) eating fast food (reverse-scored).
2.2.2. Primary Exposure: Resilience
An adapted version of the Brief Resilience Scale and the Connor–Davidson Resilience Scale were used to assess resilience (e.g., “How confident are you that you can bounce back quickly after hard times?” and “How confident are you that you can adapt to change?”). Respondents were asked to indicate their level of confidence on nine items, ranging from “extremely confident” to “not at all confident”. The Resilience Score is the mean value of the nine items and was standardized to range from 0–10. See Supplemental Appendix SA for a detailed description of the resilience items.
2.2.3. Covariates: Sociodemographics, Perceived Stress, Lifestyle (and BMI), and Mental Health
Sociodemographic Variables: Age (years), gender, race/ethnicity (White/Caucasian, Hispanic, Black/African American, Asian, and Other), education (HS or below, some college, college graduate, or graduate), and marital status (married, living with a partner, single, or other) were collected via self-reporting.
Perceived Stress: This was assessed through four items (an adapted version of the Global Measure of Perceived Stress). For example: “During the last two weeks, how often have you felt that you were not able to give enough time to the important things in your life, or handle the problems you are experiencing?” Respondents were then asked to indicate the frequency of their feelings for each item, ranging from “never” to “very often.” Scores were standardized to range from 0–10. This was reverse-scored such that higher scores indicate lower levels of perceived stress.
Lifestyle (physical activity, smoking status) and BMI variables: Physical activity was assessed through an adapted version of the International Physical Activity Questionnaire and the Stanford Leisure-Time Activity Categorical Item. Participants were asked to consider their physical activity by answering the following question: “During the past month, which statement best describes the kinds of physical activity you usually did? Do not include the time you spent working at a job”. They were given six statements to choose from, ranging from “I did not do much physical activity. I mostly did things like watching television, reading, playing cards, or playing computer games. Only occasionally, no more than once or twice a month, did I do anything more active such as going for a walk or playing tennis” to “Almost daily, that is, five or more times a week, I did vigorous activities such as running or riding hard on a bike for 30 min or more each time”. The scores ranged from 0–10. Smoking status was assessed through the options of “never”, “former”, or “current”; hypertension was self-reported (y/n); and BMI was calculated from self-reported weight and height.
Mental health (depression, positive and negative affect, and wellbeing): History of clinical depression was also self-reported, namely: “Have you ever been told by a doctor or other health professional that you had depression?” (y/n). Positive affect was assessed by a six-item inventory (designed by the WELL team), e.g., “During the last two weeks, how often did you feel content?” Respondents were then asked to indicate the frequency of their feelings for each item, ranging from “never” to “very often”. Negative affect was gauged by a five-item inventory (also WELL designed and reverse-coded). For instance, “During the last two weeks, how often did you feel sad?” Participants were then asked to indicate the frequency of their feelings for each item, ranging from “never” to “very often”. For both positive and negative affect, scores were standardized to range from 0–10. The total WELL Score was tabulated as a measure of well-being by combining scores for all 10 WELL domains, including social connectedness, lifestyle behaviors, physical health, stress and resilience, experience of emotions, purpose and meaning in life, sense of self, financial security, spirituality and religiosity, and exploration and creativity. Scores ranged from 0–100.
2.3. Statistical Analysis
Age groups were defined as: 18–24 (early young adulthood), 25–34 (late young adulthood), 35–49 (middle adulthood), and ≥50 (late adulthood). Descriptive statistics were used to describe participant characteristics overall and by age group. Pearson’s correlation coefficients were calculated for bivariate associations between age (in years), the WELL Diet Score, and the Resilience Score. Linear models regressed the WELL Diet Score on age, Resilience Score, and an age-group-by-resilience interaction term. Overall age-group-stratified linear models were presented following progressive covariate adjustments, including (1) sociodemographics (gender, race, and education), (2) perceived stress, (3) lifestyle and BMI (smoking, physical activity, and BMI), and (4) mental health (history of depression, and positive affect). Note that the total WELL Score was not included in the statistical models. Collinearity was monitored using variance inflation factors. Analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
3. Results
Our study included 6171 adults with a mean age of 39 years (38.8; see Table 1). On average, WELL participants were predominantly white (60.9%), female (71.7%), college-educated (69.1%), had a healthy BMI (18.5–24.9) (54.7%), and were non-smokers (96.4%). Nearly half the participants were married or living with a partner, with about 4% of the early young and 65% of the late adult quartiles being married. Twenty-four percent of our participants reported being depressed; similar percentages were found in each stage of adulthood. Approximately 13% of participants reported hypertension, 4% of which were early young adults and 30% of which were late adults. Overall, WELL participants reported moderate levels of perceived stress (reverse-scored) (mean of 5.5 out of 10 for the early young adults and mean of 6.5 out of 10 for late adults). Similarly, WELL participants in all stages of adulthood had moderately high perceptions of their resilience (mean of 6.7 out of 10 for the early young adults and mean of 7.0 out of 10 for late adults). Both positive and negative emotion (reverse-scored) scales demonstrated similar trends to resilience. WELL Diet Scores ranged from 58.7 in the youngest adults to 80.2 in late adulthood, with a mean for all ages of about 70 out of 120, suggesting that the overall diet quality could be improved in all age groups.

Table 1.
Participant characteristics by stages of adulthood (quartile age groups in years).
Young adults (both early and late) reported WELL Diet Scores above and below the median of the total sample (which was 71 (IQR: 56–85)) compared with middle and late adults.
We found that both resilience and WELL Diet Scores were higher in older age groups, and the latter was significantly and moderately correlated with age (r = 0.40; p < 0.001). In terms of resilience, there was a significant positive and weak correlation with age (r = 0.11; p < 0.001). WELL Diet Scores and resilience also had a significant and positive correlation (r = 0.25; p < 0.001). Perceived stress had negative and significant correlations with age (r = 0.23), the WELL Diet Score (r = 0.29), and resilience (r = 0.53), respectively (see Supplementary Figures S1–S4).
As indicated in Table 2, all models demonstrated a significant and positive relationship between diet quality and resilience. The crude assessments have beta-coefficients of 2 across all age groups, and they attenuate with each successive addition to the model such that the beta-coefficients become smaller until the values for all age groups are close to 1. In the fully adjusted model, resilience remained significantly and positively associated with diet quality among all ages, after adjustment for perceived stress, sociodemographic, lifestyle and BMI, and mental health variables. Note all models were statistically significant, with the fully adjusted models showing the strongest association between diet quality and resilience in young adults. There were no significant interactions with age group (see Figure 1).

Table 2.
Associations between resilience and the WELL Diet Score overall and by adulthood stage.
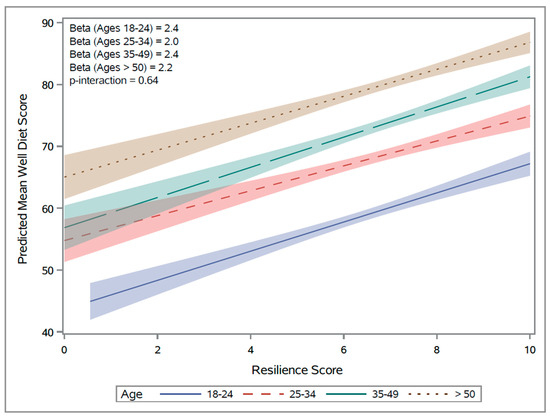
Figure 1.
Resilience Score vs. predicted WELL Diet Score. Note that the unadjusted slopes are presented here based on the crude values.
4. Discussion
Our cross-sectional study examined the associations between diet quality and resilience among participants enrolled in the WELL study (early young, late young, middle, and late adulthood). These participants were predominantly white, college-educated, and relatively healthy females from California’s Northern Bay Area. We found significant associations between diet quality and resilience overall and within each age group. Although the associations were stronger among young (18–24 and 25–34 years of age) compared with middle-aged and older adults (35–49 and 50+ years of age), in the fully adjusted model of our sample, we did not observe a significant interaction between age and resilience. Our findings add to the theoretical and empirical evidence suggesting that perceived resilience, perceived stress, and diet quality increase with age and are therefore modifiable. Considering that addressing mental health in behavioral intervention research is becoming increasingly important, resilience may be an important starting point in the development of effective dietary interventions for CVD prevention at all ages, but especially among early young adults (18–24) [47,48,49].
Over the past decade, several cross-sectional studies have found a significant and positive association between diet quality and resilience [29,30,31,32,33,34,35]. These findings extended to multiple subpopulations, including both older and younger adults in the US and abroad. For example, using data from a large sample of predominantly white older women (mean age 77 years N = 77,395) enrolled in the Women’s Health Initiative, Springfield and colleagues (2020) found that high levels of resilience (as measured by the Brief Resilience Scale) were associated with CVD-related protective factors, including 22% greater odds of having a better diet quality (as measured by the Healthy Eating Index 2015 (HEI-2015)) (OR = 1.22 (95% confidence interval (1.15–1.30)) after adjusting for perceived stress, race/ethnicity, level of education, BMI, hypertension, diabetes, and high cholesterol [29]. Likewise, Lutz and colleagues (2017) found that young male and female adult Army and Air Force recruits (mean age 21 years; N = 656) with high resilience (as measured by the Connor–Davidson Scale) reported a higher diet quality (measured by the Healthy Eating Index 2010 (HEI-2010)) after adjusting for age, sex, race and ethnicity, education, smoking, and BMI [35].
Internationally, a large cross-sectional analysis of 10,812 Italian middle-aged adults recruited in the Moli-sani study (mean age 35 yrs., 52% female) showed that diet quality (as measured by the Greek Mediterranean Diet Index, Italian Mediterranean Diet Index, and olive oil and vegetables pattern) was positively associated with resilience (per the Connor–Davidson Scale) [30]. Roberts and colleagues (2022) reported similar findings in a French sample of predominantly older white women enrolled in the NutriNet-Santé Study (73.5% female, mean age 55.4 yrs.). They found that resilience (per the Brief Resilience Scale) was significantly and positively associated with diet quality (as measured by the modified French National Nutrition and Health Program Guideline Score and the NOVA classification system for ultra-processed foods [31,50].
Despite decades of research conceptualizing the broader relationships between health behavior, stressors, coping, and resilience, little is known about the potential mechanisms relating resilience to diet quality [51]. Individuals who can effectively cope with stressors (e.g., emotional distress and low access to high-quality foods) are more likely to practice healthier dietary behaviors than those who cannot [52]. In contrast, healthier diets may have a more positive effect on brain processes and mental health through the gut microbiome [53,54,55]. More research is needed to understand these biopsychological pathways, as well as how they can build on existing resilience-related positive psychology constructs to improve diet quality, particularly in the context of psychological distress [56].
Despite our sample’s social advantages (e.g., high education, physical activity, non-smoking, and relative well-being), they reported high levels of stress and depression (pre-pandemic). Approximately 25% of our participants reported a history of depression, and these percentages may be significantly higher than national averages [57,58]. Based on self-reported data from 2021 SAMHSA reports, women had a higher prevalence of major depressive episodes (10.3%) than men (6.2%), and young adults aged 18 to 25 had the highest prevalence (18.6%) [59]. Resilience has been shown to be protective against daily and chronic stressors and to reduce the risk of depression—a risk factor for poor diet quality and related CVD outcomes [14,60,61,62,63,64,65,66,67,68,69]. Our findings and those of others suggest that resilience is significantly and positively associated with diet quality, even after adjusting for socioeconomic status and depression [46,70]. Thus, building on resilience, rather than focusing solely on deficit-based risk factors, may be a timely and important addition to dietary interventions, especially in younger adults [71].
In our study, early young adults (18–24 years of age) reported the lowest mean WELL Diet Scores, falling in the bottom half of our sample (58.7 ± 18.0 out of 120; IQR: 56–85). These had fewer resources, including significantly lower levels of education, were less likely to be married or to live with a partner, and reported slightly lower scores for measures related to mental health than older adults (including positive/negative emotions and overall well-being (see Table 1)). Several studies suggest that early young adults are targeted by and susceptible to marketing tactics for low-quality, affordable ultra-processed foods [72,73,74,75]. Perhaps younger adults are also less concerned about eating healthily due to their lower risk for diet-related diseases [76]. For example, just over 4% of early young adults reported hypertension in our sample. That percentage grew to 30% in late adults. Further research is warranted to determine whether resilience training, which includes stress management and resource mobilization, can lead to positive influences on the adherence to dietary guidelines for CVD prevention in young adults.
This study fills an important gap in the literature by providing valuable evidence on the relationship between diet quality and resilience throughout adulthood. However, the design, measures, and the generalizability of our findings have limitations. The cross-sectional design of our study inherently limits our ability to establish causal relationships between diet quality and resilience. This is because it does not allow us to assess changes over time, which are crucial for determining cause and effect. While we can examine associations, we are unable to determine whether resilience affects diet quality or vice versa. Our interpretation is that higher resilience leads to better diet quality, the primary outcome of our study.
Regarding our measures, SPRC experts developed several measures for the WELL study. In some cases, items from multiple measures were combined to assess one construct, or original scales were created. Although our adapted measures stem from validated scales, their modifications in our study context necessitate further validation to ensure their reliability and accuracy within our specific research framework. This is true for both our primary exposure (resilience) and main outcome (diet quality) measures. For instance, items from the Brief Resilience Scale and the Connor–Davidson Resilience Scale were combined to measure resilience, despite their differing definitions [77]. According to Ye and colleagues, the former is a belief-based construct, whereas the latter is a resource-based construct. Despite these differences, both scales have been associated with better diet quality in previous studies, are modifiable, and are therefore suitable for intervention [78,79,80]. In this way, their overlapping items could help to clarify the relationship between diet quality and resilience [29,35]. SPRC experts also developed the WELL Diet Score, which has been associated with the Alternative Healthy Eating Index 2010 (AHEI-2010), a diet quality measure proven to be a significant predictor of chronic disease risk [46,81,82].
Given the demographic composition of our study, which was primarily white and college-educated, the generalizability of our findings to the broader U.S. population might be somewhat limited. This is due to the potential underrepresentation of certain demographic groups in our sample. Despite the adaptation and merging of multiple measures, as well as a cumulative score for overall well-being, all WELL measures have been standardized so that they range from 0–10 to provide consistent estimates (described in Table 1). Compared with the national averages for the major racial/ethnic subgroups reported by the US Census 2020, our sample shows that Whites are correctly represented, Asians are overrepresented, and Blacks and Hispanics are underrepresented [83]. Compared with the national averages for the major racial/ethnic subgroups reported by the US Census 2020, our sample shows higher educational attainment [84]. With respect to mental health, we asked about depression over a lifetime compared with the two-week period in the SAMSHA assessment, which may have resulted in higher percentages. Despite this, our estimate may be higher than national averages. Unlike SAMHA, we also asked if depression was diagnosed by a health professional. Due to this, and the fact that depression is often undiagnosed, our estimates are likely to be conservative [85].
Furthermore, since the WELL study is focused on improving well-being, it may have attracted more health-conscious participants, yielding a selection bias. Even still, the diet quality scores remain suboptimal. This may highlight the need to conduct these studies in more racial and ethnic populations, especially those dealing with multiple forms of historical and contemporary oppression (e.g., racism, displacement, and socioeconomic disadvantage) that leave them particularly vulnerable to poor diet quality, stress, and other CVD-related risk factors [86,87].
Our study has numerous strengths and marks a significant contribution to the literature on diet quality and resilience. To the best of our knowledge, ours is the first to examine associations between diet quality and a formal measure of resilience across stages of adulthood in a US general population sample, representing both females and males who are in relatively good health. The primary outcome, of diet quality, is a comprehensive assessment designed to measure adherence to prevention guidelines, which are more robust than individual foods, food groups, or macronutrients. Our study also evaluated psychological resilience through two widely used measures that have been validated in US populations and that are associated with various physical and mental health outcomes, i.e., the Brief Resilience Scale and the Conner–Davidson Scale [88,89,90]. We had more sociodemographic diversity in our sample compared with previous studies, as well as resilience-related measures of well-being. As part of our analysis, we evaluated relevant sociodemographic and psychological confounders, such as education, depression, and positive affect. Another major strength of our study is the large sample size with a broad age range, which enables age stratification to explore potential age-related modifications in the relationship between diet quality and resilience.
5. Conclusions
We have provided foundational evidence of a significant and positive relationship between diet quality and resilience in adults across age groups. Our findings warrant further investigation into whether assessing and potentially intervening to improve resilience could help to increase the effectiveness of dietary interventions for CVD prevention, especially among young adults, who are the most vulnerable to poorer diet quality and stress management and, subsequently, to an earlier onset of other CVD risk factors. Notably, the relationship between resilience and diet quality is significant, even after adjusting for depression (despite its relatively high prevalence in our sample). This highlights the importance of addressing existing psychological assets in dietary intervention, as opposed to just deficit-based risk factors [91].
Accordingly, our findings have implications for strengths-based approaches to dietary interventions; namely, resilience increases with age, and it is modifiable and buildable. By raising awareness of existing levels of resilience before individuals engage in behavioral interventions and other psychological assets, we can create personalized behavioral plans. In turn, these can guide the practices of a wide range of healthcare professionals, including psychologists, dietitians, nurses, physicians, and behavior specialists, whose responsibilities include developing educational materials and care plans that encourage patients to adhere to dietary guidelines for chronic disease prevention and management. Also, behavioral research interventionists may benefit from our findings by incorporating resilience screens into behavioral health studies, particularly in populations with sociodemographic backgrounds that include exposure to multidimensional (multilevel, historical, and contemporary) stressors and trauma.
Considering our findings, resilience training may contribute to an increase in diet quality or an increased adherence to diet patterns for the prevention of cardiovascular disease (CVD), since it can buffer the negative effects of stress on diet quality. Understanding that additional research is needed in this area, as a next step, we will examine the relationship between diet quality and resilience resources in a diverse US representative sample of young African American women.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu16111724/s1, Figure S1 (a,b): Age vs. WELL Diet Score; Figure S2 (a,b): Age vs. Resilience Score; Figure S3 (a–c): (a) Perceived Stress vs. WELL Diet Score, (b) Perceived Stress vs. Age scatterplot, and (c) Perceived Stress vs. Resilience Score; Figure S4: WELL Diet Score vs. Resilience Score; Appendix SA: WELL Resilience Items adapted from the Brief Resilience Scale (BRS) and the Connor Davidson Resilience Scale (CD-RISC).
Author Contributions
Conceptualization, S.S.-T.; methodology, S.S.-T., C.J. and Y.-H.W.; formal analysis, C.J.; data curation, Y.-H.W. and A.W.H., writing—original draft preparation, S.S.-T. and C.J.; writing—review and editing, S.S.-T., C.J., Y.-H.W., K.C., A.W.H. and C.G.; funding acquisition, A.W.H. and C.G. All authors have read and agreed to the published version of the manuscript.
Funding
We want to acknowledge the WELL study participants and staff. WELL community partners should also be acknowledged for their support in recruiting study participants. Foundational funding for the Stanford Wellness Living Laboratory (WELL) was provided by Amway via an unrestricted gift through the Nutrilite Health Institute Wellness Fund and the NHLBI T32 Cardiovascular Prevention Fellowship. Current funding was provided by the NIH-funded ITM Sponsored Loyola University Chicago early career award (K-L2TR002387).
Institutional Review Board Statement
Stanford University’s Institutional Review Board assumed the role of IRB of record for each participant in our study. The WELL study protocol code is FWA00000935, which was approved by the Institutional Review Board on 14 March 2024.
Informed Consent Statement
The study complied with the Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects and the Unified Code of Ethics for Health Education Professionals. Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Acknowledgments
The following should be mentioned for their support of the project and assistance with the manuscript preparation: WELL participants; the Stanford Prevention Research Center staff; the Nutrition, Health Equity and Resilience lab members (including but not limited to Benny Garcia, Keyana Williams, and Quincy Rogers); and the editor Elizabeth Doyle. Our community advisory board, Black Women Nutritious and Joyful (BWNJOY), should also be acknowledged for their input on this line of research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kris-Etherton, P.M.; Petersen, K.S.; Velarde, G.; Barnard, N.D.; Miller, M.; Ros, E.; O’Keefe, J.H.; Williams, K., Sr.; Horn, L.V.; Na, M.; et al. Barriers, Opportunities, and Challenges in Addressing Disparities in Diet-Related Cardiovascular Disease in the United States. J. Am. Heart Assoc. 2020, 9, e014433. [Google Scholar] [CrossRef] [PubMed]
- Mohebi, R.; Chen, C.; Ibrahim, N.E.; McCarthy, C.P.; Gaggin, H.K.; Singer, D.E.; Hyle, E.P.; Wasfy, J.H.; Januzzi, J.L., Jr. Cardiovascular Disease Projections in the United States Based on the 2020 Census Estimates. J. Am. Coll. Cardiol. 2022, 80, 565–578. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.P. Sleep patterns, diet quality and energy balance. Physiol. Behav. 2014, 134, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef] [PubMed]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- Qiao, J.; Lin, X.; Wu, Y.; Huang, X.; Pan, X.; Xu, J.; Wu, J.; Ren, Y.; Shan, P.F. Global burden of non-communicable diseases attributable to dietary risks in 1990-2019. J. Hum. Nutr. Diet. 2022, 35, 202–213. [Google Scholar] [CrossRef] [PubMed]
- George, S.M.; Ballard-Barbash, R.; Manson, J.E.; Reedy, J.; Shikany, J.M.; Subar, A.F.; Tinker, L.F.; Vitolins, M.; Neuhouser, M.L. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: Evidence to inform national dietary guidance. Am. J. Epidemiol. 2014, 180, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Mattei, J.; Fung, T.T.; Li, Y.; Pan, A.; Willett, W.C.; Rimm, E.B.; Hu, F.B. Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation 2015, 132, 2212–2219. [Google Scholar] [CrossRef] [PubMed]
- Zhong, V.W.; Ning, H.; Van Horn, L.; Carnethon, M.R.; Wilkins, J.T.; Lloyd-Jones, D.M.; Allen, N.B. Diet Quality and Long-Term Absolute Risks for Incident Cardiovascular Disease and Mortality. Am. J. Med. 2021, 134, 490–498 e424. [Google Scholar] [CrossRef]
- Micha, R.; Peñalvo, J.L.; Cudhea, F.; Imamura, F.; Rehm, C.D.; Mozaffarian, D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA 2017, 317, 912–924. [Google Scholar] [CrossRef]
- Liu, J.; Rehm, C.D.; Onopa, J.; Mozaffarian, D. Trends in diet quality among youth in the United States, 1999–2016. JAMA 2020, 323, 1161–1174. [Google Scholar] [CrossRef] [PubMed]
- Hiza, H.A.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J. Acad. Nutr. Diet. 2013, 113, 297–306. [Google Scholar] [CrossRef] [PubMed]
- de Andrade, S.C.; Previdelli, A.N.; Cesar, C.L.G.; Marchioni, D.M.L.; Fisberg, R.M. Trends in diet quality among adolescents, adults and older adults: A population-based study. Prev. Med. Rep. 2016, 4, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Harshfield, E.L.; Pennells, L.; Schwartz, J.E.; Willeit, P.; Kaptoge, S.; Bell, S.; Shaffer, J.A.; Bolton, T.; Spackman, S.; Wassertheil-Smoller, S. Association between depressive symptoms and incident cardiovascular diseases. JAMA 2020, 324, 2396–2405. [Google Scholar] [CrossRef] [PubMed]
- Gooding, H.C.; Gidding, S.S.; Moran, A.E.; Redmond, N.; Allen, N.B.; Bacha, F.; Burns, T.L.; Catov, J.M.; Grandner, M.A.; Harris, K.M. Challenges and opportunities for the prevention and treatment of cardiovascular disease among young adults: Report from a National Heart, Lung, and Blood Institute Working Group. J. Am. Heart Assoc. 2020, 9, e016115. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, A.H.; Appel, L.J.; Vadiveloo, M.; Hu, F.B.; Kris-Etherton, P.M.; Rebholz, C.M.; Sacks, F.M.; Thorndike, A.N.; Van Horn, L.; Wylie-Rosett, J. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation 2021, 144, e472–e487. [Google Scholar] [CrossRef] [PubMed]
- Sominsky, L.; Spencer, S.J. Eating behavior and stress: A pathway to obesity. Front. Psychol. 2014, 5, 434. [Google Scholar] [CrossRef]
- Finch, L.E.; Tiongco-Hofschneider, L.; Tomiyama, A.J. Stress-induced eating dampens physiological and behavioral stress responses. In Nutrition in the Prevention and Treatment of Abdominal Obesity; Elsevier: Amsterdam, The Netherlands, 2019; pp. 175–187. [Google Scholar]
- Reichenberger, J.; Kuppens, P.; Liedlgruber, M.; Wilhelm, F.H.; Tiefengrabner, M.; Ginzinger, S.; Blechert, J. No haste, more taste: An EMA study of the effects of stress, negative and positive emotions on eating behavior. Biol. Psychol. 2018, 131, 54–62. [Google Scholar] [CrossRef]
- Lemos, T.C.; Coutinho, G.; Silva, L.A.; Stariolo, J.B.; Campagnoli, R.R.; Oliveira, L.; Pereira, M.G.; Mota, B.E.; Souza, G.G.; Canella, D.S. Ultra-Processed Foods Elicit Higher Approach Motivation Than Unprocessed and Minimally Processed Foods. Front. Public Health 2022, 10, 891546. [Google Scholar] [CrossRef]
- Campbell, N.; Browne, S.; Claudy, M.; Reilly, K.; Finucane, F.M. Ultra-Processed Food: The Tragedy of the Biological Commons. Int. J. Health Policy Manag. 2023, 12, 7557. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.-C.; Louzada, M.L.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Moubarac, J.C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-processed products are becoming dominant in the global food system. Obes. Rev. 2013, 14 (Suppl. S2), 21–28. [Google Scholar] [CrossRef]
- Moodie, R.; Stuckler, D.; Monteiro, C.; Sheron, N.; Neal, B.; Thamarangsi, T.; Lincoln, P.; Casswell, S.; Lancet, N.C.D.A.G. Profits and pandemics: Prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013, 381, 670–679. [Google Scholar] [CrossRef]
- Vilaro, M.J.; Staub, D.; Xu, C.; Mathews, A.E. Theory-Based Interventions for Long-Term Adherence to Improvements in Diet Quality: An In-depth Review. Am. J. Lifestyle Med. 2016, 10, 369–376. [Google Scholar] [CrossRef]
- Rosenbaum, D.L.; White, K.S. The relation of anxiety, depression, and stress to binge eating behavior. J. Health Psychol. 2015, 20, 887–898. [Google Scholar] [CrossRef]
- Woods, N.F.; Rillamas-Sun, E.; Cochrane, B.B.; La Croix, A.Z.; Seeman, T.E.; Tindle, H.A.; Zaslavsky, O.; Bird, C.E.; Johnson, K.C.; Manson, J.E.; et al. Aging Well: Observations From the Women’s Health Initiative Study. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71 (Suppl. S1), S3–S12. [Google Scholar] [CrossRef] [PubMed]
- Krok-Schoen, J.L.; Naughton, M.J.; Felix, A.S.; Wiley Cené, C.; Springfield, S.; Yu, M.; McLaughlin, E.M.; Shadyab, A.H.; Nolan, T.S.; Kroenke, C.H. Resiliency among Women’s Health Initiative women aged 80 and older by race, ethnicity, and neighborhood socioeconomic status. J. Gerontol. Ser. B 2023, 78, 1445–1458. [Google Scholar] [CrossRef]
- Springfield, S.; Qin, F.; Hedlin, H.; Eaton, C.B.; Rosal, M.C.; Taylor, H.; Staudinger, U.M.; Stefanick, M.L. Resilience and CVD-protective Health Behaviors in Older Women: Examining Racial and Ethnic Differences in a Cross-Sectional Analysis of the Women’s Health Initiative. Nutrients 2020, 12, 2107. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; Pounis, G.; Persichillo, M.; Cerletti, C.; Donati, M.; De Gaetano, G.; Iacoviello, L. Mediterranean-type diet is associated with higher psychological resilience in a general adult population: Findings from the Moli-sani study. Eur. J. Clin. Nutr. 2018, 72, 154–160. [Google Scholar] [CrossRef]
- Robert, M.; Shankland, R.; Bellicha, A.; Kesse-Guyot, E.; Deschasaux-Tanguy, M.; Andreeva, V.A.; Srour, B.; Hercberg, S.; Touvier, M.; Leys, C. Associations between resilience and food intake are mediated by emotional eating in the NutriNet-Santé study. J. Nutr. 2022, 152, 1907–1915. [Google Scholar] [CrossRef]
- Voss, M.L.; Currie, C.L. Sleep Quality and the Importance Women Place on Healthy Eating Interact to Influence Psychological Resilience. Am. J. Health Behav. 2022, 46, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Whatnall, M.C.; Patterson, A.J.; Siew, Y.Y.; Kay-Lambkin, F.; Hutchesson, M.J. Are psychological distress and resilience associated with dietary intake among Australian university students? Int. J. Environ. Res. Public Health 2019, 16, 4099. [Google Scholar] [CrossRef] [PubMed]
- Sinska, B.; Jaworski, M.; Panczyk, M.; Traczyk, I.; Kucharska, A. The Role of Resilience and Basic Hope in the Adherence to Dietary Recommendations in the Polish Population during the COVID-19 Pandemic. Nutrients 2021, 13, 2108. [Google Scholar] [CrossRef] [PubMed]
- Lutz, L.J.; Gaffney-Stomberg, E.; Williams, K.W.; McGraw, S.M.; Niro, P.J.; Karl, J.P.; Cable, S.J.; Cropper, T.L.; McClung, J.P. Adherence to the dietary guidelines for Americans is associated with psychological resilience in young adults: A cross-sectional study. J. Acad. Nutr. Diet. 2017, 117, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Springfield, S.; Qin, F.; Hedlin, H.; Eaton, C.B.; Rosal, M.C.; Taylor, H.; Staudinger, U.M.; Stefanick, M.L. Modifiable Resources and Resilience in Racially and Ethnically Diverse Older Women: Implications for Health Outcomes and Interventions. Int. J. Environ. Res. Public Health 2022, 19, 7089. [Google Scholar] [CrossRef] [PubMed]
- Staudinger, U.M. The positive plasticity of adult development: Potential for the 21st century. Am. Psychol. 2020, 75, 540–553. [Google Scholar] [CrossRef]
- Greve, W.; Staudinger, U.M. Resilience in later adulthood and old age: Resources and potentials for successful aging. In Developmental Psychopathology: Volume Three: Risk, Disorder, and Adaptation; Wiley: Hoboken, NJ, USA, 2015; pp. 796–840. [Google Scholar] [CrossRef]
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A.; Harvey, S.B. Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018, 8, e017858. [Google Scholar] [CrossRef] [PubMed]
- Leppin, A.L.; Gionfriddo, M.R.; Sood, A.; Montori, V.M.; Erwin, P.J.; Zeballos-Palacios, C.; Bora, P.R.; Dulohery, M.M.; Brito, J.P.; Boehmer, K.R.; et al. The efficacy of resilience training programs: A systematic review protocol. Syst. Rev. 2014, 3, 20. [Google Scholar] [CrossRef] [PubMed]
- Steinhardt, M.A.; Brown, S.A.; Dubois, S.K.; Harrison, L., Jr.; Lehrer, H.M.; Jaggars, S.S. A resilience intervention in African-American adults with type 2 diabetes. Am. J. Health Behav. 2015, 39, 507–518. [Google Scholar] [CrossRef]
- Steinhardt, M.A.; Mamerow, M.M.; Brown, S.A.; Jolly, C.A. A resilience intervention in African American adults with type 2 diabetes: A pilot study of efficacy. Diabetes Educ. 2009, 35, 274–284. [Google Scholar] [CrossRef]
- Heaney, C.A.; Avery, E.C.; Rich, T.; Ahuja, N.J.; Winter, S.J. Stanford WELL for life: Learning what it means to be well. Am. J. Health Promot. 2017, 31, 449–450. [Google Scholar]
- Chrisinger, B.W.; Gustafson, J.A.; King, A.C.; Winter, S.J. Understanding Where We Are Well: Neighborhood-Level Social and Environmental Correlates of Well-Being in the Stanford Well for Life Study. Int. J. Environ. Res. Public Health 2019, 16, 1786. [Google Scholar] [CrossRef] [PubMed]
- Rich, T.; Chrisinger, B.W.; Kaimal, R.; Winter, S.J.; Hedlin, H.; Min, Y.; Zhao, X.; Zhu, S.; You, S.-L.; Sun, C.-A. Contemplative practices behavior is positively associated with well-being in three global Multi-Regional Stanford WELL for Life Cohorts. Int. J. Environ. Res. Public Health 2022, 19, 13485. [Google Scholar] [CrossRef] [PubMed]
- Springfield, S.; Cunanan, K.; Heaney, C.; Peng, K.; Gardner, C. The WELL diet score correlates with the alternative healthy eating index-2010. Food Sci. Nutr. 2020, 8, 2710–2718. [Google Scholar] [CrossRef] [PubMed]
- Park, J.W.; Mealy, R.; Saldanha, I.J.; Loucks, E.B.; Needham, B.L.; Sims, M.; Fava, J.L.; Dulin, A.J.; Howe, C.J. Multilevel resilience resources and cardiovascular disease in the United States: A systematic review and meta-analysis. Health Psychol. 2022, 41, 278–290. [Google Scholar] [CrossRef] [PubMed]
- Love, M.F.; Wood, G.L.; Wardell, D.W.; Beauchamp, J.E.S. Resilience and associated psychological, social/cultural, behavioural, and biological factors in patients with cardiovascular disease: A systematic review. Eur. J. Cardiovasc. Nurs. 2021, 20, 604–617. [Google Scholar] [CrossRef]
- Wood, D.; Crapnell, T.; Lau, L.; Bennett, A.; Lotstein, D.; Ferris, M.; Kuo, A. Emerging adulthood as a critical stage in the life course. In Handbook of Life Course Health Development; Springer: Berlin/Heidelberg, Germany, 2018; pp. 123–143. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Wethington, E.; Glanz, K.; Schwartz, M.D. Stress, coping, and health behavior. Health Behav. Theory Res. Pract. 2015, 223, 242. [Google Scholar] [CrossRef]
- Rand, K.; Vallis, M.; Aston, M.; Price, S.; Piccinini-Vallis, H.; Rehman, L.; Kirk, S.F. “It is not the diet; it is the mental part we need help with.” A multilevel analysis of psychological, emotional, and social well-being in obesity. Int. J. Qual. Stud. Health Well-Being 2017, 12, 1306421. [Google Scholar] [CrossRef]
- Berding, K.; Vlckova, K.; Marx, W.; Schellekens, H.; Stanton, C.; Clarke, G.; Jacka, F.; Dinan, T.G.; Cryan, J.F. Diet and the Microbiota-Gut-Brain Axis: Sowing the Seeds of Good Mental Health. Adv. Nutr. 2021, 12, 1239–1285. [Google Scholar] [CrossRef]
- Barber, T.M.; Valsamakis, G.; Mastorakos, G.; Hanson, P.; Kyrou, I.; Randeva, H.S.; Weickert, M.O. Dietary Influences on the Microbiota-Gut-Brain Axis. Int. J. Mol. Sci. 2021, 22, 3502. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, G.; Ferri, A.; Clarke, G.; Cryan, J.F. Diet and the microbiota–gut–brain-axis: A primer for clinical nutrition. Curr. Opin. Clin. Nutr. Metab. Care 2022, 25, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Carrillo, A.; Feig, E.H.; Harnedy, L.E.; Huffman, J.C.; Park, E.R.; Thorndike, A.N.; Kim, S.; Millstein, R.A. The role of positive psychological constructs in diet and eating behavior among people with metabolic syndrome: A qualitative study. Health Psychol. Open 2022, 9, 20551029211055264. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Ruhm, C.J.; Puac-Polanco, V.; Hwang, I.H.; Lee, S.; Petukhova, M.V.; Sampson, N.A.; Ziobrowski, H.N.; Zaslavsky, A.M.; Zubizarreta, J.R. Estimated prevalence of and factors associated with clinically significant anxiety and depression among US adults during the first year of the COVID-19 pandemic. JAMA Netw. Open 2022, 5, e2217223. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, R.D.; Dierker, L.C.; Wu, M.; Galea, S.; Hoven, C.W.; Weinberger, A.H. Trends in US depression prevalence from 2015 to 2020: The widening treatment gap. Am. J. Prev. Med. 2022, 63, 726–733. [Google Scholar] [CrossRef] [PubMed]
- SAMHSA. Key Substance Use and Mental Health Indicators in the United States: Results from the 2020 National Survey on Drug Use and Health; HHS Publication No. PEP21-07-01-003, NSDUH Series H-56; SAMHSA: Rockville, MD, USA, 2021. [Google Scholar]
- Yap, M.C.; Wu, F.; Huang, X.; Tang, L.; Su, K.; Tong, X.; Kwok, S.C.; Wu, C.; Wang, S.; He, Z. Association between individual resilience and depression or anxiety among general adult population during COVID-19: A systematic review. J. Public Health 2023, 45, fdad144. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Sznajder, K.; Cheng, D.; Wang, S.; Cui, C.; Yang, X. Coping styles for mediating the effect of resilience on depression among medical students in web-based classes during the COVID-19 pandemic: Cross-sectional questionnaire study. J. Med. Internet Res. 2021, 23, e25259. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Zhao, Y.Y.; Wang, J.; Sun, Y.H. Academic burnout and depression of Chinese medical students in the pre-clinical years: The buffering hypothesis of resilience and social support. Psychol. Health Med. 2020, 25, 1094–1105. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Y.; Dong, X.; Zhao, J. Effects of Envy on Depression: The Mediating Roles of Psychological Resilience and Social Support. Psychiatry Investig. 2020, 17, 547–555. [Google Scholar] [CrossRef]
- Höltge, J.; Theron, L.; Ungar, M. A multisystemic perspective on the temporal interplay between adolescent depression and resilience-supporting individual and social resources. J. Affect. Disord. 2022, 297, 225–232. [Google Scholar] [CrossRef]
- de Vera García, M.; Gambarte, M. Resilience as a protective factor of chronic stress in teachers. Eur. J. Investig. Health Psychol. Educ. 2019, 9, 159–175. [Google Scholar] [CrossRef]
- Lee, J.-K.; Choi, H.-G.; Kim, J.-Y.; Nam, J.; Kang, H.-T.; Koh, S.-B.; Oh, S.-S. Self-resilience as a protective factor against development of post-traumatic stress disorder symptoms in police officers. Ann. Occup. Environ. Med. 2016, 28, 58. [Google Scholar] [CrossRef]
- Lehrer, H.M.; Steinhardt, M.A.; Dubois, S.K.; Laudenslager, M.L. Perceived stress, psychological resilience, hair cortisol concentration, and metabolic syndrome severity: A moderated mediation model. Psychoneuroendocrinology 2020, 113, 104510. [Google Scholar] [CrossRef]
- Sharpley, C.F.; Christie, D.R.; Bitsika, V.; Andronicos, N.M.; Agnew, L.L.; McMillan, M.E. Does psychological resilience buffer against the link between the 5-HTTLPR polymorphism and depression following stress. Physiol. Behav. 2017, 180, 53–59. [Google Scholar] [CrossRef]
- Breslow, A.S.; Brewster, M.E.; Velez, B.L.; Wong, S.; Geiger, E.; Soderstrom, B. Resilience and collective action: Exploring buffers against minority stress for transgender individuals. Psychol. Sex. Orientat. Gend. Divers. 2015, 2, 253. [Google Scholar] [CrossRef]
- Perna, L.; Mielck, A.; Lacruz, M.E.; Emeny, R.T.; Holle, R.; Breitfelder, A.; Ladwig, K.H. Socioeconomic position, resilience, and health behaviour among elderly people. Int. J. Public Health 2012, 57, 341–349. [Google Scholar] [CrossRef]
- Lucero, J.E.; Emerson, A.D.; Bowser, T.; Koch, B. Mental health risk among members of the millennial population cohort: A concern for public health. Am. J. Health Promot. 2021, 35, 266–270. [Google Scholar] [CrossRef]
- Bankole, E.; Harris, N.; Rutherford, S.; Wiseman, N. A systematic review of the adolescent-directed marketing strategies of transnational fast food companies in low-and middle-income countries. Obes. Sci. Pract. 2023, 9, 670–680. [Google Scholar] [CrossRef]
- Truman, E.; Elliott, C. Identifying food marketing to teenagers: A scoping review. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 67. [Google Scholar] [CrossRef]
- Ares, G.; Antúnez, L.; Alcaire, F.; Natero, V.; Otterbring, T. Is this advertisement designed to appeal to you? Adolescents’ views about Instagram advertisements promoting ultra-processed products. Public Health Nutr. 2024, 27, e96. [Google Scholar] [CrossRef]
- Mialon, M. An overview of the commercial determinants of health. Glob. Health 2020, 16, 74. [Google Scholar] [CrossRef]
- Szakos, D.; Ózsvári, L.; Kasza, G. Perception of older adults about health-related functionality of foods compared with other age groups. Sustainability 2020, 12, 2748. [Google Scholar] [CrossRef]
- Ye, Y.-C.; Wu, C.-H.; Huang, T.-Y.; Yang, C.-T. The difference between the Connor–Davidson Resilience Scale and the Brief Resilience Scale when assessing resilience: Confirmatory factor analysis and predictive effects. Glob. Ment. Health 2022, 9, 339–346. [Google Scholar] [CrossRef]
- Windle, G.; Bennett, K.M.; Noyes, J. A methodological review of resilience measurement scales. Health Qual. Life Outcomes 2011, 9, 8. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Smith, B.W.; deCruz-Dixon, N.; Schodt, K.; Torres, F. Brief resilience scale (BRS). In Handbook of Assessment in Mindfulness Research; Springer: Berlin/Heidelberg, Germany, 2023; pp. 1–19. [Google Scholar]
- Onvani, S.; Haghighatdoost, F.; Surkan, P.; Larijani, B.; Azadbakht, L. Adherence to the Healthy Eating Index and Alternative Healthy Eating Index dietary patterns and mortality from all causes, cardiovascular disease and cancer: A meta-analysis of observational studies. J. Hum. Nutr. Diet. 2017, 30, 216–226. [Google Scholar] [CrossRef]
- Hu, E.A.; Steffen, L.M.; Coresh, J.; Appel, L.J.; Rebholz, C.M. Adherence to the Healthy Eating Index-2015 and Other Dietary Patterns May Reduce Risk of Cardiovascular Disease, Cardiovascular Mortality, and All-Cause Mortality. J. Nutr. 2020, 150, 312–321. [Google Scholar] [CrossRef]
- Bureau, U.C. 2020 Census Illuminates Racial and Ethnic Composition of the Country; US Government Printing Office: Washington, DC, USA, 2020. [Google Scholar]
- McElrath, K.; Martin, M. Bachelor’s Degree Attainment in the United States: 2005 to 2019; American Community Survey Briefs, ACSBR-009; US Census Bureau: Suitland, MD, USA, 2021. [Google Scholar]
- Handy, A.; Mangal, R.; Stead, T.S.; Coffee, R.L., Jr.; Ganti, L. Prevalence and Impact of Diagnosed and Undiagnosed Depression in the United States. Cureus 2022, 14, e28011. [Google Scholar] [CrossRef]
- Johnson, A.J.; McCloyn, K.; Sims, M. Discrimination, High-Effort Coping, and Cardiovascular Risk Profiles in the Jackson Heart Study: A Latent Profile Analysis. J. Racial Ethn. Health Disparities 2022, 9, 1464–1473. [Google Scholar] [CrossRef]
- Islam, S.J.; Kim, J.H.; Topel, M.; Liu, C.; Ko, Y.A.; Mujahid, M.S.; Sims, M.; Mubasher, M.; Ejaz, K.; Morgan-Billingslea, J. Cardiovascular risk and resilience among Black adults: Rationale and design of the MECA Study. J. Am. Heart Assoc. 2020, 9, e015247. [Google Scholar] [CrossRef]
- McKay, S.; Skues, J.L.; Williams, B.J. Does the Brief Resilience Scale actually measure resilience and succumbing? Comparing artefactual and substantive models. Adv. Ment. Health 2021, 19, 192–201. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma. Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef]
- Kalisch, R.; Baker, D.G.; Basten, U.; Boks, M.P.; Bonanno, G.A.; Brummelman, E.; Chmitorz, A.; Fernàndez, G.; Fiebach, C.J.; Galatzer-Levy, I. The resilience framework as a strategy to combat stress-related disorders. Nat. Hum. Behav. 2017, 1, 784–790. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).