Carbohydrate Ingestion before Exercise for Individuals with McArdle Disease: Survey Evidence of Implementation and Perception in Real-World Settings
Highlights
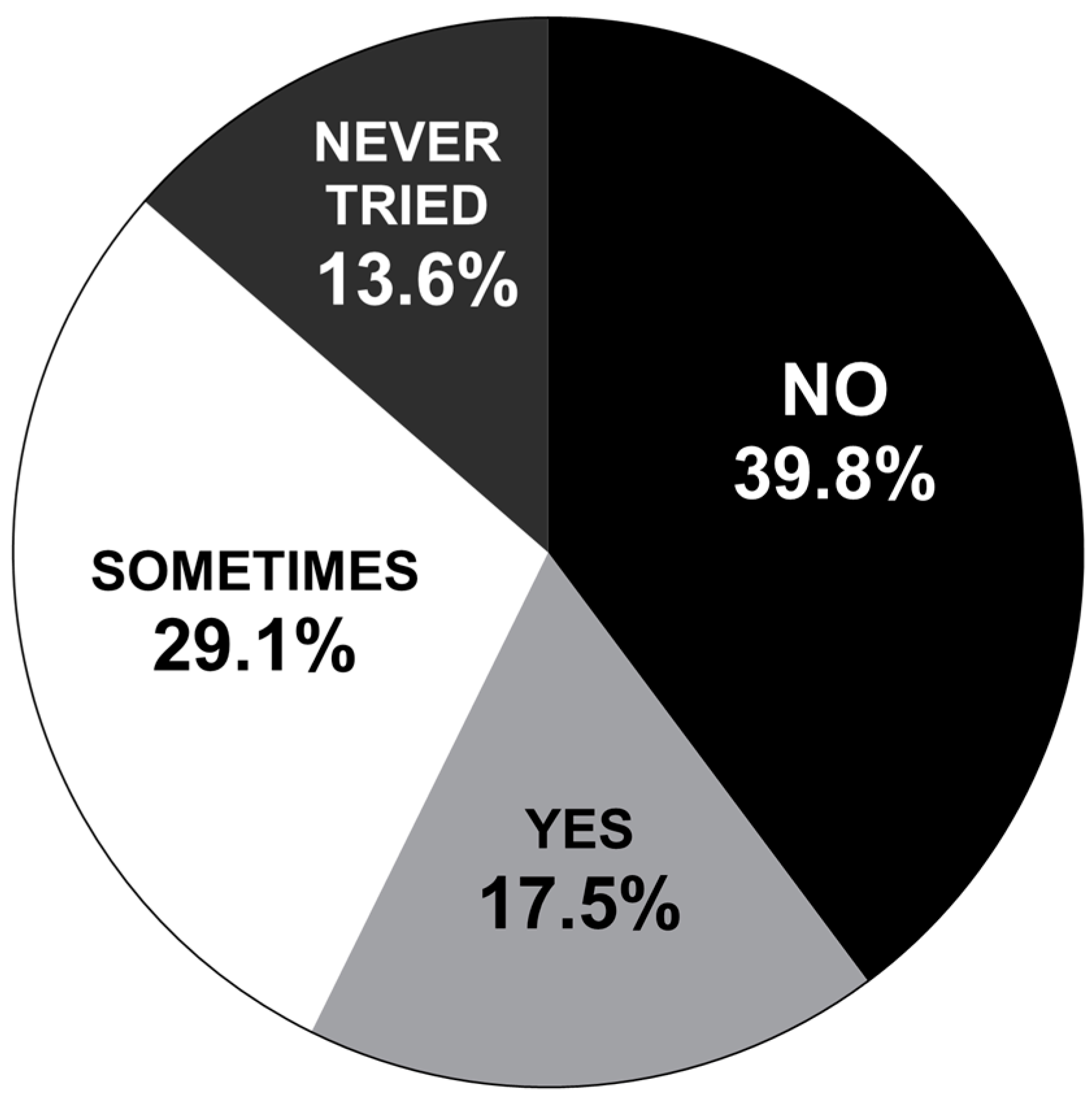
- Survey results suggest that positive outcomes (increase in exercise tolerance) achieved in prior lab-based settings regarding carbohydrate ingestion before exercise are not being effectively translated to real-world settings for the vast majority of surveyed individuals with McArdle disease.
- Potential factors for this poor translation include a poor understanding of the underlying principles for optimal application of the management method by those employing and advising it (maximizing blood glucose levels before exercise), limited detail and clarity of guidelines around the utilization of the management method, and the accuracy of prior research supporting the management methods utilization in real-world settings.
- There is a need for more educational platforms to better inform both individuals with McArdle disease and clinicians as to how to best treat and manage the condition of McArdle disease.
- There is a need for further research to determine the transferability of previous lab-based findings regarding the ingestion of carbohydrates before exercise for individuals with McArdle disease and its effectiveness in real-world settings.
Abstract
1. Introduction
2. Materials and Methods
Data Analysis
3. Results
4. Discussion
- (1)
- Type of carbohydrate consumed—The carbohydrate consumed when first attempting the technique should be sucrose. Sucrose is regular table sugar and can easily be diluted in water and consumed.
- (2)
- Amount of carbohydrate consumed—The minimum amount of carbohydrate consumed should be 37 g, as any amount less than this has not yet been investigated.
- (3)
- The consumption period—The ingestion of the carbohydrate needs to be consumed in one single bolus.
- (4)
- The waiting/priming period prior to exercise—The optimal waiting or ‘priming’ period between the ingestion of carbohydrates and the initiation of exercise is yet to be clearly established. Nevertheless, based on past research, it would be advised that a 25–30 min waiting period is used between ingestion and the initiation of exercise.
Additional Considerations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ATP | Adenosine triphosphate |
| BGL | Blood glucose level |
| IamGSD | International Association for Muscle Glycogen Storage Disease |
| IWMDs | Individuals with McArdle disease |
| MD | McArdle disease |
| RWSs | Real-world settings |
References
- Ørngreen, M.C.; Jeppesen, T.D.; Andersen, S.T.; Taivassalo, T.; Hauerslev, S.; Preisler, N.; Haller, R.G.; van Hall, G.; Vissing, J. Fat metabolism during exercise in patients with McArdle disease. Neurology 2009, 72, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Vissing, J.; Lewis, S.F.; Galbo, H.; Haller, R.G.; Gonzalez, J.T.; Fuchs, C.J.; Betts, J.A.; van Loon, L.J.C.; Krag, T.O.; Pinós, T.; et al. Effect of deficient muscular glycogenolysis on extramuscular fuel production in exercise. J. Appl. Physiol. 1992, 72, 1773–1779. [Google Scholar] [CrossRef]
- Romijn, J.A.; Coyle, E.F.; Sidossis, L.S.; Gastaldelli, A.; Horowitz, J.F.; Endert, E.; Wolfe, R.R. Regulation of endogenous fat and carbohydrate metabolism in relation to exercise intensity and duration. Am. J. Physiol. Endocrinol. Metab. 1993, 265, E380–E391. [Google Scholar] [CrossRef] [PubMed]
- Gastin, P.B. Energy System Interaction and Relative Contribution during Maximal Exercise. Sports Med. 2001, 31, 725–741. [Google Scholar] [CrossRef]
- Braakhekke, J.; De Bruin, M.; Stegeman, D.; Wevers, R.; Binkhorst, R.; Joosten, E. The second wind phenomenon in McArdle’s disease. Brain 1986, 109, 1087–1101. [Google Scholar] [CrossRef] [PubMed]
- Pearson, C.M.; Rimer, D.G.; Mommaerts, W.F. A metabolic myopathy due to absence of muscle phosphorylase. Am. J. Med. 1961, 30, 502–517. [Google Scholar] [CrossRef]
- Schmid, R.; Mahler, R. Chronic progressive myopathy with myoglobinuria: Demonstration of a glycogenolytic defect in the muscle. J. Clin. Investig. 1959, 38, 2044–2058. [Google Scholar] [CrossRef] [PubMed]
- Porte, D., Jr.; Crawford, D.W.; Jennings, D.B.; Aber, C.; McIlroy, M.B. Cardiovascular and metabolic responses to exercise in a patient with McArdle’s syndrome. N. Engl. J. Med. 1966, 275, 406–412. [Google Scholar] [CrossRef]
- Andersen, S.T.; Haller, R.G.; Vissing, J. Effect of Oral Sucrose Shortly Before Exercise on Work Capacity in McArdle Disease. Arch. Neurol. 2008, 65, 786–789. [Google Scholar] [CrossRef]
- Vissing, J.; Haller, R.G. The Effect of Oral Sucrose on Exercise Tolerance in Patients with McArdle’s Disease. N. Engl. J. Med. 2003, 349, 2503–2509. [Google Scholar] [CrossRef]
- Lucia, A.; Martinuzzi, A.; Nogales-Gadea, G.; Quinlivan, R.; Reason, S.; Bali, D.; Godfrey, R.; Haller, R.; Kishnani, P.; Laforêt, P.; et al. Clinical practice guidelines for glycogen storage disease V & VII (McArdle disease and Tarui disease) from an international study group. Neuromuscul. Disord. 2021, 31, 1296–1310. [Google Scholar] [CrossRef]
- Coakley, J.; Wagenmakers, A.; Edwards, R. Relationship between ammonia, heart rate, and exertion in McArdle’s disease. Am. J. Physiol. Endocrinol. Metab. 1992, 262, E167–E172. [Google Scholar] [CrossRef]
- Coakley, J.; Wagenmakers, A.; Edwards, R. Plasma ammonia is reduced by glucose and branched chain keto-acids during exercise in McArdle’s disease. Clin. Sci. 1989, 76, 49P. [Google Scholar] [CrossRef]
- Løkken, N.; Khawajazada, T.; Slipsager, A.; Voermans, N.C.; Vissing, J. Repeated oral sucrose dosing after the second wind is unnecessary in patients with McArdle disease: Results from a randomized, placebo-controlled, double-blind, cross-over study. J. Inherit. Metab. Dis. 2023, 46, 1139–1146. [Google Scholar] [CrossRef]
- Valenzuela, P.L.; Santalla, A.; Alejo, L.B.; Merlo, A.; Bustos, A.; Castellote-Bellés, L.; Ferrer-Costa, R.; Maffiuletti, N.A.; Barranco-Gil, D.; Pinós, T.; et al. Dose-response effect of pre-exercise carbohydrates under muscle glycogen unavailability: Insights from McArdle disease. J. Sport Health Sci. 2023, 13, 398–408. [Google Scholar] [CrossRef]
- Vissing, J.; Haller, R.G. A diagnostic cycle test for McArdle’s disease. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 2003, 54, 539–542. [Google Scholar] [CrossRef]
- Lewis, S.F.; Haller, R.G.; Cook, J.; Nunnally, R. Muscle fatigue in McArdle’s disease studied by 31P-NMR: Effect of glucose infusion. J. Appl. Physiol. 1985, 59, 1991–1994. [Google Scholar] [CrossRef]
- Haller, R.G.; Vissing, J. Spontaneous “Second Wind” and Glucose-Induced Second “Second Wind” in McArdle Disease: Oxidative Mechanisms. Arch. Neurol. 2002, 59, 1395–1402. [Google Scholar] [CrossRef]
- Haller, R.G.; Lewis, S.F.; Cook, J.; Blomqvist, C. Myophosphorylase deficiency impairs muscle oxidative metabolism. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 1985, 17, 196–199. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.T.; Jeppesen, T.D.; Taivassalo, T.; Sveen, M.-L.; Heinicke, K.; Haller, R.G.; Vissing, J. Effect of Changes in Fat Availability on Exercise Capacity in McArdle Disease. Arch. Neurol. 2009, 66, 762–766. [Google Scholar] [CrossRef] [PubMed]
- Leelayuwat, N.; Tsintzas, K.; Patel, K.; Macdonald, I.A. Metabolic Responses to Exercise after Carbohydrate Loads in Healthy Men and Women. Med. Sci. Sports Exerc. 2005, 37, 1721–1727. [Google Scholar] [CrossRef] [PubMed]
- Jeukendrup, A.E.; Rollo, I.; Carter, J.M. Carbohydrate mouth rinse: Performance effects and mechanisms. Sports Sci. Exch. 2013, 26, 1–8. [Google Scholar]
- Rollo, I.; Homewood, G.; Williams, C.; Carter, J.; Goosey-Tolfrey, V.L. The Influence of Carbohydrate Mouth Rinse on Self-Selected Intermittent Running Performance. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 550–558. [Google Scholar] [CrossRef]
- Carter, J.M.; Jeukendrup, A.E.; Jones, D.A. The Effect of Carbohydrate Mouth Rinse on 1-h Cycle Time Trial Performance. Med. Sci. Sports Exerc. 2004, 36, 2107–2111. [Google Scholar] [CrossRef]
- Walker, R.W.; Dumke, K.A.; Goran, M.I. Fructose content in popular beverages made with and without high-fructose corn syrup. Nutrition 2014, 30, 928–935. [Google Scholar] [CrossRef] [PubMed]
- Wosiacki, G.; Nogueira, A.; Frederico, F.; Vieira, R.G. Sugar composition of depectinized apple juices. Semin. Ciências Agrárias 2007, 28, 645–652. [Google Scholar] [CrossRef]
- Ferraris, R.P. Dietary and developmental regulation of intestinal sugar transport. Biochem. J. 2001, 360, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Semenza, G.; Kessler, M.; Hosang, M.; Weber, J.; Schmidt, U. Biochemistry of the Na+, d-glucose cotransporter of the small-intestinal brush-border membrane: The state of the art in 1984. Biochim. Biophys. Acta (BBA)—Rev. Biomembr. 1984, 779, 343–379. [Google Scholar] [CrossRef]
- Lecoultre, V.; Benoit, R.; Carrel, G.; Schutz, Y.; Millet, G.P.; Tappy, L.; Schneiter, P. Fructose and glucose co-ingestion during prolonged exercise increases lactate and glucose fluxes and oxidation compared with an equimolar intake of glucose. Am. J. Clin. Nutr. 2010, 92, 1071–1079. [Google Scholar] [CrossRef]
- Sun, S.Z.; Empie, M.W. Fructose metabolism in humans—What isotopic tracer studies tell us. Nutr. Metab. 2012, 9, 89. [Google Scholar] [CrossRef]
- Rowlands, D.S.; Thorburn, M.S.; Thorp, R.M.; Broadbent, S.; Shi, X. Effect of graded fructose coingestion with maltodextrin on exogenous 14C-fructose and 13C-glucose oxidation efficiency and high-intensity cycling performance. J. Appl. Physiol. 2008, 104, 1709–1719. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, G.M.; Moore, S.M.; Hamley, S.; Selathurai, A.; Bruce, C.R. The Effect of Ingested Glucose Dose on the Suppression of Endogenous Glucose Production in Humans. Diabetes 2017, 66, 2400–2406. [Google Scholar] [CrossRef]
- Awad, S.; Constantin-Teodosiu, D.; Constantin, D.; Rowlands, B.J.; Fearon, K.C.; Macdonald, I.A.; Lobo, D.N. Cellular mechanisms underlying the protective effects of preoperative feeding: A randomized study investigating muscle and liver glycogen content, mitochondrial function, gene and protein expression. Ann. Surg. 2010, 252, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Garber, A.J.; Menzel, P.H.; Boden, G.; Owen, O.E. Hepatic Ketogenesis and Gluconeogenesis in Humans. J. Clin. Investig. 1974, 54, 981–989. [Google Scholar] [CrossRef]
- Wolever, T.M.; Bolognesi, C. Prediction of glucose and insulin responses of normal subjects after consuming mixed meals varying in energy, protein, fat, carbohydrate and glycemic index. J. Nutr. 1996, 126, 2807–2812. [Google Scholar] [PubMed]


| n = 104 (Males 27, Females 77) | Mean ± SD | Range |
|---|---|---|
| Age (y) | 46 ± 15 | 18–82 |
| Weight (kg) | 86.7 ± 34.1 | 46–260 |
| BMI (kg·m2) | 30.4 ± 11.2 | 16.3–80.0 |
| Nationality | Number (n = 108) | |
| Argentina | 1 | |
| Australia | 15 | |
| Belgium | 1 | |
| Canada | 9 | |
| Colombia | 1 | |
| Czech Republic | 1 | |
| Germany | 3 | |
| Hong Kong | 2 | |
| Ireland | 2 | |
| Italy | 1 | |
| México | 1 | |
| The Netherlands | 3 | |
| New Zealand | 2 | |
| Portugal | 1 | |
| Spain | 4 | |
| Sweden | 1 | |
| United States of America | 44 | |
| United Kingdom | 16 | |
| Question 11 | |||||
|---|---|---|---|---|---|
| Question 10 | 15 min or Less | 15–30 min | 30–60 min | More than 60 min | Total |
| Once a week | 5 | 5 | 2 | 1 | 13 |
| 2–3 times a week | 4 | 14 | 12 | 4 | 34 |
| More than 3 times a week | 0 | 11 | 23 | 13 | 47 |
| Total | 9 | 30 | 37 | 18 | 94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torrens, S.L.; Parr, E.B.; McNulty, C.; Ross, L.; MacLaughlin, H.; Robergs, R.A. Carbohydrate Ingestion before Exercise for Individuals with McArdle Disease: Survey Evidence of Implementation and Perception in Real-World Settings. Nutrients 2024, 16, 1423. https://doi.org/10.3390/nu16101423
Torrens SL, Parr EB, McNulty C, Ross L, MacLaughlin H, Robergs RA. Carbohydrate Ingestion before Exercise for Individuals with McArdle Disease: Survey Evidence of Implementation and Perception in Real-World Settings. Nutrients. 2024; 16(10):1423. https://doi.org/10.3390/nu16101423
Chicago/Turabian StyleTorrens, Sam L., Evelyn B. Parr, Craig McNulty, Lynda Ross, Helen MacLaughlin, and Robert A. Robergs. 2024. "Carbohydrate Ingestion before Exercise for Individuals with McArdle Disease: Survey Evidence of Implementation and Perception in Real-World Settings" Nutrients 16, no. 10: 1423. https://doi.org/10.3390/nu16101423
APA StyleTorrens, S. L., Parr, E. B., McNulty, C., Ross, L., MacLaughlin, H., & Robergs, R. A. (2024). Carbohydrate Ingestion before Exercise for Individuals with McArdle Disease: Survey Evidence of Implementation and Perception in Real-World Settings. Nutrients, 16(10), 1423. https://doi.org/10.3390/nu16101423






