Abstract
Background: Anaemia continues to be a global public health burden affecting all age groups, particularly children. Indigenous people, including the Orang Asli (OA) population in Malaysia, are at risk of anaemia due to the vast disparities in social determinants of health in their population compared to the non-indigenous population. Objectives: This review aimed to identify the prevalence and risk factors of anaemia among OA children in Malaysia and analyse the knowledge gaps. Methods: A systematic search was conducted in PubMed, Cochrane Library, Scopus and Google Scholar databases. This review followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) guidelines. Results: This review identified six studies involving the participation of OA children from eight subtribes residing in Peninsular Malaysia. The overall prevalence of anaemia among OA children ranged from 21.6 to 80.0%, with iron deficiency anaemia prevalence at 34.0%. The risk factors of anaemia among OA children reported from one study in this review were being younger than ten years old children (AOR 2.11 (95% CI 1.23, 3.63)) and moderate to heavy Ascaris infections (AOR 2.05 (95% CI 1.12, 3.76)). There was no data from OA children from certain age groups and subtribes. Additionally, there is a paucity of data on risk factors for anaemia among OA children from the currently available evidence. Conclusion: The prevalence of anaemia among OA children poses a moderate to severe public health concern. Therefore, more comprehensive studies in the future are needed to address the gaps identified in this review, primarily regarding anaemia risk factors. This data would encourage policymakers in devising effective national prevention strategies to improve morbidity and mortality among OA children in the future.
1. Introduction
Anaemia continues to be a global burden of chronic diseases affecting about a quarter of the world population, with the most significant number of affected individuals in the Southeast Asian region (315 million) []. Anaemia is a condition in which the body’s levels of circulating red blood cells or haemoglobin fall below what is considered normal for a particular population group []. There are many aetiologies of anaemia, with iron deficiency being the most common cause in nearly all global regions, according to a systematic analysis of global anaemia []. Other causes include other micronutrient deficiencies (e.g., vitamin A, vitamin B12, folate, riboflavin), genetic haemoglobin disorders (e.g., thalassemia, sickle cell disease), infectious diseases (e.g., parasitic infections, malaria, HIV, tuberculosis) and chronic diseases []. Due to the disease’s various aetiologies and the non-specific nature of its symptoms, diagnosing anaemia can be difficult [].
Anaemia can happen at any stage of life, but it is more common in children and women who are of reproductive age. It is estimated that around 600 million preschool and school-aged children are anaemic across the globe []. In Malaysia, the latest data from National Health Morbidity Survey (NMHS) in 2019 shows that the overall prevalence of anaemia for the population aged 15 and above was 21.3% []. In another study conducted among preschool and school-aged children (6 months to 12 years old) in 2011, the prevalence of anaemia and iron deficiency anaemia (IDA) was reported at 6.6% and 4.4%, respectively []. Numerous studies have shown that untreated anaemia in children can have a variety of long-term negative impacts on them, including the impact on their physical development, cognitive development, psychomotor development, auditory function, visual function and immunity [,,].
Indigenous populations around the world are affected by anaemia, yet they are frequently unrecognised and undocumented. The term “indigenous people” in Malaysia refers to ethnic minorities made up of a variety of ethnolinguistic groups residing in Peninsular Malaysia as well as the east Malaysian states of Sarawak and Sabah []. The indigenous people that live in Peninsular Malaysia are known as Orang Asli (OA), while the rest are known as the natives of Sarawak or Sabah []. According to the Department of Orang Asli Development (JAKOA), there was a total number of 206,777 OA people living in nine states of Peninsular Malaysia as of 31st of December 2020 []. The OA people include 18 ethnic subgroups classified into three main tribes, namely Negrito (Bateq, Kensiu, Kintak, Lanoh, Jahai and Medriq), Senoi (Temiar, Che Wong, Mahmeri, Jahut, Semoq Beri and Semai) and Proto-Malay (Temuan, Kuala, Kanaq, Seletar, Jakun and Semelai) [].
Recent data nationwide showed that the prevalence of anaemia among the indigenous population is higher than the general population, affecting primarily children in most parts of the world []. There has been an increasing number of studies reporting on anaemia among the indigenous population over the past two decades [,,]. Earlier studies published over a decade ago reported that the prevalence of anaemia among OA children in Malaysia was at a severe level ranging from 41.5% to 48.5% [,,]. Thus far, the available data on anaemia among OA children in Malaysia are still limited and are obtained from small-scale studies involving only certain OA tribes.
Therefore, this study aimed to summarise the existing data on anaemia among OA children to identify the prevalence and risk factors of anaemia among OA children and to analyse the research gaps in this research area. Results from this study can be utilised to inform policymakers regarding the magnitude of anaemia among OA children to devise effective strategies to improve morbidity and mortality in this population. In addition, future research could aim for more valuable and useful data by focusing on research that could fill the gaps in this area.
2. Materials and Methods
This review of anaemia among OA children in Malaysia was conducted following the framework outlined by Arksey and O’Malley [] and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) checklist [] (Available from Supplementary Table S1). This review is registered with National Medical Research Register (NMRR) Malaysia (NMRR-20-1553-55891). The authors prepared a review protocol before the study commencement; however, it was not published anywhere.
2.1. Search Strategies
A systematic search was performed using different databases and other registries (Google, Google Scholar, reference lists of relevant articles) to identify eligible studies published during the last ten years up to the 30th of April 2022. Electronic databases searched were PubMed, Scopus, Cochrane Library and Google Scholar. The search terms used in this study based on the following keywords: (1) population (Orang Asli children, Negrito children, Senoi children and Melayu Proto children), (2) outcome (anaemia MeSH term and iron-deficiency anaemia) and (3) location (Malaysia). A detailed search strategy performed by the authors in this review is available in (Available from Supplementary Figure S1).
2.2. Eligibility Criteria
This review included published studies on the prevalence of anaemia among OA children in Malaysia. The inclusion criteria were (1) primary studies reported on the prevalence and/or risk factors of anaemia among OA children, (2) studies that include OA children with other population(s) (i.e., children of different ethnicity or adults), taking into consideration that the data for OA children were reported separately from others, (3) conducted in Malaysia, (4) published between the years 2012 and 2022 and (5) published in the Malay or English language. There was no restriction in terms of sample size. The term child was defined according to Conventions on the Rights of the Child (CRC) [], which refers to individuals below 18 years of age, while the term anaemia was defined according to the criteria outlined by the World Health Organization (WHO) []. The primary outcome of this study was the anaemia status among OA children according to WHO criteria.
2.3. Selection Process
Duplicate studies obtained from the four databases were removed. The authors (M.K.N.K., M.A.A.R., F.A.T., N.S. (Norhafizah Sahril), N.A.S., M.S.R., M.A.A.A., S.H.L., N.A.W. and N.S. (Norliza Shamsuddin)), working in pairs, performed title and/or abstract screening independently for potentially eligible studies and removed irrelevant studies. Then, M.K.N.K. and M.A.R. independently reviewed the full texts of the shortlisted studies for inclusion and showed reasons for excluding any study. Any disagreement between the two authors was resolved via consultation with another author (F.A.T.) when necessary.
2.4. Data Extraction, Synthesis and Charting
M.K.N.K. and M.A.A.R. independently extracted the data from the included studies using a standardised electronic data extraction form. The form was developed in a Microsoft Excel spreadsheet to extract relevant information from each study. The relevant information extracted were the characteristics of the study (titles, author of the studies/year of publication and study designs), population characteristics (OA tribe, age range, sample size and sampling frame) and the outcome (prevalence and risk factors of anaemia among OA children). All data extracted was checked by F.A.T. for accuracy. Then, the data were descriptively reported according to study characteristics, the prevalence of anaemia, risk factors for anaemia and research gaps identified.
3. Results
3.1. Study Results
This study search yielded 735 articles from the electronic databases (Pubmed = 21, Cochrane Library = 104, Scopus = 175 and Google Scholar = 435). No additional articles were identified from other sources. After removing 96 duplicate articles, another 619 articles were removed from title and abstract screening. Then, the full texts of twenty shortlisted articles were reviewed for inclusion, and fourteen articles were excluded with reasons. Subsequently, six articles that met the eligibility criteria were included in this review. Figure 1 summarises the study identification process.
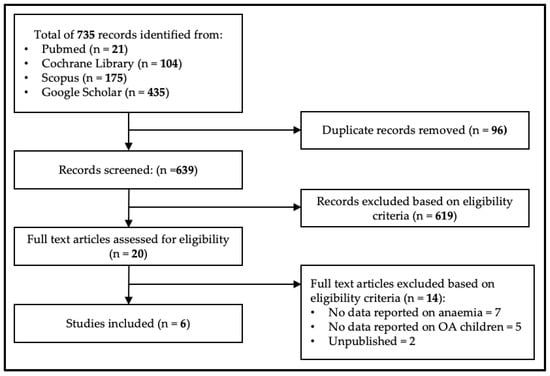
Figure 1.
Prisma flow diagram.
3.2. Characteristics of Included Studies
Among the six studies included in this review, only one was a randomised controlled trial study [], while the rest were cross-sectional surveys. Orang Asli children involved in these studies were from six states in Peninsular Malaysia: Kedah [], Perak [], Pahang [,,], Negeri Sembilan [,], Kelantan [] and Terengganu [] (Figure 2). As for the OA subtribes of the children in this study, there were two subtribes from the Proto-Malay tribe (Semelai and Temuan) and all the subtribes of the Negrito tribe (Figure 3). Furthermore, the number of participants in each study ranged from 77 to 343 children, and most of the studies, except for one [], exclusively focused on the OA children population. Among all the included studies, three studies [,,] measured anaemia as the primary outcome. The age group of OA children reported for anaemia prevalence in these studies ranged from two to thirteen years old. Apart from measuring anaemia among OA children, some studies also analysed other conditions associated with anaemia. Four studies reported soil-transmitted helminth infection [,,,], while one reported iron deficiency []. Characteristics of the included studies are summarised in Table 1.
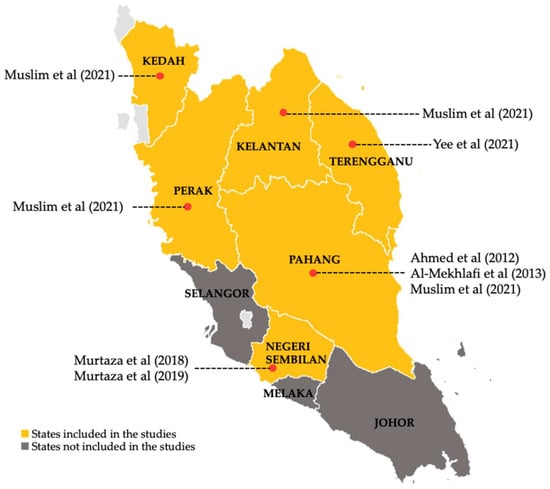
Figure 2.
Locality of Orang Asli children population participated in the studies [,,,,,].
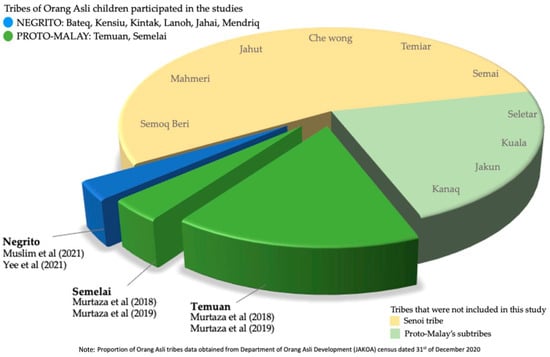
Figure 3.
Tribes of Orang Asli children participated in the studies [,,,].

Table 1.
Overall characteristics of included studies on anaemia among OA children in Malaysia, 2012–2022.
3.3. Prevalence of Anaemia among Orang Asli Children in Malaysia
The overall prevalence of anaemia among OA children in Malaysia ranged from 21.6 to 80.0%. Detailing prevalence by different age groups, two studies (N = 533) reported that the prevalence of anaemia among those 2–6 years of age was close to 22.0%, but one study (Muslim et al., N = 32) reported a significantly higher prevalence of 80.0%. Similarly, for children in the 6–13 years age group, two studies (N = 504) reported the prevalence of anaemia ranging from 41.0 to 48.5% while one study (Muslim et al., N = 76) reported a higher prevalence of 70.4%. The highest prevalence of anaemia among OA children was observed among the Negrito tribe, while the lowest was among the Proto-Malay tribe (Semelai and Temuan) (Table 1). The prevalence of IDA among OA children was 34.0%, as reported by one study [] in this review. A more recent study in this review reported that the prevalence of anaemia was higher among female OA children [], contrary to the previous study []. The prevalence of mild anaemia was 12.9%, while moderate and severe anaemia among OA children ranged from 3.0 to 8.7% [,]. One study reported on locality-specific anaemia prevalence [], which revealed a higher prevalence of anaemia of 82.4% among OA children aged 2–6 years living within inland forest territories (IJV) compared to 78.3% among those living in resettlement near town peripheries (RPS). On the contrary, a higher prevalence of anaemia of 75.0% was observed among OA children aged 7–12 years living in resettlement near town peripheries compared to 57.1% among those living within inland forest territories []. Anaemia-specific prevalence of OA children is summarised in Table 2.

Table 2.
Anaemia-specific prevalence among OA children in Malaysia.
3.4. Risk Factors of Anaemia among Orang Asli Children in Malaysia
Two studies analysed the risk factors of anaemia among OA people; however, only one was included in this review analysis []. The study found that haemoglobin was significantly lower in OA children aged less than ten years old and in those with moderate to heavy Ascaris infections with an adjusted odds ratio of 2.11 (95% CI 1.23, 3.63) and 2.05 (95% CI 1.12, 3.76), respectively (Table 1). The other study did not perform separate analyses for the OA children; hence the results were deemed irrelevant for this review purpose [].
3.5. Research Gaps Identified
There was an absence of data from certain OA children from different demographics. First, OA children residing in Selangor, Melaka and Johor states were not included in this review (Figure 2). Next, OA children from ten subtribes were not reported in this review, involving all Senoi subtribes (Temiar, Che Wong, Mahmeri, Jahut, Semai and Semoq Beri) and four Proto-Malay subtribes (Kuala, Kanaq, Seletar, and Jakun) (Figure 3). Additionally, the OA children aged less than two years old and more than thirteen years old were not reported in this review. Otherwise, this review also found varying data reporting formats on anaemia between the studies, particularly the severity and gender-specific prevalence. Finally and above all, this review revealed the paucity of data on risk factors for anaemia among OA children in Malaysia at present.
4. Discussion
The emphasis on the review subject highlights the overall determinant of health inequities among indigenous people, which contribute to the burden of anaemia in the population. It is critical to note that this review contributes to sustainable development goals (SDGs) adopted by the Malaysian government from the United Nations (UN). Striving to reduce morbidity and mortality of anaemia among OA children contributes directly to SDGs (goal 3), specifically the neonatal mortality and under-five mortality rate []. Additionally, obtaining universal health coverage is the primary goal in the SDGs to address health disparities among marginalised groups, such as indigenous people, as it provides a link between equitable social and economic growth []. In this review, we aimed to summarise the existing data on anaemia among OA children to identify the prevalence and risk factors of anaemia and the gaps in anaemia research among OA children in Malaysia between 2012 and 2022. We identified six studies based on eligibility criteria, and the results uncovered significant findings from the currently available research evidence. First, we discovered little research focus among the children, resulting in limited inclusivity of children from all age groups and subtribes. Considering the large proportion of OA children accounting for up to 35% (77,000 children) of the total OA population [], the participation of OA children in the included studies is still lacking. This is also supported by the absence of data on anaemia among Senoi tribe children, which is the largest tribe comprise of 55.1% of overall OA population []. Furthermore, we also found varying data reporting formats on anaemia between the studies, likely due to the different predetermined primary outcomes. As a result, some essential data on anaemia, like the severity prevalence, were missed in the publications. It is important to note that severe anaemia carries the highest morbidity and mortality among children [].
Next, the results from our review accentuated the magnitude of anaemia among OA children based on the available evidence. The WHO classified the public health significance of anaemia based on population prevalence as normal (≤4.9%), mild (5–19.9%), moderate (20–39.9%) and severe (≥40%). According to this, current data on the prevalence of anaemia among OA children would be classified as a moderate to severe problem. Our results revealed that the prevalence of anaemia among OA children in both age groups of 2–6 years and 6–13 years was significantly higher than the major children population in Malaysia. According to the data from a nationwide cross-sectional study conducted among children in Malaysia, Poh et al. reported the prevalence of anaemia was higher among younger children aged 4–6 (11.3 to 17.6%) years old compared to older children aged 7–12 years old (3.6 to 5.1%) []. A similar trend was observed in our data obtained from the Muslim et al. study, which included OA children of different age groups. This trend is also consistent with global estimates of anaemia by the WHO which show higher prevalence of anaemia among preschool-aged children at 47.4% compared to school-aged children at 25.4% []. In comparison, the current prevalence of anaemia among OA children in Malaysia is also higher when compared to indigenous children in other Southeast Asian countries. For instance, two studies in Chiang Mai Province in Thailand reported that the prevalence of anaemia among Karen hill-tribe children was 19.8% in the 1–6 years age group [] and 8.5% in the 8–11 years age group []. Meanwhile, the National Nutrition Survey in the Philippines reported the prevalence of anaemia among indigenous people children was 16.6% in the age group from 6 months to 5 years of age and 12.3% in the 6–12 years age group []. On another note, the significantly high prevalence of anaemia reported in our study by Muslim et al. conducted among the Negrito tribe, compared to the rest of included studies, is particularly interesting. Despite the arguably low number of respondents included in that study, it is important to note that Negrito tribe only comprise of 2.94% of overall OA population []. Thus, this data may suggest the existence of different level of socio-economic background and anaemia risk factors among the OA tribes. Studies on nutritional status among OA children of different tribes also showed majority of the indicators of malnutrition were more prevalent among the Negrito tribe [,,]. Otherwise, another important factor to consider is that OA people who are living in the remote areas can either be living in a town periphery or deep in the jungle. According to JAKOA, about 61% of OA people have been relocated to town peripheries under the resettlement plans while another 38% of OA people are still living deep in the jungle with a small portion of them still being semi-nomadic, especially the Negrito tribe [,]. Those who have been relocated to town peripheries are expected to have better living conditions as they were provided with better necessities such as housing, school, electricity and a water supply by the government.
Our results also revealed the dearth of data on risk factors for anaemia among OA children in Malaysia. While aetiologies of anaemia are multifaceted, the significant causes of anaemia among the indigenous population are nutritional deficiency, particularly iron deficiency, malaria and helminth infection []. To date, there are several studies conducted on anaemia among indigenous children in other countries [,,,,], while regrettably, our review only found a couple of anaemia risk factors reported by one study. Examples of anaemia risk factors identified among indigenous children to date were children’s age, gender, prolonged breastfeeding, maternal age, maternal education, household income, household condition, infection and more. On the other hand, previous local data published more than a decade ago identified some risk factors for anaemia among OA children, including gender, being underweight, stunting, severe trichuriasis, low level of mother’s education and having a working mother [,]. Therefore, it is clear that there is a huge gap in the current data on anaemia risk factors among OA children in Malaysia, and it should be addressed in future studies.
Indigenous children, including the OA children in Malaysia, are at risk for anaemia due to the vast disparities in social determinants of health, such as poverty, food insecurity, living environment and access to health services, compared to the general population []. A recent study revealed that the nutritional status of the OA is typically low among women and children population []. In response to this conundrum, the Ministry of Health Malaysia has made multiple efforts, including several nutritional programmes for the OA population, for instance, the Community Feeding Programme and the monthly food baskets under Rehabilitation Program for Malnourished Children []. In addition, nutritional status and parasitic infections among the OA population in Malaysia have gained more research focus, evident by increasing numbers of published articles over the last decade [,,,,,,,]. However, most of the available studies focused on nutritional status, dietary assessment and soil-transmitted helminth infection, while only a few reported on anaemia among OA people, especially children. This may be due to the hefty cost of including bio-specimen analysis in the study, limited access in some remote areas or difficulty obtaining voluntary participation from OA people, especially when an invasive investigation towards their children is involved.
4.1. Strength and Limitation
To the best of our knowledge, this review is the first to summarise available data on anaemia among OA children in Malaysia. We performed thorough search, carefully chose the studies and systematically extracted the data to obtain information on the prevalence, severity and risk factors of anaemia among OA children. However, we acknowledge several limitations in this review. First, the small number of included studies limits the data obtained in this review, primarily the risk factors of anaemia among OA children. Moreover, we did not perform bias and quality assessments of the included studies. Additionally, we excluded unpublished papers and restricted our review to only the Malay and English languages.
4.2. Recommendations for Future Research
The results from our review urge more recognition of anaemia among OA children as an essential public health concern in Malaysia. Our review results also urge for a more comprehensive epidemiological study in the future to reduce morbidity and mortality among OA children effectively. Therefore, future studies are advised to focus more on aetiologies of anaemia and associated risk factors among OA children to assist policymakers in devising effective programmes specific to OA children. Data on anaemia among OA children is extremely valuable due to the limited availability; thus, future studies are encouraged to perform in-depth analysis and reporting of data on anaemia obtained from OA children.
5. Conclusions
In Malaysia, the prevalence of anaemia among OA children constitutes a moderate to serious public health issue. Despite multiple efforts taken by the Ministry of Health Malaysia, anaemia continues to be a burden among the OA population, primarily the children. A huge research gap identified in this review predominantly concerning the associated risk factors urges for more comprehensive future research to obtain more accurate data representing the OA children population in Malaysia. This data will assist policymakers in devising more effective national prevention strategies to improve morbidity and mortality among OA children in the future.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15061493/s1, Table S1: PRISMA-ScR checklist. Figure S1: The Detailed Search Strategy. Reference [] was cited in the supplementary materials.
Author Contributions
M.K.N.K. conceptualised this study, searched the literature, screened and selected studies, extracted data and wrote the manuscript. M.A.A.R., F.A.T., N.S. (Norhafizah Sahril), N.A.S., M.S.R., M.A.A.A., S.H.L., N.A.W. and N.S. (Norliza Shamsuddin) screened the records. M.A.A.R. and F.A.T. also participated in studies selection, reviewing and editing of the manuscript. M.S.A.K. reviewed the manuscript and supervised the review. All authors have read and agreed to the published version of the manuscript.
Funding
This study received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We would like to thank the Director-General of Health Malaysia for permitting this article to be published.
Conflicts of Interest
The authors declare no conflict of interest.
References
- De Benoist, E.M.B.; Egli, I.; Cogswell, M.; World Health Organization. (2008). Worldwide Prevalence of Anaemia 1993–2005: WHO Global Database on Anaemia. 2005. Available online: https://apps.who.int/iris/handle/10665/43894 (accessed on 21 September 2022).
- WHO. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity; Technical Documents; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Kassebaum, N.J.; Jasrasaria, R.; Naghavi, M.; Wulf, S.K.; Johns, N.; Lozano, R.; Regan, M.; Weatherall, D.; Chou, D.P.; Eisele, T.P.; et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood 2014, 123, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Chaparro, C.M.; Suchdev, P.S. Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Ann. N. Y. Acad. Sci. 2019, 1450, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Cappellini, M.D.; Musallam, K.M.; Taher, A.T. Iron deficiency anaemia revisited. J. Intern. Med. 2020, 287, 153–170. [Google Scholar] [CrossRef]
- WHO. Intermittent Iron Supplementation in Preschool and School-Age Children; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Institute for Public Health NIH, Ministry of Health Malaysia. National Health and Morbidity Survey 2019: Non-communicable Diseases, Healthcare Demand and Health Literacy. 2019; Volume 1. Available online: https://iku.gov.my/nhms-2019 (accessed on 21 September 2022).
- Poh, B.K.; Ng, B.K.; Haslinda, M.D.S.; Shanita, S.N.; Wong, J.E.; Budin, S.B.; Ruzita, A.T.; Ng, L.O.; Khouw, I.; Norimah, A.K. Nutritional status and dietary intakes of children aged 6 months to 12 years: Findings of the Nutrition Survey of Malaysian Children (SEANUTS Malaysia). Br. J. Nutr. 2013, 110 (Suppl. S3), S21–S35. [Google Scholar] [CrossRef]
- Algarin, C.; Peirano, P.; Garrido, M.; Pizarro, F.; Lozoff, B. Iron deficiency anemia in infancy: Long-lasting effects on auditory and visual system functioning. Pediatr. Res. 2003, 53, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Fretham, S.J.; Carlson, E.S.; Georgieff, M.K. The role of iron in learning and memory. Adv. Nutr. 2011, 2, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Pivina, L.; Semenova, Y.; Dosa, M.D.; Dauletyarova, M.; Bjorklund, G. Iron Deficiency, Cognitive Functions, and Neurobehavioral Disorders in Children. J. Mol. Neurosci. 2019, 68, 1–10. [Google Scholar] [CrossRef]
- Khor, G.L.; Shariff, Z.M. Do not neglect the indigenous peoples when reporting health and nutrition issues of the socio-economically disadvantaged populations in Malaysia. BMC Public Health 2019, 19, 1685. [Google Scholar] [CrossRef]
- Jadual Taburan Etnik Orang Asli Mengikut Negeri: JAKOA; 2020 [Updated 22.12.2021]. Available online: https://www.jakoa.gov.my/orang-asli/jadual-taburan-etnik-orang-asli-mengikut-negeri/ (accessed on 22 September 2022).
- Masron, T.; Masami, F.; Ismail, N. Orang Asli in Peninsular Malaysia: Population, spatial distribution and socio-economic condition. J. Ritsumeikan. Soc. Sci. Hum. 2013, 6, 75–115. [Google Scholar]
- Khambalia, A.Z.; Aimone, A.M.; Zlotkin, S.H. Burden of anemia among indigenous populations. Nutr. Rev. 2011, 69, 693–719. [Google Scholar] [CrossRef]
- Udovicich, C.; Perera, K.; Leahy, C. Anaemia in school-aged children in an Australian Indigenous community. Aust. J. Rural Health 2017, 25, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Leite, M.S.; Cardoso, A.M.; Coimbra, C.E.A.; Welch, J.R.; Gugelmin, S.A.; Lira, P.C.I.; Horta, B.; Santos, R.V.; Escobar, A.L. Prevalence of anemia and associated factors among indigenous children in Brazil: Results from the First National Survey of Indigenous People’s Health and Nutrition. Nutr. J. 2013, 12, 69. [Google Scholar] [CrossRef] [PubMed]
- Tahir, E.; Ayotte, P.; Little, M.; Bélanger, R.E.; Lucas, M.; Mergler, D.; Sidi, E.A.L.; McHugh, N.G.-L.; Lemire, M. Anemia, iron status, and associated protective and risk factors among children and adolescents aged 3 to 19 years old from four First Nations communities in Quebec. Can. J. Public Health 2020, 111, 682–693. [Google Scholar] [CrossRef] [PubMed]
- Aini, U.N.; Al-Mekhlafi, M.S.H.; Azlin, M.; Shaik, A.; Sa’Iah, A.; Fatmah, M.S.; Ismail, M.G.; Firdaus, M.S.A.; Aisah, M.Y.; Rozlida, A.R.; et al. Serum iron status in Orang Asli children living in endemic areas of soil-transmitted helminths. Asia Pac. J. Clin. Nutr. 2007, 16, 724–730. [Google Scholar]
- Al-Mekhlafi, M.H.; Surin, J.; Atiya, A.S.; Ariffin, W.A.; Mahdy, A.K.M.; Abdullah, H.C. Anaemia and iron deficiency anaemia among aboriginal schoolchildren in rural Peninsular Malaysia: An update on a continuing problem. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 1046–1052. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Convention on the Rights of the Child, 20 November 1989. Annu. Rev. Popul. Law 1989, 16, 485–501.
- Al-Mekhlafi, H.M.; Al-Zabedi, E.M.; Al-Maktari, M.T.; Atroosh, W.M.; Al-Delaimy, A.K.; Moktar, N.; Sallam, A.A.; Abdullah, W.A.; Jani, R.; Surin, J. Effects of Vitamin A Supplementation on Iron Status Indices and Iron Deficiency Anaemia: A Randomized Controlled Trial. Nutrients 2014, 6, 190–206. [Google Scholar] [CrossRef]
- Muslim, A.; Lim, Y.A.-L.; Sofian, S.M.; Shaari, S.A.; Zain, Z.M. Nutritional status, hemoglobin level and their associations with soil-transmitted helminth infections between Negritos (indigenous) from the inland jungle village and resettlement at town peripheries. PLoS ONE 2021, 16, e0245377. [Google Scholar] [CrossRef]
- Ahmed, A.; Al-Mekhlafi, H.M.; Al-Adhroey, A.H.; Ithoi, I.; Abdulsalam, A.M.; Surin, J. Abdulsalam and Johari Surin. The nutritional impacts of soil-transmitted helminths infections among Orang Asli schoolchildren in rural Malaysia. Parasites Vectors 2012, 5, 119. [Google Scholar] [CrossRef]
- Murtaza, S.F.; Gan, W.Y.; Sulaiman, N.; Shariff, Z.M. Factors associated with stunting among Orang Asli preschool children in Negeri Sembilan, Malaysia. Malays. J. Nutr. 2018, 24, 215–226. [Google Scholar]
- Murtaza, S.F.; Gan, W.Y.; Sulaiman, N.; Shariff, Z.M.; Ismail, S.I.F. Sociodemographic, nutritional, and environmental factors are associated with cognitive performance among Orang Asli children in Malaysia. PLoS ONE 2019, 14, e0219841. [Google Scholar] [CrossRef] [PubMed]
- Yee, S.K.A.A.; Zakaria, N.S.; Mohd Yusof, H. Nutritional Status of Orang Asli Children in Sungai Berua, Terengganu. J. Sustain. Sci. Manag. 2021, 16, 180–190. [Google Scholar]
- Sustainable Development Goal 3: Good Health and Well-Being: United Nations Malaysia, Singapore and Brunei Darussalam. Available online: https://malaysia.un.org/en/sdgs/3 (accessed on 23 September 2022).
- Wong, Y.S.; Allotey, P.; Reidpath, D.D. Sustainable development goals, universal health coverage and equity in health systems: The Orang Asli commons approach. Glob. Health Epidemiol. Genom. 2016, 1, e12. [Google Scholar] [CrossRef]
- Zaidi, H.A. PICKids: KPLB aktifkan semula pasukan khas di perkampungan Orang Asli. Harian. Metro. Available online: https://www.hmetro.com.my/mutakhir/2022/04/831388/pickids-kplb-aktifkan-semula-pasukan-khas-di-perkampungan-orang-asli (accessed on 23 September 2022).
- Phiri, K.S.; Calis, J.C.J.; Faragher, B.; Nkhoma, E.; Ng’Oma, K.; Mangochi, B.; Molyneux, M.E.; Van Hensbroek, M.B. Long Term Outcome of Severe Anaemia in Malawian Children. PLoS ONE 2008, 3, e2903. [Google Scholar] [CrossRef]
- Tienboon, P. Micronutrient status of Karen children aged 1–6 years in Northern Thailand. Thai J. Clin. Nutr. 2009, 3, 86–89. [Google Scholar]
- Yanola, J.; Kongpan, C.; Pornprasert, S. Prevalence of Anemia, Iron Deficiency, Thalassemia and Glucose-6-Phosphate Dehydrogenase Deficiency Among Hill-Tribe School Children in Omkoi District, Chiang Mai Province, Thailand. Southeast Asian J. Trop. Med. Public Health 2014, 45, 920–925. [Google Scholar]
- Duante, C.; Austria, R.E.; Ducay, A.J.; Acuin, C.C.; Capanzana, M. Nutrition and Health Status of Indigenous Peoples (IPs) in the Philippines: Results of the 2013 National Nutrition Survey and 2015 Updating Survey. Philipp. J. Sci. 2022, 151, 513–531. [Google Scholar] [CrossRef]
- TAD, A.C.; Subapriya, S.; Hnin, P.A. Nutritional status and dietary intake of semai indigenous children below five years in perak, peninsular malaysia. Malays. J. Public Health Med. 2019, 19, 84–100. [Google Scholar]
- Pah, T.; Krishnasamy, D.; Golam Hassan, A.A. Distribution and Demography of the Orang Asli in Malaysia. 2017. Available online: https://www.ijhssi.org/papers/v6(1)/Version-2/F601024045.pdf (accessed on 24 September 2022).
- Willows, N.D.; Morel, J.; Gray-Donald, K. Prevalence of anemia among James Bay Cree infants of northern Quebec. Can. Med. Assoc. J. 2000, 162, 323–326. [Google Scholar]
- Arlappa, N.; Balakrishna, N.; Laxmaiah, A.; Brahmam, G.N. Prevalence of anaemia among rural preschool children of West Bengal, India. Ann. Hum. Biol. 2010, 37, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Leonard, D.; Buttner, P.; Thompson, F.; Makrides, M.; McDermott, R. Anaemia in early childhood among Aboriginal and Torres Strait Islander children of Far North Queensland: A retrospective cohort study. Aust. New Zealand J. Public Health 2019, 43, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Tay, J.E.F.; Ulaganathan, V.; Kua, G.Y.L.; Adan, M.A.; Lim, S.Y. Nutritional Status of Orang Asli in Malaysia. Malays. J. Med. Sci. 2022, 29, 17–29. [Google Scholar] [CrossRef]
- Chew, C.-C.; Lim, X.-J.; Low, L.-L.; Lau, K.-M.; Kari, M.; Shamsudin, U.K.; Rajan, P. The challenges in managing the growth of indigenous children in Perak State, Malaysia: A qualitative study. PLoS ONE 2022, 17, e0265917. [Google Scholar] [CrossRef] [PubMed]
- Azuwani, A.R.N.K.K.; Cheong, Y.Z.; Kok, C.C.; Aw, N.S.L.; Nadiah Mhd, S.; Abdul Rashid, K. Body Fat Percentage Distribution of an Orang Asli Group (Aborigines) in Cameron Highlands, Malaysia. Mal. J. Nutr. 2013, 19, 205–214. [Google Scholar]
- Rohin, M.A.K.; Rahim, A.F.W.J.; Zahary, M.N.; Aziz, A.A.; Him, N.A.S.N.; Yahaya, R.; Ridzwan, N.; Jumli, M.N.; Harun, S. Nutritional Status of the Temiar Orang Asli Community in Kuala Betis, Gua Musang, Kelantan. Pak. J. Nutr. 2018, 17, 311–318. [Google Scholar] [CrossRef]
- Wong, C.Y.; Zalilah, M.S.; Chua, E.Y.; Norhasmah, S.; Chin, Y.S.; Siti Nur’Asyura, A. Double-burden of malnutrition among the indigenous peoples (Orang Asli) of Peninsular Malaysia. BMC Public Health 2015, 15, 680. [Google Scholar] [CrossRef]
- Nurfahilin, T.N.S. Factors and Coping Strategies Related to Food Insecurity and Nutritional Status Among Orang Asli Women in Malaysia. Int. J. Public Health Clin. Sci. 2015, 2, 55–66. [Google Scholar]
- Al-Delaimy, A.K.; Al-Mekhlafi, H.M.; AL Lim, Y.; A Nasr, N.; Sady, H.; Atroosh, W.M.; Mahmud, R. Developing and evaluating health education learning package (HELP) to control soil-transmitted helminth infections among Orang Asli children in Malaysia. Parasites Vectors 2014, 7, 416. [Google Scholar] [CrossRef]
- Lee, S.C.; Tang, M.S.; Easton, A.V.; Devlin, J.C.; Chua, L.L.; Cho, I.; Moy, F.M.; Khang, T.F.; Lim, Y.A.L.; Loke, P. Linking the effects of helminth infection, diet and the gut microbiota with human whole-blood signatures. PLoS Pathog. 2019, 15, e1008066. [Google Scholar] [CrossRef] [PubMed]
- Nasr, N.A.; Al-Mekhlafi, H.M.; Ahmed, A.; Roslan, M.A.; Bulgiba, A. Towards an effective control programme of soil-transmitted helminth infections among Orang Asli in rural Malaysia. Part 1: Prevalence and associated key factors. Parasites Vectors 2013, 6, 27. [Google Scholar] [CrossRef] [PubMed]
- Anuar, T.S.; Ghani, M.K.; Azreen, S.N.; Salleh, F.M.; Moktar, N. Blastocystis infection in Malaysia: Evidence of waterborne and human-to-human transmissions among the Proto-Malay, Negrito and Senoi tribes of Orang Asli. Parasites Vectors 2013, 6, 40. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).