Higher Adherence to Plant-Based Diet Lowers Type 2 Diabetes Risk among High and Non-High Cardiovascular Risk Populations: A Cross-Sectional Study in Shanxi, China
Abstract
1. Introduction
2. Materials and Methods
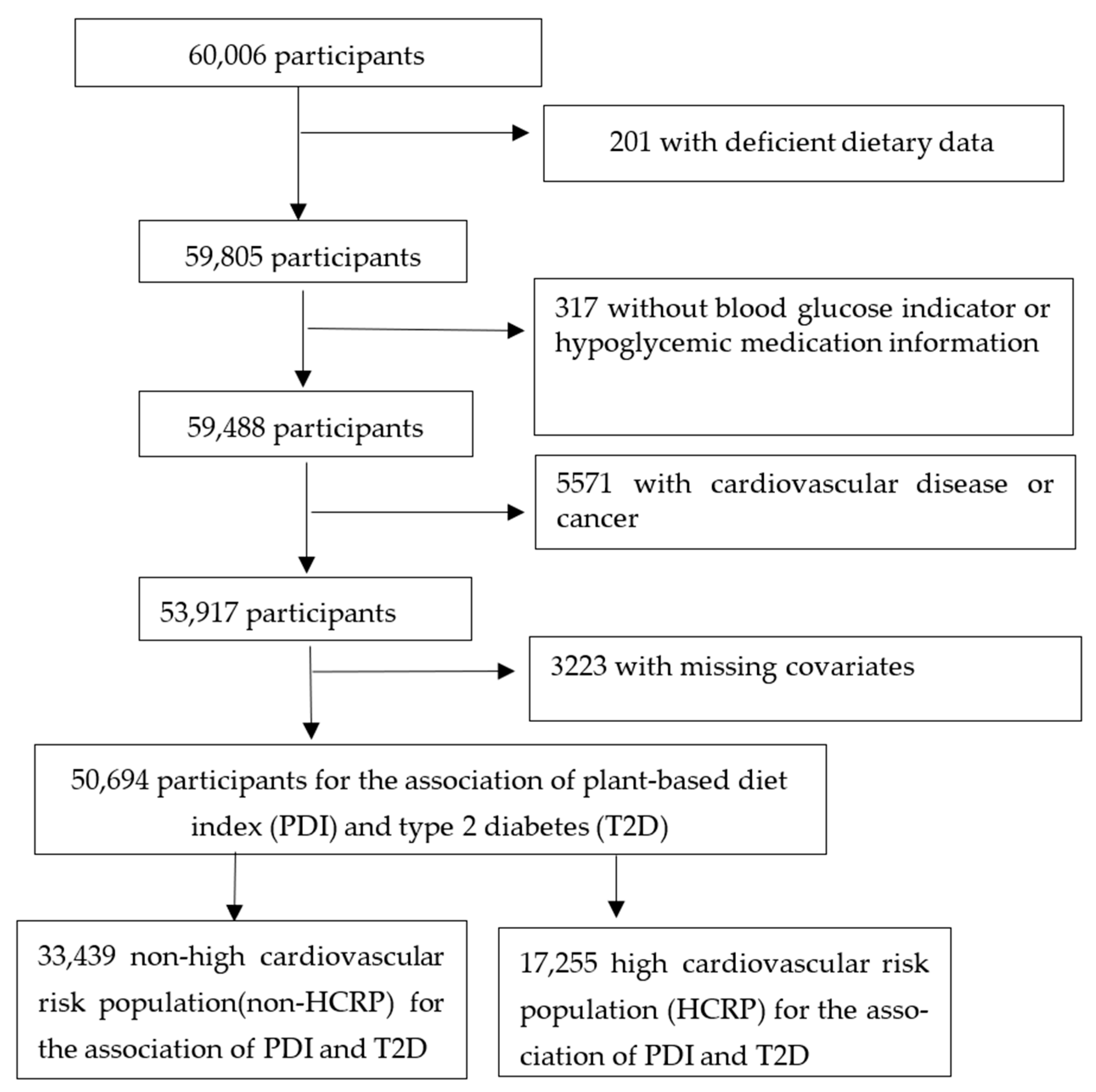
2.1. Study Design and Participants
2.2. Determining the High Cardiovascular Risk Population (HCRP)
2.3. Dietary Assessment and Plant-Based Diet Index Score
2.4. Determination of Type 2 Diabetes
2.5. Covariates
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Association between Plant-Based Diet Index and Type 2 Diabetes
3.3. Dose–Response Relationship between Plant-Based Diet Index and Type 2 Diabetes
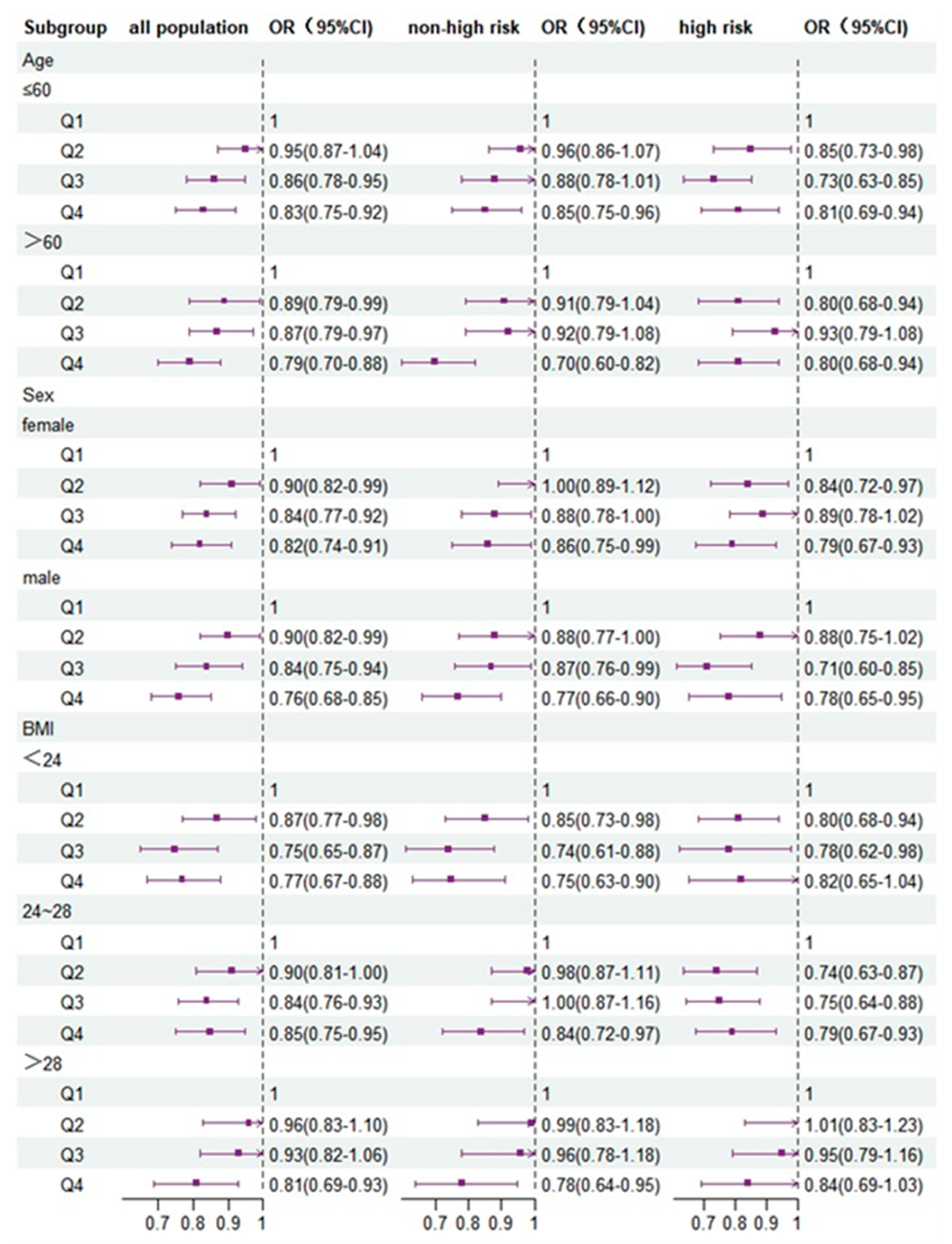
3.4. Subgroup Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ogurtsova, K.; Guariguata, L.; Barengo, N.C.; Ruiz, P.L.D.; Sacre, J.W.; Karuranga, S.; Sun, H.; Boyko, E.J.; Magliano, D.J. IDF diabetes Atlas: Global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res. Clin. Pract. 2022, 183, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Lu, Y.; Yang, H.; Bilige, W.; Li, Y.; Schulz, W.; Masoudi, F.A.; Krumholz, H.M. Characteristics of high cardiovascular risk in 1.7 million Chinese adults. Ann. Intern. Med. 2019, 170, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Teng, D.; Shi, X.; Qin, G.; Qin, Y.; Quan, H.; Shi, B.; Sun, H.; Ba, J.; Chen, B. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: National cross sectional study. BMJ 2020, 369, m997. [Google Scholar] [CrossRef]
- Chatterjee, S.; Khunti, K.; Davies, M.J. Type 2 diabetes. Lancet 2017, 389, 2239–2251. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Drouin-Chartier, J.-P.; Li, Y.; Baden, M.Y.; Manson, J.E.; Willett, W.C.; Voortman, T.; Hu, F.B.; Bhupathiraju, S.N. Changes in plant-based diet indices and subsequent risk of type 2 diabetes in women and men: Three US prospective cohorts. Diabetes Care 2021, 44, 663–671. [Google Scholar] [CrossRef]
- Aune, D.; Norat, T.; Romundstad, P.; Vatten, L.J. Whole grain and refined grain consumption and the risk of type 2 diabetes: A systematic review and dose–response meta-analysis of cohort studies. Eur. J. Epidemiol. 2013, 28, 845–858. [Google Scholar] [CrossRef]
- Matsumoto, S.; Beeson, W.L.; Shavlik, D.J.; Siapco, G.; Jaceldo-Siegl, K.; Fraser, G.; Knutsen, S.F. Association between vegetarian diets and cardiovascular risk factors in non-Hispanic white participants of the Adventist Health Study-2. J. Nutr. Sci. 2019, 8, e6. [Google Scholar] [CrossRef]
- Storz, M.A. What makes a plant-based diet? a review of current concepts and proposal for a standardized plant-based dietary intervention checklist. Eur. J. Clin. Nutr. 2022, 76, 789–800. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Shi, Z.M.; Yu, C.-Q. Progress on statistical methods in evaluating Dietary Patterns. Acta Nutr. Sin. 2021, 43, 615–618. [Google Scholar]
- Laouali, N.; Shah, S.; MacDonald, C.-J.; Mahamat-Saleh, Y.; El Fatouhi, D.; Mancini, F.; Fagherazzi, G.; Boutron-Ruault, M.-C. BMI in the Associations of Plant-Based Diets with Type 2 Diabetes and Hypertension Risks in Women: The E3N Prospective Cohort Study. J. Nutr. 2021, 151, 2731–2740. [Google Scholar] [CrossRef]
- Daneshzad, E.; Jahangir, F.; Heshmati, J.; Larijani, B.; Surkan, P.J.; Azadbakht, L. Associations between plant-based dietary indices and dietary acid load with cardiovascular risk factors among diabetic patients. Int. J. Diabetes Dev. Ctries. 2021, 41, 71–83. [Google Scholar] [CrossRef]
- Chen, Z.; Qian, F.; Liu, G.; Li, M.; Voortman, T.; Tobias, D.K.; Ley, S.H.; Bhupathiraju, S.N.; Li, L.-J.; Chavarro, J.E. Prepregnancy plant-based diets and the risk of gestational diabetes mellitus: A prospective cohort study of 14,926 women. Am. J. Clin. Nutr. 2021, 114, 1997–2005. [Google Scholar] [CrossRef]
- Chen, Z.; Zuurmond, M.G.; van der Schaft, N.; Nano, J.; Wijnhoven, H.A.H.; Ikram, M.A.; Franco, O.H.; Voortman, T. Plant versus animal based diets and insulin resistance, prediabetes and type 2 diabetes: The Rotterdam Study. Eur. J. Epidemiol. 2018, 33, 883–893. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Li, Y.; Wang, C.; Mao, Z.; Chen, Y.; Ren, P.; Fan, M.; Cui, S.; Niu, K.; Gu, R. Association of plant-based diet and type 2 diabetes mellitus in Chinese rural adults: The Henan Rural Cohort Study. J. Diabetes Investig. 2021, 12, 1569–1576. [Google Scholar] [CrossRef]
- Wang, H.; Huang, L.; Lin, L.; Chen, X.; Zhong, C.; Li, Q.; Li, N.; Gao, D.; Zhou, X.; Chen, R.; et al. The overall plant-based diet index during pregnancy and risk of gestational diabetes mellitus: A prospective cohort study in China. Br. J. Nutr. 2021, 126, 1519–1528. [Google Scholar] [CrossRef] [PubMed]
- Satija, A.; Bhupathiraju, S.N.; Spiegelman, D.; Chiuve, S.E.; Manson, J.E.; Willett, W.; Rexrode, K.M.; Rimm, E.B.; Hu, F.B. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in US adults. J. Am. Coll. Cardiol. 2017, 70, 411–422. [Google Scholar] [CrossRef]
- Kim, J.; Giovannucci, E. Healthful Plant-Based Diet and Incidence of Type 2 Diabetes in Asian Population. Nutrients 2022, 14, 3078. [Google Scholar] [CrossRef]
- Chen, G.C.; Koh, W.P.; Neelakantan, N.; Yuan, J.M.; Qin, L.Q.; van Dam, R.M. Diet Quality Indices and Risk of Type 2 Diabetes Mellitus: The Singapore Chinese Health Study. Am. J. Epidemiol. 2018, 187, 2651–2661. [Google Scholar] [CrossRef]
- Flores, A.C.; Heron, C.; Kim, J.I.; Martin, B.; Al-Shaar, L.; Tucker, K.L.; Gao, X. Prospective Study of Plant-Based Dietary Patterns and Diabetes in Puerto Rican Adults. J. Nutr. 2021, 151, 3795–3800. [Google Scholar] [CrossRef]
- Amini, M.R.; Shahinfar, H.; Djafari, F.; Sheikhhossein, F.; Naghshi, S.; Djafarian, K.; Clark, C.C.; Shab-Bidar, S. The association between plant-based diet indices and metabolic syndrome in Iranian older adults. Nutr. Health 2021, 27, 435–444. [Google Scholar] [CrossRef]
- Kim, H.; Lee, K.; Rebholz, C.M.; Kim, J. Association between unhealthy plant-based diets and the metabolic syndrome in adult men and women: A population-based study in South Korea. J. Nutr. 2021, 125, 577–590. [Google Scholar] [CrossRef]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Andrews, K.G.; Engell, R.E.; Mozaffarian, D. Global, regional and national consumption of major food groups in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open 2015, 5, e008705. [Google Scholar] [CrossRef]
- Hopping, B.N.; Erber, E.; Grandinetti, A.; Verheus, M.; Kolonel, L.N.; Maskarinec, G. Dietary fiber, magnesium, and glycemic load alter risk of type 2 diabetes in a multiethnic cohort in Hawaii. J. Nutr. 2010, 140, 68–74. [Google Scholar] [CrossRef]
- Chen, B.; Zeng, J.; Qin, M.; Xu, W.; Zhang, Z.; Li, X.; Xu, S. The Association Between Plant-Based Diet Indices and Obesity and Metabolic Diseases in Chinese Adults: Longitudinal Analyses From the China Health and Nutrition Survey. Front. Nutr. 2022, 9, 881901. [Google Scholar] [CrossRef]
- Lu, J.; Xuan, S.; Downing, N.S.; Wu, C.; Li, L.; Krumholz, H.M.; Jiang, L. Protocol for the China PEACE (Patient-centered Evaluative Assessment of Cardiac Events) million persons project pilot. BMJ Open 2016, 6, e010200. [Google Scholar] [CrossRef]
- Cournot, M.; Taraszkiewicz, D.; Cambou, J.-P.; Galinier, M.; Boccalon, H.; Hanaire-Broutin, H.; Chamontin, B.; Carrié, D.; Ferrières, J. Additional prognostic value of physical examination, exercise testing, and arterial ultrasonography for coronary risk assessment in primary prevention. Am. Heart J. 2009, 158, 845–851. [Google Scholar] [CrossRef]
- Yu, C.; Shi, Z.; Lv, J.; Guo, Y.; Bian, Z.; Du, H.; Chen, Y.; Tao, R.; Huang, Y.; Chen, J. Dietary patterns and insomnia symptoms in Chinese adults: The China Kadoorie Biobank. Nutrients 2017, 9, 232. [Google Scholar] [CrossRef]
- Chen, H.; Shen, J.; Xuan, J.; Zhu, A.; Ji, J.S.; Liu, X.; Cao, Y.; Zong, G.; Zeng, Y.; Wang, X. Plant-based dietary patterns in relation to mortality among older adults in China. Nat. Aging 2022, 2, 224–230. [Google Scholar] [CrossRef]
- Zhu, A.; Chen, H.; Shen, J.; Wang, X.; Li, Z.; Zhao, A.; Shi, X.; Yan, L.; Zeng, Y.; Yuan, C. Interaction between plant-based dietary pattern and air pollution on cognitive function: A prospective cohort analysis of Chinese older adults. Lancet Reg. Health-West. Pac. 2022, 20, 100372. [Google Scholar] [CrossRef]
- Association, A.D. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010, 33 (Suppl. S1), S62–S69. [Google Scholar] [CrossRef]
- Zhu, J.; Gao, R.; Zhao, Y.; Lu, G.; Zhao, D.; Li, J. Guidelines for the prevention and treatment of dyslipidemia in adults in China (2016 Revision). J. Chin. Inst. Eng. 2016, 31, 937–953. [Google Scholar]
- Zhu, F.; Qin, Y.; Bi, Y.; Su, J.; Cui, L.; Luo, P.; Du, W.; Miao, W.; Wang, J.; Zhou, J. Fresh vegetable and fruit consumption and carotid atherosclerosis in high-cardiovascular-risk population: A cross-sectional study in Jiangsu, China. Cad. Saúde Pública 2021, 37, e00033020. [Google Scholar] [CrossRef]
- Qian, F.; Liu, G.; Hu, F.B.; Bhupathiraju, S.N.; Sun, Q. Association between plant-based dietary patterns and risk of type 2 diabetes: A systematic review and meta-analysis. JAMA Intern. Med. 2019, 179, 1335–1344. [Google Scholar] [CrossRef]
- Kim, H.; Lee, K.; Rebholz, C.M.; Kim, J. Plant-based diets and incident metabolic syndrome: Results from a South Korean prospective cohort study. PLoS Med. 2020, 17, e1003371. [Google Scholar] [CrossRef]
- Neuenschwander, M.; Ballon, A.; Weber, K.S.; Norat, T.; Aune, D.; Schwingshackl, L.; Schlesinger, S. Role of diet in type 2 diabetes incidence: Umbrella review of meta-analyses of prospective observational studies. BMJ 2019, 366, l2368. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Bulló, M.; Estruch, R.; Ros, E.; Covas, M.-I.; Ibarrola-Jurado, N.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V. Prevention of diabetes with Mediterranean diets: A subgroup analysis of a randomized trial. Ann. Intern. Med. 2014, 160, 1–10. [Google Scholar] [CrossRef]
- Glenn, A.J.; Hernández-Alonso, P.; Kendall, C.W.; Martínez-González, M.Á.; Corella, D.; Fitó, M.; Martínez, J.A.; Alonso-Gómez, Á.M.; Wärnberg, J.; Vioque, J. Longitudinal changes in adherence to the portfolio and DASH dietary patterns and cardiometabolic risk factors in the PREDIMED-Plus study. Clin. Nutr. 2021, 40, 2825–2836. [Google Scholar] [CrossRef]
- Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Ruiz-Gutiérrez, V.; Covas, M.I.; Fiol, M.; Gómez-Gracia, E.; López-Sabater, M.C.; Vinyoles, E. Effects of a Mediterranean-style diet on cardiovascular risk factors: A randomized trial. Ann. Intern. Med. 2006, 145, 1–11. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Marfisi, R.; Levantesi, G.; Silletta, M.G.; Tavazzi, L.; Tognoni, G.; Valagussa, F.; Marchioli, R. Incidence of new-onset diabetes and impaired fasting glucose in patients with recent myocardial infarction and the effect of clinical and lifestyle risk factors. Lancet 2007, 370, 667–675. [Google Scholar] [CrossRef]
- Satija, A.; Malik, V.; Rimm, E.B.; Sacks, F.; Willett, W.; Hu, F.B. Changes in intake of plant-based diets and weight change: Results from 3 prospective cohort studies. Am. J. Clin. Nutr. 2019, 110, 574–582. [Google Scholar] [CrossRef]
- Toumpanakis, A.; Turnbull, T.; Alba-Barba, I. Effectiveness of plant-based diets in promoting well-being in the management of type 2 diabetes: A systematic review. BMJ Open Diabetes Res. Care 2018, 6, e000534. [Google Scholar] [CrossRef]
- Vitale, M.; Masulli, M.; Cocozza, S.; Anichini, R.; Babini, A.C.; Boemi, M.; Bonora, E.; Buzzetti, R.; Carpinteri, R.; Caselli, C.; et al. Sex differences in food choices, adherence to dietary recommendations and plasma lipid profile in type 2 diabetes—The TOSCA.IT study. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 879–885. [Google Scholar] [CrossRef]
- Weickert, M.O.; Pfeiffer, A.F. Impact of dietary fiber consumption on insulin resistance and the prevention of type 2 diabetes. J. Nutr. 2018, 148, 7–12. [Google Scholar] [CrossRef]
- Rienks, J.; Barbaresko, J.; Oluwagbemigun, K.; Schmid, M.; Nöthlings, U. Polyphenol exposure and risk of type 2 diabetes: Dose-response meta-analyses and systematic review of prospective cohort studies. Am. J. Clin. Nutr. 2018, 108, 49–61. [Google Scholar] [CrossRef]
- PREDIMED study investigators. Intake of total polyphenols and some classes of polyphenols is inversely associated with diabetes in elderly people at high cardiovascular disease risk. J. Nutr. 2015, 146, 767–777. [Google Scholar] [CrossRef]
- Malik, V.S.; Li, Y.; Tobias, D.K.; Pan, A.; Hu, F.B. Dietary protein intake and risk of type 2 diabetes in US men and women. Am. J. Epidemiol. 2016, 183, 715–728. [Google Scholar] [CrossRef]
- Ye, J.; Yu, Q.; Mai, W.; Liang, P.; Liu, X.; Wang, Y. Dietary protein intake and subsequent risk of type 2 diabetes: A dose–response meta-analysis of prospective cohort studies. Acta Diabetol. 2019, 56, 851–870. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Sanchez-Tainta, A.; Corella, D.; Salas-Salvado, J.; Ros, E.; Aros, F.; Gomez-Gracia, E.; Fiol, M.; Lamuela-Raventos, R.M.; Schröder, H. A provegetarian food pattern and reduction in total mortality in the Prevención con Dieta Mediterránea (PREDIMED) study. Am. J. Clin. Nutr. 2014, 100 (Suppl. S1), 320S–328S. [Google Scholar] [CrossRef]
- Mohammadifard, N.; Sajjadi, F.; Maghroun, M.; Alikhasi, H.; Nilforoushzadeh, F.; Sarrafzadegan, N. Validation of a simplified food frequency questionnaire for the assessment of dietary habits in Iranian adults: Isfahan Healthy Heart Program, Iran. ARYA Atheroscler. 2015, 11, 139. [Google Scholar]

| Q1 (n = 16,965) | Q2 (n = 10,480) | Q3 (n = 14,479) | Q4 (n = 8970) | p | |
|---|---|---|---|---|---|
| PDI | 27–44 | 45–46 | 47–49 | 50–60 | |
| Glucose (mmol/L) a | 6.00 ± 1.60 | 5.91 ± 1.45 | 5.87 ± 1.45 | 5.88 ± 1.42 | <0.001 |
| Age (years) a | 54.7 ± 9.89 | 54.9 ± 9.67 | 55.5 ± 9.55 | 56.3 ± 9.23 | <0.001 |
| Sex, n (%) | <0.001 | ||||
| Women | 9305 (54.8) | 5922 (56.5) | 8664 (60.7) | 5980 (66.7) | |
| Men | 7660 (45.2) | 4558 (43.5) | 5615 (39.3) | 2990 (33.3) | |
| Geographic region, n (%) | <0.001 | ||||
| Urban | 9264 (54.6) | 3976 (37.9) | 3599 (25.2) | 1766 (19.7) | |
| Rural | 7701 (45.4) | 6504 (62.1) | 10,680 (74.8) | 7204 (80.3) | |
| Education level, n (%) | <0.001 | ||||
| High school or above | 5862 (34.6) | 2803 (26.7) | 2980 (20.9) | 1404 (15.7) | |
| Other | 11,103 (65.4) | 7677 (73.3) | 11,299 (79.1) | 7566 (84.3) | |
| Marital status, n (%) | <0.001 | ||||
| Married/cohabiting | 16,142 (95.1) | 9944 (94.9) | 13,458 (94.3) | 8416 (93.8) | |
| Other | 823 (4.9) | 536 (5.1) | 821 (5.7) | 554 (6.2) | |
| Occupation, n (%) | <0.001 | ||||
| Farmer | 7334 (43.2) | 5811 (55.4) | 9307 (65.2) | 6514 (72.6) | |
| Retired | 4102 (24.2) | 2005 (19.1) | 2240 (15.7) | 1287 (14.3) | |
| Other | 5529 (32.6) | 2664 (25.4) | 2732 (19.1) | 1169 (13) | |
| Household income, n (%) | <0.001 | ||||
| <RMB 50,000 | 14,467 (85.3) | 9423 (89.9) | 13,142 (92) | 8466 (94.4) | |
| ≥RMB 50,000 | 2498 (14.7) | 1057 (10.1) | 1137 (8) | 504 (5.6) | |
| Physical activity, n (%) | |||||
| ≥1 day/week | 5806 (34.2) | 3171 (30.3) | 3632 (25.4) | 2320 (25.9) | |
| Other | 11,159 (65.8) | 7309 (69.7) | 10,647 (74.6) | 6650 (74.1) | |
| BMI, n (%) | <0.001 | ||||
| 24 | 6358 (37.5) | 3679 (35.1) | 4825 (33.8) | 2847 (31.7) | |
| 24–28 | 7496 (44.2) | 4641 (44.3) | 6351 (44.5) | 4044 (45.1) | |
| ≥28 | 3111 (18.3) | 2160 (20.6) | 3103 (21.7) | 2079 (23.2) | |
| Alcohol drinking, n (%) | <0.001 | ||||
| ≥2 days/week | 1517 (8.9) | 713 (6.8) | 929 (6.5) | 515 (5.7) | |
| Other | 15,448 (91.1) | 9767 (93.2) | 13,350 (93.5) | 8455 (94.3) | |
| Tobacco smoking, n (%) | <0.001 | ||||
| Never | 12,762 (75.2) | 7845 (74.9) | 11,098 (77.7) | 7201 (80.3) | |
| Other | 4203 (24.8) | 2635 (25.1) | 3181 (22.3) | 1769 (19.7) | |
| Waist circumference, n (%) | <0.001 | ||||
| Obese | 6070 (35.8) | 3576 (34.1) | 4648 (32.6) | 2839 (31.6) | |
| Normal | 10,895 (64.2) | 6904 (65.9) | 9631 (67.4) | 6131 (68.4) | |
| T2D, n (%) | <0.001 | ||||
| Yes | 2822 (16.6) | 1560 (14.9) | 2004(14) | 1268 (14.1) | |
| No | 14,143 (83.4) | 8920 (85.1) | 12,275 (86) | 7702 (85.9) | |
| Fruit, n (%) | <0.001 | ||||
| 1–3 days/month | 478 (27.8) | 1791 (17.1) | 2196 (15.4) | 1163 (13) | |
| ≥1day/week | 12,257 (72.2) | 8689 (82.9) | 12,083 (84.6) | 7807 (87) | |
| Vegetables, n (%) | <0.001 | ||||
| 1–3 days/month | 1818 (10.7) | 526 (5) | 380 (2.7) | 101 (1.1) | |
| ≥1 day/week | 15,147 (89.3) | 9954 (95) | 13,899 (97.3) | 8869 (98.9) | |
| Grain, n (%) | <0.001 | ||||
| 1–3 days/month | 4646 (27.4) | 1763 (16.8) | 1,571 (11) | 524 (5.8) | |
| ≥1 day/week | 12,319 (72.6) | 8717 (83.2) | 12,708 (89) | 8446 (94.2) | |
| Meat, n (%) | <0.001 | ||||
| Every day | 2549 (15) | 514 (4.9) | 499 (3.5) | 264 (2.9) | |
| 6 days/week | 14,416 (85) | 9966 (95.1) | 13,780 (96.5) | 8706 (97.1) | |
| Group | Score Range | n/N | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |||
| Total population | |||||
| Q1 | 27–44 | 2822/16,965 | 1.00 | 1.00 | 1.00 |
| Q2 | 45–46 | 1560/10,480 | 0.87 (0.81–0.93) * | 0.90 (0.84–0.96) * | 0.90 (0.83–0.96) * |
| Q3 | 47–49 | 2004/14,279 | 0.79 (0.74–0.84) * | 0.83 (0.78–0.89) * | 0.83 (0.78–0.89) * |
| Q4 | 50–60 | 1268/8970 | 0.78 (0.72–0.84) * | 0.83 (0.77–0.90) * | 0.82 (0.76–0.89) * |
| ptrend | <0.001 | <0.001 | <0.001 | ||
| 1SD | 0.90 (0.87–0.91) * | 0.91 (0.89–0.94) * | 0.91 (0.89–0.93) * | ||
| Non-HCRP | |||||
| Q1 | 27–43 | 1404/9573 | 1.00 | 1.00 | 1.00 |
| Q2 | 44–46 | 1340/10,129 | 0.88 (0.82–0.96) | 0.94 (0.87–1.03) | 0.94 (0.87–1.02) |
| Q3 | 47–48 | 761/6125 | 0.82 (0.74–0.90) * | 0.90 (0.82–0.99) * | 0.90 (0.82–0.99) * |
| Q4 | 49–60 | 838/7612 | 0.70 (0.63–0.76) * | 0.80 (0.73–0.89) * | 0.80 (0.72–0.88) * |
| ptrend | <0.001 | <0.001 | <0.001 | ||
| 1SD | 0.87 (0.84–0.90) * | 0.92 (0.88–0.95) * | 0.91 (0.88–0.94) * | ||
| HCRP | |||||
| Q1 | 27–45 | 1294/5839 | 1.00 | 1.00 | 1.00 |
| Q2 | 46–47 | 649/3616 | 0.77 (0.69–0.85) * | 0.83 (0.74–0.93) * | 0.83 (0.74–0.92) * |
| Q3 | 48–49 | 696/4042 | 0.72 (0.65–0.80) * | 0.82 (0.74–0.91) * | 0.82 (0.73–0.91) * |
| Q4 | 50–60 | 672/3758 | 0.73 (0.66–0.81) * | 0.81 (0.73–0.91) * | 0.81 (0.72–0.90) * |
| ptrend | 0.002 | 0.010 | <0.001 | ||
| 1SD | 0.86 (0.83–0.90) * | 0.91 (0.87–0.94) * | 0.90 (0.87–0.94) * | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Meng, Y.; Wang, J. Higher Adherence to Plant-Based Diet Lowers Type 2 Diabetes Risk among High and Non-High Cardiovascular Risk Populations: A Cross-Sectional Study in Shanxi, China. Nutrients 2023, 15, 786. https://doi.org/10.3390/nu15030786
Zhang Y, Meng Y, Wang J. Higher Adherence to Plant-Based Diet Lowers Type 2 Diabetes Risk among High and Non-High Cardiovascular Risk Populations: A Cross-Sectional Study in Shanxi, China. Nutrients. 2023; 15(3):786. https://doi.org/10.3390/nu15030786
Chicago/Turabian StyleZhang, Ying, Yaqing Meng, and Junbo Wang. 2023. "Higher Adherence to Plant-Based Diet Lowers Type 2 Diabetes Risk among High and Non-High Cardiovascular Risk Populations: A Cross-Sectional Study in Shanxi, China" Nutrients 15, no. 3: 786. https://doi.org/10.3390/nu15030786
APA StyleZhang, Y., Meng, Y., & Wang, J. (2023). Higher Adherence to Plant-Based Diet Lowers Type 2 Diabetes Risk among High and Non-High Cardiovascular Risk Populations: A Cross-Sectional Study in Shanxi, China. Nutrients, 15(3), 786. https://doi.org/10.3390/nu15030786





