Abstract
The coronavirus disease 2019 (COVID-19) is an epidemic caused by SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2). Populations at risk as well as those who can develop serious complications are people with chronic diseases such as diabetes, hypertension, and the elderly. Severe symptoms of SARS-CoV-2 infection are associated with immune failure and dysfunction. The approach of strengthening immunity may be the right choice in order to save lives. This review aimed to provide an overview of current information revealing the importance of bee products in strengthening the immune system against COVID-19. We highlighted the immunomodulatory and the antiviral effects of zinc and polyphenols, which may actively contribute to improving symptoms and preventing complications caused by COVID-19 and can counteract viral infections. Thus, this review will pave the way for conducting advanced experimental research to evaluate zinc and polyphenols-rich bee products to prevent and reduce the severity of COVID-19 symptoms.
1. Introduction
On 11 March 2020, the World Health Organization recognized the new coronavirus disease 2019 (COVID-19) as a pandemic. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was detected for the first time in Wuhan, China, at the end of 2019; the virus has not reported before in humans [1]. The virus is highly contagious and is transmitted through close contact with the contaminated person via respiratory droplets from coughing, and/or direct contact with contaminated surfaces [2]. Security measures imposed include washing hands frequently with soap and water, disinfecting them with a hydroalcoholic solution, wearing a mask when leaving the house, keeping to at least one meter away from anyone, avoid touching eyes, nose, or mouth when coughing or sneezing, and covering the nose and mouth with the bend of the elbow or with a tissue [3]. Most infected people have mild to moderate disease symptoms. The most frequent symptoms are fever, dry cough, fatigue, in addition to body aches, sore throat, diarrhea, conjunctivitis, headache, loss of smell or taste, rash, or discoloration of the fingers or toes; the most serious symptoms include difficulty in breathing or shortness of breath, feeling of tightness or pain in the chest, and loss of speech or motor skills [4,5]. Some infected people may be asymptomatic but they transmit the virus to other persons. Currently, there is no specific treatment for coronavirus infection. In non-hospitalized people, treatment aims to relieve symptoms and the most recommended active ingredient is paracetamol [6]. In other patients, doctors have introduced other drugs to treat the disease; these drugs were originally developed to treat other pathologies such as immunomodulatory drugs (e.g., interferons), and antiviral drugs which act by inhibiting the entry of the virus inside the cell (e.g., hydroxychloroquine, niclosamide, camostat), or by inhibiting viral proteases (e.g., lopinavir/ritonavir, PF-07321332, GC376, PF-07304814), other drugs inhibit viral RNA (e.g., remdesivir, molnupiravir), and finally the drugs that inhibit the host proteins which support viral protein synthesis (e.g., plitidepsin, fluvoxamine) [7]. Recently, Pfizer (New York, United States) has announced a new oral antiviral drug, ritonavir in combination with PF-07321332 (PAXLOVID™), that significantly reduces hospitalization and death by 89% of COVID-19 patients at high risk of severe disease [8,9]. The problem that still arises is the safety profile of these drugs. They require further evaluation such as evaluating the possible drug-drug interactions [10]. In addition, certain drugs are expensive and require intravenous administration supervised in a hospital [11].
The reason for the growing consumption of beehive products may be related to their health-oriented and therapeutic properties. The lookout for published studies on bee products and their ability to interact with SARS-CoV-2 and alleviate the symptoms of COVID-19 has attracted a lot of attention as they present a promising source of natural substances that can reduce severe symptoms of infected patients [12,13]. It is worth mentioning that several clinical trials have tested the combination between bee products and standard care to treat COVID-19 patients. For instance, in the trial number NCT04323345, there was a combination of honey given orally and through a nasogastric tube and standard drugs (lopinavir/ritonavir tablets or arbidol or chloroquine phosphate or hydroxychloroquine or oseltamivir with or without azithromycin) [14]. In addition, extract of standardized Brazilian green propolis, EPP-AF® combined with standard care (azithromycin, chloroquine or hydroxychloroquine, oseltamivir, corticosteroids) were used for hospitalized COVID-19 patients in a trial registered under the number NCT04480593 [15]. The outcomes of these studies revealed that combining these natural products with standard care procedures has resulted in clinical benefits for hospitalized COVID-19 patients in comparison to the patients who only received standard care, such as the reduction in hospital stay length.
As there is currently no specific treatment against the COVID-19 pandemic, strengthening the immune system remains the right way to fight the disease. In this review, we suggest that bee products especially their richness in zinc and phenolic compounds may be a beneficial way to strengthen immunity and to protect against the virus SARS-CoV-2.
2. The Role of Immunity in Combating SARS-CoV-2
2.1. Mechanisms of the Immune Response against SARS-CoV-2
The immune system refers to our body’s global ability to resist and defend against different infections (fungi, protozoan, bacteria, and viruses). SARS-CoV-2 is one of these new pathogenic agents that triggers a coordinated immune response: innate immunity (rapid response), adaptive immunity (lower-acting), and passive immunity. When the human body encounters pathogenic antigens for the first time, in some people, especially vulnerable individuals the immune system cannot function quickly, complications may arise [16]. This has been observed in the case of COVID-19. The interface between innate and adaptive immunity immediately begins when the virus (SARS-CoV-2) reaches host cells [17]. This process goes through three essential steps: the identification of the spike glycoprotein of the virus, the elimination of the virus and the infected cells, and finally the development of immunological memory.
2.1.1. The Identification of the Spike Glycoprotein of SARS-CoV-2
When the functional barrier of the immune system (respiratory tract and acid pH of the stomach etc.) fails to block SARS-CoV-2, monocytes, macrophages, and dendritic cells, antigen-presenting cells (APC) recognize and achieve it through the presence of pathogen recognition receptors (PRRs). Then, the first line of host defensive responses is activated. Owing to their intracellular Toll-like receptors (TLRs) especially, TLR3, TLR7, and TLR8, monocytes, macrophages, dendritic cells, and some other cell types recognize the single-stranded RNA of coronaviruses including SARS-CoV-2. Besides, extracellular PRRs identify the spike glycoprotein of the coronavirus coat (Figure 1A) [18,19].
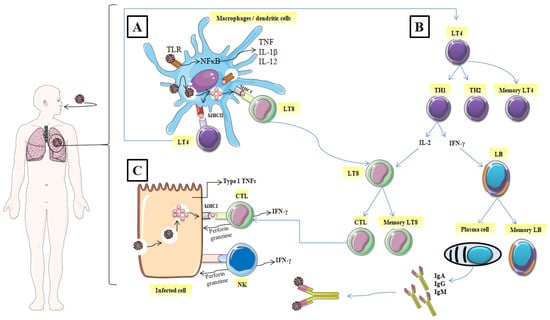
Figure 1.
Mechanisms of the immune response against SARS-CoV-2. (A) identification of the spike glycoprotein of SARS-CoV-2, (B) activation of CD4+ helper T lymphocytes, (C) Elimination of the virus and the infected cell. (TLR: Toll-like receptors; NF-κB: nuclear factor-kappa B; TNF: tumor necrosis factor; IL: interleukin; MHCI: major histocompatibility class I; MCHII: major histocompatibility class I; LT4: CD4+ helper T lymphocyte; LT8: CD8+ helper T lymphocytes; TH1: T helper 1; TH2: T helper 2; IFNγ: interferon, LB: lymphocyte B; CTL: cytotoxic T lymphocyte; NK: natural killer; IgA: immunoglobulin A; IgG: immunoglobulin G; IgM: immunoglobulin M).
2.1.2. Elimination of the Virus, and the Infected Cell
Virally infected cells present on their surface virus antigenic determinants by major histocompatibility class I (MHC I), which are subsequently recognized by antigen-specific CD8+ cytotoxic T lymphocytes and then induce their restriction by the release of the effectors’ molecules such as perforin and granzymes (Figure 1C) [19]. Likewise, Natural killer cells (NK) also recognize and kill the infected host cells. The host immune cells adopted this strategy to slow down the virus invasion and thus, the interaction between the immune system and virally infected cells continues.
After the digestion of the internalized virus, termed antigens are recognized by specific TLRs and present on the surface of the innate immune cells (macrophage or dendritic cells) via MHC I (MHC I); [Human Leukocyte Antigen (HLA) in humans] and MHC II (HLA-Cw∗08) [20]. Furthermore, the recognition of antigen by PRRs enhances the expression of typical inflammatory cytokines such as IL-2, IL-18, IL-1β, type 1 IFNs (IFN-α and IFN-β), and tumor necrosis factor (TNF); it also activates inflammatory signaling and transcription factors such as inflammasome assembly and nuclear factor kappa-B cells (NFκB) [21]. In turn, these inflammatory cytokines initiate the activation of CD4+ helper T lymphocytes with the transition into a T helper (Th) which has a double function: cytokines produce and promote B Cells to generate antibodies. Being stimulated by intracellular pathogens, T helper lymphocytes 1 (Th1) phenotype promotes the cytotoxic T lymphocyte activity by releasing IL-2 and enhances the differentiation of B lymphocytes to plasma cells which produce specific antiviral antibodies by liberating IFN-γ (Figure 1B).
T helper lymphocytes (Th2) activate and promote the degranulation and the release of chemokines, proteases, and histamines by innate immune system cells including mast cells and basophils, which increased vascular permeability and enhanced the recruitment of macrophages and other inflammatory cells [22]. Besides, Th2 migrate to lung tissue and act by inducing airway hyper-responsiveness and metaplasia of the Goblet cells as documented in allergic illnesses [23]. Interactions (between TH1, TH2, and APC) are generally described as cellular cooperation.
2.1.3. Immunological Memory
Thanks to immunological memory, the immune system can specifically recognize and immediately trigger an adequate immune response upon re-contact with an antigen previously encountered by the body (Figure 1B). In addition to the specific antibodies released into the circulation (IgM, IgA, and IgG), after the end of the active immune response, a pool of T memory cells are ready to fight against re-infection, leading to a fast elimination of the specific antigen source [24]. It has been observed that both CD8+ and CD4+ memory T cells in SARS-CoV-2 patients were effective in prompting a specific immune response from 3 months to 6 years without the presence of antigens [25]. Specific humoral immune response (anti-S-RBD IgM and anti-N IgG) against SARS-CoV-2 was found to have similar characteristics to that triggered against other coronavirus infections. IgG antibodies appear within 14 days of the onset of initial symptoms. However, IgA and IgM were detected on the fifth day after the first symptoms [26]. Positivity rates for IgM, IgA and IgG reached their maximum at weeks 4, 5 and 6, respectively [27].
3. Reasons for System Immune Failure
As an escape mechanism, SARS-CoV-2 uses different ways to beat the host immune system, lymphopenia and leukopenia being one of them [28]. After reaching the cell, SARS-CoV-2 encodes different proteins that interrupt molecules of JAKSTAT and TLRs signaling pathways. A recent study discovered that SARS-CoV-2 infection induced a high chemokine secretion and inhibits type I and type III interferon production which leads to the down expression of antiviral genes. Therefore, a decrease in the host’s immune response, especially T cells responses, is accompanied by hyper-inflammation [29]. Besides the reduction in helper T cells and suppressor T cells, SARS-CoV-2 prompts the dysfunction of effectors T cells. Persistent expression of inhibitory receptors such as programmed cell death 1 (PD-1), T cell immunoglobulin and mucin domain 3 (TIM-3), and T cell immunoglobulin and ITIM domain (TIGIT) in response to sustained antigen stimulation leads to T-cell exhaustion [30].
4. The Influence of Zinc on Immunity
4.1. Importance of Zinc in Human Health
Zinc is a trace element that is neither synthesized nor stored by the human body, therefore it must be provided by the daily diet [31]. At a concentration of between 2 and 3 g, zinc represents the second most abundant trace metal in the body after iron, 90% of this concentration is found in muscle and bone; zinc is mainly concentrated inside cells and only 0.1% of the zinc concentration was found in plasma [32]. The cellular homeostasis of Zn is necessary for the proper functioning of the organism, the control of homeostasis is carried out by the importers of the ZIP family who are responsible for the transport of zinc in the cytosol, and the proteins of the ZnT family which export zinc out of the cytosol, and ultimately through zinc-binding proteins such as metallothionein [32].
Previous reports have shown the beneficial effects of zinc. It is very effective against anemia, it stimulates erythropoiesis [33], increases hemoglobin production [34], boosts antioxidant status, and protects against heavy metal toxicity [35]. Zinc supplementation in diabetic rats alleviates hyperglycemia, reduces protein glycosylation, and urinary concentration of proteins, urea, and glucose improves insulin resistance and the alteration of pancreatic morphology [36]. Concerning the endocrine system, Zinc plays an important role in the thyroid hormonal metabolism; its deficiency can slow down the activity of type I-5′deiodinase, an important enzyme that converts the hormone T4 into T3. It has been shown that zinc stimulates leptin secretion, it also acts on insulin and it participates in glycemic control [37]. A study conducted by Ko et al. [38] showed that zinc may increase the tolerance of chronic hepatitis C patients to the treatment with interferon and ribavirin.
4.2. Zinc, Immune System, and Coronavirus
Zinc is involved in the efficiency of the immune system; it acts as a modulator of the immune response via its essential role in the activation and maturation of B and T lymphocytes. Zinc deficiency has been shown to cause a decrease in the number of T and B lymphocytes in the thymus and bone marrow and leads to increased vulnerability to infections and weakened body defenses [39]. Among the arguments which prove the important role of zinc in the immune defense against SARS-CoV-2, one shows that it is deeply involved in the proper functioning of the immune system; for instance, recently it has been reported that zinc can block the interaction between the ACE2 receptor and SARS-CoV-2 spike proteins [40].
4.3. Effect of Zinc in Thymulin
Thymulin or serum thymic factor is a nonapeptidic hormone produced by the thymus epithelial cells discovered in the 197. It has been shown that thymulin is involved in the differentiation of T lymphocytes, which are very important in the body’s defense against pathogens such as bacteria and viruses; thymulin is also an immunomodulator, it stimulates the immune system if it is weakened and it improves the actions of T cells and natural killer cells [41,42]. A study published by Nasseri et al. [43] revealed that thymulin can also alleviate inflammatory pain via the modulation of cell signaling pathways and molecular spine. Previous studies showed that the biological activity of thymulin significantly decreases during dietary zinc restriction (Figure 2), which proves that zinc contributes to the proper functioning of the immune system via its action on thymulin [41,44].
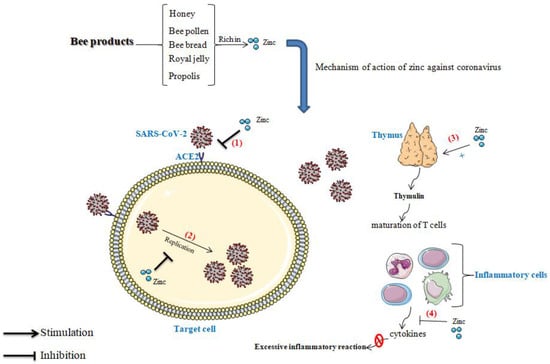
Figure 2.
Role of zinc in immunity; (1) blocks the binding of the virus to the receptor; (2) blocks viral replication, (3): Active the thymulin function, (4) inhibit the excessive inflammatory reaction. (SARS-CoV-2: Severe Acute Respiratory Syndrome-Coronavirus 2; ACE2: Angiotensin-Converting Enzyme 2).
4.4. Role of Zinc in the Blockage of Viral Replication
Zinc is a very powerful antivirus agent; zinc deficiency has been reported to be strongly associated with viral infection risk [45]. Several studies have shown the inhibitory effect of zinc on viruses’ replication (Figure 2). Suara et al. [46] found in a study conducted in vitro that zinc salts blocked the replication of Respiratory Syncytial Virus, and prevented its cell-to-cell spread in HEp-2 cell monolayers pretreated with zinc, or when zinc was added after the infection to a semi-solid recovery medium. Similarly, it has been shown that zinc can reduce the replication of the hepatitis C virus (HCV), and thus, zinc supplementation may improve hepatitis in people with HCV infection [47,48]. In the same way, it has been reported that the replication of the hepatitis E virus was blocked via the inhibition of the activity of RNA-dependent RNA polymerase [49]. More importantly, zinc has shown a promising effect in Human Immunodeficiency Virus-1 (HIV-1) by inhibiting the viral transcription [50].
4.5. Preventive Effect of Zinc against the Excessive Inflammatory Reaction
Recent studies have shown that people who are infected with the novel COVID-19 present an aggressive inflammatory response with high levels of pro-inflammatory cytokines, which include interferon, interleukins, and chemokines. The cytokine storm is among the leading causes of death in the COVID-19 pandemic [51]. Molecularly, different signaling pathways have been involved in the inflammatory process; hence, the modulation of these routes is a major key to the management of the inflammatory response. The nuclear factor kappa-B (NF-κB) signaling pathway is one of them; it was found that zinc enhances the expression of peroxisome proliferator-activated receptor α (PRAR-α) and thus negatively regulates the NF-κB signaling pathway in the DNA nuclear, which leads to the minimization of adhesion molecules and pro-inflammatory cytokines generation [52]. Likewise, Haase et al. [53] documented that zinc plays its anti-inflammatory role by activating the A20 mRNA, the induction of protein A20 inhibits gene expression of TNF and IL-1-Induced NF-κB activation; and down-regulates Toll-like receptors (TLRs) pathway by removing K63-linked ubiquitin chains from the associated adaptor protein (Figure 2).
6. Role of Bioactive Compounds in Bee Products in the Management of COVID-19
6.1. Zinc
6.1.1. The Content of Zinc in Bee Products
In addition to the several bioactive compounds presented in bee products, mineral elements present important ingredients; they are used as a marker of their quality, safety, botanical, and geographical origin [114]. Additionally, bee products present a good source of zinc, and its role as supplementary of the deficiencies cannot be overestimated. Hence, considering the importance of zinc in the treatment of COVID-19 [115,116], bee products rich in zinc could improve symptoms caused by SARS-CoV-2.
Several studies were designed to determine zinc content in beehive products from different countries. As presented in Table 1, the Moroccan bee bread contains 3.31 ± 0.4 mg/kg of zinc, the Romanian samples have a content ranging between 29.54 and 31.85 mg/kg, the Malaysian bee bread sample contains 60.6175 ± 11.8112 mg/kg, the Lithuanian bee bread contains from 11.5 to 42.7 mg/kg of zinc, and the Turkish samples contain values oscillating between 52.55 and 73.96 mg/kg [87,117,118,119,120]. On the other hand, zinc content in bee pollen samples harvested from different geographical locations in Turkey was ranged from 14.832 to 68 mg/kg [87,121,122,123]. Indeed, in Brazil, the studies showed that the zinc content ranged from 39 to 76 mg/kg in bee pollen. Furthermore, other investigations reported that bee pollen samples from Serbia, Spain, Jordan, Slovakia, Poland, China, and Greece showed high contents of zinc, ranging from 18.8 to 159.3 mg/kg [124,125,126,127,128,129,130].
Propolis is another bee product very rich in mineral elements, especially zinc. According to the studies carried out on propolis samples originating from Argentina, Turkey, Poland, Spain, Brazil, Chile, Lithuania, Serbia, Greece, the content in Zinc ranged from 5.5 to 460.7 mg/kg [120,131,132,133,134,135,136,137,138,139,140]. Honey is the most studied bee product for mineral content, and zinc has been analyzed by several researchers [141,142,143,144,145,146,147,148,149,150,151,152,153,154,155]. The lowest contents were found in honey from Kenya, where the values ranged between 0.05 and 0.35 mg/kg. However, the highest values were recorded for honey from Malaysia (from 4.70 to 173.77 mg/kg).
Concerning royal jelly, samples produced in France, China, Germany, and Lithuania were analyzed and showed a content of zinc ranging from 17.56 to 26 mg/kg [120,156,157,158].

Table 1.
The zinc content of bee products (bee bread, bee pollen, propolis, royal jelly) from different countries.
Table 1.
The zinc content of bee products (bee bread, bee pollen, propolis, royal jelly) from different countries.
| Bee Products | Country | Collection Period | Content in Zinc | Reference |
|---|---|---|---|---|
| Bee bread | Lithuania | 2018 | From 11.5 to 42.7 mg/kg | [120] |
| Morocco | - | 3.31 ± 0.4 mg/kg | [117] | |
| Romania | - | From 29.54 to 31.85 mg/kg | [119] | |
| Malaysia | - | 60.61 ± 11.81 mg/kg | [118] | |
| Turkey | April to September 2018 | From 52.55 to 73.96 mg/kg | [87] | |
| Bee pollen | Italy | 2018 | 25.5 mg/kg | [120] |
| Denmark | 2018 | 22.3 mg/kg | [120] | |
| Sweden | 2018 | 23.3 mg/kg | [120] | |
| Slovakia | 2018 | 28.7 mg/kg | [120] | |
| Poland | 2018 | 31.7 mg/kg | [120] | |
| Lithuania | 2018 | From 20.3 to 27.8 mg/kg | [120] | |
| Ukraine | 2018 | From 20.8 to 22.1 mg/kg | [120] | |
| Latvia | 2018 | From 23.5 to 24.7 mg/kg | [120] | |
| Turkey | (April to September 2018) | From 39.37 to 68 mg/kg | [87] | |
| Serbia | (spring and summer of 2011) | From 28.76 to 75.92 mg/kg | [159] | |
| Turkey | - | From 25.94 to 49.74 mg/kg | [121] | |
| Brazil | August 2005 to April 2006 | From 45.07 to 55.22 mg/kg | [160] | |
| Spain | 1993 | From 18.8 to 81.1 mg/kg | [129] | |
| Jordan | March to October 2017 | From 25.24 to 77.02 mg/kg | [124] | |
| Turkey | - | From 14.832 to 39.037 mg/kg | [122] | |
| Slovakia | Spring season 2007 | From 31.9 to 39.9 mg/kg | [128] | |
| Poland | June or August 2009. | From 75.2 to 159.3 mg/kg | [125] | |
| China | Flower season of 2010 | From 28.25 to 65.30 mg/kg | [130] | |
| Turkey | - | From 20.21 to 59.57 mg/kg | [123] | |
| Brazil | - | From 39 to 76 mg/kg | [161] | |
| Greece | March to October 2018 | From 24 to 90 mg/kg | [127] | |
| Propolis | Poland | 2018 | 52.4 mg/kg | [120] |
| Lithuania | 2018 | From 31.9 to 102.1 mg/kg | [120] | |
| Argentina | - | From 53 to 68 mg/kg | [136] | |
| Turkey | - | From 17.60 to 67.60 mg/kg | [133] | |
| Poland | - | From 16.88 to 99.68 mg/kg | [138] | |
| Spain | - | From 163 to 279 mg/kg | [131] | |
| Brazil | - | 113.5 ± 16.9 mg/kg | [139] | |
| Argentina | - | From 34.0 to 105.0 mg/kg | [132] | |
| Chile | - | From 5.5 to 105.0 mg/kg | [135] | |
| Spain | - | From 17.4 to 460.7 mg/kg | [135] | |
| Poland | from May to September 2018 | 40.1 ± 2.7 mg/kg | [120] | |
| Lithuania | from May to September 2018 | From 31.9 to 102.1 mg/kg | [120] | |
| Brazil | from January to March 2011 | From 10 to 50 mg/kg | [134] | |
| Serbia | 2013 | From 19.2 to 241 mg/kg | [140] | |
| Greece | Between spring 2013 and August 2014 | From 30.7 to 383.8 mg/kg | [137] | |
| Honey | Morocco | Summer of 2015 and 2016 | From 1.09 to 4.02 mg/kg | [145] |
| Lithuania | 2018 | From 1.08 to 5.15 mg/kg | [120] | |
| Italy | 2018 | 2.03 mg/kg | [120] | |
| Greece | 2018 | 2.18 mg/kg | [120] | |
| Serbia | 2016 | From 0.78 to 1.84 mg/kg | [153] | |
| New Zealand | Autumn 2007 | From 0.2 to 2.46 mg/kg | [155] | |
| Malaysia | From January 2013 to March 2014 | From 1.25 to 4.56 mg/kg | [144] | |
| Brazil | From July 2007 to March 2009 | From 0.07 to 1.85 mg/kg | [146] | |
| Palestine | Between April and August 2009 | From 2.06 to 8.36 mg/kg | [154] | |
| Malaysia | between July 2010 and August 2011 | From 4.70 to 173.77 mg/kg | [162] | |
| China | - | From 0.59 to 22.85 mg/kg | [152] | |
| Poland | 2004–2005 | From 0.30 to 8.40 mg/kg | [143] | |
| Egypt | Cotton season 2011 | From 1.63 to 2.57 mg/kg | [142] | |
| Ethiopia | - | From 0.370 to 1.124 mg/kg | [150] | |
| Kenya | - | From 0.05 to 0.35 mg/kg | [147,151] | |
| Cuba | - | From 0.20 to 1.71 mg/kg | [141] | |
| Mexico | -- | From 1.51 to 6.80 mg/kg | [148] | |
| Royal jelly | Germany, | 2017 | From 18.1 to 19.7 mg/kg | [120] |
| Lithuania | 2018 | 24.1 mg/kg | [120] | |
| France and china | May, June, and July 2001 | From 19.4 to 24.8 mg/kg | [156] | |
| China | Between September and October 2014 | From 17.56 to 24.91 mg/kg | [157] | |
| China | - | From 20 to 26 mg/kg | [158] |
6.1.2. Role of Zinc as Adjuvant Therapy in the Management of COVID-19: A Database of Clinical Trials
As reported in Table 2, zinc has been the subject of numerous clinical trial studies. Data were incomplete, and in most clinical investigations the results are not available or are still pending. Functional micronutrients are essential elements for the proper functioning of the immune system and play crucial roles in supporting health and nutritional well-being. To date, the Food Safety Authority (FSA) has authorized and recommended several health claims referring to the involvement of certain critical nutrients (vitamins B6, B9, B12, A, D, C, and Cu, Fe, Se) in the proper functioning of the immune system. Vitamins C D, E; Zn, and Se have been widely investigated as a promising way to boost the immune system and fight COVID-19 disease [163]. The database of clinical trials on zinc integration in COVID-19 treatment has been analyzed to better understand the benefit and drawbacks of various therapy regimes. As of 10 February 2022, 7479 clinical research studies have been registered in 220 countries, in which 69 studies have investigated the involvement of Zn against COVID-19 infection (available online at https://clinicaltrials.gov/ct2/home, accessed on 10 February 2022). Numerous preventive clinical studies have been designed to evaluate the prophylactic effect of zinc associated with hydroxychloroquine, ivermectin, and dietary supplement (vitamin A, B12, C, D3; copper and selenium). Among these studies, 3 studies have evaluated the combination of zinc and other functional micronutrients supplement (Table 2). The NCT04551339 trial focused on the association of vitamin E, vitamin C, copper, and beta-carotene in boosting the immune health to fight the COVID-19 pandemic. Beta-carotene, vitamin E, and vitamin C are known as antioxidant components with beneficial immunomodulatory actions [164,165]. In addition to zinc, these micronutrients modulate the immune response and prevent COVID-19 complications through one or multiple mechanisms of action. For instance, vitamin C, a water-soluble vitamin contains in many functional foods including beehive products, plays a crucial role as a co-factor and a modulator of numerous immune system signaling pathways. In a randomized clinical trial study, Bing et al. [166] reported that 56 hospitalized COVID-19 pneumonia patients treated with a high dose of vitamin C, 12 g/50 mL every 12 h for 7 days, 12 mL/h expressed lower levels in IL-6, and a rise in the PaO2/FiO2 (229 vs. 151 mmHg) as well as significantly improving the intensive care unit (IUC) mortality of severe patients with organ failure assessment score, SOFA score ≥ 3.

Table 2.
Zinc as adjuvant therapy in the management of COVID-19: clinical trials.
The combination of micro-antioxidant nutrients as a safe and economic intervention in the treatment/management of COVID-19 has already been documented. In a recent study, Atousa et al. [167] reported that a daily administration of vitamin C (1000 mg), vitamin E (400 IU), and the national treatment regime (hydroxychloroquine) to the adults hospitalized COVID-19 patients during the hospitalization period until hospital discharge or intensive care unit (ICU) improved the clinical signs and decreases the severity of the disease. However, this finding did not reach statistical significance. Furthermore, the NCT04468139 trial combined quercetin (500 mg), bromelain (500 mg), vitamin C (1000 mg), and zinc (50 mg) as quadruple therapy for COVID-19 patients. Quercetin, a flavonol component highly present in agro-food byproducts, has a long history as a powerful antioxidant molecule in preventing and combating the oxidative damages of several pro-oxidant agents [168]. More importantly, previous clinical trials (NCT04578158, NCT04377789, NCT04861298, and NCT04861298) have shown the importance of quercetin supplementation as a preventive or a therapeutic tool for COVID-19 treatment.
The use of zinc as an active supplement or/and adjuvant treatment was recently adopted as a management strategy of the COVID-19 outbreak and its serious complications. NCT04446104, NCT04384458, and NCT04395768 are preventive clinical trials, evaluating ivermectin, hydroxychloroquine, and/or vitamin supplements in combination with zinc as a prophylactic approach for healthcare workers at high-risk and the general public. In addition to anti malarian action, hydroxychloroquine has been documented as having various clinical effects including anti-autophagy, anti-inflammatory, and immunosuppressive activities [169]. Recently, both chloroquine and hydroxychloroquine have shown promising potential in clinical setups to fight COVID-19 and its related complications. Owing to these properties and taking into consideration the multifunctioning role of zin in the human body, the combination of zinc, antioxidant nutrients, and hydroxychloroquine has been promoted as a COVID-19 treatment and prevention medication [170,171]. Interestingly, hydroxychloroquine/chloroquine act as zinc ionophores, increasing the intracellular concentration of zinc and thus, enhancing the suppression of SARS-CoV-2 RNA-dependent-RNA polymerase [172,173]. NCT00944359, NCT04482686, and NCT04447534 trials aim to discover a better COVID-19 therapy option by combining antiviral drugs/dietary supplements with zinc. In a retrospective observational study, the combination of zinc sulfate with hydroxychloroquine and azithromycin act synergistically and significantly decrease the mortality, the likelihood of being discharge to a home, as well as reducing the need for invasive ventilation or an intensive care unit of COVID-19 patients when compared to the conventional therapy (hydroxychloroquine alone or associated with azithromycin) [174]. Moreover, a 2-center, retrospective study on critically ill COVID-19 patients documented that the incorporation of zinc as adjunctive therapy was associated with a lower odds of acute kidney injury development during ICU stay as a serious complication of SARS-CoV-2 infection [175]. On the contrary, Szarpak et al. [176] have shown that zinc supplementation did not have any beneficial impact on ICU lengths stay.
The common denominator among these clinical trials is the incorporation of zinc as a valuable micronutrient either in the prevention or treatment of COVID-19 in virtue of its antiviral, anti-inflammatory and antioxidant properties [177,178]. Based on its anti-inflammatory properties, zinc improves the severity of SARS-CoV-2 by down-regulating the NF-κB signaling pathway, a key stimulator of pro-inflammatory cytokines, and thus, boost the IFN-mediated antiviral effects [179].
Acting synergistically, several bioactive molecules, especially phenolic components, antioxidant nutrients, and some anti-viral drugs may be effective in reducing COVID-19 symptoms or preventing its progression.
6.2. Polyphenols
6.2.1. Phenolic Compounds in Bee Products
Polyphenols or phenolic compounds are a heterogeneous class of chemical compounds belonging to secondary metabolites of plants; they are composed mainly of phenolic acids, and flavonoids (flavonols, flavones, flavanols, flavanones, anthocyanidin, chalcones, and isoflavones) [80,180,181].
The phenolic composition of bee products mainly depends on their floral origin [182]. The quantification of phenolic compounds in bee products from some countries is presented in Table 3. It was found that the most common polyphenols that existed in honey are flavonoids and acid phenolic compounds. The flavonoids include apigenin, catechin, chrysin, galangin, genistein, isorhamnetin, kaempferol, luteolin, myricetin, pinobanksin, pinocembrin, quercetin, and rutin. The common phenolic acids in honey are 2-cis,4-trans abscisic acid, 2-hydroxycinnamic acid, caffeic acid, chlorogenic acid, cinnamic acid, ellagic acid, ferulic acid, gallic acid, p-coumaric acid, p-hydroxybenzoic acid, protocatechuic acid, sinapic acid, syringic acid, and vanillic acid [80]. Whereas in propolis, the phenolic compounds were divided into phenolic acids derivatives, flavones, flavonols, flavanones, and dihydroflavonols. Additionally, Brazilian propolis is characterized by the presence of chrysin, pinocembrin, galangin, caffeic acid phenylethyl ester (CAPE), pinobanksin-3-o-acetate, and artepillin C [183].
Phenolic compounds that existed in bee pollen are as follows: gallic acid, protocatechuic acid, caffeic acid, ferulic acid, chlorogenic acid, para-coumaric acid, ortho-coumaric acid, luteolin, apigenin, chrysin, quercetin, rutin (Q 3-o-rutoside), kaempferol, myricetin, galangin, naringenin, pinocembrin, genistein [184]. Concerning bee venom, many biological properties including antiviral and antioxidant activities are attributed to melittin, a major peptide component ofbeevenom [185,186].

Table 3.
Phenolic compounds in bee products.
Table 3.
Phenolic compounds in bee products.
| Bee Products | Country | Collection Period | Content in Individual Polyphenols (mg/kg) | Reference |
|---|---|---|---|---|
| Propolis | Morocco | From the first of May to mid-June 2018 | Catechin (9.6 ± 1.17); vanilic acid (5.6 ± 0.90); p-coumaric acid + epicatechin (ranged from 5.4 ± 0.21 to 190.5 ± 42.00); o-coumaric acid (ranged from 4.1 ± 0.10 to 180.2 ± 0.54); ferulic acid (ranged from 8.3 ± 0.02 to 31.0 ± 4.05); ellagic acid (ranged from 6.5 ± 0.19 to 134.8 ± 19.35); naringin (ranged between 7.6 ± 0.89 and 68.10 ± 7.81); hesperidin (ranged between 7.2 ± 1.28 and 67.2 ± 6.26); apigenin (ranged between 7.1 ± 0.12 and 262.8 ± 40.03); cinnamic acid (ranged between 0.9 ± 0.07 and 34.2 ± 3.54); resveratrol (ranged between 9.9 ± 0.04 and 38.7 ± 9.24); rosmarinic acid (ranged between 13.0 ± 0.12 and 65.6 ± 14.72); rutin (ranged between 3.7 ± 0.88 and 160.6 ± 03.85); chlorogenic acid (ranged between 8.8 ± 0.01 and 32.0 ± 7.23); quercetin (ranged between 7.1 ± 0.19 and 26.7 ± 0.05); kaempferol (ranged between 5.1 ± 0.94 and 303.2 ± 21.15) | [55] |
| Italy | Not mentioned | Chrysin (781.5 ± 80.1); Apigenin (132.1 ± 21.6); Acacetin (1133.3 ± 256.2); Tectochrysin (130.9 ± 21.6); Pinocembrin (769.4 ± 77.9); Pinostrobin (575.6 ± 48.6); Sakuranetin (152.9 ± 20.6); Galangin (70.4 ± 11.8); Kaempferide (39.8 ± 3.6); Quercetin (153.5 ± 18.6); Prenyl caffeate (33.3 ± 2.6); Benzyl caffeate (527.1 ± 61.8); caffeic acid phenylethyl ester (1745.2 ± 245.2) | [187] | |
| China | Not mentioned | Chrysin (2333.0 ± 350.0); Apigenin (178.6 ± 34.8); Acacetin (1578.0 ± 141.9); Tectochrysin (238.3 ± 24.6); Pinocembrin (2087.5 ± 347.0); Sakuranetin (146.0 ± 18.4); Galangin (1400.3 ± 126.6); Kaempferide (38.8 ± 5.0); Quercetin (70.9 ± 9.7); Prenyl caffeate (56.2 ± 6.0); Benzyl caffeate (1477.0 ± 116.6); caffeic acid phenylethyl ester (2525.0 ± 199.3) | [187] | |
| Argentina | Not mentioned | Chrysin (2347.6 ± 215.7); Apigenin (336.9 ± 41.7); Acacetin (831.5 ± 16.0); Tectochrysin (224.7 ± 29.0); Pinocembrin (3362.5 ± 418.8); Sakuranetin (27.5 ± 4.1); Galangin (2253.7 ± 294.4); Kaempferide (38.1 ± 4.6); Prenyl caffeate (29.7 ± 4.2); Benzyl caffeate (1180.1 ± 200.8); caffeic acid phenylethyl ester (1111.6 ± 125.6) | [187] | |
| Ukraine | Not mentioned | Chrysin (922.0 ± 111.2); Apigenin (177.4 ± 15.2); Acacetin (658.9 ± 67.0); Tectochrysin (153.6 ± 18.7); Pinocembrin (1196.5 ± 91.9); Pinostrobin (1479.3 ± 303.5); Sakuranetin (2184.0 ± 196.1); Galangin (952.9 ± 106.8); Kaempferide (91.9 ± 13.7); Quercetin (28.9 ± 4.1); Prenyl caffeate (53.9 ± 6.1); Benzyl caffeate (465.1 ± 31.9); caffeic acid phenylethyl ester (1145.9 ± 98.6) | [187] | |
| Macedonia | Not mentioned | Chrysin (1649.8 ± 177.5); Apigenin (236.4 ± 34.1); Acacetin (1343.0 ± 200.2); Tectochrysin (987.1 ± 104.0); Pinocembrin (2112.0 ± 184.5); Pinostrobin (3816.0 ± 397.1); Sakuranetin (2203.4 ± 269.0); Galangin (903.9 ± 88.2); Kaempferide (43.2 ± 7.0); Quercetin (94.8 ± 10.3); Benzyl caffeate (400.6 ± 62.6); caffeic acid phenylethyl ester (1263.1 ± 212.6) | [187] | |
| Morocco | May 2018 | Ferrulic acid (40.60 ± 0.6); o-Coumaric acid (35.47 ± 0.2); Chlorogenic acid (25.31 ± 0.0); Rosmarinic acid (222.02 ± 6.2); Vanilic acid (10.58 ± 0.1); Ellagic acid (37.94 ± 0.1); Catechin (18.83 ± 0.1); Naringin (290.19 ± 0.2); Hesperidin (271.77 ± 0.0); Quercetin (14.78 ± 0.2); Apigenin (50.37 ± 0.8); Kaempferol (26.48 ± 1.2); Rutin (34.37 ± 1.3); Resveratrol (86.25 ± 0.2) | [54] | |
| Morocco | July 2018 | Vanillic acid (8.61 ± 0.30); o-Coumaric acid (11.44 ± 4.63); Ferulic acid (18.84 ± 0.21); Ellagic acid (28.55 ± 1.99); Naringin (35.78 ± 4.10); Hesperidin (417.18 ± 50.0); Apigenin (38.39 ± 2.60); Resveratrol (116.89 ± 12.7); Rosmarinic acid (470.35 ± 52.00); Rutin (12.40 ± 0.42); Chlorogenic acid (16.11 ± 0.12); Quercetin (12.02 ± 0.13); Kaempferol (21.90 ± 1.60) | [56] | |
| Bee bread | Morocco | Not mentioned | Kaempferol- O-hexosyl-O-rutinoside (570 ± 10); Quercetin-O-hexosyl-O-hexoside (950 ± 30); Methylherbacetrin-O-dihexoside (545 ± 4); isorhamnetin-O-hexosyl-O-rutinoside (1480 ± 50); Quercetin-O-pentosyl-hexoside (580 ± 10); Quercetin 3-O-rutinoside (530 ± 10); methylherbacetrin-3-O-rutinoside (510 ± 10); isorhamnetin-O-pentosyl-hexoside (930 ± 10); kaempferol-3-O-rutinoside (510 ± 10); isorhamnetin-O-rhamnoside-hexoside (560 ± 10) | [117] |
| Romania | spring of 2020 | kaempferol (31.25), myricetin (3.15), luteolin (1.17), rosmarinic acid (0.23), Caffeic acid (0.10), p-Coumaric acid (0.11), Quercetin (0.06) | [188] | |
| North-East European countries | 2015 | Gallic Acid (300); Caffeic Acid (between 700 to 6400); Catechin (between 900 and 52,100); Clorogenic acid (between 800 to 1400); p-Coumaric acid (between 2300 and 11,400); Ferulic acid (between 400 and 1100); Naringenin +Quercetin (between 400 and 3200): Apigenin +Kaempferol (between 600 and 15,800); Pinocembrin (between 400 and 56,600); CAPE +Galangin (between 2400 and 71,900) | [189] | |
| South-West European countries | 2015 | Caffeic acid (between 4600 to 6600); Catechin (between 1700 and 6300); Clorogenic acid (between 400 to 7300); p-Coumaric acid (between 2000 and 12,200); Ferulic acid (between 800 and 2900); Naringenin +Quercetin (between 300 and 1000); Apigenin +Kaempferol (between 4000 and 32,200); Pinocembrin (between 13700 and 33,900); CAPE +Galangin (between 1300 and 110,600) | [189] | |
| South American tropical zone | 2015 | Gallic acid (300); Catechin (between 20800 to 34,100); Clorogenic acid (200); p-Coumaric acid (between 1200 and 2800); Ferulic acid (between 300 and 800); Naringenin +Quercetin (between 500 and 700); Apigenin +Kaempferol (between 1500 and 6500); Pinocembrin (33,300); CAPE +Galangin (between 7600 and 9000) | [189] | |
| Bee pollen | Morocco | May 2018 | Ferrulic acid (17.17 ± 0.4); cinnamic acid (46.01 ± 7.8); o-Coumaric acid (27.10 ± 1.9); Rosmarinic acid (127.30 ± 6.2); Gallic acid (32.54 ± 2.2); Vanilic acid (6.13 ± 0.1); Ellagic acid (13.02 ± 0.0); Naringin (113.71 ± 6.8); Hesperidin (15.63 ± 6.8); Quercetin (48.12 ± 2.8); Apigenin (162.85 ± 17.7); Rutin (95.36 ± 3.7); Resveratrol (44.00 ± 0.4) | [54] |
| Turkey | 2007–2008 | Gallic acid (from 9.46 to 18.59); Protocatechuic acid (from 4.73 to 19.77); p-OH benzoic acid (from 2.74 to 122.68); Chlorogenic acid (from 14.64 to 75.08); Vanillic acid (from 22.96 to 87.02); Caffeic acid (from 10.88 to 98.03); Syringic acid (from 10.55 to 259.53); Epicatechin (from 39.15 to 520.02); p-Coumaric acid (from 34.16 to 127.85); Ferulic acid (from 36.83 to 230.55); Benzoic acid (from 46.87 to 1077.64); Rutin (from 25.59 to 692.85); o-Coumaric acid (from 2.63 to 42.23); Abscisic acid (from 21.04 to 288.70); tert-Cinnamic acid (from 6.82 to 56.38); Quercetin (from 61.40 to 499.20) | [190] | |
| Chile | Not mentioned | Feluric acid (7.75 ± 0.39); Syringic acid (7.92 ± 0.40); p-coumaric acid (52.17 ± 2.60); Rutin (86.60 ± 4.30); Luteolin (28.37 ± 1.42); Cinnamic acid (5.77 ± 0.29); Quercetin (32.72 ± 1.64); Miricetin (6.76 ± 0.34) | [191] | |
| Honey | Morocco | July 2018 | Vanillic acid (2.90 ± 0.01); Ferulic acid (8.35 ± 0.01); Ellagic acid (5.09 ± 0.02); Cinnamic acid (4.25 ± 0.01); Chlorogenic acid (7.06 ± 0.11); Gallic acid (30.06 ± 0.23) | [56] |
| Chile | Not mentioned | Chlorogenic acid+caffeic acid (19.67 ± 0.98); Sinapic acid (from 17.58 to 23.86); Feluric acid (from 4.21 to 16.29); Syringic acid (4.73 ± 0.24); Luteolin (from 8.16 to 11.55); Cinnamic acid (3.00 ± 0.15); Quercetin (5.88 ± 0.29); Kaempherol (from 17.00 to 37.00) | [191] | |
| Hong Kong, Spain, Italy, Korea, China, Canada, Brazil, New Zealand, and Germany | Not mentioned | gallic acid (from 20 to 66); protocatechuic acid (from 7.1 to 63); 2,3,4-trihydroxybenzoic acid (from 11 to 28); protocatechualdehyde (from 7 to 63); p-hydroxybenzoic acid (from 8.1 to 21.7); vanillic acid (5.1); vanillin (from 4.1 to 22.7); syringic acid (from 1.1 to 87.7); caffeic acid (from 6.61 to 23.6); chlorogenic acid (from 11.4 to 21.2); p-coumaric acid (from 8.7 to 13.6); syringaldehyde (from 1.7 to 87.7); genistic acid (from 8.2 to 39.6) | [192] | |
| Morocco | Not mentioned | Methyl syringate (from 277.93 to 443.89); Epicatechin (from 30.67 to 179.29); Syringic acid (from 25.16 to 105.86); Catechin (from 14.56 to 66.13); 4-coumaric acid (from 5.13 to 49.43); Gallic acid (from 0.00 to 34.40); Quercetin (from 7.53 to 42.77); Apigenin (from 1.25 to 33.38); Luteolin (from 0.00 to 22.08); Kaempferol (from 5.24 to 19.64); Naringenin (from 0.00 to 42.41); Formononetin (from 0.87 to 17.88); Genistein (from 0.00 to 24.00); 3-coumaric acid (from 2.40 to 8.66); Daidzein + Pelargonidin (from 1.84 to 8.16); 2-coumaric acid (from 0.45 to 8.17); Biochanin A (from 0.86 to 4.10); Cyanidin (from 0.00 to 2.30) | [193] |
6.2.2. Role of Polyphenols in the Management of COVID-19
Inflammation is a major problem caused after the binding of SARS-CoV-2 to the ACE2 receptor of the host cell through spike protein and the activation of transmembrane protease serine 2 (TMPRSS2). After viral endocytosis, RAC/CDC42-activated kinase 1 (PAK1) and chemokine (C-C motif) ligand 2 (CCL2) were stimulated, reducing the production of antibodies and inducing a fibrotic process. These intracellular signals lead to the activation of nuclear transcription factor κB(NF-κB)which causes local inflammation, tissue damage, and the appearance of complications (Figure 3) [194].
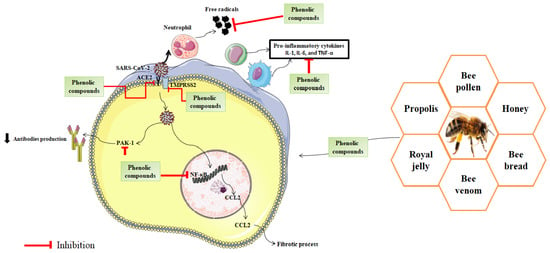
Figure 3.
Possible mechanism of action of phenolic compounds in the management of COVID-19.
Meanwhile, there is evidence that viral infections are associated with an increase in reactive oxygen species (ROS) levels and a decrease in antioxidant defenses (Figure 3). Exposure to SARS-CoV-2 leads to the inhibition of NRF2-mediated pathways and neutrophilia, which causes deleterious effects on pulmonary cells leading to hypoxic respiratory failure and the complications observed in severe COVID-19 cases [195]. Furthermore, oxidative stress leads to protein oxidation, lipid peroxidation, and DNA damage, these damages induce the release of inflammatory signals [196].
Polyphenols are natural compounds well known for their antioxidant and anti-inflammatory effects. The antioxidant activity of polyphenols is related to their capacity to react with ROS using different reaction pathways such as the inhibition of the enzymes responsible for ROS production, the up-regulation of endogenous antioxidant defenses, or scavenging reactive oxygen species [197].
It seems that the main pathways, by which polyphenols-rich bee products can attenuate SARS-CoV-2 infection, are the modulation of the immune system, the prevention of inflammatory responses, and the reduction in oxidative stress (Figure 3). It was reported that phenolic compounds modulate enzymatic and signaling pathways involved in the inflammation. For instance, it was reported that quercetin is an effective inhibitor of NF-κB, TNF-α, NO, and PLA2 pathways. Resveratrol exerted an anti-inflammatory effect by inhibiting NF-κB and TPA-induced COX-2 expression. Similarly, caffeic acid phenethyl ester (CAPE) inhibits inflammatory reaction via the reduction of NF-κB [198].
Recently, numerous published reports revealed that phenolic compounds found in bee products can react with SARS-CoV-2 and blocks its entry into human cells (Figure 3 and Table 4). It was found in a study published by Sahlan et al. that glyasperin A and broussoflavonol F, Sulawesi propolis compounds, have favorable interaction profiles with SARS-CoV-2 main protease (PDB ID 6Y2F) catalytic sites (His41 and Cys145) with binding similarities of 75% and 63%, respectively, compared to potent inhibitors [199]. Similarly, caffeic acid phenethyl ester can bind to the substrate-binding pocket of SARS-CoV-2 Mpro with efficacy and binding energies equivalent to an already claimed N3 protease inhibitor [200].

Table 4.
Efficacy of flavonoids in vitro and in silico against SARS-CoV-2.
In addition, the molecular docking of ten flavonoid compounds: apigenin, chrysin, fisetin, galangin, hesperitin, luteolin, morin, naringin, quercetin, revealed that all of the flavonoids studied have a high binding affinity with the active site of the spike protein of SARS-CoV-2 [201].
The antiviral effect of 6 compounds present in honey and propolis (3-phenyllactic acid, caffeic acid phenethyl ester, caffeic acid, chrysin, galangin, lumichrome) was studied in silico. The results showed that four compounds (caffeic acid phenethyl ester, caffeic acid, chrysin, galangin) had a strong binding affinity with a good glide score and may inhibit the COVID-19 Mpro and replication of the virus [202].
In a study conducted by Vijayakumar et al. [203], the molecular docking of natural flavonoids against essential proteins of SARS-CoV-2 (RNA dependent RNA polymerase (rdrp), main protease (Mpro) and Spike (S) protein) revealed that cyanidin may suppress rdrp by binding at asp761 catalytic residue and halting the viral replication process. In addition, the following flavonoids can interact on the spike proteins’ key rbd and inhibit the spread to receptors and thus limit viral spread: daidzein, eriodictyol, fisetin, genistein, kaempferol, myricetin, quercetin, arbutin, chalconaringenin, phloretin, and liquiritin.
A total of 220 phenolic compounds were tested in a study published by Pitsillou et al. The results of in silico and in vitro using an enzymatic inhibition assay indicated that hypericin, rutin, and cyanidin-3-O-glucoside can be considered lead compounds in the inhibition of SARS-CoV-2 papain-like protease (PLpro) [204].
In the same vein, docking studies of rutin, caffeic acid phenethyl ester, quercetin, kaempferol, pinocembrin, pinobanksin, galangin, chrysin, p-cumaric acid, and benzoic acid revealed that rutin and caffeic acid phenethyl ester have the highest affinity to COVID-19 3CL-protease and S1 Spike [69] (Table 4).
Interestingly, several clinical trials have been conducted to test the beneficial effect of polyphenols against SARS-CoV-2 infection. For instance, the NCT04666753 trial aims to describe the effect of the immunomodulation treatment (60 mg of zinc orotate, 96 μg of selenium, 20,000 IU of cholecalciferol, 300 mg of ascorbic acid, 480 mg of ferulic acid, 90 mg of resveratrol on COVID-19 patients (adults and older adults). Antioxidant compounds and other food micronutrients with valuable additional functionalities are important in resolving other COVID-19-related issues. For instance, human trial studies documented that ferulic acid and resveratrol have strong antidiabetic, cardioprotective, and renoprotective effects [205,206]. Thus, these components could be proposed as adjuvant active molecules and novel dietary approaches for the management of COVID-19 complications.
Furthermore, as of 10 February 2022, quercetin has been approved in 14 clinical trials for profylaxis and managing COVID-19 symptoms (available online at https://clinicaltrials.gov/ct2/home, accessed on 10 February 2022). For instance, the NCT04578158 trial, a randomized, open-labeled, and controlled study, investigates the adjuvant benefits of quercetin Phytosome (400 mg/day, orally for 30 days) in community-based subjects with confirmed SARS-CoV-2 infection. In addition to quercetin, resveratrol, a stilbenoid that highly presents in bee products, has been the object of 4 clinical trials (NCT04400890, NCT04799743, NCT04542993, and NCT04666753 trials). The NCT04400890 trial aims to evaluate the safety and explore the effectiveness of resveratrol treatment (1000 mg, 4 times a day, for 15 days) against COVID-19 infection. Published data support that resveratrol inhibits coronavirus replication through the down-regulation of mRNA and nucleocapsid protein expressions of SARS-CoV-2 [207,208].
7. Conclusions
In the absence of specific antiviral drugs against SARS-CoV-2, natural remedies such as apitherapy could alleviate the complications associated with COVID-19. Considering the crucial role of the immune system in fighting SARS-CoV-2 infection, boosting immunity was highly recommended. In this direction, the present review highlights and provides an overview of zinc and phenolic compounds found in bee products and their direct and indirect actions on the immune system in fighting against this emergent public health crisis. The problems which arise are that the nature, quality, and quantity of these bioactive molecules in bee products differ from one country to another. To overcome this major drawback, an international norm, ISO/TC 34/SC 19, is currently in progress to standardize the whole process and circulation of bee products.
Author Contributions
Conceptualization, M.B., H.L., D.O. and B.L.; writing—original draft preparation, M.B., H.L., D.O. and A.E.G.; writing—review and editing, H.M., I.E.-s. and B.L.; supervision, B.L. All authors have read and agreed to the published version of the manuscript.
Funding
This study was partially funded by the SNAMOPEQ laboratory, FSDM, USMBA, Fez, Morocco.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available upon request.
Acknowledgments
Open access funding provided by University of Helsinki.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mütze, T.; Friede, T. Data Monitoring Committees for Clinical Trials Evaluating Treatments of COVID-19. Contemp. Clin. Trials 2020, 98, 106154. [Google Scholar] [CrossRef] [PubMed]
- Ather, A.; Patel, B.; Ruparel, N.B.; Diogenes, A.; Hargreaves, K.M. Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care. J. Endod. 2020, 46, 584–595. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Rational Use of Personal Protective Equipment (PPE) for Coronavirus Disease (COVID-19): Interim Guidance, 19 March 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Mullol, J.; Alobid, I.; Mariño-Sánchez, F.; Izquierdo-Domínguez, A.; Marin, C.; Klimek, L.; Wang, D.-Y.; Liu, Z. The Loss of Smell and Taste in the COVID-19 Outbreak: A Tale of Many Countries. Curr. Allergy Asthma Rep. 2020, 20, 61. [Google Scholar] [CrossRef]
- Muralidar, S.; Ambi, S.V.; Sekaran, S.; Krishnan, U.M. The Emergence of COVID-19 as a Global Pandemic: Understanding the Epidemiology, Immune Response and Potential Therapeutic Targets of SARS-CoV-2. Biochimie 2020, 179, 85–100. [Google Scholar] [CrossRef] [PubMed]
- Samaee, H.; Mohsenzadegan, M.; Ala, S.; Maroufi, S.S.; Moradimajd, P. Tocilizumab for Treatment Patients with COVID-19: Recommended Medication for Novel Disease. Int. Immunopharmacol. 2020, 89, 107018. [Google Scholar] [CrossRef]
- Yavuz, S.; Çelikyurt, F.I.K. An Update of Anti-Viral Treatment of COVID-19. Turk. J. Med. Sci. 2021, 51, 3372–3390. [Google Scholar] [CrossRef]
- Drożdżal, S.; Rosik, J.; Lechowicz, K.; Machaj, F.; Szostak, B.; Przybyciński, J.; Lorzadeh, S.; Kotfis, K.; Ghavami, S.; Łos, M.J. An Update on Drugs with Therapeutic Potential for SARS-CoV-2 (COVID-19) Treatment. Drug Resist. Updat. 2021, 59, 100794. [Google Scholar] [CrossRef]
- Bolarin, J.A.; Oluwatoyosi, M.A.; Orege, J.I.; Ayeni, E.A.; Ibrahim, Y.A.; Adeyemi, S.B.; Tiamiyu, B.B.; Gbadegesin, L.A.; Akinyemi, T.O.; Odoh, C.K. Therapeutic Drugs for SARS-CoV-2 Treatment: Current State and Perspective. Int. Immunopharmacol. 2021, 90, 107228. [Google Scholar] [CrossRef]
- Heskin, J.; Pallett, S.J.; Mughal, N.; Davies, G.W.; Moore, L.S.; Rayment, M.; Jones, R. Caution Required with Use of Ritonavir-Boosted PF-07321332 in COVID-19 Management. Lancet 2022, 399, 21–22. [Google Scholar] [CrossRef]
- Parums, D.V. Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Patients. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2022, 28, e935952. [Google Scholar] [CrossRef]
- Lima, W.G.; Brito, J.C.; da Cruz Nizer, W.S. Bee Products as a Source of Promising Therapeutic and Chemoprophylaxis Strategies against COVID-19 (SARS-CoV-2). Phytother. Res. 2021, 35, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Elmahallawy, E.K.; Mohamed, Y.; Abdo, W.; El-Gohary, F.A.; Ahmed Awad Ali, S.; Yanai, T. New Insights into Potential Benefits of Bioactive Compounds of Bee Products on COVID-19: A Review and Assessment of Recent Research. Front. Mol. Biosci. 2021, 7, 513. [Google Scholar] [CrossRef] [PubMed]
- Tantawy, M. Efficacy of Natural Honey Treatment in Patients with Novel Coronavirus. Clinicaltrials.Gov. 2020. Available online: https://clinicaltrials.gov/ct2/show/NCT04323345 (accessed on 11 February 2022).
- Silveira, M.A.D.; De Jong, D.; Berretta, A.A.; Galvão, E.B.D.S.; Ribeiro, J.C.; Cerqueira-Silva, T.; Amorim, T.C.; Conceição, L.F.M.R.D.; Gomes, M.M.D.; Teixeira, M.B.; et al. Efficacy of Brazilian Green Propolis (EPP-AF®) as an Adjunct Treatment for Hospitalized COVID-19 Patients: A Randomized, Controlled Clinical Trial. Biomed. Pharmacother. 2021, 138, 111526. [Google Scholar] [CrossRef] [PubMed]
- Hoebe, K.; Janssen, E.; Beutler, B. The Interface between Innate and Adaptive Immunity. Nat. Immunol. 2004, 5, 971–974. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, M.A.; Hossain, N.; Kashem, M.A.; Shahid, M.A.; Alam, A. Immune Response in COVID-19: A Review. J. Infect. Public Health 2020, 13, 1619–1629. [Google Scholar] [CrossRef] [PubMed]
- Dosch, S.F.; Mahajan, S.D.; Collins, A.R. SARS Coronavirus Spike Protein-Induced Innate Immune Response Occurs via Activation of the NF-KappaB Pathway in Human Monocyte Macrophages in Vitro. Virus Res. 2009, 142, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Yen, Y.-T.; Singh, S.; Kao, C.-L.; Wu-Hsieh, B.A. SARS-CoV Regulates Immune Function-Related Gene Expression in Human Monocytic Cells. Viral Immunol. 2012, 25, 277–288. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.-M.A.; Liang, S.-Y.; Shih, Y.-P.; Chen, C.-Y.; Lee, Y.-M.; Chang, L.; Jung, S.-Y.; Ho, M.-S.; Liang, K.-Y.; Chen, H.-Y.; et al. Epidemiological and Genetic Correlates of Severe Acute Respiratory Syndrome Coronavirus Infection in the Hospital with the Highest Nosocomial Infection Rate in Taiwan in 2003. J. Clin. Microbiol. 2006, 44, 359–365. [Google Scholar] [CrossRef] [Green Version]
- Kaiko, G.E.; Horvat, J.C.; Beagley, K.W.; Hansbro, P.M. Immunological Decision-Making: How Does the Immune System Decide to Mount a Helper T-Cell Response? Immunology 2008, 123, 326–338. [Google Scholar] [CrossRef]
- Anaya, J.-M.; Shoenfeld, Y.; Rojas-Villarraga, A.; Levy, R.A.; Cervera, R. Autoimmunity: From Bench to Bedside; El Rosario University Press: Bogota, Colombia, 2013; ISBN 958-738-366-4. [Google Scholar]
- Paul, W.E.; Zhu, J. How Are T(H)2-Type Immune Responses Initiated and Amplified? Nat. Rev. Immunol. 2010, 10, 225–235. [Google Scholar] [CrossRef]
- Stockinger, B.; Bourgeois, C.; Kassiotis, G. CD4+ Memory T Cells: Functional Differentiation and Homeostasis. Immunol. Rev. 2006, 211, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.-Y.; Huang, Z.-T.; Li, L.; Wu, M.-H.; Yu, T.; Koup, R.A.; Bailer, R.T.; Wu, C.-Y. Characterization of SARS-CoV-Specific Memory T Cells from Recovered Individuals 4 Years after Infection. Arch. Virol. 2009, 154, 1093–1099. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, L.; Ren, L.; Yang, S.; Xiao, M.; Chang, D.; Yang, F.; Dela Cruz, C.S.; Wang, Y.; Wu, C.; Xiao, Y.; et al. Profiling Early Humoral Response to Diagnose Novel Coronavirus Disease (COVID-19). Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020, 71, 778–785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Röltgen, K.; Powell, A.E.; Wirz, O.F.; Stevens, B.A.; Hogan, C.A.; Najeeb, J.; Hunter, M.; Wang, H.; Sahoo, M.K.; Huang, C.; et al. Defining the Features and Duration of Antibody Responses to SARS-CoV-2 Infection Associated with Disease Severity and Outcome. Sci. Immunol. 2020, 5, eabe0240. [Google Scholar] [CrossRef]
- Shah, V.K.; Firmal, P.; Alam, A.; Ganguly, D.; Chattopadhyay, S. Overview of Immune Response during SARS-CoV-2 Infection: Lessons from the Past. Front. Immunol. 2020, 11, 1949. [Google Scholar] [CrossRef]
- Blanco-Melo, D.; Nilsson-Payant, B.E.; Liu, W.-C.; Uhl, S.; Hoagland, D.; Møller, R.; Jordan, T.X.; Oishi, K.; Panis, M.; Sachs, D. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell 2020, 181, 1036–1045. [Google Scholar] [CrossRef]
- Chiappelli, F.; Khakshooy, A.; Greenberg, G. COVID-19 Immunopathology and Immunotherapy. Bioinformation 2020, 16, 219. [Google Scholar] [CrossRef]
- Stefanidou, M.; Maravelias, C.; Dona, A.; Spiliopoulou, C. Zinc: A Multipurpose Trace Element. Arch. Toxicol. 2005, 80, 1. [Google Scholar] [CrossRef]
- Ishida, T. Anti-Viral Vaccine Activity of Zinc (II) for Viral Prevention, Entry, Replication, and Spreading during Pathogenesis Process. Curr. Trends Biomed. Eng. Biosci. 2019, 19, 6. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Feng, H.-L.; Jeng, S.-S. Zinc Supplementation Stimulates Red Blood Cell Formation in Rats. Int. J. Mol. Sci. 2018, 19, 2824. [Google Scholar] [CrossRef] [Green Version]
- Haboubi, N.Y.; Baker, M.A.; Gyde, O.H.; Small, N.A.; Haboubi, N. Zinc Supplementation and Erythropoiesis in the Elderly. J. Clin. Pathol. 1988, 41, 706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhardwaj, P.; Dhawan, D.K. Zinc Treatment Modulates Hematological and Morphological Changes in Rat Erythrocytes Following Arsenic Exposure. Toxicol. Ind. Health 2019, 35, 593–603. [Google Scholar] [CrossRef] [PubMed]
- Barman, S.; Srinivasan, K. Zinc Supplementation Alleviates Hyperglycemia and Associated Metabolic Abnormalities in Streptozotocin-Induced Diabetic Rats. Can. J. Physiol. Pharmacol. 2016, 94, 1356–1365. [Google Scholar] [CrossRef]
- Baltaci, A.K.; Mogulkoc, R.; Baltaci, S.B. The Role of Zinc in the Endocrine System. Pak. J. Pharm. Sci. 2019, 32, 231–239. [Google Scholar]
- Ko, W.-S.; Guo, C.-H.; Hsu, G.-S.W.; Chiou, Y.-L.; Yeh, M.-S.; Yaun, S.-R. The Effect of Zinc Supplementation on the Treatment of Chronic Hepatitis C Patients with Interferon and Ribavirin. Clin. Biochem. 2005, 38, 614–620. [Google Scholar] [CrossRef] [PubMed]
- Maares, M.; Haase, H. Zinc and Immunity: An Essential Interrelation. Arch. Biochem. Biophys. 2016, 611, 58–65. [Google Scholar] [CrossRef]
- McPherson, S.W.; Keunen, J.E.; Bird, A.C.; Chew, E.Y.; van Kuijk, F.J. Investigate Oral Zinc as a Prophylactic Treatment for Those at Risk for COVID-19. Am. J. Ophthalmol. 2020, 216, A5–A6. [Google Scholar] [CrossRef] [PubMed]
- DiSilvestro, R.A.; Dardenne, M.; Joseph, E. Comparison of Thymulin Activity with Other Measures of Marginal Zinc Deficiency. Biol. Trace Elem. Res. 2020, 199, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Haddad, J.J. Thymulin and Zinc (Zn2+)-Mediated Inhibition of Endotoxin-Induced Production of Proinflammatory Cytokines and NF-ΚB Nuclear Translocation and Activation in the Alveolar Epithelium: Unraveling the Molecular Immunomodulatory, Anti-Inflammatory Effect of Thymulin/Zn2+ in Vitro. Mol. Immunol. 2009, 47, 205–214. [Google Scholar] [CrossRef]
- Nasseri, B.; Zaringhalam, J.; Daniali, S.; Manaheji, H.; Abbasnejad, Z.; Nazemian, V. Thymulin Treatment Attenuates Inflammatory Pain by Modulating Spinal Cellular and Molecular Signaling Pathways. Int. Immunopharmacol. 2019, 70, 225–234. [Google Scholar] [CrossRef]
- Prasad, A.S. Lessons Learned from Experimental Human Model of Zinc Deficiency. J. Immunol. Res. 2020, 2020, 9207279. [Google Scholar] [CrossRef] [PubMed]
- Baum, M.K.; Shor-Posner, G.; Campa, A. Zinc Status in Human Immunodeficiency Virus Infection. J. Nutr. 2000, 130, 1421S–1423S. [Google Scholar] [CrossRef] [PubMed]
- Suara, R.O.; Crowe, J.E. Effect of Zinc Salts on Respiratory Syncytial Virus Replication. Antimicrob. Agents Chemother. 2004, 48, 783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumura, H.; Nirei, K.; Nakamura, H.; Arakawa, Y.; Higuchi, T.; Hayashi, J.; Yamagami, H.; Matsuoka, S.; Ogawa, M.; Nakajima, N.; et al. Zinc Supplementation Therapy Improves the Outcome of Patients with Chronic Hepatitis C. J. Clin. Biochem. Nutr. 2012, 51, 178–184. [Google Scholar] [CrossRef] [Green Version]
- Yuasa, K.; Naganuma, A.; Sato, K.; Ikeda, M.; Kato, N.; Takagi, H.; Mori, M. Zinc Is a Negative Regulator of Hepatitis C Virus RNA Replication. Liver Int. 2006, 26, 1111–1118. [Google Scholar] [CrossRef]
- Kaushik, N.; Anang, S.; Ganti, K.P.; Surjit, M. Zinc: A Potential Antiviral against Hepatitis E Virus Infection? DNA Cell Biol. 2018, 37, 593–599. [Google Scholar] [CrossRef]
- Haraguchi, Y.; Sakurai, H.; Hussain, S.; Anner, B.M.; Hoshino, H. Inhibition of HIV-1 Infection by Zinc Group Metal Compounds. Antiviral Res. 1999, 43, 123–133. [Google Scholar] [CrossRef]
- Ragab, D.; Salah Eldin, H.; Taeimah, M.; Khattab, R.; Salem, R. The COVID-19 Cytokine Storm; What We Know So Far. Front. Immunol. 2020, 11, 1446. [Google Scholar] [CrossRef]
- Bao, B.; Prasad, A.S.; Beck, F.W.J.; Fitzgerald, J.T.; Snell, D.; Bao, G.W.; Singh, T.; Cardozo, L.J. Zinc Decreases C-Reactive Protein, Lipid Peroxidation, and Inflammatory Cytokines in Elderly Subjects: A Potential Implication of Zinc as an Atheroprotective Agent. Am. J. Clin. Nutr. 2010, 91, 1634–1641. [Google Scholar] [CrossRef] [Green Version]
- Haase, H.; Rink, L. Functional Significance of Zinc-Related Signaling Pathways in Immune Cells. Annu. Rev. Nutr. 2009, 29, 133–152. [Google Scholar] [CrossRef]
- Laaroussi, H.; Bakour, M.; Ousaaid, D.; Aboulghazi, A.; Ferreira-Santos, P.; Genisheva, Z.; Antonio Teixeira, J.; Lyoussi, B. Effect of Antioxidant-Rich Propolis and Bee Pollen Extracts against D-Glucose Induced Type 2 Diabetes in Rats. Food Res. Int. 2020, 138, 109802. [Google Scholar] [CrossRef] [PubMed]
- Laaroussi, H.; Ferreira-Santos, P.; Genisheva, Z.; Bakour, M.; Ousaaid, D.; Teixeira, J.A.; Lyoussi, B. Unraveling the Chemical Composition, Antioxidant, α-Amylase and α-Glucosidase Inhibition of Moroccan Propolis. Food Biosci. 2021, 42, 101160. [Google Scholar] [CrossRef]
- Laaroussi, H.; Bakour, M.; Ousaaid, D.; Ferreira-Santos, P.; Genisheva, Z.; El Ghouizi, A.; Aboulghazi, A.; Teixeira, J.A.; Lyoussi, B. Protective Effect of Honey and Propolis against Gentamicin-Induced Oxidative Stress and Hepatorenal Damages. Oxid. Med. Cell. Longev. 2021, 2021, 9719906. [Google Scholar] [CrossRef] [PubMed]
- Gekker, G.; Hu, S.; Spivak, M.; Lokensgard, J.R.; Peterson, P.K. Anti-HIV-1 Activity of Propolis in CD4+ Lymphocyte and Microglial Cell Cultures. J. Ethnopharmacol. 2005, 102, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Governa, P.; Cusi, M.G.; Borgonetti, V.; Sforcin, J.M.; Terrosi, C.; Baini, G.; Miraldi, E.; Biagi, M. Beyond the Biological Effect of a Chemically Characterized Poplar Propolis: Antibacterial and Antiviral Activity and Comparison with Flurbiprofen in Cytokines Release by LPS-Stimulated Human Mononuclear Cells. Biomedicines 2019, 7, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amoros, M.; Sauvager, F.; Girre, L.; Cormier, M. In Vitro Antiviral Activity of Propolis. Apidologie 1992, 23, 231–240. [Google Scholar] [CrossRef] [Green Version]
- Búfalo, M.; Figueiredo, A.; De Sousa, J.; Candeias, J.; Bastos, J.; Sforcin, J. Anti-poliovirus Activity of Baccharis Dracunculifolia and Propolis by Cell Viability Determination and Real-time PCR. J. Appl. Microbiol. 2009, 107, 1669–1680. [Google Scholar] [CrossRef]
- Bankova, V.; Galabov, A.; Antonova, D.; Vilhelmova, N.; Di Perri, B. Chemical Composition of Propolis Extract ACF® and Activity against Herpes Simplex Virus. Phytomedicine 2014, 21, 1432–1438. [Google Scholar] [CrossRef]
- Schnitzler, P.; Neuner, A.; Nolkemper, S.; Zundel, C.; Nowack, H.; Sensch, K.H.; Reichling, J. Antiviral Activity and Mode of Action of Propolis Extracts and Selected Compounds. Phytother. Res. 2010, 24, S20–S28. [Google Scholar] [CrossRef]
- Sartori, G.; Pesarico, A.P.; Pinton, S.; Dobrachinski, F.; Roman, S.S.; Pauletto, F.; Rodrigues, L.C.; Prigol, M. Protective Effect of Brown Brazilian Propolis against Acute Vaginal Lesions Caused by Herpes Simplex Virus Type 2 in Mice: Involvement of Antioxidant and Anti-inflammatory Mechanisms. Cell Biochem. Funct. 2012, 30, 1–10. [Google Scholar] [CrossRef]
- Mazia, R.S.; de Araújo Pereira, R.R.; de Francisco, L.M.B.; Natali, M.R.M.; Dias Filho, B.P.; Nakamura, C.V.; Bruschi, M.L.; Ueda-Nakamura, T. Formulation and Evaluation of a Mucoadhesive Thermoresponsive System Containing Brazilian Green Propolis for the Treatment of Lesions Caused by Herpes Simplex Type I. J. Pharm. Sci. 2016, 105, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Miryan, M.; Soleimani, D.; Dehghani, L.; Sohrabi, K.; Khorvash, F.; Bagherniya, M.; Sayedi, S.M.; Askari, G. The Effect of Propolis Supplementation on Clinical Symptoms in Patients with Coronavirus (COVID-19): A Structured Summary of a Study Protocol for a Randomised Controlled Trial. Trials 2020, 21, 996. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C.; Garzarella, E.U.; Bocchino, B.; D’Avino, M.; Caruso, G.; Buonomo, A.R.; Sacchi, R.; Galeotti, F.; Tenore, G.C.; Zaccaria, V. A Standardized Polyphenol Mixture Extracted from Poplar-Type Propolis for Remission of Symptoms of Uncomplicated Upper Respiratory Tract Infection (URTI): A Monocentric, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Phytomedicine 2021, 80, 153368. [Google Scholar] [CrossRef]
- Kosari, M.; Noureddini, M.; Khamechi, S.P.; Najafi, A.; Ghaderi, A.; Sehat, M.; Banafshe, H.R. The Effect of Propolis plus Hyoscyamus Niger L. Methanolic Extract on Clinical Symptoms in Patients with Acute Respiratory Syndrome Suspected to COVID-19: A Clinical Trial. Phytother. Res. PTR 2021, 35, 4000–4006. [Google Scholar] [CrossRef] [PubMed]
- Bilir, O.; Kocak, A.O.; Atas, I. Evaluation of the Effect of Anatolian Propolis on COVID-19 in Healthcare Professionals: Effect of Anatolian Propolis on COVID-19. Sci. Prepr. 2021. [Google Scholar] [CrossRef]
- Refaat, H.; Mady, F.M.; Sarhan, H.A.; Rateb, H.S.; Alaaeldin, E. Optimization and Evaluation of Propolis Liposomes as a Promising Therapeutic Approach for COVID-19. Int. J. Pharm. 2021, 592, 120028. [Google Scholar] [CrossRef] [PubMed]
- Elwakil, B.H.; Shaaban, M.M.; Bekhit, A.A.; El-Naggar, M.Y.; Olama, Z.A. Potential Anti-COVID-19 Activity of Egyptian Propolis Using Computational Modeling. Future Virol. 2021, 16, 107–116. [Google Scholar] [CrossRef]
- Collazo, N.; Carpena, M.; Nuñez-Estevez, B.; Otero, P.; Simal-Gandara, J.; Prieto, M.A. Health Promoting Properties of Bee Royal Jelly: Food of the Queens. Nutrients 2021, 13, 543. [Google Scholar] [CrossRef]
- Habashy, N.H.; Abu-Serie, M.M. Major Royal-Jelly Protein 2 and Its Isoform X1 Are Two Novel Safe Inhibitors for Hepatitis C and B Viral Entry and Replication. Int. J. Biol. Macromol. 2019, 141, 1072–1087. [Google Scholar] [CrossRef]
- Hashemipour, M.A.; Tavakolineghad, Z.; Arabzadeh, S.A.M.; Iranmanesh, Z.; Nassab, S.A.H.G. Antiviral Activities of Honey, Royal Jelly, and Acyclovir Against HSV-1. Wounds Compend. Clin. Res. Pract. 2014, 26, 47–54. [Google Scholar]
- Habashy, N.H.; Abu-Serie, M.M. The Potential Antiviral Effect of Major Royal Jelly Protein2 and Its Isoform X1 against Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Insight on Their Sialidase Activity and Molecular Docking. J. Funct. Foods 2020, 75, 104282. [Google Scholar] [CrossRef]
- Abedini, A.; Shafaghi, S.; Ahmad, Z.A.; Javanmardi, E.; Ghorbani, F.; Sharif-Kashani, B.; Naghashzadeh, F.; Shafaghi, M.; Moshirpour, M.; Noorali, S. N-Chromosome Royal Jelly, Propolis and Bee Pollen Supplementation Improve the Clinical Conditions of COVID-19 Patients: A Randomized Controlled Trial. Tradit. Integr. Med. 2021, 6, 360–369. [Google Scholar] [CrossRef]
- Majtán, J.; Kovácová, E.; Bíliková, K.; Simúth, J. The Immunostimulatory Effect of the Recombinant Apalbumin 1-Major Honeybee Royal Jelly Protein-on TNFalpha Release. Int. Immunopharmacol. 2006, 6, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.-C.; Chou, W.-M.; Widowati, D.A.; Lin, I.-P.; Peng, C.-C. 10-Hydroxy-2-Decenoic Acid of Royal Jelly Exhibits Bactericide and Anti-Inflammatory Activity in Human Colon Cancer Cells. BMC Complement. Altern. Med. 2018, 18, 202. [Google Scholar] [CrossRef] [PubMed]
- Kohno, K.; Okamoto, I.; Sano, O.; Arai, N.; Iwaki, K.; Ikeda, M.; Kurimoto, M. Royal Jelly Inhibits the Production of Proinflammatory Cytokines by Activated Macrophages. Biosci. Biotechnol. Biochem. 2004, 68, 138–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machado De-Melo, A.A.; Almeida-Muradian, L.B.d.; Sancho, M.T.; Pascual-Maté, A. Composition and Properties of Apis Mellifera Honey: A Review. J. Apic. Res. 2018, 57, 5–37. [Google Scholar] [CrossRef]
- Cianciosi, D.; Forbes-Hernández, T.Y.; Afrin, S.; Gasparrini, M.; Reboredo-Rodriguez, P.; Manna, P.P.; Zhang, J.; Bravo Lamas, L.; Martínez Flórez, S.; Agudo Toyos, P. Phenolic Compounds in Honey and Their Associated Health Benefits: A Review. Molecules 2018, 23, 2322. [Google Scholar] [CrossRef] [Green Version]
- Samarghandian, S.; Farkhondeh, T.; Samini, F. Honey and Health: A Review of Recent Clinical Research. Pharmacogn. Res. 2017, 9, 121–127. [Google Scholar] [CrossRef]
- Shahzad, A.; Cohrs, R.J. In Vitro Antiviral Activity of Honey against Varicella Zoster Virus (VZV): A Translational Medicine Study for Potential Remedy for Shingles. Transl. Biomed. 2012, 3. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, K.; Rahmasari, R.; Matsunaga, A.; Haruyama, T.; Kobayashi, N. Anti-Influenza Viral Effects of Honey in Vitro: Potent High Activity of Manuka Honey. Arch. Med. Res. 2014, 45, 359–365. [Google Scholar] [CrossRef]
- Ashraf, S.; Ashraf, S.; Akmal, R.; Ashraf, M.; Kalsoom, L.; Maqsood, A.; Imran, M.A.; Farooq, I.; Ashraf, S.; Siddiqui, U.N.; et al. Prophylactic Potential of Honey and Nigella Sativa L. against Hospital and Community-Based SARS-CoV-2 Spread: A Structured Summary of a Study Protocol for a Randomised Controlled Trial. Trials 2021, 22, 618. [Google Scholar] [CrossRef] [PubMed]
- El Sayed, S.M.; Aboonq, M.S.; El Rashedy, A.G.; Aljehani, Y.T.; Abou El-Magd, R.M.; Okashah, A.M.; El-Anzi, M.E.; Alharbi, M.B.; El-Tahlawi, R.; Nabo, M.M.H.; et al. Promising Preventive and Therapeutic Effects of TaibUVID Nutritional Supplements for COVID-19 Pandemic: Towards Better Public Prophylaxis and Treatment (A Retrospective Study). Am. J. Blood Res. 2020, 10, 266–282. [Google Scholar] [PubMed]
- Mustafa, M.Z.; Shamsuddin, S.H.; Sulaiman, S.A.; Abdullah, J.M. Anti-Inflammatory Properties of Stingless Bee Honey May Reduce the Severity of Pulmonary Manifestations in COVID-19 Infections. Malays. J. Med. Sci. 2020, 27, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Mayda, N.; Özkök, A.; Bayram, N.E.; Gerçek, Y.C.; Sorkun, K. Bee Bread and Bee Pollen of Different Plant Sources: Determination of Phenolic Content, Antioxidant Activity, Fatty Acid and Element Profiles. J. Food Meas. Charact. 2020, 14, 1795–1809. [Google Scholar] [CrossRef]
- Didaras, N.A.; Dimitriou, T.; Daskou, M.; Karatasou, K.; Mossialos, D. In Vitro Assessment of the Antiviral Activity of Greek Bee Bread and Bee Collected Pollen against Enterovirus D68. J. Microbiol. Biotechnol. Food Sci. 2021, 11, e4859. [Google Scholar] [CrossRef]
- Lee, I.-K.; Hwang, B.S.; Kim, D.-W.; Kim, J.-Y.; Woo, E.-E.; Lee, Y.-J.; Choi, H.J.; Yun, B.-S. Characterization of Neuraminidase Inhibitors in Korean Papaver Rhoeas Bee Pollen Contributing to Anti-Influenza Activities in Vitro. Planta Med. 2016, 82, 524–529. [Google Scholar] [CrossRef] [Green Version]
- Wehbe, R.; Frangieh, J.; Rima, M.; El Obeid, D.; Sabatier, J.-M.; Fajloun, Z. Bee Venom: Overview of Main Compounds and Bioactivities for Therapeutic Interests. Molecules 2019, 24, 2997. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.-D.; Park, H.-J.; Chae, Y.; Lim, S. An Overview of Bee Venom Acupuncture in the Treatment of Arthritis. Evid. Based Complement. Alternat. Med. 2005, 2, 79–84. [Google Scholar] [CrossRef]
- Kasozi, K.I.; Niedbała, G.; Alqarni, M.; Zirintunda, G.; Ssempijja, F.; Musinguzi, S.P.; Usman, I.M.; Matama, K.; Hetta, H.F.; Mbiydzenyuy, N.E.; et al. Bee Venom—A Potential Complementary Medicine Candidate for SARS-CoV-2 Infections. Front. Public Health 2020, 8, 755. [Google Scholar] [CrossRef]
- Uddin, M.B.; Lee, B.-H.; Nikapitiya, C.; Kim, J.-H.; Kim, T.-H.; Lee, H.-C.; Kim, C.G.; Lee, J.-S.; Kim, C.-J. Inhibitory Effects of Bee Venom and Its Components against Viruses In Vitro and In Vivo. J. Microbiol. 2016, 54, 853–866. [Google Scholar] [CrossRef]
- Yang, W.; Hu, F.; Xu, X. Bee Venom and SARS-CoV-2. Toxicon 2020, 181, 69. [Google Scholar] [CrossRef] [PubMed]
- Cherniack, E.P.; Govorushko, S. To Bee or Not to Bee: The Potential Efficacy and Safety of Bee Venom Acupuncture in Humans. Toxicon 2018, 154, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Jagdis, A.; Sussman, G. Anaphylaxis from Bee Pollen Supplement. CMAJ 2012, 184, 1167–1169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhee, D.; Lee, H.; Chung, W.; Chang, S.; Lee, M.; Choi, J.; Moon, K.; Koh, J. Giant Dermatofibroma with Granular Cell Changes: Side-effect of Bee-venom Acupuncture? Clin. Exp. Dermatol. Clin. Dermatol. 2009, 34, e18–e20. [Google Scholar] [CrossRef]
- Padavattan, S.; Schirmer, T.; Schmidt, M.; Akdis, C.; Valenta, R.; Mittermann, I.; Soldatova, L.; Slater, J.; Mueller, U.; Markovic-Housley, Z. Identification of a B-Cell Epitope of Hyaluronidase, a Major Bee Venom Allergen, from Its Crystal Structure in Complex with a Specific Fab. J. Mol. Biol. 2007, 368, 742–752. [Google Scholar] [CrossRef]
- El-Seedi, H.R.; Eid, N.; El-Wahed, A.; Aida, A.; Rateb, M.E.; Afifi, H.S.; Algethami, A.F.; Zhao, C.; Al Naggar, Y.; Alsharif, S.M. Honey Bee Products: Preclinical and Clinical Studies of Their Anti-Inflammatory and Immunomodulatory Properties. Front. Nutr. 2022, 8, 1109. [Google Scholar]
- Aliboni, A.; D’Andrea, A.; Massanisso, P. Treatment of Propolis Specimens from Central Italy to Yield a Product with a Lower Charge of Allergenic Species. Sep. Purif. Technol. 2011, 82, 71–75. [Google Scholar] [CrossRef]
- Hwang, D.-S.; Kim, S.K.; Bae, H. Therapeutic Effects of Bee Venom on Immunological and Neurological Diseases. Toxins 2015, 7, 2413–2421. [Google Scholar] [CrossRef] [Green Version]
- Lin, T.-Y.; Hsieh, C.-L. Clinical Applications of Bee Venom Acupoint Injection. Toxins 2020, 12, 618. [Google Scholar] [CrossRef]
- Khalifa, S.A.; Elashal, M.H.; Yosri, N.; Du, M.; Musharraf, S.G.; Nahar, L.; Sarker, S.D.; Guo, Z.; Cao, W.; Zou, X. Bee Pollen: Current Status and Therapeutic Potential. Nutrients 2021, 13, 1876. [Google Scholar] [CrossRef]
- Bakour, M.; Laaroussi, H.; Ousaaid, D.; El Ghouizi, A.; Es-Safi, I.; Mechchate, H.; Lyoussi, B. Bee Bread as a Promising Source of Bioactive Molecules and Functional Properties: An Up-to-Date Review. Antibiotics 2022, 11, 203. [Google Scholar] [CrossRef]
- Medeiros, K.; Figueiredo, C.; Figueredo, T.; Freire, K.; Santos, F.; Alcântara-Neves, N.M.; Silva, T.; Piuvezam, M. Anti-Allergic Effect of Bee Pollen Phenolic Extract and Myricetin in Ovalbumin-Sensitized Mice. J. Ethnopharmacol. 2008, 119, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.-H.; Kim, Y.-H.; Kim, J.-K.; Park, K.-K. Anti-Allergic Effect of Bee Venom in an Allergic Rhinitis Mouse Model. Biol. Pharm. Bull. 2014, 37, 1295–1300. [Google Scholar] [CrossRef] [Green Version]
- Chung, H.-J.; Lee, J.; Shin, J.-S.; Kim, M.; Koh, W.; Kim, M.-J.; Lee, J.; Kim, E.J.; Lee, I.-H.; Kim, W.K. In Vitro and in Vivo Anti-Allergic and Anti-Inflammatory Effects of EBV, a Newly Developed Derivative of Bee Venom, through Modulation of IRF3 Signaling Pathway in a Carrageenan-Induced Edema Model. PLoS ONE 2016, 11, e0168120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marichal, T.; Starkl, P.; Reber, L.L.; Kalesnikoff, J.; Oettgen, H.C.; Tsai, M.; Metz, M.; Galli, S.J. A Beneficial Role for Immunoglobulin E in Host Defense against Honeybee Venom. Immunity 2013, 39, 963–975. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, G.; Bae, H. Bee Venom Phospholipase A2: Yesterday’s Enemy Becomes Today’s Friend. Toxins 2016, 8, 48. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Du, Y.; Lin, X.; Qian, Y.; Zhou, T.; Huang, Z. CD4+ CD25+ Regulatory T Cells in Tumor Immunity. Int. Immunopharmacol. 2016, 34, 244–249. [Google Scholar] [CrossRef]
- Zhou, W.; Zhao, Y.; Yan, Y.; Mi, J.; Lu, L.; Luo, Q.; Li, X.; Zeng, X.; Cao, Y. Antioxidant and Immunomodulatory Activities in Vitro of Polysaccharides from Bee Collected Pollen of Chinese Wolfberry. Int. J. Biol. Macromol. 2020, 163, 190–199. [Google Scholar] [CrossRef]
- Li, F.; Yuan, Q.; Rashid, F. Isolation, Purification and Immunobiological Activity of a New Water-Soluble Bee Pollen Polysaccharide from Crataegus Pinnatifida Bge. Carbohydr. Polym. 2009, 78, 80–88. [Google Scholar] [CrossRef]
- Shaldoum, F.; El-kott, A.F.; Ouda, M.M.A.; Abd-Ella, E.M. Immunomodulatory Effects of Bee Pollen on Doxorubicin-induced Bone Marrow/Spleen Immunosuppression in Rat. J. Food Biochem. 2021, 45, e13747. [Google Scholar] [CrossRef]
- Pohl, P.; Dzimitrowicz, A.; Greda, K.; Jamroz, P.; Lesniewicz, A.; Szymczycha-Madeja, A.; Welna, M. Element Analysis of Bee-Collected Pollen and Bee Bread by Atomic and Mass Spectrometry—Development in Addition to Environmental and Nutritional Aspects. TrAC Trends Anal. Chem. 2020, 128, 115922. [Google Scholar] [CrossRef]
- Pal, A.; Squitti, R.; Picozza, M.; Pawar, A.; Rongioletti, M.; Dutta, A.K.; Sahoo, S.; Goswami, K.; Sharma, P.; Prasad, R. Zinc and COVID-19: Basis of Current Clinical Trials. Biol. Trace Elem. Res. 2020, 199, 2882–2892. [Google Scholar] [CrossRef] [PubMed]
- Wessels, I.; Rolles, B.; Rink, L. The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis. Front. Immunol. 2020, 11, 1712. [Google Scholar] [CrossRef]
- Bakour, M.; Fernandes, Â.; Barros, L.; Sokovic, M.; Ferreira, I.C.F.R. Badiaa lyoussi Bee Bread as a Functional Product: Chemical Composition and Bioactive Properties. LWT Food Sci. Technol. 2019, 109, 276–282. [Google Scholar] [CrossRef] [Green Version]
- Mohammad, S.M.; Mahmud-Ab-Rashid, N.-K.; Zawawi, N. Botanical Origin and Nutritional Values of Bee Bread of Stingless Bee (Heterotrigona Itama) from Malaysia. J. Food Qual. 2020, 2020, 2845757. [Google Scholar] [CrossRef] [Green Version]
- Stanciu, O.G.; Marghitas, L.A.; Dezmirean, D. Macro-and Oligo-Mineral Elements from Honeybee-Collected Pollen and Beebread Harvested from Transylvania (Romania). Bull. Univ. Agric. Sci. Vet. Med. Cluj-Napoca Anim. Sci. Biotechnol. 2009, 66, 1–2. [Google Scholar]
- Adaškevičiūtė, V.; Kaškonienė, V.; Kaškonas, P.; Barčauskaitė, K.; Maruška, A. Comparison of Physicochemical Properties of Bee Pollen with Other Bee Products. Biomolecules 2019, 9, 819. [Google Scholar] [CrossRef] [Green Version]
- Kalaycıoğlu, Z.; Kaygusuz, H.; Döker, S.; Kolayli, S.; Erim, F.B. Characterization of Turkish Honeybee Pollens by Principal Component Analysis Based on Their Individual Organic Acids, Sugars, Minerals, and Antioxidant Activities. LWT Food Sci. Technol. 2017, 84, 402–408. [Google Scholar] [CrossRef]
- Sandikci, S.; Tarhan, D.; Yılmaz Aksu, F.; Barutçu, Ü.; Or, M.E. Mineral Element and Heavy Metal (Cadmium, Lead and Arsenic) Levels of Bee Pollen in Turkey. Food Sci. Technol. Camp. 2017, 37, 136–141. [Google Scholar] [CrossRef] [Green Version]
- Spulber, R.; Doğaroğlu, M.; Băbeanu, N.; Popa, O. Physicochemical Characteristics of Fresh Bee Pollen from Different Botanical Origins. Rom. Biotechnol. Lett. 2018, 23, 13357–13365. [Google Scholar]
- Aldgini, H.; Abbadi, A.; Abu-Nameh, E.; Alghazeer, R. Determination of Metals as Bio Indicators in Some Selected Bee Pollen Samples from Jordan. Saudi J. Biol. Sci. 2019, 26. [Google Scholar] [CrossRef] [PubMed]
- Formicki, G.; Greń, A.; Stawarz, R.; Zyśk, B.; Gał, A. Metal Content in Honey, Propolis, Wax, and Bee Pollen and Implications for Metal Pollution Monitoring. Pol. J. Environ. Stud. 2013, 22, 99–106. [Google Scholar]
- Kostić, A.Ž.; Barać, M.B.; Stanojević, S.P.; Milojković-Opsenica, D.M.; Tešić, Ž.L.; Šikoparija, B.; Radišić, P.; Prentović, M.; Pešić, M.B. Physicochemical Composition and Techno-Functional Properties of Bee Pollen Collected in Serbia. LWT Food Sci. Technol. 2015, 62, 301–309. [Google Scholar] [CrossRef]
- Liolios, V.; Tananaki, C.; Papaioannou, A.; Kanelis, D.; Rodopoulou, M.-A.; Argena, N. Mineral Content in Monofloral Bee Pollen: Investigation of the Effect of the Botanical and Geographical Origin. J. Food Meas. Charact. 2019, 13, 1674–1682. [Google Scholar] [CrossRef]
- Máriássyová, M.I.; Kropková, Z.K.; Kačániová, M.; Fatrcová-Šramková, K.; Nóźková, J. Microbial Properties, Nutritional Composition and Antioxidant Activity of Brassica napus subsp. napus L. Bee Pollen Used in Human Nutrition. Ecol. Chem. Eng. A 2010, 17, 45–54. [Google Scholar]
- Serra Bonvehí, J.; Escolà Jordà, R. Nutrient Composition and Microbiological Quality of Honeybee-Collected Pollen in Spain. J. Agric. Food Chem. 1997, 45, 725–732. [Google Scholar] [CrossRef]
- Yang, K.; Wu, D.; Ye, X.; Liu, D.; Chen, J.; Sun, P. Characterization of Chemical Composition of Bee Pollen in China. J. Agric. Food Chem. 2013, 61, 708–718. [Google Scholar] [CrossRef]
- Serra Bonvehí, J.; Orantes-Bermej, F.J. Element Content of Propolis Collected from Different Areas of South Spain. Environ. Monit. Assess. 2013, 185, 6035–6047. [Google Scholar] [CrossRef]
- Cantarelli, M.Á.; Camiña, J.M.; Pettenati, E.M.; Marchevsky, E.J.; Pellerano, R.G. Trace Mineral Content of Argentinean Raw Propolis by Neutron Activation Analysis (NAA): Assessment of Geographical Provenance by Chemometrics. LWT Food Sci. Technol. 2011, 44, 256–260. [Google Scholar] [CrossRef]
- DOĞAN, M.; Silici, S.; Saraymen, R.; Ilhan, I.O. Element Content of Propolis from Different Regions of Turkey. Acta Aliment. 2006, 35, 127–130. [Google Scholar] [CrossRef]
- Finger, D.; Kelte Filho, I.; Torres, Y.R.; Quináia, S.P. Propolis as an Indicator of Environmental Contamination by Metals. Bull. Environ. Contam. Toxicol. 2014, 92, 259–264. [Google Scholar] [CrossRef] [PubMed]
- González-Martín, M.I.; Escuredo, O.; Revilla, I.; Vivar-Quintana, A.M.; Coello, M.C.; Riocerezo, C.P.; Moncada, G.W. Determination of the Mineral Composition and Toxic Element Contents of Propolis by near Infrared Spectroscopy. Sensors 2015, 15, 27854–27868. [Google Scholar] [CrossRef] [PubMed]
- Lima, B.; Tapia, A.; Luna, L.; Fabani, M.; Schmeda-Hirschmann, G.; Podio, N.; Wunderlin, D.; Feresin, G. Main Flavonoids, DPPH Activity, and Metal Content Allow Determination of the Geographical Origin of Propolis from the Province of San Juan (Argentina). J. Agric. Food Chem. 2009, 57, 2691–2698. [Google Scholar] [CrossRef] [PubMed]
- Maragou, N.; Pavlidis, G.; Karasali, H.; Hatjina, F. Major and Minor Element Levels in Greek Apicultural Products. Glob. Nest J. 2017, 19, 423–429. [Google Scholar]
- Roman, A.; Madras-Majewska, B.; Popiela-Pleban, E. Comparative Study of Selected Toxic Elements in Propolis and Honey. J. Apic. Sci. 2011, 55, 97–106. [Google Scholar]
- Souza, E.; Zaluski, R.; Veiga, N.; Orsi, R. Effects of Seasonal Variations and Collection Methods on the Mineral Composition of Propolis from Apis Mellifera Linnaeus Beehives. Braz. J. Biol. 2016, 76, 396–401. [Google Scholar] [CrossRef] [Green Version]
- Tosic, S.; Stojanovic, G.; Mitic, S.; Pavlovic, A.; Alagic, S. Mineral Composition of Selected Serbian Propolis Samples. J. Apic. Sci. 2017, 61, 5–15. [Google Scholar] [CrossRef] [Green Version]
- Alvarez-Suarez, J.M.; Giampieri, F.; Damiani, E.; Astolfi, P.; Fattorini, D.; Regoli, F.; Quiles, J.L.; Battino, M. Radical-Scavenging Activity, Protective Effect against Lipid Peroxidation and Mineral Contents of Monofloral Cuban Honeys. Plant Foods Hum. Nutr. 2012, 67, 31–38. [Google Scholar] [CrossRef]
- EL-Kazafy, A.; Ali, M. Determination of Heavy Metals Content in Cotton Honey in Kafr El-Shiekh Province, Egypt. J. Plant Prot. Pathol. 2012, 3, 1211–1219. [Google Scholar] [CrossRef]
- Grembecka, M.; Szefer, P. Evaluation of Honeys and Bee Products Quality Based on Their Mineral Composition Using Multivariate Techniques. Environ. Monit. Assess. 2013, 185, 4033–4047. [Google Scholar] [CrossRef] [Green Version]
- Kek, S.P.; Chin, N.L.; Tan, S.W.; Yusof, Y.A.; Chua, L.S. Classification of Honey from Its Bee Origin via Chemical Profiles and Mineral Content. Food Anal. Methods 2017, 10, 19–30. [Google Scholar] [CrossRef]
- Laaroussi, H.; Bouddine, T.; Bakour, M.; Ousaaid, D.; Lyoussi, B. Physicochemical Properties, Mineral Content, Antioxidant Activities, and Microbiological Quality of Bupleurum Spinosum Gouan Honey from the Middle Atlas in Morocco. J. Food Qual. 2020, 2020, 7609454. [Google Scholar] [CrossRef] [Green Version]
- Liberato, M.D.C.T.C.; Morais, S.M.D.; Magalhães, C.E.D.C.; Magalhães, I.L.; Cavalcanti, D.B.; Silva, M.M.D.O. Physicochemical Properties and Mineral and Protein Content of Honey Samples from Ceará State, Northeastern Brazil. Food Sci. Technol. 2013, 33, 38–46. [Google Scholar] [CrossRef]
- Maiyo, W.; Kituyi, J.; Mitei, Y.; Kagwanja, S. Heavy Metal Contamination in Raw Honey, Soil and Flower Samples Obtained from Baringo and Keiyo Counties, Kenya. Int. J. Emerg. Sci. Eng. 2014, 2, 5–9. [Google Scholar]
- Mondragón-Cortez, P.; Ulloa, J.; Rosas-Ulloa, P.; Rodríguez-Rodríguez, R.; Resendiz Vázquez, J. Physicochemical Characterization of Honey from the West Region of México. CyTA-J. Food 2013, 11, 7–13. [Google Scholar] [CrossRef]
- Moniruzzaman, M.; Khalil, I.; Sulaiman, S.A.; Gan, S.H. Physicochemical and Antioxidant Properties of Malaysian Honeys Produced by Apis cerana, Apis dorsata and Apis mellifera. BMC Complement. Altern. Med. 2013, 13, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nigussie, K.; Subramanian, P.; Mebrahtu, G. Physicochemical Analysis of Tigray Honey: An Attempt to Determine Major Quality Markers of Honey. Bull. Chem. Soc. Ethiop. 2012, 26, 26. [Google Scholar] [CrossRef] [Green Version]
- Mbiri, A.; Onditi, A.; Oyaro, N.; Murago, E. Determination of Essential and Heavy Metals in Kenyan Honey by Atomic Absorption and Emission Spectroscopy. J. Agric. Sci. Technol. 2011, 13, 107–115. [Google Scholar]
- Ru, Q.-M.; Feng, Q.; He, J.-Z. Risk Assessment of Heavy Metals in Honey Consumed in Zhejiang Province, Southeastern China. Food Chem. Toxicol. 2013, 53, 256–262. [Google Scholar] [CrossRef]
- Sakač, M.B.; Jovanov, P.T.; Marić, A.Z.; Pezo, L.L.; Kevrešan, Ž.S.; Novaković, A.R.; Nedeljković, N.M. Physicochemical Properties and Mineral Content of Honey Samples from Vojvodina (Republic of Serbia). Food Chem. 2019, 276, 15–21. [Google Scholar] [CrossRef]
- Swaileh, K.M.; Abdulkhaliq, A. Analysis of Aflatoxins, Caffeine, Nicotine and Heavy Metals in Palestinian Multifloral Honey from Different Geographic Regions. J. Sci. Food Agric. 2013, 93, 2116–2120. [Google Scholar] [CrossRef] [PubMed]
- Vanhanen, L.P.; Emmertz, A.; Savage, G.P. Mineral Analysis of Mono-Floral New Zealand Honey. Food Chem. 2011, 128, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Stocker, A.; Schramel, P.; Kettrup, A.; Bengsch, E. Trace and Mineral Elements in Royal Jelly and Homeostatic Effects. J. Trace Elem. Med. Biol. 2005, 19, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ma, L.; Zhang, W.; Cui, X.; Wang, H.; Xu, B. Comparison of the Nutrient Composition of Royal Jelly and Worker Jelly of Honey Bees (Apis mellifera). Apidologie 2016, 47, 48–56. [Google Scholar] [CrossRef] [Green Version]
- Zhang, G.; Zhang, W.; Cui, X.; Xu, B. Zinc Nutrition Increases the Antioxidant Defenses of Honey Bees. Entomol. Exp. Appl. 2015, 156, 201–210. [Google Scholar] [CrossRef]
- Kostić, A.Ž.; Pešić, M.B.; Mosić, M.D.; Dojčinović, B.P.; Natić, M.M.; Trifković, J.Đ. Mineral Content of Bee Pollen from Serbia. Arh. Hig. Rada Toksikol. 2015, 66, 251–258. [Google Scholar] [CrossRef] [Green Version]
- Carpes, S.T.; Cabral, I.S.R.; Luz, C.F.P.; Capeletti, J.P.; Alencar, S.M. Palynological and Physicochemical Characterization of Apis mellifera L. Bee Pollen in the Southern Region of Brazil. J. Food Agric. Environ. 2009, 7, 667–673. [Google Scholar]
- Costa, M.C.A.; Morgano, M.A.; Ferreira, M.M.C.; Milani, R.F. Quantification of Mineral Composition of Brazilian Bee Pollen by near Infrared Spectroscopy and PLS Regression. Food Chem. 2019, 273, 85–90. [Google Scholar] [CrossRef]
- Moniruzzaman, M.; Chowdhury, M.A.Z.; Rahman, M.A.; Sulaiman, S.A.; Gan, S.H. Determination of Mineral, Trace Element, and Pesticide Levels in Honey Samples Originating from Different Regions of Malaysia Compared to Manuka Honey. BioMed Res. Int. 2014, 2014, 359890. [Google Scholar] [CrossRef]
- European Commission. EU Register of Nutrition and Health Claims Made on Food; European Commission. 2016. Available online: https://ec.europa.eu/food/safety/labelling_nutrition/claims/register/public/?event=register.home (accessed on 8 February 2022).
- Polak, E.; Stępień, A.E.; Gol, O.; Tabarkiewicz, J. Potential Immunomodulatory Effects from Consumption of Nutrients in Whole Foods and Supplements on the Frequency and Course of Infection: Preliminary Results. Nutrients 2021, 13, 1157. [Google Scholar] [CrossRef]
- Ferreira-Santos, P.; Genisheva, Z.; Botelho, C.; Rocha, C.; Teixeira, J.A. Valorization of Natural Antioxidants for Nutritional and Health Applications. In Antioxidants; IntechOpen: London, UK, 2021. [Google Scholar]
- Zhao, B.; Ling, Y.; Li, J.; Peng, Y.; Huang, J.; Wang, Y.; Qu, H.; Gao, Y.; Li, Y.; Hu, B. Beneficial Aspects of High Dose Intravenous Vitamin C on Patients with COVID-19 Pneumonia in Severe Condition: A Retrospective Case Series Study. Ann. Palliat. Med. 2021, 10, 1599–1609. [Google Scholar] [CrossRef] [PubMed]
- Hakamifard, A.; Soltani, R.; Maghsoudi, A.; Rismanbaf, A.; Aalinezhad, M.; Tarrahi, M.; Mashayekhbakhsh, S.; Dolatshahi, K. The Effect of Vitamin E and Vitamin C in Patients with COVID-19 Pneumonia; a Randomized Controlled Clinical Trial. Immunopathol. Persa 2021, 7, e08. [Google Scholar]
- Azeem, M.; Hanif, M.; Mahmood, K.; Ameer, N.; Chughtai, F.R.S.; Abid, U. An Insight into Anticancer, Antioxidant, Antimicrobial, Antidiabetic and Anti-Inflammatory Effects of Quercetin: A Review. Polym. Bull. 2022, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Alijotas-Reig, J.; Esteve-Valverde, E.; Belizna, C.; Selva-O’Callaghan, A.; Pardos-Gea, J.; Quintana, A.; Mekinian, A.; Anunciacion-Llunell, A.; Miró-Mur, F. Immunomodulatory Therapy for the Management of Severe COVID-19. Beyond the Anti-Viral Therapy: A Comprehensive Review. Autoimmun. Rev. 2020, 19, 102569. [Google Scholar] [CrossRef] [PubMed]
- Derwand, R.; Scholz, M. Does Zinc Supplementation Enhance the Clinical Efficacy of Chloroquine/Hydroxychloroquine to Win Today’s Battle against COVID-19? Med. Hypotheses 2020, 142, 109815. [Google Scholar] [CrossRef]
- Pastick, K.A.; Okafor, E.C.; Wang, F.; Lofgren, S.M.; Skipper, C.P.; Nicol, M.R.; Pullen, M.F.; Rajasingham, R.; McDonald, E.G.; Lee, T.C. Hydroxychloroquine and Chloroquine for Treatment of SARS-CoV-2 (COVID-19); Oxford University Press: New York, NY, USA, 2020; Volume 7, p. ofaa130. [Google Scholar]
- Xue, J.; Moyer, A.; Peng, B.; Wu, J.; Hannafon, B.N.; Ding, W.-Q. Chloroquine Is a Zinc Ionophore. PLoS ONE 2014, 9, e109180. [Google Scholar] [CrossRef] [Green Version]
- Te Velthuis, A.J.W.; van den Worm, S.H.E.; Sims, A.C.; Baric, R.S.; Snijder, E.J.; van Hemert, M.J. Zn2+ Inhibits Coronavirus and Arterivirus RNA Polymerase Activity in Vitro and Zinc Ionophores Block the Replication of These Viruses in Cell Culture. PLoS Pathog. 2010, 6, e1001176. [Google Scholar] [CrossRef]
- Carlucci, P.M.; Ahuja, T.; Petrilli, C.; Rajagopalan, H.; Jones, S.; Rahimian, J. Zinc Sulfate in Combination with a Zinc Ionophore May Improve Outcomes in Hospitalized COVID-19 Patients. J. Med. Microbiol. 2020, 69, 1228. [Google Scholar] [CrossRef]
- Al Sulaiman, K.; Aljuhani, O.; Al Shaya, A.I.; Kharbosh, A.; Kensara, R.; Al Guwairy, A.; Alharbi, A.; Algarni, R.; Al Harbi, S.; Vishwakarma, R. Evaluation of Zinc Sulfate as an Adjunctive Therapy in COVID-19 Critically Ill Patients: A Two Center Propensity-Score Matched Study. Crit. Care 2021, 25, 363. [Google Scholar] [CrossRef]
- Szarpak, L.; Pruc, M.; Gasecka, A.; Jaguszewski, M.J.; Michalski, T.; Peacock, F.W.; Smereka, J.; Pytkowska, K.; Filipiak, K.J. Should We Supplement Zinc in COVID-19 Patients? Evidence from Meta-Analysis. Pol. Arch. Intern. Med. 2021, 131, 802–807. [Google Scholar] [CrossRef]
- Gupta, S.; Read, S.A.; Shackel, N.A.; Hebbard, L.; George, J.; Ahlenstiel, G. The Role of Micronutrients in the Infection and Subsequent Response to Hepatitis C Virus. Cells 2019, 8, 603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giménez, V.M.M.; Bergam, I.; Reiter, R.J.; Manucha, W. Metal Ion Homeostasis with Emphasis on Zinc and Copper: Potential Crucial Link to Explain the Non-Classical Antioxidative Properties of Vitamin D and Melatonin. Life Sci. 2021, 281, 119770. [Google Scholar] [CrossRef] [PubMed]
- Von Bülow, V.; Dubben, S.; Engelhardt, G.; Hebel, S.; Plümäkers, B.; Heine, H.; Rink, L.; Haase, H. Zinc-Dependent Suppression of TNF-α Production Is Mediated by Protein Kinase A-Induced Inhibition of Raf-1, IκB Kinase β, and NF-ΚB. J. Immunol. 2007, 179, 4180–4186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jalal, Z.; Bakour, M.; Lyoussi, B. Medicinal Plants and Zinc: Impact on COVID-19 Pandemic. Sci. World J. 2021, 2021, 9632034. [Google Scholar] [CrossRef] [PubMed]
- Abbas, M.; Saeed, F.; Anjum, F.M.; Afzaal, M.; Tufail, T.; Bashir, M.S.; Ishtiaq, A.; Hussain, S.; Suleria, H.A.R. Natural Polyphenols: An Overview. Int. J. Food Prop. 2017, 20, 1689–1699. [Google Scholar] [CrossRef] [Green Version]
- Bakour, M.; Campos, M.d.G.; Imtara, H.; Lyoussi, B. Antioxidant Content and Identification of Phenolic/Flavonoid Compounds in the Pollen of Fourteen Plants Using HPLC-DAD. J. Apic. Res. 2019, 59, 35–41. [Google Scholar] [CrossRef]
- Galeotti, F.; Capitani, F.; Fachini, A.; Volpi, N. Recent Advances in Analytical Approaches for the Standardization and Quality of Polyphenols of Propolis. J. Med. Plants Res. 2019, 13, 487–500. [Google Scholar]
- Rzepecka-Stojko, A.; Stojko, J.; Kurek-Górecka, A.; Górecki, M.; Kabała-Dzik, A.; Kubina, R.; Moździerz, A.; Buszman, E. Polyphenols from Bee Pollen: Structure, Absorption, Metabolism and Biological Activity. Molecules 2015, 20, 21732–21749. [Google Scholar] [CrossRef] [Green Version]
- Memariani, H.; Memariani, M.; Moravvej, H.; Shahidi-Dadras, M. Melittin: A Venom-Derived Peptide with Promising Anti-Viral Properties. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 5–17. [Google Scholar] [CrossRef]
- Sobral, F.; Sampaio, A.; Falcão, S.; Queiroz, M.J.R.; Calhelha, R.C.; Vilas-Boas, M.; Ferreira, I.C. Chemical Characterization, Antioxidant, Anti-Inflammatory and Cytotoxic Properties of Bee Venom Collected in Northeast Portugal. Food Chem. Toxicol. 2016, 94, 172–177. [Google Scholar] [CrossRef] [Green Version]
- Medana, C.; Carbone, F.; Aigotti, R.; Appendino, G.; Baiocchi, C. Selective Analysis of Phenolic Compounds in Propolis by HPLC-MS/MS. Phytochem. Anal. Int. J. Plant Chem. Biochem. Tech. 2008, 19, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Dranca, F.; Ursachi, F.; Oroian, M. Bee Bread: Physicochemical Characterization and Phenolic Content Extraction Optimization. Foods 2020, 9, 1358. [Google Scholar] [CrossRef]
- Osés, S.M.; Marcos, P.; Azofra, P.; de Pablo, A.; Fernández-Muíño, M.Á.; Sancho, M.T. Phenolic Profile, Antioxidant Capacities and Enzymatic Inhibitory Activities of Propolis from Different Geographical Areas: Needs for Analytical Harmonization. Antioxidants 2020, 9, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulusoy, E.; Kolayli, S. Phenolic Composition and Antioxidant Properties of Anzer Bee Pollen. J. Food Biochem. 2014, 38, 73–82. [Google Scholar] [CrossRef]
- Velásquez, P.; Montenegro, G.; Giordano, A.; Retamal, M.; Valenzuela, L. Bioactivities of Phenolic Blend Extracts from Chilean Honey and Bee Pollen. CyTA-J. Food 2019, 17, 754–762. [Google Scholar] [CrossRef] [Green Version]
- Cheung, Y.; Meenu, M.; Yu, X.; Xu, B. Phenolic Acids and Flavonoids Profiles of Commercial Honey from Different Floral Sources and Geographic Sources. Int. J. Food Prop. 2019, 22, 290–308. [Google Scholar] [CrossRef]
- Elamine, Y.; Lyoussi, B.; Miguel, M.G.; Anjos, O.; Estevinho, L.; Alaiz, M.; Girón-Calle, J.; Martín, J.; Vioque, J. Physicochemical Characteristics and Antiproliferative and Antioxidant Activities of Moroccan Zantaz Honey Rich in Methyl Syringate. Food Chem. 2021, 339, 128098. [Google Scholar] [CrossRef] [PubMed]
- Berretta, A.A.; Silveira, M.A.D.; Capcha, J.M.C.; De Jong, D. Propolis and Its Potential against SARS-CoV-2 Infection Mechanisms and COVID-19 Disease: Running Title: Propolis against SARS-CoV-2 Infection and COVID-19. Biomed. Pharmacother. 2020, 131, 110622. [Google Scholar] [CrossRef] [PubMed]
- Laforge, M.; Elbim, C.; Frère, C.; Hémadi, M.; Massaad, C.; Nuss, P.; Benoliel, J.-J.; Becker, C. Tissue Damage from Neutrophil-Induced Oxidative Stress in COVID-19. Nat. Rev. Immunol. 2020, 20, 515–516. [Google Scholar] [CrossRef]
- Yahfoufi, N.; Alsadi, N.; Jambi, M.; Matar, C. The Immunomodulatory and Anti-Inflammatory Role of Polyphenols. Nutrients 2018, 10, 1618. [Google Scholar] [CrossRef] [Green Version]
- Hussain, T.; Tan, B.; Yin, Y.; Blachier, F.; Tossou, M.C.; Rahu, N. Oxidative Stress and Inflammation: What Polyphenols Can Do for Us? Oxid. Med. Cell. Longev. 2016, 2016, 7432797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoon, J.-H.; Baek, S.J. Molecular Targets of Dietary Polyphenols with Anti-Inflammatory Properties. Yonsei Med. J. 2005, 46, 585–596. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sahlan, M.; Irdiani, R.; Flamandita, D.; Aditama, R.; Alfarraj, S.; Ansari, M.J.; Khayrani, A.C.; Pratami, D.K.; Lischer, K. Molecular Interaction Analysis of Sulawesi Propolis Compounds with SARS-CoV-2 Main Protease as Preliminary Study for COVID-19 Drug Discovery. J. King Saud Univ.-Sci. 2021, 33, 101234. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Dhanjal, J.K.; Kaul, S.C.; Wadhwa, R.; Sundar, D. Withanone and Caffeic Acid Phenethyl Ester Are Predicted to Interact with Main Protease (Mpro) of SARS-CoV-2 and Inhibit Its Activity. J. Biomol. Struct. Dyn. 2021, 39, 3842–3854. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.S.; Sushma, P.; Dharmashekar, C.; Beelagi, M.S.; Prasad, S.K.; Shivamallu, C.; Prasad, A.; Syed, A.; Marraiki, N.; Prasad, K.S. In Silico Evaluation of Flavonoids as Effective Antiviral Agents on the Spike Glycoprotein of SARS-CoV-2. Saudi J. Biol. Sci. 2021, 28, 1040–1051. [Google Scholar] [CrossRef]
- Hashem, H. In Silico Approach of Some Selected Honey Constituents as SARS-CoV-2 Main Protease (COVID-19) Inhibitors. EJMO. 2020, 3, 196–200. [Google Scholar] [CrossRef]
- Vijayakumar, B.G.; Ramesh, D.; Joji, A.; Kannan, T. In Silico Pharmacokinetic and Molecular Docking Studies of Natural Flavonoids and Synthetic Indole Chalcones against Essential Proteins of SARS-CoV-2. Eur. J. Pharmacol. 2020, 886, 173448. [Google Scholar] [CrossRef]
- Pitsillou, E.; Liang, J.; Ververis, K.; Hung, A.; Karagiannis, T.C. Interaction of Small Molecules with the SARS-CoV-2 Papain-like Protease: In Silico Studies and in Vitro Validation of Protease Activity Inhibition Using an Enzymatic Inhibition Assay. J. Mol. Graph. Model. 2021, 104, 107851. [Google Scholar] [CrossRef]
- Bumrungpert, A.; Lilitchan, S.; Tuntipopipat, S.; Tirawanchai, N.; Komindr, S. Ferulic Acid Supplementation Improves Lipid Profiles, Oxidative Stress, and Inflammatory Status in Hyperlipidemic Subjects: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Nutrients 2018, 10, 713. [Google Scholar] [CrossRef] [Green Version]
- Abdollahi, S.; Salehi-Abargouei, A.; Toupchian, O.; Sheikhha, M.H.; Fallahzadeh, H.; Rahmanian, M.; Tabatabaie, M.; Mozaffari-Khosravi, H. The Effect of Resveratrol Supplementation on Cardio-metabolic Risk Factors in Patients with Type 2 Diabetes: A Randomized, Double-blind Controlled Trial. Phytother. Res. 2019, 33, 3153–3162. [Google Scholar] [CrossRef]
- Marinella, M.A. Indomethacin and Resveratrol as Potential Treatment Adjuncts for SARS-CoV-2/COVID-19. Int. J. Clin. Pract. 2020, 74, e13535. [Google Scholar] [CrossRef] [PubMed]
- McKee, D.L.; Sternberg, A.; Stange, U.; Laufer, S.; Naujokat, C. Candidate Drugs against SARS-CoV-2 and COVID-19. Pharmacol. Res. 2020, 157, 104859. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).