Abstract
Although the association between meat consumption and cardiovascular diseases (CVDs) has been extensively investigated, studies focusing specifically on the relationship between white meat consumption and CVD risk factors are fewer with controversial findings. The aim was to evaluate the relationship between white meat consumption and the incidence of cardiometabolic risk factors. A comprehensive literature search of PubMed articles was conducted from 2010 to 2022 (1 November), according to PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines. Thirteen prospective cohort studies were selected studying mainly poultry, with the exception of one study that also analyzed rabbit meat. From the seven studies on the risk of type 2 diabetes mellitus, four studies found no association, two studies found positive associations, and two studies found inverse associations when comparing poultry to other meats. Of the two studies on the risk of hypertension, one observed no association and one a positive association. Of the two studies on weight management, one observed a positive association with weight gain, the other study observed the same relationship only for chicken with skin, while for chicken without skin a positive relationship with relative weight loss was found. As for metabolic syndrome and its components, two studies revealed inverse associations with white meat intake. Only fresh lean white meat consumption seems to have potential beneficial effects on cardiometabolic risk factors. Future research should scrutinize consumption habits related to white meat intake when investigating its association with cardiometabolic risk factors.
1. Introduction
A rise in the previously declining age-standardized rate of cardiovascular disease (CVD) that has been observed might be attributed to the increasing prevalence of CVD risk factors such as type 2 diabetes mellitus, hypertension, hypercholesterolemia, and obesity [1]. International dietary guidelines [2] as well as the Sustainable Development Goals [3] recommend a reduction of meat consumption and a better adherence to a more plant-based diet; however, meat consumption is still high, especially in the Western world or for people adopting a westernized diet. With the exception of some African and Asian territories, in the majority of the world, daily meat consumption is expected to be over 165 g per day per person in 2030 [4,5], i.e., numbers which far surpass the recommended cooked meat consumption of 350–500 g per week [6].
Beyond the serious environmental concerns of the increased meat consumption [7], a lot of studies have been conducted relevant to the association between meat consumption and health outcomes. Specifically, meta-analyses have shown controversial results highlighting the need for differentiation between the types of meat consumed and their association with CVD risk. For instance, in a recently conducted meta-analysis, a reduction of processed as well as unprocessed red meat consumption was associated with small reductions in risk for cardiovascular mortality, stroke, myocardial infarction (MI), and type 2 diabetes mellitus (T2DM) albeit the evidence was of low certainty [8].
Other meta-analyses have shown a robust positive association between red and processed meat consumption and incidence of CVD and diabetes [9,10]. On the contrary, white meat has recently been proposed as a potential healthier alternative to red meat showing a neutral association with CVD mortality and morbidity [11]. To the best of our knowledge, studies focusing specifically on the relationship between white and in particular lean meat consumption and CVD risk factors are fewer with unclear findings.
Thus, the aim of this study was to review the relationship between white meat consumption and cardiometabolic risk factors based on recent prospective cohort studies; we hypothesized that lean white meat is beneficial for reducing the incidence of cardiometabolic risk factors.
2. Methods
2.1. Search Strategy
A comprehensive literature search of PubMed articles was carried out from 1 January 2010 to 1 November 2022, according to PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines [12]. Using appropriate Boolean operators (AND, OR, and NOT), the key words used in the search string were (“poultry” or “white meat” or “chicken” or “turkey” or “rabbit”) and (“hypertension” OR “diabetes mellitus” OR “obesity” OR “hypercholesterolemia” OR “triglycerides” OR “non-alcoholic fatty liver disease” OR “metabolic syndrome”) and (“meat” or “consumption” or “intake” or “serving”). Two review authors independently extracted all data and a third author resolved disagreements.
The flow-chart regarding the details of the literature search is reported in Figure 1; from a total of 1915 reports found through the search string, 464 remained after the use of filters according to inclusion and exclusion criteria (i.e., humans, adult: 19+ years, language: English, publication date: 2010–2022). To search for relevant studies, a hierarchical approach was used (i.e., screening the title or abstract for the 464 records, choosing 23 records for retrieval and reading the full-text manuscript of 21 articles that were successfully retrieved). References of retrieved articles were also manually searched, but no additional studies that matched the criteria were found.
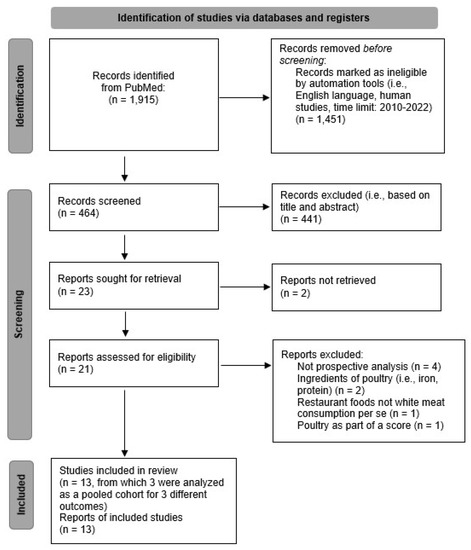
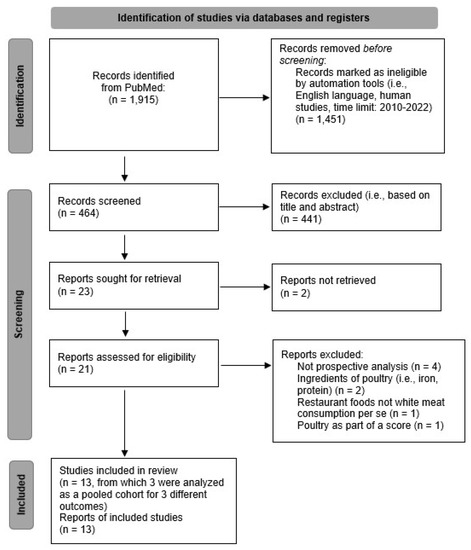
Figure 1.
The flow diagram of study identification, screening, and inclusion process based on PRISMA guidelines [13].
2.2. Inclusion and Exclusion Criteria
The CoCoPop (condition, context, and population) [14] method was used to formulate and narrow the focus of the research question (Is white meat consumption of healthy adults associated with the occurrence of cardiometabolic risk factors?); thus, inclusion and exclusion criteria were formulated, as shown in Table 1.

Table 1.
Inclusion and exclusion criteria of this review according to the CoCoPop method.
2.3. Data Collection
Key information manually extracted from the 13 selected studies and then displayed on an Excel spreadsheet included: “Author and Publication Year”, “Study name”, “Country”, “Length of follow-up”, “Number of participants”, “Sex”, “Age”, “Dietary assessment method”, “White meat type”, “Comparison group”, “CVD risk factor”, “Findings”, and “Adjustments” as shown in Table 2.

Table 2.
Study characteristics of recent prospective cohort studies included in this review.
3. Results
3.1. Study Characteristics
A total of 13 prospective cohort studies were selected to be included in the present review. Details concerning all of the above studies are shown in Table 2. Included studies focused on white meat consumption usually referred to as “poultry intake” (i.e., chicken, turkey). No studies relevant to the risk of non-alcoholic fatty liver disease, matching the inclusion criteria, were found.
From the 13 studies found, 7 addressed the risk of type 2 diabetes mellitus [15,16,17,18,19,20,21], 2 investigated the risk of hypertension [22,23], 2 studied the risk of weight gain or change [24,25], and 2 evaluated metabolic syndrome and its six components (i.e., systolic blood pressure (SBP), diastolic blood pressure (DBP), high density lipoprotein (HDL), triacyclglycerols (TAG), fasting glucose, waist circumference) [26,27]. Of note, 3 of the 13 studies were a pooled analysis of the Nurses’ Health Study (NHS), Nurses’ Health Study II (NHS II), and Health Professionals Follow-up Study (HPFS) cohorts, but each study investigated a different CVD risk factor outcome; therefore, all 3 were included [21,22,25]. Across the studies, time to follow-up ranged from 2 [27] to 24 years [25]. The minimum number of participants was 1126 [27] and the maximum number was 461,036 [20]. Finally, seven of the included studies evaluated white meat intake more than one time, via FFQs, making the evaluation of white meat consumption in these studies more representative of the populations’ actual intake [17,20,21,22,23,25,26].
3.2. Participants’ Characteristics
The participants of the included studies were healthy adults of the general population without CVD or CVD risk factors (inclusion criterion), of all ages (minimum age: 18 years), and with the exception of one study (i.e., men: 73%) [27], in all other included studies, the majority of the participants was women. Finally, the included populations were mostly from the US [15,21,22,25,27] and Asia [17,18,20,23,26], followed by Europe [16,19,24].
3.3. White Meat and CVD Risk Factors
3.3.1. White Meat and Diabetes Mellitus
From the seven studies addressing the risk of type 2 diabetes mellitus that were found [15,16,17,18,19,20,21], four studies found no association of poultry intake and the risk of T2DM [15,16,17,20], while two studies reported positive associations; the study conducted by Steinbrecher et al. [15] observed that processed poultry intake (5th vs. 1st quintile) was associated with an increased risk of T2DM by 23–30% (HRmen: 1.30, 95%CI: 1.17, 1.44; HRwomen: 1.23, 95%CI: 1.10, 1.38). The other study showed that poultry intake (4th vs. 1st quartile) was associated with 15% higher risk of T2DM (HR: 1.15, 95% CI: 1.06, 1.24, P for trend = 0.004); moreover, this association was mediated by heme iron intake [18]. On the contrary, when comparing white meat, namely poultry, to other meats, inverse associations were found in two studies [19,21]. One study concluded that when replacing 150 g/week of processed red meat with poultry, the risk of T2DM was reduced by 4% (HR: 0.96, 95% CI 0.93, 0.99), but no association was observed when poultry intake replaced low fat or high fat red meat [19]. In another study, which included 46,023 women from the Nurses’ Health Study (NHS), 75,196 women from the Nurses’ Health Study II (NHS II), and 27,634 men from the Health Professionals Follow-Up Study (HPFS), during a 4-year period, findings showed that when increasing poultry consumption (per 1 serving/day, i.e., serving size range: 112–168 g) while concomitantly decreasing the intake of red meat, 18% lower risk of T2DM in the subsequent 4-year period was observed (pooled HR: 0.82, 95% CI: 0.75, 0.90) [21].
3.3.2. White Meat and Hypertension
Regarding the association between white meat consumption and the risk of hypertension, a prospective study from Tehran Lipid and Glucose Study found no association of poultry intake and the 3-year incidence of hypertension when poultry was studied either as a continuous variable (i.e., per 1 g/d) or as a categorical one (3rd vs. 1st tertile) [23]. However, another study with 188,518 non-hypertensive individuals from the NHS, NHS II, and HPFS reported that the highest (≥1 servings/day, serving size range: 112–168 g) compared to the lowest (<1 serving/month) category of poultry intake was positively associated with risk of hypertension (pooled HR: 1.22, 95%CI: 1.12, 1.34; p-trend < 0.001), although this association was null in the subgroup of women from the NHS [22].
3.3.3. White Meat and Weight Management
Regarding the association of white meat with weight management, one study found a positive association between poultry intake and weight gain [24]. Another study with 120,784 participants free of chronic disease or obesity at baseline from the NHS, NHS II, and HPFS, studying chicken with and without skin (per increase of 1 serving/day, serving size range: 112–168 g), concluded that consumption of chicken with skin was positively associated with long-term weight gain of approximately +0.5 kg every 4 years, while consumption of chicken without skin was positively associated with a relative weight loss of approximately −0.5 kg every 4 years [25].
3.3.4. White Meat and Metabolic Syndrome
Finally, two studies investigating the association between metabolic syndrome (MetS) and its six components (i.e., fasting glucose, SBP, DBP, HDL, TAG, waist circumference) and white meat consumption [26,27] found inverse associations. Specifically, Hajihashemi et al. [26] found that an increase in the frequency of poultry intake was inversely associated with the risk of metabolic syndrome in multi-adjusted models (OR 0.78; 95% CI: 0.72–0.85) in 6504 adults free of MetS at baseline prospectively studied for a median of approximately 11 years. Moreover, Riseberg et al. [27] concluded that unprocessed poultry intake was inversely associated with TAG (b: 24.5, SE: 9.13) but not with other CVD risk factors (i.e., fasting glucose, SBP, DBP, HDL, waist circumference) in 1126 participants followed for 2 years.
4. Discussion
Meat consumption is one of the major modifiable food groups that affect disease risk, thus it is of the greatest importance to identify the type of meat that could decrease the risk of morbidity and mortality of CVD. From the present review, it seems that the adverse health effects associated with red and processed meat consumption are not shared by white meat and in particular from lean unprocessed white meat. Poultry consumption does not seem to affect the incidence of type 2 diabetes, and thus it is prudent for white meat to be consumed as a replacement of red or processed meat. Although poultry consumption was associated with a negative effect on weight loss, lean cuts were proven to be beneficial for weight management. Poultry consumption is beneficial for preventing metabolic syndrome or reducing TAG. Lastly, the association between white meat consumption and hypertension ranges from neutral to aggravating, which could be attributed to potential confounding factors [28].
Indeed, multiple confounding factors may have affected the aforementioned relationships. The most important factors that were pinpointed in the reviewed studies are the type of white meat consumed (processed or with the skin vs. unprocessed or without the skin) as well as the type of food replaced by white meat. For instance, as shown in a study [25], eating chicken with or without skin might “transform” chicken consumption from harmful (with skin) to beneficial (without skin) for long-term weight management. Of note, chicken skin is high in saturated fat, possibly explaining the observed difference [29]. Additionally, in the study conducted by Steinbrecher et al. [15] on 75,512 participants of the multiethnic cohort (i.e., Caucasians, Japanese Americans, and Native Hawaiians), with a median follow-up of 13.5 years, only the consumption of processed poultry was positively associated with type 2 diabetes incidence and not that of fresh poultry. Population characteristics such as age, sex, ethnicity/nationality, as well as the baseline diet or the quantity of the white meat consumed might also play a role. For instance, there was no uniformity of serving size, with serving size ranging from 98 g to 168 g between the included studies [21,22,25,27,30,31]. Furthermore, study characteristics such as the diagnostic criteria of each cardiometabolic outcome or the time to follow-up might have influenced the results as well.
Certain meat ingredients (i.e., heme iron, saturated fat) might explain the association between white meat and cardiometabolic risk factors. For instance, heme iron has been shown to be detrimental for CVD risk and mortality, but compared to red meat, white meat has lower concentrations of heme iron [32,33]. Interestingly, in one of the included studies, the harmful relation between poultry intake and the risk of type 2 diabetes was completely mediated by heme iron intake [18]. Furthermore, white meat has lower concentrations of saturated fat compared to other meats, especially the lean cuts, and a better lipid profile consisting mainly of unsaturated fatty acids, with the exception of the skin which is full of saturated fat [10,12,34].
In addition, total white meat consumption is usually computed via FFQs and may include different cuts/parts (e.g., chicken breast vs. drumsticks/legs), processed white meat (e.g., turkey sausage), as well as mixed dishes (e.g., chicken/turkey/duck with rice). Therefore, the observed harmful association between white meat consumption and certain cardiovascular risk factors [18,22,24] could be attributed to the lack of differentiation regarding parts/cuts consumed (skin or without skin), kind of white meat consumed (processed vs. unprocessed), or cooking method employed (fried or grilled). Indeed, foods are rarely eaten alone; therefore, food ingredients such as refined grains or sources of saturated fat (e.g., butter, cheese, mayonnaise) can be eaten concomitantly with white meat. Thus, one could presume that food combinations with white meat may mask the potential beneficial effects of lean white meat. For instance, common ingredients accompanying white meat, such as refined grain intake (e.g., white rice, white bread), are associated with increased risk of cardiometabolic risk factors [35,36], while vegetable consumption is associated with decreased cardiometabolic risk [37].
Concerning cooking methods (i.e., processing, addition of sodium/preservatives or fat sources, cooking temperature) [34], the literature showed that processed meat having a high content of sodium, preservatives, and dietary advanced glycation and lipoxidation end-products [38] affects adversely cardiometabolic risk beyond blood pressure [39,40]. Based on another analysis of a pooled cohort from the NHS, NHS II, and HPFS with 12–16 years of follow-up, a higher frequency of open-flame and/or high-temperature cooking for chicken (as well as red meat) was independently associated with an increased risk of T2DM, weight gain, and obesity [41].
For people consuming high amounts of animal protein, turning to plant-based diets—even though protective for their health—might be humanly impossible. Therefore, white meat such as chicken, turkey, rabbit, duck, and goose might be a good alternative for reducing the elevated cardiometabolic risk that is associated with red and processed meat [8]. This substitution might also be beneficial for planet sustainability. Although sustainable diets are plant-based, animal protein is a part of them. Given that beef, a main animal protein, is the most energy-consuming food to be produced [42], lean white meat could be considered as a prime candidate for the space of animal protein in the planetary health diet [43].
Strengths and Limitations
One of the limitations of this review is that only one database was searched (i.e., PubMed) and the lack of the assessment of study quality (risk of bias). However, a systematic process was used for retrieving studies. To the best of our knowledge, this is the first review analyzing the recent evidence regarding white meat consumption and the occurrence of cardiometabolic risk factors based on prospective cohort studies.
In addition, this review contains different populations and base diets, and that fact might have influenced the results, which makes these findings more generalizable. Nevertheless, publication bias might have existed [44], and that might point to an over-estimation of the relationship between white meat and CVD risk factors. Finally, an inherent limitation of most prospective cohort studies is the use of FFQs, which entail recall bias.
5. Conclusions
In conclusion, it was observed that only fresh/unprocessed and lean white meat consumption seems to have potential beneficial effects on cardiometabolic risk factors. Future research should scrutinize consumption habits related to white meat intake when investigating its relationship with cardiometabolic risk factors. Therefore, unprocessed lean white meat is a good alternative to red meat and a sustainable prime source of high-quality protein and vitamins.
Author Contributions
Conceptualization, D.B.P.; methodology, R.I.K.; writing—original draft preparation, E.D.; writing—review and editing, R.I.K.; supervision, D.B.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
No applicable.
Informed Consent Statement
No applicable.
Data Availability Statement
No applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Dietary Guidelines for Americans, 2020–2025 and Online Materials | Dietary Guidelines for Americans. Available online: https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials (accessed on 11 November 2022).
- The 2030 Agenda and the Sustainable Development Goals: An Opportunity for Latin America and the Caribbean. 2030, 94. Available online: https://repositorio.cepal.org/bitstream/handle/11362/40156/S1801140_en.pdf (accessed on 10 November 2022).
- FAOSTAT. Available online: https://www.fao.org/faostat/en/#data/FBS (accessed on 11 November 2022).
- Daily Meat Consumption per Person. Available online: https://ourworldindata.org/grapher/daily-meat-consumption-per-person (accessed on 11 November 2022).
- World Health Organization. Regional Office for Europe. Food-Based Dietary Guidelines in the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2003. [Google Scholar]
- González, N.; Marquès, M.; Nadal, M.; Domingo, J.L. Meat Consumption: Which Are the Current Global Risks? A Review of Recent (2010–2020) Evidences. Food Res. Int. 2020, 137, 109341. [Google Scholar] [CrossRef] [PubMed]
- Zeraatkar, D.; Han, M.A.; Guyatt, G.H.; Vernooij, R.W.M.; El Dib, R.; Cheung, K.; Milio, K.; Zworth, M.; Bartoszko, J.J.; Valli, C.; et al. Red and Processed Meat Consumption and Risk for All-Cause Mortality and Cardiometabolic Outcomes: A Systematic Review and Meta-Analysis of Cohort Studies. Ann. Intern. Med. 2019, 171, 703–710. [Google Scholar] [CrossRef]
- Micha, R.; Michas, G.; Mozaffarian, D. Unprocessed Red and Processed Meats and Risk of Coronary Artery Disease and Type 2 Diabetes--an Updated Review of the Evidence. Curr. Atheroscler. Rep. 2012, 14, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Bechthold, A.; Boeing, H.; Schwedhelm, C.; Hoffmann, G.; Knüppel, S.; Iqbal, K.; De Henauw, S.; Michels, N.; Devleesschauwer, B.; Schlesinger, S.; et al. Food Groups and Risk of Coronary Heart Disease, Stroke and Heart Failure: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Crit. Rev. Food Sci. Nutr. 2019, 59, 1071–1090. [Google Scholar] [CrossRef] [PubMed]
- Lupoli, R.; Vitale, M.; Calabrese, I.; Giosuè, A.; Riccardi, G.; Vaccaro, O. White Meat Consumption, All-Cause Mortality, and Cardiovascular Events: A Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 676. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Munn, Z.; Moola, S.; Lisy, K.; Riitano, D.; Tufanaru, C. Methodological Guidance for Systematic Reviews of Observational Epidemiological Studies Reporting Prevalence and Cumulative Incidence Data. Int. J. Evid. Based Healthc. 2015, 13, 147–153. [Google Scholar] [CrossRef]
- Steinbrecher, A.; Erber, E.; Grandinetti, A.; Kolonel, L.N.; Maskarinec, G. Meat Consumption and Risk of Type 2 Diabetes: The Multiethnic Cohort. Public Health Nutr. 2011, 14, 568–574. [Google Scholar] [CrossRef]
- van Woudenbergh, G.J.; Kuijsten, A.; Tigcheler, B.; Sijbrands, E.J.G.; van Rooij, F.J.A.; Hofman, A.; Witteman, J.C.M.; Feskens, E.J.M. Meat Consumption and Its Association with C-Reactive Protein and Incident Type 2 Diabetes: The Rotterdam Study. Diabetes Care 2012, 35, 1499–1505. [Google Scholar] [CrossRef]
- Kurotani, K.; Nanri, A.; Goto, A.; Mizoue, T.; Noda, M.; Oba, S.; Kato, M.; Matsushita, Y.; Inoue, M.; Tsugane, S.; et al. Red Meat Consumption Is Associated with the Risk of Type 2 Diabetes in Men but Not in Women: A Japan Public Health Center-Based Prospective Study. Br. J. Nutr. 2013, 110, 1910–1918. [Google Scholar] [CrossRef] [PubMed]
- Talaei, M.; Wang, Y.-L.; Yuan, J.-M.; Pan, A.; Koh, W.-P. Meat, Dietary Heme Iron, and Risk of Type 2 Diabetes Mellitus: The Singapore Chinese Health Study. Am. J. Epidemiol. 2017, 186, 824–833. [Google Scholar] [CrossRef] [PubMed]
- Ibsen, D.B.; Warberg, C.K.; Würtz, A.M.L.; Overvad, K.; Dahm, C.C. Substitution of Red Meat with Poultry or Fish and Risk of Type 2 Diabetes: A Danish Cohort Study. Eur. J. Nutr. 2019, 58, 2705–2712. [Google Scholar] [CrossRef] [PubMed]
- Du, H.; Guo, Y.; Bennett, D.A.; Bragg, F.; Bian, Z.; Chadni, M.; Yu, C.; Chen, Y.; Tan, Y.; Millwood, I.Y.; et al. Red Meat, Poultry and Fish Consumption and Risk of Diabetes: A 9 Year Prospective Cohort Study of the China Kadoorie Biobank. Diabetologia 2020, 63, 767–779. [Google Scholar] [CrossRef]
- Würtz, A.M.L.; Jakobsen, M.U.; Bertoia, M.L.; Hou, T.; Schmidt, E.B.; Willett, W.C.; Overvad, K.; Sun, Q.; Manson, J.E.; Hu, F.B.; et al. Replacing the Consumption of Red Meat with Other Major Dietary Protein Sources and Risk of Type 2 Diabetes Mellitus: A Prospective Cohort Study. Am. J. Clin. Nutr. 2021, 113, 612–621. [Google Scholar] [CrossRef]
- Borgi, L.; Curhan, G.C.; Willett, W.C.; Hu, F.B.; Satija, A.; Forman, J.P. Long-Term Intake of Animal Flesh and Risk of Developing Hypertension in Three Prospective Cohort Studies. J. Hypertens. 2015, 33, 2231–2238. [Google Scholar] [CrossRef]
- Golzarand, M.; Bahadoran, Z.; Mirmiran, P.; Azizi, F. Protein Foods Group and 3-Year Incidence of Hypertension: A Prospective Study From Tehran Lipid and Glucose Study. J. Ren. Nutr. 2016, 26, 219–225. [Google Scholar] [CrossRef]
- Vergnaud, A.-C.; Norat, T.; Romaguera, D.; Mouw, T.; May, A.M.; Travier, N.; Luan, J.; Wareham, N.; Slimani, N.; Rinaldi, S.; et al. Meat Consumption and Prospective Weight Change in Participants of the EPIC-PANACEA Study. Am. J. Clin. Nutr. 2010, 92, 398–407. [Google Scholar] [CrossRef]
- Smith, J.D.; Hou, T.; Ludwig, D.S.; Rimm, E.B.; Willett, W.; Hu, F.B.; Mozaffarian, D. Changes in Intake of Protein Foods, Carbohydrate Amount and Quality, and Long-Term Weight Change: Results from 3 Prospective Cohorts. Am. J. Clin. Nutr. 2015, 101, 1216–1224. [Google Scholar] [CrossRef]
- Hajihashemi, P.; Hassannejad, R.; Haghighatdoost, F.; Mohammadifard, N.; Sadeghi, M.; Roohafza, H.; Sajjadi, F.; Sarrafzadegan, N. The Long-Term Association of Different Dietary Protein Sources with Metabolic Syndrome. Sci. Rep. 2021, 11, 19394. [Google Scholar] [CrossRef]
- Riseberg, E.; Lopez-Cepero, A.; Mangano, K.M.; Tucker, K.L.; Mattei, J. Specific Dietary Protein Sources Are Associated with Cardiometabolic Risk Factors in the Boston Puerto Rican Health Study. J. Acad. Nutr. Diet. 2022, 122, 298–308.e3. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, D.-Z. Red Meat, Poultry, and Egg Consumption with the Risk of Hypertension: A Meta-Analysis of Prospective Cohort Studies. J. Hum. Hypertens. 2018, 32, 507–517. [Google Scholar] [CrossRef] [PubMed]
- FoodData Central. Available online: https://fdc.nal.usda.gov/fdc-app.html#/ (accessed on 11 November 2022).
- Hu, F.B.; Rimm, E.; Smith-Warner, S.A.; Feskanich, D.; Stampfer, M.J.; Ascherio, A.; Sampson, L.; Willett, W.C. Reproducibility and Validity of Dietary Patterns Assessed with a Food-Frequency Questionnaire. Am. J. Clin. Nutri. 1999, 69, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Tucker, K.L.; Bianchi, L.A.; Maras, J.; Bermudez, O.I. Adaptation of a Food Frequency Questionnaire to Assess Diets of Puerto Rican and Non-Hispanic Adults. Am. J. Epidemiol. 1998, 148, 507–518. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; An, P.; Wang, H.; Wang, X.; Shen, X.; Li, X.; Min, J.; Liu, S.; Wang, F. Dietary Intake of Heme Iron and Risk of Cardiovascular Disease: A Dose-Response Meta-Analysis of Prospective Cohort Studies. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Han, M.; Guan, L.; Ren, Y.; Zhao, Y.; Liu, D.; Zhang, D.; Liu, L.; Liu, F.; Chen, X.; Cheng, C.; et al. Dietary Iron Intake and Risk of Death Due to Cardiovascular Diseases: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Asia Pac. J. Clin. Nutr. 2020, 29, 309–321. [Google Scholar] [CrossRef]
- Micha, R.; Michas, G.; Lajous, M.; Mozaffarian, D. Processing of Meats and Cardiovascular Risk: Time to Focus on Preservatives. BMC Med. 2013, 11, 136. [Google Scholar] [CrossRef]
- Marshall, S.; Petocz, P.; Duve, E.; Abbott, K.; Cassettari, T.; Blumfield, M.; Fayet-Moore, F. The Effect of Replacing Refined Grains with Whole Grains on Cardiovascular Risk Factors: A Systematic Review and Meta-Analysis of Randomized Controlled Trials with GRADE Clinical Recommendation. J. Acad. Nutr. Diet. 2020, 120, 1859–1883.e31. [Google Scholar] [CrossRef]
- Sawicki, C.M.; Jacques, P.F.; Lichtenstein, A.H.; Rogers, G.T.; Ma, J.; Saltzman, E.; McKeown, N.M. Whole- and Refined-Grain Consumption and Longitudinal Changes in Cardiometabolic Risk Factors in the Framingham Offspring Cohort. J. Nutr. 2021, 151, 2790–2799. [Google Scholar] [CrossRef]
- Hartley, L.; Igbinedion, E.; Holmes, J.; Flowers, N.; Thorogood, M.; Clarke, A.; Stranges, S.; Hooper, L.; Rees, K. Increased Consumption of Fruit and Vegetables for the Primary Prevention of Cardiovascular Diseases. Cochrane Database Syst. Rev. 2013, 6, CD009874. [Google Scholar] [CrossRef]
- White, D.L.; Collinson, A. Red Meat, Dietary Heme Iron, and Risk of Type 2 Diabetes: The Involvement of Advanced Lipoxidation Endproducts12. Adv. Nutr. 2013, 4, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Alderman, M.H. Evidence Relating Dietary Sodium to Cardiovascular Disease. J. Am. Coll. Nutr. 2006, 25, 256S–261S. [Google Scholar] [CrossRef] [PubMed]
- Farquhar, W.B.; Edwards, D.G.; Jurkovitz, C.T.; Weintraub, W.S. Dietary Sodium and Health: More Than Just Blood Pressure. J. Am. Coll. Cardiol. 2015, 65, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Zong, G.; Wu, K.; Hu, Y.; Li, Y.; Willett, W.C.; Eisenberg, D.M.; Hu, F.B.; Sun, Q. Meat Cooking Methods and Risk of Type 2 Diabetes: Results From Three Prospective Cohort Studies. Diabetes Care 2018, 41, 1049–1060. [Google Scholar] [CrossRef] [PubMed]
- Horrigan, L.; Lawrence, R.S.; Walker, P. How Sustainable Agriculture Can Address the Environmental and Human Health Harms of Industrial Agriculture. Environ. Health Perspect. 2002, 110, 445–456. [Google Scholar] [CrossRef] [PubMed]
- The EAT-Lancet Commission on Food, Planet, Health–EAT Knowledge. Available online: https://eatforum.org/eat-lancet-commission/ (accessed on 11 November 2022).
- Joober, R.; Schmitz, N.; Annable, L.; Boksa, P. Publication Bias: What Are the Challenges and Can They Be Overcome? J. Psychiatry Neurosci. 2012, 37, 149–152. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).