Abstract
The coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is spreading rapidly around the world and has led to millions of infections and deaths. Growing evidence indicates that iron metabolism is associated with COVID-19 progression, and iron-related biomarkers have great potential for detecting these diseases. However, the results of previous studies are conflicting, and there is not consistent numerical magnitude relationship between those biomarkers and COVID-19. Thereby, we aimed to integrate the results of current studies and to further explore their relationships through a meta-analysis. We searched peer-reviewed literature in PubMed, Scopus and Web of Science up to 31 May 2022. A random effects model was used for pooling standard mean difference (SMD) and the calculation of the corresponding 95% confidence interval (CI). I2 was used to evaluate heterogeneity among studies. A total of 72 eligible articles were included in the meta-analysis. It was found that the ferritin levels of patients increased with the severity of the disease, whereas their serum iron levels and hemoglobin levels showed opposite trends. In addition, non-survivors had higher ferritin levels (SMD (95%CI): 1.121 (0.854, 1.388); Z = 8.22 p for Z < 0.001; I2 = 95.7%, p for I2 < 0.001), lower serum iron levels (SMD (95%CI): −0.483 (−0.597, −0.368), Z = 8.27, p for Z < 0.001; I2 = 0.9%, p for I2 =0.423) and significantly lower TIBC levels (SMD (95%CI): −0.612 (−0.900, −0.324), Z = 4.16, p for Z < 0.001; I2 = 71%, p for I2 = 0.016) than survivors. This meta-analysis demonstrates that ferritin, serum iron, hemoglobin and total iron banding capacity (TIBC) levels are strongly associated with the risk, severity and mortality of COVID-19, providing strong evidence for their potential in predicting disease occurrence and progression.
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1], has become a global pandemic, resulting in 525,646,754 confirmed cases and 6,299,346 deaths as of 31 May 2020 [2,3]. The rapid spread of this disease has put enormous pressure on local medical institutions and their finances. Thus, it is very critical to identify and prevent the spread of COVID-19 early.
The clinical manifestations of COVID-19 are various, from asymptomatic infection to death. Therefore, it is very necessary to find a reliable early biomarker to identify the emergence and progression of disease [3,4]. Numerous studies indicated that iron distribution was closely linked to the onset and progression of COVID-19. In the process of viral pathogen invasion, the defense system is very crucial [5], especially the immune system, which relies on the supply of micronutrients. Iron is not only an important component of micronutrients, but also plays an important role in various fundamental biological processes between human and pathogen, ranging from deoxyribonucleic acid (DNA) synthesis to adenosine triphosphate (ATP) generation [6,7]. Furthermore, some symptoms of COVID-19, such as pneumonia, thrombo-embolism and acute respiratory distress syndrome (ARDS), are also related to iron by its functions in the immune system and circulatory system. Therefore, the application of iron-related biomarkers in identifying infection and severity in COVID-19 patients has attracted widespread attention.
Though serum or plasma iron is a main indicator for iron homeostasis, ferritin, hemoglobin, hepcidin, TIBC and transferrin saturation (TSAT) would explain iron distribution more roundly. Previous studies have investigated the relationships among iron, ferritin, hemoglobin, hepcidin, TIBC, TSAT and COVID-19, but their results are conflicting and inconsistent. Most studies about serum iron have shown that lower iron levels are found in more at-risk groups, such as non-survivors compared to survivors [8,9,10,11,12,13], severe disease groups compared to non-severe disease groups [10,13,14,15,16] and cases to controls [10,16,17,18,19,20,21], whereas others expressed the opposite results [7,22,23]. In all relevant studies, the hemoglobin levels were found to be lower in severe groups than those in controls [7,10,24] or non-severe groups [22,25,26,27,28,29]. However, in the comparisons between severity [7,10,15,17,18,19,23,24,30,31,32,33,34,35,36,37] and mortality [10,30,38,39,40,41], there was not a consistent numerical magnitude relationship between them. In addition, studies on TIBC [8,10,12,13] and TSAT [8,13] only refer to mortality. Most of those studies found lower levels in non-survivor groups, except for one about TSAT [10]. Lower levels of hepcidin in cases than controls was documented in a study [10], whereas the other studies reported an inverse result [18,20,24]. Unusually, more dangerous groups had higher ferritin levels in almost all relevant comparisons [4,6,10,11,12,13,14,15,17,18,19,20,21,22,24,25,26,27,28,29,30,32,34,35,36,37,38,39,40,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72].
Considering that any individual study may not have the sufficient power to obtain a reliable conclusion, this meta-analysis was conducted to: (1) Summarize and evaluate the results of numerous papers on the relationships between serum iron, ferritin, hemoglobin, TIBC, TSAT and hepcidin levels and the mortality and clinical severity of SARS-CoV-2 patients. (2) Assess the potential between-study heterogeneity; and eventually investigate the potential publication bias.
2. Materials and Methods
2.1. Literature Search and Data Selection Criteria
Our meta-analysis searched peer-reviewed literature on PubMed [73], Web of Science [74] and Scopus [75] up to May 2022 published in English. Our keyword combinations included (Fe OR iron OR ferritin) AND (COVID-19 OR human coronavirus disease 2019 OR SARS-CoV-2 OR severe acute respiratory syndrome coronavirus 2). Moreover, in order to identify extra studies which were not included by databases, we reviewed the references of all searched literature.
2.2. Data Selection Criteria
Articles were included based on the following four criteria: (1) the cases had COVID-19; (2) observational study design; (3) samples were from blood; (4) data were reported as mean ± standard deviation (SD) or the other forms could be translated to mean ± SD. Some studies were excluded if they were: (1) experimental studies (2) reviews.
If the data were duplicated in one study, only the one that involved the largest number of cases was included. Two investigators searched for the articles and extracted data independently. The disagreements about eligibility of an article were settled by discussion.
2.3. Data Extraction
On each article, the following information and data were recorded: the first author, county (continent), publication year, study design, disease assessment, outcome groups, gender, mean age, number of cases, number of controls, number of non-survivors, number of survivors, numbers of severe and non-severe cases, mean ± SD of these groups and data units. If just standard error mean (SEM) was available, SD was calculated by the formula SEM = SD/. If there were available median and interquartile range, mean and SD were to be calculated using the website [76].
2.4. Statistical Analyses
The meta-analysis was performed using the software Stata 15.0 (Stata Corporation, College Station, TX, USA). In order to estimate the association between serum-iron-related biomarkers and the onset and progression of COVID-19, we used the standard mean difference (SMD) with the corresponding 95% confidence interval (CI) as the effect size. The SMD is the ratio of the mean difference to the pooled standard deviation. I2 was used to assess the heterogeneity among studies. For the purpose of pooling effect sizes and all the analyses, we used a random effects model. All reported probabilities (p-values) were two-sided, and p < 0.05 was recognized as statistically significant. If meta-regression demonstrated sources of heterogeneity in continent, publication year, study design and subgroup analyses were performed.
3. Results
3.1. Characteristics of Studies
After the preliminary search, 6916 articles were identified, 2040 from PubMed, 1390 from Web of Science and 3486 from Scopus (Figure 1). After screening the duplicated and irrelative articles, 157 articles were included. Among them, 85 articles were further excluded because: six were mechanism research; the data of 16 were not analyzable; 25 expressed the data in odds ratios, relative risks or correlation coefficients; 16 were systematic reviews; and 22 were experimental studies. Eventually, a total of 72 eligible articles were involved in this meta-analysis: 17 were case–control studies, 20 studies were cohort studies and 35 were cross-sectional studies. (Table 1)
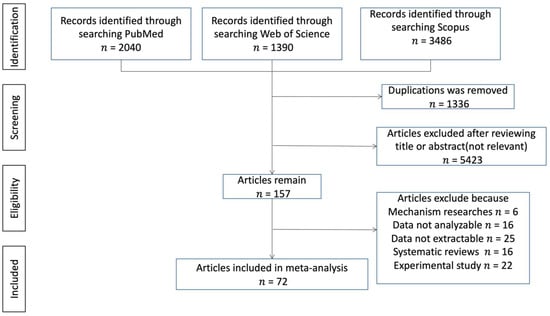
Figure 1.
Flow diagram of the literature search.

Table 1.
Characteristics of 72 included studies of iron-related biomarkers.
3.2. Ferritin Level and COVID-19
A total of twenty-nine studies assessed the connections between ferritin levels and the mortality of SARS-CoV-2 patients in this meta-analysis, involving 2131 non-survivors and 7813 survivors. The ferritin levels were significantly higher in the dead patients than that in survivors (SMD (95%CI): 1.121 (0.854, 1.388); Z = 8.22 p for Z < 0.001; I2 = 95.7%, p for I2 < 0.001; Table 2, Figure 2). A subgroup analysis by publication year indicated that the dead had higher ferritin levels in 2020 (SMD (95%CI): 1.881 (1.137, 2.625); Figure S1), 2021 (SMD (95%CI): 0.847 (0.575, 1.119)), and 2022 (SMD (95%CI): 0.550 (0.393, 0.707); Figure S1). More details about subgroup analysis are in Table 2.

Table 2.
Subgroup analyses of studies on the associations of iron-related biomarkers with mortality in SARS-CoV-2 patients.
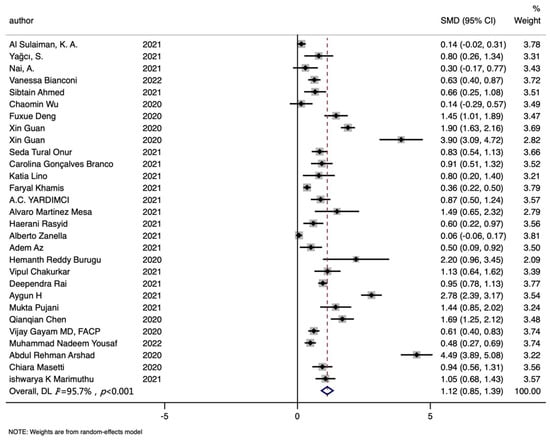
Figure 2.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CIs) of studies [8,10,11,12,13,30,38,39,40,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64] on ferritin levels in non-survivors and survivors. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
Seventeen studies about ferritin were included in the COVID-19 risk analysis, including 964 cases and 966 controls. The overall comparison demonstrated that cases had higher ferritin levels than controls (SMD (95%CI): 1.383 (0.792, 1.975); Z = 4.58 p for Z < 0.001; I2 = 96.3%, p for I2 < 0.001; Table 3, Figure 3). In the subgroup analysis by study type, higher ferritin levels were found in cases compared with controls about risk analysis (SMD (95%CI): 0.872 (0.443, 1.300); Figure S1). More detailed records of subgroup analysis are shown in Table 3.

Table 3.
Subgroup analyses of studies on the associations of iron-related biomarkers with severity in SARS-CoV-2 patients.
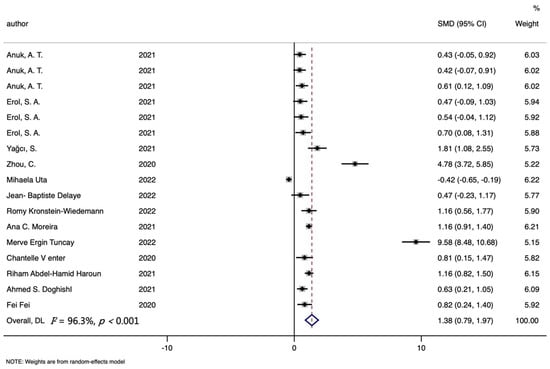
Figure 3.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CI) of studies [10,17,18,19,20,21,24,36,37,42,43,44,72] on ferritin levels in COVID-19 cases and controls. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
In terms of the relationship between ferritin and the severity of COVID-19, a total of thirty-nine studies were included, involving 1681 severe, 1337 non-severe, 433 moderate and 1416 mild individuals. The results reported that the ferritin levels of severe groups were higher than those of the non-severe groups (SMD (95%CI): 0.864 (0.389, 1.338); Z = 3.57 p for Z < 0.001; I2 = 96.00%, p for I2 < 0.001; Table 3, Figure S2) and mild groups (SMD (95%CI): 1.414 (0.995, 1.834); Z = 6.61 p for Z < 0.001; I2 = 92.7%, p for I2 < 0.001; Table 3, Figure S2). In addition, a significant difference was also observed between moderate groups and mild groups (SMD (95%CI): 1.551 (0.535, 2.566); Z = 2.99 p for Z = 0.003; I2 = 97.2%, p for I2 < 0.001; Table 3, Figure S2). The subgroup analysis based on publication year indicated that similar association was found in 2020 (SMD (95%CI): 2.802 (0.678, 4.925); Figure S1) and in 2021(SMD (95%CI): 0.400 (0.207, 0.592); Figure S1). With regard to continent, significant differences were found among Asia (SMD (95%CI): 0.976 (0.362, 1.591); Figure S1), Europe (SMD (95%CI): 0.581 (0.259, 0.903); Figure S1) and Africa (SMD (95%CI): 5.319 (4.718, 5.920); Figure S1). More details were described in Table 3.
3.3. Serum or Plasma Iron Level and COVID-19
A total of seven studies included analyses of serum iron levels and the mortality of SARS-CoV-2 patients, involving 456 non-survivors and 1508 survivors. The serum iron level in dead patients was significantly lower than that in alive patients (SMD (95%CI): −0.483 (−0.597, −0.368), Z = 8.27, p for Z < 0.001; I2 = 0.9%, p for I2 =0.423; Table 2, Figure 4).
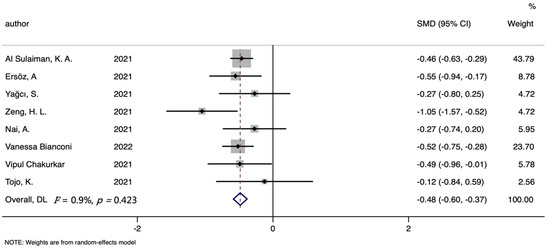
Figure 4.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CIs) of studies [7,8,9,10,11,12,13,22] on serum iron levels in non-survivors and survivors. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
Seven studies were included in the serum iron and COVID-19 risk meta-analysis, including 492 cases and 704 controls. Figure 5 showed that lower serum iron levels were found in cases than controls (SMD (95%CI): −1.384 (−2.175, −0.592); Z = 3.43 p for Z = 0.001; I2 = 96.7%, p for I2 < 0.001; Table 3). In the subgroup analysis by continent, the same difference was discovered between Asia (SMD (95%CI): −3.403 (−5.974, −0.832); Figure S1) and Europe (SMD (95%CI): −0.580 (−0.791, −0.370); Figure S1). More details are described in Table 3.
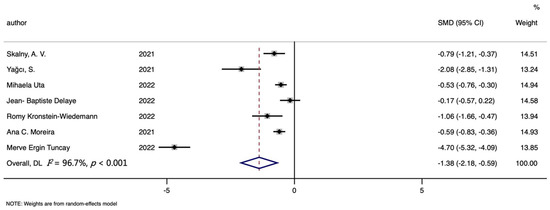
Figure 5.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CIs) of studies [10,16,17,18,19,20,21] on serum iron levels in COVID-19 cases and controls. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
A total of ten studies were included in the analysis of the relationship between the severity of COVID-19 and serum iron, involving 298 severe, 113 mild and 340 non-severe patients. Severe groups had lower iron levels than the mild groups (SMD (95%CI): −0.293 (−0.561, −0.024); Z = 2.13 p for Z = 0.033; I2 = 0.00%, p for I2 =0.545; Table 3, Figure S2) and non-severe groups (SMD (95%CI): −1.144 (−2.060, −0.227); Z = 2.45 p for Z = 0.014; I2 = 94.2%, p for I2 < 0.001; Table 3, Figure S2).
3.4. Hemoglobin Level and COVID-19
Regarding the connection between hemoglobin level and the mortality of COVID-19, a total of six studies were included, involving 276 the deceased and 1029 survivors. However, no significant differences were found between the hemoglobin levels of dead and recovered patients (SMD (95%CI): −0.186 (−0.571, 0.198), Z = 0.95, p for Z = 0.343; I2 = 82.5%, p for I2 < 0.001; Table 2, Figure 6). In addition, the subgroup analysis based on publication year indicated lower hemoglobin levels in the dead in 2021 (SMD (95%CI): −0.632 (−1.070, −0.194); Figure S1). More details about subgroup analysis are summarized in Table 2.
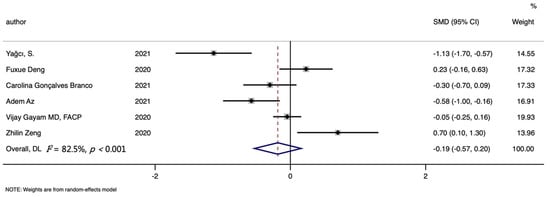
Figure 6.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CIs) of studies [10,30,38,39,40,41] on hemoglobin levels in non-survivors and survivors. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
Seven studies were included in the hemoglobin level and COVID-19 risk meta-analysis, involving 367 cases and 511 controls. Figure 7 showed that lower hemoglobin levels were found in cases than controls (SMD (95%CI): −0.612 (−0.159, −0.065); Z = 2.19 p for Z = 0.028; I2 = 87.9%, p for I2 < 0.001; Table 3).
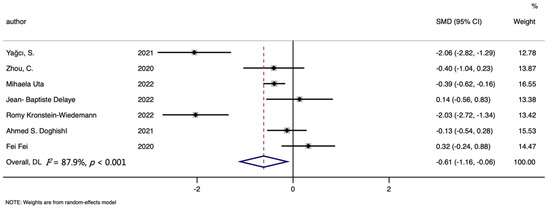
Figure 7.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CIs) of studies [10,17,18,19,24,36,37] on hemoglobin levels in COVID-19 cases and controls. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
In terms of the analysis of severity, a total of twenty studies were included, including 1060 severe, 524 mild and 851 non-severe individuals. Though the difference between severe and mild groups (SMD (95%CI): −0.073 (−0.209, 0.064); Z = 1.040 p for Z = 0.298; I2 = 5.80%, p for I2 =0.386; Table 3) was not significant, the results demonstrated lower hemoglobin levels were found in severe groups than that in non-severe groups (SMD (95%CI): −0.394 (−0.703, −0.086); Z = 2.500 p for Z = 0.012; I2 = 86.50%, p for I2 < 0.001; Table 3, Figure S2).
3.5. Hepcidin Level and COVID-19
A total of three studies on the relationships between hepcidin and the mortality of COVID-19 were included in this meta-analysis, including 66 non-survivors and 224 survivors. Dead patients had slightly higher hepcidin levels than recovered patients, but this was not significant (SMD (95%CI): 0.447 (−0.287, 1.182); Z = 1.190 p for Z = 0.232; I2 = 84.8%, p for I2 =0.001; Table 2, Figure 8).
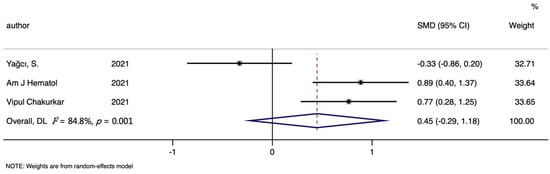
Figure 8.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CIs) of studies [10,11,13] on hepcidin levels in non-survivors and survivors. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
The analysis of COVID-19 risk included four studies totally, with 177 cases and 261 controls. Though higher hepcidin level was found in cases than that in controls, the difference was not significant (SMD (95%CI): 0.750 (−0.805, 2.306); Z = 0.95 p for Z = 0.345; I2 = 96.40%, p for I2 < 0.001; Table 3, Figure 9).
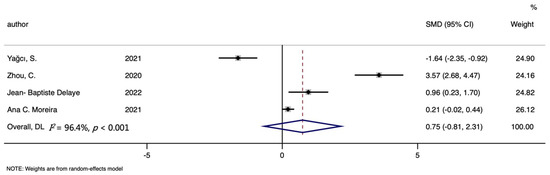
Figure 9.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CIs) of studies [10,18,20,24] on hepcidin levels in COVID-19 cases and controls. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
3.6. TIBC, TSAT and the Mortality of COVID-19
Four studies about TIBC were included in the analyses of mortality, including 382 non-survivors and 719 survivors. Analyses about TSAT involved three studies, 281 non-survivors and 458 survivors totally. The TIBC level was significantly lower in the death group than in the survivors group (SMD (95%CI): −0.612 (−0.900, −0.324), Z = 4.16, p for Z < 0.001; I2 = 71%, p for I2 = 0.016; Table 2, Figure 10). In addition, no significant differences were found in all analyses of TSAT (SMD (95%CI): −0.112 (−0.455, 0.231), Z = 0.64, p for Z = 0.521; I2 = 59.6%, p for I2 = 0.084; Table 2, Figure 11).
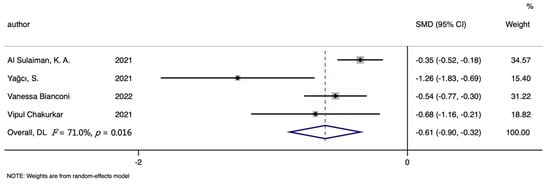
Figure 10.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CIs) of studies [8,10,12,13] on TIBC levels in non-survivors and survivors. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
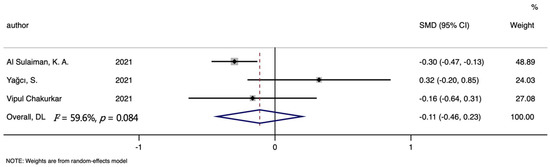
Figure 11.
Forest plot of standard mean difference (SMD) with corresponding 95% confidence intervals (CIs) of studies [8,10,13] on TSAT levels in non-survivors and survivors. The solid diamond and horizontal line represent the study-specific effect and 95%CI, respectively; the size of the grey square is positively correlated with the weight distributed to each study in the meta-analysis. The center of open diamond with the vertical dashed line expresses the pooled SMD, and the width expresses the pooled 95%CI.
3.7. Sources of Heterogeneity and Publication Bias
Strong evidence of heterogeneity among studies was documented for the relationships between these iron-related biomarkers and mortality, clinical severity or risk in SARS-CoV-2 patients. The heterogeneity for the between-study was explored through the univariate meta-regression with the covariates of continent, gender, study types, years, ages and numbers of samples in the analysis. Meta-regression indicated that 75.02% of the heterogeneity in the COVID-19 risk analysis in serum iron was explained by continent. In terms of ferritin, publication year and sample size of the death group explained 18.33% and 14.78% of the heterogeneity of the mortality analysis, respectively; study type contributed 21.04% of the heterogeneity of overall analysis; and publication year contributed 20.33% of the heterogeneity of the severe–mild comparison. In addition, publication year and continent explained 46.95% and 46.09% of the heterogeneity of the moderate–mild analysis in ferritin, respectively. Regarding the heterogeneity of hemoglobin and mortality analysis, publication year accounted for 69.79%.
Considering the potential small-study effects, Galbraith plot showed the contribution of results from the different relevant studies to the heterogeneity. Then the “leave- one-out” sensitivity analyses used I2 > 50% as the criterion to evaluate the robustness of conclusion of ferritin. Twelve studies [8,38,47,48,51,55,57,58,59,60,62] on mortality (Figure 12) and four [17,20,21,24] studies on risk (Figure 13) were found to be the main reasons for the high heterogeneity. After excluding these studies, low heterogeneity and robust results without the small-study effect were demonstrated for mortality (SMD = 0; Z = 7.47; p < 0.001; I2 = 44.2%) and risk (SMD = 0; Z = 7.39; p < 0.001; I2 = 44.8%) analyses of ferritin.
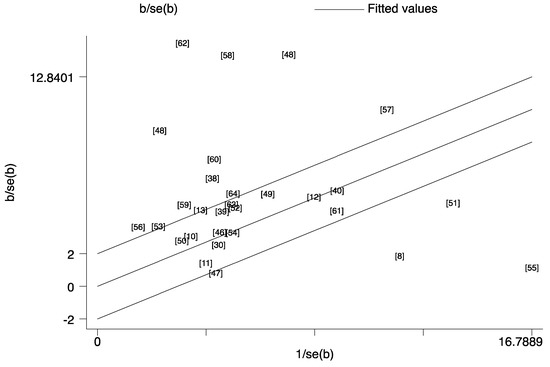
Figure 12.
Galbraith plot for the contribution of results from the different studies [8,10,11,12,13,30,38,39,40,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,] about mortality for ferritin to the heterogeneity. This analysis was based on the relevant data listed in Table 1 and the number orders in the plot were same to the reference list.
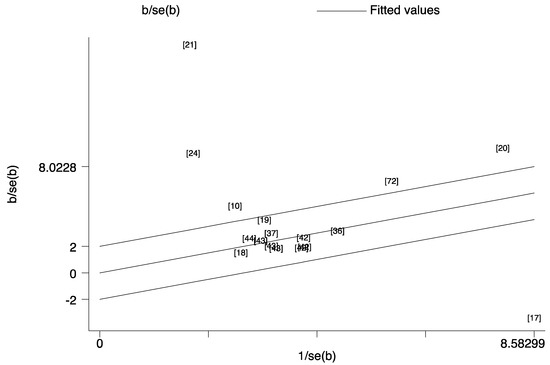
Figure 13.
Galbraith plot for the contribution of results from the different studies [10,17,18,19,20,21,24,36,37,42,43,44,72] about risk for ferritin to the heterogeneity. This analysis was based on the relevant data listed in Table 1 and the number orders in the plot were same to the reference list.
The results of sensitivity analysis indicated that no individual study had an excessive influence on the pooled measure for all comparisons (Figures S3–S5). Egger’s test reported no publication bias in mortality analysis (p = 0.930) or risk analysis (p = 0.129) of serum iron. However, the risk (p = 0.009) and mortality analyses (p < 0.001) of ferritin had significant publication bias. In terms of hemoglobin, Egger’s test demonstrated no publication bias in the analyses of mortality (p = 0.700) and risk (p = 0.483). Publication bias in mortality analyses of TIBC (p = 0.077) and TSAT (p = 0.358) was also not found. Moreover, no publication bias was found in the mortality (p = 0.065) and risk analyses (p = 0.699) of hepcidin.
4. Discussion
Our meta-analysis was based on 72 articles, containing 148 studies, of which 85 were about ferritin, 22 were about serum iron, 27 were about hemoglobin, 7 were about hepcidin, 3 were about TSAT and 4 were about TIBC. Mortality analyses included 29 studies on ferritin, 8 on serum iron, 6 on hemoglobin, 3 on hepcidin, 4 on TIBC and 3 on TSAT. Our results indicated that the serum iron and TIBC levels of the deceased were significantly lower than those of the survivors, but higher ferritin levels were found in the deceased. In terms of hemoglobin, hepcidin and TSAT, we did not find an association with death outcome. The risk analyses included 17 articles on ferritin, 7 on serum iron, 7 on hemoglobin and 4 on hepcidin. It was shown that cases had lower serum iron and hemoglobin levels, but higher ferritin levels than controls. There were not significant results in hepcidin analyses. Regarding the analyses of clinical severity, 39 studies on ferritin, 14 on hemoglobin and 7 on serum iron were included. All of them were found to be related to the severity of COVID-19.
According to previous studies, excessive inflammation is a characteristic of COVID-19 [82]. Iron plays an essential role in this process [9]. Serum iron, ferritin, hemoglobin, hepcidin, TIBC and TSAT represent the iron levels in the body; however, some of them have other important physiological functions.
Hepcidin is a main regulatory factor of iron metabolism that is associated with body iron level [83,84]. However, we did not observe significant links between that and COVID-19 onset or progression because of the limited numbers of studies. Differently from us, Denggao Peng et al. [85] classified the groups based on the clinical findings and reported that the hepcidin levels of severe COVID-19 cases were higher than those of non-severe cases. It is common that hepcidin is upregulated after a viral infection, especially for the COVID-19 patients with inflammation [86]. Moreover, thanks to this special change, hepcidin binds to ferroprotein and accelerates its degradation, so that iron uptake decreases and the iron storage in macrophages increases [87], influencing SARS-COV-2.
Ferritin is also recognized as an acute phase reactant of inflammation, influenced by the presence of iron, hepcidin [46,50,88,89,90] and pro-inflammatory cytokines. Inflammation promotes ferritin synthesis and release in the liver [91,92]. Moreover, ferritin also is the storage form of iron in macrophages, explaining the decrease in serum iron [93,94,95]. Henry et al. [90] found the associations between ferritin and COVID-19 severity. Similarly, we further documented the differences between their associations with COVID-19 risk and mortality. Though serum iron is an important indicator of disease, it cannot accurately represent the iron level because of the various related forms in the human body. Serum iron is essential for both humans and viruses [96,97,98]. In order to deprive SARS-CoV-2 of iron and support immunity, macrophages intake more iron, and the intestinal tract absorbs less, leading to a decrease in serum iron [81,82]. In addition, a study by Ehsani [99] reported a structural similarity between the hepcidin protein and the spiked glycoprotein cytoplasmic tail of SARS-CoV-2. This indicates that SARS-CoV-2 can simulate hepcidin’s action, contributing to the decreased serum iron [100]. A decreased hemoglobin level is usually a symbol of anemia, caused by decreased serum iron. TSAT reflects serum iron availability and is frequently used in clinical practice to detect states of iron deficiency or iron overload [101,102].
In meta-analysis, between-study heterogeneity is common. Thus, exploring the sources of between-study heterogeneity is essential. We performed univariate meta-regression, with covariables such as continent, study type, publication year and sample size. The regression results explained part of the heterogeneity in our meta-analysis, but there was still some heterogeneity not being detected. In addition, the Galbraith analysis indicated that high heterogeneity in ferritin resulted from twelve mortality analysis studies and five risk analysis studies. After excluding these studies, low heterogeneity and robust results without small-study effect were documented. However, the final results of ferritin were not changed.
There were some strengths in our meta-analysis: First of all, as far as we know, our study has unified a large number of studies on the associations of iron-related biomarkers with risk, clinical severity and mortality in COVID-19 patients, avoiding inaccurate conclusions of individual studies. More importantly, the random effects were used to estimate the pooled SMD. Thus, it was still possible to draw convincing results though the inconsistent measurement conditions and units for iron-related biomarkers in different studies.
However, our study has several limitations. Firstly, high heterogeneity was found in almost all indicator analyses, but some of analytical results were not explained by meta-regression or subgroup analysis. We cannot get a more accurate evaluation for the sources of the heterogeneity due to the lack of corresponding study-level covariates in the reported articles. Moreover, the differences in iron-related biomarkers’ reference values between females and males illustrated the importance of gender for our study. However, we could not conduct meta-analysis including gender for the reason that there was not enough information about it.
5. Conclusions
Our meta-analysis showed that the levels of serum iron and TIBC in dead patients were significantly lower than in survivors, and the ferritin level was higher in death groups than in survivors, whereas the relationship between hemoglobin and mortality was not significant. Moreover, serum iron and hemoglobin levels were lower in cases and negatively correlated with the severity; on the contrary, ferritin level was higher in cases. In addition, no statistically significant results were found in the hepcidin and TSAT levels of the severity and mortality groups. That was possibly due to the limited number of studies.
In conclusion, we found that ferritin, serum iron, hemoglobin and TIBC levels are closely associated with the risk, severity or mortality of COVID-19. These results provide strong evidence for the applications of iron-related biomarkers in the prediction of the COVID-19 occurrence and development. Moreover, lower serum iron and hemoglobin levels could provide clues for explaining the deteriorated process of COVID-19. However, future studies are needed to further confirm these results in future research.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14163406/s1, Table S1: Quality assessment of studies included in the meta-analysis, Figure S1: Forest plot of standard mean difference (SMD) with corresponding 95% confidence interval (CI) of studies on iron-related biomarkers levels about severity meta-analysis, Figure S2: Forest plot of standard mean difference (SMD) with corresponding 95% confidence interval (CI) of studies on subgroup analysis by publication year, continent and study type, Figure S3: The influence analysis results of iron-related biomarkers levels about mortality meta-analysis, Figure S4: The influence analysis results of iron-related biomarkers levels about risk meta-analysis, Figure S5: The influence analysis results of iron-related biomarkers levels about severity meta-analysis.
Author Contributions
Conceptualization: S.L.; methodology: S.Z., H.L. and S.L.; formal analysis: S.Z. and H.L.; investigation: S.Z. and H.L.; resources: S.Z. and H.L.; data curation: S.Z. and H.L.; writing—original draft preparation: S.Z. and H.L.; writing—review and editing, S.Z. and H.L.; project administration: S.Z. and H.L; and funding acquisition: S.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. And The APC was funded by S.L.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used in this review come from published articles, all of which are identified in the references. The data used in the meta-analysis have been provided in the tables.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Karakaya Molla, G.; Ünal Uzun, Ö.; Koç, N.; Özen Yeşil, B.; Bayhan, G. Evaluation of nutritional status in pediatric patients diagnosed with COVID-19 infection. Clin. Nutr. ESPEN 2021, 44, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Shakeri, H.; Azimian, A.; Ghasemzadeh-Moghaddam, H.; Safdari, M.; Haresabadi, M.; Daneshmand, T.; Namdar Ahmadabad, H. Evaluation of the relationship between serum levels of zinc, vitamin B12, vitamin D, and clinical outcomes in patients with COVID-19. J. Med. Virol. 2022, 94, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Dahan, S.; Segal, G.; Katz, I.; Hellou, T.; Tietel, M.; Bryk, G.; Amital, H.; Shoenfeld, Y.; Dagan, A. Ferritin as a Marker of Severity in COVID-19 Patients: A Fatal Correlation. Isr. Med. Assoc. J. 2020, 22, 494–500. [Google Scholar]
- Zhou, P.; Yang, X.L.; Wang, X.G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.R.; Zhu, Y.; Li, B.; Huang, C.L.; et al. Addendum: A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 588, E6. [Google Scholar] [CrossRef]
- Lv, Y.; Chen, L.; Liang, X.; Liu, X.; Gao, M.; Wang, Q.; Wei, Q.; Liu, L. Association between iron status and the risk of adverse outcomes in COVID-19. Clin. Nutr. 2021, 40, 3462–3469. [Google Scholar] [CrossRef]
- Tojo, K.; Sugawara, Y.; Oi, Y.; Ogawa, F.; Higurashi, T.; Yoshimura, Y.; Miyata, N.; Hayami, H.; Yamaguchi, Y.; Ishikawa, Y.; et al. The U-shaped association of serum iron level with disease severity in adult hospitalized patients with COVID-19. Sci. Rep. 2021, 11, 13431. [Google Scholar] [CrossRef]
- Al Sulaiman, K.A.; Aljuhani, O.; Eljaaly, K.; Alharbi, A.A.; Al Shabasy, A.M.; Alsaeedi, A.S.; Al Mutairi, M.; Badreldin, H.A.; Al Harbi, S.A.; Al Haji, H.A.; et al. Clinical features and outcomes of critically ill patients with coronavirus disease 2019 (COVID-19): A multicenter cohort study. Int. J. Infect. Dis. 2021, 105, 180–187. [Google Scholar] [CrossRef]
- Ersöz, A.; Yılmaz, T.E. The association between micronutrient and hemogram values and prognostic factors in COVID-19 patients: A single-center experience from Turkey. Int. J. Clin. Pract. 2021, 75, e14078. [Google Scholar] [CrossRef]
- Yağcı, S.; Serin, E.; Acicbe, Ö.; Zeren, M.; Odabaşı, M.S. The relationship between serum erythropoietin, hepcidin, and haptoglobin levels with disease severity and other biochemical values in patients with COVID-19. Int. J. Lab. Hematol. 2021, 43 (Suppl. 1), 142–151. [Google Scholar] [CrossRef]
- Nai, A.; Lorè, N.I.; Pagani, A.; De Lorenzo, R.; Di Modica, S.; Saliu, F.; Cirillo, D.M.; Rovere-Querini, P.; Manfredi, A.A.; Silvestri, L. Hepcidin levels predict COVID-19 severity and mortality in a cohort of hospitalized Italian patients. Am. J. Hematol. 2021, 96, e32–e35. [Google Scholar] [CrossRef]
- Bianconi, V.; Mannarino, M.R.; Figorilli, F.; Cosentini, E.; Batori, G.; Marini, E.; Banach, M.; Sahebkar, A.; Pirro, M. The detrimental impact of elevated Ferritin to Iron ratio on in-hospital prognosis of patients with COVID-19. Expert Rev. Mol. Diagn. 2022, 22, 469–478. [Google Scholar] [CrossRef]
- Chakurkar, V.; Rajapurkar, M.; Lele, S.; Mukhopadhyay, B.; Lobo, V.; Injarapu, R.; Sheikh, M.; Dholu, B.; Ghosh, A.; Jha, V. Increased serum catalytic iron may mediate tissue injury and death in patients with COVID-19. Sci. Rep. 2021, 11, 19618. [Google Scholar] [CrossRef]
- Claise, C.; Saleh, J.; Rezek, M.; Vaulont, S.; Peyssonnaux, C.; Edeas, M. Low transferrin levels predict heightened inflammation in patients with COVID-19: New insights. Int. J. Infect. Dis. 2022, 116, 74–79. [Google Scholar] [CrossRef]
- Kilercik, M.; Ucal, Y.; Serdar, M.; Serteser, M.; Ozpinar, A.; Schweigert, F.J. Zinc protoporphyrin levels in COVID-19 are indicative of iron deficiency and potential predictor of disease severity. PLoS ONE 2022, 17, e0262487. [Google Scholar] [CrossRef]
- Skalny, A.V.; Timashev, P.S.; Aschner, M.; Aaseth, J.; Chernova, L.N.; Belyaev, V.E.; Grabeklis, A.R.; Notova, S.V.; Lobinski, R.; Tsatsakis, A.; et al. Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers. Metabolites 2021, 11, 244. [Google Scholar] [CrossRef]
- Uta, M.; Neamtu, R.; Bernad, E.; Mocanu, A.G.; Gluhovschi, A.; Popescu, A.; Dahma, G.; Dumitru, C.; Stelea, L.; Citu, C.; et al. The Influence of Nutritional Supplementation for Iron Deficiency Anemia on Pregnancies Associated with SARS-CoV-2 Infection. Nutrients 2022, 14, 836. [Google Scholar] [CrossRef]
- Delaye, J.B.; Alarcan, H.; Vallet, N.; Veyrat-Durebex, C.; Bernard, L.; Hérault, O.; Ropert, M.; Marlet, J.; Gyan, E.; Andres, C.; et al. Specific changes of erythroid regulators and hepcidin in patients infected by SARS-CoV-2. J. Investig. Med. 2022, 70, 934–938. [Google Scholar] [CrossRef]
- Kronstein-Wiedemann, R.; Stadtmüller, M.; Traikov, S.; Georgi, M.; Teichert, M.; Yosef, H.; Wallenborn, J.; Karl, A.; Schütze, K.; Wagner, M.; et al. SARS-CoV-2 Infects Red Blood Cell Progenitors and Dysregulates Hemoglobin and Iron Metabolism. Stem Cell Rev. Rep. 2022, 18, 1809–1821. [Google Scholar] [CrossRef]
- Moreira, A.C.; Teles, M.J.; Silva, T.; Bento, C.M.; Alves, I.S.; Pereira, L.; Guimarães, J.T.; Porto, G.; Oliveira, P.; Gomes, M.S. Iron Related Biomarkers Predict Disease Severity in a Cohort of Portuguese Adult Patients during COVID-19 Acute Infection. Viruses 2021, 13, 2482. [Google Scholar] [CrossRef]
- Ergin Tuncay, M.; Neselioglu, S.; Asfuroglu Kalkan, E.; Inan, O.; Sena Akkus, M.; Ates, I.; Erel, O. Modified Proline Metabolism and Prolidase Enzyme in COVID-19. Lab. Med. 2022, 6, lmac017. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.L.; Yang, Q.; Yuan, P.; Wang, X.; Cheng, L. Associations of essential and toxic metals/metalloids in whole blood with both disease severity and mortality in patients with COVID-19. FASEB J. 2021, 35, e21392. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Huang, J.; Dai, D.; Feng, Y.; Liu, L.; Nie, S. Serum Iron Level as a Potential Predictor of Coronavirus Disease 2019 Severity and Mortality: A Retrospective Study. Open Forum Infect. Dis. 2020, 7, ofaa250. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Chen, Y.; Ji, Y.; He, X.; Xue, D. Increased Serum Levels of Hepcidin and Ferritin Are Associated with Severity of COVID-19. Med. Sci. Monit. 2020, 26, e926178. [Google Scholar] [CrossRef]
- Rahman, M.A.; Shanjana, Y.; Tushar, M.I.; Mahmud, T.; Rahman, G.M.S.; Milan, Z.H.; Sultana, T.; Chowdhury, A.; Bhuiyan, M.A.; Islam, M.R.; et al. Hematological abnormalities and comorbidities are associated with COVID-19 severity among hospitalized patients: Experience from Bangladesh. PLoS ONE 2021, 16, e0255379. [Google Scholar] [CrossRef]
- Aly, M.M.; Meshref, T.S.; Abdelhameid, M.A.; Ahmed, S.A.; Shaltout, A.S.; Abdel-Moniem, A.E.; Hamad, D.A. Can Hematological Ratios Predict Outcome of COVID-19 Patients? A Multicentric Study. J. Blood Med. 2021, 12, 505–515. [Google Scholar] [CrossRef]
- Huang, H.; Song, B.; Xu, Z.; Jiao, Y.; Huang, L.; Zhao, P.; Huang, J.; Zhou, Z.; Zhao, Z.; Tian, J.; et al. Predictors of Coronavirus Disease 2019 Severity: A Retrospective Study of 64 Cases. Jpn. J. Infect. Dis. 2021, 74, 54–60. [Google Scholar] [CrossRef]
- Sana, A.; Avneesh, M. Identification of hematological and inflammatory parameters associated with disease severity in hospitalized patients of COVID-19. J. Family Med. Prim. Care 2022, 11, 260–264. [Google Scholar] [CrossRef]
- Huang, C.Y.; Tsai, H.W.; Liu, C.Y.; Liu, T.H.; Huang, H.L.; Chang, C.C.; Chen, W.C.; Sun, J.T. The predictive and prognostic role of hematologic and biochemical parameters in the emergency department among coronavirus disease 2019 patients. Chin. J. Physiol. 2021, 64, 306–311. [Google Scholar]
- Az, A.; Sogut, O.; Akdemir, T.; Ergenc, H.; Dogan, Y.; Cakirca, M. Impacts of Demographic and Clinical Characteristics on Disease Severity and Mortality in Patients with Confirmed COVID-19. Int. J. Gen. Med. 2021, 14, 2989–3000. [Google Scholar] [CrossRef]
- Ghweil, A.A.; Hassan, M.H.; Khodeary, A.; Mohamed, A.O.; Mohammed, H.M.; Abdelazez, A.A.; Osman, H.A.; Bazeed, S.E.S. Characteristics, Outcomes and Indicators of Severity for COVID-19 Among Sample of ESNA Quarantine Hospital’s Patients, Egypt: A Retrospective Study. Infect. Drug Resist. 2020, 13, 2375–2383. [Google Scholar] [CrossRef]
- Ramadan, H.K.; Mahmoud, M.A.; Aburahma, M.Z.; Elkhawaga, A.A.; El-Mokhtar, M.A.; Sayed, I.M.; Hosni, A.; Hassany, S.M.; Medhat, M.A. Predictors of Severity and Co-Infection Resistance Profile in COVID-19 Patients: First Report from Upper Egypt. Infect. Drug Resist. 2020, 13, 3409–3422. [Google Scholar] [CrossRef]
- Yamamoto, A.; Wada, H.; Ichikawa, Y.; Mizuno, H.; Tomida, M.; Masuda, J.; Makino, K.; Kodama, S.; Yoshida, M.; Fukui, S.; et al. Evaluation of Biomarkers of Severity in Patients with COVID-19 Infection. J. Clin. Med. 2021, 10, 3775. [Google Scholar] [CrossRef]
- Abdelhakam, D.A.; Badr, F.M.; Abd El Monem Teama, M.; Bahig Elmihi, N.M.; El-Mohamdy, M.A. Serum amyloid A, ferritin and carcinoembryonic antigen as biomarkers of severity in patients with COVID-19. Biomed. Rep. 2022, 16, 13. [Google Scholar] [CrossRef]
- Emsen, A.; Sumer, S.; Tulek, B.; Cizmecioglu, H.; Vatansev, H.; Goktepe, M.H.; Kanat, F.; Koksal, Y.; Arslan, U.; Artac, H. Correlation of myeloid-derived suppressor cells with C-reactive protein, ferritin and lactate dehydrogenase levels in patients with severe COVID-19. Scand. J. Immunol. 2022, 95, e13108. [Google Scholar] [CrossRef]
- Doghish, A.S.; Elkhatib, W.F.; Hassan, E.A.; Elkhateeb, A.F.; Mahmoud, E.E.; Ahmed, M.I.; Khalil, M.A.F. Clinical characteristics of Egyptian male patients with COVID-19 acute respiratory distress syndrome. PLoS ONE 2021, 16, e0249346. [Google Scholar]
- Fei, F.; Smith, J.A.; Cao, L. Clinical laboratory characteristics in patients with suspected COVID-19: One single-institution experience. J. Med. Virol. 2021, 93, 1665–1671. [Google Scholar] [CrossRef]
- Deng, F.; Zhang, L.; Lyu, L.; Lu, Z.; Gao, D.; Ma, X.; Guo, Y.; Wang, R.; Gong, S.; Jiang, W. Increased levels of ferritin on admission predicts intensive care unit mortality in patients with COVID-19. Med. Clin. (Engl. Ed.) 2021, 156, 324–331. [Google Scholar]
- Valeri, A.M.; Robbins-Juarez, S.Y.; Stevens, J.S.; Ahn, W.; Rao, M.K.; Radhakrishnan, J.; Gharavi, A.G.; Mohan, S.; Husain, S.A. Presentation and Outcomes of Patients with ESKD and COVID-19. J. Am. Soc. Nephrol. 2020, 31, 1409–1415. [Google Scholar] [CrossRef]
- Gayam, V.; Chobufo, M.D.; Merghani, M.A.; Lamichhane, S.; Garlapati, P.R.; Adler, M.K. Clinical characteristics and predictors of mortality in African-Americans with COVID-19 from an inner-city community teaching hospital in New York. J. Med. Virol. 2021, 93, 812–819. [Google Scholar] [CrossRef]
- Zeng, Z.; Yu, H.; Chen, H.; Qi, W.; Chen, L.; Chen, G.; Yan, W.; Chen, T.; Ning, Q.; Han, M.; et al. Longitudinal changes of inflammatory parameters and their correlation with disease severity and outcomes in patients with COVID-19 from Wuhan, China. Crit. Care 2020, 24, 525. [Google Scholar] [CrossRef]
- Anuk, A.T.; Polat, N.; Akdas, S.; Erol, S.A.; Tanacan, A.; Biriken, D.; Keskin, H.L.; Moraloglu Tekin, O.; Yazihan, N.; Sahin, D. The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection During Pregnancy. Biol. Trace Elem. Res. 2021, 199, 3608–3617. [Google Scholar] [CrossRef]
- Erol, S.A.; Polat, N.; Akdas, S.; Aribal Ayral, P.; Anuk, A.T.; Ozden Tokalioglu, E.; Goncu Ayhan, Ş.; Kesikli, B.; Ceylan, M.N.; Tanacan, A.; et al. Maternal selenium status plays a crucial role on clinical outcomes of pregnant women with COVID-19 infection. J. Med. Virol. 2021, 93, 5438–5445. [Google Scholar] [CrossRef]
- Venter, C.; Bezuidenhout, J.A.; Laubscher, G.J.; Lourens, P.J.; Steenkamp, J.; Kell, D.B.; Pretorius, E. Erythrocyte, Platelet, Serum Ferritin, and P-Selectin Pathophysiology Implicated in Severe Hypercoagulation and Vascular Complications in COVID-19. Int. J. Mol. Sci. 2020, 21, 8234. [Google Scholar] [CrossRef]
- Mehri, F.; Rahbar, A.H.; Ghane, E.T.; Souri, B.; Esfahani, M. Changes in oxidative markers in COVID-19 patients. Arch. Med. Res. 2021, 52, 843–849. [Google Scholar] [CrossRef]
- Ahmed, S.; Ansar Ahmed, Z.; Siddiqui, I.; Haroon Rashid, N.; Mansoor, M.; Jafri, L. Evaluation of serum ferritin for prediction of severity and mortality in COVID-19- A cross sectional study. Ann. Med. Surg. 2021, 63, 102163. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef]
- Guan, X.; Zhang, B.; Fu, M.; Li, M.; Yuan, X.; Zhu, Y.; Peng, J.; Guo, H.; Lu, Y. Clinical and inflammatory features based machine learning model for fatal risk prediction of hospitalized COVID-19 patients: Results from a retrospective cohort study. Ann. Med. 2021, 53, 257–266. [Google Scholar] [CrossRef]
- Tural Onur, S.; Altın, S.; Sokucu, S.N.; Fikri, B.; Barça, T.; Bolat, E.; Toptaş, M. Could ferritin level be an indicator of COVID-19 disease mortality? J. Med. Virol. 2021, 93, 1672–1677. [Google Scholar] [CrossRef]
- Lino, K.; Guimarães, G.M.C.; Alves, L.S.; Oliveira, A.C.; Faustino, R.; Fernandes, C.S.; Tupinambá, G.; Medeiros, T.; Silva, A.A.D.; Almeida, J.R. Serum ferritin at admission in hospitalized COVID-19 patients as a predictor of mortality. Braz. J. Infect. Dis. 2021, 25, 101569. [Google Scholar] [CrossRef]
- Khamis, F.; Memish, Z.; Bahrani, M.A.; Dowaiki, S.A.; Pandak, N.; Bolushi, Z.A.; Salmi, I.A.; Al-Zakwani, I. Prevalence and predictors of in-hospital mortality of patients hospitalized with COVID-19 infection. J. Infect. Public Health 2021, 14, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Yardımcı, A.C.; Yıldız, S.; Ergen, E.; Ballı, H.; Ergene, E.; Guner, Y.S.; Karnap, M.; Demırbas Keskın, D.; Yuksel, H.; Bocutoglu, F.; et al. Association between platelet indices and the severity of the disease and mortality in patients with COVID-19. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 6731–6740. [Google Scholar] [PubMed]
- Martinez Mesa, A.; Cabrera César, E.; Martín-Montañez, E.; Sanchez Alvarez, E.; Lopez, P.M.; Romero-Zerbo, Y.; Garcia-Fernandez, M.; Velasco Garrido, J.L. Acute Lung Injury Biomarkers in the Prediction of COVID-19 Severity: Total Thiol, Ferritin and Lactate Dehydrogenase. Antioxidants 2021, 10, 1221. [Google Scholar] [CrossRef] [PubMed]
- Rasyid, H.; Sangkereng, A.; Harjianti, T.; Soetjipto, A.S. Impact of age to ferritin and neutrophil-lymphocyte ratio as biomarkers for intensive care requirement and mortality risk in COVID-19 patients in Makassar, Indonesia. Physiol. Rep. 2021, 9, e14876. [Google Scholar] [CrossRef] [PubMed]
- Zanella, A.; Florio, G.; Antonelli, M.; Bellani, G.; Berselli, A.; Bove, T.; Cabrini, L.; Carlesso, E.; Castelli, G.P.; Cecconi, M.; et al. Time course of risk factors associated with mortality of 1260 critically ill patients with COVID-19 admitted to 24 Italian intensive care units. Intensive Care Med. 2021, 47, 995–1008. [Google Scholar] [PubMed]
- Burugu, H.R.; Kandi, V.; Kutikuppala, L.V.S.; Suvvari, T.K. Activities of Serum Ferritin and Treatment Outcomes among COVID-19 Patients Treated with Vitamin C and Dexamethasone: An Uncontrolled Single-Center Observational Study. Cureus 2020, 12, e11442. [Google Scholar] [CrossRef]
- Rai, D.; Ranjan, A.; Ameet, H.; Pandey, S. Clinical and Laboratory Predictors of Mortality in COVID-19 Infection: A Retrospective Observational Study in a Tertiary Care Hospital of Eastern India. Cureus 2021, 13, e17660. [Google Scholar] [CrossRef]
- Aygun, H.; Eraybar, S. Can ferritin/lymphocyte percentage ratio, a new indicator, predict the clinical course of COVID-19 cases? Bratisl. Lek. Listy 2021, 122, 799–804. [Google Scholar] [CrossRef]
- Pujani, M.; Raychaudhuri, S.; Singh, M.; Kaur, H.; Agarwal, S.; Jain, M.; Chandoke, R.K.; Singh, K.; Sidam, D.; Chauhan, V. An analysis of hematological, coagulation and biochemical markers in COVID-19 disease and their association with clinical severity and mortality: An Indian outlook. Am. J. Blood Res. 2021, 11, 580–591. [Google Scholar]
- Chen, Q.; Kong, H.; Qi, X.; Ding, W.; Ji, N.; Wu, C.; Huang, C.; Wu, W.; Huang, M.; Xie, W.; et al. Carcinoembryonic Antigen: A Potential Biomarker to Evaluate the Severity and Prognosis of COVID-19. Front. Med. 2020, 7, 579543. [Google Scholar] [CrossRef]
- Yousaf, M.N.; Sarwar, S.; Tarique, S.; Ahmed, M.; Tahir, H. Mortality in Patients of COVID-19 Infection: Biochemical Markers and its Cut-off Values for Predicting Outcome. J. Coll. Phys. Surg. Pak. 2022, 32, 37–41. [Google Scholar]
- Arshad, A.R.; Khan, I.; Shahzad, K.; Arshad, M.; Haider, S.J.; Aslam, M.J. Association of Inflammatory Markers with Mortality in COVID-19 Infection. J. Coll. Phys. Surg. Pak. 2020, 30, 158–163. [Google Scholar]
- Masetti, C.; Generali, E.; Colapietro, F.; Voza, A.; Cecconi, M.; Messina, A.; Omodei, P.; Angelini, C.; Ciccarelli, M.; Badalamenti, S.; et al. High mortality in COVID-19 patients with mild respiratory disease. Eur. J. Clin. Investig. 2020, 50, e13314. [Google Scholar] [CrossRef]
- Marimuthu, A.K.; Anandhan, M.; Sundararajan, L.; Chandrasekaran, J.; Ramakrishnan, B. Utility of various inflammatory markers in predicting outcomes of hospitalized patients with COVID-19 pneumonia: A single-center experience. Lung. India 2021, 38, 448–453. [Google Scholar] [CrossRef]
- Allard, L.; Ouedraogo, E.; Molleville, J.; Bihan, H.; Giroux-Leprieur, B.; Sutton, A.; Baudry, C.; Josse, C.; Didier, M.; Deutsch, D.; et al. Malnutrition: Percentage and Association with Prognosis in Patients Hospitalized for Coronavirus Disease 2019. Nutrients 2020, 12, 3679. [Google Scholar] [CrossRef]
- Bats, M.L.; Rucheton, B.; Fleur, T.; Orieux, A.; Chemin, C.; Rubin, S.; Colombies, B.; Desclaux, A.; Rivoisy, C.; Mériglier, E.; et al. Covichem: A biochemical severity risk score of COVID-19 upon hospital admission. PLoS ONE 2021, 16, e0250956. [Google Scholar] [CrossRef]
- Kirtana, J.; Kumar, A.; Kumar, S.S.; Singh, A.K.; Shankar, S.H.; Sharma, A.; Kumar, A.; Kaur, R.; Khan, M.A.; Ranjan, P.; et al. Mild COVID-19 infection-predicting symptomatic phase and outcome: A study from AIIMS, New Delhi. J. Family Med. Prim. Care 2020, 9, 5360–5365. [Google Scholar]
- Sukrisman, L.; Sinto, R. Coagulation profile and correlation between D-dimer, inflammatory markers, and COVID-19 severity in an Indonesian national referral hospital. J. Int. Med. Res. 2021, 49, 3000605211059939. [Google Scholar] [CrossRef]
- San Segundo, D.; Arnáiz de Las Revillas, F.; Lamadrid-Perojo, P.; Comins-Boo, A.; González-Rico, C.; Alonso-Peña, M.; Irure-Ventura, J.; Olmos, J.M.; Fariñas, M.C.; López-Hoyos, M. Innate and Adaptive Immune Assessment at Admission to Predict Clinical Outcome in COVID-19 Patients. Biomedicines 2021, 9, 917. [Google Scholar] [CrossRef]
- Yasui, Y.; Yasui, H.; Suzuki, K.; Saitou, T.; Yamamoto, Y.; Ishizaka, T.; Nishida, K.; Yoshihara, S.; Gohma, I.; Ogawa, Y. Analysis of the predictive factors for a critical illness of COVID-19 during treatment—Relationship between serum zinc level and critical illness of COVID-19. Int. J. Infect. Dis. 2020, 100, 230–236. [Google Scholar] [CrossRef]
- García-Gasalla, M.; Ferrer, J.M.; Fraile-Ribot, P.A.; Ferre-Beltrán, A.; Rodríguez, A.; Martínez-Pomar, N.; Ramon-Clar, L.; Iglesias, A.; Losada-López, I.; Fanjul, F.; et al. Predictive Immunological, Virological, and Routine Laboratory Markers for Critical COVID-19 on Admission. Can. J. Infect. Dis. Med. Microbiol. 2021, 2021, 9965850. [Google Scholar] [CrossRef] [PubMed]
- Haroun, R.A.; Osman, W.H.; Eessa, A.M. Interferon-γ-induced protein 10 (IP-10) and serum amyloid A (SAA) are excellent biomarkers for the prediction of COVID-19 progression and severity. Life Sci. 2021, 269, 119019. [Google Scholar] [CrossRef] [PubMed]
- Pubmed. Available online: https://pubmed.ncbi.nlm.nih.gov/ (accessed on 31 May 2022).
- Web of Science. Available online: http://apps.webofknowledge.com (accessed on 31 May 2022).
- Scopus. Available online: https://www.scopus.com/search/form.uri?display=basic#basic (accessed on 31 May 2022).
- Estimating the Sample Mean and Standard Deviation from the Sample Size, Median, Range and/or Interquartile Range. Available online: https://www.math.hkbu.edu.hk/~tongt/papers/median2mean.html (accessed on 31 May 2022).
- Beigmohammadi, M.T.; Bitarafan, S.; Abdollahi, A.; Amoozadeh, L.; Salahshour, F.; Mahmoodi Ali Abadi, M.; Soltani, D.; Motallebnejad, Z.A. The association between serum levels of micronutrients and the severity of disease in patients with COVID-19. Nutrition 2021, 91–92, 111400. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, F.T.; Tercan, M.; Patmano, G.; Bingol Tanrıverdi, T.; Demir, H.A.; Yurekli, U.F. Can Ferritin Levels Predict the Severity of Illness in Patients with COVID-19? Cureus 2021, 13, e12832. [Google Scholar] [CrossRef] [PubMed]
- Sukrisman, L.; Sinto, R.; Priantono, D. Hematologic Profiles and Correlation between Absolute Lymphocyte Count and Neutrophil/Lymphocyte Ratio with Markers of Inflammation of COVID-19 in an Indonesian National Referral Hospital. Int. J. Gen. Med. 2021, 14, 6919–6924. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Gasalla, M.; Berman-Riu, M.; Pons, J.; Rodríguez, A.; Iglesias, A.; Martínez-Pomar, N.; Llompart-Alabern, I.; Riera, M.; Ferré Beltrán, A.; Figueras-Castilla, A.; et al. Hyperinflammatory State and Low T1 Adaptive Immune Response in Severe and Critical Acute COVID-19 Patients. Front. Med. 2022, 9, 828678. [Google Scholar] [CrossRef] [PubMed]
- Nizami, D.J.; Raman, V.; Paulose, L.; Hazari, K.S.; Mallick, A.K. Role of laboratory biomarkers in assessing the severity of COVID-19 disease. A cross-sectional study. J. Family Med. Prim. Care 2021, 10, 2209–2215. [Google Scholar] [CrossRef]
- Bastin, A.; Shiri, H.; Zanganeh, S.; Fooladi, S.; Momeni Moghaddam, M.A.; Mehrabani, M.; Nematollahi, M.H. Iron Chelator or Iron Supplement Consumption in COVID-19? The Role of Iron with Severity Infection. Biol. Trace Elem. Res. 2021, 1–11. [Google Scholar] [CrossRef]
- Nicolas, G.; Bennoun, M.; Devaux, I.; Beaumont, C.; Grandchamp, B.; Kahn, A.; Vaulont, S. Lack of hepcidin gene expression and severe tissue iron overload in upstream stimulatory factor 2 (USF2) knockout mice. Proc. Natl. Acad. Sci. USA 2001, 98, 8780–8785. [Google Scholar] [CrossRef]
- Pigeon, C.; Ilyin, G.; Courselaud, B.; Leroyer, P.; Turlin, B.; Brissot, P.; Loréal, O. A new mouse liver-specific gene, encoding a protein homologous to human antimicrobial peptide hepcidin, is overexpressed during iron overload. J. Biol. Chem. 2001, 276, 7811–7819. [Google Scholar] [CrossRef]
- Peng, D.; Gao, Y.; Zhang, L.; Liu, Z.; Wang, H.; Liu, Y. The Relationship between Hepcidin-Mediated Iron Dysmetabolism and COVID-19 Severity: A Meta-Analysis. Front. Public Health 2022, 10, 881412. [Google Scholar]
- Drakesmith, H.; Prentice, A. Viral infection and iron metabolism. Nat. Rev. Microbiol. 2008, 6, 541–552. [Google Scholar] [CrossRef]
- Nemeth, E.; Tuttle, M.S.; Powelson, J.; Vaughn, M.B.; Donovan, A.; Ward, D.M.; Ganz, T.; Kaplan, J. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science 2004, 306, 2090–2093. [Google Scholar] [CrossRef]
- Mahroum, N.; Alghory, A.; Kiyak, Z.; Alwani, A.; Seida, R.; Alrais, M.; Shoenfeld, Y. Ferritin—From iron, through inflammation and autoimmunity, to COVID-19. J. Autoimmun. 2022, 126, 102778. [Google Scholar] [CrossRef]
- Kell, D.B.; Pretorius, E. Serum ferritin is an important inflammatory disease marker, as it is mainly a leakage product from damaged cells. Metallomics 2014, 6, 748–773. [Google Scholar] [CrossRef]
- Henry, B.M.; de Oliveira, M.H.S.; Benoit, S.; Plebani, M.; Lippi, G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chem. Lab. Med. 2020, 58, 1021–1028. [Google Scholar] [CrossRef]
- Jiang, Z.B.; Gao, J.; Chai, Y.H.; Li, W.; Luo, Y.F.; Chen, Y.Z. Astragaloside alleviates alcoholic fatty liver disease by suppressing oxidative stress. Kaohsiung J. Med. Sci. 2021, 37, 718–729. [Google Scholar] [CrossRef]
- Andriopoulos, B.; Pantopoulos, K. Hepcidin generated by hepatoma cells inhibits iron export from co-cultured THP1 monocytes. J. Hepatol. 2006, 44, 1125–1131. [Google Scholar] [CrossRef]
- Turi, J.L.; Yang, F.; Garrick, M.D.; Piantadosi, C.A.; Ghio, A.J. The iron cycle and oxidative stress in the lung. Free Radic. Biol. Med. 2004, 36, 850–857. [Google Scholar] [CrossRef]
- Gudjoncik, A.; Guenancia, C.; Zeller, M.; Cottin, Y.; Vergely, C.; Rochette, L. Iron, oxidative stress, and redox signaling in the cardiovascular system. Mol. Nutr. Food Res. 2014, 58, 1721–1738. [Google Scholar] [CrossRef]
- Braumann, A.; Wulfhekel, U.; Nielsen, P.; Balkenhol, B.; Düllmann, J. Pattern of iron storage in the rat heart following iron overloading with trimethylhexanoyl-ferrocene. Acta Anat 1994, 150, 45–54. [Google Scholar] [CrossRef]
- Shah, K.K.; Verma, R.; Oleske, J.M.; Scolpino, A.; Bogden, J.D. Essential trace elements and progression and management of HIV infection. Nutr. Res. 2019, 71, 21–29. [Google Scholar] [CrossRef]
- Georgopoulou, U.; Dimitriadis, A.; Foka, P.; Karamichali, E.; Mamalaki, A. Hepcidin and the iron enigma in HCV infection. Virulence 2014, 5, 465–476. [Google Scholar] [CrossRef]
- Toyokuni, S. Iron-induced carcinogenesis: The role of redox regulation. Free Radic. Biol. Med. 1996, 20, 553–566. [Google Scholar] [CrossRef]
- Ehsani, A.H.; Nasimi, M.; Bigdelo, Z. Pityriasis rosea as a cutaneous manifestation of COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e436–e437. [Google Scholar] [CrossRef]
- Ehsani, S. COVID-19 and iron dysregulation: Distant sequence similarity between hepcidin and the novel coronavirus spike glycoprotein. Biol. Direct 2020, 15, 19. [Google Scholar] [CrossRef]
- Elsayed, M.E.; Sharif, M.U.; Stack, A.G. Transferrin Saturation: A Body Iron Biomarker. Adv. Clin. Chem. 2016, 75, 71–97. [Google Scholar]
- Hippchen, T.; Altamura, S.; Muckenthaler, M.U.; Merle, U. Hypoferremia is Associated with Increased Hospitalization and Oxygen Demand in COVID-19 Patients. Hemasphere 2020, 4, e492. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).