Abstract
The association of meat consumption with mortality and morbidity for non-communicable diseases has been extensively studied. However, the relation of white meat consumption with health outcomes remains controversial. The present meta-analysis was conducted to comprehensively analyze the available evidence on the consistency and strength of the association between the consumption of white meat, death from any cause and incidence of fatal and non-fatal cardiovascular (CV) events. PubMed, Web of Science, Scopus and Embase databases were searched for articles published up to April 30, 2020. We included prospective cohort studies reporting relative risks and pertinent 95% confidence intervals (CI) for all-cause mortality and/or CV events (fatal or non-fatal). A total of 22 studies were included in the meta-analysis. Eleven studies (14 data sets) reported data on all-cause mortality, 10 studies (15 datasets) on cardiovascular disease (CVD) mortality and 10 studies (11 datasets) on non-fatal CV events. When comparing the highest versus the lowest consumption of white meat, the pooled OR and pertinent 95% CI were 0.94 (0.90, 0.97, p < 0.001) for all-cause mortality, 0.95 (0.89, 1.01, p = 0.13) for CV mortality, and 0.99 (0.95, 1.02, p = 0.48) for non-fatal CV events. In conclusion, the study shows for the first time a robust and inverse association between white meat consumption and all-cause mortality and a neutral association with CV mortality and morbidity. This highlights the importance of differentiating the meat types for what concerns their health effects and suggests that white meat might be a healthier alternative to read and processed meat consumption.
1. Introduction
The relationship between dietary habits and chronic non-communicable diseases (NCDs) has been extensively investigated [1,2,3,4,5,6]. Although randomized trials with hard end points have not been feasible for most dietary factors, other lines of evidence, including long-term prospective observational studies and short-term trials with intermediate outcomes, have provided supporting evidence for potential causal relationships between dietary factors and health. A high-quality diet, comprising whole grains, fruits, vegetables, nuts, non-tropical vegetable oils, and fish, is one of the most important factors in preventing early death and non-communicable diseases worldwide [1,7], more than any other risk factors globally, including tobacco smoking [1,8,9]. On the contrary, high consumption of animal food sources (meat, in particular processed meat) and sodium intake are the main dietary risk factors for early death and disabilities due to NCDs [1]. A large body of evidence from prospective cohort studies has shown that high versus low meat consumption, is associated with an excess risk of all-cause and cause-specific mortality [10,11]. However, when type of meat consumed is analyzed disjointedly, different associations have been observed. In fact, while several reviews and meta-analyses have convincingly shown a positive association between red and processed meat consumption and risk of all-cause mortality [7,12,13,14,15], incidence of CVD, diabetes and some types of cancers [16,17,18,19,20,21], the association of white meat with mortality and morbidity for NCD is not clearly established [11,15,22,23]. There is evidence that the substitution of one daily serving of red meat with white meat, mainly poultry, is associated with a 19% reduction of cardiovascular risk [24], but this finding was not confirmed by other studies [11,15,22]. The most comprehensive work on this topic is a meta-analysis of prospective cohort studies on the relationship between white meat consumption and total mortality showing a weak inverse association in women when comparing the highest vs. the lowest consumption category [15]. In this same study, no association was reported with CVD mortality in either men or women and no data were provided on non-fatal CV events. As discussed by the authors, the small number, and the high heterogeneity of the meta-analyzed studies, does not allow to reach conclusive results. Following this work completed in 2014, several large prospective cohort studies have investigated the relationship of white meat consumption with health outcomes, some of these studies report also data on non-fatal CV endpoints [5,25,26,27,28,29,30,31,32]. We have carried out the present meta-analysis to comprehensively analyze the most updated available evidence on the consistency and strength of the association between the consumption of white meat, death from any cause and incidence of fatal or non-fatal cardiovascular events.
2. Materials and Methods
2.1. Search Strategy and Study Selection
A systematic research of all the prospective cohort studies published until April 30, 2020 on the association of white meat consumption with all-cause mortality, incidence of cardiovascular disease and coronary heart disease, was performed according to PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines [25].
The research was carried out in the electronic databases (PubMed, Web of Science, Scopus, Embase) using the following key words in all possible combinations: (“poultry” or “white meat” or “chicken” or “turkey” or “rabbit”) and (“myocardial” or “coronary” or “mortality” or “cardiovascular” or “ischemic” or “stroke” or “cerebrovascular” or “death” or “fatal” or “fatality” or “events”) and (“meat” or “consumption” or “intake” or “serving”). The search was limited to human studies and had no language restrictions.
We included studies defining “white meat” as poultry (chicken, turkey, duck and goose) and rabbit. Exclusion criteria were: (i) retrospective studies; (ii) studies conducted on vegetarian people; and (iii) studies in which it was not possible to evaluate white meat alone because part of combined meals. When several publications of the same study were identified, only the most recent, or most detailed publication was used.
The reference lists of selected studies and reviews were also searched to identify additional articles not previously included. In addition, the lists of the retrieved articles were manually reviewed. In case of missing data, the Authors were contacted by e-mail to acquire the original data. This meta-analysis has been registered on Prospero (https://www.crd.york.ac.uk/PROSPERO (accessed on 26 January 2021)) with the registration number: CRD42020198126.
2.2. Data Extraction and Study Quality
Two reviewers (I.C. and A.G.) assessed the titles and abstracts of all identified studies and independently reviewed and extracted relevant data from each study, including first author and year of publication, country, study design, sample size, participant characteristics, follow-up duration, number of subjects in comparison groups, type of white meat, and main results of the outcomes investigated. In case of disagreement, a third investigator was consulted (M.V.). Discrepancies were resolved by consensus.
The evaluation of methodological quality of each study was performed with the Newcastle-Ottawa scale (NOS), which is specifically developed to assess quality of non-randomized observational studies [33]. The scoring system encompasses three major domains (selection, comparability, exposure) and a resulting score range between 0 and 8, a higher score representing a better methodological quality. Results of the NOS quality assessment are reported in Supplemental Table S1.
2.3. Statistical Analysis
The primary outcome was all-cause mortality defined as death for any cause (vascular and non-vascular). Secondary outcomes were CV mortality and non-fatal CV events (including ischemic heart disease, ischemic stroke, and hemorrhagic stroke). Data synthesis and statistical analysis were carried out using comprehensive meta-analysis (Version 3, Biostat, Englewood, NJ, USA, 2006) software. The pooled probability of all-cause mortality, cardiovascular mortality and cardiovascular events in subjects in the highest versus the lowest category of white meat consumption was expressed as OR with pertinent 95% confidence intervals (CI). The overall effect was tested by Z-scores, with p < 0.05 being considered statically significant.
Statistical heterogeneity among studies was assessed by chi square Cochran’s Q test and with I2 statistic, which measure the inconsistency across study results and describe the proportion of total variation in study estimates due to heterogeneity rather than sampling error. In detail, an I2 value of 25% corresponds to low, 25–50% to moderate, and 50% to high heterogeneity. Publication bias was assessed by the Egger’s test and funnel plots of the log OR versus the standard error were used as graphical representation.
To address possible small-study effect, funnel plots were visually inspected for asymmetry and the Egger’s test was used to assess publication bias, over and above any subjective evaluation, with p < 0.10 being considered statistically significant. In case of a significant publication bias, the Duval and Tweedie’s trim and fill method with the random-effect model was used to allow for the estimation of an adjusted effect size. In order to be as conservative as possible, the random-effect method was used to take into account both the within-study and between-study variability.
2.4. Subgroup Analyses and Meta-Regression Analyses
Separate analyses were performed by stratifying results for geographical area where each study was carried out. Analyses were repeated after excluding studies judged as low quality according to NOS score.
We performed meta-regression analyses in order to assess whether differences in the risk of all-cause mortality, CV mortality and CV events observed between highest and lowest white meat consumption categories were confounded by demographic (age, male gender) or clinical variables (body mass index, hypertension, diabetes mellitus, previous CV events, smoking habit) or follow-up duration. The regression models were carried out using differences in the risk of all-cause mortality, CV mortality and CV events observed between highest and lowest white meat consumption categories as the dependent variables (y) and the above-mentioned co-variates as independent variables (x). Comprehensive meta-analysis software (Version 3, Biostat, Englewood, NJ, USA, 2006) was used for the multivariate approach.
3. Results
3.1. Study Selection and Main Characteristics
After excluding duplicates, the search retrieved 1355 articles. Of these, 1291 were excluded because they were off the topic after scanning the title and/or the abstract; 42 because they were reviews/comments/case reports or lacked data of interest or did not match the inclusion and exclusion criteria. More in detail, among the studies excluded based on study design are also the study of Sinha et al. [11], because fish was combined with white meat, and the study of Sun et al. [34] which specifically focused on fried poultry only, at variance with all the other studies we included (Figure 1).
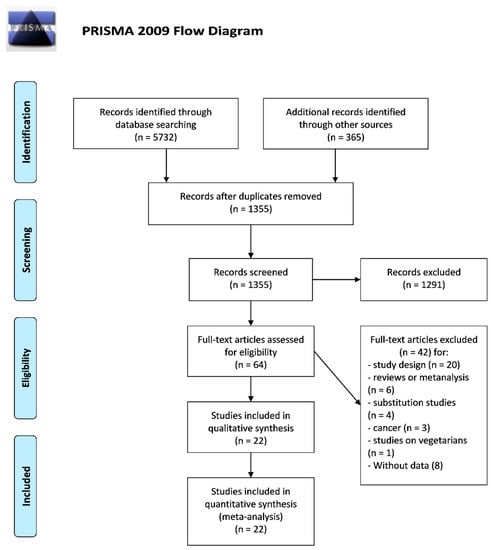
Figure 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagram.
Among the included studies Lee et al. [10], Nagao et al. [35], Wurtz et al. [36], provided separate data for males and females; the study by Etemadi et al. [26] separately analyzed data for consumption of processed and unprocessed white meat and provided separate outcomes for ischemic heart disease and stroke; the study by Sluik et al. [27] provided separate data for diabetic and non-diabetic participants. In all these cases, the different populations were analyzed as separate datasets. Thus, a total of 22 studies [5,10,22,26,27,28,29,30,31,32,35,36,37,38,39,40,41,42,43,44,45,46] on 3,132,149 subjects were included in the final meta-analysis. The main characteristics of included studies are summarized in Table 1. Eight studies [22,26,31,37,38,39,44,45] were carried out in America, seven in Asia [10,28,29,32,35,41,46] and seven in Europe [5,27,30,36,40,42,43]. Eleven studies (14 data-sets) [10,26,27,31,39,40,41,42,43,44,46] reported data on all-cause mortality, 10 studies (15 datasets) [10,26,29,35,39,40,41,42,43,46] on CV mortality and 10 studies (11 datasets) [5,22,28,30,32,36,37,38,44,45] on non-fatal CV events. The evaluation of methodological quality of each study showed a median NOS score of 6.

Table 1.
Characteristics of the prospective cohort studies included in the analysis
3.2. All-Cause Mortality, CVD Mortality and CVD Events
Of the 22 studies included in the meta-analysis, 11 studies reported data on all-cause mortality [10,26,27,31,39,40,41,42,43,44,46], four of these were conducted in America [12,26,39,44], three in Asia [10,41,46] and four in Europe [27,40,42,43]. One study reported separate data for processed and unprocessed white meat [26], one reported data by gender [10], and one reported data for people with or without diabetes [27]. Eleven studies were not included because there were no data on all-cause mortality [5,22,28,29,30,32,35,36,37,38,45]. The analysis of the 11 studies (14 datasets) on all-cause mortality showed a statistically significant lower mortality rate for subjects in the highest vs. lowest white meat consumption category (OR: 0.94, 95% CI: 0.90, 0.97, p < 0.001; Figure 2).
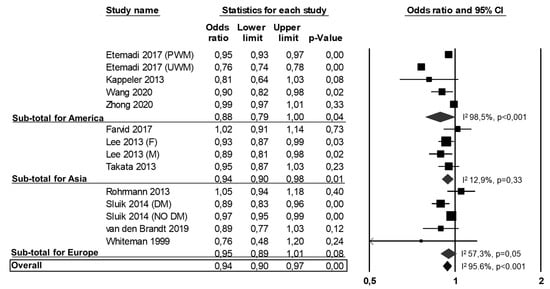
Figure 2.
Association between white meat consumption (highest vs. lowest) and all-cause mortality. PWD: processed white meat; UWM: unprocessed white meat; F: females; M: males; DM: diabetes mellitus.
Heterogeneity among studies was significant (I2: 95.6%, p < 0.001) and it was not reduced by the exclusion of one study at a time. Results were consistently confirmed when specifically analyzing the 4 studies (5 datasets) from America [26,31,39,44] (OR: 0.88, 95% CI: 0.79, 1.00, p = 0.04; I2: 98.5%, p < 0.001; Figure 2) and the 3 studies (4 datasets) from Asia [10,41,46] (OR: 0.94, 95% CI: 0.90, 0.98, p = 0.01; I2: 12.9%, p = 0.33; Figure 2), while a non-significant association was found in the 4 studies (5 datasets) conducted in Europe [27,40,42,43] (OR: 0.95, 95% CI: 0.89, 1.01, p = 0.08; I2: 57.3%, p = 0.05; Figure 2).
Of the 22 studies included in the meta-analysis, 10 reported data on CV mortality (i.e., stroke mortality, IHD mortality, or CVD mortality as a composite outcome) [10,26,29,35,39,40,41,42,43,46], two of these studies were conducted in America [26,39], five in Asia [10,29,35,41,46] and three in Europe [40,42,43]. One study reported data on processed and unprocessed white meat [26], and two studies reported separate data for males and females [10,35]. Twelve studies were not included because there were no data on CV mortality [5,12,22,27,28,30,32,36,37,38,44,45]. The analysis of the 10 studies (15 datasets) with CV outcomes showed no difference in CV mortality between subjects in the highest versus the lowest white meat consumption categories (OR: 0.95, 95% CI: 0.89, 1.01, p = 0.13; Figure 3).
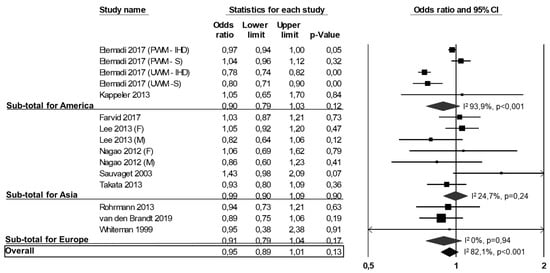
Figure 3.
Association between white meat consumption (highest vs. lowest) and CVD mortality. PWD-IHD: processed white meat-ischemic heart disease; PWD-S: processed white meat-stroke; UWM-IHD: unprocessed white meat-ischemic heart disease; UWM-S: unprocessed white meat-stroke; F: females; M: males.
Heterogeneity among studies was significant (I2: 82.1%, p < 0.001) and was not reduced by the exclusion of one study at a time. As shown in Figure 3, we found similar results when specifically analyzing studies from America [26,39] (OR: 0.90, 95% CI: 0.79, 1.03, p = 0.12; I2: 93.8%, p < 0.001), Asia [10,29,35,41,46] (OR: 0.99, 95% CI: 0.90, 1.09, p = 0.90; I2: 24.7%, p = 0.24) or Europe [40,42,43] (OR: 0.91, 95% CI: 0.79, 1.04, p = 0.17; I2: 0%, p = 0.94).
Of the 22 studies included in the meta-analysis, 10 studies (11 datasets) reported data on non-fatal CV events [5,22,28,30,32,36,37,38,44,45], five were from America [22,37,38,44,45], two from Asia [28,32] and three from Europe [5,30,36]. One study reported data on males and females [36]. Twelve studies were not included because there were no data on CV incidence [10,12,26,27,29,35,39,40,41,42,43,46]. On the overall no difference was observed in the risk of non-fatal CV events between subjects in the highest versus the lowest white meat consumption categories (OR: 0.99, 95% CI: 0.95, 1.02, p = 0.48; Figure 4).
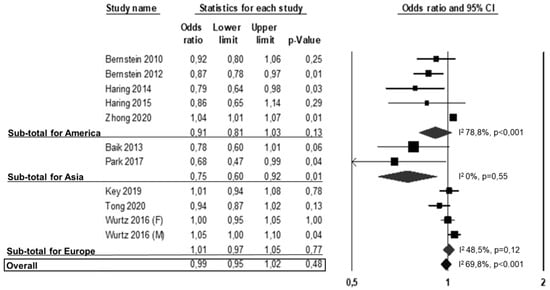
Figure 4.
Association between white meat consumption (highest vs. lowest) and non-fatal CV events. F: females; M: males.
Heterogeneity among studies was significant (I2: 69.8%, p < 0.001) and was not reduced by the exclusion of one study at a time. Results were confirmed when separately analyzing studies from America (OR: 0.91, 95% CI: 0.81, 1.03, p = 0.13; I2: 78.8%, p < 0.001) or Europe (Figure 4) (OR: 1.01, 95% CI: 0.97, 1.05, p = 0.77; I2: 48.5%, p = 0.12), while a significant risk reduction emerged from the Asian studies [28,32] (OR: 0.75, 95% CI: 0.60, 0.92, p = 0.01; I2: 0%, p = 0.55).
After excluding low quality studies (i.e., NOS < 6), the results were entirely confirmed for all-cause mortality (OR: 0.95, 95% CI: 0.91, 0.99, p = 0.02), CV mortality (OR: 0.94, 95% CI: 0.87, 1.02, p = 0.12) and non-fatal CV events (OR: 0.99, 95% CI: 0.96, 1.03, p = 0.78).
3.3. Publication Bias and Meta-Regressions
Funnel plot examination (Supplemental Figure S1) suggested the absence of publication bias and of small-study effect, confirmed by the Egger’s test for all-cause mortality and CVD mortality (Egger’s p = 0.713 and p = 0.852, respectively; Supplemental Figure S1). A significant publication bias (Egger’s p < 0.001) was observed for studies on CVD events. These results were confirmed by Duval and Tweedie’s trim and fill analysis.
Regression models showed that none of the clinical and demographic characteristics evaluated impacted on the difference in all-cause mortality between subjects in the highest versus lowest white meat consumption categories (Supplemental Table S2). No meta-regression analyses were performed for CV mortality and CV events due to the lack of statistically significant differences in the main analysis.
4. Discussion
Diet is one of the major modifiable factors that affect disease risk, thus it is of the greatest importance to identify dietary habits that decrease the risk of disease and death. The relationship of red and processed meat consumption with increased risk of all-cause death and incidence of CVD has been consistently demonstrated [5,10,12,13,14,15,17,31,37,38,39,41,42,46]; however, it remains unclear whether the adverse health effects associated with red and processed meat consumption are also shared by white meat [11,15,22,23]. We conducted a comprehensive meta-analysis of cohort studies exploring the relationship between withe meat consumption, total mortality and incident CV events (fatal or non-fatal).
The results have shown a 6% significantly lower all-cause mortality for subjects in the highest vs. the lowest white meat consumption category and an overall neutral association with CV mortality and morbidity. The findings for all cause death and CV death were fairly consistent when the analyses were stratified by geographical area (i.e., America, Asia, Europe) to partly account for different background diet and unmeasured lifestyle-related factors, including food preparation techniques. As for non-fatal CV events, the Asian studies indicated a significant risk reduction at variance with those from America and Europe. These should be further investigated due to the low number of meta-analyzed studies. There were not enough studies to perform the analyses by gender; however, the meta-regression analyses indicated that the clinical and demographic characteristics of the participants, including gender, did not impact on the difference in all-cause mortality.
In a previous meta-analysis of six studies, one of which also included fish in the white meat definition, Abete et al. have shown a weak and inverse association between white meat consumption and all-cause death in women only, and no relationship with CV mortality [15]. These conclusions, according to the authors themselves, were however weak, due to the small number and low quality of the meta-analyzed studies; furthermore, no data were available on non-fatal CV endpoints. Following the completion of the study by Abete et al. in 2014 several large prospective studies on the topic have been published, including some with non-fatal CV end points [5,26,28,30,36,38,42,44,46]. The present meta-analysis significantly expands current knowledge on the association of white meat consumption with total and CV mortality by including a much larger number of studies with a greater variety in geographical attribution, and studies with non-fatal cardiovascular outcomes. This allows a larger statistical power and a sub-analysis by geographical area and by type of outcome (i.e., fatal or non-fatal CVD). Furthermore, we better defined white meat by excluding studies on fish, due to the different health impact of fish and poultry consumption, which may have confounded prior analyses.
The interpretation of the effects of white meat consumption on health is a difficult task, as subjects consuming more white meat are, at the same time, consuming less red meat. On the other hand, people with a low red meat intake may prefer others protein sources, such as proteins from vegetable origin that could have per se a beneficial impact on cardiovascular health. However, it is important to underline that white meat, unlike products of vegetable origin, is a source of high-quality proteins and may therefore fully substitute red meat.
Furthermore, the background diet and the food preparation techniques, associated with the regular consumption of the different types of meat may also have a role which is difficult to account for. There are, however, plausible mechanisms which may partly mediate a different association of processed and red meat or white meat with health outcomes [47]. Meats are broadly classified into red (i.e., beef, pork, lamb) or white (i.e., chicken, turkey, rabbit) based on the contents of fat, cholesterol, and iron; furthermore, meats can be consumed fresh or processed with the addition of salt and chemicals. The different kinds of meats have important nutritional differences which may impact on health outcomes. Poultry meats, as compared with beef, lamb, or pork meat are characterized by a lower fat content, a more favorable fatty acid profile (i.e., mostly unsaturated fatty acids) [17,18,19] and a lower content of heme iron. Both saturated fat and heme iron are recognized factors involved in the promotion of atherosclerosis [48,49]. In addition, preservatives, such as sodium and nitrates, largely used in the preparation of processed meat, promote hypertension, insulin resistance and endothelial dysfunction, all of which are established CV risk factors.
Last, but not least, the study findings need to be evaluated also in the light of the growing awareness on the importance of the foods and beverages we produce, choose and consume in relation to their environmental sustainability [50,51]. It has been estimated that producing poultry meat has a substantially lower ecological impact than producing beef meat [50,51]. Therefore, promoting a moderate consumption of unprocessed white meat, particularly if in substitution of red and processed meat, emerges as a potential strategy to improve human health and, at the same time, limit environmental deterioration.
This study has some strengths. First, it includes a large number of studies and participants (11 studies for all cause death, 10 studies for CV death, and 10 for non-fatal CV events), thus allowing sufficient statistical power, second it provides data on non-fatal CV events which were not available before, furthermore, the analysis by geographical area confers internal consistency to the results by partly adjusting for unmeasured cultural and lifestyle related factors including background diet and procedures of food preparation.
The potential limitations need also to be discussed. First, we must acknowledge that studies included in this meta-analysis have different inclusion and exclusion criteria and therefore subjects with different clinical and demographic characteristics were considered in the overall analysis. Moreover, meta-analyses are performed on aggregate data and the multivariate approach allows for the adjustment for some, but not all, potential confounders. Thus, although meta-regression models were used to refine our analyses by assessing the influence of most clinical and demographic variables on the observed results, caution is necessary in the interpretation of results due to potential residual confounding. Finally, our results were affected by a significant heterogeneity. Although it was not possible to definitively establish sources of such heterogeneity, all findings were substantially confirmed by appropriate sensitivity and subgroup analyses and the impact of clinical and demographic variables on the study results was evaluated by means of meta-regression models. Furthermore, we excluded the presence of publication bias by using different methods, and in case of significant bias our results were confirmed after trimming and imputing studies. In addition, we found heterogeneity among studies in the definition of white meat intake in the lowest and the highest consumption group (for example, servings per day or per week, or grams per day) and in some studies there was missing information regarding type of white meat (for example, total white meat, or only chicken). Moreover, the potential confounding of cooking methods and preparation techniques could not be assessed.
5. Conclusions
In conclusion, the study shows a robust and inverse association between the consumption of unprocessed white meat and all-cause mortality, and a neutral association with CV mortality and morbidity. These findings highlight the importance of differentiating the meat types and suggest that white meat might be a ‘healthy’ and environmentally more sustainable alternative to red and processed meat consumption. Most people consume meats on a regular basis and therefore, notwithstanding the relatively modest risk reduction (6%), the findings of this study have relevant public health implications and provide evidence to inform dietary guidelines for a healthy and environmentally sustainable nutrition.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/13/2/676/s1, Figure S1: Funnel plots of the log OR versus the standard error for studies evaluating all-cause mortality (Panel A), CVD mortality (Panel B), and CVD events (Panel C), Table S1: Quality of studies assessment (Newcastle-Ottawa scale) for included studies, Table S2: Meta-regression analyses for all-cause mortality.
Author Contributions
G.R. and O.V. are responsible for study design; R.L., M.V., I.C., A.G., G.R., O.V., are responsible for writing; G.R. and O.V. have primary responsibility for the final content. All authors have read and agreed to the published version of the manuscript.
Funding
The present analyses have been supported by a research grant from the “Barilla Center for Food and Nutrition Foundation (BCFN)” within the framework of a project aimed at an evidence based reformulation of the Food Pyramid for the prevention of cardiovascular disease. The funder had no role in study design, collection, analysis, and interpretation of data; in the writing of the manuscript and in the decision to submit the article for publication.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Meier, T.; Gräfe, K.; Senn, F.; Sur, P.; Stangl, G.I.; Dawczynski, C.; März, W.; Kleber, M.E.; Lorkowski, S. Cardiovascular mortality attributable to dietary risk factors in 51 countries in the WHO European Region from 1990 to 2016: A systematic analysis of the Global Burden of Disease Study. Eur. J. Epidemiol. 2019, 34, 37–55. [Google Scholar] [CrossRef]
- Calabrese, I.; Riccardi, G. Effectiveness of changes in diet composition on reducing the incidence of cardiovascular disease. Curr. Cardiol. Rep. 2019, 21, 88. [Google Scholar] [CrossRef] [PubMed]
- Riccardi, G.; Vaccaro, O.; Costabile, G.; Rivellese, A.A. How well can we control dyslipidemias through lifestyle modifications? Curr. Cardiol. Rep. 2016, 18, 66. [Google Scholar] [CrossRef]
- Key, T.J.; Appleby, P.N.; Bradbury, K.E.; Sweeting, M.; Wood, A.; Johansson, I.; Kühn, T.; Steur, M.; Weiderpass, E.; Wennberg, M.; et al. Consumption of meat, fish, dairy products, and eggs and risk of ischemic heart disease. Circulation 2019, 139, 2835–2845. [Google Scholar] [CrossRef]
- Tieri, M.; Ghelfi, F.; Vitale, M.; Vetrani, C.; Marventano, S.; Lafranconi, A.; Godos, J.; Titta, L.; Gambera, A.; Alonzo, E.; et al. Whole grain consumption and human health: An umbrella review of observational studies. Int. J. Food Sci. Nutr. 2020, 71, 668–677. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Lampousi, A.M.; Knüppel, S.; Iqbal, K.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food groups and risk of all-cause mortality: A systematic review and me-ta-analysis of prospective studies. Am. J. Clin. Nutr. 2017, 105, 1462–1473. [Google Scholar] [CrossRef] [PubMed]
- Forouzanfar, M.H.; Alexander, L.W.G.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.T.; Casey, D.; Coates, M.M.; Cohen, A.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef]
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef]
- Lee, J.E.; McLerran, D.F.; Rolland, B.; Chen, Y.; Grant, E.J.; Vedanthan, R.; Inoue, M.; Tsugane, S.; Gao, Y.-T.; Tsuji, I.; et al. Meat intake and cause-specific mortality: A pooled analysis of Asian prospective cohort studies. Am. J. Clin. Nutr. 2013, 98, 1032–1041. [Google Scholar] [CrossRef]
- Sinha, R.; Cross, A.J.; Graubard, B.I.; Leitzmann, M.F.; Schatzkin, A. Meat intake and mortality. Arch. Intern. Med. 2009, 169, 562–571. [Google Scholar] [CrossRef]
- Wang, X.; Lin, X.; Ouyang, Y.Y.; Liu, J.; Zhao, G.; Pan, A.; Hu, F.B. Red and processed meat consumption and mortality: Dose–response meta-analysis of prospective cohort studies. Public Health Nutr. 2016, 19, 893–905. [Google Scholar] [CrossRef]
- Larsson, S.C.; Orsini, N. Red meat and processed meat consumption and all-cause mortality: A meta-analysis. Am. J. Epidemiol. 2014, 179, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Zeraatkar, D.; Han, M.A.; Guyatt, G.H.; Vernooij, R.W.; El Dib, R.; Cheung, K.; Milio, K.; Zworth, M.; Bartoszko, J.J.; Valli, C.; et al. Red and processed meat consumption and risk for all-cause mortality and cardiometabolic outcomes. Ann. Intern. Med. 2019, 171, 703. [Google Scholar] [CrossRef]
- Abete, I.; Romaguera, D.; Vieira, A.R.; De Munain, A.L.; Norat, T. Association between total, processed, red and white meat consumption and all-cause, CVD and IHD mortality: A meta-analysis of cohort studies. Br. J. Nutr. 2014, 112, 762–775. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Ursin, G.; Veierød, M.B. Meat consumption and the risk of type 2 diabetes: A systematic review and meta-analysis of cohort studies. Diabetologia 2009, 52, 2277–2287. [Google Scholar] [CrossRef]
- Micha, R.; Wallace, S.K.; Mozaffarian, D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus. Circulation 2010, 121, 2271–2283. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Michas, G.; Mozaffarian, D. Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes—An updated review of the evidence. Curr. Atheroscler. Rep. 2012, 14, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Michas, G.; Lajous, M.; Mozaffarian, D. Processing of meats and cardiovascular risk: Time to focus on preservatives. BMC Med. 2013, 11, 136. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.S.M.; Lau, R.; Aune, D.; Vieira, R.; Greenwood, D.C.; Kampman, E.; Norat, T. Red and processed meat and colorectal cancer incidence: Meta-analysis of prospective studies. PLoS ONE 2011, 6, e20456. [Google Scholar] [CrossRef]
- Bechthold, A.; Boeing, H.; Schwedhelm, C.; Hoffmann, G.; Knüppel, S.; Iqbal, K.; De Henauw, S.; Michels, N.; Devleesschauwer, B.; Schlesinger, S.; et al. Food groups and risk of coronary heart disease, stroke and heart failure: A systematic review and dose-response meta-analysis of prospective studies. Crit. Rev. Food Sci. Nutr. 2019, 59, 1071–1090. [Google Scholar] [CrossRef]
- Bernstein, A.M.; Sun, Q.; Hu, F.B.; Stampfer, M.J.; Manson, J.E.; Willett, W.C. Major dietary protein sources and risk of coronary heart disease in women. Circulation 2010, 122, 876–883. [Google Scholar] [CrossRef]
- Becerra-Tomás, N.; Babio, N.; Martínez-González, M.Á.; Corella, D.; Estruch, R.; Ros, E.; Fitó, M.; Serra-Majem, L.; Salaverria, I.; Lamuela-Raventós, R.M.; et al. Replacing red meat and processed red meat for white meat, fish, legumes or eggs is associated with lower risk of incidence of metabolic syndrome. Clin. Nutr. 2016, 35, 1442–1449. [Google Scholar] [CrossRef]
- Hu, F.B. Protein, body weight, and cardiovascular health. Am. J. Clin. Nutr. 2005, 82, 242S–247S. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Etemadi, A.; Sinha, R.; Ward, M.H.; Graubard, B.I.; Inoue-Choi, M.; Dawsey, S.M.; Abnet, C.C. Mortality from different causes associated with meat, heme iron, nitrates, and nitrites in the NIH-AARP Diet and Health Study: Population based cohort study. BMJ 2017, 357, j1957. [Google Scholar] [CrossRef]
- Sluik, D.; Boeing, H.; Li, K.; Kaaks, R.; Johnsen, N.F.; Tjønneland, A.; Arriola, L.; Barricarte, A.; Masala, G.; Grioni, S.; et al. Lifestyle factors and mortality risk in individuals with diabetes mellitus: Are the associations different from those in individuals without diabetes? Diabetologia 2013, 57, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Son, J.; Jang, J.; Kang, R.; Chung, H.-K.; Lee, K.W.; Lee, S.-M.; Lim, H.; Shin, M.-J. Unprocessed meat consumption and incident cardiovascular diseases in Korean adults: The Korean Genome and Epidemiology study (KoGES). Nutrients 2017, 9, 498. [Google Scholar] [CrossRef] [PubMed]
- Sauvaget, C.; Nagano, J.; Allen, N.; Grant, E.J.; Beral, V. Intake of animal products and stroke mortality in the Hiroshima/Nagasaki Life Span study. Int. J. Epidemiol. 2003, 32, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Tong, T.Y.N.; Appleby, P.N.; Key, T.J.; Dahm, C.C.; Overvad, K.; Olsen, A.; Tjønneland, A.; Katzke, V.; Kühn, T.; Boeing, H.; et al. The associations of major foods and fibre with risks of ischaemic and haemorrhagic stroke: A prospective study of 418,329 participants in the EPIC cohort across nine European countries. Eur. Heart J. 2020, 41, 2632–2640. [Google Scholar] [CrossRef]
- Wang, Y.; Jacobs, E.J.; Shah, R.A.; Stevens, V.L.; Gansler, T.; McCullough, M.L. Red and processed meat, poultry, fish, and egg intakes and cause-specific and all-cause mortality among men with nonmetastatic prostate cancer in a U.S. cohort. Cancer Epidemiol. Biomark. Prev. 2020, 29, 1029–1038. [Google Scholar] [CrossRef] [PubMed]
- Baik, I.; Cho, N.H.; Kim, S.H.; Shin, C. Dietary information improves cardiovascular disease risk prediction models. Eur. J. Clin. Nutr. 2012, 67, 25–30. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Department of Epidemiology and Community Medicine, University of Ottawa, Canada, 2011. University of Ottawa, Canada. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 19 February 2021).
- Sun, Y.; Liu, B.; Snetselaar, L.G.; Robinson, J.G.; Wallace, R.B.; Peterson, L.L.; Bao, W. Association of fried food consumption with all cause, cardiovascular, and cancer mortality: Prospective cohort study. BMJ 2019, 364, k5420. [Google Scholar] [CrossRef] [PubMed]
- Nagao, M.A.; Iso, H.; Yamagishi, K.; Date, C.; Tamakoshi, A. Meat consumption in relation to mortality from cardiovascular disease among Japanese men and women. Eur. J. Clin. Nutr. 2012, 66, 687–693. [Google Scholar] [CrossRef]
- Würtz, A.M.L.; Hansen, M.D.; Tjønneland, A.; Rimm, E.B.; Schmidt, E.B.; Overvad, K.; Jakobsen, M.U. Substitution of meat and fish with vegetables or potatoes and risk of myocardial infarction. Br. J. Nutr. 2016, 116, 1602–1610. [Google Scholar] [CrossRef] [PubMed]
- Haring, B.; Gronroos, N.; Nettleton, J.A.; Von Ballmoos, M.C.W.; Selvin, E.; Alonso, A. Dietary protein intake and coronary heart disease in a large community based cohort: Results from the Atherosclerosis Risk in Communities (ARIC) study. PLoS ONE 2014, 9, e109552. [Google Scholar] [CrossRef] [PubMed]
- Haring, B.; Misialek, J.R.; Rebholz, C.M.; Petruski-Ivleva, N.; Gottesman, R.F.; Mosley, T.H.; Alonso, A. Association of dietary protein consumption with incident silent cerebral infarcts and stroke. Stroke 2015, 46, 3443–3450. [Google Scholar] [CrossRef]
- Kappeler, R.; Eichholzer, M.; Rohrmann, S. Meat consumption and diet quality and mortality in NHANES III. Eur. J. Clin. Nutr. 2013, 67, 598–606. [Google Scholar] [CrossRef] [PubMed]
- Rohrmann, S.; Overvad, K.; Bueno-De-Mesquita, H.B.; Jakobsen, M.U.; Egeberg, R.; Tjønneland, A.; Nailler, L.; Boutron-Ruault, M.-C.; Clavel-Chapelon, F.; Krogh, V.; et al. Meat consumption and mortality—Results from the European Prospective Investigation into Cancer and Nutrition. BMC Med. 2013, 11, 63. [Google Scholar] [CrossRef] [PubMed]
- Takata, Y.; Shu, X.-O.; Gao, Y.-T.; Li, H.; Zhang, X.; Gao, J.; Cai, H.; Yang, G.; Xiang, Y.-B.; Zheng, W. Red meat and poultry intakes and risk of total and cause-specific mortality: Results from cohort studies of Chinese adults in Shanghai. PLoS ONE 2013, 8, e56963. [Google Scholar] [CrossRef] [PubMed]
- Van den Brandt, P.A. Red meat, processed meat, and other dietary protein sources and risk of overall and cause-specific mortality in The Netherlands Cohort Study. Eur. J. Epidemiol. 2019, 34, 351–369. [Google Scholar] [CrossRef]
- Whiteman, D.; Muir, J.; Jones, L.; Murphy, M.; Key, T. Dietary questions as determinants of mortality: The OXCHECK experience. Public Health Nutr. 1999, 2, 477–487. [Google Scholar] [CrossRef]
- Zhong, V.W.; Van Horn, L.; Greenland, P.; Carnethon, M.R.; Ning, H.; Wilkins, J.T.; Lloyd-Jones, D.M.; Allen, N.B. Associations of processed meat, unprocessed red meat, poultry, or fish intake with incident cardiovascular disease and all-cause mortality. JAMA Intern. Med. 2020, 180, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, A.M.; Pan, A.; Rexrode, K.M.; Stampfer, M.; Hu, F.B.; Mozaffarian, D.; Willett, W.C. Dietary protein sources and the risk of stroke in men and women. Stroke 2012, 43, 637–644. [Google Scholar] [CrossRef]
- Farvid, M.S.; Malekshah, A.F.; Pourshams, A.; Poustchi, H.; Sepanlou, S.G.; Sharafkhah, M.; Khoshnia, M.; Farvid, M.; Abnet, C.C.; Kamangar, F.; et al. Dietary protein sources and all-cause and cause-specific mortality: The Golestan Cohort study in Iran. Am. J. Prev. Med. 2017, 52, 237–248. [Google Scholar] [CrossRef]
- Durante, A.; Bronzato, S. A contemporary review of the relationship between red meat consumption and cardiovascular risk. Int. J. Prev. Med. 2017, 8, 40. [Google Scholar] [CrossRef]
- Fang, X.; An, P.; Wang, H.; Wang, X.; Shen, X.; Li, X.; Min, J.; Liu, S.; Wang, F. Dietary intake of heme iron and risk of cardiovascular disease: A dose–response meta-analysis of prospective cohort studies. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 24–35. [Google Scholar] [CrossRef]
- Han, M.; Guan, L.; Ren, Y.; Zhao, Y.; Liu, D.; Zhang, D.; Liu, L.; Liu, F.; Chen, X.; Cheng, C.; et al. Dietary iron intake and risk of death due to cardiovascular diseases: A systematic review and dose-response meta-analysis of prospective cohort studies. Asia Pac. J. Clin. Nutr 2020, 29, 309–321. [Google Scholar] [PubMed]
- Rosi, A.; Mena, P.; Pellegrini, N.; Turroni, S.; Neviani, E.; Ferrocino, I.; Di Cagno, R.; Ruini, L.; Ciati, R.; Angelino, D.; et al. Environmental impact of omnivorous, ovo-lacto-vegetarian, and vegan diet. Sci. Rep. 2017, 7, 6105. [Google Scholar] [CrossRef] [PubMed]
- Carlsson-Kanyama, A.; González, A.D. Potential contributions of food consumption patterns to climate change. Am. J. Clin. Nutr. 2009, 89, 1704S–1709S. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).