Geographical Variability Affects CCHFV Detection by RT–PCR: A Tool for In-Silico Evaluation of Molecular Assays
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Phylogenetic Analysis
2.3. Software Description
2.4. Assays Evaluation
- The primers/probe set of the assay must not have had more than 3 mismatches with respect to every genome in the clade;
- The primers of the assay must not have had more than 1 critical mismatch, i.e., a mismatch located at the last 5 positions of 3’-end;
- Within a clade, more than 50% of viral strains must have had fully matched the primers/probe set (therefore, we could expect that new sequences owing to the same clade would not have too many mismatches).
3. Results
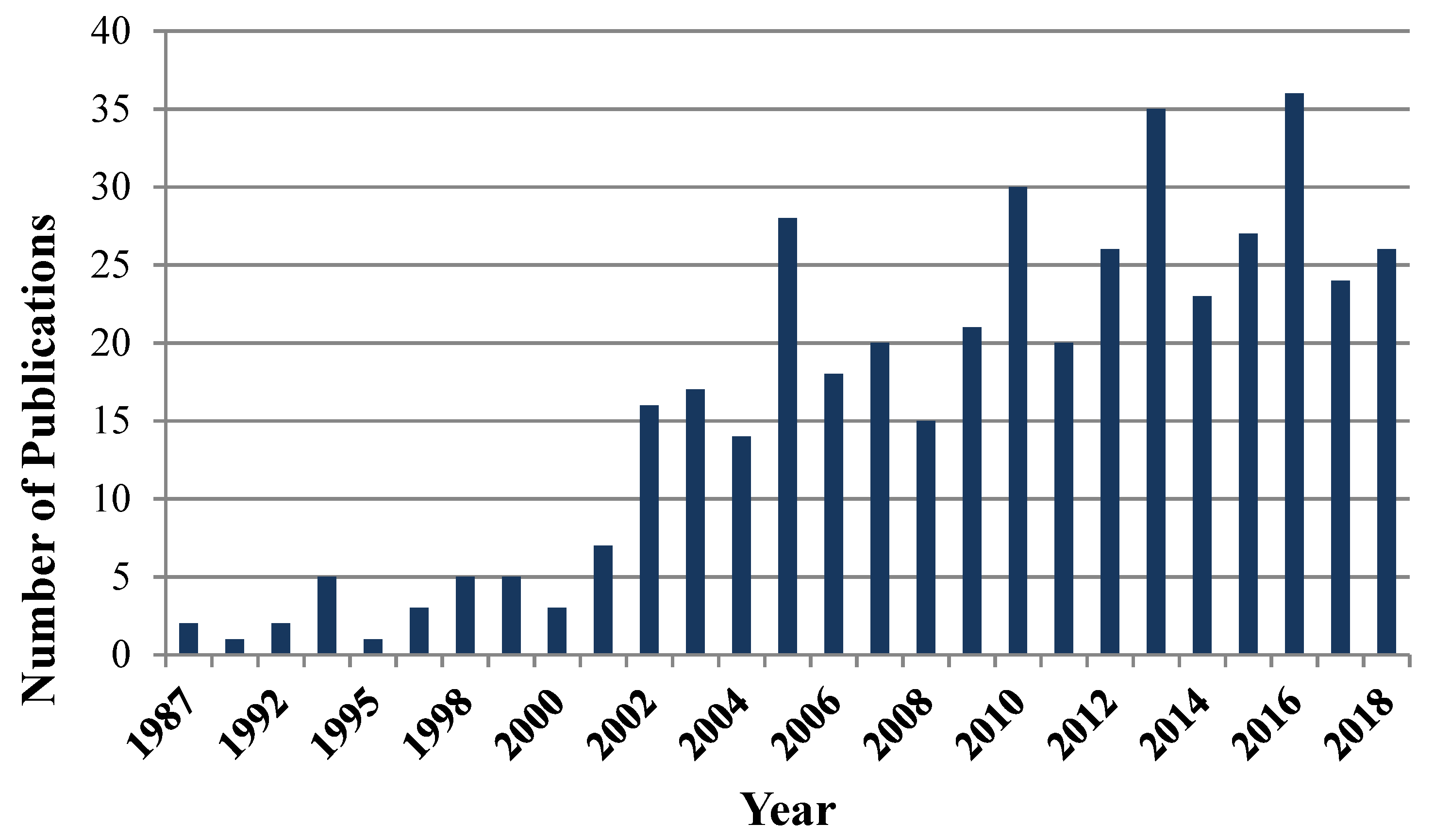
3.1. Data Collection
3.2. Phylogenetic Analysis
3.3. Assays Evaluation
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- WHO Roadmap for Research and Product Development against Crimean-Congo Haemorrhagic Fever (CCHF). Available online: http://www.who.int/blueprint/priority-diseases/key-action/cchf-draft-r-and-d-roadmap.pdf?ua=1 (accessed on 12 June 2019).
- European Centre for Disease Prevention and Control. Public Health Risks Related to Communicable Diseases During the 2018 Hajj, Saudi Arabia, 19–24 August 2018–2 August 2018; ECDC: Stockholm, Sweden, 2018; Available online: https://ecdc.europa.eu/sites/portal/files/documents/risks-diseases-hajj-saudi-arabia-rapid-risk-assessment-24-august-2018.pdf (accessed on 12 June 2019).
- Ergönül, Ö.; Keske, Ş.; Çeldir, M.G.; Kara, İ.A.; Pshenichnaya, N.; Abuova, G.; Blumberg, L.; Gönen, M. Systematic Review and Meta-analysis of Postexposure Prophylaxis for Crimean-Congo Hemorrhagic Fever Virus among Healthcare Workers. Emerg. Infect. Dis. 2018, 24, 1642–1648. [Google Scholar] [CrossRef] [PubMed]
- Bartolini, B.; Gruber, C.E.; Koopmans, M.; Avšič, T.; Bino, S.; Christova, I.; Grunow, R.; Hewson, R.; Korukluoglu, G.; Lemos, C.M.; et al. Laboratory management of Crimean-Congo haemorrhagic fever virus infections: Perspectives from two European networks. Eurosurveillance 2019, 24. [Google Scholar] [CrossRef] [PubMed]
- Bente, D.A.; Forrester, N.L.; Watts, D.M.; McAuley, A.J.; Whitehouse, C.A.; Bray, M. Crimean-Congo hemorrhagic fever: History, epidemiology, pathogenesis, clinical syndrome and genetic diversity. Antivir. Res. 2013, 100, 159–189. [Google Scholar] [CrossRef] [PubMed]
- James, N. Bunyaviridae. In Fenner’s Veterinary Virology; Elsevier: Amsterdam, The Netherlands, 2017; pp. 411–424. ISBN 978-0-12-800946-8. [Google Scholar]
- Palomar, A.M.; Portillo, A.; Santibáñez, P.; Mazuelas, D.; Arizaga, J.; Crespo, A.; Gutiérrez, Ó.; Cuadrado, J.F.; Oteo, J.A. Crimean-Congo Hemorrhagic Fever Virus in Ticks from Migratory Birds, Morocco1. Emerg. Infect. Dis. 2013, 19, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Gargili, A.; Estrada-Peña, A.; Spengler, J.R.; Lukashev, A.; Nuttall, P.A.; Bente, D.A. The role of ticks in the maintenance and transmission of Crimean-Congo hemorrhagic fever virus: A review of published field and laboratory studies. Antivir. Res. 2017, 144, 93–119. [Google Scholar] [CrossRef]
- Sadeuh-Mba, S.A.; Wansi, G.M.; Demanou, M.; Gessain, A.; Njouom, R. Serological evidence of rift valley fever Phlebovirus and Crimean-Congo hemorrhagic fever orthonairovirus infections among pygmies in the east region of Cameroon. Virol. J. 2018, 15, 63. [Google Scholar] [CrossRef] [PubMed]
- Balinandi, S.; Patel, K.; Ojwang, J.; Kyondo, J.; Mulei, S.; Tumusiime, A.; Lubwama, B.; Nyakarahuka, L.; Klena, J.D.; Lutwama, J.; et al. Investigation of an isolated case of human Crimean-Congo hemorrhagic fever in Central Uganda, 2015. Int. J. Infect. Dis. 2018, 68, 88–93. [Google Scholar] [CrossRef]
- Zehender, G.; Ebranati, E.; Shkjezi, R.; Papa, A.; Luzzago, C.; Gabanelli, E.; Lo Presti, A.; Lai, A.; Rezza, G.; Galli, M.; et al. Bayesian Phylogeography of Crimean-Congo Hemorrhagic Fever Virus in Europe. PLoS ONE 2013, 8, 79663. [Google Scholar] [CrossRef]
- Emmerich, P.; Jakupi, X.; von Possel, R.; Berisha, L.; Halili, B.; Günther, S.; Cadar, D.; Ahmeti, S.; Schmidt-Chanasit, J. Viral metagenomics, genetic and evolutionary characteristics of Crimean-Congo hemorrhagic fever orthonairovirus in humans, Kosovo. Infect. Genet. Evol. 2018, 65, 6–11. [Google Scholar] [CrossRef]
- Lukashev, A.N.; Deviatkin, A.A. Phylodynamics of Crimean Congo hemorrhagic fever virus in South Russia. Infect. Genet. Evol. 2018, 59, 23–27. [Google Scholar] [CrossRef]
- Yadav, P.D.; Patil, D.Y.; Shete, A.M.; Kokate, P.; Goyal, P.; Jadhav, S.; Sinha, S.; Zawar, D.; Sharma, S.K.; Kapil, A.; et al. Nosocomial infection of CCHF among health care workers in Rajasthan, India. BMC Infect. Dis. 2016, 16, 624. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.D.; Thacker, S.; Patil, D.Y.; Jain, R.; Mourya, D.T. Crimean-Congo Hemorrhagic Fever in Migrant Worker Returning from Oman to India, 2016. Emerg. Infect. Dis. 2017, 23, 1005–1008. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Shen, S.; Fang, Y.; Liu, J.; Su, Z.; Liang, J.; Zhang, Z.; Wu, Q.; Wang, C.; Abudurexiti, A.; et al. Isolation, Characterization, and Phylogenetic Analysis of Two New Crimean-Congo Hemorrhagic Fever Virus Strains from the Northern Region of Xinjiang Province, China. Virol. Sin. 2018, 33, 74–86. [Google Scholar] [CrossRef] [PubMed]
- Moming, A.; Yue, X.; Shen, S.; Chang, C.; Wang, C.; Luo, T.; Zhang, Y.; Guo, R.; Hu, Z.; Zhang, Y.; et al. Prevalence and Phylogenetic Analysis of Crimean-Congo Hemorrhagic Fever Virus in Ticks from Different Ecosystems in Xinjiang, China. Virol. Sin. 2018, 33, 67–73. [Google Scholar] [CrossRef]
- Papa, A.; Chaligiannis, I.; Kontana, N.; Sourba, T.; Tsioka, K.; Tsatsaris, A.; Sotiraki, S. A novel AP92-like Crimean-Congo hemorrhagic fever virus strain, Greece. Ticks Tick-Borne Dis. 2014, 5, 590–593. [Google Scholar] [CrossRef]
- Ozkaya, E.; Dincer, E.; Carhan, A.; Uyar, Y.; Ertek, M.; Whitehouse, C.A.; Ozkul, A. Molecular epidemiology of Crimean-Congo hemorrhagic fever virus in Turkey: Occurrence of local topotype. Virus Res. 2010, 149, 64–70. [Google Scholar] [CrossRef]
- Estrada-Peña, A.; Palomar, A.M.; Santibáñez, P.; Sánchez, N.; Habela, M.A.; Portillo, A.; Romero, L.; Oteo, J.A. Crimean-Congo Hemorrhagic Fever Virus in Ticks, Southwestern Europe, 2010. Emerg. Infect. Dis. 2012, 18, 179–180. [Google Scholar] [CrossRef]
- Negredo, A.; Habela, M.Á.; Ramírez de Arellano, E.; Diez, F.; Lasala, F.; López, P.; Sarriá, A.; Labiod, N.; Calero-Bernal, R.; Arenas, M.; et al. Survey of Crimean-Congo Hemorrhagic Fever Enzootic Focus, Spain, 2011–2015. Emerg. Infect. Dis. 2019, 25, 1177–1184. [Google Scholar] [CrossRef]
- Negredo, A.; de la Calle-Prieto, F.; Palencia-Herrejón, E.; Mora-Rillo, M.; Astray-Mochales, J.; Sánchez-Seco, M.P.; Bermejo Lopez, E.; Menárguez, J.; Fernández-Cruz, A.; Sánchez-Artola, B.; et al. Autochthonous Crimean-Congo Hemorrhagic Fever in Spain. N. Engl. J. Med. 2017, 377, 154–161. [Google Scholar] [CrossRef]
- ECDC Communicable Disease Threats Report (CDTR) Week 50, 9–15 December 2018. Available online: https://ecdc.europa.eu/sites/portal/files/documents/communicable-disease-threats-report-18-aug-2018.pdf (accessed on 12 June 2019).
- Papa, A.; Papadopoulou, E.; Tsioka, K.; Kontana, A.; Pappa, S.; Melidou, A.; Giadinis, N.D. Isolation and whole-genome sequencing of a Crimean-Congo hemorrhagic fever virus strain, Greece. Ticks Tick-Borne Dis. 2018, 9, 788–791. [Google Scholar] [CrossRef]
- Corman, V.M.; Rasche, A.; Baronti, C.; Cadar, D.; Goorhuis, A.; Schinkel, J.; Molenkamp, R.; Bleicker, T.; Brünink, S.; Eschbach, M.; et al. Clinical comparison, standardization and optimization of Zika virus molecular detection. Bull. World Health Organ. 2016, 829, 27. [Google Scholar]
- Lefever, S.; Pattyn, F.; Hellemans, J.; Vandesompele, J. Single-Nucleotide Polymorphisms and Other Mismatches Reduce Performance of Quantitative PCR Assays. Clin. Chem. 2013, 59, 1470–1480. [Google Scholar] [CrossRef] [PubMed]
- Stadhouders, R.; Pas, S.D.; Anber, J.; Voermans, J.; Mes, T.H.M.; Schutten, M. The Effect of Primer-Template Mismatches on the Detection and Quantification of Nucleic Acids Using the 5′ Nuclease Assay. J. Mol. Diagn. 2010, 12, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Basu, C. PCR Primer Design: Methods in Molecular Biology, 2nd ed.; Humana Press: New York, NY, USA, 2015; ISBN 978-1-4939-2364-9. [Google Scholar]
- Kim, H.; Kang, N.; Chon, K.-W.; Kim, S.; Lee, N.; Koo, J.; Kim, M.-S. MRPrimer: A MapReduce-based method for the thorough design of valid and ranked primers for PCR. Nucleic Acids Res. 2015, 43, 130. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Seco, M.P. (National Centre of Microbiology, Institute of Health “Carlos III”, Majadahonda, 28220 Madrid, Spain). Personal communication, 2018.
- Lukashev, A.N.; Klimentov, A.S.; Smirnova, S.E.; Dzagurova, T.K.; Drexler, J.F.; Gmyl, A.P. Phylogeography of Crimean Congo Hemorrhagic Fever Virus. PLoS ONE 2016, 11, 166744. [Google Scholar] [CrossRef]
- Vanneste, K.; Garlant, L.; Broeders, S.; Van Gucht, S.; Roosens, N.H. Application of whole genome data for in silico evaluation of primers and probes routinely employed for the detection of viral species by RT-qPCR using dengue virus as a case study. BMC Bioinf. 2018, 19, 312. [Google Scholar] [CrossRef]
- Cornish-Bowden, A. Nomenclature for incompletely specified bases in nucleic acid sequences: Recommendations 1984. Eur. J. Biochem. 1985, 13, 3021. [Google Scholar] [CrossRef]
- Drosten, C.; Gottig, S.; Schilling, S.; Asper, M.; Panning, M.; Schmitz, H.; Gunther, S. Rapid Detection and Quantification of RNA of Ebola and Marburg Viruses, Lassa Virus, Crimean-Congo Hemorrhagic Fever Virus, Rift Valley Fever Virus, Dengue Virus, and Yellow Fever Virus by Real-Time Reverse Transcription-PCR. J. Clin. Microbiol. 2002, 40, 2323–2330. [Google Scholar] [CrossRef]
- Deyde, V.M.; Khristova, M.L.; Rollin, P.E.; Ksiazek, T.G.; Nichol, S.T. Crimean-Congo Hemorrhagic Fever Virus Genomics and Global Diversity. J. Virol. 2006, 80, 8834–8842. [Google Scholar] [CrossRef]
- Schwarz, T.F.; Longson, M.; Shurie, H.; Acharya, U.G.; Gilch, S.; Zahir, A.R.M.; Nitschko, H.; Ameen, A.; Nsanze, H.; Jager, G. Polymerase Chain Reaction for Diagnosis and Identification of Distinct Variants of Crimean-Congo Hemorrhagic Fever Virus in the United Arab Emirates. Am. J. Trop. Med. Hyg. 1996, 55, 190–196. [Google Scholar] [CrossRef]
- Midilli, K.; Gargılı, A.; Ergonul, O.; Şengöz, G.; Ozturk, R.; Bakar, M.; Jongejan, F. Imported Crimean-Congo hemorrhagic fever cases in Istanbul. BMC Infect. Dis. 2007, 7, 54. [Google Scholar] [CrossRef] [PubMed]
- Midilli, K.; Gargılı, A.; Ergonul, O.; Elevli, M.; Ergin, S.; Turan, N.; Şengöz, G.; Ozturk, R.; Bakar, M. The first clinical case due to AP92 like strain of Crimean-Congo Hemorrhagic Fever virus and a field survey. BMC Infect. Dis. 2009, 9, 90. [Google Scholar] [CrossRef] [PubMed]
- Elata, A.T.; Karsany, M.S.; Elageb, R.M.; Hussain, M.A.; Eltom, K.H.; Elbashir, M.I.; Aradaib, I.E. A nosocomial transmission of crimean-congo hemorrhagic fever to an attending physician in north kordufan, Sudan. Virol. J. 2011, 8, 303. [Google Scholar] [CrossRef] [PubMed]
- Yapar, M.; Aydogan, H.; Pahsa, A.; Besirbellioglu, B.A.; Bodur, H.; Basustaoglu, A.C.; Guney, C.; Avci, I.Y.; Sener, K.; Setteh, M.H.A.; et al. Rapid and Quantitative Detection of Crimean-Congo Hemorrhagic Fever Virus by One-Step Real-Time Reverse Transcriptase-PCR. Jpn. J. Infect. Dis. 2005, 58, 358. [Google Scholar]
- Duh, D.; Saksida, A.; Petrovec, M.; Dedushaj, I.; Avšič-Županc, T. Novel one-step real-time RT-PCR assay for rapid and specific diagnosis of Crimean-Congo hemorrhagic fever encountered in the Balkans. J. Virol. Methods 2006, 133, 175–179. [Google Scholar] [CrossRef]
- Garrison, A.R.; Alakbarova, S.; Kulesh, D.A.; Khodjaev, S.; Endy, T.P.; Shezmukhamedova, D.; Paragas, J. Development of a TaqMan®—Minor Groove Binding Protein Assay for the Detection and Quantification of Crimean-Congo Hemorrhagic Fever Virus. Am. J. Trop. Med. Hyg. 2007, 77, 514–520. [Google Scholar] [CrossRef][Green Version]
- Wölfel, R.; Paweska, J.T.; Petersen, N.; Grobbelaar, A.A.; Leman, P.A.; Hewson, R.; Georges-Courbot, M.-C.; Papa, A.; Günther, S.; Drosten, C. Virus Detection and Monitoring of Viral Load in Crimean-Congo Hemorrhagic Fever Virus Patients. Emerg. Infect. Dis. 2007, 13, 1097–1100. [Google Scholar] [CrossRef]
- Wolfel, R.; Paweska, J.T.; Petersen, N.; Grobbelaar, A.A.; Leman, P.A.; Hewson, R.; Georges-Courbot, M.-C.; Papa, A.; Heiser, V.; Panning, M.; et al. Low-Density Macroarray for Rapid Detection and Identification of Crimean-Congo Hemorrhagic Fever Virus. J. Clin. Microbiol. 2009, 47, 1025–1030. [Google Scholar] [CrossRef]
- Atkinson, B.; Chamberlain, J.; Logue, C.H.; Cook, N.; Bruce, C.; Dowall, S.D.; Hewson, R. Development of a Real-Time RT-PCR Assay for the Detection of Crimean-Congo Hemorrhagic Fever Virus. Vector-Borne Zoonotic Dis. 2012, 12, 786–793. [Google Scholar] [CrossRef]
- Jääskeläinen, A.J.; Kallio-Kokko, H.; Ozkul, A.; Bodur, H.; Korukruoglu, G.; Mousavi, M.; Pranav, P.; Vaheri, A.; Mirazimi, A.; Vapalahti, O. Development and Evaluation of a Real-Time RT-qPCR for Detection of Crimean-Congo Hemorrhagic Fever Virus Representing Different Genotypes. Vector-Borne Zoonotic Dis. 2014, 14, 870–872. [Google Scholar] [CrossRef]
- Kamboj, A.; Pateriya, A.K.; Mishra, A.; Ranaware, P.; Kulkarni, D.D.; Raut, A.A. Novel Molecular Beacon Probe-Based Real-Time RT-PCR Assay for Diagnosis of Crimean-Congo Hemorrhagic Fever Encountered in India. BioMed Res. Int. 2014, 2014, 1–4. [Google Scholar] [CrossRef]
- Pang, Z.; Li, A.; Li, J.; Qu, J.; He, C.; Zhang, S.; Li, C.; Zhang, Q.; Liang, M.; Li, D. Comprehensive Multiplex One-Step Real-Time TaqMan qRT-PCR Assays for Detection and Quantification of Hemorrhagic Fever Viruses. PLoS ONE 2014, 9, 95635. [Google Scholar] [CrossRef] [PubMed]
- Koehler, J.W.; Delp, K.L.; Hall, A.T.; Olschner, S.P.; Kearney, B.J.; Garrison, A.R.; Altamura, L.A.; Rossi, C.A.; Minogue, T.D. Sequence Optimized Real-Time Reverse Transcription Polymerase Chain Reaction Assay for Detection of Crimean-Congo Hemorrhagic Fever Virus. Am. J. Trop. Med. Hyg. 2018, 98, 211–215. [Google Scholar] [CrossRef]
- Sas, M.A.; Vina-Rodriguez, A.; Mertens, M.; Eiden, M.; Emmerich, P.; Chaintoutis, S.C.; Mirazimi, A.; Groschup, M.H. A one-step multiplex real-time RT-PCR for the universal detection of all currently known CCHFV genotypes. J. Virol. Methods 2018, 255, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Schneeberger, P.H.H.; Pothier, J.F.; Bühlmann, A.; Duffy, B.; Beuret, C.; Utzinger, J.; Frey, J.E. Development and evaluation of a bioinformatics approach for designing molecular assays for viral detection. PLoS ONE 2017, 12, 178195. [Google Scholar] [CrossRef] [PubMed]
- Osman, H.A.M.; Eltom, K.H.; Musa, N.O.; Bilal, N.M.; Elbashir, M.I.; Aradaib, I.E. Development and evaluation of loop-mediated isothermal amplification assay for detection of Crimean Congo hemorrhagic fever virus in Sudan. J. Virol. Methods 2013, 190, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Bonney, L.C.; Watson, R.J.; Afrough, B.; Mullojonova, M.; Dzhuraeva, V.; Tishkova, F.; Hewson, R. A recombinase polymerase amplification assay for rapid detection of Crimean-Congo Haemorrhagic fever Virus infection. PLoS Negl. Trop. Dis. 2017, 11, 6013. [Google Scholar] [CrossRef] [PubMed]
- Escadafal, C.; Ölschläger, S.; Avšič-Županc, T.; Papa, A.; Vanhomwegen, J.; Wölfel, R.; Mirazimi, A.; Teichmann, A.; Donoso-Mantke, O.; Niedrig, M. First International External Quality Assessment of Molecular Detection of Crimean-Congo Hemorrhagic Fever Virus. PLoS Negl. Trop. Dis. 2012, 6, 1706. [Google Scholar] [CrossRef]

| Assay Type | First Author | Year | Reference Testing Material | Declared Sensitivity/ Specificity |
|---|---|---|---|---|
| Single Round | Drosten | 2002 | Human clinical samples | LOD: 2779 copies/mL |
| Deyde | 2006 | Human and animal laboratory isolates | N.D. | |
| Nested | Schwarz | 1996 | Human serum samples | N.D. |
| Midilli | 2007 | Human serum samples | N.D. | |
| Midilli (A) | 2009 | Human serum samples | N.D. | |
| Midilli (B) | 2009 | Human serum samples | N.D. | |
| Elata | 2011 | Human serum samples | N.D. | |
| Negredo | 2017 | Human serum samples | N.D. | |
| Real Time | Yapar | 2005 | Human serum samples | LOD: 100 copies/mL |
| Duh | 2006 | Human serum samples | LOD: 300 PFU/mL | |
| Garrison | 2007 | Laboratory isolates | LOD: 10 copies/mL | |
| Wolfel | 2007 | Human serum samples | LOD: 10 copies/mL | |
| Wolfel | 2009 | Laboratory isolates and human serum samples | LOD: 540 copies/mL | |
| Atkinson | 2012 | Laboratory isolates | LOD: 100 copies/mL | |
| Jaaskelainen | 2014 | Laboratory isolates and human serum samples | Sensitivity: N.D.; specificity: 97% | |
| Kamboj | 2014 | Animal | LOD: 7.6 copies (per reaction) | |
| Pang | 2014 | Laboratory isolates | LOD: 2000 copies/mL | |
| Koehler | 2018 | Laboratory isolates | LOD: 256 PFU/mL | |
| Sas | 2018 | Animals, humans and tick samples | LOD: 2000 copies/mL (gen II, IV, V and VI); 2 × 105 copies/mL (gen III and I) | |
| Sybr Green | Schneeberger | 2017 | Laboratory isolates | N.D. |
| LAMP | Osmann | 2013 | Human serum samples | LOD: ≥0.1 fg of viral RNA |
| RPA | Bonney | 2017 | Tick homogenates and clinical samples | LOD: between 500 and 50 copies (per reaction) |
| Type | Assay | Prim / Prob | Clade | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Africa 1 | Africa 2 | Africa 3 | Africa 4 | Asia 1 | Asia 2 | Europe 1 | Europe 2 | Europe 3 | |||
| N = 2 | N = 5 | N = 29 | N = 2 | N = 30 | N = 33 | N = 76 | N = 2 | N = 2 | |||
| Single Round | Drosten 2002 | 3 | 3 (0.0%) | 5’ (0.0%) | 4 (0.0%) | 3 (0.0%) | 4 (0.0%) | 2’ (60.6%) | 5 (0.0%) | 9’ (0.0%) | 4 (0.0%) |
| Nested | Schwarz 1996 | 4 | 5 (0.0%) | 5’ (0.0%) | 7’ (0.0%) | 8’ (0.0%) | 11’ (0.0%) | 6’ (0.0%) | 5 (0.0%) | 13’’ (0.0%) | 12’ (0.0%) |
| Midilli 2007 | 3 | 5’ (0.0%) | 8’’ (0.0%) | 2’ (75.9%) | 9’ (0.0%) | 4’ (83.3%) | 1 (84.8%) | 1 (84.2%) | 4’ (0.0%) | 6’ (0.0%) | |
| Midilli 2009 (A) | 4 | 16’’ (0.0%) | 20’’ (0.0%) | 21’’ (0.0%) | 20’’ (0.0%) | 21’’ (0.0%) | 21’’ (0.0%) | 21’’ (0.0%) | 4’ (50.0%) | 16’’ (0.0%) | |
| Midilli 2009 (B) | 4 | 11’’ (0.0%) | 10’’ (0.0%) | 14’’ (0.0%) | 8’’ (0.0%) | 12’’ (0.0%) | 11’’ (0.0%) | 4’ (71.1%) | 12’ (0.0%) | 10’’ (0.0%) | |
| Elata 2011 | 4 | 11’’ (0.0%) | 10’ (0.0%) | 8’ (62.1%) | 12’ (0.0%) | 11’ (0.0%) | 11’ (0.0%) | 10’’ (0.0%) | 14’’ (0.0%) | 14’’ (0.0%) | |
| Negredo 2017 | 4 | 0 (100%) | 4’’ (20.0%) | 1 (89.7%) | 4 (0.0%)* | 3’’ (80.0%) | 2’ (87.9%) | 1 (86.8%) | 0 (100%) | 4 (0.0%) | |
| Real Time | Yapar 2005 | 2 / 1 | 0 (100%) | 1 (40.0%) | 2 (0.0%) | 2 (0.0%) | 4’ (0.0%) | 1 (60.6%) | 1 (93.4%) | 2 (0.0%) | 1 (0.0%) |
| Duh 2006 | 2 / 1 | 11’ (0.0%) | 7’ (0.0%) | 9’ (0.0%) | 5’’ (0.0%) | 8’ (0.0%) | 8’ (0.0%) | 3’ (25.0%) | 9’ (0.0%) | 7’ (0.0%) | |
| Garrison 2007 | 2 / 1 | 10’ (0.0%) | 4 (0.0%) | 9’’ (0.0%) | 7’ (0.0%) | 9’’ (0.0%) | 5’ (12.1%) | 7’ (0.0%) | 11’’ (0.0%) | 5’ (0.0%) | |
| Wolfel 2007 | 2 / 2 | 8’ (0.0%) | 6 (0.0%) | 7’ (0.0%) | 4 (0.0%) | 3 (0.0%) | 4’ (9.1%) | 6’ (0.0%) | 6’ (0.0%) | 9 (0.0%) | |
| Wolfel 2009 | 6 / 13 | 7 (0.0%) | 8 (0.0%) | 6’’ (24.1%) | 2 (0.0%) | 3’’ (73.3%) | 5’’ (0.0%) | 5’ (0.0%) | 8’’ (0.0%) | 5 (0.0%) | |
| Jaaskelainen 2014 | 3 / 3 | 4’’ (0.0%) | 6 (0.0%) | 4 (37.9%) | 6 (0.0%) | 7’ (0.0%) | 7’ (0.0%) | 3’ (81.6%) | 4’’ (0.0%) | 6 (0.0%) | |
| Pang 2014 | 2 / 1 | 9’ (0.0%) | 11 (0.0%) | 3 (3.4%) | 4’ (0.0%) | 3’ (0.0%) | 5’’ (0.0%) | 4’ (14.5%) | 12 (0.0%) | 12’ (0.0%) | |
| Koehler 2018 | 2 / 1 | 2 (0.0%) | 2 (80.0%) | 3’ (72.4%) | 3 (0.0%) | 4’’ (0.0%) | 3 (24.2%) | 2 (85.5%) | 5’’ (0.0%) | 4’ (0.0%) | |
| Sas 2018 | 14 / 2 | 0 (100%) | 3 (0.0%) | 3’ (37.9%) | 2 (0.0%) | 3 (73.3%) | 3’ (51.5%) | 2 (82.9%) | 2 (50.0%) | 7 (0.0%) | |
| Sybr Green | Schneeberger 2017 | 2 | 6’ (0.0%) | 6’ (0.0%) | 3’ (17.2%) | 3 (0.0%) * | 5’ (0.0%) | 2’’ (27.3%) | 7’ (0.0%) | 9’ (0.0%) | 4 (0.0%) |
| LAMP | Osmann 2013 | 8 | 24’’ (0.0%) | 23’ (0.0%) | 8’’ (6.9%) | 19’ (0.0%) | 19’’ (0.0%) | 23’’ (0.0%) | 21’’ (0.0%) | 28’’ (0.0%) | 25’ (0.0%) |
| Type | Assay | Number of Primers/Probes | Clade | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Africa 1 | Africa 2 | Africa 3 | Africa 4 | Asia 1 | Asia 2 | Europe 1 | Europe 2 | Europe 3 | |||
| N = 2 | N = 1 | N = 15 | N = 0 | N = 16 | N = 20 | N = 33 | N = 2 | N = 0 | |||
| PCR | Deyde 2006 | 2 primers | 0 (100.0%) | 0 (100.0%) | 1 (93.3%) | - (-) | 9 (87.5%) | 2’’ (90.0%) | 1 (90.9%) | 0 (100.0%) | - (-) |
| N = 2 | N = 2 | N = 21 | N = 0 | N = 17 | N = 24 | N = 33 | N = 2 | N = 0 | |||
| RealTime | Atkinson 2012 | 2 primers / 1 probe | 3 (0.0%) | 6 (0.0%) | 3 (0.0%) | - (-) | 15’ (0.0%) | 6 (0.0%) | 5 (0.0%) | 5 (0.0%) | - (-) |
| N = 2 | N = 4 | N = 27 | N = 1 | N = 21 | N = 29 | N = 72 | N = 2 | N = 2 | |||
| RealTime | Kamboj 2014 | 2 primers / 1 probe | 7’ (0.0%) | 12’’ (0.0%) | 5’’ (0.0%) | 7’’ (0.0%) | 8’’ (0.0%) | 3’’ (24.1%) | 9’’ (0.0%) | 8’’ (0.0%) | 15’’ (0.0%) |
| N = 2 | N = 2 | N = 22 | N = 0 | N = 19 | N = 24 | N = 58 | N = 2 | N = 0 | |||
| RPA | Bonney 2017 | 2 primers / 1 probe | 9’ (0.0%) | 11 (0.0%) | 8’ (0.0%) | - (-) | 10 (0.0%) | 9 (0.0%) | 5 (46.6%) | 11 (0.0%) | - (-) |
| Clade | Best Assay Combination | Equivalent Combination | Max Mismatches Per Seq | Max Mismatches in Last 5 nt | Perfect Matched Sequences | |
|---|---|---|---|---|---|---|
| Africa 1 | N = 2 | Negredo 2017 | Yapar 2005 OR Sas 2018 | 0 | 0 | 100.0% |
| Africa 2 | N = 5 | Yapar 2005 + Koehler 2018 | 1 | 0 | 80.0% | |
| Africa 3 | N = 29 | Elata 2011 + Negredo 2017 | 0 | 0 | 100.0% | |
| Africa 4 | N = 2 | Sas 2018 + Yapar 2005 | Yapar 2005 + Drosten 2002 | 1 | 0 | 0.0% |
| Asia 1 | N = 30 | Midilli 2007 + Wolfel 2009 + Koehler 2018 | 1 | 0 | 90.0% | |
| Asia 2 | N = 33 | Midilli 2007 + Schneeberger 2017 + Drosten 2002 | Midilli 2007 + Schneeberger 2017 + Kamboj 2014 OR Negredo 2017 + Schneeberger 2017 + Kamboj 2014 OR Negredo 2017 + Schneeberger 2017 + Drosten 2002 | 0 | 0 | 100.0% |
| Europe 1 | N = 76 | Yapar 2005 + Midilli 2007 | Yapar 2005 + Negredo 2017 | 0 | 0 | 100.0% |
| Europe 2 | N = 2 | Negredo 2017 | 0 | 0 | 100.0% | |
| Europe 3 | N = 2 | Yapar 2005 | 1 | 0 | 0.0% | |
| All | N = 181 | Yapar 2005 + Negredo 2017 + Koehler 2018 + Drosten 2002 + Wolfel 2009 | 1 | 0 | 93.4% | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gruber, C.E.M.; Bartolini, B.; Castilletti, C.; Mirazimi, A.; Hewson, R.; Christova, I.; Avšič, T.; Grunow, R.; Papa, A.; Sánchez-Seco, M.P.; et al. Geographical Variability Affects CCHFV Detection by RT–PCR: A Tool for In-Silico Evaluation of Molecular Assays. Viruses 2019, 11, 953. https://doi.org/10.3390/v11100953
Gruber CEM, Bartolini B, Castilletti C, Mirazimi A, Hewson R, Christova I, Avšič T, Grunow R, Papa A, Sánchez-Seco MP, et al. Geographical Variability Affects CCHFV Detection by RT–PCR: A Tool for In-Silico Evaluation of Molecular Assays. Viruses. 2019; 11(10):953. https://doi.org/10.3390/v11100953
Chicago/Turabian StyleGruber, Cesare E. M., Barbara Bartolini, Concetta Castilletti, Ali Mirazimi, Roger Hewson, Iva Christova, Tatjana Avšič, Roland Grunow, Anna Papa, María P. Sánchez-Seco, and et al. 2019. "Geographical Variability Affects CCHFV Detection by RT–PCR: A Tool for In-Silico Evaluation of Molecular Assays" Viruses 11, no. 10: 953. https://doi.org/10.3390/v11100953
APA StyleGruber, C. E. M., Bartolini, B., Castilletti, C., Mirazimi, A., Hewson, R., Christova, I., Avšič, T., Grunow, R., Papa, A., Sánchez-Seco, M. P., Koopmans, M., Ippolito, G., Capobianchi, M. R., Reusken, C. B. E. M., & Di Caro, A. (2019). Geographical Variability Affects CCHFV Detection by RT–PCR: A Tool for In-Silico Evaluation of Molecular Assays. Viruses, 11(10), 953. https://doi.org/10.3390/v11100953







