Abstract
COVID-19 has significantly affected the work environment of nurses. In the face of the challenges posed by stressors in clinical practice, some nurses adapt and prove to be resilient. In the face of the COVID-19 pandemic, the nature of care itself and the new ways of working are potentially very stressful. We aim to analyze the resilience of care nurses to the psychological impact of the COVID-19 pandemic. This study is a systematic review of nurse caregiver resilience to the COVID-19 pandemic in 2021. Our search was conducted in the WOS, Medline/PubMed, Cochrane, BVS/LILACS, and Cuiden databases. The inclusion criteria were: studies published in Spanish or English; carried out from March 2020 to May 2021 on nurses caring for patients with COVID-19; and investigating the factors influencing the psychological impact, resilience, strategies to develop it, and interventions to promote it during this pandemic and others, such as SARS, MERS, or ebola. The quality of the studies and the risk of bias were evaluated following ICROMS, STROBE and AMSTAR-2 criteria. Twenty-two studies were selected. Most of the studies highlighted the presence of stressors in nurses, emphasizing those of the environment, which converged in dysfunctional responses that hurt their resilience. The most persuasive factors were social and organizational support. Coping strategies developed by nurses and especially interventions by organizations were detected as instruments to foster resilience, but have not been well researched. Resilience has a key moderating role in mitigating the psychological impact of nurses in the face of the COVID-19 pandemic.
1. Introduction
In 2018, the International Council of Nurses (ICN) and the World Health Organization (WHO) launched the Nursing Now movement to raise the status and profile of nurses, capping it off with the year 2020 [1]. The iconic year of nurses sees the emergence of COVID-19, an emerging infectious disease caused by the new SARS-CoV-2 coronavirus, which was first identified in Wuhan on 31 December 2019 [2]. The WHO declared the disease a pandemic on 11 March 2020 due to its rapid spread in most countries of the world [3]. COVID-19 has been a dramatic global disruption, as the global number of deceased and infected patients with this disease was 4.7 million and 229.6 million, respectively, as of September 2021 [4]. The latest ICN analysis shows that as of November 2020, the number of nurses who have died after contracting COVID-19 is 1500, as many as in World War I [5]. This figure, which includes nurses from only 44 of the world’s 195 countries, is known to be a low estimate of the actual number of deaths.
Nurses are particularly at risk of psychological problems due to the highly stressful work situations to which they are exposed; this fact can be more challenging when applied in the context of a pandemic, as working in the face of such a situation can be exhausting [6]. Currently, nurses have not only experienced an increase in the volume and intensity of their work [7] but have to adapt to new protocols and new normality. A Spanish study showed that one in seven healthcare workers tested positive for a disabling mental disorder during the first wave of the COVID-19 pandemic, such as major depressive disorder, generalized anxiety disorder, panic attacks, and post-traumatic stress disorder [8]. In previous epidemics or pandemics [9,10], nurses presented the highest levels of occupational stress and distress compared to other personnel involved, indicating that they may have subsequently developed mental disorders. However, in the face of the negative consequences of stressors in clinical practice, there are nurses who demonstrate resilience after being exposed to a traumatic event and are successful in the face of the same challenges and limitations [11]. The American Psychological Association [12] defines resilience as the ability to adapt to adversity, trauma, tragedy, threats, or other significant sources of stress and, from this, seek a drive to cope and emerge successfully.
From the nursing discipline and perspective, this concept is related to Dorothy Johnson’s Behavioral Systems Model, which focuses on how present or potential stress can affect a person’s ability to adapt. For Johnson, the person is an interactive, interdependent, and integrated behavioral system with patterned, repetitive, and intentional forms of behavior [13,14]. The author reflects in her model that the human system is constantly subjected to stressors [14,15,16], which correspond to internal or external stimuli that produce tension and a certain degree of instability, giving rise to constructive or destructive behavioral changes, which can lead to equilibrium or imbalance. In view of this, the objective of the model is to maintain and recover equilibrium, helping the person to achieve an optimal level of functioning. This is why it is directly related to the term resilience [13], which is being increasingly researched within the field of nursing, since it is a capacity that is influenced by various factors and which allows the person to continue to project him/herself despite destabilizing events, both in patients and in the nursing staff itself. It has been shown that the most resilient nurses can better tolerate the hostile environment of pain, suffering, and death that they encounter throughout the workday [17], an environment that is especially aggressive during the pandemic.
Given the continuous exposure of nurses to human suffering and an adverse work environment, resilience has become so important that it is considered an inherent characteristic of nurses during the course of healthcare; there is evidence that resilience ameliorates the effects of work stress and largely avoids its long-term consequences [13]. Resilient nurses are seen as a crucial element in an ever-changing healthcare system [18], especially during the new SARS-CoV-2 pandemic situation.
In view of the above, it is relevant to explore care nurses’ resilience in the face of the impact of the COVID-19 pandemic. Researching this could allow us to identify which aspects modulate its development, obtaining information on those nurses who prosper and continue to find satisfaction in their profession despite the current challenges and problems posed by this pandemic. This study aims to answer the research question: “Does resilience modulate the psychological impact on nurses of the COVID-19 pandemic?”. Additionally, therefore, the aim of this study is to analyze the resilience of care nurses to the psychological impact of the COVID-19 pandemic.
2. Materials and Methods
2.1. Design
Systematic review was conducted between March 2020 and May 2021 according to PRISMA guidelines [19].
2.2. Protocol Development and PICO Question
The review protocol was developed to meet PRISMA [19], which was designed to answer PICO (Population, Intervention, Comparison, Outcome).
However, the stated focus question, “Does resilience modulate the psychological impact of nurses in the face of the COVID-19 pandemic?” was an adaptation of a PIO format question (Population, Intervention, Outcome) [20]: nurses (P), resilience (I), and psychological impact in the face of the COVID-19 pandemic (O).
The protocol for this review was not registered due to the rush to collect data in the midst of the pandemic and the desire to share our findings quickly.
2.3. Selection Criteria
2.3.1. Inclusion Criteria
We included studies published in Spanish or English; conducted (from March 2020 to May 2021) on nurses who cared for patients with COVID-19; investigating the influential factors of the psychological impact, resilience, strategies to develop it, or interventions to promote it during this pandemic and during others, such as SARS, MERS, or Ebola.
2.3.2. Exclusion Criteria
We excluded studies conducted on pediatric nurses, literature reviews, and papers that did not meet the necessary methodological quality.
2.4. Search Strategy
An exhaustive search was initiated in different databases. Electronic databases: Web of Science, Medline/Pubmed, Cochrane Collaboration (The Cochrane Library), BVS Biblioteca Virtual en Salud/LILACS, and CUIDEN. Subsequently, a manual review of the bibliographic references of the selected articles was carried out in order to include other potentially valid studies for the review. The keywords used concerned Medical Subject Headings (Mesh) [21]: nursing/nurses; coronavirus infections; resilience, psychological; adaptation, psychological; burnout, psychological; stress, psychological; uncertainty. In order to combine these terms, AND and OR were used as Boolean operators. Truncation operators were used as accuracy operators. Two researchers reviewed the selected and eliminated papers; if there were any discrepancies, a third reviewer intervened to decide their inclusion or exclusion.
The search strategy consisted of elaborating different search strings based on the above descriptors and free text (Table 1).

Table 1.
Search strategy.
2.5. Study Variables
The variables in the review were: influential factors on the psychological impact of the COVID-19 pandemic, behavioral responses exhibited by nurses, level of nurses’ resilience, influential factors on observed resilience, resilience-development strategies, and healthcare organization interventions to promote resilience in professionals.
Documentary quality assessment:
Documentary quality was assessed through levels of evidence of effectiveness according to the Joana Briggs Institute (JBI) [22]; these are designed to align with the GRADE approach to pre-ranking findings based on the study design, which are then upgraded or downgraded depending on a number of factors.
Regarding the tool used to assess the methodological quality and the risk of bias of the articles, ICROMS [23] was used; it brings together different quality and methodological bias tools in a single document, allowing the quick and efficient selection and evaluation of different aspects and indicators of methodological quality. The tool consists of two parts: a list of quality criteria specific for each study design, as well as criteria applicable across all study designs by using a scoring system, and a "decision matrix", which specifies the robustness of the study by identifying minimum requirements according to the study type and the relevance of the study to the review question. The decision matrix directly determines inclusion or exclusion of a study in the review. ICROMS was used to analyze the quality and bias of the qualitative studies, whose minimum score was 16.
To assess the quality of systematic reviews, the AMSTAR-2 [24] tool was used, which was developed to evaluate systematic reviews. It allows a more detailed evaluation of the SRs that also include non-randomized studies of health interventions, which are increasingly incorporated in the SR. This questionnaire contains 16 domains with simple response options: “yes”, when the result is positive; “no”, when the standard was not met or there is insufficient information to answer; and “partial yes”, in cases where there was partial adherence to the standard. Amstar-2 identifies the quality of reviews as high, moderate, low, or critically low quality.
Quality assessment of the cross-sectional studies in this review was performed using the STROBE [25] tool. The STROBE Statement is a list composed of 22 points that are considered essential for adequate communication of observational studies, allowing a critical evaluation of them. The cutoff score was 18/22.
3. Results
The total number of records obtained at the end of the literature search was (n = 1578), of which 22 were finally selected. The selection process can be seen in Figure 1, which was performed by two independent reviewers. The bibliographic search and the selection of documents are described in Figure 1. A total of 22 studies were chosen to be included in this review. Regarding the design of the studies that formed part of this systematic review, seventeen cross-sectional descriptive observational studies [26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43], one mixed-methods systematic review [44], one meta-analysis and systematic review [45], one scoping review [46], and one qualitative study [47] were identified.
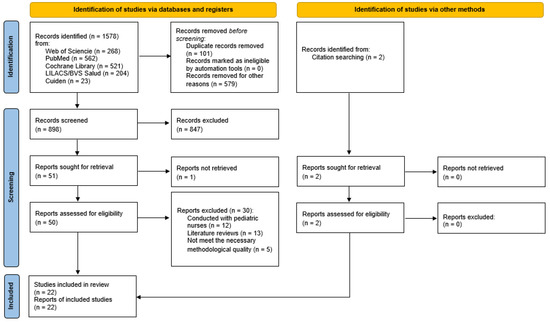
Figure 1.
Flow chart.
The factors that predominated with respect to the influence of the psychological impact of nurses were those related to gender [27,31,32,39,45], age [28,31,32,38,41,43], work experience [29,31,33,35,36,43], family [27,31,38,41], working conditions, use of personal protective equipment, degree of training [27,35,36,37,38], socioeconomic level, social support and organizational support [35,36,37,39].
An increase in tension and stress among nurses was detected compared to before the pandemic [33]. The most notable responses included fear, helplessness, discomfort with the scarcity and prolonged use of PPE, emotional distress, perception of providing poor nursing care [29,31,36,38,42,45], and concern and uncertainty for their safety and that of their families [29,36,38,40,42], even to the point of considering leaving the profession [36,38]. Physical symptoms related to the psychological burden were also detected [31,32,36,41].
About the level of resilience, the research used different validated scales to measure this variable, such as the Connor–Davidson Resilience Scale (CD-RISC) [26,27,29,33,34,36,37,40,42] and the Brief Resilient Coping Scale (BRCS) [35,38]. A total of eight articles referred to low–moderate levels of resilience in nurses [26,29,33,34,35,36,37,38], and three studies reported high levels [27,40,42], also alluding to the impact of resilience on the quality of care provided to patients with COVID-19 [32,34,35,45].
All studies highlighted the protective role of resilience in the psychological impact of the pandemic on these professionals. The factors that influenced the resilience of the nurses facing this outbreak were: organizational support [26,27,31,32,34]; the perception of greater social support [27,32,35,45]; having training, work, and emergency experience [26,30,31,35,45]; having an optimistic, tenacious, and confident attitude [33,45]; and sociodemographic variables, such as being older, being male, and having a medium–high socioeconomic level [30,31,43].
Among the strategies developed by the nurses to favor their resilience and mitigate the psychological impact, the following prevailed: seeking socio-familial support [28,38,42,43], carrying out recreational and health-promoting activities [28,42,44], seeking information sources on psychological resources and clinical practice [29,42,43], and developing a positive and tenacious attitude [38,42,43,44,45]. These strategies helped to stabilize the nurses emotionally and strengthen their resilience. The strategy they used the least was seeking professional psychological support [29,30,38,42].
Research indicated that nurses tended to adopt positive strategies in the face of the psychological impact of the COVID-19 [43] pandemic [28,29,38,42]. It was found that women were less likely to use coping strategies [28,29] and that nurses who suffered stress due to insufficient preparation and fear of contagion did not establish adequate strategies [29,33].
Concerning interventions to favor resilience and reduce the psychological impact of nurses in the face of this pandemic, the following were highlighted: offering training and clear instructions on the approach to patients with COVID-19, improving the working environment and working conditions, providing optimal protective material, promoting basic needs, and psychoemotional management [31,34,38,39,42,46,47]. Two articles classified interventions in terms of temporality, i.e., those to be carried out before exposure to the outbreak [42,46] (such as the provision of optimal education and training for the management of patients’ psychological problems, diagnosis, and treatment; guidelines for infection prevention and control; resilience training to create a sense of preparedness for clinical practice); and during exposure [42,46] (such as providing personal protective equipment; favoring a good working environment; improving resilience through the adequate provision of information, psychosocial support, and treatment; monitoring the health status of professionals; and using various forms and contents of psychosocial support). Several barriers and guidelines were identified for the implementation of interventions to support nurses’ resilience [44], such as the lack of awareness of practitioners’ needs by organizations and limited resources, including a lack of materials, time, and staff skills.
The synthesis of the articles with the most relevant information from the retrieved documents can be seen in Table 2.

Table 2.
Summary of results.
4. Discussion
This review was based on Dorothy Johnson’s Behavioral Model [13,14,15,16,48] to broadly and holistically analyze the resilience of nurses in the face of the impact of the COVID-19 pandemic, which was a key competence to reducing or controlling the effects of the stress generated by this catastrophe. To this end, we explored the factors that influenced the psychological impact of the nurses, categorized by Johnson as internal stressing factors (ISF) and external stressing factors (ESF) [14], the behavioral and psychological responses in which they converged, as well as the determination of the nurses’ resilience levels and the factors that influence it, classified as intrapersonal resilience factors (IRF) and environmental resilience factors (ERF), among other factors studied (Figure 2).
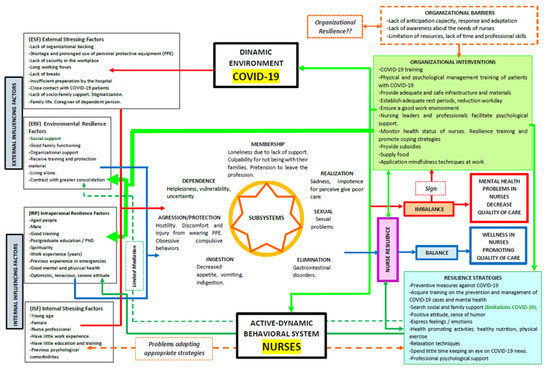
Figure 2.
Intrapersonal resilience factors, environmental resilience factors, and other factors studied.
As in the current study, a high prevalence of stressors led to responses leading to psychological imbalance and distress in nurses in previous outbreaks, such as Ebola, H1N1, and SARS [49,50,51,52]. Evidence showed that female nurses had a significant risk of psychological distress, consistent with previous findings [49,50,51,52,53]. In this sense, nurses generally tend to be predominantly female, thus presenting higher additional workloads [54]. Being a nurse idiosyncratically implies having close contact with patients with COVID-19 and, therefore, a higher risk of becoming infected [33,38,39,43]; this aspect was identified as a key ESF for nurses in the context of this outbreak, as it has implications not only for their own health but also for that of their families [55].
It was detected that the preponderance of ESF has primarily induced dysfunctional psychological responses [33,36,38,39,42,43] in the affiliation, dependence, fulfillment, and aggression/protection subsystems, as well as dysfunctional physical responses [28,35,41,43] in the ingestion, elimination, and sexual subsystems, generating an imbalance in the nurses. This relates to Johnson’s theory that a person’s attempts to regain equilibrium in the face of a powerful force may require extraordinary energy consumption, even affecting biological processes [14]. These findings are in line with experiences in previous epidemics [52,56,57] and may indicate that mental disorders may develop in the long term.
The fundamentally low–moderate levels of resilience detected in nurses in the review [26,29,33,34,35,36,37,38] were consistent with research conducted in other outbreaks, where concern was expressed about their low resilience [58,59,60,61]. Even resilient nurses were found to be stressed, albeit to a lesser degree. This fact is consistent with Jonhson’s postulation that balance can also occur in illness [16]. Therefore, being resilient does not mean that nurses cannot experience feelings of emotional distress but rather that they have the skills to adapt to such a situation.
Nevertheless, the three studies that reported high levels of resilience [27,40,42] agreed that the aspects that marked this difference for other nurses were primarily related to ARF. This was in line with Johnson’s approach, influenced by F. Nightingale, on the importance of approaching the person by focusing on his or her relationship with the environment, not with the disease [48]. The evidence was unanimous in indicating that the perception of social support was linked to less distress [29,32,33,34,35,41], as this variable is an ERF known to be effective in reducing stress among nurses [13,62,63]. They especially valued social support from their families, a fact that is compatible with data from research on resilience. This may be the case because an individual’s first social relationship is usually with his or her family. In the COVID-19 pandemic, this type of support was scarce [29,33,35,41], probably due to the isolating conditions caused by this virus, in addition to the fact that many were rejected by family and friends. Nurses not only had to deal with the COVID-19 pandemic but also with their concern for their families and the stigmatization of the public [31,41], so they had limited access to one of the key elements to foster their resilience, which in this study was a relevant ESF.
Because of this, organizational support from governments, hospitals, supervisors, and coworkers is especially important to fill this gap, being another ERF with an important positive influence on resilience [26,30,32,39,43]. Some studies state that higher levels of organizational support are significantly associated with effective work outcomes, fostering organizational identity, positive work attitudes, satisfaction, job commitment, and improved physical and mental health of nurses [62,64]. However, several articles in this review [26,29,33,34,35,36,38] in which nurses had lower levels of resilience coincided with reporting a deficit of organizational support, making it a relevant ESF. Therefore, it was detected in this research that the fluctuation of resilience levels was significantly influenced by the presence of ERF.
The coping strategies developed by the nurses denoted a mediating role between resilience and stress. They were an effective tool to develop and reinforce IRF [27,28,30,31,37,41,43] and, at the same time, act primarily against EIFs since, due to the peculiarities of the transmission of this virus, the nurses had limited access to ARFs. Previous research has shown that problem-focused strategies are positively related to indicators of resilience, decreased stress, and psychological distress [65,66]; however, evidence from this study showed the opposite. This could occur because aspects such as the effort made to control the problems related to this virus, being permanently informed about it, and the fear of infection presented a relationship with greater stress, apart from the fact that they, in turn, were ISF detected in this review. Studies before the COVID-19 pandemic also concluded that emotion-focused strategies presented more inconsistent results in their relationship with nurses’ well-being [66,67,68], but in this research, they presented a stronger connection with resilience. This could be because these types of strategies included, for example, adopting a positive attitude, performing relaxation techniques, or performing health-promoting activities [27,30,31,37,41,43], which were linked to a pragmatic way of embodying nurses’ IRF.
Through this review, a group was revealed that requires special attention due to its greater vulnerability: nurses who are female, younger, and with less work experience [28,29,33] (three variables corresponding to ISF detected in this study). This could be related to the fact that many of this group are assigned jobs in special services or in areas of higher acuity/gravity. Additionally, some countries accelerated their final-year nursing students to join the nursing team earlier [69]. Mental health screenings would entail an approach that could help monitor both nurses’ distress and the use of appropriate coping strategies. In fact, in this review, several studies [29,38,42] agreed that the strategy least used by nurses was seeking professional psychological support. We believe that this is due to the fear of being stigmatized for the use of this type of resource and reluctance to acknowledge the need for help.
Although relatively few studies investigated organizational interventions to promote nurses’ resilience in the face of this pandemic, it is worth noting that the findings were extremely consistent, as the studies where higher levels of resilience were reported were those where organizational interventions were applied [27,40,42]. This lends confidence to the suggestion that implementing IRF and ERF through interventions are important targets for reducing the imbalance generated by both ISF and ESF and could even contain them and strengthen resilience. It may be too early to achieve published work in this area, but in other outbreaks or epidemics, common or similar barriers and facilitators were developed [44]; some research in other epidemics [70,71,72,73] suggests that providing education, training in resilience, providing psychological support, and providing the necessary resources are aspects that increase resilience and a sense of empowerment among nurses. This is consistent with previous experiences, in which it is reported that nurses repeatedly feel ignored by their managers when they raise concerns about their mental health [74].
Evidence from this study identified several barriers to the implementation of interventions by organizations, such as their lack of awareness of health workers’ needs, along with resource constraints, including a lack of equipment, time, and staff skills. Organizational resilience [75] is defined as the ability of an organization to anticipate, prepare for, respond to, and adapt to incremental changes and sudden disruptions to survive and thrive, so this study shows that the impact of COVID-19 has been an additional assault on nurses’ resilience, as nurses already had stressors in the healthcare environment before the pandemic [44,76]. The pandemic has also influenced the resilience of organizations, which was already impaired [75]. If organizations are weak, they will not be resilient and therefore will not be able to effectively develop interventions to develop competence in nurses, who in turn are part of these structures. Increasingly, evidence supports the close relationship between organizational resilience and outcomes [77], as nursing resilience must be approached as a collective and organizational responsibility, as it is not built alone, nor is it solely an individual responsibility.
Among the limitations found in this review, in addition to those of each of the papers reviewed (which, due to their design, do not generate a high level of evidence), it should be noted that in several cases, the interventions carried out by the organizations were communicated through brief comments, letters to the editor, editorials, or communications at congresses, probably driven by the urgent desire to share the findings during the period of the health crisis. By discarding these sources of information from the selection criteria, confidence that all relevant research was found is reduced.
The study results were collected in the most critical period of the pandemic, and therefore, some studies published later may not have been included in this review. Some psychosocially focused databases were not used, as a more clinical approach was intended; this may also have caused some articles to be missed. On the other hand, given that during the worst moments of the COVID-19 pandemic, scientific production was necessarily rapid and agile, it is logical that many cross-sectional observational articles were published, which we decided to include in the study despite the low evidence they provide. To evaluate them, we chose the STROBE tool, which, although it does not evaluate bias, is one of the tools used in Cochrane and is commonly used in published reviews, also of a systematic type.
5. Conclusions
Resilience has a key moderating role in mitigating the psychological impact of the COVID-19 pandemic on nurses in care, promoting their equilibrium, and promoting the quality of their work.
The COVID-19 pandemic has provoked massive exposure to stressors in nurses; external stressors are the main contributors to the responses generated, converging in those of psychological and physical etiology.
The levels of resilience of nurses in the face of this health crisis are predominantly low–moderate, whose fluctuation is due to the interaction between intrapersonal and especially environmental factors, along with the presence of stressors.
The strategies developed by nurses to cope with the psychological impact are useful to promote IRFs, partially promote ARFs, and combat SIFs. Identifying when nurses may possess factors that expose them to developing negative coping strategies, ineffective coping, and finding ways to foster more positive approaches to managing stress will be key to nurses ultimately achieving optimal levels of resilience while avoiding imbalances and the risks of adverse health consequences.
Interventions developed by healthcare organizations play the most relevant role in fostering nurses’ resilience in the face of this pandemic, as it is through them that this skill can be holistically and comprehensively trained and promoted.
Author Contributions
Conceptualization, E.S.-G., E.M.S.-P. and V.G.-C.; methodology, E.S.-G., E.M.S.-P., C.S.-O., R.J.-V. and V.G.-C.; software, E.S.-G.; validation, E.S.-G. and A.R.-H.; investigation, E.S.-G., C.S.-O. and R.J.-V.; resources, A.R.-H.; writing—original draft preparation, E.S.-G.; writing—review and editing, R.J.-V., V.G.-C.; visualization, E.M.S.-P. and A.R.-H.; supervision, V.G.-C., E.M.S.-P. and C.S.-O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- International Council of Nurses El Consejo Internacional de Enfermeras y Nursing Now Celebran la Declaración de 2020 Como el Año Internacional de la Enfermera y la Partera. Available online: https://www.icn.ch/es/noticias/el-consejo-internacional-de-enfermeras-y-nursing-now-celebran-la-declaracion-de-2020-como (accessed on 10 September 2021).
- Hui, D.S.; Azhar, E.I.; Madani, T.A.; Ntoumi, F.; Kock, R.; Dar, O.; Ippolito, G.; Mchugh, T.D.; Memish, Z.A.; Drosten, C.; et al. The Continuing 2019-NCoV Epidemic Threat of Novel Coronaviruses to Global Health—The Latest 2019 Novel Coronavirus Outbreak in Wuhan, China. Int. J. Infect. Dis. 2020, 91, 264–266. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Announces COVID-19 Outbreak a Pandemic. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed on 10 September 2021).
- Center for Systems Sciencie and Engineering at JHU COVID-19 Dashboard. 2021. Available online: https://gisanddata.maps.arcgis.com/apps/dashboards/bda7594740fd40299423467b48e9ecf6 (accessed on 22 September 2021).
- International Council of Nurses. El CIE Confirma el Fallecimiento de 1500 Enfermeras por COVID-19 en 44 Países y Estima que las Muertes de Trabajadores Sanitarios por Esta Enfermedad Podrían Superar las 20,000 en Todo el Mundo. Available online: https://www.icn.ch/es/noticias/el-cie-confirma-el-fallecimiento-de-1-500-enfermeras-por-covid-19-en-44-paises-y-estima (accessed on 10 September 2021).
- Garbern, S.C.; Ebbeling, L.G.; Bartels, S.A. A Systematic Review of Health Outcomes among Disaster and Humanitarian Responders. Prehosp. Disaster Med. 2016, 31, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Tahan, H.M. Essential Case Management Practices Amidst the Novel Coronavirus Disease 2019 (COVID-19) Crisis: Part 2. Prof. Case Manag. 2020, 25, 267–284. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Vilagut, G.; Mortier, P.; Ferrer, M.; Alayo, I.; Aragón-Peña, A.; Aragonès, E.; Campos, M.; Cura-González, I.D.; Emparanza, J.I.; et al. Mental Health Impact of the First Wave of COVID-19 Pandemic on Spanish Healthcare Workers: A Large Cross-Sectional Survey. Rev. Psiquiatr. Salud Ment. 2021, 14, 90–105. [Google Scholar] [CrossRef] [PubMed]
- Shih, F.-J.; Turale, S.; Lin, Y.-S.; Gau, M.-L.; Kao, C.-C.; Yang, C.-Y.; Liao, Y.-C. Surviving a Life-Threatening Crisis: Taiwan’s Nurse Leaders’ Reflections and Difficulties Fighting the SARS Epidemic. J. Clin. Nurs. 2009, 18, 3391–3400. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Kang, W.S.; Cho, A.-R.; Kim, T.; Park, J.K. Psychological Impact of the 2015 MERS Outbreak on Hospital Workers and Quarantined Hemodialysis Patients. Compr. Psychiatry 2018, 87, 123–127. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Galea, S.; Bucciarelli, A.; Vlahov, D. What Predicts Psychological Resilience after Disaster? The Role of Demographics, Resources, and Life Stress. J. Consult. Clin. Psychol. 2007, 75, 671–682. [Google Scholar] [CrossRef] [PubMed]
- García del Castillo, J.; García del Castillo-López, Á.; López-Sánchez, C.; Dias, P. Conceptualización Teórica de La Resiliencia Psicosocial y Su Relación Con La Salud. Health Addict. Drog. 2016, 16, 59. [Google Scholar] [CrossRef]
- Caro Alonso, P.Á.; Rodríguez-Martín, B.; Caro Alonso, P.Á.; Rodríguez-Martín, B. Potencialidades de La Resiliencia Para Los Profesionales de Enfermería. Index Enferm. 2018, 27, 42–46. [Google Scholar]
- Marriner Tomey, A.; Raile Alligood, M. Modelos y Teorías En Enfermería, 7th ed.; Elsevier Masson: Paris, France, 2011; 856p. [Google Scholar]
- Cortés Recaball, J.E. La Resiliencia: Una Mirada Desde la Enfermería. Cienc. Enferm. 2010, 16, 27–32. [Google Scholar] [CrossRef][Green Version]
- Benavent Garcés, A.; Ferrer Ferrandis, E.; Francisco del Rey, C. Fundamentos de Enfermería, 2nd ed.; DAE: Madrid, Spain, 2003. [Google Scholar]
- Cleary, M.; Kornhaber, R.; Thapa, D.K.; West, S.; Visentin, D. The Effectiveness of Interventions to Improve Resilience among Health Professionals: A Systematic Review. Nurse Educ. Today 2018, 71, 247–263. [Google Scholar] [CrossRef] [PubMed]
- Arrogante, O.; Pérez-García, A.M.; Aparicio-Zaldívar, E.G. Recursos personales relevantes para el bienestar psicológico en el personal de enfermería. Enferm. Intensiva 2016, 27, 22–30. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Stone, P.W. Popping the (PICO) Question in Research and Evidence-Based Practice. Appl. Nurs. Res. ANR 2002, 15, 197–198. [Google Scholar] [CrossRef] [PubMed]
- MeSH Browser. Medical Subject Headings 2021. Available online: https://meshb.nlm.nih.gov/search (accessed on 10 September 2021).
- The Joanna Briggs Institute. New JBI Levels of Evidence. Available online: https://jbi.global/sites/default/files/2019-05/JBI-Levels-of-evidence_2014_0.pdf (accessed on 10 September 2021).
- Zingg, W.; Castro-Sanchez, E.; Secci, F.V.; Edwards, R.; Drumright, L.N.; Sevdalis, N.; Holmes, A.H. Innovative Tools for Quality Assessment: Integrated Quality Criteria for Review of Multiple Study Designs (ICROMS). Public Health 2016, 133, 19–37. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Grimshaw, J.M.; Wells, G.A.; Boers, M.; Andersson, N.; Hamel, C.; Porter, A.C.; Tugwell, P.; Moher, D.; Bouter, L.M. Development of AMSTAR: A Measurement Tool to Assess the Methodological Quality of Systematic Reviews. BMC Med. Res. Methodol. 2007, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Declaración de La Iniciativa STROBE (Strengthening the Reporting of Observational Studies in Epidemiology): Directrices Para La Comunicación de Estudios Observacionales. Gac. Sanit. 2008, 22, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Afshari, D.; Nourollahi-darabad, M.; Chinisaz, N. Demographic Predictors of Resilience among Nurses during the COVID-19 Pandemic. Work 2021, 68, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Balay-odao, E.M.; Alquwez, N.; Inocian, E.P.; Alotaibi, R.S. Hospital Preparedness, Resilience, and Psychological Burden Among Clinical Nurses in Addressing the COVID-19 Crisis in Riyadh, Saudi Arabia. Front. Public Health 2021, 8, 943. [Google Scholar] [CrossRef]
- Cai, H.; Tu, B.; Ma, J.; Chen, L.; Fu, L.; Jiang, Y.; Zhuang, Q. Psychological Impact and Coping Strategies of Frontline Medical Staff in Hunan between January and March 2020 During the Outbreak of Coronavirus Disease 2019 (COVID-19) in Hubei, China. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020, 26, e924171. [Google Scholar] [CrossRef]
- Cai, W.; Lian, B.; Song, X.; Hou, T.; Deng, G.; Li, H. A Cross-Sectional Study on Mental Health among Health Care Workers during the Outbreak of Corona Virus Disease 2019. Asian J. Psychiatry 2020, 51, 102111. [Google Scholar] [CrossRef] [PubMed]
- De Pinho, L.G.; Sampaio, F.; Sequeira, C.; Teixeira, L.; Fonseca, C.; Lopes, M.J. Portuguese Nurses’ Stress, Anxiety, and Depression Reduction Strategies during the COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2021, 18, 3490. [Google Scholar] [CrossRef] [PubMed]
- Del Pozo-Herce, P.; Garrido-García, R.; Santolalla-Arnedo, I.; Gea-Caballero, V.; García-Molina, P.; Ruiz de Viñaspre-Hernández, R.; Rodríguez-Velasco, F.J.; Juárez-Vela, R. Psychological Impact on the Nursing Professionals of the Rioja Health Service (Spain) Due to the SARS-CoV-2 Virus. Int. J. Environ. Res. Public Health 2021, 18, 580. [Google Scholar] [CrossRef] [PubMed]
- Giusti, E.M.; Pedroli, E.; D’Aniello, G.E.; Stramba Badiale, C.; Pietrabissa, G.; Manna, C.; Stramba Badiale, M.; Riva, G.; Castelnuovo, G.; Molinari, E. The Psychological Impact of the COVID-19 Outbreak on Health Professionals: A Cross-Sectional Study. Front. Psychol. 2020, 11, 1684. [Google Scholar] [CrossRef]
- Kim, S.C.; Quiban, C.; Sloan, C.; Montejano, A. Predictors of Poor Mental Health among Nurses during COVID-19 Pandemic. Nurs. Open 2021, 8, 900–907. [Google Scholar] [CrossRef]
- Kılınç, T.; Çelik, A.S. Relationship between the Social Support and Psychological Resilience Levels Perceived by Nurses during the COVID-19 Pandemic: A Study from Turkey. Perspect. Psychiatr. Care 2021, 57, 1000–1008. [Google Scholar] [CrossRef]
- Labrague, L.J.; de los Santos, J. COVID-19 Anxiety among Frontline Nurses: Predictive Role of Organisational Support, Personal Resilience and Social Support. J. Nurs. Manag. 2020, 28, 1653–1661. [Google Scholar] [CrossRef]
- Leng, M.; Wei, L.; Shi, X.; Cao, G.; Wei, Y.; Xu, H.; Zhang, X.; Zhang, W.; Xing, S.; Wei, H. Mental Distress and Influencing Factors in Nurses Caring for Patients with COVID-19. Nurs. Crit. Care 2021, 26, 94–101. [Google Scholar] [CrossRef]
- Lorente, L.; Vera, M.; Peiró, T. Nurses´ Stressors and Psychological Distress during the COVID-19 Pandemic: The Mediating Role of Coping and Resilience. J. Adv. Nurs. 2020, 77, 1335–1344. [Google Scholar] [CrossRef]
- Luceño-Moreno, L.; Talavera-Velasco, B.; García-Albuerne, Y.; Martín-García, J. Symptoms of Posttraumatic Stress, Anxiety, Depression, Levels of Resilience and Burnout in Spanish Health Personnel during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5514. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The Psychological and Mental Impact of Coronavirus Disease 2019 (COVID-19) on Medical Staff and General Public—A Systematic Review and Meta-Analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- Lyu, H.; Yao, M.; Zhang, D.; Liu, X. The Relationship among Organizational Identity, Psychological Resilience and Work Engagement of the First-Line Nurses in the Prevention and Control of COVID-19 Based on Structural Equation Model. Risk Manag. Healthc. Policy 2020, 13, 2379–2386. [Google Scholar] [CrossRef] [PubMed]
- Nie, A.; Su, X.; Zhang, S.; Guan, W.; Li, J. Psychological Impact of COVID-19 Outbreak on Frontline Nurses: A Cross-Sectional Survey Study. J. Clin. Nurs. 2020, 29, 4217–4226. [Google Scholar] [CrossRef] [PubMed]
- Ou, X.; Chen, Y.; Liang, Z.; Wen, S.; Li, S.; Chen, Y. Resilience of Nurses in Isolation Wards during the COVID-19 Pandemic: A Cross-Sectional Study. Psychol. Health Med. 2021, 26, 98–106. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, C.; Pan, W.; Zheng, J.; Gao, J.; Huang, X.; Cai, S.; Zhai, Y.; Latour, J.M.; Zhu, C. Stress, Burnout, and Coping Strategies of Frontline Nurses During the COVID-19 Epidemic in Wuhan and Shanghai, China. Front. Psychiatry 2020, 11, 565520. [Google Scholar] [CrossRef]
- Pollock, A.; Campbell, P.; Cheyne, J.; Cowie, J.; Davis, B.; McCallum, J.; McGill, K.; Elders, A.; Hagen, S.; McClurg, D.; et al. Interventions to Support the Resilience and Mental Health of Frontline Health and Social Care Professionals during and after a Disease Outbreak, Epidemic or Pandemic: A Mixed Methods Systematic Review. Cochrane Database Syst. Rev. 2020, 11, CD013779. [Google Scholar] [CrossRef]
- Cunill Olivas, M.; Aymerich Andreu, M.; Serdà Ferrer, B.-C.; Patiño Masó, J. The Impact of COVID-19 on Spanish Health Professionals: A Description of Physical and Psychological Effects. Int. J. Ment. Health Promot. 2020, 22, 185–198. [Google Scholar] [CrossRef]
- Rieckert, A.; Schuit, E.; Bleijenberg, N.; ten Cate, D.; de Lange, W.; de Man-van Ginkel, J.M.; Mathijssen, E.; Smit, L.C.; Stalpers, D.; Schoonhoven, L.; et al. How Can We Build and Maintain the Resilience of Our Health Care Professionals during COVID-19? Recommendations Based on a Scoping Review. BMJ Open 2021, 11, e043718. [Google Scholar] [CrossRef]
- Rodriguez-Vega, B.; Palao, Á.; Muñoz-Sanjose, A.; Torrijos, M.; Aguirre, P.; Fernández, A.; Amador, B.; Rocamora, C.; Blanco, L.; Marti-Esquitino, J.; et al. Implementation of a Mindfulness-Based Crisis Intervention for Frontline Healthcare Workers During the COVID-19 Outbreak in a Public General Hospital in Madrid, Spain. Front. Psychiatry 2020, 11, 1170. [Google Scholar] [CrossRef]
- Molina, F.J.C. Nosocomios higienistas: El caso Florence Nightingale. Cult. Cuid. 2013, 36, 96–105. [Google Scholar] [CrossRef][Green Version]
- Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Sadavoy, J.; Verhaeghe, L.M.; Steinberg, R.; Mazzulli, T. The Immediate Psychological and Occupational Impact of the 2003 SARS Outbreak in a Teaching Hospital. CMAJ Can. Med. Assoc. J. 2003, 168, 1245–1251. [Google Scholar]
- Xiang, Y.-T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely Mental Health Care for the 2019 Novel Coronavirus Outbreak Is Urgently Needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The Psychological Impact of the SARS Epidemic on Hospital Employees in China: Exposure, Risk Perception, and Altruistic Acceptance of Risk. Can. J. Psychiatry Rev. Can. Psychiatr. Assoc. 2009, 54, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Chew, Q.H.; Wei, K.C.; Vasoo, S.; Chua, H.C.; Sim, K. Narrative Synthesis of Psychological and Coping Responses towards Emerging Infectious Disease Outbreaks in the General Population: Practical Considerations for the COVID-19 Pandemic. Singap. Med. J. 2020, 61, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Chou, L.-P.; Li, C.-Y.; Hu, S.C. Job Stress and Burnout in Hospital Employees: Comparisons of Different Medical Professions in a Regional Hospital in Taiwan. BMJ Open 2014, 4, e004185. [Google Scholar] [CrossRef]
- Maunder, R.G.; Lancee, W.J.; Rourke, S.; Hunter, J.J.; Goldbloom, D.; Balderson, K.; Petryshen, P.; Steinberg, R.; Wasylenki, D.; Koh, D.; et al. Factors Associated With the Psychological Impact of Severe Acute Respiratory Syndrome on Nurses and Other Hospital Workers in Toronto. Psychosom. Med. 2004, 66, 938–942. [Google Scholar] [CrossRef] [PubMed]
- Koh, D.; Lim, M.K.; Chia, S.E.; Ko, S.M.; Qian, F.; Ng, V.; Tan, B.H.; Wong, K.S.; Chew, W.M.; Tang, H.K.; et al. Risk Perception and Impact of Severe Acute Respiratory Syndrome (SARS) on Work and Personal Lives of Healthcare Workers in Singapore: What Can We Learn? Med. Care 2005, 43, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Chung, B.P.M.; Wong, T.K.S.; Suen, E.S.B.; Chung, J.W.Y. SARS: Caring for Patients in Hong Kong. J. Clin. Nurs. 2005, 14, 510–517. [Google Scholar] [CrossRef]
- Khalid, I.; Khalid, T.J.; Qabajah, M.R.; Barnard, A.G.; Qushmaq, I.A. Healthcare Workers Emotions, Perceived Stressors and Coping Strategies During a MERS-CoV Outbreak. Clin. Med. Res. 2016, 14, 7–14. [Google Scholar] [CrossRef]
- Leng, M.; Xiu, H.; Yu, P.; Feng, J.; Wei, Y.; Cui, Y.; Zhang, M.; Zhou, Y.; Wei, H. Current State and Influencing Factors of Nurse Resilience and Perceived Job-Related Stressors. J. Contin. Educ. Nurs. 2020, 51, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.-F.; Cross, W.; Plummer, V.; Lam, L.; Luo, Y.-H.; Zhang, J.-P. Exploring Resilience in Chinese Nurses: A Cross-Sectional Study. J. Nurs. Manag. 2017, 25, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Chua, S.E.; Cheung, V.; Cheung, C.; McAlonan, G.M.; Wong, J.W.S.; Cheung, E.P.T.; Chan, M.T.Y.; Wong, M.M.C.; Tang, S.W.; Choy, K.M.; et al. Psychological Effects of the SARS Outbreak in Hong Kong on High-Risk Health Care Workers. Can. J. Psychiatry Rev. Can. Psychiatr. Assoc. 2004, 49, 391–393. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-S.; Lee, E.-H.; Park, N.-R.; Choi, Y.H. Mental Health of Nurses Working at a Government-Designated Hospital during a MERS-CoV Outbreak: A Cross-Sectional Study. Arch. Psychiatr. Nurs. 2018, 32, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Bradley, J.R.; Cartwright, S. Social Support, Job Stress, Health, and Job Satisfaction among Nurses in the United Kingdom. Int. J. Stress Manag. 2002, 9, 163–182. [Google Scholar] [CrossRef]
- Hu, S.H.; Yu, Y.-M.; Chang, W.-Y.; Lin, Y.-K. Social Support and Factors Associated with Self-Efficacy among Acute-Care Nurse Practitioners. J. Clin. Nurs. 2018, 27, 876–882. [Google Scholar] [CrossRef]
- Tusaie, K.; Dyer, J. Resilience: A Historical Review of the Construct. Holist. Nurs. Pract. 2004, 18, 3–8. [Google Scholar] [CrossRef]
- Stanisławski, K. The Coping Circumplex Model: An Integrative Model of the Structure of Coping with Stress. Front. Psychol. 2019, 10, 694. [Google Scholar] [CrossRef]
- Lazarus, R. Toward Better Research on Stress and Coping. Am. Psychol. 2000, 55, 665–673. [Google Scholar] [CrossRef]
- Day, A.L.; Livingstone, H.A. Gender Differences in Perceptions of Stressors and Utilization of Social Support among University Students. Can. J. Behav. Sci. 2003, 35, 73–83. [Google Scholar] [CrossRef]
- González-Morales, M.G.; Rodríguez, I.; Peiró, J.M. A Longitudinal Study of Coping and Gender in a Female-Dominated Occupation: Predicting Teachers’ Burnout. J. Occup. Health Psychol. 2010, 15, 29–44. [Google Scholar] [CrossRef]
- Jackson, D.; Bradbury-Jones, C.; Baptiste, D.; Gelling, L.; Morin, K.; Neville, S.; Smith, G.D. Life in the Pandemic: Some Reflections on Nursing in the Context of COVID-19. J. Clin. Nurs. 2020, 29, 2041–2043. [Google Scholar] [CrossRef] [PubMed]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr. Psychiatry Rep. 2020, 22, 43. [Google Scholar] [CrossRef] [PubMed]
- Kemper, K.J.; Mo, X.; Khayat, R. Are Mindfulness and Self-Compassion Associated with Sleep and Resilience in Health Professionals? J. Altern. Complement. Med. 2015, 21, 496–503. [Google Scholar] [CrossRef]
- Greenberg, N.; Wessely, S.; Wykes, T. Potential Mental Health Consequences for Workers in the Ebola Regions of West Africa—A Lesson for All Challenging Environments. J. Ment. Health 2015, 24, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Kamal-Yanni, M. Never Again: Building Resilient Health Systems and Learning from the Ebola Crisis; Oxfam International: Nairobi, Kenya, 2015; Volume 12, Available online: https://oxfamilibrary.openrepository.com/bitstream/handle/10546/550092/bp-never-again-resilient-health-systems-ebola-160415-fr.pdf (accessed on 10 September 2021).
- Traynor, M. Guest Editorial: What’s Wrong with Resilience. J. Res. Nurs. 2018, 23, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Kruk, M.E.; Myers, M.; Varpilah, S.T.; Dahn, B.T. What Is a Resilient Health System? Lessons from Ebola. Lancet 2015, 385, 1910–1912. [Google Scholar] [CrossRef]
- Jackson, D.; Firtko, A.; Edenborough, M. Personal Resilience as a Strategy for Surviving and Thriving in the Face of Workplace Adversity: A Literature Review. J. Adv. Nurs. 2007, 60, 1–9. [Google Scholar] [CrossRef]
- McAllister, M.; McKinnon, J. The Importance of Teaching and Learning Resilience in the Health Disciplines: A Critical Review of the Literature. Nurse Educ. Today 2009, 29, 371–379. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).