Abstract
Background and Objectives: Obesity is a significant risk factor for cardiovascular disease. Physical exercise has been established as an effective intervention for reducing cardiovascular mortality. This systematic review aimed to investigate the effects of various exercise modalities on cardiovascular risk factors in men with obesity. Materials and Methods: This review included randomized controlled trials (RCTs) published between 2005 and November 2023. Studies were eligible if they assessed the impact of exercise interventions on blood pressure (BP), lipid profiles, and glucose/insulin regulation in males aged 18 years or older with a body mass index (BMI) of 25 kg/m2 or greater. The quality of included studies was evaluated using the Physiotherapy Evidence Database (PEDro) scale. Results: A total of 25 RCTs were included in the analysis, with PEDro scores ranging from 3 to 7. High-intensity interval training (HIIT) was associated with significant reductions in BP, with an average decrease of 12.5 mmHg. However, the magnitude of BP reduction varied across studies, likely due to differences in training protocols and study quality. Resistance training (RT) was associated with modest improvements in glycemic control, with some studies reporting a reduction in fasting blood glucose levels by 5–10%. Combined exercise (CT) programs, which included both aerobic and resistance training, as well as aerobic exercise alone, were shown to improve lipid profiles, with some studies showing reductions in total cholesterol levels ranging from 10–15%. However, the findings were inconsistent, highlighting the need for further research to better understand the potential benefits and optimal exercise regimens. Conclusions: This systematic review supports the potential of exercise training in reducing cardiovascular risk factors in men with obesity, though the effectiveness varies depends on the type of exercise. Combined exercise programs have shown promise for lipid profiles, but further research is needed to confirm these effects. HIIT has been linked to BP reductions in some studies, although the results are inconsistent and depend on protocols and study quality. The limitations in study quality may impact the reliability of these findings.
1. Introduction
Obesity, defined as a body mass index (BMI) of 30 kg/m2 or greater, is a chronic condition with profound health and economic consequences. Its global prevalence has risen sharply in recent decades. According to the World Health Organization (WHO), 43% of adults were overweight in 2022, with 16% classified as obese. Obesity rates are particularly high in North America, Europe, and the Western Pacific, but low- and middle-income countries are also experiencing significant increases [1,2]. Projections suggest that by 2030, 20% of women and 15% of men globally will be affected by obesity [3], contributing to as much as 2.8% of national healthcare costs [4].
Obesity is a critical risk factor for the development of various chronic diseases, including cardiovascular disease (CVD), type 2 diabetes, and certain types of cancer [5]. Given its strong association with hypertension and dyslipidemia, obesity is recognized as one of the top 10 CVD risk factors by the American Society for Preventive Cardiology (ASPC) [6].
The health risks associated with obesity increase proportionally with higher BMI [7]. These risks are closely linked to metabolic disturbances, such as altered glucose and fat metabolism [8] and elevated BP [9]. While the association between weight gain and hypertension is well-established, the precise underlying mechanisms, including insulin resistance and hyperinsulinemia, remain subjects of ongoing investigation [7].
Physical inactivity exacerbates obesity-related health risks and is a leading cause of preventable mortality worldwide [10]. Exercise, particularly aerobic exercise and RT, is an essential component in the management of overweight and obesity [11]. Aerobic exercise can help reduce visceral fat, improve lean body mass, lower BP, enhance lipid profiles, and decrease triglyceride levels, all of which may contribute to better cardiovascular health [12]. The World Health Organization (WHO) underscores aerobic exercise as a beneficial approach to supporting cardiovascular health. Activities such as walking, cycling, and swimming are believed to contribute to improvements in blood pressure, triglyceride levels, and HDL cholesterol. Evidence indicates that regular aerobic exercise might help lower triglycerides by 10–20%, which could have a positive impact on cardiovascular risk in individuals with obesity [13].
Resistance training (RT), while not as immediately impactful as aerobic exercise on certain cardiovascular markers, has been associated with potential benefits such as maintaining muscle mass, promoting insulin sensitivity, and influencing metabolic rate. These factors may contribute to the management of obesity over time [14].
High-intensity interval training (HIIT), which involves short bursts of intense activity followed by recovery periods, has been suggested to improve vascular function and lead to modest reductions in blood pressure, potentially offering benefits beyond those of traditional moderate-intensity exercise. Some studies indicate that HIIT might help reduce visceral fat and modestly enhance insulin sensitivity, which could contribute to better regulation of blood glucose levels in individuals with obesity [15]. However, due to its higher intensity, HIIT may not be ideal for everyone, particularly individuals with specific cardiovascular conditions, and its demanding nature could pose challenges for adherence and long-term sustainability [16].
Combining aerobic exercise and RT is considered a potentially effective strategy for supporting metabolic health and addressing multiple risk factors. Some studies suggest that this combined approach might contribute to improvements in body composition, insulin sensitivity, and lipid profiles compared to focusing on a single type of exercise [17].
Despite these findings, much of the existing literature has concentrated on isolated exercise modalities, with relatively limited exploration of how combined exercise strategies influence cardiovascular risk factors in individuals with overweight or obesity. This gap highlights an opportunity for a more comprehensive understanding of how diverse exercise approaches can synergistically address metabolic health. While previous reviews have predominantly focused on individual exercise types, this review uniquely emphasizes the comparative effects of HIIT, MICT, CT, and resistance training RT on cardiovascular health indicators, such as lipid profiles, BP, glucose regulation, and insulin sensitivity. Given the widespread prevalence of obesity and its well-documented association with cardiovascular risk, understanding the relative and combined impacts of different exercise modalities is an important area of study.
This systematic review aims to evaluate the effectiveness of various exercise interventions in improving cardiovascular risk factors—specifically lipid profiles, blood pressure, BP levels, and insulin sensitivity—in men with overweight or obesity. By synthesizing the available evidence, this study aims to offer informed recommendations for exercise prescriptions tailored to this population.
2. Methods
This systematic review was conducted following the guidelines provided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [18].
2.1. Data Sources and Search Strategy
Two researchers independently conducted a comprehensive search for studies published between 2005 and November 2023. The following electronic databases were searched systematically: PubMed, Web of Science, PEDro, ScienceDirect, and Google Scholar. The search strategy used a combination of relevant terms related to exercise, cardiovascular risk factors, and obesity. The key search terms included the following:
Exercise-related terms: “Exercise training”, “exercise”, “training”, “resistance training”, “strength training”, “aerobic exercise”, “aerobic training”, “high-intensity interval training”, “moderate-intensity continuous training”, “HIIT”, “HIT”, “MICT”, “physical activity”.
Cardiovascular risk factors: “lipid profile”, “HDL”, “LDL”, “VLDL”, “cholesterol”, “triglycerides”, “TG”, “high-density lipoprotein”, “low-density lipoprotein”, “very-low-density lipoprotein cholesterol”, “insulin”, “insulin resistance”, “insulin sensitivity”, “glucose”, “glucose tolerance”, “blood pressure”, “systolic BP”, “diastolic BP”.
Obesity-related terms: “Obese males”, “obese male”, “obesity”, “overweight males”.
The search terms were combined using Boolean operators, such as AND to link different concepts (e.g., “exercise AND cardiovascular risk factors AND obesity”), and OR to include synonyms for key terms. Only studies published in English were considered.
2.2. Eligibility Criteria
To be eligible for inclusion, studies had to be randomized controlled trials (RCTs) that compared the effects of any type of exercise training (aerobic, RT, HIIT, MICT, or a combination of exercises) against a no-exercise control group or another exercise modality. Studies must have provided detailed information about the type, intensity, frequency, and duration of the exercise intervention.
The following inclusion criteria were applied:
Participants: Males aged 18 years or older with a body mass index (BMI) ≥ 25, classified as overweight or obese.
Interventions: Studies must involve structured exercise interventions with specified parameters (type, intensity, duration, and frequency).
Control Group: Studies must include a comparison group that did not engage in any exercise or involved a different exercise modality.
Outcomes: Studies must report on cardiovascular risk factors such as lipid profiles, blood pressure (BP), blood glucose, and insulin sensitivity.
2.3. Exclusion Criteria Included
Single-session interventions: Studies that involved one-off interventions were excluded. We did not aim to investigate the acute effects of a single exercise session, as single-session interventions often lack the necessary duration and consistency to produce meaningful, lasting changes in cardiovascular risk factors. In fact, our goal was to identify exercise interventions that lead to long-term improvements in cardiovascular risk factors. Numerous studies have highlighted the importance of the frequency, intensity, and duration of exercise in determining its effectiveness.
Participants with existing cardiovascular or other chronic diseases: Studies that involved participants with diagnosed cardiovascular diseases, diabetes, or other major chronic conditions were excluded unless the study provided separate data for healthy male participants.
Mixed-gender studies: Studies that reported combined results for both male and female participants were included only if data specific to males were available.
Non-RCT studies: Only randomized controlled trials were included in the review.
Duplicates and studies not meeting the eligibility criteria were excluded during the initial screening process.
2.4. Data Extraction and Verification
Data from eligible studies were independently extracted by two reviewers (Author 1 and Author 2) using a standardized form. The following data were extracted: study characteristics (authors, year of publication, sample size, and demographic information), details of the exercise intervention (type, frequency, intensity, and duration), and the outcomes of interest (e.g., blood pressure, lipid profiles, glucose levels, and insulin sensitivity). Discrepancies between reviewers were resolved through discussion and if consensus was not reached a third reviewer (Author 3) was consulted to make a final decision.
2.5. Quality Assessment
The methodological quality of the included studies was assessed using the Physiotherapy Evidence Database (PEDro) scale, which scores studies from 0 to 10 based on their methodological rigor. Studies scoring 9–10 were considered of “excellent” quality, scores between 6–8 were rated as “good”, and studies scoring 4–5 were deemed “fair”. Studies scoring below 4 were excluded from the review due to methodological concerns. While the inclusion of studies with PEDro scores of 4–5 may limit the strength of the evidence, such studies were included because they contributed valuable information to the research question. However, these studies’ findings were interpreted with caution due to their lower methodological quality [19].
2.6. The Evidence Levels
The strength of the evidence was classified according to the Sackett scale [20].
Level 1a (strong evidence): At least two high-quality RCTs with similar results.
Level 1b (moderate evidence): One high-quality RCT.
Level 2a (limited evidence): At least one fair-quality RCT.
Level 2b (limited evidence): At least one poor-quality RCT.
2.7. PRISMA Flowchart
A PRISMA flowchart was used to visually represent the study selection process, showing the number of studies identified, screened, assessed for eligibility, and ultimately included in the review. Reasons for exclusions were recorded at each stage of the process, including irrelevant study designs, failure to meet inclusion criteria, or insufficient reporting of outcomes.
2.8. Data Analysis and Synthesis
Due to the variations in exercise protocols across the studies included in this review, some degree of variability (heterogeneity) in the results was anticipated, which may affect the overall interpretation. Although a meta-analysis was not possible because of considerable differences in both the exercise modalities and participant characteristics, we performed a descriptive assessment to examine the heterogeneity. A qualitative synthesis was used to summarize the findings, grouping studies by the type of exercise intervention (e.g., aerobic exercise, resistance training, HIIT, MICT, or CT) and the cardiovascular risk factors measured (e.g., lipid profiles, blood pressure, glucose, and insulin sensitivity).
In addition, we examined potential sources of variability, including factors such as exercise intensity, duration, frequency, and characteristics of the study participants (e.g., age, BMI, and baseline health status). For instance, variations in exercise intensity, such as the differences between HIIT and MICT, could influence cardiovascular risk factors differently, and we incorporated these aspects into the synthesis of the results.
3. Results
3.1. Study Selection
A total of 2541 studies were initially identified. After removing duplicates and irrelevant studies, 529 studies remained. Following screening of titles and abstracts, 105 studies were selected for full-text review. Of these, 22 were excluded for failing to meet the inclusion criteria, leaving 83 studies. After further excluding non-RCT studies, 25 articles were ultimately included in the final review. The study selection process is depicted in Figure 1.
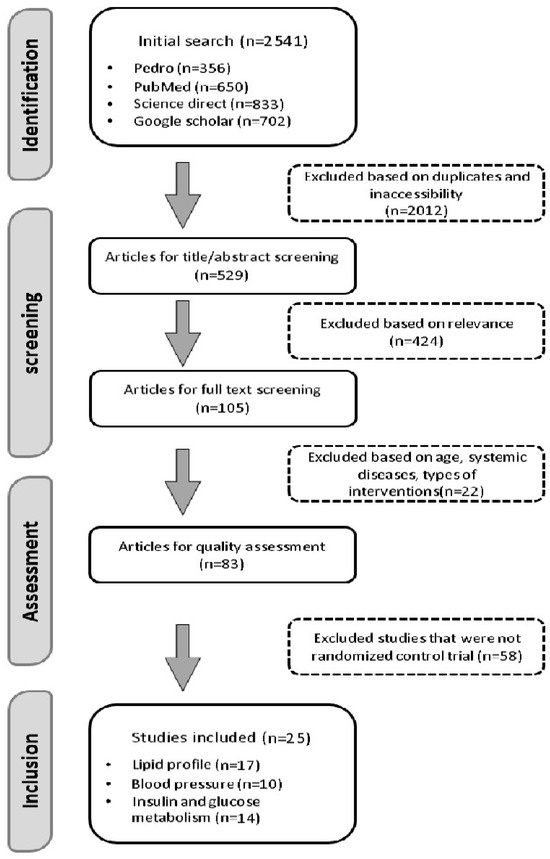
Figure 1.
PRISMA flow chart of search strategy. This figure illustrates the selection process of the reviewed studies.
3.2. Characteristics of the Included Studies
The 25 studies included 2374 male participants aged 18 to 72 years, all classified as overweight or obese (BMI ≥ 25). None of the participants had a history of cardiovascular disease or other chronic conditions. BMI classifications were used to define overweight (25.0 to <30 kg/m2) and obese (≥30 kg/m2) participants. The details of the included studies’ quality are presented in Table 1.

Table 1.
The quality of the reviewed studies using the PEDro scale.
Due to significant heterogeneity across the studies in terms of exercise protocols (type, frequency, duration, and intensity), it was not feasible to conduct a meta-analysis. A qualitative synthesis was therefore performed as presented in Table 2.

Table 2.
Sackett’s levels of evidence for outcomes.
3.3. Characteristics of Exercise Programs
Endurance Training (ET): Training regimens varied between six [43] and 22 [38] weeks, performed three to five days per week at moderate intensity.
HIIT: The training duration ranged from 3 [37] weeks through to 6 [24], 8 [22,44], 12 [26], and 16 [35] weeks, with one to three sessions per week at high intensity (80–100%). Session durations ranged from 30 to 60 min.
RT: Interventions varied from eight [27,33,36] to 12 [14,34] and 24 [41] weeks at moderate to high intensity, performed three times per week, with each session lasting approximately 60 min.
CT: Training programs lasted between 12 [23,25,29,32,42], 22 [38], and 24 [28,30] weeks, performed three days per week at moderate intensity, and each session lasted between 60 to 120 min.
Strength Training: Strength training was examined in one study with 22 [38] week protocols, performed three times per week at 90% of one-repetition maximum (1RM).
3.4. Outcomes
3.4.1. Blood Pressure
Studies and Participants: A total of 818 participants from 10 studies, aged 18–50+, with overweight or obesity, were analyzed.
Exercise Interventions: Interventions included HIIT, MICT (3 studies) [22,24,26], CT (3 studies) [23,25,29], RT (1 study) [14], aerobic exercise (2 studies) [39,43], boxing (1 study) [21], and tai chi (1 study) [29].
Findings: HIIT consistently demonstrated significant reductions in blood pressure (BP) across all studies. MICT showed no significant difference compared to HIIT. One RT study and interventions like boxing and tai chi also reported significant reductions. Aerobic exercise demonstrated non-significant reductions in BP.
Quality and Evidence: HIIT and MICT provided limited evidence (Level 2a) for BP reduction based on three fair-quality RCTs. CT showed moderate evidence (Level 1b), supported by one high-quality and two fair-quality RCTs. Aerobic exercise showed limited evidence (Level 2a) from two fair-quality RCTs (Table 3).

Table 3.
Summary of study characteristics and findings on the effects of exercise training on blood pressure in overweight or obese males.
3.4.2. Blood Insulin and Glucose
Studies and Participants: Fourteen RCT studies with 456 total participants were reviewed.
Exercise Interventions: HIIT, MICT [22,35,37,44], CT [28,30,32,42], RT [14,27,33,34,36], and aerobic exercise [31] were analyzed.
Findings: HIIT led to significant reductions in insulin and glucose in only one of five studies. RT demonstrated significant improvements in all five studies, while aerobic exercise showed no significant changes. CT produced reductions in insulin and glucose in two out of three studies.
Quality and Evidence: HIIT and MICT demonstrated limited evidence (Level 1b) for reducing insulin and glucose. RT provided moderate evidence (Level 2a) from five fair-quality RCTs. CT also showed moderate evidence (Level 2a) based on three fair-quality RCTs (Table 4 and Table 5).

Table 4.
Summary of study characteristics and findings on the effects of exercise training on blood insulin and glucose in males with overweight or obesity.

Table 5.
Summary of study characteristics and findings on the effects of exercise training on lipid profile in males with overweight or obesity.
3.4.3. Lipid Profile
Studies and Participants: Seventeen RCT studies involving 1100 participants with obesity or overweight.
Exercise Interventions: HIIT, MICT [22,24,35,37], CT [23,25,28,29,42], RT [14,33,41], aerobic exercise [31,39,40,43], strength training [38], and tai chi [29] were included.
Finding:
HDL: HIIT showed significant increases in HDL in one of five studies, while MICT and RT yielded mixed results. CT showed improvements in HDL in two of five studies, and aerobic exercise showed positive effects in three of five studies.
LDL: HIIT showed significant reductions in LDL in one of three studies, with similar results in MICT. RT showed mixed results, while CT showed reductions in LDL in two of four studies.
Triglycerides (TG): HIIT and MICT did not significantly reduce TG. However, RT and strength training demonstrated positive outcomes.
Total Cholesterol (TC): HIIT and RT did not show significant reductions in TC, while CT and aerobic exercise resulted in significant reductions.
Quality and Evidence:
HDL: HIIT and MICT demonstrated moderate evidence (Level 1b) for improvements in HDL.
LDL and TG: RT and CT showed mixed evidence; however, CT provided moderate evidence (Level 1b) based on high-quality RCTs.
TC: Aerobic exercise and CT demonstrated moderate evidence (Level 1b) for TC reduction.
4. Discussion
This systematic review aimed to assess the effects of various exercise modalities—HIIT, MICT, RT, CT, and aerobic exercise—on cardiovascular risk factors in overweight and obese males (Table 6, Table 7 and Table 8). The overall results indicate that exercise interventions generally resulted in positive changes in BP, glucose levels, insulin sensitivity, and lipid profiles. However, significant heterogeneity across studies limits the ability to draw definitive conclusions. This variability likely arises from differences in exercise protocols (e.g., duration, intensity, and frequency), study designs, and participant characteristics.

Table 6.
Summary table (effects of exercise training on blood pressure in males with overweight or obesity).

Table 7.
Summary table (effects of exercise training on blood insulin and glucose in males with overweight or obesity).

Table 8.
Summary table (effects of exercise training on lipid profile in males with overweight or obesity).
Inter-study variability constitutes a key factor in interpreting these findings. Divergences in exercise modalities, encompassing duration, intensity, frequency, and specific type (e.g., HIIT, MICT, or RT), emerged as significant sources of this heterogeneity. For instance, HIIT interventions typically spanned durations of 6 to 16 weeks, with 1 to 3 sessions per week. In contrast, MICT programs were generally longer, extending from 12 to 24 weeks, and often involved 3 to 5 sessions per week. Furthermore, the intensity of HIIT was substantially greater than that of MICT or aerobic exercise, which may explain the more pronounced improvements in BP and insulin sensitivity observed in some HIIT studies. While MICT demonstrated beneficial effects, these were generally less pronounced compared to the outcomes observed with HIIT.
Most of the included studies were assessed as having fair quality. Some studies presented with limitations such as small sample sizes, short follow-up periods, or methodological shortcomings (e.g., inadequate randomization or blinding). These methodological limitations may have influenced the observed findings and potentially reduced the generalizability of the results. Notably, studies investigating HIIT demonstrated consistent benefits in reducing BP, whereas those examining RT and aerobic exercise exhibited more varied results. This variability in study quality raises concerns regarding the robustness of the evidence, particularly for RT and aerobic exercise, where smaller sample sizes and methodological flaws may have exerted a significant impact on the observed outcomes.
Several studies reported non-significant findings, particularly with respect to glucose and lipid profiles. This observation suggests that exercise interventions alone, in the absence of concomitant dietary or pharmacological interventions, may not be sufficient to induce significant improvements in these crucial cardiovascular risk factors within the context of obesity. However, it is important to emphasize that non-significant results do not necessarily imply the ineffectiveness of the exercise interventions. The lack of statistically significant effects could be attributed to factors such as small sample sizes or short intervention durations, which may not have been sufficient to allow for the observation of meaningful clinical changes. Furthermore, the modest improvements observed in some studies may reflect the inherent complexities associated with managing metabolic conditions in individuals with obesity.
Participant demographics, including age, BMI, and baseline health status, also exerted a significant influence on the observed outcomes. For instance, studies involving older adults or individuals with more severe obesity demonstrated distinct responses to exercise interventions compared to younger individuals with milder obesity. This observed demographic variability underscores the critical need for targeted research that meticulously accounts for individual differences in exercise response.
4.1. Blood Pressure
High-intensity interval training was associated with a consistent reduction in BP in males with obesity, with similar effects observed for MICT. However, HIIT appeared to produce somewhat greater improvements, particularly in systolic BP, compared to other exercise modalities, which is consistent with findings from previous systematic reviews and original studies [16,45]. These improvements are likely attributable to a reduction in peripheral vascular resistance, a consequence of enhanced endothelial function and increased vascular shear stress induced by high-intensity exercise [21]. It is noteworthy that, despite the considerably shorter duration of HIIT interventions compared to other exercise modalities (for example, one study implemented five 1 min bouts with 1 minute of active recovery), reductions in systolic blood pressure were still observed. Furthermore, variations in exercise frequency, ranging from one to three days per week, did not significantly alter the observed outcomes (reviewed in a single study).
Resistance training (RT) demonstrated a more limited effect on blood pressure (BP) compared to other interventions. The modest improvements observed in RT studies may be attributed to several factors, including the small number of studies (n = 1) and its relatively brief duration (≤12 weeks). While shorter RT programs may not lead to significant BP reductions, previous research indicates that longer RT interventions might yield greater improvements in BP [46]. The variability in RT protocols, including intensity, volume, and short durations, likely limited BP improvements. Low-intensity RT may also be insufficient for significant cardiovascular benefits, highlighting the importance of considering program duration and intensity for BP management in obesity.
Combined training (CT) may offer some benefits for BP, although the underlying mechanisms are not fully understood. The possible reasons for the observed BP improvements include changes in arterial stiffness or reductions in plasma epinephrine levels. The variability in CT protocols, such as different combinations of aerobic and resistance training modalities complicates the ability to draw definitive conclusions regarding its effectiveness for BP management. Some combined exercise protocols were implemented concurrently, while others were conducted in separate sessions. Additionally, the duration of each session varied, ranging from 60 min to 120 min. In comparison, aerobic exercise alone typically shows more limited effects on BP, with some studies indicating no significant reductions. This finding is consistent with other research, suggesting that the impact of aerobic exercise on BP may vary, potentially influenced by factors such as the intensity and duration of exercise, or the integration of different training modalities [47,48].
It is crucial to acknowledge that the quality of the included studies exhibited variability. The studies focusing on HIIT had a higher quality rating (1b) compared to the other studies (2a). Furthermore, two studies investigating combined training and endurance training had small sample sizes, with only 6 and 9 participants in each group, respectively. These small sample sizes may have influenced the findings and affected the overall reliability of the results.
4.2. Blood Insulin and Glucose
HIIT was linked to slight improvements in insulin resistance in obese men, though its impact on glucose and insulin regulation was not significant. These findings may be influenced by variations in participant characteristics, such as age. The participants in these studies ranged in age from 18 to 50 years. It is likely that older men might respond differently to exercise compared to younger individuals, which could explain the differences in the study outcomes. Some studies reported no significant effects on glucose metabolism, suggesting that other factors, such as alterations in body composition, may exert a more substantial influence on improving insulin sensitivity than exercise intensity alone [49]. Although some studies have noted a reduction in body fat percentage or BMI, others have found no significant changes in body fat levels, as several systematic reviews have concluded that exercise interventions alone may not induce clinically significant weight loss [50]. Resistance training (RT) demonstrated beneficial effects on insulin sensitivity and blood insulin levels, while exhibiting minimal effects on glucose tolerance. These improvements may be attributed to an increase in lean body mass and enhanced muscle metabolic properties [51]. The effectiveness of RT in improving insulin levels and sensitivity appears to be influenced by the intensity and volume of the exercises. Non-periodized protocols (characterized by steady intensity and volume) and linear periodization (which involves a gradual increase in intensity and a decrease in volume) did not significantly affect insulin levels. In contrast, an undulating periodized protocol, which incorporates a weekly progression in exercise intensity, resulted in significant improvements in insulin regulation (reviewed in a single study). Combined training (CT), incorporating both aerobic and resistance exercises, also exerted a positive influence on insulin and glucose regulation, whereas aerobic exercise alone exhibited limited effects on fasting glucose [48]. This suggests that a CT approach may offer more comprehensive benefits for glucose regulation compared to any single exercise modality. It is important to note that CT protocols reviewed in this study had a longer duration compared to aerobic exercise alone (24 weeks vs. 8 weeks). Additionally, the duration of each training session in the CT studies was longer than that in aerobic exercise (60 min vs. 30 min). These differences in both training duration and session length may influence the results, independent of the type of exercise performed.
Resistance training (RT) and CT studies included in this review exhibited higher methodological quality than the HIIT and IT studies (1b VS. 2a), it is important to note that the RT studies involved younger participants (ranging from 23 to 36 years) and showed less age variability. In contrast, the studies with HIIT and ET had a wider age range (18 to 68 years), which may have contributed to greater variability in the effects of exercise.
4.3. Lipid Profile
This review found that HIIT exhibited minimal effects on most lipid factors, including triglycerides and total cholesterol, while demonstrating slight improvements in HDL and LDL levels in males with obesity. These findings are consistent with the observations of Batacan et al. (2017), who suggested that longer-duration HIIT interventions may be required to observe significant alterations in lipid profiles [52]. The majority of studies examining the effect of HIIT on lipid profiles were short-term and utilized very high-intensity protocols, such as 10 repetitions of 1 min running bouts at 80–90% HR max. The lack of substantial lipid improvements may be attributed to HIIT’s potential to reduce fatty acid release into the bloodstream by limiting blood flow to adipose tissue, although further research is necessary to elucidate this mechanism [53]. Furthermore, the variability in HIIT protocols, including differences in intensity, duration, and frequency across studies, likely contributes to the mixed results observed (e.g., 10 one-minute bouts vs. 5 two-minute bouts, each performed at varying intensities). For example, the short-term nature of many HIIT interventions, as well as the use of high-intensity protocols, may limit the long-term effects on lipid metabolism.
Resistance training (RT) exhibited minimal effects on lipid profiles, with no discernible changes in total cholesterol. Previous research on RT has demonstrated mixed results, likely attributable to variations in genetic factors, age, and intervention duration [54]. The RT studies included in this review involved participants aged between 20 and 72 years, with intervention durations ranging from 8 to 24 weeks. This variation in both age and the length of the interventions across the studies makes it difficult to draw clear conclusions about the effects of RT on lipid profiles. In addition, another key observation in the studies is that the intensity of the exercises appears to be more influential than the duration. For instance, 24 weeks of RT at an intensity ranging from 50% to 80% of 1 repetition maximum did not significantly impact the lipid profile. In contrast, 12 weeks of higher-intensity RT (65–85% of 1 repetition maximum) resulted in a more pronounced improvement in lipid profiles. The inconsistencies in these factors may contribute to variability in the outcomes, highlighting the importance of more consistent study designs to better understand the potential influence of RT on lipid metabolism.
Combined training (CT) programs seem to have a moderate, indirect effect on lipid profiles, particularly enhancing HDL cholesterol levels. These outcomes are attributed to both the direct impact of these interventions on lipid metabolism observed in three studies and their contribution to reducing body fat percentage, which may also play a role in improving lipid profiles. In these three studies, both resistance and aerobic exercises were performed simultaneously within a single session, with the intensity of the resistance exercises being notably high. Studies by Ho et al. [55] and Park et al. [25] reported significant reductions in body weight, BMI, and body fat percentage in individuals engaging in CT programs. This combined approach is particularly relevant for reducing abdominal fat, a critical factor due to its strong association with an increased risk of type 2 diabetes and cardiovascular disease. One potential mechanism underlying these beneficial effects may involve improvements in the leptin–catecholamine axis and reductions in plasma epinephrine levels, contributing to enhanced body composition and improved cardiovascular function [56]. It is important to note that the findings regarding the impact of this intervention on the lipid profile are based on evidence of relatively high quality (1a), allowing for a more reliable interpretation of the results.
Aerobic exercise has been shown to be associated with modest improvements in lipid factors, including a potential increase in HDL cholesterol levels, consistent with findings from several studies demonstrating improvements in lipid profiles, specifically an increase in HDL cholesterol [57]. Given the role of aerobic exercise in reducing body fat percentage, as reported in three studies, it may contribute to improvements in lipid profiles through this mechanism. Based on the studies reviewed in this paper, it appears that three sessions of aerobic exercise per week may not be sufficient to induce significant changes in lipid profile. In contrast, protocols with higher frequency (4 to 5 days per week) and progressive elements seem to be more effective. Additionally, it seems that a minimum session duration of 45 min may be necessary to achieve optimal effects on lipid metabolism. In this context, factors such as exercise frequency, progression, and session duration may play a more influential role in improving lipid profiles than the intensity or overall duration of the exercise protocol. However, it is important to acknowledge that the participants in these studies were primarily over 45 years of age, with considerable variation in their ages. This factor may influence the results, particularly when compared to younger populations. Furthermore, the overall quality of the included studies was rated at 2a level, which provides a moderate degree of confidence in the evidence. As a result, the findings should be viewed with caution, taking into account the possibility of biases and confounding variables.
4.4. Limitations
This study has several limitations. Firstly, the inclusion criteria were limited to English-language, peer-reviewed journals. Secondly, the literature search was restricted to four databases (PubMed, PEDro, ScienceDirect, and Google Scholar), which may have resulted in the exclusion of relevant studies. Incorporating additional databases (e.g., EMBASE and Scopus) and conducting comprehensive manual searches could enhance the comprehensiveness of the review. Thirdly, some cardiovascular risk factors, such as fibrinogen, were excluded from the analysis due to a limited number of studies investigating their relationship with exercise in this population. Fourthly, several studies did not report their results with sufficient clarity, and attempts to contact the corresponding authors for clarification were unsuccessful.
Future research also should investigate the effects of various exercise protocols on a broader range of cardiovascular risk factors, including fibrinogen and blood viscosity, in individuals with obesity. Studies should also consider more precise evaluations of key variables, examine different obesity classifications (e.g., based on body fat percentage), and focus on more homogeneous populations to minimize confounding factors.
5. Practical Recommendation
This review highlights the effectiveness of various exercise modalities in reducing cardiovascular risk factors in obese males. Results of this systematic review indicate that HIIT effectively reduces systolic blood pressure, but may not be suitable for individuals with cardiovascular issues. In addition, resistance training improves glycemic control and insulin sensitivity, especially with longer interventions, while aerobic exercise is essential for improving HDL cholesterol and body composition. Applying exercise programs based on evidence in clinical settings, incorporating structured exercise plans into workplace and community wellness programs, and customizing these plans for specific groups, such as older adults or individuals with severe obesity, can improve health outcomes and increase participation in physical activity. Policymakers should encourage physical activity programs and work with insurance companies to increase participation. Future research should focus on how to maintain long-term participation, combine interventions, assess cost-effectiveness, and include a wider range of populations to make the findings more applicable (Figure 2).
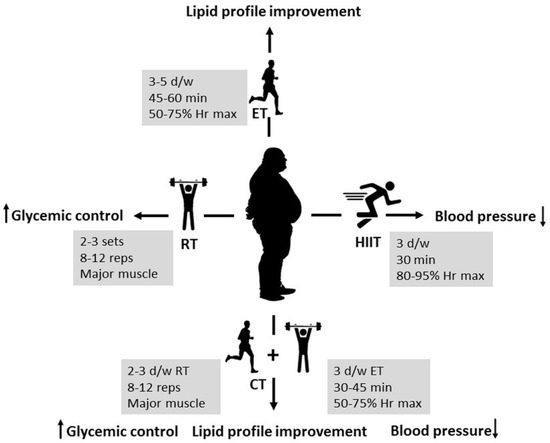
Figure 2.
Summary of the results (HIIT: high-intensity interval training; RT: resistance training; CT: combined training; ET: endurance training; W: week; d/w: days per week; Hr: heart rate, reps: repetitions).
6. Conclusions
This systematic review indicates that exercise training can positively influence cardiovascular health in males with obesity, though the effects depend on the exercise type and the specific cardiovascular risk factors being addressed. High-intensity interval training (HIIT) has shown some effectiveness in reducing blood pressure, with certain studies reporting up to a 10 mmHg reduction in systolic blood pressure after 12 weeks. However, the evidence supporting HIIT as the most effective approach for blood pressure reduction is not consistent across all studies. Aerobic exercise may require longer or more intense programs to produce substantial improvements in lipid profiles, with some studies showing modest increases, particularly in HDL cholesterol levels. Resistance training (RT) has shown potential in improving glycemic control, though the findings are inconclusive. Factors such as age, gender, race, baseline cardiovascular risk, and the specifics of the RT regimen may influence the effectiveness of RT in improving glucose metabolism and these aspects require further investigation. Combined training (CT), which includes both aerobic and resistance exercises, may have some potential for improving cardiovascular risk factors, such as lipid profiles, glucose levels, and insulin sensitivity. However, the evidence remains mixed; for example, only two out of five studies on CT reported significant improvements in HDL levels. Despite these inconsistencies, combined training remains a practical approach, with consistent participation (approximately 60 min, three times per week) potentially yielding cardiovascular health benefits. Future research should focus on more consistent age ranges, have higher-quality designs, and include both sexes to better understand the effects across genders. Additionally, long-term studies exploring the impact of various exercise modalities, considering baseline fitness and pre-existing health conditions, are needed.
Author Contributions
A.P. conducted the scientific work and wrote the manuscript; S.S. was responsible for supervision, as well as reviewing and editing the manuscript. A.S. discussed the results and contributed to the final manuscript. R.S. helped supervise the project and approved the final version. All authors have read and agreed to the published version of the manuscript.
Funding
Start-up grants by Research Committee of Hong Kong Baptist University “RC-STARTUP/22-23/22”.
Data Availability Statement
The data presented in this study are available within this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef] [PubMed]
- WHO. Overweight and Obesity; WHO: Geneva, Switzerland, 2023. [Google Scholar]
- World Obesity Federation. World Obesity Atlas 2023; World Obesity Federation: London, UK, 2022. [Google Scholar]
- Long, D.A.; Reed, R.; Lehman, G. The cost of lifestyle health risks: Obesity. J. Occup. Environ. Med. 2006, 48, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Bays, H.E.; Taub, P.R.; Epstein, E.; Michos, E.D.; Ferraro, R.A.; Bailey, A.L.; Kelli, H.M.; Ferdinand, K.C.; Echols, M.R.; Weintraub, H. Ten things to know about ten cardiovascular disease risk factors. Am. J. Prev. Cardiol. 2021, 5, 100149. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A. Obesity and cardiovascular risk. Growth Horm. IGF Res. 2003, 13, S10–S17. [Google Scholar] [CrossRef] [PubMed]
- Longo, M.; Zatterale, F.; Naderi, J.; Parrillo, L.; Formisano, P.; Raciti, G.A.; Beguinot, F.; Miele, C. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int. J. Mol. Sci. 2019, 20, 2358. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.E. Pathophysiology of obesity hypertension. Curr. Hypertens. Rep. 2000, 2, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Elagizi, A.; Kachur, S.; Carbone, S.; Lavie, C.J.; Blair, S.N. A review of obesity, physical activity, and cardiovascular disease. Curr. Obes. Rep. 2020, 9, 571–581. [Google Scholar] [CrossRef]
- Petrick, H.L.; King, T.J.; Pignanelli, C.; Vanderlinde, T.E.; Cohen, J.N.; Holloway, G.P.; Burr, J.F. Endurance and Sprint Training Improve Glycemia and V˙ O2peak but only Frequent Endurance Benefits Blood Pressure and Lipidemia. Med. Sci. Sports Exerc. 2021, 53, 1194–1205. [Google Scholar] [CrossRef] [PubMed]
- Verheggen, R.; Maessen, M.; Green, D.J.; Hermus, A.; Hopman, M.; Thijssen, D. A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: Distinct effects on body weight and visceral adipose tissue. Obes. Rev. 2016, 17, 664–690. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Croymans, D.; Krell, S.; Oh, C.; Katiraie, M.; Lam, C.; Harris, R.A.; Roberts, C. Effects of resistance training on central blood pressure in obese young men. J. Hum. Hypertens. 2014, 28, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Clark, T.; Morey, R.; Jones, M.D.; Marcos, L.; Ristov, M.; Ram, A.; Hakansson, S.; Franklin, A.; McCarthy, C.; De Carli, L. High-intensity interval training for reducing blood pressure: A randomized trial vs. moderate-intensity continuous training in males with overweight or obesity. Hypertens. Res. 2020, 43, 396–403. [Google Scholar] [CrossRef]
- Costa, E.C.; Hay, J.L.; Kehler, D.S.; Boreskie, K.F.; Arora, R.C.; Umpierre, D.; Szwajcer, A.; Duhamel, T.A. Effects of high-intensity interval training versus moderate-intensity continuous training on blood pressure in adults with pre-to established hypertension: A systematic review and meta-analysis of randomized trials. Sports Med. 2018, 48, 2127–2142. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.P.; Duarte-Mendes, P.; Teixeira, A.M.; Silva, F.M. Effects of combined training on metabolic profile, lung function, stress and quality of life in sedentary adults: A study protocol for a randomized controlled trial. PLoS ONE 2022, 17, e0263455. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Elkins, M.R.; Moseley, A.M.; Sherrington, C.; Herbert, R.D.; Maher, C.G. Growth in the Physiotherapy Evidence Database (PEDro) and use of the PEDro scale. Br. J. Sports Med. 2013, 47, 188–189. [Google Scholar] [CrossRef] [PubMed]
- Haynes, R.B.; Sackett, D.L.; Richardson, W.S.; Rosenberg, W.; Langley, G.R. Evidence-based medicine: How to practice & teach EBM. Can. Med. Assoc. J. 1997, 157, 788. [Google Scholar]
- Cheema, B.S.; Davies, T.B.; Stewart, M.; Papalia, S.; Atlantis, E. The feasibility and effectiveness of high-intensity boxing training versus moderate-intensity brisk walking in adults with abdominal obesity: A pilot study. BMC Sports Sci. Med. Rehabil. 2015, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Chin, E.C.; Yu, A.P.; Lai, C.W.; Fong, D.Y.; Chan, D.K.; Wong, S.H.; Sun, F.; Ngai, H.H.; Yung, P.S.; Siu, P.M. Low-frequency HIIT improves body composition and aerobic capacity in overweight men. Med. Sci. Sports Exerc. 2020, 52, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Amaro-Gahete, F.J.; Ponce-González, J.G.; Corral-Pérez, J.; Velázquez-Díaz, D.; Lavie, C.J.; Jiménez-Pavón, D. Effect of a 12-week concurrent training intervention on cardiometabolic health in obese men: A pilot study. Front. Physiol. 2021, 12, 630831. [Google Scholar] [CrossRef] [PubMed]
- Gerosa-Neto, J.; Panissa, V.L.G.; Monteiro, P.A.; Inoue, D.S.; Ribeiro, J.P.J.; Figueiredo, C.; Zagatto, A.M.; Little, J.P.; Lira, F.S. High-or moderate-intensity training promotes change in cardiorespiratory fitness, but not visceral fat, in obese men: A randomised trial of equal energy expenditure exercise. Respir. Physiol. Neurobiol. 2019, 266, 150–155. [Google Scholar] [CrossRef]
- Park, W.; Jung, W.-S.; Hong, K.; Kim, Y.-Y.; Kim, S.-W.; Park, H.-Y. Effects of moderate combined resistance-and aerobic-exercise for 12 weeks on body composition, cardiometabolic risk factors, blood pressure, arterial stiffness, and physical functions, among obese older men: A pilot study. Int. J. Environ. Res. Public Health 2020, 17, 7233. [Google Scholar] [CrossRef] [PubMed]
- Reljic, D.; Frenk, F.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Low-volume high-intensity interval training improves cardiometabolic health, work ability and well-being in severely obese individuals: A randomized-controlled trial sub-study. J. Transl. Med. 2020, 18, 419. [Google Scholar] [CrossRef]
- Ahmadizad, S.; Ghorbani, S.; Ghasemikaram, M.; Bahmanzadeh, M. Effects of short-term nonperiodized, linear periodized and daily undulating periodized resistance training on plasma adiponectin, leptin and insulin resistance. Clin. Biochem. 2014, 47, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Bonfante, I.L.P.; Chacon-Mikahil, M.P.T.; Brunelli, D.T.; Gaspari, A.F.; Duft, R.G.; Lopes, W.A.; Bonganha, V.; Libardi, C.A.; Cavaglieri, C.R. Combined training, FNDC5/irisin levels and metabolic markers in obese men: A randomised controlled trial. Eur. J. Sport Sci. 2017, 17, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Siu, P.M.; Yu, A.P.; Chin, E.C.; Yu, D.S.; Hui, S.S.; Woo, J.; Fong, D.Y.; Wei, G.X.; Irwin, M.R. Effects of Tai Chi or conventional exercise on central obesity in middle-aged and older adults: A three-group randomized controlled trial. Ann. Intern. Med. 2021, 174, 1050–1057. [Google Scholar] [CrossRef] [PubMed]
- Duft, R.G.; Castro, A.; Bonfante, I.L.; Brunelli, D.T.; Chacon-Mikahil, M.P.; Cavaglieri, C.u.R. Metabolomics approach in the investigation of metabolic changes in obese men after 24 weeks of combined training. J. Proteome Res. 2017, 16, 2151–2159. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Nam, J.S.; Yeo, D.W.; Kim, K.R.; Suh, S.H.; Ahn, C.W. The effects of aerobic exercise training on serum osteocalcin, adipocytokines and insulin resistance on obese young males. Clin. Endocrinol. 2015, 82, 686–694. [Google Scholar] [CrossRef]
- Kim, S.-W.; Jung, W.-S.; Park, W.; Park, H.-Y. Twelve weeks of combined resistance and aerobic exercise improves cardiometabolic biomarkers and enhances red blood cell hemorheological function in obese older men: A randomized controlled trial. Int. J. Environ. Res. Public Health 2019, 16, 5020. [Google Scholar] [CrossRef]
- Kolahdouzi, S.; Baghadam, M.; Kani-Golzar, F.A.; Saeidi, A.; Jabbour, G.; Ayadi, A.; De Sousa, M.; Zouita, A.; Abderrahmane, A.B.; Zouhal, H. Progressive circuit resistance training improves inflammatory biomarkers and insulin resistance in obese men. Physiol. Behav. 2019, 205, 15–21. [Google Scholar] [CrossRef]
- Nikseresht, M.; Agha-Alinejad, H.; Azarbayjani, M.A.; Ebrahim, K. Effects of nonlinear resistance and aerobic interval training on cytokines and insulin resistance in sedentary men who are obese. J. Strength Cond. Res. 2014, 28, 2560–2568. [Google Scholar] [CrossRef] [PubMed]
- Poon, E.T.-C.; Siu, P.M.-F.; Wongpipit, W.; Gibala, M.; Wong, S.H.-S. Alternating high-intensity interval training and continuous training is efficacious in improving cardiometabolic health in obese middle-aged men. J. Exerc. Sci. Fit. 2022, 20, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Safarzade, A.; Alizadeh, H.; Bastani, Z. The effects of circuit resistance training on plasma progranulin level, insulin resistance and body composition in obese men. Horm. Mol. Biol. Clin. Investig. 2020, 41, 20190050. [Google Scholar] [CrossRef] [PubMed]
- Smith-Ryan, A.E.; Melvin, M.N.; Wingfield, H.L. High-intensity interval training: Modulating interval duration in overweight/obese men. Physician Sportsmed. 2015, 43, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Moraleda, B.R.; Morencos, E.; Peinado, A.B.; Bermejo, L.; Candela, C.G.; Benito, P.J.; PRONAF Study Group. Can the exercise mode determine lipid profile improvements in obese patients? Nutr. Hosp. 2013, 28, 607–617. [Google Scholar]
- Saremi, A.; Asghari, M.; Ghorbani, A. Effects of aerobic training on serum omentin-1 and cardiometabolic risk factors in overweight and obese men. J. Sports Sci. 2010, 28, 993–998. [Google Scholar] [CrossRef]
- Varady, K.A.; Bhutani, S.; Klempel, M.C.; Kroeger, C.M. Comparison of effects of diet versus exercise weight loss regimens on LDL and HDL particle size in obese adults. Lipids Health Dis. 2011, 10, 119. [Google Scholar] [CrossRef] [PubMed]
- Vincent, H.K.; Bourguignon, C.; Vincent, K.R. Resistance training lowers exercise-induced oxidative stress and homocysteine levels in overweight and obese older adults. Obesity 2006, 14, 1921–1930. [Google Scholar] [CrossRef] [PubMed]
- Saeidi, A.; Nouri-Habashi, A.; Razi, O.; Ataeinosrat, A.; Rahmani, H.; Mollabashi, S.S.; Bagherzadeh-Rahmani, B.; Aghdam, S.M.; Khalajzadeh, L.; Al Kiyumi, M.H. Astaxanthin Supplemented with High-Intensity Functional Training Decreases Adipokines Levels and Cardiovascular Risk Factors in Men with Obesity. Nutrients 2023, 15, 286. [Google Scholar] [CrossRef]
- Hematinezhad Touli, M.; Elmieh, A.; Hosseinpour, A. The effect of six-week aerobic exercise combined with green tea consumption on PON1 and VO2max increase and apelin, blood pressure, and blood lipids reduction in young obese men. Arch. Razi Inst. 2022, 77, 2115–2123. [Google Scholar] [PubMed]
- Rezaeimanesh, D. The response of serum adipolin levels and insulin resistance index to high-intensity interval training in overweight men. Rev. Latinoam. De Hipertens. 2023, 18, 163–169. [Google Scholar]
- Grace, F.; Herbert, P.; Elliott, A.D.; Richards, J.; Beaumont, A.; Sculthorpe, N.F. High intensity interval training (HIIT) improves resting blood pressure, metabolic (MET) capacity and heart rate reserve without compromising cardiac function in sedentary aging men. Exp. Gerontol. 2018, 109, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Lemes, Í.R.; Ferreira, P.H.; Linares, S.N.; Machado, A.F.; Pastre, C.M.; Netto, J. Resistance training reduces systolic blood pressure in metabolic syndrome: A systematic review and meta-analysis of randomised controlled trials. Br. J. Sports Med. 2016, 50, 1438–1442. [Google Scholar] [CrossRef] [PubMed]
- Montero, D.; Roberts, C.K.; Vinet, A. Effect of aerobic exercise training on arterial stiffness in obese populations: A systematic review and meta-analysis. Sports Med. 2014, 44, 833–843. [Google Scholar] [CrossRef] [PubMed]
- Wewege, M.A.; Thom, J.M.; Rye, K.-A.; Parmenter, B.J. Aerobic, resistance or combined training: A systematic review and meta-analysis of exercise to reduce cardiovascular risk in adults with metabolic syndrome. Atherosclerosis 2018, 274, 162–171. [Google Scholar] [CrossRef]
- Hayes, L.D.; Herbert, P.; Sculthorpe, N.; Grace, F. High intensity interval training (HIIT) produces small improvements in fasting glucose, insulin, and insulin resistance in sedentary older men but not masters athletes. Exp. Gerontol. 2020, 140, 111074. [Google Scholar] [CrossRef] [PubMed]
- Johns, D.J.; Hartmann-Boyce, J.; Jebb, S.A.; Aveyard, P.; Group, B.W.M.R. Diet or exercise interventions vs combined behavioral weight management programs: A systematic review and meta-analysis of direct comparisons. J. Acad. Nutr. Diet. 2014, 114, 1557–1568. [Google Scholar] [CrossRef] [PubMed]
- Yaspelkis III, B.B. Resistance training improves insulin signaling and action in skeletal muscle. Exerc. Sport Sci. Rev. 2006, 34, 42–46. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Batacan, R.B.; Duncan, M.J.; Dalbo, V.J.; Tucker, P.S.; Fenning, A.S. Effects of high-intensity interval training on cardiometabolic health: A systematic review and meta-analysis of intervention studies. Br. J. Sports Med. 2017, 51, 494–503. [Google Scholar] [CrossRef]
- Richard, A.J.; White, U.; Elks, C.M.; Stephens, J.M. Adipose tissue: Physiology to metabolic dysfunction. In Endotext [Internet]; MDText.com, Inc.: South Dartmouth, MA, USA, 2020. [Google Scholar]
- Westcott, W.L. Resistance training is medicine: Effects of strength training on health. Curr. Sports Med. Rep. 2012, 11, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.S.; Dhaliwal, S.S.; Hills, A.P.; Pal, S. The effect of 12 weeks of aerobic, resistance or combination exercise training on cardiovascular risk factors in the overweight and obese in a randomized trial. BMC Public Health 2012, 12, 704. [Google Scholar] [CrossRef] [PubMed]
- Lucotti, P.; Monti, L.D.; Setola, E.; Galluccio, E.; Gatti, R.; Bosi, E.; Piatti, P. Aerobic and resistance training effects compared to aerobic training alone in obese type 2 diabetic patients on diet treatment. Diabetes Res. Clin. Pract. 2011, 94, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.; Alkhawam, H.; Madanieh, R.; Shah, N.; Kosmas, C.E.; Vittorio, T.J. Aerobic vs. anaerobic exercise training effects on the cardiovascular system. World J. Cardiol. 2017, 9, 134. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).