Contemporary Management of Popliteal Artery Aneurysms: A Comprehensive Review
Abstract
1. Introduction
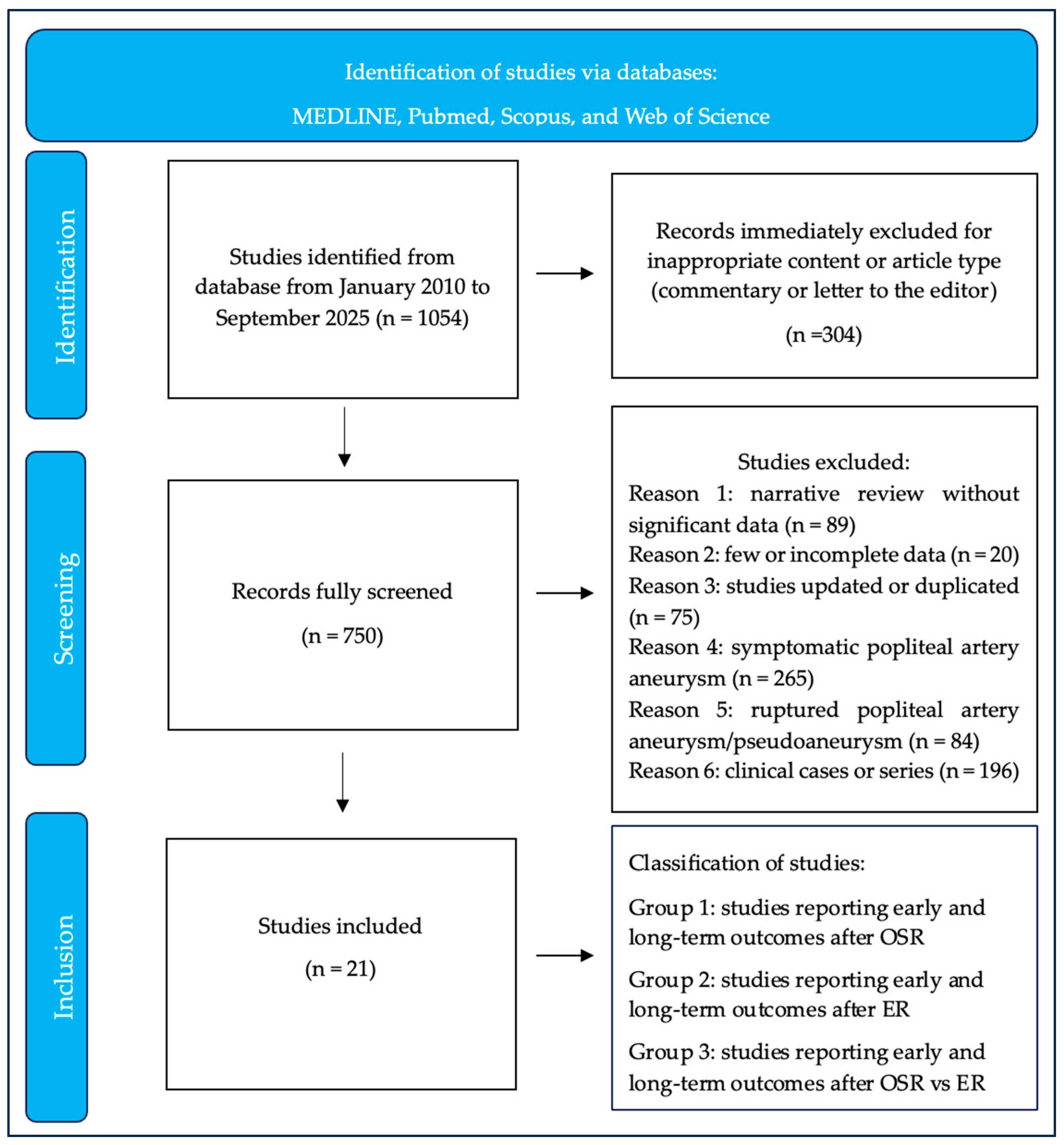
2. Materials and Methods
“Popliteal artery aneurysm AND endovascular treatment” (textword).
“Popliteal artery aneurysm AND open surgery” (textword).
“Popliteal artery aneurysm AND (endovascular treatment OR endovascular repair)” (textword).
“Popliteal artery aneurysm AND (open surgery OR open surgical repair)” (textword).
- Reason 1: narrative review without significant data
- Reason 2: studies with few or incomplete data
- Reason 3: studies updated or duplicated
- Reason 4: symptomatic PAAs (for ALI)
- Reason 5: ruptured PAAs
- Reason 6: clinical cases or series
- Group 1: studies reporting early and/or long-term outcomes after OSR only;
- Group 2: studies reporting early and/or long-term outcomes after EPAR only;
- Group 3: studies reporting and comparing early and/or long-term outcomes after both OPAR and EPAR.
2.1. Definitions
2.2. Outcomes Measures
2.3. Statistical Analysis
3. Results
3.1. Open Popliteal Aneurysm Repair (OPAR)
3.2. Endovascular Popliteal Aneurysm Repair (EPAR)
3.3. Open vs. Endovascular Popliteal Aneurysm Repair (OPAR vs. EPAR)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tuveson, V.; Löfdahl, H.E.; Hultgren, R. Patients with abdominal aortic aneurysm have a high prevalence of popliteal artery aneurysms. Vasc. Med. 2016, 21, 369–375. [Google Scholar] [CrossRef]
- Cecenarro, R.R.; Allende, J.N.; Barreras Molinelli, L.; Antueno, F.J.; Gramática, L. Aneurismas de la Arteria Poplitea: Revisión bibliográfica y presentación de un caso [Popliteal Artery Aneurysms: Literature Review and presentation of case]. Rev. Fac. Cien. Med. Univ. Nac. Cordoba 2018, 75, 41–45. [Google Scholar] [CrossRef]
- Joshi, D.; James, R.L.; Jones, L. Endovascular versus open repair of asymptomatic popliteal artery aneurysm. Cochrane Database Syst. Rev. 2014, CD010149. [Google Scholar] [CrossRef]
- Pomatto, S.; Faggioli, G.; Pini, R.; Ficarelli, I.; Pini, A.; Angherà, C.; Rocchi, C.; Caputo, S.; Vacirca, A.; Ruotolo, C.; et al. Limb salvage and survival after urgent surgical treatment of popliteal artery aneurysm. World J. Emerg. Surg. 2023, 18, 49. [Google Scholar] [CrossRef]
- Farber, A.; Angle, N.; Avgerinos, E.; Dubois, L.; Eslami, M.; Geraghty, P.; Haurani, M.; Jim, J.; Ketteler, E.; Pulli, R.; et al. The Society for Vascular Surgery clinical practice guidelines on popliteal artery aneurysms. J. Vasc. Surg. 2022, 75 (Suppl. S1), 109S–120S. [Google Scholar] [CrossRef]
- Kim, T.I.; Sumpio, B.E. Management of Asymptomatic Popliteal Artery Aneurysms. Int. J. Angiol. 2019, 28, 5–10. [Google Scholar] [CrossRef]
- Serrano Hernando, F.J.; Martínez López, I.; Hernández Mateo, M.M.; Hernando Rydings, M.; Sánchez Hervás, L.; Rial Horcajo, R.; Moñux Ducajú, G.; Martín Conejero, A. Comparison of popliteal artery aneurysm therapies. J. Vasc. Surg. 2015, 61, 655–661. [Google Scholar] [CrossRef]
- Eslami, M.H.; Rybin, D.; Doros, G.; Farber, A. Open repair of asymptomatic popliteal artery aneurysm is associated with better outcomes than endovascular repair. J. Vasc. Surg. 2015, 61, 663–669. [Google Scholar] [CrossRef]
- Leake, A.E.; Segal, M.A.; Chaer, R.A.; Eslami, M.H.; Al-Khoury, G.; Makaroun, M.S.; Avgerinos, E.D. Meta-analysis of open and endovascular repair of popliteal artery aneurysms. J. Vasc. Surg. 2017, 65, 246–256.e2. [Google Scholar] [CrossRef]
- Shah, N.G.; Rokosh, R.S.; Garg, K.; Safran, B.; Rockman, C.B.; Maldonado, T.S.; Sadek, M.; Lamparello, P.; Jacobowitz, G.R.; Barfield, M.E.; et al. Endovascular treatment of popliteal artery aneurysms has comparable long-term outcomes to open repair with shorter lengths of stay. J. Vasc. Surg. 2021, 74, 1565–1572.e1. [Google Scholar] [CrossRef]
- Troisi, N.; Bertagna, G.; Saratzis, A.; Zayed, H.; Torsello, G.B.; Dorigo, W.; Antonello, M.; Prouse, G.; Bonardelli, S.; Berchiolli, R. Elective Surgical Repair of Popliteal Artery Aneurysms with Posterior Approach vs. Endovascular Exclusion: Early and Long Term Outcomes of Multicentre PARADE Study. Eur. J. Vasc. Endovasc. Surg. 2025, 69, 110–117. [Google Scholar] [CrossRef]
- Troisi, N.; Bertagna, G.; Berchiolli, R.; PARADE Study Collaborative Group. Re: Enhancing the Reliability of Popliteal Artery Aneurysm Treatment Outcomes: A Critical Review of the PARADE Study. Eur. J. Vasc. Endovasc. Surg. 2025, 69, 342. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Koelemay, M.J.; Vermeulen, H. Quick Guide to Systematic Reviews and Meta-analysis. Eur. J. Vasc. Endovasc. Surg. 2016, 51, 309. [Google Scholar] [CrossRef]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef]
- Dorigo, W.; Pulli, R.; Alessi Innocenti, A.; Azas, L.; Fargion, A.; Chiti, E.; Matticari, S.; Pratesi, C. A 33-year experience with surgical management of popliteal artery aneurysms. J. Vasc. Surg. 2015, 62, 1176–1182. [Google Scholar] [CrossRef]
- Chang, H.; Veith, F.J.; Rockman, C.B.; Siracuse, J.J.; Jacobowitz, G.R.; Cayne, N.S.; Patel, V.I.; Garg, K. Comparison of Outcomes for Open Popliteal Artery Aneurysm Repair Using Vein and Prosthetic Conduits. Ann. Vasc. Surg. 2021, 75, 69–78. [Google Scholar] [CrossRef]
- Troisi, N.; Bertagna, G.; Andreini, M.; Scarati, V.; Berchiolli, R.; PARADE Study Collaborative Group. Great saphenous vein versus expanded polytetrafluoroethylene graft in patients undergoing elective treatment of popliteal artery aneurysm with a posterior approach. J. Vasc. Surg. 2025, 82, 845–853.e2. [Google Scholar] [CrossRef]
- Kim, Y.; Loanzon, R.S.; Southerland, K.W.; Long, C.A.; Williams, Z.F.; Mohapatra, A. Prosthetic Conduit Use Does Not Adversely Impact Outcomes after Open Repair of Popliteal Artery Aneurysms. Ann. Vasc. Surg. 2024, 98, 124–130. [Google Scholar] [CrossRef]
- Van Leeuwen, G.; Baggel, S.; Tielliu, I.F.J.; Schuurmann, R.C.L.; van Walraven, L.A.; de Vries, J.P.M. Long Term Follow Up after Endovascular Popliteal Artery Aneurysm Repair: A Two Centre, Retrospective Cohort Study (1998–2023). Eur. J. Vasc. Endovasc. Surg. 2025, 70, 483–489. [Google Scholar] [CrossRef]
- Guzzardi, G.; Natrella, M.; Del Sette, B.; Petullà, M.; Fanelli, G.; Porta, C.; Carriero, A.; Laganà, D. Endovascular repair of popliteal artery aneurysms: An Italian multicenter study. Radiol. Med. 2019, 124, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Speziale, F.; Sirignano, P.; Menna, D.; Capoccia, L.; Mansour, W.; Serrao, E.; Ronchey, S.; Alberti, V.; Esposito, A.; Mangialardi, N. Ten years’ experience in endovascular repair of popliteal artery aneurysm using the Viabahn endoprosthesis: A report from two Italian vascular centers. Ann. Vasc. Surg. 2015, 29, 941–949. [Google Scholar] [CrossRef]
- Troisi, N.; Bertagna, G.; Lepidi, S.; Berchiolli, R.; Badalamenti, G.; D’Oria, M.; PARADE Study Collaborative Group. Late outcomes of Viabahn self-expandable covered stent for the elective treatment of popliteal artery aneurysms. J. Vasc. Surg. 2025, 82, 1658–1668. [Google Scholar] [CrossRef]
- Golchehr, B.; Tielliu, I.F.; Verhoeven, E.L.; Möllenhoff, C.; Antonello, M.; Zeebregts, C.J.; Reijnen, M.M. Clinical Outcome of Isolated Popliteal Artery Aneurysms Treated with a Heparin-bonded Stent Graft. Eur. J. Vasc. Endovasc. Surg. 2016, 52, 99–104. [Google Scholar] [CrossRef]
- Midy, D.; Berard, X.; Ferdani, M.; Alric, P.; Brizzi, V.; Ducasse, E.; Sassoust, G.; AURC French University Association for Vascular Surgery. A retrospective multicenter study of endovascular treatment of popliteal artery aneurysm. J. Vasc. Surg. 2010, 51, 850–856. [Google Scholar] [CrossRef]
- Piazza, M.; Menegolo, M.; Ferrari, A.; Bonvini, S.; Ricotta, J.J.; Frigatti, P.; Grego, F.; Antonello, M. Long-term outcomes and sac volume shrinkage after endovascular popliteal artery aneurysm repair. Eur. J. Vasc. Endovasc. Surg. 2014, 48, 161–168. [Google Scholar] [CrossRef][Green Version]
- Cervin, A.; Tjärnström, J.; Ravn, H.; Acosta, S.; Hultgren, R.; Welander, M.; Björck, M. Treatment of Popliteal Aneurysm by Open and Endovascular Surgery: A Contemporary Study of 592 Procedures in Sweden. Eur. J. Vasc. Endovasc. Surg. 2015, 50, 342–350. [Google Scholar] [CrossRef]
- Galiñanes, E.L.; Dombrovskiy, V.Y.; Graham, A.M.; Vogel, T.R. Endovascular versus open repair of popliteal artery aneurysms: Outcomes in the US Medicare population. Vasc. Endovasc. Surg. 2013, 47, 267–273. [Google Scholar] [CrossRef]
- Del Tatto, B.; Lejay, A.; Meteyer, V.; Roussin, M.; Georg, Y.; Thaveau, F.; Geny, B.; Chakfe, N. Open and Endovascular Repair of Popliteal Artery Aneurysms. Ann. Vasc. Surg. 2018, 50, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Ripepi, M.; Gibello, L.; Ferrero, E.; Scevola, M.; Manzo, P.; Varetto, G.; Quaglino, S.; Chiera, L.; Boero, M.; Ferri, M.; et al. Open Versus Endovascular Repair of Patent Popliteal Artery Aneurysms in an Elective Setting: A Multicenter Retrospective Study with Long-Term Follow-Up. Ann. Vasc. Surg. 2025, 117, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Dorigo, W.; Fargion, A.; Masciello, F.; Piffaretti, G.; Pratesi, G.; Giacomelli, E.; Pratesi, C. A Matched Case-Control Study on Open and Endovascular Treatment of Popliteal Artery Aneurysms. Scand. J. Surg. 2018, 107, 236–243. [Google Scholar] [CrossRef]
- Leake, A.E.; Avgerinos, E.D.; Chaer, R.A.; Singh, M.J.; Makaroun, M.S.; Marone, L.K. Contemporary outcomes of open and endovascular popliteal artery aneurysm repair. J. Vasc. Surg. 2016, 63, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Pulli, R.; Dorigo, W.; Fargion, A.; Pratesi, G.; Innocenti, A.A.; Angiletta, D.; Pratesi, C. Comparison of early and midterm results of open and endovascular treatment of popliteal artery aneurysms. Ann. Vasc. Surg. 2012, 26, 809–818. [Google Scholar] [CrossRef] [PubMed]
- Satam, K.; Brahmandam, A.; Zheng, X.; Mao, J.; Goodney, P.; Ochoa Chaar, C.I. Long-term outcomes of elective endovascular vs open repair of popliteal artery aneurysms in the VISION database. J. Vasc. Surg. 2025, 81, 672–681.e2. [Google Scholar] [CrossRef] [PubMed]
- Jung, G.; Leinweber, M.E.; Karl, T.; Geisbüsch, P.; Balzer, K.; Schmandra, T.; Dietrich, T.; Derwich, W.; Gray, D.; Schmitz-Rixen, T. Real-world data of popliteal artery aneurysm treatment: Analysis of the POPART registry. J. Vasc. Surg. 2022, 75, 1707–1717.e2. [Google Scholar] [CrossRef]
- Troisi, N.; Bertagna, G.; Berchiolli, R.; RIVAS Collaborative Study Group. RIvaroxaban and VAscular Surgery (RIVAS): Insights from a multicenter, worldwide web-based survey. Int. Angiol. 2024, 43, 306–308. [Google Scholar] [CrossRef]
| Study | N° of Patients (Limbs Treated) | Early and Mid-Term Outcomes | % | Long-Term Outcomes | % | ||||
|---|---|---|---|---|---|---|---|---|---|
| Dorigo, W. et al. [16] J. Vasc. Surg. 2015 | 196 (234) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 1% - 7.7% | Estimated 13-year: -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 50.8% 45% 55.1% - 68% 62% | ||||
| Chang, H. et al. [17] Ann. Vasc. Surg. 2021 | 1065 (1146) | -technical success -mortality -MACEs -graft occlusion(s) | 100% - - - | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | GSV - - 87% - 96% - | PC - - 91% - 95% - | p - - NS - NS - | ||
| Troisi, N. et al. [18] J. Vasc. Surg. 2025 | 525 (525) | -technical success -mortality -MACEs -graft occlusion(s) | GSV 100% 0.4% 1.2% 2.8% | ePTFE 100% 0% 1.1% 0.8% | p - 0.480 0.601 0.081 | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | GSV 84.7% 99.1% 89.5% - 94.9% 92.8% | ePTFE 86.1% 99.6% 76.2% - 89.4% 80.6% | p 0.097 0.567 0.007 - 0.068 0.011 |
| Kim, Y. et al. [19] Ann. Vasc. Surg. 2024 | 101 (101) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 0 - - | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | GSV 98% 80.8% - - - - | PC 98% 76.7% - - - - | p - 0.47 - - - - | ||
| Study | N° of Patients (Limbs Treated) | Early and Mid-Term Outcomes | % | Long-Term Outcomes | % |
|---|---|---|---|---|---|
| Guzzardi, G. et al. [21] Radiol. Med. 2019 | 48 (48) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 0 - 10.4% | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 100% 100% 70.8% - 89.6% 75% |
| Speziale, F. et al. [22] Ann. Vasc. Surg. 2015 | 53 (53) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 0 3.8% 0 | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 96.2% 100% 73.2% - 92.4% 81.1% |
| van Leeuwen, GL. et al. [20] Eur. J. Vasc. Endovasc. Surg. 2025 | 105 (123) | -technical success -mortality -MACEs -graft occlusion(s) | 98.4% 0 - 3.3% | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 77% 98.4% 54% 58% 73% 69% |
| Troisi, N. et al. [23] J. Vasc. Surg. 2025 | 326 (326) | -technical success -mortality -MACEs -graft occlusion(s) | 99.4% 0.6% 1.2% 3.7% | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 82.7% 98.2% 65.8% 86.5% 84.9% 70.5% |
| Golchehr, B. et al. [24] Eur. J. Vasc. Endovasc. Surg. 2016 | 70 (72) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 0 0 0 | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 90% 100% 69% 74% 76% 82% |
| Midy, D. et al. [25] J. Vasc. Surg. 2010 | 50 (57) | -technical success -mortality -MACEs -graft occlusion(s) | 98.2% 0 - 16% | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 91% 96.5% 87.5% - 83% 96.2% |
| Piazza, M. et al. [26] Eur. J. Vasc. Endovasc. Surg. 2014 | 42 (46) | -technical success -mortality -MACEs -graft occlusion(s) | 98% 0 - 5% | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 84% 98% 76% - 82% 63% |
| Study | N° of Patients (Treated Limbs) | Early and Mid-Term Outcomes | OPAR | EPAR | p | Long-Term Outcomes | OPAR | EPAR | p |
|---|---|---|---|---|---|---|---|---|---|
| Troisi, N. et al. [11] Eur. J. Vasc. Endovasc. Surg. 2025 | 605 (605) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 0.7% 1.6% 2.3% | 98.8% 0.6% 0.6% 4.2% | - 0.18 0.31 0.15 | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 84.4% 99% 79.8% - 90.7% 82.2% | 79.4% 98.% 63.8% - 85.2% 68.4% | 0.050 0.73 0.012 - 0.25 0.021 |
| Galiñanes, EL. et al. [28] Vasc. Endovascular. Surg. 2013 | 2962 (2962) | -technical success -mortality -MACEs -graft occlusion(s) | - - 2.3% - | - - 0.9% - | - - 0.04 - | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | - - - - - 95.4% | - - - - - 88.2% | - - - - - 0.001 |
| Del Tatto, B. et al. [29] Ann. Vasc. Surg. 2018 | 126 (153) | -technical success -mortality -MACEs -graft occlusion(s) | - - - 4.9% | - - - 12% | - - - NS | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 97.7% 89.5% 77.8% 85% 92.8% - | 92.4% 97.7% 44.4% 69.3% 84.3% - | - - 0.02 - 0.048 - |
| Ripepi, M. et al. [30] Ann. Vasc. Surg. 2025 | 120 (143) | -technical success -mortality -MACEs -graft occlusion(s) | - 0 - 1.4% | - 0 - 5.5% | - NS - 0.2 | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 94.3% 100% 81% - 90.6% 95.7% | 91.8% 99% 64.1% - 88.4% 70.9% | 0.04 0.5 0.01 - 0.3 0.02 |
| Cervin, A. et al. [27] Eur. J. Vasc. Endovasc. Surg. 2015 | 499 (592) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 0 - - | 100% 0 - - | NA NA - - | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 98.8% 97.8% 89% - 93.5% - | 94.6% 92.3% 67.4% - 83.7% - | 0.045 0.048 <0.001 - 0.026 - |
| Eslami, MH. et al. [8] J. Vasc. Surg. 2015 | 390 (390) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 0 0.6% - | 100% 0 1.8% - | NA NA NS - | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 95.5% 91.8% 95.9% - 91.1% - | 98.2% 77.2% 92.3% - 76.6% - | 0.32 0.008 0.368 - 0.006 - |
| Dorigo, W. et al. [31] Scand J. Surg. 2018 | 309 (309) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 0 7% 1.7% | 100% 1.7% - 3.5% | NA 0.3 - 0.4 | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 89.5% 86.4% 64% - 71% 76% | 94% 94% 72% - 74% 65.5% | 0.4 0.3 0.8 - 0.9 0.2 |
| Leake, AE. et al. [32] J. Vasc. Surg. 2016 | 156 (186) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 1.6% - 1.8% | 100% 0 - 0 | NA 0.67 - NA | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 96% 96.8% 79.5% 83.7% 85% 96.8% | 96% 100% 73.2% 76.3% 83% 91.1% | NS 0.23 0.630 0.495 0.963 0.28 |
| Pulli, R. et al. [33] Ann. Vasc. Surg. 2012 | 59 (64) | -technical success -mortality -MACEs -graft occlusion(s) | - 4.5% - 4.5% | 100% 4.7% - 14.2% | - 0.9 - 0.2 | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 96.5% 92.7% 78.1% - 81.6% 79% | 96.5% 95% 59.4% - 78.4% 61.5% | - 0.7 0.1 - 0.9 0.2 |
| Satam, K. et al. [34] J. Vasc. Surg. 2025 | 1159 (1159) | -technical success -mortality -MACEs -graft occlusion(s) | 100% 1.8% - - | 100% 1.7% - - | NA NA - - | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 97% 97.1% - - - 96% | 97% 98% - - - 91.1% | NA 0.76 - - - 0.56 |
| Jung, G. et al. [35] J. Vasc. Surg. 2022 | 794 (768) | -technical success -mortality -MACEs -graft occlusion(s) | - 0.5% 0.8% 0.4% | - 1.9% 0.9% 1.9% | - 0.143 0.591 0.655 | -overall survival -amputation-free survival -primary patency -primary assisted patency -secondary patency -freedom from reintervention | 92% - 74.2% - - - | 92% - 29.1% - - - | NA - <0.005 - - - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertagna, G.; Scarati, V.; Troisi, N.; Berchiolli, R. Contemporary Management of Popliteal Artery Aneurysms: A Comprehensive Review. Medicina 2025, 61, 2026. https://doi.org/10.3390/medicina61112026
Bertagna G, Scarati V, Troisi N, Berchiolli R. Contemporary Management of Popliteal Artery Aneurysms: A Comprehensive Review. Medicina. 2025; 61(11):2026. https://doi.org/10.3390/medicina61112026
Chicago/Turabian StyleBertagna, Giulia, Valentina Scarati, Nicola Troisi, and Raffaella Berchiolli. 2025. "Contemporary Management of Popliteal Artery Aneurysms: A Comprehensive Review" Medicina 61, no. 11: 2026. https://doi.org/10.3390/medicina61112026
APA StyleBertagna, G., Scarati, V., Troisi, N., & Berchiolli, R. (2025). Contemporary Management of Popliteal Artery Aneurysms: A Comprehensive Review. Medicina, 61(11), 2026. https://doi.org/10.3390/medicina61112026







