Abstract
Diabetes mellitus and atrial fibrillation (AF) frequently coexist, creating a complex bidirectional relationship that exacerbates cardiovascular risk and challenges clinical management. Diabetes fosters a profibrotic, pro-inflammatory, and proarrhythmic atrial substrate through a constellation of pathophysiologic mechanisms, including metabolic remodeling, oxidative stress, mitochondrial dysfunction, ion channel dysregulation, and autonomic imbalance, thereby promoting AF initiation and progression. Conventional rhythm control strategies remain less effective in diabetic individuals, underscoring the need for innovative, substrate-targeted interventions. In this context, sodium–glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists have emerged as promising agents with pleiotropic antiarrhythmic properties, modulating fibrosis, inflammation, and mitochondrial integrity. Moreover, advances in anti-inflammatory, antifibrotic, and ion channel-modulating therapeutics, coupled with novel mitochondrial-targeted strategies, are reshaping the therapeutic landscape. Multi-omics approaches are further refining our understanding of diabetes-associated AF, facilitating precision medicine and biomarker-guided interventions. This review delineates the molecular nexus linking diabetes and AF, critically appraises emerging rhythm control strategies, and outlines translational avenues poised to advance individualized management in this high-risk population.
1. Introduction
Diabetes mellitus (DM) has emerged as a major public health concern, with a significant increase expected in the number of diagnosed individuals over the next two decades [1]. Beyond its well-established association with cardiovascular disease, DM has also been recognized as an independent risk factor for atrial fibrillation (AF) [2]. AF, the most prevalent sustained arrhythmia among adults worldwide, imposes a substantial burden on patients, healthcare systems, and the global economy, affecting more than 59 million individuals globally [3].
DM and AF frequently coexist, with DM affecting approximately 25% of individuals diagnosed with AF [4]. Emerging data indicate that individuals with type 2 DM (T2DM) are estimated to have a 38.6% likelihood of developing incidental AF [5]. Persistent DM accompanied by inadequate glycemic control further increases this risk by an additional 3% annually [6]. Moreover, type 1 diabetes mellitus (T1DM) has been linked to a moderate increase in AF risk among men (approximately 13%) and a substantially higher risk among women, reaching up to 50% [7]. The combination of DM and AF is associated with an impaired quality of life and a poorer prognosis characterized by increased mortality, a higher incidence of cardiovascular complications, and elevated healthcare costs [8,9]. The risk of developing AF increases in association with the severity of hyperglycemia, heightened glycemic variability, and prolonged duration of DM exposure [6,10,11].
AF represents the most common sustained cardiac arrhythmia encountered in contemporary clinical practice and is intricately linked to heightened morbidity, elevated all-cause and cardiovascular mortality, and a substantial increase in healthcare resource utilization and economic burden—regardless of symptomatic presentation [12,13]. Over the past decades, there has been significant progress in the antiarrhythmic treatment of AF, including both pharmacological and non-pharmacological approaches [14]. Despite technological advances in catheter ablation, the presence of DM, particularly when poorly controlled, is associated with a higher risk of post-ablation AF recurrence [15,16,17]. In terms of pharmacological treatment, several novel agents are now available for managing DM. Among these, sodium–glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists, owing to their multifaceted actions, have been proposed as valuable agents in the management of AF via their direct and predominantly indirect antiarrhythmic properties [18,19,20]
The growing prevalence of individuals with both AF and diabetes DM presents a complex public health challenge, primarily due to the complexities involved in managing these coexisting conditions [21]. This overlap exposes notable deficiencies in current treatment strategies, including clinicians’ reluctance to employ rhythm-control approaches in patients with DM, despite evidence that early rhythm control is associated with a reduced risk of DM-related complications and mortality [9,22,23]. Paradoxically, although DM patients are more likely to present with persistent or permanent AF, they are less frequently treated with rhythm-control therapies compared to euglycemic individuals [9]. Hence, there remains an unmet need for more effective, personalized, holistic, and molecularly targeted therapies to address the multifaceted clinical demands of patients affected by both DM and AF.
This review aims to summarize current evidence on the pathophysiologic link between AF and DM and explores emerging molecularly targeted therapies to better address the multifaceted clinical demands of patients with both conditions, with particular emphasis on rhythm-control strategies.
2. Methods
The present review was undertaken to critically synthesize contemporary evidence on the mechanistic interplay between diabetes mellitus and atrial fibrillation, with particular emphasis on pathophysiological substrates and emerging rhythm control strategies. A comprehensive literature search was conducted across PubMed, Scopus, and Web of Science databases up to June 2025. The search strategy employed combinations of controlled vocabulary and free-text terms, including but not limited to atrial fibrillation, diabetes mellitus, atrial remodeling, electrophysiological alterations, fibrosis, inflammation, GLP-1 receptor agonists, and SGLT2 inhibitors. Original experimental studies, clinical trials, meta-analyses, and high-quality mechanistic reviews published in English were screened for inclusion based on relevance to the scope of this study. Additional references were identified through manual citation tracking of pertinent articles.
3. Pathophysiologic Nexus Between Diabetes and Atrial Fibrillation
3.1. Metabolic Remodeling
Beyond electrical and structural remodeling, emerging research highlights significant alterations in cellular metabolism associated with AF [24] (Figure 1). Known as metabolic remodeling, this process often precedes AF-related structural and electrophysiological alterations and involves changes in energy utilization within the atrial myocardium to meet the increased metabolic demands of AF. Over time, these changes can become maladaptive, impairing atrial function and contributing to both the onset and persistence of the arrhythmia [24,25].
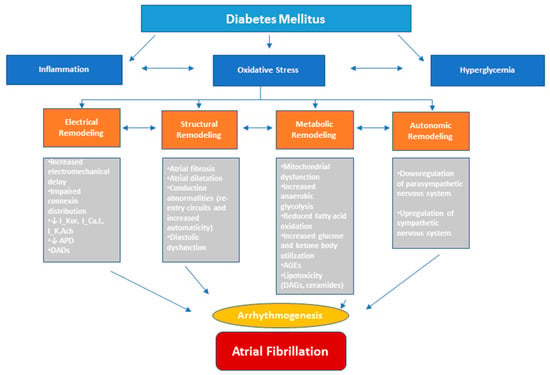
Figure 1.
Pathophysiological drivers of diabetes mellitus (DM) in atrial fibrillation (AF). DM-associated AF arises from a convergence of multiple upstream mechanisms, including inflammation activation, oxidative stress, glucose fluctuations, and autonomic dysregulation. These processes contribute to the structural, electrical, metabolic, autonomic remodeling of the atrial myocardium, promoting both the initiation and perpetuation of AF. APD, action potential duration; DADs, delayed afterdepolarizations; AGEs, advanced glycation end-products; DAGs, diacylglycerols.
Under normal conditions, the heart meets about 95% of its energy needs through mitochondrial oxidative phosphorylation, with fatty acid oxidation providing 40–60% of this ATP. The rest originates from pyruvate derived from glucose, lactate, and ketones. During AF, metabolic shifts occur, including increased anaerobic glycolysis, reduced glucose and fatty acid oxidation, and greater reliance on ketone metabolism [26]. Key molecular pathways implicated in these changes include Sirtuins3 (SIRT3)/AMP-activated protein kinase (AMPK) signaling, carnitine palmitoyltransferase-1 (CPT-1), acetyl-CoA carboxylase (ACC), peroxisome proliferator-activated receptor α (PPARα), and the downregulation of glucose transporter type 4 (GLUT4) [27,28,29].
T2DM promotes metabolic remodeling in AF by many ways such as altering energy substrate use, inducing mitochondrial dysfunction, and increasing oxidative stress and inflammation [24]. Additionally, T2DM causes lipotoxicity due to an imbalance between fatty acid uptake and oxidation, leading to the accumulation of toxic lipid intermediates such as diacylglycerols (DAGs) and ceramides [30]. These metabolites activate inflammatory signaling pathways—particularly through protein kinase C (PKC) and nuclear factor kappa B (NF-κB)—resulting in insulin resistance, apoptosis, and elevated pro-inflammatory cytokines like tumor necrosis factor (TNF), which contribute to atrial electrical and structural remodeling [31,32,33]. Furthermore, hyperglycemia promotes the formation of advanced glycation end-products (AGEs), which interact with their receptors (RAGE) to stimulate pro-fibrotic pathways, such as the upregulation of connective tissue growth factor (CTGF), causing atrial fibrosis in diabetic hearts [34,35].
Insulin resistance (IR) has been proposed as an independent risk factor for AF, even prior to the onset of diabetes, though clinical evidence remains mixed. Some studies, using HOMA-IR, show strong associations in individuals without T2DM [36], while others report no significant link [37,38]. However, animal studies consistently support a causal role for IR in developing AF, likely through molecular pathways involving increased transforming growth factor beta-1 (TGF-β1), oxidative stress, Rac1 activation, and disrupted calcium handling mediated by oxidized calcium/calmodulin-dependent protein kinase type II delta (CaMKIIδ), all contributing to atrial remodeling and arrhythmogenesis [39].
3.2. Inflammatory Signaling and Oxidative Stress
Inflammation, local and systemic, and oxidative stress are well-established factors contributing to the pathogenesis of AF in diabetic hearts. DM provokes systemic inflammation, characterized by elevated levels of inflammatory markers such as C-reactive protein (CRP), TNF-α, interleukin-6 (IL-6), and TGF-β1. These inflammatory mediators induce atrial anatomical and electrical remodeling [40,41]. Additionally, DM-related activation of NF-κB and NOD-like receptor protein 3 (NLRP3) inflammasome pathways further sustains inflammation within the atrial myocardium, enhancing the development of an AF-maintaining substrate [42,43]. Dysfunctional adipose tissues, particularly the epicardial fat layer, also contribute to the release of pro-inflammatory cytokines, while the release of anti-inflammatory adipokines diminishes. This imbalance leads to vascular endothelial damage, myocardial injury, oxidative stress, and increased thrombosis [44].
Oxidative stress, characterized by the enhanced production of reactive oxygen species (ROS), results from mitochondrial dysfunction and increased activation of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase and xanthine oxidase [45]. Patients with DM exhibit both elevated levels of ROS and reduced activity of antioxidant enzymes such as glutathione peroxidase and superoxide dismutase, indicating a heightened burden of oxidative stress [40,42]. ROS contribute to the formation of a pro-arrhythmic substrate that facilitates the development and maintenance of AF through multiple molecular interrelated mechanisms. Specifically, ROS increase the oxidation of ryanodine receptor-2 (RyR2) and CaMKII, which promote arrhythmogenic Ca2+ leakage in atrial cardiomyocytes [45]. Furthermore, activation of the stress-responsive c-Jun N-terminal kinase isoform 2 (JNK2) facilitates RyR2-mediated diastolic sarcoplasmic reticulum (SR) Ca2+ leak via CaMKII, while independently enhancing sarco/endoplasmic reticulum Ca2+-ATPase (SERCA2) activity, which contributes to arrhythmogenesis [46,47]. In addition, persistent ROS activity activates the TGFβ1/Smad3 signaling pathway, which promotes fibrosis by upregulating fibrotic markers and enhancing the growth of fibroblasts [48]. Oxidative stress also contributes to electrical remodeling by activating PKC, which in turn leads to activation of the acetylcholine-regulated K+ current (IK,Ach) and shortening of action potential duration (APD), promoting the maintenance of AF [49]. Last, impaired nitroso–redox balance (increased ROS and reduced nitric oxide) may further contribute to arrhythmogenesis through the production of delayed afterdepolarizations (DADs) [42].
3.3. Fibrosis and Extracellular Matrix Remodeling
Atrial fibrosis plays a fundamental role in the development of atrial cardiomyopathy and contributes to both the genesis and progression of AF. It is characterized by the excessive accumulation of extracellular matrix (ECM) components, which enhances tissue stiffness and impairs normal cardiac structure and function. The pathophysiology underlying atrial fibrosis in AF is multifaceted and dynamic, involving stretch-induced fibroblast activation, fibrofatty infiltrations, localized and systemic inflammation, oxidative stress, and activation of coagulation pathways. In the context of AF, distinct patterns of fibrosis, such as reactive and replacement fibrosis, are observed and disrupt atrial tissue architecture. This structural remodeling promotes conduction abnormalities, facilitating re-entry circuits and increasing automaticity, both of which contribute to the persistence of AF [50,51].
AF-related atrial fibrosis is driven by complex molecular pathways that regulate ECM remodeling. One of the key mediators is TGF-β1, which activates the Smad signaling cascade, leading to enhanced transcription of fibrotic genes and significant dysregulations in the synthesis and degradation of collagen I, III, and IV [52,53]. The activated renin–angiotensin–aldosterone system (RAAS), primarily through angiotensin II, further enhances TGF-β1 expression and induces oxidative stress, both of which promote fibroblast activation and ECM deposition [53]. In this context, excessive ventricular myocardial fibrosis can lead to diastolic dysfunction, predisposing individuals with diabetes to abnormal ventricular filling and subsequent atrial enlargement [24]. Inflammatory cytokines, including TNF-α, IL-6, and IL-1β, also contribute to the process by enhancing pro-fibrotic signaling and subsequent fibroblast activation [54]. Additionally, the matrix metalloproteinase (MMP)/tissue inhibitor of metalloproteinases (TIMP) balance is impaired in AF, promoting fibrotic remodeling. Elevated levels of RECK, a membrane-anchored MMP inhibitor, further inhibit matrix degradation, exacerbating atrial structural remodeling [52].
DM creates a favorable environment that amplifies the fibrotic processes described above. In fact, DM is associated with myocardial fibrosis, independent of the presence of coronary artery disease or hypertension [53]. This association is mediated by enhancing key fibrosis-induced mechanisms, including oxidative stress and inflammation, activation of pro-fibrotic signaling pathways, accumulation of AGEs, and activation of RAAS [53]. These processes contribute to fibroblast activation and increased collagen ECM deposition, thereby leading to atrial structural remodeling and impaired myocardial function [50].
3.4. Electrophysiological Remodeling and Ion Channel Dysfunction
Electrophysiological remodeling constitutes a major substrate for diabetes-related AF. The majority of our current knowledge regarding electric and electromechanical alterations in diabetic hearts is derived from animal studies, owing to the limited amount of research conducted for this subject in the AF–DM population. Studies in diabetic animal models have quantified increases in inter-atrial conduction time (IACT), effective refractory period dispersion (AERPD), and prolongation of atrial APD [55,56]. These abnormal electrophysiological patterns are closely linked to changes in the expression and function of various ion channels in atrial myocytes (ion channel remodeling) which contribute to the increased AF susceptibility in DM [57]. Regarding sodium channels, studies have shown that sodium channel current (INa) is reduced in the atrial myocyte tissue of Akita T1DM mice, primarily due to decreased expression of SCN5A mRNA and NaV1.5 protein [58]. In contrast, the late sodium current (INa,L) is increased in diabetic mice [59]. Of note, this basal INa,L is mainly generated by the NaV1.5 isoform and is regulated by CaMKII [60]. Furthermore, diabetic-induced alterations of depolarizing L-type Ca2+ channels (ICa,L) and repolarizing atrial-specific K+ channels, such as the Ca2+-activated small-conductance K+ current (ISK), the IK,ACh, and the ultrarapid delayed-rectifier K+ current (IKur), can modify APD, thereby contributing to increased arrhythmogenicity [24].
Additional AF-induced electrophysiological features observed in diabetic hearts include reduced atrial conduction velocity, resulting from impaired connexin distribution [61] and decreased peak sodium current (ΙNa,Peak) [58], and an increased incidence of arrhythmogenic Ca2+ release events, driven by CaMKII activation and increased oxidative stress associated with DM [24]. Moreover, DM is frequently associated with impaired atrial excitation–contraction coupling and prolonged conduction times, leading to electromechanical delay (EMD), which is a recognized independent predictor of both new-onset and recurrent AF [62,63].
In summary, the electrophysiological remodeling in DM, encompassing ion channel alterations, prolonged APD, and reduced conduction velocity, can contribute to an increased susceptibility to AF.
3.5. Mitochondrial Dysfunction and Energetic Impairment
Mitochondrial dysfunction plays a critical role in both the initiation and maintenance of AF in diabetic hearts, driven by various underlying mechanisms [64,65]. As previously mentioned, diabetes-related mitochondrial impairment is associated with excessive ROS generation which contributes to mitochondrial DNA damage, altered gene transcription, enhanced activity of xanthine oxidase and NADPH oxidase, and activation of inflammatory pathways (NF-κB, caspase-1, and NLRP-3 inflammasome) [66,67]. Oxidative stress further promotes arrhythmogenesis by increasing the oxidation of ryanodine receptors and CaMKII, and by enhancing atrial fibrosis, an important factor of atrial structural remodeling [57].
In the context of DM, IR and subsequent hyperglycemia shift myocardial energy metabolism towards increased fatty acid oxidation and less towards carbohydrates, which is less efficient in terms of ATP production, thereby unable to meet the high energy demands of fibrillating atria [68]. This metabolic inflexibility further leads to elevated oxygen consumption and increased production of ROS derived from mitochondrial dysfunction. These changes cause significant anatomical and functional alterations in the atrial myocardium, such as fibrosis and dilation, which have proarrhythmic effects that facilitate the onset and progression of AF [69]. Furthermore, decreased ATP levels promote arrhythmogenesis by rapidly activating the sarcoplasmic ATP-sensitive potassium (KATP) channels, which shorten APD and reduce action potential amplitude (APA) [70]. Moreover, mitochondrial biogenesis and function are compromised due to the downregulation of key regulatory proteins such as AMPK, PGC-1α, and SIRT1. This resulting energy shortfall disrupts ATP-dependent ion transport mechanisms, such as including SERCA2a and the Na+/K+-ATPase, thereby contributing to calcium dysregulation, electrical instability, and atrial structural changes. These metabolic and electrophysiological alterations synergically create a pro-arrhythmic substrate, facilitating both the development and persistence of AF in individuals with diabetes [71].
3.6. Autonomic Dysfunction
Autonomic imbalances, commonly observed in patients with DM, contribute to the development of atrial cardiomyopathy and increase the risk of AF [51]. In T2DM, cardiac autonomic neuropathy is characterized by increased sympathetic activity and reduced parasympathetic tone, as evidenced by findings from heart rate variability studies [72,73]. Parasympathetic stimulation can induce macro–reentrant circuits, whereas sympathetic activation may enhance abnormal automaticity and trigger activity. Moreover, autonomic dysfunction often precedes clinical diagnosis as blunted vagal responses and reduced acetylcholine release. These alterations impair atrial electrophysiology, thereby promoting the onset and maintenance of AF [74].
4. Emerging Molecular Targets for Rhythm Control in Diabetes-Associated AF
4.1. Anti-Inflammatory Pathways
Targeting inflammatory signaling has emerged as a promising therapeutic option, given the critical role of inflammation in the pathogenesis of AF among individuals with diabetes [75]. A key component of this inflammatory process is the activation of the NLRP3 inflammasome, observed in individuals with DM and paroxysmal, chronic, and postoperative AF [76]. Inhibition of the NLRP3 inflammasome can be achieved by therapeutic compounds targeting different signaling pathways [77]. Colchicine, a widely recognized and affordable anti-inflammatory drug, has been identified as a potential agent for the prevention of cardiovascular diseases by inhibiting the inflammatory axis. It exerts its anti-inflammatory effect by disrupting cytoskeletal functions in neutrophils and monocytes, inhibiting β-tubulin polymerization into microtubules, and suppressing chemotaxis [78]. Given that the spatial organization of the NLRP3 inflammasome is dependent on the integrity of the microtubule network, colchicine may serve as a promising therapeutic option for AF [79]. Incorporating insights from several trials suggest a general favorable trend of colchicine in preventing AF relative to placebo [77]. However, findings from the most recent randomized, placebo-controlled COP-AF trial showed that administration of colchicine in patients undergoing major thoracic surgery did not significantly reduce the incidence of post-operative AF [80]. Furthermore, several other compounds have been identified as direct inhibitors of the NLRP3 inflammasome and are currently under investigation for their antiarrhythmic effects. For instance, MCC950 reduced myocardial fibrosis, suppressed collagen production in animal models, and alleviated the risk of AF, while CY-09, RRx-001, JC-121, JC-124, and dapansutrile demonstrated favorable cardioprotective effects [77]. However, large-scale, randomized trials are necessary to evaluate their efficacy in preventing AF.
Targeting key products of the activated NLRP3 inflammasome, such as IL-1β, IL-18, and TNFα, may also be a promising approach for AF management, as these cytokines are upregulated in the serum of AF and post-operative AF patients and induce arrhythmogenesis [77]. Anakinra, an interleukin-1 receptor antagonist, and etanercept, a biologic TNF inhibitor, are potent anti-inflammatory drugs currently under clinical investigation for indications beyond cardiovascular diseases [79]. Canakinumab, a monoclonal IL-1β neutralizing antibody, has been proven to significantly reduce major cardiac events in patients with atherosclerosis (CANTOS trial) [81]. In 2020, the randomized, double-blind, placebo-controlled CONVERT-AF trial was conducted to evaluate the impact of canakinumab on preventing AF recurrence in patients with persistent AF undergoing electrical cardioversion to restore sinus rhythm. Although statistical significance for the primary endpoint was not achieved (p = 0.09), a promising trend was observed, with AF recurrence at 6 months occurring in 77% of patients in the placebo group and 36% in the canakinumab group [82].
Another category of agents with anti-inflammatory effects includes NF-κB inhibitors. Pinocembrin, an abundant flavonoid, has shown potential anti-AF properties in experimental MI animal model by mitigating atrial fibrosis, ameliorating autonomic and electrical remodeling, and suppressing inflammatory responses [83]. Additionally, experimental evidence suggests a critical role for the S100 protein family in the pathogenesis of various cardiovascular diseases [84]. Tasquinimod, an inhibitor of S100A8/A9 interaction and TLR4, improved the left ventricular systolic function and reduced the regulation of IL-1β, interferon-gamma (IFNγ), and TNFα in mice models, imposing as a potential antiarrhythmic agent [85]. Other targeting NLRP3 inflammasome-related pathways include the blockage of caspace-1, inflammasome component ASC, and NF-κB by compounds which are currently under investigation [77].
Beyond these pathways, another inflammatory mechanism that promotes AF is the infiltration of CCR2+ pro-inflammatory macrophages into the atrial myocardium, leading to pathological structural remodeling [86]. AF-related inflammation is associated with the recruitment of CCR2+ SPP1+ macrophages in the diseased human atrial myocardium, a process also seen in AF-vulnerable mice models [87]. SPP1+, also known as osteopontin, promotes atrial fibrosis and mediates signaling between immune cells. Studies in HOMER mice have shown that transplanting Spp1 bone marrow reduces AF maintenance and atrial fibrosis. Similar results were achieved using an antibody–siRNA conjugate to silence Spp1 in cardiac macrophages [88].
4.2. Anti-Fibrotic Signaling
Dissolving pre-existing collagen deposits in atrial tissue remains a significant therapeutic challenge. Current pharmacological approaches primarily aim to prevent the progression of atrial fibrosis associated with various cardiac conditions [89,90,91,92,93]. Targeting the RAAS through ACE inhibitors, angiotensin II receptor blockers (ARBs), or mineralocorticoid receptor antagonists (MRAs) may delay or prevent the development of atrial fibrosis [90,91,92,94]. Notably, finerenone, a nonsteroidal MRA, has been recently shown to reduce the risk of new-onset AF/AFL across the cardio–kidney–metabolic spectrum [95]. Several molecular pathways, including NF-κB, NADPH oxidase, lysyl oxidase homolog 2 (LOXL2), and the TGFβ1–SMAD2/3 signaling cascade, have been implicated in angiotensin II-induced atrial fibrosis [96,97,98,99]. Inhibiting these pathways may help reduce atrial fibrosis progression and lower the incidence of AF.
Additionally, endothelin 1 signaling has been shown to induce atrial remodeling in spontaneously hypertensive rats and exacerbate cardiac fibrosis in diabetic mice [100,101]. Macitentan, an endothelin receptor antagonist, decreased atrial endothelin 1 levels and prevented pacing-induced increases in pro-endothelin 1 mRNA. It also reduced atrial pro-inflammatory signaling, though it had minimal impact on calcium-regulating proteins, hypertrophy markers, and fibrosis indicators [100]. Protease-activated receptors 1 and 2 (PAR1 and PAR2) are also potential therapeutic targets for preventing atrial fibrosis in diabetic patients, but their effects are context-dependent, with evidence showing varied responses across cell types and experimental models, highlighting the need for further well-designed clinical trials to evaluate their efficacy [102,103,104,105].
Several microRNAs (miRNAs), such as miR-29, miR-30, miR-133, miR-21, and miR-590, regulate gene expression linked to cardiac fibrosis, with some inhibiting collagen production and others affecting TGFβ1 or SMAD3 expression [106]. miR-135b-5p and miR-138-5p influence glycosaminoglycan biosynthesis, though further validation is needed. Additionally, epigenetic mechanisms, like histone deacetylases and EZH2 expression, play roles in fibrosis regulation, suggesting new therapeutic opportunities for atrial fibrosis and AF [107,108,109,110,111,112,113,114,115]. Moreover, lutein, a naturally occurring carotenoid with metabolic benefits, also demonstrates potential anti-inflammatory, antioxidant, and antifibrotic effects in cardiac injury, although its therapeutic use is constrained by bioavailability challenges [116,117,118,119]. Furthermore, Wu et al. [120] investigated the role of the NLRP3 inflammasome-CASP1-galectin 3 pathway in AF and atrial remodeling, and evaluated the effects of glibenclamide, a hypoglycemic agent and NLRP3 inflammasome inhibitor, in diabetic rabbits. Their findings showed that glibenclamide treatment attenuated atrial fibrosis, restored epicardial conduction and conduction homogeneity, and decreased the inducibility of AF, all linked to the inhibition of the NLRP3 inflammasome [120].
4.3. Ion Channel and Calcium Handling Modulators
Given the limitations of classical antiarrhythmic agents, recent research in the field of AF has focused on identifying atrial-specific molecular targets, particularly ion channels and their upstream modulators, to achieve rhythm control with reduced proarrhythmic risk and fewer non-cardiac adverse effects.
Atrial electrical remodeling following hyperglycemia plays a pivotal role in the pathogenesis of AF, contributing to its onset and progression in DM [121]. This process is characterized by alterations in transmembrane ionic currents, involving the downregulation of L-type calcium current (ICa,L) and the upregulation of inward rectifier potassium current (IK1) and IK,ACh. These changes synergistically shorten the atrial AP duration and refractory period, promoting reentry and ectopic activity [122,123,124,125]. Oxidative stress in DM further exacerbates these electrical alterations via redox-sensitive signaling pathways, notably those depended on CaMKII, a key modulator of metabolic and electrical remodeling in AF [24].
Among the most promising atrial-selective targets is IKur current, primarily mediated by the Kv1.5 channel. Kv1.5 is expressed almost exclusively in atrial tissue, making it an ideal target for atrial-selective blockade. Experimental compounds such as AVE0118, primarily an IKur, Ito, and IK,ACh blocker, and XEN-D0101, a highly selective IKur blocker, have demonstrated efficacy in prolonging atrial refractory periods without affecting ventricular repolarization, thereby minimizing the risk of a proarrhythmic event [126,127,128,129,130,131,132,133,134].
Another important target is the INa,L current, which is enhanced in diabetic cardiomyocytes due to oxidative alterations of Na+ channels. This contributes to prolonged depolarization and Ca2+ overload. Ranolazine, a selective inhibitor of INa,L, has demonstrated atrial-specific antiarrhythmic properties and is particularly promising in the context of diabetes-related electrical remodeling [135,136,137,138,139,140,141].
Another promising investigational pharmacological strategy for developing new anti-AF agents involves targeting gap junctions—clusters of ion channels that facilitate intercellular communication and connectivity. Each gap junction is composed of two hemichannels (connexons), and each connexon consists of six connexin proteins. Human atria particularly express connexin 40 and connexin 43 [142,143]. Under pathological conditions such as ischemia and diabetes-induced fibrosis, gap junction channels become dysfunctional, increasing the risk of arrhythmogenesis [144,145]. This dysfunction is characterized by reduced conduction and shortened APD, leading to greater dispersion of the refractory period [144]. Several selective gap junction enhancer peptides—such as AAP10, ZP123, and GAP-134—have been synthesized to regulate gap junction conduction, but their clinical efficacy remains to be fully investigated [146].
NCX has been identified as a potential therapeutic target for the prevention of AF, as its excessive reverse mode may promote arrhythmia by increasing the incidence of delayed afterdepolarizations. Experimental evidence suggests that NCX blockers, such as SEA-0400 and KBR7943, may prevent the onset and occurrence of AF. Despite these findings, large clinical studies are required to evaluate NCX blockers antiarrhythmic effects [147,148,149,150,151].
Furthermore, the ROS-CaMKII axis has garnered significant attention as a central arrhythmogenic molecular pathway in DM. Excessive ROS promotes the activation of CaMKII, which phosphorylates various ion channels including RyR2 and Na_v1.5, enhancing spontaneous Ca2+ release and INa,L [152]. In preclinical studies, inhibitors of CaMKII, such as KN-93 analogs, have shown promising results in suppressing AF by stabilizing calcium homeostasis and reducing INa,L-mediated depolarizations [153,154]. In addition, abnormal sarcoplasmic reticulum (SR) Ca2+ leak via RyR2 has been implicated as one of the major mechanisms of afterdepolarizations and triggered activity in various AF models [154,155]. RyR2 stabilizers, such as JTV519 which enhances the binding affinity of FKBP12.6 to RyR2, may exert anti-AF effects by mitigating Ca2+ leak [156]. SERCA2a, another key calcium modulator, often shows diminished activity in the diabetic heart due to increased expression of phospholamban. The resulting calcium overload exacerbates delayed afterdepolarizations DADs and impairs atrial contractility. Targeting SERCA2a, through gene therapy using adenoviral-based delivery of Ca2+ binding proteins, may improve rhythm control [124].
4.4. Mitochondria-Targeted Therapeutics
Mitochondrial dysfunction and diabetes-associated AF have a close etiopathogenetic relationship. Diabetic atrial cardiomyocytes exhibit enhanced ROS production and mitochondrial hyperpolarization, leading to increased susceptibility to AF [157]. Several commonly used drugs, such as ACE inhibitors and statins, as well as nutraceuticals like CoQ10 and N-acetylcysteine, exert indirect effects on mitochondrial function and may offer a potential therapeutic approach for treating AF [158]. However, large-scale randomized trials are needed to confirm their efficacy and validate their role in AF prevention.
Novel antiarrhythmic approaches, such as mitochondria-targeted antioxidants, membrane stabilizers, and modulators of mitochondria biogenesis, represent exciting avenues but are still in early preclinical stages and face translational hurdles. Elamipretide is a mitochondria-targeted peptide that preserves the integrity of cardiolipin and improves the coupling of the electron transport chain. While some benefits have been observed in heart failure patients, its potential anti-arrhythmic effects against AF, remain to be established [159]. MitoQ, a mitochondria-targeted antioxidant, has demonstrated beneficial effects on the cardiovascular system, including the reduction in aortic stiffness and enhancement of endothelial function. It may also exert favorable effects on atrial remodeling by neutralizing ROS within the mitochondria [160]. Trimetazidine, a metabolic modulator, targets the respiratory chain by activating complex I and regulates the expression of factors involved in mitochondrial biogenesis. It is suggested that trimetazidine may exhibit antiarrhythmic properties by mitigating atrial structural remodeling, preventing the onset and maintenance of AF [161]. Moreover, KL1333, a novel NAD+ modulator, may exert its antiarrhythmic properties via enhancing the activity of AMPK/SIRT1/PGC-1a axis, which is crucial for maintaining mitochondrial metabolic homeostasis [162].
Gene-based approaches targeting key mitochondrial regulators such as PGC-1a, mitochondrial catalase (mCAT), and mitochondrial transcription factor A (TFAM) represent promising avenues for clinical translation [161]. Additionally, innovative technologies like lipid nanoparticle delivery systems and adenovirus vectors hold promise in addressing the arrhythmogenic substrate in diabetes-associated AF [50].
5. Modulation of AF Substrate by SGLT2 Inhibitors and GLP-1 Receptor Agonists
5.1. SGLT2 Inhibitors
SGLT2 inhibitors represent a relatively novel category of oral antidiabetic agents that function by inhibiting the renal reabsorption of sodium and filtered glucose. This action declines the renal threshold for glucose absorption in the proximal convoluted tubules, thereby causing glycosuria and natriuresis. These agents have demonstrated unique cardio–renal–metabolic benefits, with emerging evidence revealing their surprisingly significant benefits in various cardiovascular conditions, including AF onset or maintenance, regardless of glycemic status [20,163,164,165]. Indeed, SGLT2is, owing to their multifaceted pathophysiological actions, have emerged as valuable agents in the treatment of AF due to their direct and indirect antiarrhythmic properties [20].
Inflammation induces the development and progression of atrial structural and electrical remodeling, particularly in diabetes [20]. Emerging evidence from animal and human studies suggests that SGLT2is could be beneficial to prevent AF episodes by attenuating the inflammatory response [166,167]. SGLT2is suppress the release of circulating pro-inflammatory and inflammatory cytokines such as CRP, TNF-α, IL-6, MCP-1, TGF-β [167,168,169], regulate NO bioavailability [170], and modulate the activity of NLRP-3 inflammasome, thereby reducing the release of IL-1β and IL-18 [171]. Furthermore, SGLT2is enhance the reduction in EAT, a highly metabolically active tissue which contributes to the onset and progression of AF [172,173].
Mitochondrial dysfunction and oxidative stress are pivotal in atrial cardiomyopathy and AF progression across both individuals with and without diabetes [68]. ROS generated from mitochondrial dysfunction contribute to atrial fibrosis, dilation, and hypertrophy, exerting proarrhythmic effects and facilitating the onset and progression of AF [69,70]. Experimental animal studies have demonstrated that SGLT2is reduce ROS production, improve mitochondrial respiratory capacity, increase mitochondrial biogenesis, and regulate intracellular calcium handling, thereby leading to the reversal of atrial myopathy [174,175]. In addition, SGLT2is enhance cellular autophagy by activating key metabolic regulators, including AMPK, sirtuins (SIRT1, SIRT3, SIRT6), and PGC1-α, while concurrently suppressing the activity of mammalian target of rapamycin (mTOR) [176]. Furthermore, SGLT2is induce a metabolic shift from glucose to ketone bodies, thereby enhancing myocardial energy efficiency [20].
Atrial fibrosis plays a critical role in both the initiation and progression of AF. SGLT2is attenuate atrial fibrosis through multiple mechanisms. As mentioned above, these agents enhance mitochondrial function and reduce the production of ROS, thereby suppressing pro-fibrotic signaling pathways such as the TGF-β/SMAD axis [177]. In diabetic db/db mice, treatment with empagliflozin also led to the downregulation of pro-fibrotic proteins, including serum/glucocorticoid-regulated kinase 1 (SGK1) and the epithelial sodium channel (ENaC), resulting in reduced interstitial fibrosis in atrial tissue [178]. In addition, SGLT2 inhibitors exhibit anti-inflammatory properties by lowering circulating levels of cytokines like IL-6 and TNF-α involved in cardiac fibroblast activation and ECM remodeling [171,179,180]. Furthermore, their natriuretic and diuretic effects reduce atrial wall stretch and pressure, thereby alleviating mechanical stress-induced fibrosis [20,181].
Further, indirect antiarrhythmic mechanisms of SGLT2is include the stimulation of erythropoietin production and release, which enhance atrial oxygen delivery, the reduction in plasma uric acid levels, a known AF-risk factor, and the renal reabsorption of Mg2+ [20]. Moreover, SGLT2is enhance autonomic nervous system regulation by suppressing GPR41 in aortic, cardiac, and renal tissues, along with avoiding hypoglycemia and significant alterations in intravascular fluid volume [182,183].
Recent studies highlight the direct effects of SGLT2is on atrial electrophysiology. In a recent study, the acute treatment of increased single-dose dapagliflozin on human atrial cardiomyocytes suppressed action potential formation by directly inhibiting INa,peak and, to a lesser extent, Ito. These findings indicate the acute class I antiarrhythmic effects of dapagliflozin [184]. Also, SGLT2is inhibit INa,L in cardiomyocytes by interacting with Nav1.5 sodium channels, thereby providing cardioprotective and antiarrhythmic effects [185]. SGLT2is further reduce intracellular Na+ by inhibiting sodium–hydrogen exchanger 1 (NHE-1), thereby reversing calcium overload [186]. Muller et al. showed that dapagliflozin directly interacts with human atrial K+ channels, and that the activation of K2P2.1 and K2P17.1 currents may contribute to its beneficial antiarrhythmic effects [187]. Regarding Ca2+ homeostasis, data from animal studies reveal that empagliflozin can modify Ca2+ regulation and Na+/hydrogen-exchanger currents, contributing to its antiarrhythmic properties [188]. Furthermore, empagliflozin reduces CaMKII activity and CaMKII-dependent sarcoplasmic reticulum Ca2+ leak, which improves myocardial calcium homeostasis and helps alleviate contractile dysfunction and arrhythmias [189]. Similarly, dapagliflozin contributes to inhibiting Ang II-induced ox-CaMKII upregulation, leading to beneficial modification of the electrical and structural atrial substrate [190].
A meta-analysis of 22 clinical trials involving 52,115 patients demonstrated that treatment with SGLT2 inhibitors significantly reduced the risk of AF (relative risk [RR]: 0.82, 95% CI: 0.70–0.96) and embolic stroke (RR: 0.32, 95% CI: 0.12–0.85), irrespective of baseline glycemic status [191]. Another meta-analysis of 22 trials assessing the incidence of AF and atrial flutter (AFL) in patients with T2DM and HF, SGLT2 inhibitors led to an 18% reduction in AF/AFL occurrence compared to the placebo [192]. Similar findings were reported in a post hoc analysis of the DECLARE-TIMI 58 trial which showed fewer episodes of AF in T2DM patients treated with dapagliflozin [193]. Furthermore, these agents reduced atrial tachyarrhythmias by 22% in patients with cardiac implantable electronic devices (CIEDs) [194].
5.2. GLP-1 Receptor Agonists
GLP-1 RAs are a well-established class of antidiabetic drugs that exert their glucose-lowering effects by stimulating glucose-dependent insulin release and suppressing glucagon secretion [195]. GLP-1 RAs have demonstrated remarkable cardioprotective effects in patients with T2DM, consistently reducing the risks of nonfatal myocardial infarction, stroke, and cardiovascular death [196,197]. However, these studies were not powered to investigate the effect of GLP-1 RA treatment on AF risk, although a metanalysis suggested potential antiarrhythmic benefits compared to other antidiabetic agents [198].
Experimental studies in animal models of DM have demonstrated a reduction in AF burden after treatment with GLP-1 RAs. In a canine model of pacing-induced AF, liraglutide reduced AF inducibility and improved electrophysiological parameters, including the shortening of the atrial effective refractory period and a reduction in conduction velocity compared to the placebo [199]. Consistent with these favorable findings, treatment with liraglutide in the db/db mouse model of T2DM reduced both AF susceptibility and duration by preventing atrial fibrosis and adverse atrial electrical remodeling. At a molecular level, this study showed that chronic treatment with liraglutide prevented the reductions in Ito current and IKur current, restored the steady-state inactivation of INa current, and normalized the expression of collagen-related genes Col1a and Col3a in atrial myocytes of db/db mice [200].
Emerging preclinical in vitro and in vivo data suggest that GLP-1 receptor agonists may exert antiarrhythmic effects through a range of cytoprotective molecular mechanisms. GLP-1 RAs directly counteract atrial fibrosis by modulating cardiac fibroblast activity through GLP-1 receptor activation. This action suppresses pro-fibrotic molecular pathways, including TGF-β and CTGF, and attenuates ECM deposition [201,202]. In addition, GLP-1 RAs significantly reduce systemic and local inflammation by attenuating macrophage infiltration and pro-inflammatory cytokine levels, such as TNF-α and IL-1β [203,204]. By promoting glucose uptake through p38MAPK-dependent increased translocation of GLUTs and enhancing fatty acid oxidation, these agents optimize cardiac metabolism, reducing metabolic stress that contributes to arrhythmogenesis [205]. GLP-1 RAs also bolster antioxidant and anti-apoptotic defenses mediated by activated PKA and Epac signaling pathways [206], diminishing oxidative stress and its fibrotic consequences [207]. Moreover, liraglutide has been shown to prevent IL-1β-induced impairments in mitochondrial homeostasis by enhancing the phosphorylation of AMPK and ACC, and upregulating PGC-1α, CPT1, and diacylglycerol acyltransferase 1 (DGAT1) [208]. Last, GLP-1 RAs alleviate indirectly cardiac hypertrophy via the angiotensin II/AT1R/ACE2 and AMPK/mTOR/p70S6K pathways, lessening mechanical strain on atrial tissue and further mitigating AF burden [209].
Clinical trials evaluating GLP-1 receptor agonists, such as the LEADER trial for liraglutide and the SUSTAIN-6 trial for semaglutide, demonstrated reductions in cardiovascular death, nonfatal myocardial infarction, and stroke. However, these studies were not designed to draw definitive conclusions about their impact on arrhythmic events, including AF [195,196]. While these medications have not been associated with an increased risk of AF as an adverse effect [210], comparative analyses suggest they are less effective than SGLT2 inhibitors in preventing new-onset AF in both the general population and high-risk populations, including older adults, women, and patients with cardiovascular disease or chronic kidney disease [211]. However, a recent meta-analysis showed that GLP-1 RAs are associated with a reduced risk of AF recurrence in patients undergoing AF ablation therapy [212].
6. Multi-Omics Approaches to Unravel Molecular Networks in Diabetes-Associated AF
Emerging advances in multi-omics strategies, integrating genomics, transcriptomics, epigenomics, proteomics, and metabolomics, have revolutionized our ability to dissect the molecular complexity of multifactorial diseases such as diabetes-associated AF. These integrative approaches enable a systems-level understanding that supports the identification of novel therapeutic targets and the development of precision medicine strategies.
A widely used method for identifying genetic variants linked to common diseases is the genome-wide association study (GWAS). This method enables researchers to examine and compare allele frequency, such as single-nucleotide polymorphisms (SNPs), between affected and unaffected individuals. GWAS have identified numerous AF- associated loci, like PITX2, RAP1A/KCND3, ZFHX3, HNF4G, and KCNN3, some of which regulate developmental, electrophysiological, contractile, and structural pathways [213,214,215]. However, a Mendelian randomization analysis involving over one million individuals of European ancestry found no clinically significant causal relationship between genetically determined T2DM, fasting blood glucose (FBG), or hemoglobin A1c (HbA1c) levels and the risk of developing AF [216]. This underscores the complexity of the relationship and the need for further investigation into the genomic underpinnings of diabetes-associated AF.
Transcriptomic analyses have significantly advanced our understanding of the molecular basis of diabetes-associated AF, revealing key alterations in gene expression that contribute to ion channel remodeling, inflammation, oxidative stress, thrombogenesis, and fibrosis [217]. A recent study using bioinformatics and network analysis identified more than 100 common differentially expressed genes (DEGs) in EAT from T2DM and AF datasets. Among them, CEBPZ, PAK1IP1, and BCCIP were revealed as central regulators in EAT, influencing the pathology of T2DM and AF [218]. Regarding microRNAs (miRNAs), a recent meta-analysis identified miR-4798, miR-133a, miR-150, miR-21, hsa-miR-4443, and miR-20a-5p as significantly associated with AF. The overall association between circulating miRNAs and AF showed an odds ratio (OR) of 2.51 [95% CI: 1.99–3.16; I2 = 99%], suggesting their potential as biomarkers for AF [219]. Furthermore, several miRNAs have been identified as potential regulators of gene expression associated with DM-related AF. For instance, upregulated miR-21 promotes fibrosis after MI by targeting TGF-β/Smad7 signaling pathway [220]. In contrast, overexpression of miR-133 and miR-30c reduces CTGF levels, thereby suppressing the production of collagens [221]. These miRNAs, as modulators of fibrosis, represent potential therapeutic targets for diabetes-associated AF.
Epigenetic regulatory mechanisms, such as DNA methylation, histone modifications, along with various non-coding RNAs, including miRNAs and circular RNAs (circRNAs), may play a role in the onset and progression of AF [222]. In DM, epigenomic research indicates that prolonged hyperglycemia leads to sustained changes in DNA methylation and histone modifications. These epigenetic alterations play a significant role in the onset and progression of diabetic complications [223,224]. Notably, class I histone deacetylase (HDAC) inhibitors have demonstrated anti-fibrotic effects in the heart, suggesting their potential as a novel therapeutic class for diabetes-associated AF [225].
Proteomics enables the detection of AF-related protein alterations, offering potential in the identification of diagnostic or prognostic biomarkers and novel therapeutic targets in individuals with diabetes. For instance, in a recent study, investigators examined proteomic differences between AF patients with and without T2DM. A total of 1548 proteins were identified, and 899 were quantified using label-free quantification (LFQ) analysis. This revealed 100 significantly dysregulated proteins—21 upregulated and 79 downregulated—in T2DM hearts. Notably, DPP9 and ATP1A2 were overexpressed, while INPPL1 and ARID5A were underexpressed [226].
Metabolomic studies have revealed significant metabolic disturbances in atrial AF, particularly in pathways related to energy metabolism, oxidative stress, and lipid utilization. In a notable study, Mayr et al. [227] performed integrated metabolomic and proteomic profiling of human atrial appendage tissues from patients with persistent AF. They reported a coordinated downregulation of enzymes involved in fatty acid oxidation and a concomitant upregulation of glycolytic enzymes, including triosephosphate isomerase and glyceraldehyde-3-phosphate dehydrogenase [227]. Given the established link between myocardial metabolism and ion channel expression, these metabolic shifts may contribute to arrhythmogenesis [228].
The integration of multi-omics data through network analysis enhances the understanding of complex molecular interactions in diabetes-associated AF and aids in identifying novel diagnostic markers and therapeutic targets.
7. Translational Perspective: Precision Rhythm Control in Individuals with Diabetes
The updated guidelines for the management of AF reinforce the urgent need to approach AF as a complex cardiovascular condition that requires disease prevention, risk-factor modification, as well as aggressive early rhythm control to prevent its progression. This therapeutic approach carries greater significance in the context of DM-associated AF, where clinicians must address multiple challenges [229].
As discussed in the current review, DM creates an arrhythmogenic substrate in the atrial myocardium via multiple pathophysiological mechanisms, leading to an increased risk of developing AF [5]. Hence, successful rhythm control requires a rather holistic approach that also includes effective glycemic control and proper management of comorbidities (Figure 2). It is known that DM often coexists with other known risk factors that promote the onset of AF, such as hypertension, coronary artery disease, obstructive sleep apnea, and obesity, all of which must be carefully managed through appropriate pharmacotherapy and lifestyle modifications in order to achieve rhythm control [229].
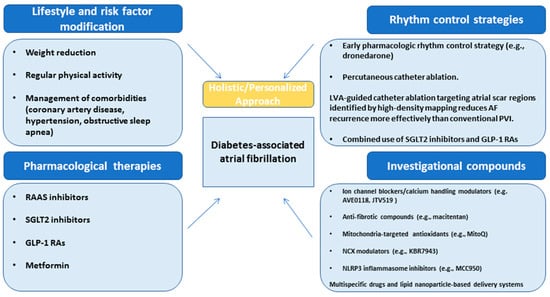
Figure 2.
Therapeutic strategies span from upstream prevention to disease modification and downstream rhythm stabilization. Key upstream targets encompass lifestyle interventions, including sustained weight management and optimal treatment of comorbidities such as coronary artery disease, hypertension, and sleep apnea. Targeted approaches addressing neurohormonal and metabolic pathways—using agents such as RAAS inhibitors, SGLT2 inhibitors, and GLP-1 receptor agonists—address fundamental mechanisms of atrial remodeling. Treatment strategies focusing on NLRP3 inflammasome activation, mitochondrial dysfunction, specific atrial ion channels, and fibro-inflammatory signaling offer mechanistically precise avenues for reducing AF burden in diabetic patients. Rhythm control strategies, particularly early catheter ablation, employing novel techniques such as LVA-guided ablation, play a critical role. This comprehensive framework represents a paradigm shift toward substrate-focused, disease-modifying strategies in the management of DM-associated AF including RAAS, renin–angiotensin–aldosterone system; SGLT2, sodium–glucose cotransporter 2; GLP-1 RAs, glucagon-like peptide-1 receptor agonists; LVA, low-voltage area; PVI, pulmonary vein isolation.
Glucose-lowering pharmacological interventions offer the potential to prevent atrial remodeling and reduce the risk of AF. However, not all antidiabetic drugs are equally effective in maintaining sinus rhythm. Metformin, the most commonly prescribed oral antidiabetic agent, mitigates AF burden through several mechanisms [230]. It attenuates oxidative stress by decreasing ROS production, exhibits anti-inflammatory properties, reducing circulating levels of cytokines IL-6 and TNF-α, improves calcium homeostasis, upregulates the expression of connexin-43 gap junction, restores current in small conductance Ca2+-activated K+ channels, activates AMPK, and modulates adiponectin signaling in the adipose tissue [231,232,233,234]. Thiazolidinediones (TZDs), another class of antidiabetic agents, have been shown to attenuate atrial fibrosis and reduce interatrial activation time, thereby potentially reducing AF vulnerability [235]. However, various clinical trials have yielded conflicted results regarding their overall efficacy in AF prevention [236,237,238]. Moreover, insulin use has been linked to an increased risk of new-onset AF in patients with T2DM, likely due to hypoglycemic episodes that trigger sympathetic activation and the more advanced stage of DM in these individuals [239]. Similarly, sulfonylureas are also associated with a significantly increased risk of new-onset AF [240,241]. Moving to more novel antidiabetic agents, a metanalysis of six clinical trials with 5250 DM patients showed that dipeptidyl peptidase-4 (DPP-4) inhibitors did not have any significant impact on AF risk, and in fact, increased the risk of atrial flutter [242]. SGLT2 inhibitors and GLP1 RAs are antidiabetic agents with potential antiarrhythmic effects. These drugs have demonstrated unique cardio–renal–metabolic benefits [243,244,245] with emerging evidence indicating their effectiveness in preventing AF incidence or recurrence, irrespective of baseline diabetes status [20,164,165].
Of note, while accumulating evidence suggests that certain glucose-lowering therapies may modulate AF risk, it is important to recognize that most large-scale cardiovascular outcome trials (CVOTs), to date, were not designed with arrhythmia endpoints as primary outcomes. Instead, AF incidence was typically captured as an exploratory or post hoc finding, limiting the strength of mechanistic and clinical inferences. For instance, the DECLARE-TIMI 58 trial observed fewer AF events in patients receiving dapagliflozin compared to placebo [193]; however, AF was not a prespecified endpoint, and systematic rhythm monitoring was lacking. In this context, a 2024 meta-analysis by Xu et al. [246], encompassing 32 randomized placebo-controlled trials and over 60,000 patients with T2DM, provides more targeted insight. The study demonstrated a statistically significant reduction in the risk of atrial arrhythmias (RR: 0.86; 95% CI: 0.74–0.99; p = 0.04) and atrial fibrillation/flutter (RR: 0.85; 95% CI: 0.74–0.99; p = 0.03) with SGLT2 inhibitor therapy—particularly among individuals with elevated cardiovascular risk and prolonged follow-up. Notably, the analysis did not show significant benefit for ventricular arrhythmias or bradyarrhythmias, underscoring the atrial-specific benefit of these agents [246]. Nonetheless, even this meta-analysis relies on heterogeneous trials with varying definitions, durations, and arrhythmia ascertainment methods. Therefore, ongoing prospective trials such as EMPA-AF (NCT04583813) and DAPA-AF (NCT05174052), which are explicitly designed to assess arrhythmic endpoints, will be instrumental in clarifying the rhythm-modifying potential of SGLT2 inhibitors and guiding evidence-based clinical decision-making in diabetes-associated AF.
To date, various studies have demonstrated that T2DM is associated with a reduced immediate success rate of cardioversion, as well as a decreased likelihood of maintaining sinus rhythm. In fact, T2DM has been identified as an independent risk factor for cardioversion failure within 30 days [247,248,249]. Similarly, animal studies suggest that antiarrhythmic drugs may be less effective in patients with T2DM; however, clinical evidence supporting this observation remains limited. Indeed, a single-center study reported no significant difference in cardioversion success rates between individuals with and without diabetes [250]. Regarding specific drug classes, T2DM did not appear to affect the efficacy of propafenone in achieving cardioversion, while dronedarone use was associated with a longer AF-free period [251,252].
Percutaneous catheter ablation is a well-established treatment for AF and has demonstrated effectiveness in patients with DM. Early intervention with this technique holds promise in attenuating the progression of atrial cardiomyopathy, provided the procedure is conducted in the early stages of the disease and achieves complete suppression of AF [253]. Some reports suggest that catheter ablation may be less effective in individuals with T2DM compared to those without, possibly due to the greater extent of atrial fibrosis commonly observed in this population [254]. Hence, targeting these fibrotic areas that contribute to an arrhythmogenic substrate may translate into improved survival free from AF recurrences. Indeed, low-voltage area (LVA)-guided ablation targeting LVAs, which represent atria scars, identified via high-density mapping, have shown to significantly reduced AF recurrences compared to conventional pulmonary vein isolation (PVI) [255]. Further, the use of late gadolinium enhancement cardiac magnetic resonance (LGE-CMR) to quantify atrial fibrosis may enhance the efficacy of fibrosis-guided ablation strategies, though further validation is required [50]. Of note, these approaches align with the growing emphasis on personalized, substrate-based therapeutic strategies in DM patients.
To further support the efficacy of catheter ablation in T2DM individuals, the combined use of SGLT2 inhibitors and GLP-1 RAs may synergistically attenuate AF burden by inhibiting the progression of DM-related atrial cardiomyopathy through complementary pathways. Both drug categories reduce oxidative stress and inflammation, mitigate neurohormonal activation, reduce pro-fibrotic signaling, provide metabolic efficiency, and improve endothelial function [20,164,165]. Furthermore, SGLT2 inhibitors’ diuretic effects [256] and GLP-1RAs’ impact on cardiac hypertrophy [257] reduce atrial wall stress, addressing mechanical drivers of atrial remodeling. By targeting multiple facets of atrial cardiomyopathy, the combination of these agents offers a comprehensive strategy for preventing post-ablation AF recurrence in individuals with diabetes. However, future clinical studies need to be conducted to determine whether the pathophysiological basis of their synergistic effects translates into a documented reduction in AF occurrence after catheter ablation.
Regarding cardiovascular implantable electronic devices (CIEDs), although their role in AF prevention may be limited, their rhythm-monitoring capabilities provide invaluable insights into the management of AF. In patients with CIEDs and an underlying AF substrate, a progressive decline in atrial electrogram amplitudes may indicate the development of atrial cardiomyopathy, imposing the importance of closer monitoring and strict managing of risk factors. Of note, DM has a high predictive ability of AF (OR 2.24, 95% CI 1.20–4.19, p = 0.011) for CIED-patients [258].
8. Future Directions and Knowledge Gaps
Despite significant advances in the management of diabetes-associated AF, there is an emerging need for effective treatment options capable of restoring and maintaining sinus rhythm in affected individuals. To achieve this goal, extensive research is currently focused on identifying previously unrecognized molecular mechanisms that can enhance our knowledge for the development of AF and permit the identification of novel therapeutic targets.
Classic antiarrhythmic drugs currently employed in AF-management are far from being ideal, and their already limited effectiveness in suppressing AF is further reduced in the presence of DM. Moreover, these agents raise safety concerns, and individuals with diabetes may face a heightened risk of adverse effects due to often concomitant QTc prolongation, coronary artery disease, and renal impairment [259].
Recent progress in elucidating the molecular pathophysiological links between DM and AF have paved the way for the development of targeted antiarrhythmic therapies (Table 1). These emerging strategies involve the modulation of previously overlooked ion channels, the inhibition of AF-related remodeling processes, and the targeting of specific molecular events implicated in AF generation. For these approaches to be applicable in clinical practice, they should exhibit high affinity for the atrial myocardium, while posing minimal proarrhythmic risk, avoiding non-cardiac adverse effects, supporting chronic administration, and preserving key homeostatic processes. To overcome these challenges, novel approaches, such as multispecific drugs and lipid nanoparticle-based delivery systems, represent exciting avenues; however, these technologies remain in early preclinical stages and face significant translational hurdles [50,260]. Furthermore, a broader use of omics technologies, such as genomics, transcriptomics, proteomics, and metabolomics, can uncover novel biomarkers and potential therapeutic targets, paving the way for personalized approaches tailored to each patient’s molecular profile [261]. For instance, it is conceivable that blood-based gene expression profiling could be used to screen candidates for catheter ablation, indicating those who are at lower risk of post-ablation AF.

Table 1.
Summary of promising drugs and investigational compounds for the treatment of diabetes-associated atrial fibrillation.
In addition, SGLT2is and GLP-1RAs have emerged as potent therapeutic agents that extend their benefits beyond glycemic control. The ability of SGLT2is and GLP-1RAs to modulate multiple molecular pathways involved in atrial cardiomyopathy presents significant implications for the management of diabetes-associated AF. To definitively establish their efficacy in reducing the risk of AF in patients with diabetes, future research should prioritize on conducting large-scale RCTs with predefined AF endpoints. These studies should also align with the growing emphasis on personalized treatment and aim to address current heterogeneities by standardizing population characteristics, follow-up durations, and the specific SGLT2is and GLP-1RAs used. Furthermore, the precise role of these agents in preventing post-operative AF has yet to be determined. An additional key area for further investigation is whether SGLT2is and GLP-1 RAs can synergistically reduce the risk of diabetes-associated AF.
Regarding non-pharmacological antiarrhythmic strategies, catheter ablation appears to be less effective in diabetes-associated AF, primarily due to the presence of extensive atrial fibrosis. Identifying and targeting DM-induced fibrotic regions, responsible for creating an arrhythmogenic substrate, and performing ablation beyond the pulmonary veins, may improve outcomes and reduce AF recurrence in individuals with diabetes. These advancements underscore the importance of refining patient selection criteria and incorporating low-voltage mapping alongside advanced imaging techniques, such as LGE-CMR, into standardized ablation protocols. However, to achieve better clinical outcomes, ongoing refinements are required. For instance, while electro-anatomical mapping provides surrogate markers such as LVAs, these measures correlate inconsistently with histological findings and lack specificity for scar tissue, thereby limiting the efficacy of LVA-guided ablation. Similarly, LGE-CMR lacks standardization and sufficient spatial resolution to accurately quantify the extent of atrial fibrosis. Moreover, the high cost and limited availability of specialized centers and trained personnel restrict the accessibility of catheter ablation for many symptomatic AF patients worldwide. Lastly, it is important to note that catheter ablation does not address the underlying atrial cardiomyopathy that contributes to AF development.
Refining these aforementioned approaches and bridging existing knowledge gaps will require collaborative efforts across basic, translational, and clinical research domains.
9. Conclusions
The escalating global burden of both DM and AF has brought renewed focus to their complex, bidirectional interplay—an intersection now recognized as a critical frontier in cardiovascular research and clinical practice. In this review, we delineated the multifaceted pathophysiological mechanisms by which diabetes fosters an arrhythmogenic atrial substrate and highlighted emerging molecular targets and innovative rhythm control strategies poised to transform therapeutic paradigms.
Moving forward, the management of diabetes-associated AF demands a paradigm shift toward integrative and precision-guided approaches. This will necessitate the elucidation of targetable molecular pathways, the clinical translation of novel technologies—such as microRNA therapeutics, lipid nanoparticle-based drug delivery, and multi-omics biomarker discovery—and the refinement of diagnostic tools like low-voltage area (LVA) mapping and fibrosis quantification.
To establish the clinical efficacy of these strategies, robust validation through well-powered, multicenter randomized controlled trials is imperative. Ultimately, by closing current mechanistic gaps and embracing translational innovation, the field can advance toward a more tailored, disease-modifying framework for rhythm control—one that not only attenuates AF burden in patients with diabetes but also improves long-term cardiovascular outcomes at a population level.
Author Contributions
K.G.: conceptualization, methodology, investigation, visualization, writing—original draft, writing—review and editing,. P.K.: conceptualization, methodology, investigation, project administration, writing—original draft, writing—review and editing. K.P.: writing—review and editing. P.T.: writing—review and editing. D.P.: writing—review and editing. E.K.: writing—review and editing. B.F.: writing—review and editing. A.P.A.: writing—review and editing. N.F.: conceptualization, methodology, investigation, writing—review and editing, validation, supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors for its design or conduct.
Data Availability Statement
All data generated in this research is included within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Levy, D.; Vaziri, S.M.; D’Agostino, R.B.; Belanger, A.J.; Wolf, P.A. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Study. JAMA 1994, 271, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.; Zhou, J.; Veang, T.; Lin, Q.; Liu, Q. Global, regional, and national burden of atrial fibrillation and atrial flutter from 1990 to 2021: Sex differences and global burden projections to 2046—A systematic analysis of the Global Burden of Disease Study 2021. Europace 2025, 27, euaf027. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.Y.; Kotalczyk, A.; Boriani, G.; Marin, F.; Blomström-Lundqvist, C.; Potpara, T.S.; Fauchier, L.; Lip, G.Y.H.; ESC-EHRA EORP-AF Long-Term General Registry Investigators. Impact of diabetes on the management and outcomes in atrial fibrillation: An analysis from the ESC-EHRA EORP-AF Long-Term General Registry. Eur. J. Intern. Med. 2022, 103, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Ugowe, F.E.; Jackson, L.R.; Thomas, K.L. Atrial fibrillation and diabetes mellitus. Circ. Arrhythmia Electrophysiol. 2019, 12, e007351. [Google Scholar] [CrossRef] [PubMed]
- Dublin, S.; Glazer, N.L.; Smith, N.L.; Psaty, B.M.; Lumley, T.; Wiggins, K.L.; Page, R.L.; Heckbert, S.R. Diabetes mellitus, glycemic control, and risk of atrial fibrillation. J. Gen. Intern. Med. 2010, 25, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Dahlqvist, S.; Rosengren, A.; Gudbjörnsdottir, S.; Pivodic, A.; Wedel, H.; Kosiborod, M.; Svensson, A.M.; Lind, M. Risk of atrial fibrillation in people with type 1 diabetes compared with matched controls from the general population: A prospective case-control study. Lancet Diabetes Endocrinol. 2017, 5, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Proietti, M.; Romiti, G.F.; Basili, S. The case of diabetes mellitus and atrial fibrillation: Underlining the importance of non-cardiovascular comorbidities. Eur. J. Intern. Med. 2022, 103, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Echouffo-Tcheugui, J.B.; Shrader, P.; Thomas, L.; Gersh, B.J.; Kowey, P.R.; Mahaffey, K.W.; Singer, D.E.; Hylek, E.M.; Go, A.S.; Peterson, E.D.; et al. Care Patterns and Outcomes in Atrial Fibrillation Patients With and Without Diabetes: ORBIT-AF Registry. J. Am. Coll. Cardiol. 2017, 70, 1325–1335. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.C.; Yang, Y.Y.; Chuang, S.L.; Yu, C.C.; Lin, L.Y. Higher long-term visit-to-visit glycemic variability predicts new-onset atrial fibrillation in patients with diabetes mellitus. Cardiovasc. Diabetol. 2021, 20, 148. [Google Scholar] [CrossRef] [PubMed]
- Qi, W.; Zhang, N.; Korantzopoulos, P.; Letsas, K.P.; Cheng, M.; Di, F.; Tse, G.; Liu, T.; Li, G. Serum Glycated Hemoglobin Level as a Predictor of Atrial Fibrillation: A Systematic Review with Meta-analysis and Meta-regression. PLoS ONE 2017, 12, e0170955. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Pamporis, K.; Siontis, K.C.; Theofilis, P.; Samaras, A.; Patoulias, D.; Stachteas, P.; Karagiannidis, E.; Stavropoulos, G.; Tzikas, A.; et al. Major clinical outcomes in symptomatic vs. asymptomatic atrial fibrillation: A meta-analysis. Eur. Heart J. 2025, 46, 1189–1202. [Google Scholar] [CrossRef] [PubMed]
- Pamporis, K.; Karakasis, P.; Sagris, M.; Theofilis, P.; Milaras, N.; Pantelidaki, A.; Mourouzis, I.; Fragakis, N.; Vlachos, K.; Kordalis, A.; et al. Prevalence of asymptomatic atrial fibrillation and risk factors associated with asymptomatic status: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2025, zwaf138. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Theofilis, P.; Sagris, M.; Pamporis, K.; Stachteas, P.; Sidiropoulos, G.; Vlachakis, P.K.; Patoulias, D.; Antoniadis, A.P.; Fragakis, N. Artificial Intelligence in Atrial Fibrillation: From Early Detection to Precision Therapy. J. Clin. Med. 2025, 14, 2627. [Google Scholar] [CrossRef] [PubMed]
- Creta, A.; Providência, R.; Adragão, P.; de Asmundis, C.; Chun, J.; Chierchia, G.; Defaye, P.; Schmidt, B.; Anselme, F.; Finlay, M.; et al. Impact of type-2 diabetes mellitus on the outcomes of catheter ablation of atrial fibrillation (European observational multicentre study). Am. J. Cardiol. 2020, 125, 901–906. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Truong, T.; Black-Maier, E.; Green, C.; Campbell, K.B.; Barnett, A.S.; Febre, J.; Loring, Z.; Al-Khatib, S.M.; Atwater, B.D.; et al. Catheter ablation of atrial fibrillation in patients with diabetes mellitus. Heart Rhythm O2 2020, 1, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Luo, D.; Yang, G.; Huang, W.; Tang, Y.; Xu, B.; He, G.; Yang, Y.; He, J.; Sun, H.; et al. The Effect of Non-insulin-based Insulin Resistance Indices on the Prediction of Recurrence in Patients with Atrial Fibrillation Undergoing Radiofrequency Catheter Ablation. Cardiovasc. Diabetol. 2024, 23, 291. [Google Scholar] [CrossRef] [PubMed]
- Manolis, A.A.; Manolis, T.A.; Melita, H.; Manolis, A.S. Sodium-glucose cotransporter type 2 inhibitors and cardiac arrhythmias. Trends Cardiovasc. Med. 2023, 33, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Stoll, L.; Lo, J.C. GLP-1 Receptor Agonists, the Holy Grail Preventing Atrial Fibrillation in Patients With T2D? JACC Basic Transl. Sci. 2023, 8, 937–938. [Google Scholar] [CrossRef] [PubMed]
- Stachteas, P.; Nasoufidou, A.; Karagiannidis, E.; Patoulias, D.; Karakasis, P.; Alexiou, S.; Samaras, A.; Zormpas, G.; Stavropoulos, G.; Tsalikakis, D.; et al. The Role of Sodium Glucose Co-Transporter 2 Inhibitors in Atrial Fibrillation: A Comprehensive Review. J. Clin. Med. 2024, 13, 5408. [Google Scholar] [CrossRef] [PubMed]
- Gumprecht, J.; Lip, G.Y.H.; Sokal, A.; Średniawa, B.; Mitręga, K.; Stokwiszewski, J.; Wierucki, Ł.; Rajca, A.; Rutkowski, M.; Zdrojewski, T.; et al. Relationship between diabetes mellitus and atrial fibrillation prevalence in the Polish population: A report from the Non-invasive Monitoring for Early Detection of Atrial Fibrillation (NOMED-AF) prospective cross-sectional observational study. Cardiovasc. Diabetol. 2021, 20, 128. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.R.; Choi, J.; Choi, E.K.; Lee, H.; Han, M.; Ahn, H.J.; Kwon, S.; Lee, S.W.; Han, K.D.; Oh, S.; et al. Early rhythm control on diabetes-related complications and mortality in patients with type 2 diabetes mellitus and atrial fibrillation. Diabetes Res. Clin. Pract. 2023, 206, 111020. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Tzeis, S.; Pamporis, K.; Schuermans, A.; Theofilis, P.; Milaras, N.; Tsiachris, D.; Efremidis, M.; Antoniadis, A.P.; Fragakis, N. Impact of Catheter Ablation Timing According to Duration of Atrial Fibrillation History on Arrhythmia Recurrences and Clinical Outcomes: A Meta-Analysis. EP Europace 2025, 27, euaf110. [Google Scholar] [CrossRef] [PubMed]
- Bode, D.; Pronto, J.R.D.; Schiattarella, G.G.; Voigt, N. Metabolic remodelling in atrial fibrillation: Manifestations, mechanisms and clinical implications. Nat. Rev. Cardiol. 2024, 21, 682–700. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, P.; Nattel, S.; Nanthakumar, K. Linking cellular energy state to atrial fibrillation pathogenesis: Potential role of adenosine monophosphate–activated protein kinase. Heart Rhythm 2020, 17, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; Jin, L.; Gong, H.; Zheng, Q. Electro-metabolic coupling in atrial fibrillation: A deeper understanding of the metabolic driver. Biomed. Pharmacother. 2024, 180, 117536. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Bai, F.; Liu, N.; Ouyang, F.; Liu, Q. The Warburg effect: A new insight into atrial fibrillation. Clin. Chim. Acta 2019, 499, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.H.; Ning, Z.H.; Xie, Z.; Ou, Y.; Yang, J.Y.; Liu, Y.X.; Huang, H.; Tang, H.F.; Jiang, Z.S.; Hu, H.J. SIRT3/AMPK Signaling Pathway Regulates Lipid Metabolism and Improves Vulnerability to Atrial Fibrillation in Dahl Salt-sensitive Rats. Am. J. Hypertens. 2024, 37, 901–908. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Gao, F.; Gong, H.; Fu, Y.; Liu, B.; Qin, X.; Zheng, Q. Intermittent fasting attenuates obesity-related atrial fibrillation via SIRT3-mediated insulin resistance mitigation. Biochim. Biophys. Acta Mol. Basis Dis. 2023, 1869, 166638. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, K.; Nzirorera, C.; Kienesberger, P.C. Lipid metabolism and signaling in cardiac lipotoxicity. Biochim. Biophys. Acta 2016, 1861, 1513–1524. [Google Scholar] [CrossRef] [PubMed]
- Trappe, K.; Thomas, D.; Bikou, O.; Kelemen, K.; Lugenbiel, P.; Voss, F.; Becker, R.; Katus, H.A.; Bauer, A. Suppression of persistent atrial fibrillation by genetic knockdown of caspase 3: A pre-clinical pilot study. Eur. Heart J. 2013, 34, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Scott, L.; Li, N.; Dobrev, D. Role of inflammatory signaling in atrial fibrillation. Int. J. Cardiol. 2019, 287, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Harada, M.; Van Wagoner, D.R.; Nattel, S. Role of inflammation in atrial fibrillation pathophysiology and management. Circ. J. 2015, 79, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Yamashita, T.; Sekiguchi, A.; Tsuneda, T.; Sagara, K.; Takamura, M.; Kaneko, S.; Aizawa, T.; Fu, L.T. AGEs-RAGE system mediates atrial structural remodeling in the diabetic rat. J. Cardiovasc. Electrophysiol. 2008, 19, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Goldin, A.; Beckman, J.A.; Schmidt, A.M.; Creager, M.A. Advanced glycation end products. Circulation 2006, 114, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Cha, S.J.; Park, J.H.; Shin, J.H.; Lim, Y.H.; Park, H.C.; Shin, J.; Kim, C.K.; Park, J.K. Association between Insulin Resistance and Risk of Atrial Fibrillation in Non-diabetics. Eur. J. Prev. Cardiol. 2020, 27, 1934–1941. [Google Scholar] [CrossRef] [PubMed]
- Fontes, J.D.; Lyass, A.; Massaro, J.M.; Rienstra, M.; Dallmeier, D.; Schnabel, R.B.; Wang, T.J.; Vasan, R.S.; Lubitz, S.A.; Magnani, J.W.; et al. Insulin resistance and atrial fibrillation (from the Framingham Heart Study). Am. J. Cardiol. 2012, 109, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Garg, P.K.; Biggs, M.L.; Kaplan, R.; Kizer, J.R.; Heckbert, S.R.; Mukamal, K.J. Fasting and Post-glucose Load Measures of Insulin Resistance and Risk of Incident Atrial Fibrillation: The Cardiovascular Health Study. Nutr. Metab. Cardiovasc. 2018, 28, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.H.; Chang, G.J.; Lai, Y.J.; Chen, W.J.; Chang, S.H.; Hung, L.M.; Kuo, C.T.; Yeh, Y.H. Atrial fibrillation and its arrhythmogenesis associated with insulin resistance. Cardiovasc. Diabetol. 2019, 18, 125. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Lip, G.Y.H.; Apostolakis, S. Inflammation in atrial fibrillation. J. Am. Coll. Cardiol. 2012, 60, 2263–2270. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Mondragón, R.; Galindo, C.A.; Avila, G. Role of TGF-beta on cardiac structural and electrical remodeling. Vasc. Health Risk Manag. 2008, 4, 1289–1300. [Google Scholar] [CrossRef] [PubMed]
- Ziolo, M.T.; Mohler, P.J. Defining the role of oxidative stress in atrial fibrillation and diabetes. J. Cardiovasc. Electrophysiol. 2015, 26, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Yao, C.; Veleva, T.; Scott, L., Jr.; Cao, S.; Li, L.; Chen, G.; Jeyabal, P.; Pan, X.; Alsina, K.M.; Abu-Taha, I.; et al. Enhanced Cardiomyocyte NLRP3 Inflammasome Signaling Promotes Atrial Fibrillation. Circulation 2018, 138, 2227–2242. [Google Scholar] [CrossRef] [PubMed]
- Hajer, D.R.; van Haeften, T.W.; Visseren, F.L.J. Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur. Heart J. 2008, 29, 2959–2971. [Google Scholar] [CrossRef] [PubMed]
- Xie, W.; Santulli, G.; Reiken, S.R.; Yuan, Q.; Osborne, B.W.; Chen, B.X.; Marks, A.R. Mitochondrial oxidative stress promotes atrial fibrillation. Sci. Rep. 2015, 5, 11427. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Zhao, W.; Thomson, J.K.; Gao, X.; DeMarco, D.M.; Carrillo, E.; Chen, B.; Wu, X.; Ginsburg, K.S.; Bakhos, M.; et al. Stress Signaling JNK2 Crosstalk With CaMKII Underlies Enhanced Atrial Arrhythmogenesis. Circ. Res. 2018, 122, 821–835. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Bare, D.J.; DeSantiago, J.; Zhao, W.; Mei, Y.; Chen, Z.; Ginsburg, K.; Solaro, R.J.; Wolska, B.M.; Bers, D.M.; et al. JNK2, a Newly-Identified SERCA2 Enhancer, Augments an Arrhythmic [Ca2+] SR Leak-Load Relationship. Circ. Res. 2021, 128, 455–470. [Google Scholar] [CrossRef] [PubMed]
- Biernacka, A.; Cavalera, M.; Wang, J.; Russo, I.; Shinde, A.; Kong, P.; Gonzalez-Quesada, C.; Rai, V.; Dobaczewski, M.; Lee, D.W.; et al. Smad3 Signaling Promotes Fibrosis While Preserving Cardiac and Aortic Geometry in Obese Diabetic Mice. Circ. Heart Fail. 2015, 8, 788–798. [Google Scholar] [CrossRef] [PubMed]
- Makary, S.; Voigt, N.; Maguy, A.; Wakili, R.; Nishida, K.; Harada, M.; Dobrev, D.; Nattel, S. Differential protein kinase C isoform regulation and increased constitutive activity of acetylcholine-regulated potassium channels in atrial remodeling. Circ. Res. 2011, 109, 1031–1043. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Theofilis, P.; Vlachakis, P.K.; Korantzopoulos, P.; Patoulias, D.; Antoniadis, A.P.; Fragakis, N. Atrial fibrosis in Atrial Fibrillation: Mechanistic Insights, Diagnostic Challenges, and Emerging Therapeutic Targets. Int. J. Mol. Sci. 2024, 26, 209. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Vlachakis, P.K.; Theofilis, P.; Ktenopoulos, N.; Patoulias, D.; Fyntanidou, B.; Antoniadis, A.P.; Fragakis, N. Atrial Cardiomyopathy in Atrial Fibrillation: A Multimodal Diagnostic Framework. Diagnostics 2025, 15, 1207. [Google Scholar] [CrossRef] [PubMed]
- Polyakova, V.; Miyagawa, S.; Szalay, Z.; Risteli, J.; Kostin, S. Atrial extracellular matrix remodelling in patients with atrial fibrillation. J. Cell Mol. Med. 2008, 12, 189–208. [Google Scholar] [CrossRef] [PubMed]
- Russo, I.; Frangogiannis, N.G. Diabetes-associated cardiac fibrosis: Cellular effectors, molecular mechanisms and therapeutic opportunities. J. Mol. Cell Cardiol. 2016, 90, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Abe, I.; Teshima, Y.; Kondo, H.; Kaku, H.; Kira, S.; Ikebe, Y.; Saito, S.; Fukui, A.; Shinohara, T.; Yufu, K.; et al. Association of Fibrotic Remodeling and Cytokines/chemokines Content in Epicardial Adipose Tissue with Atrial Myocardial Fibrosis in Patients with Atrial Fibrillation. Heart Rhythm 2018, 15, 1717–1727. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Fu, H.; Li, J.; Yang, W.; Cheng, L.; Liu, T. Hyperglycemia aggravates atrial interstitial fibrosis, ionic remodeling and vulnerability to atrial fibrillation in diabetic rabbits. Anadolu Kardiyol Derg 2012, 12, 543. Available online: https://link.gale.com/apps/doc/A352493933/AONE?u=anon~2d8b3dec&sid=googleScholar&xid=f5ae61e2 (accessed on 1 July 2025). [CrossRef] [PubMed]
- Watanabe, M.; Yokoshiki, H.; Mitsuyama, H.; Mizukami, K.; Ono, T.; Tsutsui, H. Conduction and refractory disorders in the diabetic atrium. Am. J. Physiol. Heart Circ. Physiol. 2012, 303, H86. [Google Scholar] [CrossRef] [PubMed]
- Qian, L.; Liu, X.; Li, X.; Yang, F.; Wang, R. Effects of Electrical Remodeling on Atrial Fibrillation in Diabetes Mellitus. Rev. Cardiovasc. Med. 2023, 24, 3. [Google Scholar] [CrossRef] [PubMed]
- Polina, I.; Jansen, H.J.; Li, T.; Moghtadaei, M.; Bohne, L.J.; Liu, Y.; Krishnaswamy, P.; Egom, E.E.; Belke, D.D.; Rafferty, S.A.; et al. Loss of insulin signaling may contribute to atrial fibrillation and atrial electrical remodeling in type 1 diabetes. Proc. Natl. Acad. Sci. USA 2020, 117, 7990–8000. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Jiang, Y.; Xue, G.; Yuan, Y.; Zhu, H.; Zhan, L.; Zhuang, Y.; Huang, Q.; Shi, L.; Zhao, Y.; et al. Increase of late sodium current contributes to enhanced susceptibility to atrial fibrillation in diabetic mice. Eur. J. Pharmacol. 2019, 857, 172444. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Belardinelli, L. Basal late sodium current is a significant contributor to the duration of action potential of guinea pig ventricular myocytes. Physiol. Rep. 2017, 5, e13295. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Liu, H.H.; Zhang, L.; Zhang, X.L.; Zhang, J.; Li, F.; Zhao, N.; Zhang, Z.Y.; Kong, Q.; Liu, X.Y.; et al. Advanced glycation end products downregulate connexin 43 and connexin 40 in diabetic atrial myocytes via the AMPK pathway. Diabetes Metab. Syndr. Obes. 2023, 16, 3045–3056. [Google Scholar] [CrossRef] [PubMed]
- De Vos, C.B.; Weijs, B.; Crijns, H.J.; Cheriex, E.C.; Palmans, A.; Habets, J.; Prins, M.H.; Pisters, R.; Nieuwlaat, R.; Tieleman, R.G. Atrial tissue Doppler imaging for prediction of new-onset atrial fibrillation. Heart 2009, 95, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Demir, K.; Avci, A.; Kaya, Z.; Marakoglu, K.; Ceylan, E.; Yilmaz, A.; Ersecgin, A.; Armutlukuyu, M.; Altunkeser, B.B. Assessment of atrial electromechanical delay and P-wave dispersion in patients with type 2 diabetes mellitus. J. Cardiol. 2016, 67, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Rudokas, M.W.; McKay, M.; Toksoy, Z.; Eisen, J.N.; Bögner, M.; Young, L.H.; Akar, F.G. Mitochondrial network remodeling of the diabetic heart: Implications to ischemia related cardiac dysfunction. Cardiovasc. Diabetol. 2024, 23, 261. [Google Scholar] [CrossRef] [PubMed]
- Fossier, L.; Panel, M.; Butruille, L.; Colombani, S.; Azria, L.; Woitrain, E.; Decoin, R.; Torrente, A.G.; Thireau, J.; Lacampagne, A.; et al. Enhanced Mitochondrial Calcium Uptake Suppresses Atrial Fibrillation Associated With Metabolic Syndrome. J. Am. Coll. Cardiol. 2022, 80, 2205–2219. [Google Scholar] [CrossRef] [PubMed]
- Shan, J.; Xie, W.; Betzenhauser, M.; Reiken, S.; Chen, B.X.; Wronska, A.; Marks, A.R. Calcium leak through ryanodine receptors leads to atrial fibrillation in 3 mouse models of catecholaminergic polymorphic ventricular tachycardia. Circ. Res. 2012, 111, 708–717. [Google Scholar] [CrossRef] [PubMed]
- Jeganathan, J.; Saraf, R.; Mahmood, F.; Pal, A.; Bhasin, M.K.; Huang, T. Mitochondrial Dysfunction in Atrial Tissue of Patients Developing Postoperative Atrial Fibrillation. Ann. Thorac. Surg. 2017, 104, 1547–1555. [Google Scholar] [CrossRef] [PubMed]
- Bugger, H.; Abel, E.D. Mitochondria in the diabetic heart. Cardiovasc. Res. 2010, 88, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Tadic, M.; Cuspidi, C. Type 2 diabetes mellitus and atrial fibrillation: From mechanisms to clinical practice. Arch. Cardiovasc. Dis. 2015, 108, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Solhjoo, S.; Millare, B.; Plank, G.; Abraham, M.R.; Cortassa, S.; Trayanova, N.; O’Rourke, B. Effects of regional mitochondrial depolarization on electrical propagation: Implications for arrhythmogenesis. Circ. Arrhythm. Electrophysiol. 2014, 7, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Mason, F.E.; Pronto, J.R.D.; Alhussini, K.; Alhussini, K.; Maack, C.; Voigt, N. Cellular and mitochondrial mechanisms of atrial fibrillation. Basic. Res. Cardiol. 2020, 115, 72. [Google Scholar] [CrossRef] [PubMed]
- Kuehl, M.; Stevens, M.J. Cardiovascular autonomic neuropathies as complications of diabetes mellitus. Nat. Rev. Endocrinol. 2012, 8, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.W.; Lee, T.I.; Lin, Y.K.; Chen, Y.C.; Kao, Y.H.; Chen, Y.J. Effect of antidiabetic drugs on the risk of atrial fibrillation: Mechanistic insights from clinical evidence and translational studies. Cell Mol. Life Sci. 2021, 78, 923–934. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-Almorós, A.; Casado Cerrada, J.; Álvarez-Sala Walther, L.-A.; Méndez Bailón, M.; Lorenzo González, Ó. Atrial Fibrillation and Diabetes Mellitus: Dangerous Liaisons or Innocent Bystanders? J. Clin. Med. 2023, 12, 2868. [Google Scholar] [CrossRef] [PubMed]
- Karam, B.S.; Chavez-Moreno, A.; Koh, W.; Akar, J.G.; Akar, F.G. Oxidative stress and inflammation as central mediators of atrial fibrillation in obesity and diabetes. Cardiovasc. Diabetol. 2017, 16, 120. [Google Scholar] [CrossRef] [PubMed]
- Ajoolabady, A.; Nattel, S.; Lip, G.Y.H.; Ren, J. Inflammasome Signaling in Atrial Fibrillation: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2022, 79, 2349–2366. [Google Scholar] [CrossRef] [PubMed]
- Niskala, A.; Heijman, J.; Dobrev, D.; Jespersen, T.; Saljic, A. Targeting the NLRP3 inflammasome signaling for the management of atrial fibrillation. Br. J. Pharmacol. 2024, 181, 4939–4957. [Google Scholar] [CrossRef] [PubMed]
- Deftereos, S.G.; Beerkens, F.J.; Shah, B.; Giannopoulos, G.; Vrachatis, D.A.; Giotaki, S.G.; Siasos, G.; Nicolas, J.; Arnott, C.; Patel, S.; et al. Colchicine in Cardiovascular Disease: In-Depth Review. Circulation 2022, 145, 61–78. [Google Scholar] [CrossRef] [PubMed]
- Saljic, A.; Heijman, J.; Dobrev, D. Emerging Antiarrhythmic Drugs for Atrial Fibrillation. Int. J. Mol. Sci. 2022, 23, 4096. [Google Scholar] [CrossRef] [PubMed]
- Conen, D.; Ke Wang, M.; Popova, E.; Chan, M.T.V.; Landoni, G.; Cata, J.P.; Reimer, C.; McLean, S.R.; Srinathan, S.K.; Reyes, J.C.T.; et al. Effect of Colchicine on Perioperative Atrial Fibrillation and Myocardial Injury after Non-Cardiac Surgery in Patients Undergoing Major Thoracic Surgery (COP-AF): An International Randomised Trial. Lancet 2023, 402, 1627–1635. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef] [PubMed]
- Krisai, P.; Blum, S.; Schnabel, R.B.; Sticherling, C.; Kühne, M.; von Felten, S.; Ammann, P.; Pruvot, E.; Albert, C.M.; Conen, D.; et al. Canakinumab After Electrical Cardioversion in Patients With Persistent Atrial Fibrillation: A Pilot Randomized Trial. Circ. Arrhythm. Electrophysiol. 2020, 13, e008197. [Google Scholar] [CrossRef] [PubMed]
- Ye, T.; Zhang, C.; Wu, G.; Wan, W.; Liang, J.; Liu, X.; Liu, D.; Yang, B. Pinocembrin attenuates autonomic dysfunction and atrial fibrillation susceptibility via inhibition of the NF-κB/TNF-α pathway in a rat model of myocardial infarction. Int. Immunopharmacol. 2019, 77, 105926. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Xie, Q.; Hu, T.; Yao, Q.; Zhao, J.; Wu, Q.; Tang, Q. S100A8/A9 in Myocardial Infarction: A Promising Biomarker and Therapeutic Target. Front. Cell Dev. Biol. 2020, 8, 603902. [Google Scholar] [CrossRef] [PubMed]
- Jakobsson, G.; Papareddy, P.; Andersson, H.; Mulholland, M.; Bhongir, R.; Ljungcrantz, I.; Engelbertsen, D.; Björkbacka, H.; Nilsson, J.; Manea, A.; et al. Therapeutic S100A8/A9 Blockade Inhibits Myocardial and Systemic Inflammation and Mitigates Sepsis-Induced Myocardial Dysfunction. Crit. Care 2023, 27, 374. [Google Scholar] [CrossRef] [PubMed]
- Sweat, M.E.; Pu, W.T. Genetic and Molecular Underpinnings of Atrial Fibrillation. npj Cardiovasc. Health 2024, 1, 35. [Google Scholar] [CrossRef] [PubMed]
- Liaw, L.; Birk, D.E.; Ballas, C.B.; Whitsitt, J.S.; Davidson, J.M.; Hogan, B.L. Altered Wound Healing in Mice Lacking a Functional Osteopontin Gene (Spp1). J. Clin. Investig. 1998, 101, 1468–1478. [Google Scholar] [CrossRef] [PubMed]
- Momin, N.; Pabel, S.; Rudra, A.; Kumowski, N.; Lee, I.H.; Mentkowski, K.; Yamazoe, M.; Stengel, L.; Muse, C.G.; Seung, H.; et al. Therapeutic Spp1 Silencing in TREM2+ Cardiac Macrophages Suppresses Atrial Fibrillation. bioRxiv 2024. [Google Scholar] [CrossRef]
- Du, L.; Qin, M.; Yi, Y.; Chen, X.; Jiang, W.; Zhou, L.; Zhang, D.; Xu, K.; Yang, Y.; Li, C.; et al. Eplerenone Prevents Atrial Fibrosis via the TGF-β Signaling Pathway. Cardiology 2017, 138, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Takemoto, Y.; Ramirez, R.J.; Kaur, K.; Salvador-Montañés, O.; Ponce-Balbuena, D.; Ramos-Mondragón, R.; Ennis, S.R.; Guerrero-Serna, G.; Berenfeld, O.; Jalife, J. Eplerenone Reduces Atrial Fibrillation Burden Without Preventing Atrial Electrical Remodeling. J. Am. Coll. Cardiol. 2017, 70, 2893–2905. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, W.; Yang, B.; Han, W.; Dong, D.; Xue, J.; Li, B.; Yang, S.; Sheng, L. Effects of Cilazapril on Atrial Electrical, Structural and Functional Remodeling in Atrial Fibrillation Dogs. J. Electrocardiol. 2007, 40, 100.e1–100.e6. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, K.; Nakashima, H.; Urata, H.; Gondo, N.; Arakawa, K.; Saku, K. Effects of Angiotensin II Type 1 Receptor Antagonist on Electrical and Structural Remodeling in Atrial Fibrillation. J. Am. Coll. Cardiol. 2003, 41, 2197–2204. [Google Scholar] [CrossRef] [PubMed]
- Kapelios, C.J.; Murrow, J.R.; Nührenberg, T.G.; Montoro Lopez, M.N. Effect of Mineralocorticoid Receptor Antagonists on Cardiac Function in Patients with Heart Failure and Preserved Ejection Fraction: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Heart Fail. Rev. 2019, 24, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Patoulias, D.; Popovic, D.S.; Pamporis, K.; Theofilis, P.; Nasoufidou, A.; Stachteas, P.; Samaras, A.; Tzikas, A.; Giannakoulas, G.; et al. Effects of Mineralocorticoid Receptor Antagonists on New-Onset or Recurrent Atrial Fibrillation: A Bayesian and Frequentist Network Meta-Analysis of Randomized Trials. Curr. Probl. Cardiol. 2024, 49, 102742. [Google Scholar] [CrossRef] [PubMed]
- Pabon, M.A.; Filippatos, G.; Claggett, B.L.; Miao, M.Z.; Desai, A.S.; Jhund, P.S.; Henderson, A.; Brinker, M.; Schloemer, P.; Hofmeister, L.; et al. Finerenone Reduces New-Onset Atrial Fibrillation Across the Spectrum of Cardio-Kidney-Metabolic Syndrome: The FINE-HEART Pooled Analysis. J. Am. Coll. Cardiol. 2025, 85, 1649–1660. [Google Scholar] [CrossRef] [PubMed]
- Wolke, C.; Bukowska, A.; Goette, A.; Lendeckel, U. Redox Control of Cardiac Remodeling in Atrial Fibrillation. Biochim. Biophys. Acta 2015, 1850, 1555–1565. [Google Scholar] [CrossRef] [PubMed]
- Goette, A.; Bukowska, A.; Dobrev, D.; Pfeiffenberger, J.; Morawietz, H.; Strugala, D.; Wiswedel, I.; Röhl, F.W.; Wolke, C.; Bergmann, S.; et al. Acute Atrial Tachyarrhythmia Induces Angiotensin II type 1 Receptor-mediated Oxidative Stress and Microvascular Flow Abnormalities in the Ventricles. Eur. Heart J. 2009, 30, 1411–1420. [Google Scholar] [CrossRef] [PubMed]
- Paw, M.; Kusiak, A.A.; Nit, K.; Litewka, J.J.; Piejko, M.; Wnuk, D.; Sarna, M.; Fic, K.; Stopa, K.B.; Hammad, R.; et al. Hypoxia Enhances Anti-fibrotic Properties of Extracellular Vesicles Derived from HiPSCs via the MiR302b-3p/TGFβ/SMAD2 Axis. BMC Med. 2023, 21, 412. [Google Scholar] [CrossRef] [PubMed]
- Hai, Z.; Wu, Y.; Ning, Z. Salidroside Attenuates Atrial Fibrosis and Atrial Fibrillation Vulnerability Induced by Angiotensin-II through Inhibition of LOXL2-TGF-B1-Smad2/3 Pathway. Heliyon 2023, 9, e21220. [Google Scholar] [CrossRef] [PubMed]
- Bukowska, A.; Nikonova, Y.; Wolke, C.; Lendeckel, U.; Kockskämper, J.; Goette, A. Anti-Inflammatory Effects of Endothelin Receptor Blockade in Left Atrial Tissue of Spontaneously Hypertensive Rats. Int. J. Cardiol. Heart Vasc. 2022, 42, 101088. [Google Scholar] [CrossRef] [PubMed]
- Widyantoro, B.; Emoto, N.; Nakayama, K.; Anggrahini, D.W.; Adiarto, S.; Iwasa, N.; Yagi, K.; Miyagawa, K.; Rikitake, Y.; Suzuki, T.; et al. Endothelial cell-derived endothelin-1 promotes cardiac fibrosis in diabetic hearts through stimulation of endothelial-to-mesenchymal transition. Circulation 2010, 121, 2407–2418. [Google Scholar] [CrossRef] [PubMed]
- Ruf, L.; Bukowska, A.; Gardemann, A.; Goette, A. Coagulation Factor Xa Has No Effects on the Expression of PAR1, PAR2, and PAR4 and No Proinflammatory Effects on HL-1 Cells. Cells 2023, 12, 2849. [Google Scholar] [CrossRef] [PubMed]
- Bukowska, A.; Zacharias, I.; Weinert, S.; Skopp, K.; Hartmann, C.; Huth, C.; Goette, A. Coagulation factor Xa Induces an Inflammatory Signalling by Activation of Protease-activated Receptors in Human Atrial Tissue. Eur. J. Pharmacol. 2013, 718, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Bukowska, A.; Schild, L.; Bornfleth, P.; Peter, D.; Wiese-Rischke, C.; Gardemann, A.; Isermann, B.; Walles, T.; Goette, A. Activated Clotting Factor X Mediates Mitochondrial Alterations and Inflammatory Responses via Protease-activated Receptor Signaling in Alveolar Epithelial Cells. Eur. J. Pharmacol. 2020, 869, 172875. [Google Scholar] [CrossRef] [PubMed]
- Spronk, H.M.; De Jong, A.M.; Verheule, S.; De Boer, H.C.; Maass, A.H.; Lau, D.H.; Rienstra, M.; van Hunnik, A.; Kuiper, M.; Lumeij, S.; et al. Hypercoagulability Causes Atrial Fibrosis and Promotes Atrial Fibrillation. Eur. Heart J. 2017, 38, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Theofilis, P.; Milaras, N.; Vlachakis, P.K.; Patoulias, D.; Karamitsos, T.; Antoniadis, A.P.; Fragakis, N. Epigenetic Drivers of Atrial Fibrillation: Mechanisms, Biomarkers, and Therapeutic Targets. Int. J. Mol. Sci. 2025, 26, 5253. [Google Scholar] [CrossRef] [PubMed]
- Shan, H.; Zhang, Y.; Lu, Y.; Zhang, Y.; Pan, Z.; Cai, B.; Wang, N.; Li, X.; Feng, T.; Hong, Y.; et al. Downregulation of miR-133 and miR-590 Contributes to Nicotine-induced Atrial Remodelling in Canines. Cardiovasc. Res. 2009, 83, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yuan, B.; Xu, Y.; Zhou, N.; Zhang, R.; Lu, L.; Feng, Z. MiR-208b/miR-21 Promotes the Progression of Cardiac Fibrosis Through the Activation of the TGF-β1/Smad-3 Signaling Pathway: An in vitro and in vivo Study. Front. Cardiovasc. Med. 2022, 9, 924629. [Google Scholar] [CrossRef] [PubMed]
- Rubiś, P.; Totoń-Żurańska, J.; Kołton-Wróż, M.; Wołkow, P.; Pitera, E.; Wiśniowska-Śmiałek, S.; Dziewięcka, E.; Garlitski, A.; Podolec, P. Twelve-month kinetics of circulating fibrosis-linked microRNAs (miR-21, miR-29, miR-30, and miR-133a) and the relationship with extracellular matrix fibrosis in dilated cardiomyopathy. Arch. Med. Sci. 2019, 18, 480–488. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Afzal, J.; Vakrou, S.; Greenland, G.V.; Talbot, C.C., Jr.; Hebl, V.B.; Guan, Y.; Karmali, R.; Tardiff, J.C.; Leinwand, L.A.; et al. Differences in microRNA-29 and Pro-fibrotic Gene Expression in Mouse and Human Hypertrophic Cardiomyopathy. Front. Cardiovasc. Med. 2019, 6, 170. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, N.W.E.; Kawasaki, M.; Nariswari, F.A.; Fabrizi, B.; Neefs, J.; van der Made, I.; Wesselink, R.; van Boven, W.J.P.; Driessen, A.H.G.; Jongejan, A.; et al. MicroRNAs in atrial fibrillation target genes in structural remodelling. Cell Tissue Res. 2023, 394, 497–514. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, Y.; Han, J.; Li, Y.; Xie, C.; Xie, L.; Shi, J.; Zhang, J.; Yang, B.; Chen, D.; et al. Integrated analysis of microRNA and mRNA expression profiles in the left atrium of patients with nonvalvular paroxysmal atrial fibrillation: Role of miR-146b-5p in atrial fibrosis. Heart Rhythm 2015, 12, 1018–1026. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Hu, X.; Henning, R.H.; Brundel, B.J. Keeping up the balance: Role of HDACs in cardiac proteostasis and therapeutic implications for atrial fibrillation. Cardiovasc. Res. 2016, 109, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Song, S.; Zhang, R.; Mo, B.; Chen, L.; Liu, L.; Yu, Y.; Cao, W.; Fang, G.; Wan, Y.; Gu, Y.; et al. EZH2 as a novel therapeutic target for atrial fibrosis and atrial fibrillation. J. Mol. Cell Cardiol. 2019, 135, 119–133. [Google Scholar] [CrossRef] [PubMed]
- van Ouwerkerk, A.F.; Hall, A.W.; Kadow, Z.A.; Lazarevic, S.; Reyat, J.S.; Tucker, N.R.; Nadadur, R.D.; Bosada, F.M.; Bianchi, V.; Ellinor, P.T.; et al. Epigenetic and Transcriptional Networks Underlying Atrial Fibrillation. Circ. Res. 2020, 127, 34–50. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Chen, L.; Li, F.; Cao, Y.; Li, D.; Xiong, Q.; Ling, Z. Biomimetic nanoparticles loaded lutein functionalized by macrophage membrane for targeted amelioration pressure overload-induced cardiac fibrosis. Biomed. Pharmacother. 2023, 167, 115579. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.N.; Lee, S.Y.; Lee, S.; Youn, H.; Im, H.J. Lipid nanoparticles for delivery of RNA therapeutics: Current status and the role of in vivo imaging. Theranostics 2022, 12, 7509–7531. [Google Scholar] [CrossRef] [PubMed]
- Jardin, B.; Epstein, J.A. Emerging mRNA therapies for cardiac fibrosis. Am. J. Physiol. Cell Physiol. 2024, 326, C107–C111. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wakili, R.; Xiao, J.; Wu, C.T.; Luo, X.; Clauss, S.; Dawson, K.; Qi, X.; Naud, P.; Shi, Y.F.; et al. Detailed Characterization of MicroRNA Changes in a Canine Heart Failure Model: Relationship to Arrhythmogenic Structural Remodeling. J. Mol. Cell. Cardiol. 2014, 77, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Liu, Y.; Tu, D.; Liu, X.; Niu, S.; Suo, Y.; Liu, T.; Li, G.; Liu, C. Role of NLRP3-inflammasome/caspase-1/galectin-3 Pathway on Atrial Remodeling in Diabetic Rabbits. J. Cardiovasc. Transl. Res. 2020, 13, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Rao, F.; Lian, F.; Yang, H.; Kuang, S.; Wu, S.; Deng, C.; Xue, Y. Mechanism of electrical remodeling of atrial myocytes and its influence on susceptibility to atrial fibrillation in diabetic rats. Life Sci. 2019, 239, 116903. [Google Scholar] [CrossRef] [PubMed]
- Allessie, M.; Ausma, J.; Schotten, U. Electrical, contractile and structural remodeling during atrial fibrillation. Cardiovasc. Res. 2002, 54, 230–246. [Google Scholar] [CrossRef] [PubMed]
- Nattel, S.; Burstein, B.; Dobrev, D. Atrial remodeling and atrial fibrillation: Mechanisms and implications. Circ. Arrhythm. Electrophysiol. 2008, 1, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Jost, N.; Kohajda, Z.; Kristóf, A.; Kovács, P.P.; Husti, Z.; Juhász, V.; Kiss, L.; Varró, A.; Virág, L.; Baczkó, I. Atrial remodeling and novel pharmacological strategies for antiarrhythmic therapy in atrial fibrillation. Curr. Med. Chem. 2011, 18, 3675–3694. [Google Scholar] [CrossRef] [PubMed]
- Nattel, S.; Dobrev, D. The multidimensional role of calcium in atrial fibrillation pathophysiology: Mechanistic insights and therapeutic opportunities. Eur. Heart J. 2012, 33, 1870–1877. [Google Scholar] [CrossRef] [PubMed]
- Wirth, K.J.; Paehler, T.; Rosenstein, B.; Knobloch, K.; Maier, T.; Frenzel, J.; Brendel, J.; Busch, A.E.; Bleich, M. Atrial effects of the novel K(+)-channel-blocker AVE0118 in anesthetized pigs. Cardiovasc. Res. 2003, 60, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Christ, T.; Wettwer, E.; Voigt, N.; Hála, O.; Radicke, S.; Matschke, K.; Várro, A.; Dobrev, D.; Ravens, U. Pathology-specific effects of the IKur/Ito/IK,ACh blocker AVE0118 on ion channels in human chronic atrial fibrillation. Br. J. Pharmacol. 2008, 154, 1619–1630. [Google Scholar] [CrossRef] [PubMed]
- Oros, A.; Volders, P.G.; Beekman, J.D.; van der Nagel, T.; Vos, M.A. Atrial-specific drug AVE0118 is free of torsades de pointes in anesthetized dogs with chronic complete atrioventricular block. Heart Rhythm 2006, 3, 1339–1345. [Google Scholar] [CrossRef] [PubMed]
- de Haan, S.; Greiser, M.; Harks, E.; Blaauw, Y.; van Hunnik, A.; Verheule, S.; Allessie, M.; Schotten, U. AVE0118, blocker of the transient outward current (I(to)) and ultrarapid delayed rectifier current (I(Kur)), fully restores atrial contractility after cardioversion of atrial fibrillation in the goat. Circulation 2006, 114, 1234–1242. [Google Scholar] [CrossRef] [PubMed]
- Blaauw, Y.; Schotten, U.; van Hunnik, A.; Neuberger, H.R.; Allessie, M.A. Cardioversion of persistent atrial fibrillation by a combination of atrial specific and non-specific class III drugs in the goat. Cardiovasc. Res. 2007, 75, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Almquist, J.; Wallman, M.; Jacobson, I.; Jirstrand, M. Modeling the effect of Kv1.5 block on the canine action potential. Biophys. J. 2010, 99, 2726–2736. [Google Scholar] [CrossRef] [PubMed]
- Shiroshita-Takeshita, A.; Ford, J.; Madge, D.; Pinnock, R.; Nattel, S. Electrophysiological and atrial antiarrhythmic effects of a novel IKur/Kv1.5 blocker in dogs with atrial tachycardia remodeling. Heart Rhythm 2006, 3, S183. [Google Scholar] [CrossRef]
- Ford, J.; Milnes, J.; Wettwer, E.; Christ, T.; Rogers, M.; Sutton, K.; Madge, D.; Virag, L.; Jost, N.; Horvath, Z.; et al. Human electrophysiological and pharmacological properties of XEN-D0101: A novel atrial-selective Kv1.5/IKur inhibitor. J. Cardiovasc. Pharmacol. 2013, 61, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Ford, J.; Milnes, J.; El Haou, S.; Wettwer, E.; Loose, S.; Matschke, K.; Tyl, B.; Round, P.; Ravens, U. The positive frequency-dependent electrophysiological effects of the IKur inhibitor XEN-D0103 are desirable for the treatment of atrial fibrillation. Heart Rhythm 2016, 13, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Flenner, F.; Friedrich, F.W.; Ungeheuer, N.; Christ, T.; Geertz, B.; Reischmann, S.; Wagner, S.; Stathopoulou, K.; Söhren, K.D.; Weinberger, F.; et al. Ranolazine antagonizes catecholamine-induced dysfunction in isolated cardiomyocytes, but lacks long-term therapeutic effects in vivo in a mouse model of hypertrophic cardiomyopathy. Cardiovasc. Res. 2016, 109, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Sag, C.M.; Mallwitz, A.; Wagner, S.; Hartmann, N.; Schotola, H.; Fischer, T.H.; Ungeheuer, N.; Herting, J.; Shah, A.M.; Maier, L.S.; et al. Enhanced late INa induces proarrhythmogenic SR Ca leak in a CaMKII-dependent manner. J. Mol. Cell. Cardiol. 2014, 76, 94–105. [Google Scholar] [CrossRef] [PubMed]
- Poulet, C.; Wettwer, E.; Grunnet, M.; Jespersen, T.; Fabritz, L.; Matschke, K.; Knaut, M.; Ravens, U. Late Sodium Current in Human Atrial Cardiomyocytes from Patients in Sinus Rhythm and Atrial Fibrillation. PLoS ONE 2015, 10, e0131432. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Ma, J.; Li, H.; Wang, C.; Grandi, E.; Zhang, P.; Luo, A.; Bers, D.M.; Shryock, J.C.; Belardinelli, L. Late sodium current contributes to the reverse rate-dependent effect of IKr inhibition on ventricular repolarization. Circulation 2011, 123, 1713–1720. [Google Scholar] [CrossRef] [PubMed]
- Ravens, U. Antiarrhythmic therapy in atrial fibrillation. Pharmacol. Ther. 2010, 128, 129–145. [Google Scholar] [CrossRef] [PubMed]
- De Ferrari, G.M.; Maier, L.S.; Mont, L.; Schwartz, P.J.; Simonis, G.; Leschke, M.; Gronda, E.; Boriani, G.; Darius, H.; Guillamón Torán, L.; et al. Ranolazine in the treatment of atrial fibrillation: Results of the dose-ranging RAFFAELLO (Ranolazine in Atrial Fibrillation Following An ELectricaL CardiOversion) study. Heart Rhythm 2015, 12, 872–878. [Google Scholar] [CrossRef] [PubMed]
- Reiffel, J.A.; Camm, A.J.; Belardinelli, L.; Zeng, D.; Karwatowska-Prokopczuk, E.; Olmsted, A.; Zareba, W.; Rosero, S.; Kowey, P.; the HARMONY Investigators. The HARMONY Trial: Combined Ranolazine and Dronedarone in the Management of Paroxysmal Atrial Fibrillation: Mechanistic and Therapeutic Synergism. Circ. Arrhythm. Electrophysiol. 2015, 8, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- Kanter, H.L.; Saffitz, J.E.; Beyer, E.C. Cardiac myocytes express multiple gap junction proteins. Circ. Res. 1992, 70, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.M.; Rodefeld, M.E.; Green, K.; Beyer, E.C.; Saffitz, J.E. Gap junction protein phenotypes of the human heart and conduction system. J. Cardiovasc. Electrophysiol. 1995, 6, 813–822. [Google Scholar] [CrossRef] [PubMed]
- Carmeliet, E. Cardiac ionic currents and acute ischemia: From channels to arrhythmias. Physiol. Rev. 1999, 79, 917–1017. [Google Scholar] [CrossRef] [PubMed]
- Spach, M.S.; Heidlage, J.F.; Barr, R.C.; Dolber, P.C. Cell size and communication: Role in structural and electrical development and remodeling of the heart. Heart Rhythm 2004, 1, 500–515. [Google Scholar] [CrossRef] [PubMed]
- Jost, N.; Christ, T.; Magyar, J. New Strategies for the Treatment of Atrial Fibrillation. Pharmaceuticals 2021, 14, 926. [Google Scholar] [CrossRef] [PubMed]
- Pogwizd, S.M. Clinical potential of sodium-calcium exchanger inhibitors as antiarrhythmic agents. Drugs 2003, 63, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Tóth, A.; Kiss, L.; Varró, A.; Nánási, P.P. Potential therapeutic effects of Na+/Ca2+ exchanger inhibition in cardiac diseases. Curr. Med. Chem. 2009, 16, 3294–3321. [Google Scholar] [CrossRef] [PubMed]
- Kovács, P.P.; Simon, J.; Christ, T.; Wettwer, E.; Varró, A.; Ravens, U. NCX current is increased in human chronic atrial fibrillation: A possible explanation for contractile dysfunction? Cardiovasc. Res. 2010, 87, S50. [Google Scholar]
- Elias, C.L.; Lukas, A.; Shurraw, S.; Scott, J.; Omelchenko, A.; Gross, G.J.; Hnatowich, M.; Hryshko, L.V. Inhibition of Na+/Ca2+ exchange by KB-R7943: Transport mode selectivity and antiarrhythmic consequences. Am. J. Physiol. Heart Circ. Physiol. 2001, 281, H1334–H1345. [Google Scholar] [CrossRef] [PubMed]
- Birinyi, P.; Tóth, A.; Jóna, I.; Acsai, K.; Almássy, J.; Nagy, N.; Prorok, J.; Gherasim, I.; Papp, Z.; Hertelendi, Z.; et al. The Na+/Ca2+ exchange blocker SEA0400 fails to enhance cytosolic Ca2+ transient and contractility in canine ventricular cardiomyocytes. Cardiovasc. Res. 2008, 78, 476–484. [Google Scholar] [CrossRef] [PubMed]
- Lebek, S.; Pichler, K.; Reuthner, K.; Trum, M.; Tafelmeier, M.; Mustroph, J.; Camboni, D.; Rupprecht, L.; Schmid, C.; Maier, L.S.; et al. Enhanced CaMKII-Dependent Late INa Induces Atrial Proarrhythmic Activity in Patients with Sleep-disordered Breathing. Circ. Res. 2020, 126, 603–615. [Google Scholar] [CrossRef] [PubMed]
- Nattel, S.; Heijman, J.; Zhou, L.; Dobrev, D. Molecular basis of atrial fibrillation pathophysiology and therapy: A translational perspective. Circ. Res. 2020, 127, 51–72. [Google Scholar] [CrossRef] [PubMed]
- Chelu, M.G.; Sarma, S.; Sood, S.; Wang, S.; van Oort, R.J.; Skapura, D.G.; Li, N.; Santonastasi, M.; Müller, F.U.; Schmitz, W.; et al. Calmodulin kinase II-mediated sarcoplasmic reticulum Ca2+ leak promotes atrial fibrillation in mice. J. Clin. Investig. 2009, 119, 1940–1951. [Google Scholar] [CrossRef] [PubMed]
- Vest, J.A.; Wehrens, X.H.; Reiken, S.R.; Lehnart, S.E.; Dobrev, D.; Chandra, P.; Danilo, P.; Ravens, U.; Rosen, M.R.; Marks, A.R. Defective cardiac ryanodine receptor regulation during atrial fibrillation. Circulation 2005, 111, 2025–2032. [Google Scholar] [CrossRef] [PubMed]
- Dincer, U.D. Cardiac ryanodine receptor in metabolic syndrome: Is JTV519 (K201) future therapy? Diabetes Metab. Syndr. Obes. 2012, 5, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Nassif, M.E.; Windsor, S.L.; Tang, F.; Khariton, Y.; Husain, M.; Inzucchi, S.E.; McGuire, D.K.; Pitt, B.; Scirica, B.M.; Austin, B.; et al. Dapagliflozin effects on biomarkers, symptoms, and functional status in patients with heart failure with reduced ejection fraction: The DEFINE-HF trial. Circulation 2019, 140, 1463–1476. [Google Scholar] [CrossRef] [PubMed]
- Mauriello, A.; Correra, A.; Molinari, R.; Del Vecchio, G.E.; Tessitore, V.; D’Andrea, A.; Russo, V. Mitochondrial Dysfunction in Atrial Fibrillation: The Need for a Strong Pharmacological Approach. Biomedicines 2024, 12, 2720. [Google Scholar] [CrossRef] [PubMed]
- Chatfield, K.C.; Sparagna, G.C.; Chau, S.; Phillips, E.K.; Ambardekar, A.V.; Aftab, M.; Mitchell, M.B.; Sucharov, C.C.; Miyamoto, S.D.; Stauffer, B.L. Elamipretide Improves Mitochondrial Function in the Failing Human Heart. JACC Basic Transl. Sci. 2019, 4, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Sulaimon, L.A.; Afolabi, L.O.; Adisa, R.A.; Ayankojo, A.G.; Afolabi, M.O.; Adewolu, A.M.; Wan, X. Pharmacological significance of MitoQ in ameliorating mitochondria-related diseases. Adv. Redox Res. 2022, 5, 100037. [Google Scholar] [CrossRef]
- Muszyński, P.; Bonda, T.A. Mitochondrial Dysfunction in Atrial Fibrillation—Mechanisms and Pharmacological Interventions. J. Clin. Med. 2021, 10, 2385. [Google Scholar] [CrossRef] [PubMed]
- Seo, K.S.; Kim, J.H.; Min, K.N.; Moon, J.A.; Roh, T.C.; Lee, M.J.; Lee, K.W.; Min, J.E.; Lee, Y.M. KL1333, a novel NAD+ modulator, improves energy metabolism and mitochondrial dysfunction in MELAS fibroblasts. Front. Neurol. 2018, 9, 552. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Patoulias, D.; Kassimis, G.; Koufakis, T.; Klisic, A.; Doumas, M.; Fragakis, N.; Rizzo, M. Therapeutic Potential of Sodium-glucose Co-transporter-2 Inhibitors and Glucagon-like peptide-1 Receptor Agonists for Patients with Acute Coronary Syndrome: A Review of Clinical Evidence. Curr. Pharm. Des. 2024, 30, 2109–2119. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Pamporis, K.; Stachteas, P.; Patoulias, D.; Bougioukas, K.I.; Fragakis, N. Efficacy and safety of sodium-glucose cotransporter-2 inhibitors in heart failure with mildly reduced or preserved ejection fraction: An overview of 36 systematic reviews. Heart Fail. Rev. 2023, 28, 1033–1051. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Popovic, D.S.; Patoulias, D.; Koufakis, T.; Papanas, N.; Fragakis, N.; Rizzo, M. The Effect of Sodium-glucose Cotransporter Inhibitors on Renal Function as Adjunctive to Insulin in Adults with Type 1 diabetes: An Updated Multilevel Meta-analysis of Randomized Controlled Trials. Diabetes Ther. 2024, 15, 521–532. [Google Scholar] [CrossRef] [PubMed]
- Mylonas, N.; Nikolaou, P.E.; Karakasis, P.; Stachteas, P.; Fragakis, N.; Andreadou, I. Endothelial protection by sodium-glucose cotransporter 2 inhibitors: A literature review of in vitro and in vivo studies. Int. J. Mol. Sci. 2024, 25, 7274. [Google Scholar] [CrossRef] [PubMed]
- Nakatsu, Y.; Kokubo, H.; Bumdelger, B.; Yoshizumi, M.; Yamamotoya, T.; Matsunaga, Y.; Ueda, K.; Inoue, Y.; Inoue, M.K.; Fujishiro, M.; et al. The SGLT2 inhibitor Luseogliflozin Rapidly Normalizes Aortic mRNA Levels of Inflammation-related but not Lipid-Metabolism-Related Genes and Suppresses Atherosclerosis in Diabetic ApoE KO mice. Int. J. Mol. Sci. 2017, 18, 1704. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Zhan, F.; He, M.; Liu, Z.; Song, X. Anti-inflammatory effects of sodium-glucose co-transporter 2 inhibitors on atherosclerosis. Vascul. Pharmacol. 2020, 133–134, 106779. [Google Scholar] [CrossRef] [PubMed]
- Garvey, W.T.; Van Gaal, L.; Leiter, L.A.; Vijapurkar, U.; List, J.; Cuddihy, R.; Ren, J.; Davies, M.J. Effects of canagliflozin versus glimepiride on adipokines and inflammatory biomarkers in type 2 diabetes. Metabolism 2018, 85, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Uthman, L.; Homayr, A.; Juni, R.P.; Spin, E.L.; Kerindongo, R.; Boomsma, M.; Hollmann, M.W.; Preckel, B.; Koolwijk, P.; van Hinsbergh, V.W.M.; et al. Empagliflozin and Dapagliflozin Reduce ROS Generation and Restore NO Bioavailability in Tumor Necrosis Factor α-stimulated Human Coronary Arterial Endothelial Cells. Cell. Physiol. Biochem. 2019, 53, 865–886. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.R.; Lee, S.G.; Kim, S.H.; Kim, J.H.; Choi, E.; Cho, W.; Rim, J.H.; Hwang, I.; Lee, C.J.; Lee, M.; et al. SGLT2 inhibition modulates NLRP3 inflammasome activity via ketones and insulin in diabetes with cardiovascular disease. Nat. Commun. 2020, 11, 2127. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Aizawa, Y.; Yuasa, S.; Kishi, S.; Fuse, K.; Fujita, S.; Ikeda, Y.; Kitazawa, H.; Takahashi, M.; Sato, M.; et al. The effect of dapagliflozin treatment on epicardial adipose tissue volume. Cardiovasc. Diabetol. 2018, 17, 6. [Google Scholar] [CrossRef] [PubMed]
- Stachteas, P.; Karakasis, P.; Patoulias, D.; Clemenza, F.; Fragakis, N.; Rizzo, M. The effect of sodium-glucose co-transporter-2 inhibitors on markers of subclinical atherosclerosis. Ann. Med. 2023, 55, 2304667. [Google Scholar] [CrossRef] [PubMed]
- Olgar, Y.; Turan, B. A sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin comparison with insulin shows important effects on Zn2+-transporters in cardiomyocytes from insulin-resistant metabolic syndrome rats through inhibition of oxidative stress. Can. J. Physiol. Pharmacol. 2019, 97, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Schauer, A.; Adams, V.; Kämmerer, S.; Langner, E.; Augstein, A.; Barthel, P.; Männel, A.; Fabig, G.; Alves, P.K.N.; Günscht, M.; et al. Empagliflozin improves diastolic function in HFpEF by restabilizing the mitochondrial respiratory chain. Circ. Heart Fail. 2024, 17, e011107. [Google Scholar] [CrossRef] [PubMed]
- Packer, M. Critical Reanalysis of the Mechanisms Underlying the Cardiorenal Benefits of SGLT2 Inhibitors and Reaffirmation of the Nutrient Deprivation Signaling/Autophagy Hypothesis. Circulation 2022, 146, 1383–1405. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Zhang, M.; Suo, M.; Liu, D.; Wang, X.; Liu, M.; Pan, J.; Jin, T.; An, F. Dapagliflozin alleviates cardiac fibrosis through suppressing EndMT and fibroblast activation via AMPKα/TGF-β/Smad signalling in type 2 diabetic rats. J. Cell. Mol. Med. 2021, 25, 7642–7659. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.; Shiou, Y.L.; Jhuo, S.J.; Chang, C.Y.; Liu, P.L.; Jhuang, W.J.; Dai, Z.K.; Chen, W.Y.; Chen, Y.F.; Lee, A.S. The sodium-glucose co-transporter 2 inhibitor empagliflozin attenuates cardiac fibrosis and improves ventricular hemodynamics in hypertensive heart failure rats. Cardiovasc. Diabetol. 2019, 18, 45. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Zhang, X.; Wang, Q. Effects and mechanisms of SGLT2 inhibitors on the NLRP3 inflammasome, with a focus on atherosclerosis. Front. Endocrinol. 2022, 13, 992937. [Google Scholar] [CrossRef] [PubMed]
- Scisciola, L.; Cataldo, V.; Taktaz, F.; Fontanella, R.A.; Pesapane, A.; Ghosh, P.; Franzese, M.; Puocci, A.; De Angelis, A.; Sportiello, L.; et al. Anti-inflammatory role of SGLT2 inhibitors as part of their anti-atherosclerotic activity: Data from basic science and clinical trials. Front. Cardiovasc. Med. 2022, 9, 1008922. [Google Scholar] [CrossRef] [PubMed]
- Dyck, J.R.B.; Sossalla, S.; Hamdani, N.; Coronel, R.; Weber, N.C.; Light, P.E.; Zuurbier, C.J. Cardiac mechanisms of the beneficial effects of SGLT2 inhibitors in heart failure: Evidence for potential off-target effects. J. Mol. Cell. Cardiol. 2022, 167, 17–31. [Google Scholar] [CrossRef] [PubMed]
- Andersen, A.; Bagger, J.I.; Sørensen, S.K.; Baldassarre, M.P.A.; Pedersen-Bjergaard, U.; Forman, J.L.; Gislason, G.; Lindhardt, T.B.; Knop, F.K.; Vilsbøll, T. Associations of hypoglycemia, glycemic variability and risk of cardiac arrhythmias in insulin-treated patients with type 2 diabetes: A prospective, observational study. Cardiovasc. Diabetol. 2021, 20, 241. [Google Scholar] [CrossRef] [PubMed]
- Saito, S.; Teshima, Y.; Fukui, A.; Kondo, H.; Nishio, S.; Nakagawa, M.; Saikawa, T.; Takahashi, N. Glucose fluctuations increase the incidence of atrial fibrillation in diabetic rats. Cardiovasc. Res. 2014, 104, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Paasche, A.; Wiedmann, F.; Kraft, M.; Seibertz, F.; Herlt, V.; Blochberger, P.L.; Jávorszky, N.; Beck, M.; Weirauch, L.; Seeger, T.; et al. Acute antiarrhythmic effects of SGLT2 inhibitors—Dapagliflozin lowers the excitability of atrial cardiomyocytes. Basic Res. Cardiol. 2024, 119, 93–112. [Google Scholar] [CrossRef] [PubMed]
- Philippaert, K.; Kalyaanamoorthy, S.; Fatehi, M.; Long, W.; Soni, S.; Byrne, N.J.; Barr, A.; Singh, J.; Wong, J.; Palechuk, T.; et al. Cardiac late sodium channel current is a molecular target for the sodium/glucose cotransporter 2 inhibitor empagliflozin. Circulation 2021, 143, 2188–2204. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.S.; Singh, T.; Newby, D.E.; Singh, J. Sodium-glucose co-transporter 2 inhibitor therapy: Mechanisms of action in heart failure. Heart 2021, 107, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.E.; Petersenn, F.; Hackbarth, J.; Pfeiffer, J.; Gampp, H.; Frey, N.; Lugenbiel, P.; Thomas, D.; Rahm, A.K. Electrophysiological Effects of the Sodium-glucose Co-transporter-2 (SGLT2) Inhibitor Dapagliflozin on Human Cardiac Potassium Channels. Int. J. Mol. Sci. 2024, 25, 5701. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.I.; Chen, Y.C.; Lin, Y.K.; Chung, C.C.; Lu, Y.Y.; Kao, Y.H.; Chen, Y.J. Empagliflozin Attenuates Myocardial Sodium and Calcium Dysregulation and Reverses Cardiac Remodeling in Streptozotocin-induced Diabetic Rats. Int. J. Mol. Sci. 2019, 20, 1680. [Google Scholar] [CrossRef] [PubMed]
- Mustroph, J.; Wagemann, O.; Lücht, C.M.; Trum, M.; Hammer, K.P.; Sag, C.M.; Lebek, S.; Tarnowski, D.; Reinders, J.; Perbellini, F.; et al. Empagliflozin reduces Ca/calmodulin-dependent kinase II activity in isolated ventricular cardiomyocytes. ESC Heart Fail. 2018, 5, 642–648. [Google Scholar] [CrossRef] [PubMed]
- Zhan, G.; Wang, X.; Wang, X.; Li, J.; Tang, Y.; Bi, H.; Yang, X.; Xia, Y. Dapagliflozin: A sodium-glucose cotransporter 2 inhibitor, attenuates angiotensin II-induced atrial fibrillation by regulating atrial electrical and structural remodeling. Eur. J. Pharmacol. 2024, 978, 176712. [Google Scholar] [CrossRef] [PubMed]
- Li, H.L.; Lip, G.Y.H.; Feng, Q.; Fei, Y.; Tse, Y.K.; Wu, M.Z.; Ren, Q.W.; Tse, H.F.; Cheung, B.Y.; Yiu, K.H. Sodium-Glucose Cotransporter 2 Inhibitors (SGLT2i) and Cardiac Arrhythmias: A Systematic Review and Meta-analysis. Cardiovasc. Diabetol. 2021, 20, 100. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zhang, Y.; Wang, Z.; Liu, D.; Mao, S.; Liang, B. The effectiveness of SGLT2 inhibitor in the incidence of atrial fibrillation/atrial flutter in patients with type 2 diabetes mellitus/heart failure: A systematic review and meta-analysis. J. Thorac. Dis. 2022, 14, 1620–1637. [Google Scholar] [CrossRef] [PubMed]
- Zelniker, T.A.; Bonaca, M.P.; Furtado, R.H.M.; Mosenzon, O.; Kuder, J.F.; Murphy, S.A.; Bhatt, D.L.; Leiter, L.A.; McGuire, D.K.; Wilding, J.P.H.; et al. Effect of Dapagliflozin on Atrial Fibrillation in Patients with Type 2 Diabetes Mellitus: Insights From the DECLARE-TIMI 58 trial. Circulation 2020, 141, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Younis, A.; Arous, T.; Klempfner, R.; Kharsa, A.; McNitt, S.; Schleede, S.; Polonski, B.; Abdallah, Z.; Buttar, R.; Bodurian, C.; et al. Effect of sodium glucose cotransporter 2 inhibitors on atrial tachy-arrhythmia burden in patients with cardiac implantable electronic devices. J. Cardiovasc. Electrophysiol. 2023, 34, 1595–1604. [Google Scholar] [CrossRef] [PubMed]
- Marso, S.P.; Bain, S.C.; Consoli, A.; Eliaschewitz, F.G.; Jódar, E.; Leiter, L.A.; Lingvay, I.; Rosenstock, J.; Seufert, J.; Warren, M.L.; et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 1834–1844. [Google Scholar] [CrossRef] [PubMed]
- Marso, S.P.; Daniels, G.H.; Brown-Frandsen, K.; Kristensen, P.; Mann, J.F.; Nauck, M.A.; Nissen, S.E.; Pocock, S.; Poulter, N.R.; Ravn, L.S.; et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Fragakis, N.; Patoulias, D.; Theofilis, P.; Sagris, M.; Koufakis, T.; Vlachakis, P.K.; Rangraze, I.R.; El Tanani, M.; Tsioufis, K.; et al. The Emerging Role of Glucagon-like Peptide-1 Receptor Agonists in the Management of Obesity-Related Heart Failure with Preserved Ejection Fraction: Benefits beyond What Scales Can Measure? Biomedicines 2024, 12, 2112. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Zhang, W.; Zhang, D.; Ren, G.; Wang, P.; Gao, L.; Chen, H.; Ding, C. Comparison of the effect of glucose-lowering agents on the risk of atrial fibrillation: A network meta-analysis. Heart Rhythm 2021, 18, 1090–1096. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Niwano, S.; Niwano, H.; Fukaya, H.; Murakami, M.; Kishihara, J.; Satoh, A.; Yoshizawa, T.; Ishizue, N.; Igarashi, T.; et al. Liraglutide suppresses atrial electrophysiological changes. Heart Vessel. 2019, 34, 1389–1393. [Google Scholar] [CrossRef] [PubMed]
- Bohne, L.J.; Jansen, H.J.; Dorey, T.W.; Daniel, I.M.; Jamieson, K.L.; Belke, D.D.; McRae, M.D.; Rose, R.A. Glucagon-Like Peptide-1 Protects Against Atrial Fibrillation and Atrial Remodeling in Type 2 Diabetic Mice. JACC Basic Transl. Sci. 2023, 8, 922–936. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, G.Y.; Maeng, H.J.; Kim, H.; Bae, J.H.; Kim, K.M.; Lim, S. Effects of glucagon-like peptide-1 analogue and fibroblast growth factor 21 combination on the atherosclerosis-related process in a type 2 diabetes mouse model. Endocrinol. Metab. 2021, 36, 157–170. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.; Khurana, A.; Bhatti, J.S.; Weiskirchen, R.; Navik, U. Glucagon-like peptide 1 and fibroblast growth factor-21 in non-alcoholic steatohepatitis: An experimental to clinical perspective. Pharmacol. Res. 2022, 184, 106426. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, S.H. Anti-inflammatory role of glucagon-like peptide 1 receptor agonists and its clinical implications. Ther. Adv. Endocrinol. Metab. 2024, 15, 20420188231222367. [Google Scholar] [CrossRef] [PubMed]
- Mehdi, S.F.; Pusapati, S.; Anwar, M.S.; Lohana, D.; Kumar, P.; Nandula, S.A.; Nawaz, F.K.; Tracey, K.; Yang, H.; LeRoith, D.; et al. Glucagon-like peptide-1: A multi-faceted anti-inflammatory agent. Front. Immunol. 2023, 14, 1148209. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Lin, Y.; Wang, S.; Zhang, L.; Guo, L. GLP-1 Inhibits High-Glucose-Induced Oxidative Injury of Vascular Endothelial Cells. Sci. Rep. 2017, 7, 8008. [Google Scholar] [CrossRef] [PubMed]
- Mangmool, S.; Hemplueksa, P.; Parichatikanond, W.; Chattipakorn, N. Epac is required for GLP-1R-mediated inhibition of oxidative stress and apoptosis in cardiomyocytes. Mol. Endocrinol. 2015, 29, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Oh, Y.S.; Jun, H.S. Effects of Glucagon-Like Peptide-1 on Oxidative Stress and Nrf2 Signaling. Int. J. Mol. Sci. 2017, 19, 26. [Google Scholar] [CrossRef] [PubMed]
- Pandey, S.; Mangmool, S.; Parichatikanond, W. Multifaceted Roles of GLP-1 and Its Analogs: A Review on Molecular Mechanisms with a Cardiotherapeutic Perspective. Pharmaceuticals 2023, 16, 836. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Fan, S.; Xiong, Q.; Niu, Y.; Zhang, X.; Qin, J.; Shi, Y.; Zhang, L. Glucagon-like peptide-1 attenuates cardiac hypertrophy via the AngII/AT1R/ACE2 and AMPK/mTOR/p70S6K pathways. Acta Biochim. Biophys. Sin. 2021, 53, 1189–1197. [Google Scholar] [CrossRef] [PubMed]
- Nreu, B.; Dicembrini, I.; Tinti, F.; Sesti, G.; Mannucci, E.; Monami, M. Major cardiovascular events, heart failure, and atrial fibrillation in patients treated with glucagon-like peptide-1 receptor agonists: An updated meta-analysis of randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1106–1114. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, F.C.; Yen, K.C.; Chao, T.F.; Chen, S.W.; Chan, Y.H.; Chu, P.H. New-Onset Atrial Fibrillation in Patients With Type 2 Diabetes Treated With Novel Glucose-Lowering Therapies. J. Clin. Endocrinol. Metab. 2022, 107, 2493–2499. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Fragakis, N.; Patoulias, D.; Theofilis, P.; Kassimis, G.; Karamitsos, T.; El-Tanani, M.; Rizzo, M. Effects of Glucagon-Like Peptide 1 Receptor Agonists on Atrial Fibrillation Recurrence After Catheter Ablation: A Systematic Review and Meta-Analysis. Adv. Ther. 2024, 41, 3749–3756. [Google Scholar] [CrossRef] [PubMed]
- Christophersen, I.E.; Rienstra, M.; Roselli, C.; Yin, X.; Geelhoed, B.; Barnard, J.; Lin, H.; Arking, D.E.; Smith, A.V.; Albert, C.M.; et al. Large-Scale analyses of common and rare variants identify 12 new loci associated with atrial fibrillation. Nat. Genet. 2017, 49, 946–952. [Google Scholar] [CrossRef] [PubMed]
- Miyazawa, K.; Ito, K.; Ito, M.; Zou, Z.; Kubota, M.; Nomura, S.; Matsunaga, H.; Koyama, S.; Ieki, H.; Akiyama, M.; et al. Cross-ancestry genome-wide analysis of atrial fibrillation unveils disease biology and enables cardioembolic risk prediction. Nat. Genet. 2023, 55, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.W.; Chen, J.J.; Wang, C.H.; Chang, S.N.; Chiu, F.C.; Huang, P.S.; Chua, S.K.; Chuang, E.Y.; Tsai, C.T. Identification of a new genetic locus associated with atrial fibrillation in the Taiwanese population by genome-wide and transcriptome-wide association studies. EP Eur. 2025, 27, euaf042. [Google Scholar] [CrossRef] [PubMed]
- Harati, H.; Zanetti, D.; Rao, A.; Gustafsson, S.; Perez, M.; Ingelsson, E.; Knowles, J.W. No evidence of a causal association of type 2 diabetes and glucose metabolism with Atrial Fibrillation. Diabetologia 2019, 62, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Steenman, M. Insight into Atrial Fibrillation through Analysis of the Coding Transcriptome in Humans. Biophys. Rev. 2020, 12, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Li, T.L.; Zhu, N.N.; Yin, Z.; Sun, J.; Guo, J.P.; Yuan, H.T.; Shi, X.M.; Guo, H.Y.; Li, S.X.; Shan, Z.L. Transcriptomic analysis of epicardial adipose tissue reveals the potential crosstalk genes and immune relationship between type 2 diabetes mellitus and atrial fibrillation. Gene 2024, 920, 148528. [Google Scholar] [CrossRef] [PubMed]
- Menezes Junior, A.D.S.; Ferreira, L.C.; Barbosa, L.J.V.; Silva, D.M.E.; Saddi, V.A.; Silva, A.M.T.C. Circulating MicroRNAs as Specific Biomarkers in Atrial Fibrillation: A Meta-Analysis. Noncoding RNA 2023, 9, 13. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.; Chen, H.; Ge, D.; Xu, Y.; Xu, H.; Yang, Y.; Gu, M.; Zhou, Y.; Zhu, J.; Ge, T.; et al. Mir-21 Promotes Cardiac Fibrosis After Myocardial Infarction Via Targeting Smad7. Cell Physiol. Biochem. 2017, 42, 2207–2219. [Google Scholar] [CrossRef] [PubMed]
- Duisters, R.F.; Tijsen, A.J.; Schroen, B.; Leenders, J.J.; Lentink, V.; van der Made, I.; Herias, V.; van Leeuwen, R.E.; Schellings, M.W.; Barenbrug, P.; et al. miR-133 and miR-30 regulate connective tissue growth factor: Implications for a role of microRNAs in myocardial matrix remodeling. Circ. Res. 2009, 104, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Nie, J.; Han, Y.; Ni, L. Epigenetic Mechanism and Therapeutic Implications of Atrial Fibrillation. Front. Cardiovasc. Med. 2022, 8, 763824. [Google Scholar] [CrossRef] [PubMed]
- Vigorelli, V.; Resta, J.; Bianchessi, V.; Lauri, A.; Bassetti, B.; Agrifoglio, M.; Pesce, M.; Polvani, G.; Bonalumi, G.; Cavallotti, L.; et al. Abnormal DNA Methylation Induced by Hyperglycemia Reduces CXCR4 Gene Expression in CD34+ Stem Cells. J. Am. Heart Assoc. 2019, 8, e010012. [Google Scholar] [CrossRef] [PubMed]
- Cooper, M.E.; El-Osta, A. Epigenetics: Mechanisms and implications for diabetic complications. Circ. Res. 2010, 107, 1403–1413. [Google Scholar] [CrossRef] [PubMed]
- Nural-Guvener, H.F.; Zakharova, L.; Nimlos, J.; Popovic, S.; Mastroeni, D.; Gaballa, M.A. HDAC class I inhibitor, Mocetinostat, reverses cardiac fibrosis in heart failure and diminishes CD90+ cardiac myofibroblast activation. Fibrogenesis Tissue Repair 2014, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Atzemian, N.; Androutsopoulou, V.; Portokallidou, K.; Leonidis, G.; Pallikarou, M.; Ragia, G.; Karangelis, D.; Mikroulis, D.; Manolopoulos, V. Insights into Type 2 Diabetes Mellitus in Atrial Fibrillation Patients: A Proteomics Approach. Eur. Heart J. 2024, 45 (Suppl. S1), ehae666.446. [Google Scholar] [CrossRef]
- Mayr, M.; Yusuf, S.; Weir, G.; Chung, Y.L.; Mayr, U.; Yin, X.; Ladroue, C.; Madhu, B.; Roberts, N.; De Souza, A.; et al. Combined Metabolomic and Proteomic Analysis of Human Atrial Fibrillation. J. Am. Coll. Cardiol. 2008, 51, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Rohun, J.; Dudzik, D.; Raczak-Gutknecht, J.; Wabich, E.; Młodziński, K.; Markuszewski, M.J.; Daniłowicz-Szymanowicz, L. Metabolomics in Atrial Fibrillation: Unlocking Novel Biomarkers and Pathways for Diagnosis, Prognosis, and Personalized Treatment. J. Clin. Med. 2024, 14, 34. [Google Scholar] [CrossRef] [PubMed]
- Van Gelder, I.C.; Rienstra, M.; Bunting, K.V.; Casado-Arroyo, R.; Caso, V.; Crijns, H.J.G.M.; De Potter, T.J.R.; Dwight, J.; Guasti, L.; Hanke, T.; et al. 2024 ESC Guidelines for the Management of Atrial Fibrillation Developed in Collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2024, 45, 3314–3414. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.H.; Wu, L.S.; Chiou, M.J.; Liu, J.R.; Yu, K.H.; Kuo, C.F.; Wen, M.S.; Chen, W.J.; Yeh, Y.H.; See, L.C. Association of Metformin with Lower Atrial Fibrillation Risk among Patients with Type 2 Diabetes Mellitus: A Population-Based Dynamic Cohort and In Vitro Studies. Cardiovasc. Diabetol. 2014, 13, 123. [Google Scholar] [CrossRef] [PubMed]
- Foretz, M.; Guigas, B.; Viollet, B. Metformin: Update on Mechanisms of Action and Repurposing Potential. Nat. Rev. Endocrinol. 2023, 19, 460–476. [Google Scholar] [CrossRef] [PubMed]
- Bai, F.; Liu, Y.; Tu, T.; Li, B.; Xiao, Y.; Ma, Y.; Qin, F.; Xie, J.; Zhou, S.; Liu, Q. Metformin Regulates Lipid Metabolism in a Canine Model of Atrial Fibrillation through AMPK/PPAR-α/VLCAD Pathway. Lipids Health Dis. 2019, 18, 109. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Po, S.S.; Zhang, B.; Bai, F.; Li, J.; Qin, F.; Liu, N.; Sun, C.; Xiao, Y.; Tu, T.; et al. Metformin Regulates Adiponectin Signalling in Epicardial Adipose Tissue and Reduces Atrial Fibrillation Vulnerability. J. Cell. Mol. Med. 2020, 24, 7751–7766. [Google Scholar] [CrossRef] [PubMed]
- Nantsupawat, T.; Wongcharoen, W.; Chattipakorn, S.C.; Chattipakorn, N. Effects of Metformin on Atrial and Ventricular Arrhythmias: Evidence from Cell to Patient. Cardiovasc. Diabetol. 2020, 19, 198. [Google Scholar] [CrossRef] [PubMed]
- Shimano, M.; Tsuji, Y.; Inden, Y.; Kitamura, K.; Uchikawa, T.; Harata, S.; Nattel, S.; Murohara, T. Pioglitazone, a peroxisome proliferator-activated receptor-gamma activator, attenuates atrial fibrosis and atrial fibrillation promotion in rabbits with congestive heart failure. Heart Rhythm 2008, 5, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Chao, T.F.; Leu, H.B.; Huang, C.C.; Chen, J.W.; Chan, W.L.; Lin, S.J.; Chen, S.A. Thiazolidinediones can prevent new onset atrial fibrillation in patients with non-insulin dependent diabetes. Int. J. Cardiol. 2012, 156, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Park, S.Y.; Kim, B.; Min, C.; Cho, W.; Yon, D.K.; Kim, J.Y.; Han, K.D.; Rhee, E.J.; Lee, W.Y.; et al. Association between antidiabetic drugs and the incidence of atrial fibrillation in patients with type 2 diabetes: A nationwide cohort study in South Korea. Diabetes Res. Clin. Pract. 2023, 198, 110626. [Google Scholar] [CrossRef] [PubMed]
- Pallisgaard, J.L.; Brooks, M.M.; Chaitman, B.R.; Boothroyd, D.B.; Perez, M.; Hlatky, M.A.; Bypass Angioplasty Revascularization Investigation 2 Diabetes Study Group. Thiazolidinediones and Risk of Atrial Fibrillation Among Patients with Diabetes and Coronary Disease. Am. J. Med. 2018, 131, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Liou, Y.S.; Yang, F.Y.; Chen, H.Y.; Jong, G.P. Antihyperglycemic drugs use and new-onset atrial fibrillation: A population-based nested case control study. PLoS ONE 2018, 13, e0197245. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Zhang, G.; Chang, C.; Chou, O.H.I.; Lee, S.; Leung, K.S.K.; Wong, W.T.; Liu, T.; Wai, A.K.C.; Cheng, S.H.; et al. Metformin versus sulphonylureas for new onset atrial fibrillation and stroke in type 2 diabetes mellitus: A population-based study. Acta Diabetol. 2022, 59, 697–709. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.Y.; Yang, F.Y.; Jong, G.P.; Liou, Y.S. Antihyperglycemic drugs use and new-onset atrial fibrillation in elderly patients. Eur. J. Clin. Investig. 2017, 47, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Patoulias, D.I.; Boulmpou, A.; Teperikidis, E.; Katsimardou, A.; Siskos, F.; Doumas, M.; Papadopoulos, C.E.; Vassilikos, V. Cardiovascular efficacy and safety of dipeptidyl peptidase-4 inhibitors: A meta-analysis of cardiovascular outcome trials. World J. Cardiol. 2021, 13, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Sagris, M.; Patoulias, D.; Koufakis, T.; Theofilis, P.; Klisic, A.; Fragakis, N.; El Tanani, M.; Rizzo, M. Mitigating Increased Cardiovascular Risk in Patients with Obstructive Sleep Apnea Using GLP-1 Receptor Agonists and SGLT2 Inhibitors: Hype or Hope? Biomedicines 2024, 12, 2503. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Patoulias, D.; Fragakis, N.; Bernal-López, M.R.; Gómez-Huelgas, R. Glucagon-like peptide-1 receptor agonists and sodium-glucose cotransporter-2 inhibitors combination therapy versus monotherapy and major adverse cardiovascular events: Do the benefits add up? Eur. J. Intern. Med. 2024, 130, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Theofilis, P.; Patoulias, D.; Vlachakis, P.K.; Pamporis, K.; Sagris, M.; Ktenopoulos, N.; Kassimis, G.; Antoniadis, A.P.; Fragakis, N. Sodium-Glucose Cotransporter 2 Inhibitors in Aortic Stenosis: Toward a Comprehensive Cardiometabolic Approach. Int. J. Mol. Sci. 2025, 26, 4494. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Kang, B.; Zhou, J. Sodium glucose cotransporter 2 inhibitors with cardiac arrhythmias in patients with type 2 diabetes mellitus: A systematic review and meta-analysis of randomized placebo-controlled trials. Clin. Res. Cardiol. 2024, 113, 910–923. [Google Scholar] [CrossRef] [PubMed]
- Ebert, M.; Stegmann, C.; Kosiuk, J.; Dinov, B.; Richter, S.; Arya, A.; Müssigbrodt, A.; Sommer, P.; Hindricks, G.; Bollmann, A. Predictors, management, and outcome of cardioversion failure early after atrial fibrillation ablation. Europace 2018, 20, 1428–1434. [Google Scholar] [CrossRef] [PubMed]
- Grönberg, T.; Hartikainen, J.E.; Nuotio, I.; Biancari, F.; Vasankari, T.; Nikkinen, M.; Ylitalo, A.; Airaksinen, K.E. Can we predict the failure of electrical cardioversion of acute atrial fibrillation? The FinCV study. Pacing Clin. Electrophysiol. 2015, 38, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Soran, H.; Banerjee, M.; Mohamad, J.B.; Adam, S.; Ho, J.H.; Ismaeel, S.M.; Dhage, S.; Syed, A.A.; Abdulla, I.M.A.; Younis, N.; et al. Risk Factors for Failure of Direct Current Cardioversion in Patients with Type 2 Diabetes Mellitus and Atrial Fibrillation. Biomed Res. Int. 2018, 2018, 5936180. [Google Scholar] [CrossRef] [PubMed]
- Kriz, R.; Freynhofer, M.K.; Weiss, T.W.; Egger, F.; Gruber, S.C.; Eisenburger, P.; Wojta, J.; Huber, K.; Koch, J. Safety and efficacy of pharmacological cardioversion of recent-onset atrial fibrillation: A single-center experience. Am. J. Emerg. Med. 2016, 34, 1486–1490. [Google Scholar] [CrossRef] [PubMed]
- Ergene, U.; Ergene, O.; Cete, Y.; Fowler, J.; Nazli, C.; Oktay, C. Predictors of success in the conversion of new-onset atrial fibrillation using oral propafenone. Eur. J. Emerg. Med. 1998, 5, 425–428. [Google Scholar] [CrossRef]
- Handelsman, Y.; Bunch, T.J.; Rodbard, H.W.; Steinberg, B.A.; Thind, M.; Bigot, G.; Konigsberg, L.; Wieloch, M.; Kowey, P.R. Impact of dronedarone on patients with atrial fibrillation and diabetes: A sub-analysis of the ATHENA and EURIDIS/ADONIS studies. J. Diabetes Complicat. 2022, 36, 108227. [Google Scholar] [CrossRef] [PubMed]
- Walters, T.E.; Nisbet, A.; Morris, G.M.; Tan, G.; Mearns, M.; Teo, E.; Lewis, N.; Ng, A.; Gould, P.; Lee, G.; et al. Progression of atrial remodeling in patients with high-burden atrial fibrillation: Implications for early ablative intervention. Heart Rhythm 2016, 13, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.H.; Yu, H.T.; Park, Y.J.; Kim, T.H.; Joung, B.; Lee, M.H.; Pak, H.N. Diabetes Mellitus Is an Independent Risk Factor for a Stiff Left Atrial Physiology After Catheter Ablation for Atrial Fibrillation. Front. Cardiovasc. Med. 2022, 9, 828478. [Google Scholar] [CrossRef] [PubMed]
- Huo, Y.; Gaspar, T.; Schönbauer, R.; Wójcik, M.; Fiedler, L.; Roithinger, F.X.; Martinek, M.; Pürerfellner, H.; Kirstein, B.; Richter, U.; et al. Low-Voltage Myocardium-Guided Ablation Trial of Persistent Atrial Fibrillation. NEJM Evid. 2022, 1, EVIDoa2200141. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A.; Testani, J.M. SGLT2 inhibitors and diuretics in heart failure: Clicking reset on the renal volume setpoint? Eur. Heart J. 2023, 44, 2944–2946. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; Ostrominski, J.W.; Wang, X.; Shah, S.J.; Borlaug, B.A.; Butler, J.; Davies, M.J.; Kitzman, D.W.; Verma, S.; Abildstrøm, S.Z.; et al. STEP-HFpEF Trial Committees and Investigators. Effect of Semaglutide on Cardiac Structure and Function in Patients With Obesity-Related Heart Failure. J. Am. Coll. Cardiol. 2024, 84, 1587–1602. [Google Scholar] [CrossRef] [PubMed]
- Kantharia, B.K.; Lip, G.Y.H.; Martin, D.T. Alterations in atrial electrogram amplitude as steady sinus rhythm transitions to paroxysmal atrial fibrillation during continuous monitoring in patients with implantable cardiac devices: Insights from the IMPACT study. J. Cardiovasc. Electrophysiol. 2021, 32, 1357–1363. [Google Scholar] [CrossRef] [PubMed]
- Scirica, B.M.; Bhatt, D.L.; Braunwald, E.; Steg, P.G.; Davidson, J.; Hirshberg, B.; Ohman, P.; Frederich, R.; Wiviott, S.D.; Hoffman, E.B.; et al. SAVOR-TIMI 53 Steering Committee and Investigators. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N. Engl. J. Med. 2013, 369, 1317–1326. [Google Scholar] [CrossRef] [PubMed]
- Deshaies, R.J. Multispecific drugs herald a new era of biopharmaceutical innovation. Nature 2020, 580, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Molla, G.; Bitew, M. Revolutionizing Personalized Medicine: Synergy with Multi-Omics Data Generation, Main Hurdles, and Future Perspectives. Biomedicines 2024, 12, 2750. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).