Abstract
Breast cancer survivors have to deal with notable challenges even after successful treatment, such as body image issues, depression and anxiety, the stress related to changes in lifestyle, and the continual challenges inherent to health management. The literature suggests that emotional abilities, such as emotional intelligence, emotion management, mood repair, and coping play a fundamental role in such challenges. We performed a systematic review to systematize the evidence available on the role of emotional abilities in quality of life and health management in breast cancer survivors. The search was performed on three scientific databases (Pubmed, Scopus, and PsycINFO) and, after applying exclusion criteria, yielded 33 studies, mainly of a cross-sectional nature. The results clearly support the hypothesis that emotional abilities play multiple important roles in breast cancer survivors’ quality of life. Specifically, the review highlighted that coping/emotional management plays multiple roles in breast cancer survivors’ well-being and health management, affecting vitality and general adjustment to cancer positivity and promoting benefit findings related to the cancer experience; however, rare negative results exist in the literature. This review highlights the relevance of emotional abilities to promoting quality of life in breast cancer survivors. Future review efforts may explore other breast cancer survivors’ emotional abilities, aiming at assessing available instruments and proposing tailored psychological interventions.
1. Introduction
Breast cancer is the most common and curable type of cancer in women []. Last decades’ improvements in radiotherapy, chemotherapy, surgery, as well as in the precision medicine approach notably improved the number of breast cancer survivors. Breast cancer survivors are people who are still alive five years after diagnosis and completed the oncological treatments [,,]. In this sense, cancer survivors have rapidly increased due to the increase in the proportion of the elderly, the growing rates of detection and incidence, and improvement in survival [,]. For example, more than 53,000 women annually receive a breast cancer diagnosis in Italy alone []. However, successful cancer treatment does not mean that survivors have reached a satisfactory level of health and well-being. On the contrary, breast cancer survivorship is associated with several physical and psychological issues possibly lasting for one’s life.
Firstly, cancer treatments bring along issues that negatively affect cancer survivors’ body image, chronic pain, and quality of life []. Undesirable appearance-related side effects, such as visible scarring, hair loss, skin discoloration, muscle weakness, loss or deformities in the breasts, and weight fluctuation, affect physical appearance so that the survivors develop intensive negative feelings, such as anxiety and depression [,,,]. Moreover, sexual dysfunctions frequently lead to dissatisfaction in intimate relationships [,,,]. Secondly, because of the need for continuous care and monitoring, breast cancer survivors have to make and maintain important changes in their lifestyles and life plans (e.g., if and how to return to work or usual activities), which can be associated with stress and persistent negative emotions []. Lastly, women with a history of tumor typically experience fear of recurrence [,,,], namely the persistent fear that cancer may return, which could generate pathological anxiety, depressive episodes, and notable fluctuations in survivors’ motivation to continue managing their own health. It is well-established in the scientific literature that emotions play a major role in all of these processes. Emotions are the cognitive and physiological processes that allow people to understand the relevance of stimuli and events in the external environment for their present life and objectives []; the arousal or physiological activation generated by the perception of the stimulus is elaborated by an appraisal process that allows the individual to identify the behavior to respond to the stimuli (e.g., approaching a pleasant stimulus or avoiding a dangerous one). However, people differ in their ability to deal with their emotions and consequently in adopting optimal reactions to avoid any dysfunctional effects of environmental stimuli and emotions themselves [,]. For this reason, it is important to develop tools and resources to assess and possibly improve people’s ability to recognize and manage emotions, especially within delicate contexts such as chronic health management. Secondarily, the experience of emotions directly influences the outcomes of decision-making; emotions affect attention, memory, and notably contribute to the generation of meaning [,]. A breast cancer survivor who would be proficient in recognition of her own and others’ emotions would also be more able to make optimal decisions regarding her care, and reduce the influence of cognitive biases typical of chronic disease management [] as well as make good use of social support resources.
Given the prominent role of emotions in breast cancer survivors’ quality of life and health management, it is important to consider the individual abilities to understand and manage emotions so that they do not constitute an obstacle to health and well-being []. Psychological research has identified several abilities, sometimes different, partially overlapping constructs that pertain to the effective management of emotions. Emotional intelligence, functional coping, emotional management, and mood repair are all concepts that belong to psychological science’s theoretical background and pertain to the abilities to recognize, manage, and make good use of emotions to achieve health and well-being.
Emotional intelligence could be defined as a type of social intelligence that involves the ability to perceive, monitor, and express one’s and others’ emotions, discriminate among them, and use such information to guide and manage one’s thinking and actions voluntarily [,]. While this popular concept has yielded an impressive number of studies in the last decades, it is still an object of controversy []. Specifically, psychologists debate whether emotional intelligence should be considered a collection of cognitive capacities, to be measured by performance tasks similar to those used to measure “cognitive” intelligence, or a complexity of convictions about one’s abilities regarding emotions, plausibly rooted in successful mastery of emotion-related tasks, ultimately similar to a specific type of self-efficacy or a personality trait. While developing emotional intelligence measurement tools based on performance tasks is difficult (e.g., how to determine the “right emotions” to feel within a given scenario?), the trait-like conception of emotional intelligence has allowed researchers to develop some self-report measures such as the TEIQUE and the BEIS. These scales demonstrated good reliability as well as the capacity to predict quality of life and health management outcomes [].
Across emotion studies, coping and emotional management are broad terms that refer to the cognitive strategies an individual may use to manage emotions, especially when trying to avoid excessive emotional activation negatively influencing daily life. Most theoretical models on coping distinguish between multiple strategies. In general, the research shows that dysfunctional strategies relate to disengagement, avoidance, or the suppression of the emotion; those strategies tend to be effective in the short term, but they are scarcely related to long-term achievements and positive behavioral change. On the contrary, mature strategies involve re-appraisal and problem solving focused on the emotional stimulus, and are positively associated with several aspects of well-being and negatively related to distress or other negative states.
While emotions are usually conceptualized as the response to specific internal or external stimuli, mood can be defined as a diffuse, nonspecific affective state which lasts relatively long periods (e.g., days) [,,]; a person in a “bad mood” may be unsure about the exact reason for his or her emotional state, yet may feel more or less impaired in some tasks (e.g., putting low effort in everyday activities; engaging in rumination and negative thoughts). In this sense, mood repair refers to the ability to modify one’s mood, for example by voluntarily recovering positive memories or engaging in pleasant activities [].
The research on emotional abilities in cancer survivors can be traced back to the first decade of 2000, with a strong focus on coping/emotion regulation. A recent meta-analysis [] on emotion regulation and its effects on psychological distress in cancer survivors (not only breast) found studies equally distributed across the globe (Europe: five; Americas: four; and Asia: six). However, the authors also reported that high variability among the reviewed studies (e.g., type of cancer and country), also considering their relatively small number, made it difficult to explain some inconsistent results (i.e., positive, negative or inexistent association between emotion regulation strategies and distress). Furthermore, only studies on emotional suppression were included in the meta-analysis, possibly implying that the literature in its entirety was not ready for meta-analytic efforts. In any case, it is still paramount to identify the role of emotional abilities in psychological processes relevant to the quality of life and health management, not only psychological distress; therefore, we planned the present systematic review limiting the focus to breast cancer (along with its specific psychological issues described above) but extending it regarding all emotional abilities and variables relevant to breast cancer survivors’ quality of life and well-being.
On these bases, we conducted this systematic review to identify the role of emotion-related abilities (emotion regulation/coping, emotional intelligence, and mood regulation) in breast cancer survivors’ overall quality of life. Given the complexity of the topic, we adopted a broad approach by systematically searching for studies that assess the multiple constructs that fall under the aegis of emotion-related abilities.
2. Methods
We conducted a systematic review of the published literature in January 2022 on three databases (PUBMED, PsycINFO, and Scopus) without temporal limits. The present literature review was performed according to PRISMA guidelines [] (Figure 1 features the systematic review flow), and studies were identified through the keywords “emotional intelligence” OR “emotion regulation” OR “mood repair” OR “emotional management” OR “coping” AND “breast cancer survivors” OR “breast cancer survivorship”. These key terms were considered able to retrieve contributions that assess the role of emotion-related abilities in the quality of life of breast cancer survivors. Studies were included if they met the following four criteria: (1) studies that assess emotion-related abilities; (2) studies that examined the impact of emotion abilities on quality of life; (3) breast cancer survivors as a sample (at least one group in case of multiple experimental groups); and (4) studies written in English. As stated in other studies (e.g., [,,,]), the authors placed a priori restrictions by excluding “gray literature” (e.g., doctoral dissertation, conference abstracts, and other non-peer-reviewed sources) to improve review manageability. We placed no limitations on the age of participants and statistical presentation of results.
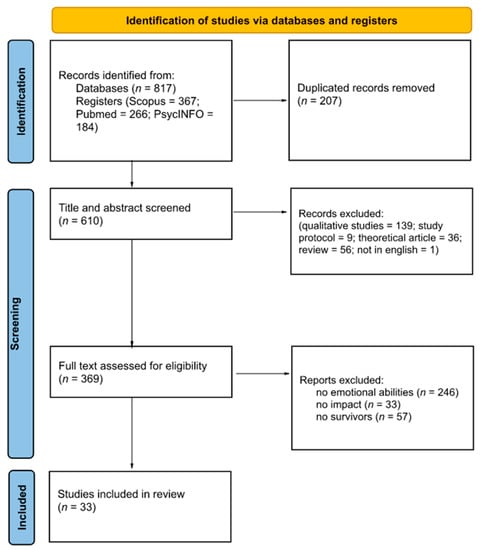
Figure 1.
PRISMA diagram.
Moreover, as the keywords show, we did not focus on specific measures of quality of life; indeed, the definition of quality of life is still challenged to this day [], and it notably varies across different studies, cultures, and methodological approaches. For this reason, we avoided looking only for studies that explicitly mentioned the quality of life; on the contrary, we demanded the quality of life features to the further selection phases, therefore including any study that analyzed the effects of emotional abilities on variables relevant to the quality of life (e.g., psychological well-being, resilience, psychological distress, adjustment to the disease, reduction in psychopathological symptoms, etc.). This allowed the search to identify useful studies beyond the limitations inherent to the concept of the “quality of life”, and to recognize the importance of research focused on specific variables that affect the overall quality of breast cancer survivors’ everyday living and health management.
Study Selection
The search process resulted in the identification of 817 articles. We then removed 207 articles as duplicates. The first screening was done on the title and abstract of the resulting 610 contributions. Four researchers (I.D., S.T., L.S., and V.S.) coded the studies. Discrepancies were resolved through discussions between raters to reach a consensus.
Only research articles have been considered (reviews, opinions, study protocol, and editorials were excluded). According to Marzorati and colleagues [], we considered breast cancer survivors all the participants who have completed the oncological treatments and satisfied the defined inclusion criteria.
At the end of this first screening phase, 241 articles were excluded. Subsequently, the full texts of the retrieved articles (369) were analyzed to identify articles that involved emotional abilities to improve the quality of life in breast cancer survivors. We excluded articles in which the term “coping” or others relevant for the present review were used in a broad sense (e.g., patients engaging in activities and hobbies to improve wellness but not in the sense of emotion regulation strategies). Secondarily, we also excluded articles that used the term “breast cancer survivors” but actually featured other samples in the studies (e.g., patients still undergoing treatment; survivors’ caregivers) and articles that dealt with emotion-related abilities to some extent but did not measure their impact on quality of life (e.g., coping abilities were the dependent variable). At the end of this screening phase, 336 articles were excluded. Thus, 33 studies were included in this systematic review (see Figure 1). All the studies were published between 2000 and 2021.
To control for potential selection bias, the raters independently screened 20% of the 33 articles potentially relevant for inclusion in this systematic review. Cohen’s k for the interrater agreement was 1.00.
For each selected study, two researchers extracted in a blinded manner: authors, study design, sample, brief study description, and outcomes of interest for the present review.
3. Results
The methodological quality of each study was assessed by two authors independently (L.S. and V.S.). The Cochrane risk of bias tool, version 2 [] was used to evaluate each domain and its specific risks, indicating as “low risk”, “some concerns”, and “high risk”. The overall quality of the studies is high if the assessment of all the domains results in low. Discrepancies between raters were resolved through discussions with the first and the second authors (I.D. and S.T.). The results of the analysis are presented in Table 1.

Table 1.
Risk-of-bias analysis of the selected studies.
The results of the present review clearly support the hypothesis that emotional abilities play multiple important roles in breast cancer survivors’ quality of life and health management (see Table 2 for a synthesis of the studies and Table 3 for a list of the tools used in the selected articles to assess the quality of life or related variables). As clearly summarized in Table 2, all the outcome variables explored in the selected studies fall into different dimension(s) of quality of life: emotional, cognitive, social, physical, and spiritual.

Table 2.
Synthesis of studies included in the review according to study design, sample, aim, outcomes of interest. The “Quality of life area” column refers to the dimension(s) of quality of life that are affected by the study, taking into consideration the outcome variables.

Table 3.
List of the tools used to assess Quality of Life or related variables and related ranges.
The emotional area was the most investigated area across the reviewed studies. Studies included in this area mainly explored the coping/emotional management, or the adoption of different cognitive strategies to manage one’s emotions. Certainly, emotional abilities have an important impact on the emotional dimension of quality of life as their direct effect is improving the management of affective experiences. However, the reviewed studies clearly show that emotional abilities influence other dimensions of quality of life, depending on the focus of the individual study. For example, when studies focused on patient-physician relationship or the ability to find social support, emotional abilities such as coping demonstrated to help patients communicate their mental and physical health effectively, which could be construed as improvement in the social dimension of QoL [,]. Similarly, improvements in physical quality of life were observed in studies that included treatment outcomes and/or adherence to physical exercise [,,,,,]; conversely, dysfunctional emotional management appeared associated with lower physical QoL as well as with fatigue and lower adherence to exercise. Regarding cognitive QoL, active coping skills and emotional intelligence appear associated with the development of cognitive abilities (e.g., reframing) that help patients to avoid biases and potentially-disruptive representations of their condition (e.g., rumination) [,,]. Moreover, active emotional management predicts the ability to adopt healthy mental representations of the illness experience (e.g., benefit finding, acceptance) [,]. Finally, two studies included in the sample referred to spiritual aspects, which can be considered a further area for QoL [,]: they report that religious beliefs could inform emotional management strategies. Most of the reviewed studies are consistent with one of the main tenets of coping theories, that is, emotional management strategies may be functional or dysfunctional, leading to opposite effects in terms of quality of life in the specific population of breast cancer survivors.
Optimal, functional strategies typically relate to reappraisal, problem-solving and achieving control over emotional situations and stimuli. The reviewed studies showed that the adoption of active coping strategies and problem-solving techniques predicts factors important for quality of life and health management, such as optimism [], benefit finding [], vitality and cancer adjustment [], finding new possibilities, and promoting appreciation for life []; they also directly impact quality of life, well-being, and psychological symptoms, such as depression and anxiety [45, 47,49–57]. Additionally, some authors highlighted that coping skills allow breast cancer survivors to improve their cognitive reframing [], and to reduce distress and fatigue []. From a psychological point of view, coping self-efficacy beliefs, and reassurance-seeking behaviors, were significant predictors of lower fear of recurrence [].
One reviewed study also revealed the impact of coping on physical-related symptoms (i.e., somatic symptoms []). Active coping predicts important factors related to social relationships and the relationships with others [], and support seeking [].
Other studies showed that the adoption of passive or avoidant coping strategies could have a negative impact on breast cancer survivors’ quality of life [,] influencing psychological distress [,], and depression []. Additionally, disengagement-oriented coping and brooding (indicator of rumination thinking) partially mediated the relationship between social constraints and adjustment []. Negative coping, such as dysfunctional coping, could also affect people’s perception of control over their own clinical plan (e.g., treatment control []) and could promote negative emotions such as depression and anxiety []. Ambivalence over emotional expression was associated with lower follow-up quality of life beyond the effect of expressive suppression [].
Although these studies highlighted the positive impact of coping strategies on breast cancer survivors’ quality of life, two studies included in the review highlighted some negative results related to the impact of emotional abilities on people’s well-being. Specifically, Ridner and colleagues [] highlighted that the involvement in intervention focused on improving well-being and the coping strategies resulted in no significant differences between the experimental and control groups. In addition, Lelorain and colleagues [] reported a non-significant negative relationship between active coping and quality of life and Lyons and colleagues [] found that coping styles were not correlated with changes in quality of life, depression, or anxiety.
Additionally, emotional intelligence and its sub-components may promote resilience in breast cancer survivors, decreasing vulnerability and mood repair []. As highlighted by Rocio Guil and colleagues [], personal abilities to recognize, discriminate, and regulate emotional states are positively associated with personal growth after the oncological diagnosis. Although the cancer diagnosis is related to negative emotional reactions, it seems that people are able to increase their capacity to repair them effectively.
On the other hand, emotional intelligence is not always beneficial. People who pay great attention to their personal emotions can also have harmful consequences. For example, their ability to regulate emotions could be reduced, acting as a non-protective factor for the promotion of quality of life. This could be related to the level of specific abilities in each person.
We feel it is interesting to report that a number of articles (6) emerged in our first search that did not feature data focused on the impact of emotional abilities but were all focused on the specific construct of self-compassion. We discussed the possibility that self-compassion could be considered an emotional ability such as coping or emotional intelligence, but we decided it is not an “ability” in a strict sense. It is more described as a tendency to experience feelings of kindness towards oneself, as well as a compassionate look towards one’s own failures or flaws []. In this sense, it seems to be conceptualized more as a personality trait or attitude. Yet, it is possible that it is related to positive reframing of negative events; indeed, it is associated with adaptive coping [,] and emotional stability [] and it contributes to predicting health and well-being also in chronic illness contexts [,]. An interesting aim for future review efforts could be to explore the relationship or partial overlapping between emotional abilities and self-compassion.
4. Discussion
This review aims to identify the role of breast cancer survivors’ emotional abilities to improve aspects relevant to the overall quality of life, which the studies assessed according to multiple constructs, including coping/emotional management, emotional intelligence, and mood repair. The first relevant aspect emerging from the retrieved articles is that coping/emotional management play multiple important roles in breast cancer survivors’ well-being and health management. In general, the reviewed studies on proactive coping revealed that these strategies positively affect vitality and general adjustment to cancer. Indeed, active coping strategies (e.g., positive reframing and acceptance) affected benefit findings related to cancer experience. However, at least one study [] reported a non-significant negative relationship between active coping and quality of life, measured by the MOS SF-36 tool. Authors speculated that active coping could become an exhausting strategy during highly stressful events, such as health management after cancer diagnosis. In other words, even active coping strategies may be ineffective and, at the same time, tiring for people dealing with continual health management challenges.
This is consistent with Baziliansky and Coehn’s meta-analysis [], which was focused on emotion regulation and its effects on psychological distress in cancer survivors: they found that coping strategies were correlated with distress, but also negative and non-significant relationships were reported [,]. To sum up, while especially active coping strategies deserve to be promoted in breast cancer survivors, as they appear consistently associated with positive outcomes, clinicians should take into account that the enactment of coping strategies could generate fatigue, especially when individuals have to deal with long-lasting challenges such as health management in chronic conditions.
Taking into consideration all emotional abilities, coping/emotional management was notably over-represented in the reviewed studies.
Much to our surprise, the application of inclusion criteria led to identifying one study only whose main theoretical construct was emotional intelligence []. Notably, this study found that EI (higher in breast cancer survivors than in healthy women) predicted resilience. This result supports the idea that emotional intelligence directly affects one’s ability to deal with challenging circumstances, withstanding and adapting to traumatic and adverse events. This calls for further research on the relationship between personal resources in cancer survivorship and emotional intelligence. Even when it is understood as “perceived EI” or “emotional self-efficacy”, this emotional ability goes beyond the tendency to adopt one more or less effective coping strategy and reflects breast cancer survivors’ perceived ability to understand and manage their own and others’ emotions. As speculation, a patient/survivor who has high emotional intelligence is not more able to manage a specific emotion only, but also to effectively design their own journey across care and health management (e.g., by better understanding their doctor; by helping caregivers in their task without feeling like a burden; by engaging in less biased decision making about treatment and changes in lifestyle; etc.). Indeed, emotional intelligence entails access to a rich “toolbox” of resources one could effectively employ to adapt to challenging contexts, this way improving resilience. Accordingly, one recent study [], published after the completion of this review process, found that perceived EI and survivorship predicted 37.8% of the variance of depression; the article also suggested that subcomponents of EI are particularly important to develop when facing the experience of breast cancer, namely emotional clarity (the extent to which individuals can unambiguously identify, label, and mentally represent the type and source or of emotions they feel) and emotional repair (the capacity to successfully improve negative moods). It seems that emotional intelligence deserves more research in the field of psycho-oncology, paying attention to its impact on quality of life and protection against negative outcomes such as depression. Its conceptualization as a form of emotional self-efficacy or actual intelligence may be more helpful to develop interventions aimed at its improvement than the conceptualization as a personality trait, that hints at stability over time and leaves less room for modification. Furthermore, it could be interesting to analyze by dedicated research how specific emotional intelligence sub-constructs affect specific needs of breast cancer survivors across their health journey (e.g., when accessing health services, when building social support, or others). Regarding the third emotional ability, namely mood repair, the present review did not yield results focused on this construct specifically, besides the study by Rocio-Guil and colleagues [], which considered it a component of emotional intelligence. Mood repair is associated with the ability to modify one’s own overall mood during the day, as a subtle, unspecific emotional state independent of simulations that could be identified clearly within the environment []. As a direction for future research, it could be interesting to explore this specific construct, both in terms of breast cancer survivors’ quality of life and of the actual degree of its independence from the other emotional abilities, which scholars tend to conceptualize as focused on emotions generated by specific stimuli or events.
While the main results of the present review confirm that active coping strategies are important and effective and should be promoted in cancer survivors, future research may explore further the emotion-related abilities, beyond the mere selection of coping strategies. The concept of “emotional management” should not be reduced to one’s ability to reduce or avoid negative emotions. On the contrary, understanding one’s own emotional journey in depth permits the cultivation of new personal resources, as it happens for example in post-traumatic growth []. It is possible that new and more nuanced theoretical constructs are needed to guide future studies in the field of emotion-related abilities for chronic health management.
To sum up, this review highlights the relevance of emotional abilities to promote quality of life, well-being and health management in breast cancer survivors. Our study has some limitations. Although three databases can be regarded as a sufficient number for a systematic review, employing more sources could allow future reviews to be more comprehensive on similar issues. Secondarily, we decided not to include “quality of life” as a keyword in order to find contributions relevant to a broad conception of quality of life (even those papers that did not explicitly refer to this construct); while such approach allowed us to include more relevant studies than focused review efforts [] and possibly to obtain more information on psychological processes related to emotions, it could be interesting to analyze the relationship between emotional abilities and validated measures specifically focused on quality of life. This could be both a direction for future research and reviews, taking into account that the construct of “quality of life” has been recently challenged due to its instability across different theoretical approaches and cultural contexts []. Future reviews may also explore other breast cancer survivors’ emotional abilities, aiming at assessing available instruments and proposing tailored psychological interventions. Moreover, the present review highlighted the importance to study the effects of specific emotional abilities on multiple variables relevant to quality of life: aiming for specificity beyond coping strategies would allow health professionals and researchers to design different kinds of interventions to improve breast cancer survivors’ ability to cope with the illness and achieve a desirable level of psychological well-being. It could be interesting to assess emotional management related to specific issues that are common in the experience of chronic patients and survivors, such as for example return to work [,], intimacy and couple infertility [,], and choice of treatment []. Furthermore, the review highlights that the same conceptualization of emotional abilities deserves to be further improved, recognizing their impact within the specific context of individual chronic illnesses and health journeys in order to develop intervention tools focused on patient experience.
Author Contributions
Conceptualization, I.D.; methodology, I.D. and S.T.; formal analysis, I.D., S.T., L.S. and V.S.; resources, G.P.; data curation, I.D., S.T., L.S. and V.S.; writing—original draft preparation, I.D. and S.T.; writing—review and editing, I.D., S.T., L.S. and V.S.; supervision, G.P. All authors have read and agreed to the published version of the manuscript.
Funding
There was no specific funding for this research.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.
Acknowledgments
This work was partially supported by the Italian Ministry of Health with Ricerca Corrente and 5 × 1000 funds for IEO European Institute of Oncology IRCCS. ID was supported by Fondazione IEO-CCM. LS and VS are Ph.D. students within the European School of Molecular Medicine (SEMM).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Maleki, M.; Mardani, A.; Ghafourifard, M.; Vaismoradi, M. Qualitative Exploration of Sexual Life among Breast Cancer Survivors at Reproductive Age. BMC Womens Health 2021, 21, 56. [Google Scholar] [CrossRef]
- Invernizzi, M.; de Sire, A.; Venetis, K.; Cigna, E.; Carda, S.; Borg, M.; Cisari, C.; Fusco, N. Quality of Life Interventions in Breast Cancer Survivors: State of the Art in Targeted Rehabilitation Strategies. Anti-Cancer Agents Med. Chem. 2022, 22, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.M.; Park, S.M. Care for Breast Cancer Survivors. In Translational Research in Breast Cancer; Noh, D., Han, W., Toi, M., Eds.; Springer: New York, NY, USA, 2021; pp. 511–524. [Google Scholar] [CrossRef]
- Carreira, H.; Williams, R.; Dempsey, H.; Stanway, S.; Smeeth, L.; Bhaskaran, K. Quality of Life and Mental Health in Breast Cancer Survivors Compared with Non-Cancer Controls: A Study of Patient-Reported Outcomes in the United Kingdom. J. Cancer Surviv. 2021, 15, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Coebergh, J.; Janssen-Heijnen, M.; Louwman, W.; Voogd, A. Cancer Incidence and Survival in the South of the Netherlands, 1955–1999 and Incidence in the North of Belgium, 1996–1998; Comprehensive Cancer Centre South (IKZ): Eindhoven, The Netherlands, 2001. [Google Scholar]
- Coleman, M.P.; Gatta, G.; Verdecchia, A.; Estève, J.; Sant, M.; Storm, H.; Allemani, C.; Ciccolallo, L.; Santaquilani, M.; Berrino, F. EUROCARE-3 Summary: Cancer Survival in Europe at the End of the 20th Century. Ann. Oncol. 2003, 14, v128–v149. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Rodriguez, J.L.; O’Brien, K.M.; Nichols, H.B.; Hodgson, M.E.; Weinberg, C.R.; Sandler, D.P. Health-related Quality of Life Outcomes among Breast Cancer Survivors. Cancer 2021, 127, 1114–1125. [Google Scholar] [CrossRef] [PubMed]
- Triberti, S.; Savioni, L.; Sebri, V.; Pravettoni, G. EHealth for Improving Quality of Life in Breast Cancer Patients: A Systematic Review. Cancer Treat. Rev. 2019, 74, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Reich, M.; Lesur, A.; Perdrizet-Chevallier, C. Depression, Quality of Life and Breast Cancer: A Review of the Literature. Breast Cancer Res. Treat. 2008, 110, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Triberti, S.; Gorini, A.; Savioni, L.; Sebri, V.; Pravettoni, G. Avatars and the Disease: Digital Customization as a Resource for Self-Perception Assessment in Breast Cancer Patients. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 558–564. [Google Scholar] [CrossRef]
- Falk Dahl, C.A.; Reinertsen, K.V.; Nesvold, I.-L.; Fosså, S.D.; Dahl, A.A. A Study of Body Image in Long-Term Breast Cancer Survivors. Cancer 2010, 116, 3549–3557. [Google Scholar] [CrossRef]
- Male, D.A.; Fergus, K.D.; Cullen, K. Sexual Identity after Breast Cancer: Sexuality, Body Image, and Relationship Repercussions. Curr. Opin. Support. Palliat. Care 2016, 10, 66–74. [Google Scholar] [CrossRef]
- Wilmoth, M.C. The Aftermath of Breast Cancer: An Altered Sexual Self. Cancer Nurs. 2001, 24, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Sebri, V.; Durosini, I.; Triberti, S.; Pravettoni, G. The Efficacy of Psychological Intervention on Body Image in Breast Cancer Patients and Survivors: A Systematic-Review and Meta-Analysis. Front. Psychol. 2021, 12, 611954. [Google Scholar] [CrossRef] [PubMed]
- Słowik, A.Ž.D.; Jabłoński, M.; Michałowska-Kaczmarczyk, A.; Jach, R. Evaluation of Quality of Life in Women with Breast Cancer, with Particular Emphasis on Sexual Satisfaction, Future Perspectives and Body Image, Depending on the Method of Surgery. Psychiatr. Pol. 2017, 51, 871–888. [Google Scholar] [CrossRef] [PubMed]
- Lucas, A.; Focht, B.; Cohn, D.; Klatt, M.; Buckworth, J. Recruiting Endometrial Cancer Survivors to Studies Examining Lifestyle Behaviors and Quality of Life: Challenges Faced and Lessons Learned. J. Cancer Educ. 2018, 12, 857–864. [Google Scholar] [CrossRef]
- Dunn, L.B.; Langford, D.J.; Paul, S.M.; Berman, M.B.; Shumay, D.M.; Kober, K.; Merriman, J.D.; West, C.; Neuhaus, J.M.; Miaskowski, C. Trajectories of Fear of Recurrence in Women with Breast Cancer. Support. Care Cancer 2015, 23, 2033–2043. [Google Scholar] [CrossRef]
- Ozga, M.; Aghajanian, C.; Myers-Virtue, S.; McDonnell, G.; Jhanwar, S.; Hichenberg, S.; Sulimanoff, I. A Systematic Review of Ovarian Cancer and Fear of Recurrence. Palliat. Support. Care 2013, 13, 1771–1780. [Google Scholar] [CrossRef]
- Northouse, L.L. Mastectomy Patients and the Fear of Cancer Recurrence. Cancer Nurs. 1981, 4, 213–220. [Google Scholar] [CrossRef]
- Simard, S.; Thewes, B.; Humphris, G.; Dixon, M.; Hayden, C.; Mireskandari, S.; Ozakinci, G. Fear of Cancer Recurrence in Adult Cancer Survivors: A Systematic Review of Quantitative Studies. J. Cancer Surviv. 2013, 7, 300–322. [Google Scholar] [CrossRef]
- Frijda, N.H. The Emotions: Studies in Emotion and Social Interaction; Cambridge University Press: Cambridge, UK, 1986; p. 560. [Google Scholar] [CrossRef]
- Kreibig, S.D. Autonomic Nervous System Activity in Emotion: A Review. Biol. Psychol. 2010, 84, 394–421. [Google Scholar] [CrossRef]
- Stemmler, G.; Wacker, J. Personality, Emotion, and Individual Differences in Physiological Responses. Biol. Psychol. 2010, 84, 541–551. [Google Scholar] [CrossRef]
- Mazzocco, K.; Masiero, M.; Carriero, M.C.; Pravettoni, G. The Role of Emotions in Cancer Patients’ Decision-Making. Ecancermedicalscience 2019, 13, 914. [Google Scholar] [CrossRef] [PubMed]
- Triberti, S.; Chirico, A.; La Rocca, G.; Riva, G. Developing Emotional Design: Emotions as Cognitive Processes and Their Role in the Design of Interactive Technologies. Front. Psychol. 2017, 8, 1773. [Google Scholar] [CrossRef] [PubMed]
- Savioni, L.; Triberti, S. Cognitive Biases in Chronic Illness and Their Impact on Patients’ Commitment. Front. Psychol. 2020, 11, 579455. [Google Scholar] [CrossRef] [PubMed]
- Pourfallahi, M.; Gholami, M.; Tarrahi, M.J.; Toulabi, T.; Kordestani Moghadam, P. The Effect of Informational-Emotional Support Program on Illness Perceptions and Emotional Coping of Cancer Patients Undergoing Chemotherapy. Support. Care Cancer 2020, 28, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Salovey, P.; Mayer, J.D. Emotional Intelligence and Its Relationship to Other Intelligences. Imagin. Cogn. Pers. 1990, 9, 185–211. [Google Scholar] [CrossRef]
- Brackett, M.A.; Rivers, S.E.; Salovey, P. Emotional Intelligence: Implications for Personal, Social, Academic, and Workplace Success. Soc. Personal. Psychol. Compass 2011, 5, 88–103. [Google Scholar] [CrossRef]
- Guil, R.; Ruiz-González, P.; Merchán-Clavellino, A.; Morales-Sánchez, L.; Zayas, A.; Gómez-Molinero, R. Breast Cancer and Resilience: The Controversial Role of Perceived Emotional Intelligence. Front. Psychol. 2020, 11, 595713. [Google Scholar] [CrossRef]
- Durosini, I.; Triberti, S.; Ongaro, G.; Pravettoni, G. Validation of the Italian Version of the Brief Emotional Intelligence Scale (BEIS-10). Psychol. Rep. 2020, 124, 003329412095977. [Google Scholar] [CrossRef]
- Forgas, J.P. Mood Effects on Decision Making Strategies. Aust. J. Psychol. 1989, 41, 197–214. [Google Scholar] [CrossRef]
- Frijda, N.H. Appraisal and Beyond: Special Issue of Cognition and Emotion; Erlbaum: Hillsdale, NJ, USA, 1993. [Google Scholar]
- Russell, J.A. Core Affect and the Psychological Construction of Emotion. Psychol. Rev. 2003, 110, 145–172. [Google Scholar] [CrossRef]
- Chen, L.; Zhou, S.; Bryant, J. Temporal Changes in Mood Repair through Music Consumption: Effects of Mood, Mood Salience, and Individual Differences. Media Psychol. 2007, 9, 695–713. [Google Scholar] [CrossRef]
- Baziliansky, S.; Cohen, M. Emotion regulation and psychological distress in cancer survivors: A systematic review and meta-analysis. Stress Health 2021, 37, 3–18. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Heckel, L.; Heynsbergh, N.L.; Livingston, P.M. Are cancer helplines effective in supporting caregivers? A systematic review. Support. Care Cancer 2019, 27, 3219–3231. [Google Scholar] [CrossRef] [PubMed]
- Pan-Weisz, T.M.; Kryza-Lacombe, M.; Burkeen, J.; Hattangadi-Gluth, J.; Malcarne, V.L.; McDonald, C.R. Patient-reported health-related quality of life outcomes in supportive-care interventions for adults with brain tumors: A systematic review. Psycho-Oncol. 2019, 28, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Durosini, I.; Aschieri, F. Therapeutic assessment efficacy: A meta-analysis. Psychol. Assess. 2021, 33, 962–972. [Google Scholar] [CrossRef] [PubMed]
- Barbagelata, K.; Eadi, J.; McNamara, M.; Sayles, M.; Smith, J.M. Aquatic Therapy Reduces Pain and Fatigue in Breast Cancer Survivors: A Systematic Review. Rehab. Oncol. 2021, 39, E35–E41. [Google Scholar] [CrossRef]
- Haraldstad, K.; Wahl, A.; Andenæs, R.; Andersen, J.R.; Andersen, M.H.; Beisland, E.; Borge, C.R.; Engebretsen, E.; Eisemann, M.; Halvorsrud, L.; et al. A systematic review of quality of life research in medicine and health sciences. Qual. Life Res. 2019, 28, 2641–2650. [Google Scholar] [CrossRef] [PubMed]
- Marzorati, C.; Riva, S.; Pravettoni, G. Who is a cancer survivor? A systematic review of published definitions. J. Cancer Educ. 2017, 32, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Karademas, E.C.; Karvelis, S.; Argyropoulou, K. Stress-related predictors of optimism in breast cancer survivors. Stress Health J. Int. Soc. Investig. Stress 2007, 23, 161–168. [Google Scholar] [CrossRef]
- Wen, K.Y.; Ma, X.S.; Fang, C.; Song, Y.; Tan, Y.; Seals, B.; Ma, G.X. Psychosocial Correlates of Benefit Finding in Breast Cancer Survivors in China. J. Health Psychol. 2017, 22, 1731–1742. [Google Scholar] [CrossRef]
- Low, C.A.; Stanton, A.L.; Thompson, N.; Kwan, L.; Ganz, P.A. Contextual Life Stress and Coping Strategies as Predictors of Adjustment to Breast Cancer Survivorship. Ann. Behav. Med. 2006, 32, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Bellizzi, K.M.; Blank, T.O. Predicting posttraumatic growth in breast cancer survivors. Health Psychol. 2006, 25, 47. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.T.; Ho, S.M.Y.; Liu, W.K.; Hou, Y.C.; Lim, L.C.; Gao, S.Y.; Chang, W.Y.; Wang, G.L. Cancer-Coping Profile Predicts Long-Term Psychological Functions and Quality of Life in Cancer Survivors. Support. Care Cancer 2019, 27, 933–941. [Google Scholar] [CrossRef]
- Boehmer, U.; Glickman, M.; Winter, M.; Clark, M.A. Lesbian and Bisexual Women’s Adjustment After a Breast Cancer Diagnosis. J. Am. Psychiatr. Nurses Assoc. 2013, 19, 280–292. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Gallagher, M.W.; Loh, A.; Young, L. Expressive Writing Intervention Improves Quality of Life among Chinese-American Breast Cancer Survivors: A Randomized Controlled Trial. Ann. Behav. Med. 2018, 52, 952–962. [Google Scholar] [CrossRef]
- Gall, T.L. Integrating religious resources within a general model of stress and coping: Long-term adjustment to breast cancer. J. Relig. Health 2000, 39, 167–182. [Google Scholar] [CrossRef]
- Mishel, M.H.; Germino, B.B.; Gil, K.M.; Belyea, M.; LaNey, I.C.; Stewart, J.; Porter, L.; Clayton, M. Benefits from an uncertainty management intervention for African-American and Caucasian older long-term breast cancer survivors. Psycho Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2005, 14, 962–978. [Google Scholar] [CrossRef]
- Johns, S.A.; Stutz, P.V.; Talib, T.L.; Cohee, A.A.; Beck-Coon, K.A.; Brown, L.F.; Wilhelm, L.R.; Monahan, P.O.; LaPradd, M.L.; Champion, V.L.; et al. Acceptance and commitment therapy for breast cancer survivors with fear of cancer recurrence: A 3-arm pilot randomized controlled trial. Cancer 2020, 126, 211–218. [Google Scholar] [CrossRef]
- Chu, Q.; Wong, C.C.Y.; Lu, Q. Acculturation moderates the effects of expressive writing on post-traumatic stress symptoms among Chinese American breast cancer survivors. Int. J. Behav. Med. 2019, 26, 185–194. [Google Scholar] [CrossRef]
- Carpenter, K.M.; Stoner, S.A.; Schmitz, K.; McGregor, B.A.; Doorenbos, A.Z. An online stress management workbook for breast cancer. J. Behav. Med. 2014, 37, 458–468. [Google Scholar] [CrossRef] [PubMed]
- Beatty, L.; Oxlad, M.; Koczwara, B.; Wade, T.D. A randomised pilot of a self-help workbook intervention for breast cancer survivors. Support. Care Cancer 2010, 18, 1597–1603. [Google Scholar] [CrossRef]
- Levkovich, I.; Cohen, M.; Alon, S.; Kuchuk, I.; Nissenbaum, B.; Evron, E.; Pollack, S.; Fried, G. Symptom cluster of emotional distress, fatigue and cognitive difficulties among young and older breast cancer survivors: The mediating role of subjective stress. J. Geriatr. Oncol. 2018, 9, 469–475. [Google Scholar] [CrossRef] [PubMed]
- McGinty, H.L.; Small, B.J.; Laronga, C.; Jacobsen, P.B. Predictors and patterns of fear of cancer recurrence in breast cancer survivors. Health Psychol. 2016, 35, 1. [Google Scholar] [CrossRef] [PubMed]
- Karademas, E.C.; Argyropoulou, K.; Karvelis, S. Psychological symptoms of breast cancer survivors: A comparison with matched healthy controls and the association with cancer-related stress and coping. J. Psychosoc. Oncol. 2007, 25, 59–74. [Google Scholar] [CrossRef]
- Fischer, M.J.; Wiesenhaan, M.E.; Heijer, A.D.D.; Kleijn, W.C.; Nortier, J.W.R.; Kaptein, A.A. From Despair to Hope: A Longitudinal Study of Illness Perceptions and Coping in a Psycho-Educational Group Intervention for Women with Breast Cancer. Br. J. Health Psychol. 2013, 18, 526–545. [Google Scholar] [CrossRef]
- Achimas-Cadariu, P.; Iancu, M.; Pop, F.; Vlad, C.; Irimie, A. Psychological screening and health related quality of life in Romanian breast cancer survivors. J. Evid. Based Psychother. 2015, 15, 267. [Google Scholar]
- Charlier, C.; Pauwels, E.; Lechner, L.; Spittaels, H.; Bourgois, J.; De Bourdeaudhuij, I.; Van Hoof, E. Physical activity levels and supportive care needs for physical activity among breast cancer survivors with different psychosocial profiles: A cluster-analytical approach. Eur. J. Cancer Care 2012, 21, 790–799. [Google Scholar] [CrossRef] [PubMed]
- Cohee, A.; Johns, S.A.; Alwine, J.S.; Talib, T.; Monahan, P.O.; Stump, T.E.; Cella, D.; Champion, V.L. The Mediating Role of Avoidant Coping in the Relationships between Physical, Psychological, and Social Wellbeing and Distress in Breast Cancer Survivors. Psychooncology 2021, 30, 1129–1136. [Google Scholar] [CrossRef]
- Perez-Tejada, J.; Garmendia, L.; Labaka, A.; Vegas, O.; Gómez-Lazaro, E.; Arregi, A. Active and Passive Coping Strategies Comparing Psychological Distress, Cortisol, and Proinflammatory Cytokine Levels in Breast Cancer Survivors. Clin. J. Oncol. Nurs. 2019, 23, 583–590. [Google Scholar] [CrossRef]
- Radin, A.; Ganz, P.A.; Van Dyk, K.; Stanton, A.L.; Bower, J.E. Executive Functioning and Depressive Symptoms after Cancer: The Mediating Role of Coping. Psychosom. Med. 2021, 83, 291–299. [Google Scholar] [CrossRef]
- Kolokotroni, P.; Anagnostopoulos, F.; Hantzi, A. The Role of Optimism, Social Constraints, Coping, and Cognitive Processing in Psychosocial Adjustment among Breast Cancer Survivors. J. Clin. Psychol. Med. Settings 2018, 25, 452–462. [Google Scholar] [CrossRef]
- Lan, M.; Zhang, L.; Zhang, Y.; Yan, J. The Relationship among Illness Perception, Coping and Functional Exercise Adherence in Chinese Breast Cancer Survivors. J. Adv. Nurs. 2019, 75, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Romeo, A.; Di Tella, M.; Ghiggia, A.; Tesio, V.; Stanizzo, M.R.; Torta, R.; Castelli, L. The Traumatic Experience of Breast Cancer: Which Factors Can Relate to the Post-Traumatic Outcomes? Front. Psychol. 2019, 10, 1–9. [Google Scholar] [CrossRef]
- Lu, Q.; Tsai, W.; Chu, Q.; Xie, J. Is expressive suppression harmful for Chinese American breast cancer survivors? J. Psychosom. Res. 2018, 109, 51–56. [Google Scholar] [CrossRef]
- Ridner, S.H.; Dietrich, M.S.; Davis, A.J.; Sinclair, V. A randomized clinical trial comparing the impact of a web-based multimedia intervention versus an educational pamphlet on patient outcomes in breast cancer survivors with chronic secondary lymphedema. J. Women′s Health 2020, 29, 734–744. [Google Scholar] [CrossRef]
- Lelorain, S.; Tessier, P.; Florin, A.; Bonnaud-Antignac, A. Predicting Mental Quality of Life in Breast Cancer Survivors Using Comparison Participants. J. Psychosoc. Oncol. 2011, 29, 430–449. [Google Scholar] [CrossRef]
- Lyons, K.D.; Hull, J.G.; Kaufman, P.A.; Li, Z.; Seville, J.L.; Ahles, T.A.; Kornblith, A.B.; Hegel, M.T. Development and initial evaluation of a telephone-delivered, behavioral activation, and problem-solving treatment program to address functional goals of breast cancer survivors. J. Psychosoc. Oncol. 2015, 33, 199–218. [Google Scholar] [CrossRef] [PubMed]
- Wonghongkul, T.; Dechaprom, N.; Phumivichuvate, L.; Losawatkul, S. Uncertainty appraisal coping and quality of life in breast cancer survivors. Cancer Nurs. 2006, 29, 250–257. [Google Scholar] [CrossRef]
- Raque-Bogdan, T.L.; Lent, R.W.; Lamphere, B. Test of a social cognitive model of well-being among breast cancer survivors. J. Health Psychol. 2019, 24, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Arambasic, J.; Sherman, K.A.; Elder, E.; Breast Cancer Network Australia. Attachment styles, self-compassion, and psychological adjustment in long-term breast cancer survivors. Psycho Oncol. 2019, 28, 1134–1141. [Google Scholar] [CrossRef] [PubMed]
- Neff, K.D. The Development and Validation of a Scale to Measure Self-Compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Mantzios, M.; Wilson, J.C.; Giannou, K. Psychometric Properties of the Greek Versions of the Self-Compassion and Mindful Attention and Awareness Scales. Mindfulness 2015, 6, 123–132. [Google Scholar] [CrossRef]
- Neff, K.D.; Tóth-Király, I.; Yarnell, L.M.; Arimitsu, K.; Castilho, P.; Ghorbani, N.; Guo, H.X.; Hirsch, J.K.; Hupfeld, J.; Hutz, C.S.; et al. Examining the Factor Structure of the Self-Compassion Scale in 20 Diverse Samples: Support for Use of a Total Score and Six Subscale Scores. Psychol. Assess. 2019, 31, 27–45. [Google Scholar] [CrossRef]
- Leary, M.R.; Tate, E.B.; Adams, C.E.; Batts Allen, A.; Hancock, J. Self-Compassion and Reactions to Unpleasant Self-Relevant Events: The Implications of Treating Oneself Kindly. J. Pers. Soc. Psychol. 2007, 92, 887–904. [Google Scholar] [CrossRef]
- Phillips, W.J.; Hine, D.W. Self-Compassion, Physical Health, and Health Behaviour: A Meta-Analysis. Health Psychol. Rev. 2021, 15, 113–139. [Google Scholar] [CrossRef]
- Cohen, M. The association of cancer patients’ emotional suppression and their self-rating of psychological distress on short screening tools. Behav. Med. 2013, 39, 29–35. [Google Scholar] [CrossRef]
- Ando, N.; Iwamitsu, Y.; Kuranami, M.; Okazaki, S.; Nakatani, Y.; Yamamoto, K.; Watanabe, M.; Miyaoka, H. Predictors of psychological distress after diagnosis in breast cancer patients and patients with benign breast problems. Psychosomatics 2011, 52, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Guil, R.; Morales-Sánchez, L.; Ruiz-González, P.; Gómez-Molinero, R.; Gil-Olarte, P. The Key Role of Emotional Repair and Emotional Clarity on Depression among Breast Cancer Survivors. Int. J. Environ. Res. Public Health 2022, 19, 4652. [Google Scholar] [CrossRef]
- Jayawickreme, E.; Blackie, L.E. Post–traumatic growth as positive personality change: Evidence, controversies and future directions. Eur. J. Personal. 2014, 28, 312–331. [Google Scholar] [CrossRef]
- Spelten, E.R.; Sprangers, M.A.; Verbeek, J.H. Factors reported to influence the return to work of cancer survivors: A literature review. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2002, 11, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Gorini, A.; Pravettoni, G. Return to work. Hope or reality? Breast 2018, 41, S5. [Google Scholar] [CrossRef]
- Gullo, G.; Cucinella, G.; Perino, A.; Gullo, D.; Segreto, D.; Laganà, A.S.; Buzzaccarini, G.; Donarelli, Z.; Marino, A.; Allegra, A.; et al. The gender gap in the diagnostic-therapeutic journey of the infertile couple. Int. J. Environ. Res. Public Health 2021, 18, 6184. [Google Scholar] [CrossRef]
- Gullo, G.; Petousis, S.; Papatheodorou, A.; Panagiotidis, Y.; Margioula-Siarkou, C.; Prapas, N.; D’Anna, R.; Perino, A.; Cucinella, G.; Prapas, Y. Closed vs. Open oocyte vitrification methods are equally effective for blastocyst embryo transfers: Prospective study from a sibling oocyte donation program. Gynecol. Obstet. Investig. 2020, 85, 206–212. [Google Scholar] [CrossRef]
- Mandelblatt, J.S.; Edge, S.B.; Meropol, N.J.; Senie, R.; Tsangaris, T.; Grey, L.; Peterson, B.M.; Hwang, Y.T.; Kerner, J.; Weeks, J. Predictors of long-term outcomes in older breast cancer survivors: Perceptions versus patterns of care. J. Clin. Oncol. 2003, 21, 855–863. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).