Interventional Oncology
A topical collection in Medicina (ISSN 1648-9144). This collection belongs to the section "Oncology".
Viewed by 60170Editors
Interests: interventional oncology; percutaneous ablations (cryoablation, electroporation, microwave ablation, radiofrequency ablation); osteoplasty and fixation; soft tissue; bone; spine; pain management
Special Issues, Collections and Topics in MDPI journals
Interests: interventional radiology; interventional oncology; percutaneous ablation techniques; targeted tumor drug delivery; patient-radiologist relationship
Interests: interventional radiology; pain management; interventional neuroradiology; vertebroplasty; neurolysis; infiltration; CT guidance
Interests: interventional oncology; ablation; vertebral augmentation; MSK interventions
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
Interventional oncology (IO) is a medical specialty offering innovative diagnostic and therapeutic minimally invasive procedures in the oncologic field, but also allowing the management of all issues related to cancer. One critical aspect of IO is that the concept unifying these procedures remains imaging guidance.
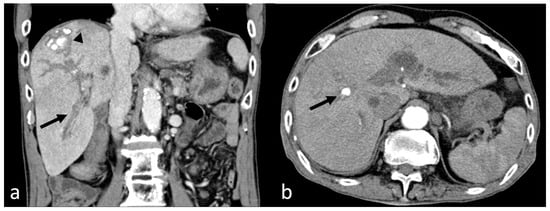
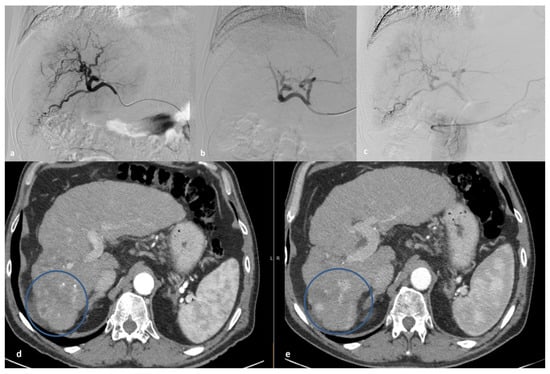
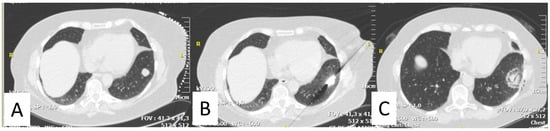
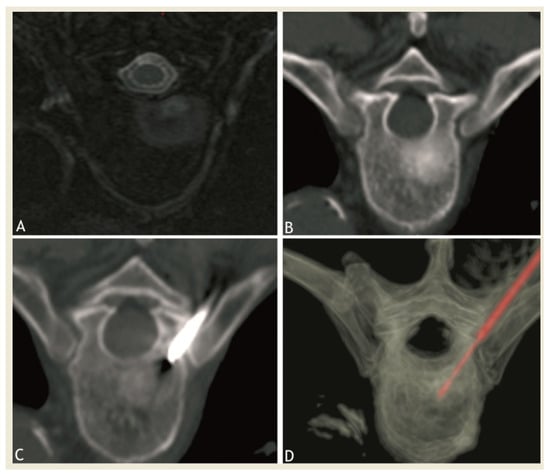
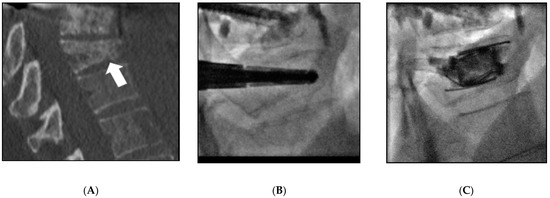
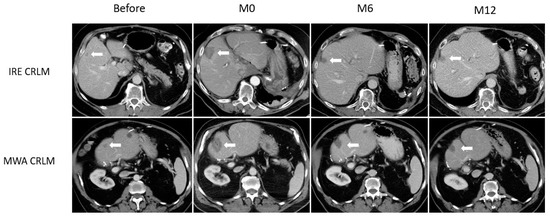
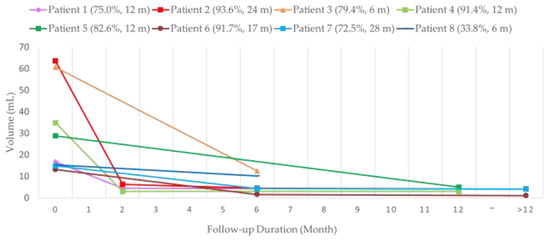
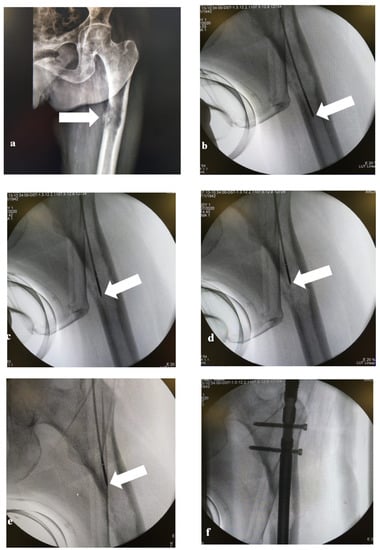
IO has made considerable improvements over the last few years, driven by breakthrough innovations and technological developments. Percutaneous biopsies are widely proposed for the diagnosis of cancer but also now iteratively to offer critical insights into a disease, allowing the provision of the best care in the era of personalized medicine. Furthermore, IO treatments now include a wide array of techniques that are able to provide local control or symptomatic relief. Ablations (cryoablation, radio frequency ablation, microwave ablation, electroporation) are routinely used in the liver, kidney, lung, bone, or soft tissues. A better understanding of biological effects has been observed thanks to preclinical evaluation. Embolization is also commonly performed. Osteoplasty and fixation are gaining importance in pain palliation. They interest a large community of physicians, including oncologists, radiation therapists, surgeons, anesthesiologists, and interventional radiologists.
The purpose of this topical collection is to present these image-guided treatments as alternatives to conservative therapies or surgery and to promote basic and clinical research on this topic as these techniques can serve as attractive alternatives to other options, with a clear effect on quality of life.
We encourage authors to submit both preclinical and clinical studies in the field. Clinical studies may include systematic reviews, retrospective studies, case reports, and prospective studies emphasizing the role and need for IO.
We remain at your disposal for additional questions.
Prof. Dr. François Cornelis
Dr. Matthias Barral
Dr. Adrian Kastler
Dr. Dimitrios Filippiadis
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Medicina is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2200 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- interventional oncology
- cancer
- image guidance
- biopsy
- percutaneous thermal ablation
- cryoablation
- radiofrequency ablation
- electroporation
- microwave ablation
- embolization
- local control
- pain palliation
- vertebroplasty
- osteoplasty
- fixation
- osteosynthesis