- Article
Finite Element Analysis of Low-Profile Reconstruction Plates for Atrophic Mandibles—Part II: A Comparison of Customized Plates with 3D Grid-Type and Conventional Designs
- Bianca Pulino,
- Robert Sader and
- Raphael Capelli Guerra
- + 4 authors
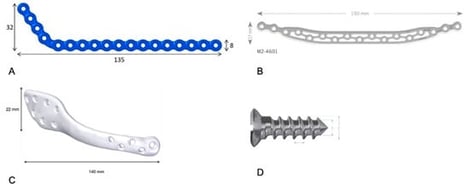
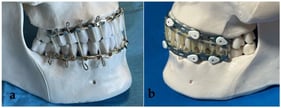
Objectives: The aim of this study was to compare the stiffness-related mechanical response and peak von Mises stress distribution of low-profile 2.4 mm mandibular reconstruction systems (a conventional reconstruction plate, a 3D grid-type plate, and a customized plate) in a virtual atrophic mandible model with a 5 cm segmental defect. Materials and Methods: A CT-based three-dimensional mandible model was created and instrumented with three plate configurations (G1–G3). Linear static finite element analyses were performed under a 300-N masticatory load combined with literature-based muscle force vectors. Peak von Mises stresses were recorded for plates and screws, and the locations of maximum stress concentration were identified. Results: Peak plate stress was highest in the conventional reconstruction plate (G1: 695.5 MPa), followed by the 3D grid-type plate (G2: 595.6 MPa), and lowest in the customized plate (G3: 185.2 MPa). The peak screw stress was 692.9 MPa (G1), 898.0 MPa (G2), and 595.6 MPa (G3). The 3D grid-type plate increased construct stiffness but shifted stress concentration toward the mandibular angle and adjacent screws, whereas the customized plate reduced the peak plate stress and limited the extent of the high-stress region across the defect. Conclusions: Within the limitations of a linear static FEA (stiffness/stress distribution rather than failure load or fatigue resistance), the customized plate (G3) demonstrated the most favorable biomechanical performance (lowest peak plate stress). The 3D grid-type plate (G2) reduced peak plate stress compared with the conventional design (G1) but produced the highest peak screw stress. Practical considerations such as manufacturing lead time and resource requirements may favor off-the-shelf plates; however, a formal cost or operative-time analysis was not performed.
23 January 2026