Pediatric Emergency Medicine
A special issue of Children (ISSN 2227-9067). This special issue belongs to the section "Pediatric Emergency Medicine & Intensive Care Medicine".
Deadline for manuscript submissions: closed (10 October 2024) | Viewed by 20128
Special Issue Editors
Interests: pediatric emergency; pediatric advanced life support; high-fidelity simulation; non-technical skills
Special Issues, Collections and Topics in MDPI journals
Interests: interests: pediatric emergency; pediatric procedural sedation and pain management; pediatric bioethics
Special Issues, Collections and Topics in MDPI journals
Special Issue Information
Dear Colleagues,
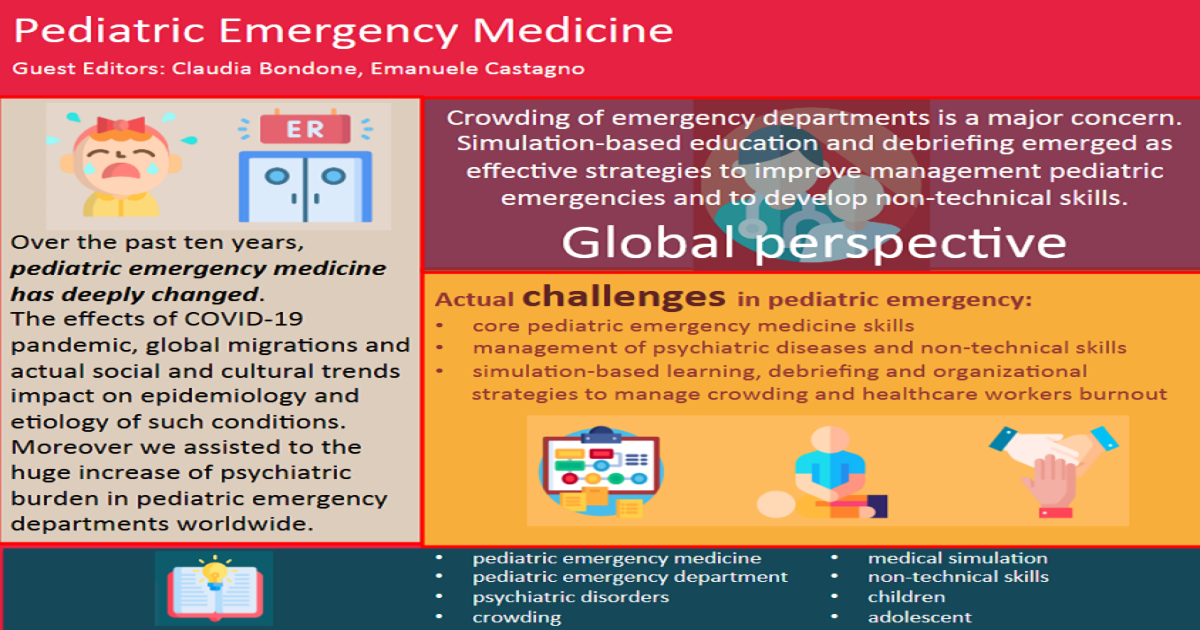
Over the past ten years, pediatric emergency medicine has deeply changed.
Sepsis, trauma, respiratory diseases and seizure management are still priorities in pediatric emergency departments, but the effects of the COVID-19 pandemic, global migrations, and actual social and cultural trends have had an impact on the epidemiology and etiology of such conditions. Moreover, these factors assisted in largely increasing the psychiatric burden in pediatric emergency departments worldwide.
From a global perspective, the crowding of pediatric emergency departments is a major patient safety concern and has consequences for healthcare providers regarding burnout and their well-being.
Simulation-based education and debriefing have emerged as effective strategies to improve the management of low-frequency/high-impact conditions like pediatric emergencies. More recently, such training programs have been also used to develop non-technical skills in critical situations.
This Special Issue will focus on actual challenges in pediatric emergency medicine. Special emphasis will be given to core pediatric emergency medicine skills, such as the management of medical and traumatic emergencies and procedural competences, but also the management of psychiatric diseases and non-technical skills, like crisis resource management, teamwork and communication. Papers that focus on simulation-based learning, debriefing and organizational strategies to manage crowding and help healthcare workers deal with burnout are welcome.
Dr. Claudia Bondone
Dr. Emanuele Castagno
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 250 words) can be sent to the Editorial Office for assessment.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Children is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2400 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- pediatric emergency medicine
- pediatric emergency department
- psychiatric disorders
- crowding
- medical simulation
- non-technical skills
- children
- adolescent
Benefits of Publishing in a Special Issue
- Ease of navigation: Grouping papers by topic helps scholars navigate broad scope journals more efficiently.
- Greater discoverability: Special Issues support the reach and impact of scientific research. Articles in Special Issues are more discoverable and cited more frequently.
- Expansion of research network: Special Issues facilitate connections among authors, fostering scientific collaborations.
- External promotion: Articles in Special Issues are often promoted through the journal's social media, increasing their visibility.
- Reprint: MDPI Books provides the opportunity to republish successful Special Issues in book format, both online and in print.
Further information on MDPI's Special Issue policies can be found here.






