Abstract
Pure red cell aplasia (PRCA) following major ABO-mismatched allogeneic hematopoietic stem cell transplantation (HSCT) is a challenging complication, affecting 7–10% of patients and significantly impacts quality of life. Despite half of patients showing a resolution within three–six months after HSCT, PRCA might require treatment. Various therapeutic approaches have been investigated, including erythropoietin, plasmapheresis or immunomodulatory therapies (rituximab, bortezomib, corticosteroids, donor lymphocyte infusion (DLI), or the early tapering of immunosuppressive drugs), and TPO-mimetic agents, though responses have generally remained suboptimal. Recently, daratumumab has emerged as a promising, safe, and effective treatment for PRCA, documented by numerous case reports and series. We present a case of PRCA arising in a patient with mixed chimerism following a sibling HSCT for aplastic anemia (AA). In line with the literature, our findings highlight the effectiveness of daratumumab in PRCA from the first dose, although daratumumab administrations were delayed by the onset of infectious complications. Our case supports the earlier introduction of daratumumab in the treatment strategy of PRCA to avoid patient exposure to ineffective therapies that carry risks of increased immunosuppression and infections. Indeed, in our specific case, the early introduction of daratumumab may interrupt the immune hematologic mechanism underlying PRCA, which, in the context of mixed chimerism, could increase the risk of graft failure.
1. Introduction
Pure red cell aplasia (PRCA) is a critical complication arising after ABO-mismatch hematopoietic stem cell transplantation (HSCT), observed in approximately 7–10% of cases [1]. PRCA necessitates prolonged transfusions, which increase the risk of iron overload and significantly diminish patients’ quality of life [2]. The pathological mechanism behind PRCA may involve residual host plasma cell clones [3]. In this context, various therapeutic strategies have been explored, including immunosuppressive agents, TPO mimetics, and plasma exchange, though response rates have been inconsistent, and nowadays, there is no standard of care for PRCA [4,5,6].
Over the past decade, daratumumab—a human IgG1κ monoclonal antibody targeting CD38—has emerged as one of the most promising and effective treatments. Multiple studies have documented sustained responses to daratumumab, which improves quality of life and mitigates the risk of graft failure (GF) associated with PRCA [7,8,9].
We present a case of aplastic anemia (AA) in a patient who underwent HSCT from a sibling donor with a major ABO mismatch. In the post-transplant follow-up, the patient documented a mixed chimerism and developed anemia due to PRCA. Mixed chimerism is a well-recognized condition in AA post-HSCT and does not typically predispose to GF, although there is a relative risk of it. In our patient, therefore, two conditions coexisted, which could potentially increase the risk of GF. Daratumumab administered in the second line—after rituximab—led to a rapid and remarkable response of PRCA. Despite the first cycle being delayed due to the onset of several infectious complications, the patients achieved transfusion independence soon after the first dose. Our case, consistent with existing literature, supports the early use of daratumumab in treating PRCA to prevent the burden of ineffective treatments that can increase infection risk.
2. Case Presentation
In October 2023, a 29-year-old female presented at our center with fatigue and hemorrhagic symptoms. The blood count showed pancytopenia (hemoglobin level (Hb) 7 g/dL; white blood cell count (WBC) 3000/mmc; neutrophils (N) 300/mmc; lymphocytes (Ly) 2500/mmc; platelets (Plts) 15,000/mmc). Bone marrow (BM) aspiration and biopsy showed hypocellularity without blast cells. The virological screening for cytomegalovirus (CMV), parvovirus B19, Epstein–Barr virus (EBV), hepatitis B/C viruses (HBV, HCV), herpesviridae (HHV6-7-8), and human immunodeficiency virus (HIV) resulted negative. Cytogenetic analysis showed a normal female karyotype, and fluorescent in situ hybridization (FISH) did not reveal pathological chromosomal aberrations. Next-generation sequencing (NGS) showed EZH2 missense mutations with variant allele frequency (VAF) of 51.3%.
The immunophenotype revealed a little clone of paroxysmal nocturnal hemoglobinuria (EPN) < 0.5%, while the diepoxybutane (DEB) test resulted negative. A diagnosis of aplastic anemia (AA) was made. In January 2024, the patient underwent transplantation with a bone marrow stem cell graft from an ABO-mismatched HLA-identical sibling donor (recipient O+, donor male A+). The conditioning regimen consisted of fludarabine at a dose of 30 mg/m2 of body surface area per day and cyclophosphamide at a dose of 30 mg per kilogram of body weight from day −5 to day −2. To avoid hemorrhagic cystitis, uromitexan at the dose of 30 mg per kilogram of body weight was made from day −5 to day −2. For graft-versus-host disease (GvHD) prophylaxis, thymoglobulin was given from day −4 to day −2, methotrexate on days 1, 3, 6, and 11 after transplantation, while cyclosporine was started on day −1. Letermovir was administered from day +1 to day +100 post-HSCT, while at day +5, the patient received rituximab (total dose of 300 mg) as EBV prophylaxis.
Because of the anti-A isohemagglutinin were detected at a high titer of 1:2048, the day of transplantation, the patient underwent plasmapheresis and subsequently received bone marrow stem cells graft at a dose of 1.96 × 106 CD34+ cells per kilogram. The bone marrow product was previously depleted of red cells. Neutrophil and platelet engraftment were observed on days +22 and + 35, respectively.
On day +30 BM, aspiration showed a normal cellularity with a reduction in erythroid progenitors. The chimerism evaluation by microsatellite DNA fingerprinting (also known short tandem repeat (STR)) resulted 93% and 89% in BM and peripheral blood (PB), respectively. The chimerism study by FISH analysis was 95% XY, confirming a condition of mixed chimerism (MC).
In the following weeks, the patients presented in good clinical state; no signs of GvHD were detected, although a complete red cell engraftment was not reached, requiring 0+ blood transfusions approximately once a week and the start of erythropoietin. Indeed, †granulocyte colony-stimulating factor (G-CSF) was administered on-demand if the WBC count resulted <1000/mmc.
After 3 months of follow-up, the patient continued to be transfusion-dependent. A diagnostic work-up showed the absence of reticulocytes, the negativity of BM viruses responsible for aplasia (parvovirus B19, adenovirus, HHV 6-7-8), as well as the signs of hemolysis. The BM biopsy confirmed the reduction in erythroid elements confirming a diagnosis of PRCA. At this time, chimerism by STR resulted in 87% and 95% in BM and PB, respectively, while by FISH was 88% XY. Because of the increase in ferritin value to 5500 ng/mL, iron chelation therapy with deferasirox was started.
After 6 months of follow-up, BM aspiration confirmed an MC with donor chimerism by STR of 79% and 85% on BM and PB, respectively. The immunoglobulin levels have been closely monitored, resulting in IgG 9 g/dL. The immunohematological study showed that the patient still resulted as 0-positive, and the titer of anti-A antibodies was 1:256.
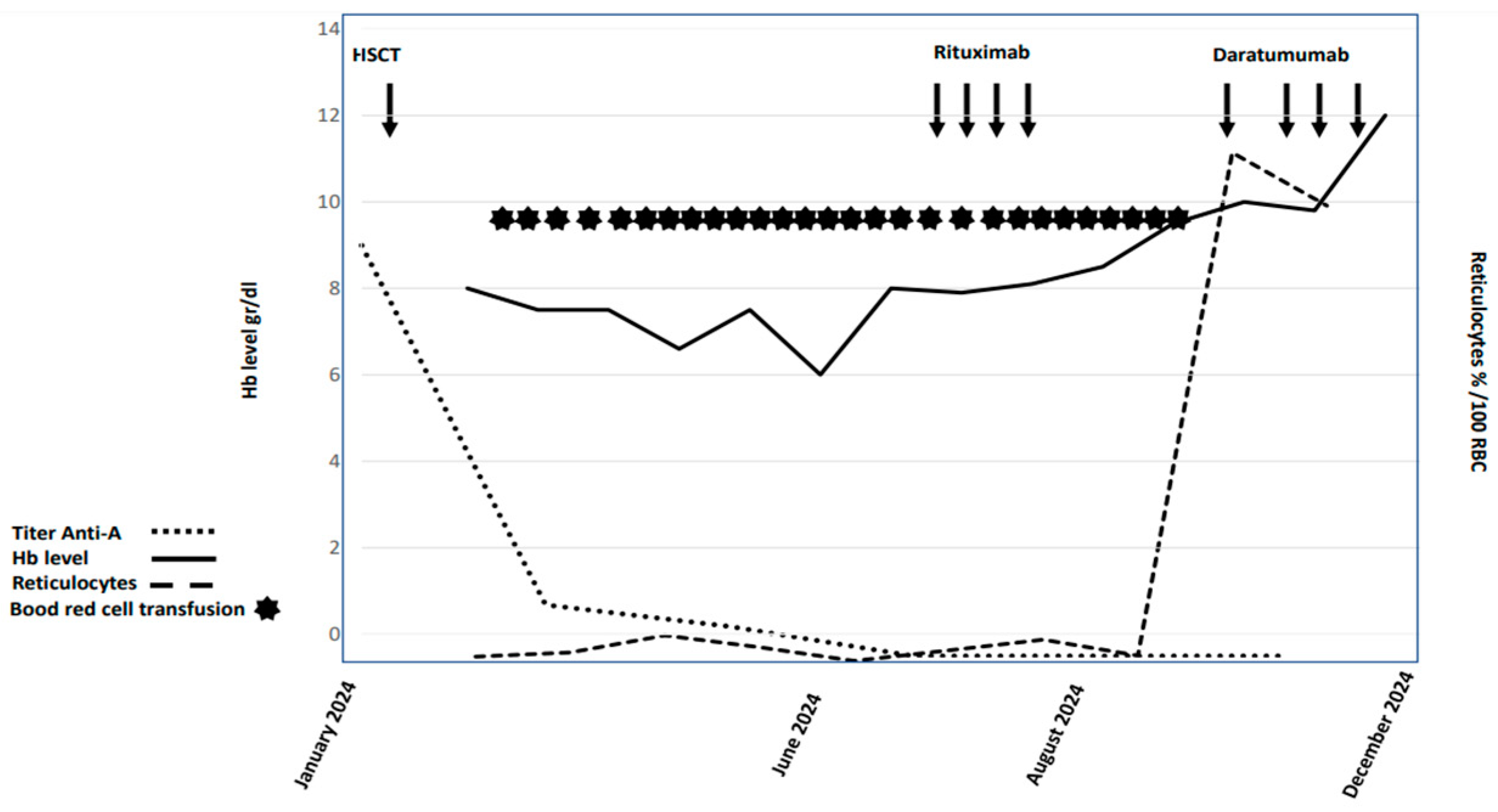
Rituximab at the dose of 375 mg/m2 once a week for 4 weeks was started. At the end of treatment, the patients still required red blood cell transfusion (1 to 2 units per week), no reticulocytosis was observed, and the anti-A titer resulted in 1:128. In August 2024, after failing standard lines of treatment, daratumumab as compassionate use was requested. In September 2024, the patient started daratumumab at a dose of 1800 mg in subcutaneous formulation. One week after the first dose of daratumumab, the patient experienced a flu-syndrome with cough and muscle pain requiring the start of antibiotics. Microbiological exams and the thorax computed tomography scan resulted negative. The patient resumed daratumumab after 2 weeks from the first dose, and during this stop-period, the patient maintained an Hb level above 8 g/dL. She received a total of four doses of daratumumab without infusion-related complications. A week after the last infusion, she presented with a second episode of fever, coinciding with a CMV reactivation (869 IU/mL by polymerase chain reaction (PCR)), requiring antiviral therapy with valganciclovir. Currently, the patient no longer needs transfusion support, the hemoglobin level is stable at 12 g/dL, the CMV-PCR results negative, and chimerism analysis shows the persistence of MC by STR and FISH. In December 2024, the immunohematological study showed the patient’s blood type converted to A-positive, with no detectable anti-A antibodies. Figure 1 summarizes the hemoglobin, reticulocytes, and titer anti-A trend.
Figure 1.
Graphic summary of hemoglobin and reticulocytosis trend and anti-A titer of the patient.
3. Discussion
We present the case of an allografted patient for AA with two conditions that may increase the risk of GF: PRCA and MC. MC arises from bidirectional immune tolerance between donor and recipient, and while it is not synonymous with GF, it can remain stable for extended periods in non-malignant hematologic diseases, such as AA [10,11]. In the setting of MC, several risk factors have been linked to GF related to donor characteristics and conditioning strategies. For instance, sex mismatch, especially with a male donor and female recipient, and a conditioning regimen using cyclophosphamide plus ATG have been associated with an elevated risk of GF. Conversely, in recent years, fludarabine-based regimens combined with low doses of cyclophosphamide (CTX) have shown a lower incidence of MC. Unlike leukemia cases that can be successfully managed by tapering immunosuppression, this approach is not recommended in the setting of AA in which close monitoring is essential. With regard to PRCA, several considerations can be deduced. First, consistent with existing literature, our report demonstrates a rapid response to daratumumab following a single dose, with sustained remission, despite the discontinuation of therapy due to infectious complications. This response allowed our patient to achieve transfusion independence, significantly improving her quality of life. Second, the risk of infection was influenced not only by the patient’s medical history and the immunosuppressive burden due to previous therapy but also to rituximab, which has been an ineffective treatment in resolving PRCA. The delay in the initiation of daratumumab increased the burden of immunosuppressive treatment that was ineffective in resolving the anemia, consequently worsening the transfusion load, the onset of infections, and the reduction in the quality of life. Indeed, the resolution of PRCA, which is related to the decrease in anti-A titer, eliminated one potential cause of GF. These factors underscore the potential benefits of the early administration of daratumumab, within 3–6 months from HSCT, particularly in those cases with ABO-mismatch incompatibility and a higher isoagglutinin titer.
The major limitation of our experience is the short follow-up, but the impressive response together with the other experiences previously reported suggests a sustained result in the future.
4. Conclusions
PRCA represents a serious complication for which no standardized treatment is currently available. In recent years, daratumumab has emerged as a promising therapeutic option, demonstrating safety and sustained response. The early initiation of daratumumab therapy is crucial, as it addresses complications related to transfusion dependence, such as iron overload and diminished quality of life, with associated psychological implications. Furthermore, the immunosuppressive burden of ineffective treatments not only fails to control the disease but also increases the risk of infections. In our specific case, daratumumab could be administered earlier considering the delicate framework of MC in which the host plasma cells contributed to the pathophysiology of PRCA. The evidence of rapid and effective responses to daratumumab underscores the need for further prospective clinical trials exploring other anti-CD38 antibodies, such as isatuximab, to expand therapeutic options and optimize outcomes in this challenging setting (ClinicalTrial.gov Identifier: NCT05559827).
Author Contributions
M.C. (Martina Canichella) and P.d.F. designed and wrote the manuscript. M.C. (Martina Canichella), M.C. (Mariagiovanna Cefalo) and L.C. collected clinical data. C.S. and A.M. performed immunehematology tests and revised this part in the main text. G.A., P.Z. and F.C. collected laboratory data. V.V. and G.S. collected the bibliography. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Lazio Area 2, protocol code 0019299/2024 on 23 August 2024.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Correction Statement
This article has been republished with a minor correction to the Informed Consent Statement. This change does not affect the scientific content of the article.
References
- Longval, T.; Galimard, J.; Leprêtre, A.; Suarez, F.; Amiranoff, D.; Cazaux, M.; Kaphan, E.; Michonneau, D.; Dhedin, N.; Coman, T.; et al. Treatment for pure red cell aplasia after major ABO-incompatible allogeneic stem cell transplantation: A multicentre study. Br. J. Haematol. 2021, 193, 814–826. [Google Scholar] [CrossRef] [PubMed]
- Hirokawa, M.; Fukuda, T.; Ohashi, K.; Hidaka, M.; Ichinohe, T.; Iwato, K.; Kanamori, H.; Murata, M.; Sakura, T.; Imamura, M.; et al. Efficacy and long-term outcome of treatment for pure red cell aplasia after allogeneic stem cell transplantation from major ABO-incompatible donors. Biol. Blood Marrow Transplant. 2013, 19, 1026–1032. [Google Scholar] [CrossRef] [PubMed]
- Griffith, L.M.; McCoy, J.P.; Bolan, C.D.; Stroncek, D.F.; Pickett, A.C.; Linton, G.F.; Lundqvist, A.; Srinivasan, R.; Leitman, S.F.; Childs, R.W. Persistence of recipient plasma cells and anti-donor isohaemagglutinins in patients with delayed donor erythropoiesis after major ABO incompatible non-myeloablative haematopoietic cell transplantation. Br. J. Haematol. 2005, 128, 668–675. [Google Scholar] [PubMed]
- Chapuy, C.I.; Kaufman, R.M.; Alyea, E.P.; Connors, J.M. Daratumumab for delayed red-cell engraftment after allogeneic transplantation. N. Engl. J. Med. 2018, 379, 1846–1850. [Google Scholar] [PubMed]
- Bathini, S.; Holtzman, N.G.; Koka, R.; Singh, Z.; Wilding, E.; Zou, Y.; Ruehle, K.; Kocoglu, M.H.; Badros, A.; Hardy, N.; et al. Refractory postallogeneic stem cell transplant pure red cell aplasia in remission after treatment with daratumumab. Am. J. Hematol. 2019, 94, E216–E219. [Google Scholar] [PubMed]
- Metafuni, E.; Barreto, M.T.B.; Valentini, C.G.; Giammarco, S.; Limongiello, M.A.; Sorà, F.; Bianchi, M.; Massini, G.; Piccirillo, N.; Putzulu, R.; et al. Pure red cell aplasia among ABO mismatched hematopoietic stem cell transplant recipients: A 13-years retrospective study and literature review. Front. Oncol. 2024, 14, 1386670. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Salas, M.Q.; Alahmari, A.; Lipton, J.H. Successful treatment of refractory red cell aplasia after allogeneic hematopoietic cell transplantation with daratumumab. Eur. J. Haematol. 2020, 104, 145–147. [Google Scholar] [CrossRef] [PubMed]
- Rautenberg, C.; Kaivers, J.; Germing, U.; Haas, R.; Ackerstaff, S.; Hoffmann, T.; Kobbe, G.; Schroeder, T. Daratumumab for treatment of pure red cell aplasia after allogeneic stem cell transplantation. Bone Marrow Transplant. 2020, 55, 1191–1193. [Google Scholar] [PubMed]
- Henig, I.; Yehudai-Ofir, D.; Zohar, Y.; Zuckerman, T. Pure Red cell aplasia following ABO-mismatched allogeneic hematopoietic stem cell transplantation: Resolution with daratumumab treatment. Acta Haematol. 2021, 144, 683–687. [Google Scholar] [CrossRef] [PubMed]
- Shamshad, G.U.; Ahmed, S.; Bhatti, F.A.; Ali, N. Mixed donor chimerism in non-malignant haematological diseases after allogeneic bone marrow transplantation. J. Coll. Physicians Surg. Pak. 2012, 22, 765–768. [Google Scholar] [PubMed]
- Lawler, M.; McCann, S.R.; Marsh, J.C.W.; Ljungman, P.; Hows, J.; Vandenberghe, E.; O’riordan, J.; Locasciulli, A.; Socié, G.; Kelly, A.; et al. Serial chimerism analyses indicate that mixed hematopoietic chimerism influences the probability of graft rejection and disease recurrence following allogeneic stem cell transplantation (SCT) for severe aplastic anaemia (SAA): Indication for routine assessment of chimerism post SCT for SAA. Br. J. Haematol. 2009, 144, 933–945. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).