Abstract
(1) Background: Interprofessional supervision is an emerging approach in health professions education that strengthens collaborative practice competencies while maintaining profession-specific expertise. Understanding current evidence regarding supervision models, outcomes, and implementation factors is crucial for advancing this field. (2) Methods: This narrative review analyzed 28 studies, including quantitative, qualitative, mixed-methods studies, and systematic reviews. Studies were analyzed for supervision models, outcome measures, evidence of effectiveness, and implementation factors. (3) Results: Six categories of interprofessional supervision models were identified: clinical practice-based, group supervision, competency-based training, skills training, case-based learning, and mentorship/coaching. Across models, interprofessional supervision consistently enhanced collaborative competencies, professional development, clinical skills, and organizational outcomes. Organizational support, structured curricula, interprofessional leadership, and individual readiness facilitated implementation success. Barriers included limited resources, professional silos, and challenges in curriculum integration. (4) Conclusions: Interprofessional supervision shows consistently positive outcomes across diverse models and settings, though more rigorous research designs and standardized outcome measures are needed. Successful implementation requires systematic attention to multiple factors at multiple levels, from organizational support to individual readiness. Interprofessional supervision is positioned for significant advancement through the application of implementation science frameworks and continued research on optimal model characteristics and implementation strategies.
1. Introduction
The evolution of healthcare delivery toward increasingly complex, team-based care models has created an urgent need for health professionals to function effectively in interprofessional teams [1]. Consequently, this recognition has led to growing interest in interprofessional education (IPE) approaches that cultivate collaborative practice competencies while maintaining the integrity of profession-specific expertise [2]. Within health professions education, these efforts increasingly emphasize workplace-based learning approaches that prepare learners for collaborative practice in clinical settings.
Interprofessional supervision has emerged as one such educational approach that directly addresses this challenge by integrating supervision and mentorship activities across health professional boundaries, within clinical contexts, and with an educational intent. In this review, interprofessional supervision is situated within health professions education and practice-based training, focusing on students, residents, and early-career healthcare professionals in medicine, nursing, and allied health professions in the clinical setting. Included settings are clinical and practice-based environments in which supervision is embedded in routine clinical services. It involves supervisors and supervisees from different health professions working together to develop both profession-specific and interprofessional competencies [3]. This approach has been shown to mitigate professional isolation, enhance exposure to other professional perspectives, and prepare learners for collaborative practice.
The theoretical foundations of interprofessional supervision draw from interprofessional education theory, clinical supervision frameworks, and collaborative practice models. The World Health Organization’s Framework for Action on Interprofessional Education and Collaborative Practice provides a foundational understanding of the conditions necessary for effective interprofessional learning, emphasizing the importance of institutional support, curriculum design, and faculty development [1]. Clinical supervision theory, particularly Proctor’s three-function model encompassing managerial, educational, and supportive functions, provides a framework for understanding the mechanisms by which supervision fosters professional development [4]. Complementing these perspectives, collaborative practice models emphasize the importance of shared decision-making, mutual respect, and role clarity as essential components for effective interprofessional teamwork [5].
Despite growing interest in interprofessional supervision, the evidence base remains fragmented and diverse, with studies utilizing different models, outcome measures, and implementation approaches. This diversity reflects both the field’s evolving nature and the complexity of interprofessional competency development across professions and settings. Understanding the current state of evidence regarding interprofessional supervision models, their effectiveness, and the factors that influence successful implementation is essential to inform practice, strengthen future research design, and guide policy.
This narrative review aims to provide a comprehensive synthesis of current evidence on interprofessional supervision in health professions education. The synthesis was structured around three primary domains: (1) supervision models and their characteristics, (2) outcomes and evidence of effectiveness, and (3) implementation factors, including facilitators and barriers. These domains were selected to align with narrative synthesis principles and to reflect the key questions relevant to both educational theory and practice: what interprofessional supervision looks like, what it achieves, and what influences its successful implementation in real-world settings. Perceived advantages and disadvantages of interprofessional supervision were not treated as a separate domain but were included within the outcomes and implementation factors. This approach enabled a more integrated, practice-relevant synthesis of literature.
2. Methods
2.1. Search Strategy
Two researchers (C.D., V.R.) did the literature search to identify studies examining interprofessional clinical supervision in healthcare and health professions education. Searches were performed in the databases PubMed, Scopus, CINAHL, and PsycINFO. These databases were selected to capture literature across medicine, nursing, allied health, and psychology.
Search terms combined keywords related to clinical supervision, interprofessional or multidisciplinary practice, and health professions education. Core search terms included combinations of: clinical supervision, educational supervision, professional supervision, interprofessional, multidisciplinary, healthcare, health professions education, training, and workplace learning. Search strategies were adapted for each database. The search covered studies published from January 2000 to December 2024, reflecting contemporary models of interprofessional practice and supervision.
2.2. Study Selection
Study selection followed a staged process. After duplicates were removed, titles and abstracts were screened for relevance to interprofessional supervision in healthcare or health professions education. Full-text reviews were conducted for studies that appeared to meet the inclusion criteria or for which eligibility was unclear.
Studies were included if they:
- (1)
- Examined clinical supervision, educational supervision, or structured supervisory practices involving two or more health professions;
- (2)
- Were conducted within healthcare, clinical training, or health professions education settings;
- (3)
- Reported empirical findings from quantitative, qualitative, or mixed-methods studies, or were systematic, scoping, or rapid reviews with an explicit focus on supervision; and
- (4)
- Addressed supervision-related outcomes, processes, or implementation factors relevant to interprofessional practice, learning, or workforce development.
Studies were excluded if they:
- (1)
- Focused solely on single-profession supervision without an interprofessional or cross-disciplinary component;
- (2)
- Examined mentoring, coaching, or informal support activities without an explicit supervisory function;
- (3)
- Were opinion pieces, editorials, commentaries, or conference abstracts without sufficient empirical detail; or
- (4)
- Were conducted outside healthcare or health professions education contexts.
2.3. Data Extraction
Data from each included study were extracted using a structured template adapted from the narrative synthesis framework described by Popay et al. [6]. The template was designed to capture both descriptive and analytical information to support the synthesis’s iterative stages.
The professional groups represented in the studies included medicine (14 studies), social work (13 studies), occupational therapy (6 studies), physiotherapy (6 studies), nursing (5 studies), psychology (5 studies), and pharmacy (4 studies), reflecting the multidisciplinary nature of interprofessional supervision research. Study settings ranged from academic medical centers and universities to community and rural healthcare facilities, as well as specialized clinical services, providing insights into interprofessional supervision across diverse practice environments.
Two authors (C.D., E.W.Y.L.) independently extracted data from 14 studies each. Following initial extraction, the two authors (C.D., E.W.Y.L.) independently reviewed the 14 studies extracted by the other to ensure completeness, accuracy, and consistency of interpretation. Any discrepancies or uncertainties were resolved through discussion and consensus. For each study, we recorded bibliographic details, study aims, design, setting, participant characteristics, and characteristics of supervision or educational interventions. We also extracted information on outcomes measured, key quantitative and qualitative findings, and reported implementation factors or contextual influences relevant to interprofessional supervision in healthcare.
The complete extraction table was used as the foundation for developing narrative synthesis, exploring relationships within and across studies, and assessing the robustness of the synthesis. To enhance readability and accommodate journal layout constraints, a condensed summary of key study characteristics is presented in the main manuscript (Table 1), while the full data extraction table is provided as Supplementary Table S1 and made available in an external repository.

Table 1.
Characteristics of included studies.
2.4. Synthesis and Assessment of Study Quality
Our synthesis was informed by Popay et al.’s four-stage approach [6] (Figure 1). We began by outlining a preliminary theoretical framework to consider how, why, and for whom interprofessional supervision interventions in healthcare might work, drawing on existing conceptual models and insights from the included studies. We then organized and tabulated data from the 28 studies to construct an initial synthesis, grouping findings by intervention type, professional group, setting, and reported outcomes. Subsequently, we examined relationships within and across studies to explore how contextual factors, target populations, and implementation strategies might shape the observed effects. This included comparing findings from qualitative and quantitative evidence, identifying potential moderators and mediators, and considering the influence of methodological quality. Finally, we assessed the robustness of the synthesis through critical reflection on the strength and consistency of the evidence, attention to potential biases, and the use of multiple reviewers to check data interpretation. This iterative process allowed us to integrate diverse forms of evidence into a coherent account of the current state of knowledge on interprofessional supervision.
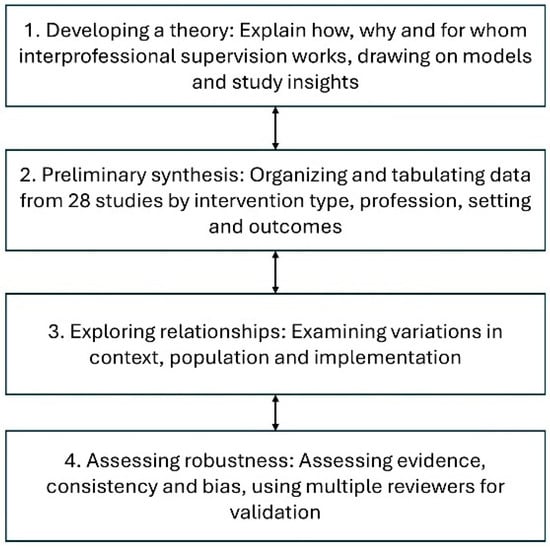
Figure 1.
Popay et al.’s [6] four-stage approach.
Quality appraisal was conducted using a customized tool adapted from established critical appraisal frameworks, including the EPPI-Centre Weight of Evidence framework [35], the Critical Appraisal Skills Programme (CASP) checklists, and the Joanna Briggs Institute (JBI) Critical Appraisal Tools. The following criteria were assessed: relevance to the review question, methodological quality, clarity of reporting, risk of bias, and justification. Consistent with narrative synthesis approaches, quality appraisal was done to support transparent interpretation of the evidence rather than to exclude studies. Quality ratings were used during data extraction and synthesis to contextualize findings and guide the interpretation of results. Table 2 summarizes the quality of each reviewed study.

Table 2.
Quality Appraisal of Studies.
3. Results
3.1. Interprofessional Supervision Models
As summarized in Table 3, the reviewed studies revealed considerable heterogeneity in interprofessional supervision models, reflecting differences in context, professional mix, and intended outcomes. Clinical practice-based models offered the most immersive integration of supervision with patient care, embedding supervision within clinical encounters such as interprofessional pain clinics or primary care settings [9,25]. These models enabled real-time application of profession-specific and interprofessional competencies; however, they typically required sustained faculty involvement, protected time, and coordination across professions, which may limit scalability in resource-constrained settings.

Table 3.
Summary of interprofessional supervision models.
Group supervision models leveraged peer learning and facilitated interprofessional reflection around shared cases, ethical challenges, or professional experiences [8,13]. Participants commonly reported enhanced role understanding and reflective capacity, although evidence of sustained practice or knowledge change was less consistent and relied largely on self-reported outcomes.
Competency-based and skills-focused training models provide structured, measurable gains in targeted domains [10,11,31,34]; however, their narrower scope may overlook broader relational and identity-forming dimensions of interprofessional work. Case-based learning approaches similarly demonstrated promise for fostering deep engagement with complex scenarios through structured, sequential discussions. Still, outcome measures primarily captured self-reported learning rather than objective changes in practice [16].
Mentorship and coaching models showed potential for supporting long-term professional development and interdisciplinary collaboration, particularly within longitudinal or workforce development programs. However, the supporting evidence was predominantly qualitative and context-specific, relying heavily on participant narratives and experiential accounts, which limited generalizability [26,32].
Across models, positive trends in teamwork, role clarity, and clinical knowledge were reported in the majority of included studies (approximately two-thirds), particularly in clinical practice-based and group supervision models. These outcomes were commonly assessed using short-term, self-reported measures, and the overall evidence base was stronger for interprofessional competency development than for patient-level or organizational outcomes.
3.2. Organizational and System-Level Impacts
Organizational and system-level outcomes were reported in a smaller subset of studies, most commonly regarding staff satisfaction, retention, and interprofessional collaboration. They were typically measured indirectly through participant-reported outcomes rather than objective organizational indicators. Ducat & Kumar [12] reported that supervision reduced burnout and improved job satisfaction and retention, with rural practitioners reporting particular benefit. Gardner et al. [14] showed sustained effectiveness over five years following the implementation of an organizational supervision framework, with supervisor choice, seniority, and session frequency enhancing outcomes, contributing to stable Manchester Clinical Supervision Scale (MCSS-26) scores. Tatla et al. [32] demonstrated that collaborative coaching improved team cohesion and communication, though quantitative outcomes were less evident. Overall, organizational impacts were more robustly supported by moderate-quality longitudinal or mixed-methods studies than by short-term evaluations.
3.3. Patient Outcomes and Quality of Care
Evidence linking supervision to patient outcomes was limited but promising; however, this evidence was derived primarily from systematic and rapid reviews and a small number of moderate-quality primary studies, with few high-quality controlled designs directly measuring patient-level outcomes.
A review by Snowdon et al. [29] found improvements in processes of care in 12 of 14 studies, some gains in health outcomes in 3 of 6 studies, and positive patient experiences in 3 of 3 studies. Notably, most patient-related outcomes were indirect, focusing on care processes, communication, or patient satisfaction rather than clinical endpoints.
Cao & Hull [9] reported high satisfaction with team-based pain management delivered through a supervised interprofessional clinic, although specific health outcomes were not measured. The integration of interprofessional supervision with direct patient care appeared to create positive experiences for both learners and patients [11,29]. Across the reviewed literature, direct links between interprofessional supervision and patient-level clinical outcomes were infrequently examined and were primarily derived from reviews or moderate-quality primary studies.
3.4. Measurement Approaches
The studies included used diverse methods to assess interprofessional supervision outcomes. Common validated tools included the Interprofessional Education Perception Scale (IEPS) [9,16], the Interprofessional Collaborative Competency Attainment Survey (ICCAS) [25], and the Manchester Clinical Supervision Scale (MCSS-26) [14]. These instruments were used in approximately half of the included studies and primarily captured self-reported perceptions of learning, collaboration, or supervisory effectiveness.
Qualitative approaches, such as interviews and focus groups, offered rich insights into participants’ experiences, contextual influences, and perceived mechanisms of change [8,13]. Mixed-methods designs, such as the BU CHAMPs study [25], integrated survey data with qualitative findings related to patient-centered care, team dynamics, and role clarity. While qualitative and mixed-methods studies offered depth and contextual understanding, they also contributed to variability in outcome reporting and limited comparability across studies.
3.5. Implementation Factors
3.5.1. Organizational and System-Level Facilitators
Leadership support and organizational alignment were critical to success [11,19]. Dolansky et al. [11] showed that projects aligned with institutional priorities achieved the strongest outcomes. Goode et al. [15] highlighted the need for senior buy-in, protected time, and ongoing training; without these, programs struggled to secure resources and achieve intended outcomes. Organizational culture also shaped outcomes: Bullington et al. [8] observed that supportive environments or cultures fostered collaboration and psychological safety. Adequate resources and protected time were essential for sustained implementation [17].
3.5.2. Educational and Curricular Facilitators
Structured curricula promoted engagement and measurable outcomes. Gooding et al. [16] demonstrated that sequential case-based sessions improved confidence and role clarity. Faculty development was equally vital: Harvey et al. [17] reported substantial gains in supervisory knowledge, skills, and confidence following structured supervisor training. Embedding supervision in authentic clinical practice, as in the SSIPPC study [9], enhanced both competency development and patient satisfaction.
3.5.3. Professional and Interprofessional Facilitators
Interprofessional champions and leaders drove program success by modeling collaboration across professions [11]. Supervision also reinforced professional identity while promoting teamwork [8]. Peer support networks were particularly valuable in rural and resource-limited settings, where access to profession-specific supervision was more constrained [13].
3.5.4. Barriers to Implementation
Significant barriers included a lack of protected time and competing priorities [15], unsupportive organizational cultures resistant to new supervisory frameworks [8], and entrenched silos or professional hierarchies that hindered collaboration [8]. Faculty inexperience also posed challenges; Harvey et al. [17] emphasized the need for structured training to prepare supervisors for interprofessional roles. These barriers were most frequently reported in lower- and moderate-quality studies, underscoring the influence of contextual constraints on implementation outcomes.
4. Discussion
4.1. Synthesis of Evidence
The narrative synthesis reveals a promising but evolving evidence base for interprofessional supervision in health professions education. The consistency of positive outcomes across diverse models, settings, and populations suggests that interprofessional supervision interventions can produce meaningful improvements in interprofessional competencies, professional development, clinical knowledge and skills, and organizational outcomes. This consistency is particularly noteworthy given the diversity of approaches, measurement methods, and contexts represented in the studies [8,9,11,13,25].
The evidence suggests that multiple approaches to interprofessional supervision can be effective, ranging from intensive, clinical practice-based models to group supervision approaches and competency-based training programs [8,12,16]. This diversity indicates that the field has moved beyond a one-size-fits-all approach to recognize that different contexts, populations, and objectives may require different supervision models. The effectiveness of diverse approaches also suggests that the core principles of interprofessional supervision, such as collaborative learning, mutual respect, and shared reflection, can be operationalized through various mechanisms [11,12,32].
The strength of evidence varies considerably across outcome domains, with the most substantial evidence for interprofessional competencies and professional development outcomes, moderate evidence for clinical knowledge and skills outcomes, and limited evidence for patient outcomes and long-term sustainability [12,29]. This pattern reflects both the relative ease of measuring individual-level outcomes compared to system-level impacts and the field’s early stage of development.
4.2. Theoretical Implications
The evidence from this review has important implications for the theoretical understanding of interprofessional supervision. The consistent positive outcomes across diverse models suggest that interprofessional supervision operates through multiple mechanisms that may be more important than specific model characteristics. These mechanisms appear to include increased exposure to other professional perspectives, opportunities for collaborative problem-solving, peer support and mutual learning, and the integration of profession-specific and interprofessional competencies [8,32].
Importantly, the finding that interprofessional supervision can strengthen rather than threaten professional identity has important theoretical implications for understanding the relationship between profession-specific and interprofessional competencies. The evidence suggests that well-designed interprofessional supervision programs can enhance both domains simultaneously, challenging traditional assumptions about potential conflicts between professional and interprofessional identity development [8,19].
The importance of contextual factors in determining implementation success has implications for the theoretical understanding of interprofessional supervision as a complex intervention that must be adapted to local circumstances. The evidence suggests that successful implementation requires attention to multiple levels of factors, from organizational culture to individual readiness, and that these factors interact in complex ways to influence program outcomes [11,19].
4.3. Methodological Considerations
The diversity of measurement methods across studies reflects both the complex nature of interprofessional competencies and the challenges inherent in evaluating multifaceted educational interventions. While this diversity provides rich insights into different dimensions of interprofessional supervision effectiveness, it also complicates cross-study comparisons and limits the potential for evidence synthesis.
Many studies employed pre–post or cross-sectional designs without control groups, which limits causal inference [9,11,32]. Sample sizes were generally small, and few studies incorporated longitudinal follow-up. Measures of supervision effectiveness were often self-reported, introducing subjectivity and recall bias [12,25,29]. Although the consistent positive outcomes across diverse studies offer some confidence in the findings, greater methodological rigor is needed. Future research should prioritize mixed-methods and longitudinal designs to better capture developmental and behavioral changes over time [11,15,29].
The predominance of short-term follow-up periods in most studies limits understanding of the sustainability and long-term impact of interprofessional supervision interventions. The few studies that evaluated longer-term outcomes, such as the organizational framework study by Gardner et al. [14], provide valuable insights into sustainability but represent only a small proportion of the available evidence.
4.4. Practical Implications
The evidence has important practical implications for educators, administrators, and policymakers seeking to implement interprofessional supervision programs. The diversity of effective approaches suggests that organizations have flexibility in choosing supervision models that align with their contexts, resources, and objectives [11,19]. However, the evidence also suggests that certain core elements, such as organizational support, structured curriculum design, and faculty development, are important regardless of the chosen model.
The importance of implementation factors suggests that successful interprofessional supervision requires more than simply adopting a proven model. Organizations must carefully assess their readiness for implementation, address potential barriers, and develop comprehensive implementation strategies that attend to multiple levels of factors simultaneously [11,19].
The evidence for positive organizational outcomes, including improved job satisfaction and team dynamics, suggests that interprofessional supervision can provide value beyond individual professional development [12,14]. This broader value proposition may be important for securing organizational support and resources for supervision programs.
4.5. Limitations and Future Directions
The evidence base is limited by short follow-up, scarce use of control groups, and varied outcome measures, factors which weaken causal claims and comparability. Evidence linking supervision to patient outcomes is still sparse, despite its centrality to interprofessional care.
Future research should adopt rigorous designs, standardized outcome sets, and extended follow-up to examine sustainability and contextual influences. Integrating implementation-science frameworks can clarify how organizational culture, leadership, and professional hierarchies shape success. Continued research should also investigate cost-effectiveness and scalability, ensuring that interprofessional supervision becomes an embedded component of workforce and educational policy.
5. Conclusions
Interprofessional supervision shows clear potential to support collaborative practice by strengthening interprofessional competencies and professional development across diverse settings. The current evidence base, however, remains uneven, with comparatively limited and methodologically weaker evidence for patient-level outcomes and long-term sustainability.
Future research should prioritize rigorous and longitudinal study designs, adopt more standardized outcome measures, and apply implementation science frameworks to understand better how interprofessional supervision can be effectively embedded and sustained within healthcare systems. With appropriate institutional support and robust evaluation, interprofessional supervision can become a scalable, integral component of health professions education.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ime5010004/s1, Table S1: Overview of Included Studies and Key Characteristics.
Author Contributions
Conceptualization, V.R. and C.D.; methodology, V.R., C.D. and E.W.Y.L.; data extraction, C.D. and E.W.Y.L.; data validation, V.R., C.D., E.W.Y.L. and C.C.Y.; writing—original draft preparation, V.R. and C.D.; writing—review and editing, C.D., E.W.Y.L. and C.C.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
We acknowledge the use of OpenAI’s ChatGPT-5.2 for assistance in language refinement and preliminary thematic analysis of qualitative data. All intellectual contributions, interpretations, and conclusions remain our own.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| DTT | Discrete Trial Teaching |
| IPE | Interprofessional Education |
| IPES | Interprofessional Education Perception Scale |
| JBI | Joanna Briggs Institute |
| QI | Quality Improvement |
References
- World Health Organization. Framework for Action on Interprofessional Education and Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Institute of Medicine. Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes; The National Academies Press: Washington, DC, USA, 2015. [Google Scholar]
- Interprofessional Education Collaborative. Core Competencies for Interprofessional Collaborative Practice: 2016 Update; Interprofessional Education Collaborative: Washington, DC, USA, 2016. [Google Scholar]
- Proctor, B. Training for the supervision alliance attitude, skills and intention. In Fundamentals Themes In Clinical Supervision; Cutcliffe, J.R., Butterworth, T., Proctor, B., Eds.; Routledge: London, UK, 2001; pp. 25–46. [Google Scholar]
- Canadian Interprofessional Health Collaborative. A National Interprofessional Competency Framework; Canadian Interprofessional Health Collaborative: Vancouver, Canada, 2010. [Google Scholar]
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N.; Roen, K.; Duffy, S. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme; Lancaster University: Lancaster, UK, 2006. [Google Scholar]
- Alfonsson, S.; Lundgren, T.; Andersson, G. Clinical supervision in cognitive behavior therapy improves therapists’ competence: A single-case experimental pilot study. Cogn. Behav. Ther. 2020, 49, 425–438. [Google Scholar] [CrossRef] [PubMed]
- Bullington, J.; Cronqvist, A. Group supervision for healthcare professionals within primary care for patients with psychosomatic health problems: A pilot intervention study. Scand. J. Caring Sci. 2018, 32, 108–116. [Google Scholar] [CrossRef]
- Cao, L.; Hull, S.Z. Effectiveness of educating health care professionals in managing chronic pain patients through a supervised student inter-professional pain clinic. Med. Sci. Educ. 2021, 31, 479–488. [Google Scholar] [CrossRef]
- Cruz, Y.; Kriss, J.; Welsh, T.M.; Bailey, J.S. Teaching supervisory skills to behavior analysts and improving therapist-delivered discrete trial teaching. J. Organ. Behav. Manag. 2023, 43, 256–278. [Google Scholar] [CrossRef]
- Dolansky, M.A.; Edmiston, E.A.; Vehovec, A.; Harris, A.; Singh, M.K. An interprofessional postgraduate quality improvement curriculum: Results and lessons learned over a 5-year implementation. Med. Educ. Online 2024, 29, 2408842. [Google Scholar] [CrossRef]
- Ducat, W.; Kumar, S. A systematic review of professional supervision experiences and effects for allied health practitioners working in non-metropolitan health care settings. J. Multidiscip. Healthc. 2015, 8, 397–407. [Google Scholar] [CrossRef]
- Gardner, M.; McKinstry, C.; Perrin, B. Group clinical supervision for allied health professionals. Aust. J. Rural Health 2021, 29, 538–548. [Google Scholar] [CrossRef]
- Gardner, M.J.; McKinstry, C.; Perrin, B. Effectiveness of allied health clinical supervision following the implementation of an organisational framework. BMC Health Serv. Res. 2022, 22, 261. [Google Scholar] [CrossRef] [PubMed]
- Goode, S.; Cross, D.; Hodge, G. An evaluation of a quality improvement initiative examining benefits and enablers and challenges and barriers of implementing and embedding core clinical supervision in primary care. Pract. Nurs. 2024, 35, 298–307. [Google Scholar] [CrossRef]
- Gooding, H.C.; Ziniel, S.; Touloumtzis, C.; Pitts, S.; Goncalves, A.; Emans, J.; Burke, P. Case-based teaching for interprofessional postgraduate trainees in adolescent health. J. Adolesc. Health 2016, 58, 567–572. [Google Scholar] [CrossRef]
- Harvey, S.; Spurr, P.; Sidebotham, M.; Fenwick, J. Describing and evaluating a foundational education/training program preparing nurses, midwives and other helping professionals as supervisors of clinical supervision using the role development model. Nurse Educ. Pract. 2020, 42, 102671. [Google Scholar] [CrossRef] [PubMed]
- Haynes, C.; Yamamoto, M.; Dashiell-Earp, C.; Gunawardena, D.; Gupta, R.; Simon, W. Continuity clinic practice feedback curriculum for residents: A model for ambulatory education. J. Grad. Med. Educ. 2019, 11, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.R.; Dadiz, R.; Baldwin, C.D.; Alpert-Gillis, L.; Jee, S.H. Integrated behavioral health education using simulated patients for pediatric residents engaged in a primary care community of practice. Fam. Syst. Health 2022, 40, 472–483. [Google Scholar] [CrossRef]
- Martin, P. Clinical supervision in the bush: Is it any different? Int. J. Integr. Care 2018, 18, 127. [Google Scholar] [CrossRef]
- Martin, P.; Lizarondo, L.; Kumar, S.; Snowdon, D. Impact of clinical supervision of health professionals on organizational outcomes: A mixed methods systematic review protocol. JBI Evid. Synth. 2020, 18, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Martin, P.; Tian, E.; Kumar, S.; Lizarondo, L. A rapid review of the impact of COVID-19 on clinical supervision practices of healthcare workers and students in healthcare settings. J. Adv. Nurs. 2022, 78, 3531–3539. [Google Scholar] [CrossRef]
- McCarron, R.H.; Eade, J.; Delmage, E. The experience of clinical supervision for nurses and healthcare assistants in a secure adolescent service: Affecting service improvement. J. Psychiatr. Ment. Health Nurs. 2018, 25, 145–156. [Google Scholar] [CrossRef]
- McGuinness, S.; Guerin, S. Interprofessional supervision among allied health professionals: A systematic scoping review. J. Interprof. Care 2024, 38, 739–758. [Google Scholar] [CrossRef]
- Miselis, H.H.; Zawacki, S.; White, S.; Yinusa-Nyahkoon, L.; Mostow, C.; Furlong, J.; Mott, K.K.; Kumar, A.; Winter, M.R.; Berklein, F.; et al. Interprofessional education in the clinical learning environment: A mixed-methods evaluation of a longitudinal experience in the primary care setting. J. Interprof. Care 2022, 36, 845–855. [Google Scholar] [CrossRef]
- O’Mahony, S.; Baron, A.; Ansari, A.; Deamant, C.; Nelson-Becker, H.; Fitchett, G.; Levine, S. Expanding the interdisciplinary palliative medicine workforce: A longitudinal education and mentoring program for practicing clinicians. J. Pain Symptom Manag. 2020, 60, 602–612. [Google Scholar] [CrossRef]
- Riveros Perez, E.; Jimenez, E.; Yang, N.; Rocuts, A. Evaluation of anesthesiology residents’ supervision skills: A tool to assess transition towards independent practice. Cureus 2019, 11, e4137. [Google Scholar] [CrossRef]
- Rothwell, C.; Kehoe, A.; Farook, S.F.; Illing, J. Enablers and barriers to effective clinical supervision in the workplace: A rapid evidence review. BMJ Open 2021, 11, e052929. [Google Scholar] [CrossRef]
- Snowdon, D.A.; Leggat, S.G.; Taylor, N.F. Does clinical supervision of healthcare professionals improve effectiveness of care and patient experience? A systematic review. BMC Health Serv. Res. 2017, 17, 786. [Google Scholar] [CrossRef]
- Starks, H.; Coats, H.; Paganelli, T.; Mauksch, L.; Van Schaik, E.; Lindhorst, T.; Hurd, C.; Doorenbos, A. Pilot study of an interprofessional palliative care curriculum: Course content and participant-reported learning gains. Am. J. Hosp. Palliat. Med. 2018, 35, 390–397. [Google Scholar] [CrossRef]
- Suddarth, K.H.; Jones, R.R.; O’Malley, C.W.; Paje, D.; Yamazaki, K.; Zaas, A.K.; Meade, L.B. Implementation of milestones-based assessment for a safe and effective discharge. Am. J. Med. 2016, 129, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Tatla, S.K.; Howard, D.; Antunes Silvestre, A.; Burnes, S.; Husson, M.; Jarus, T. Implementing a collaborative coaching intervention for professionals providing care to children and their families: An exploratory study. J. Interprof. Care 2017, 31, 604–612. [Google Scholar] [CrossRef]
- Wingo, M.T.; Halvorsen, A.J.; Leasure, E.L.; Wallace, J.A.; Huber, J.M.; Mathias, T.R.; Thomas, K.G. Enhancing team development in an internal medicine resident continuity clinic. Med. Educ. Online 2024, 29, 2430570. [Google Scholar] [CrossRef] [PubMed]
- Winn, A.S.; Marcus, C.H.; Williams, K.; Smith, G.C.; Gorbounova, I.; Sectish, T.C.; Landrigan, C.P. Development, implementation, and assessment of the Intensive Clinical Orientation for Residents (ICOR) curriculum: A pilot intervention to improve intern clinical preparedness. Acad. Pediatr. 2018, 18, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Gough, D. Weight of evidence: A framework for the appraisal of the quality and relevance of evidence. Res. Pap. Educ. 2007, 22, 213–228. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Academic Society for International Medical Education. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.