Abstract
This study assessed the needs and perceptions of mentorship among students and staff at the Faculty of Medical Sciences (FMS) across all University of the West Indies (UWI) campuses. A cross-sectional survey was conducted from February to May 2023, targeting FMS students and staff across four UWI locations. Data analysis included descriptive statistics and inferential tests, with results presented in proportions and averages. A total of 234 responses were received (138 students, 96 staff). The majority of students (88%) and staff (71%) were affiliated with the Bachelor of Medicine, Bachelor of Surgery (MBBS) programme. Both groups agreed that mentoring should focus on career guidance, professional goals, networking, and role modelling. Interest in mentorship was high among students (77%) and staff (89%), with no gender preference. Most mentees (72%) preferred faculty mentors, and mentors preferred to guide two to five mentees. A blended mentorship model was most preferred. While 29% of students had a mentor, 65% of staff reported prior mentorship experience (p < 0.001). These findings highlight the need for structured mentorship programmes in Caribbean medical education. Implementing and monitoring mentorship initiatives within UWI’s FMS can enhance professional development and academic success for both mentors and mentees.
1. Introduction
Mentoring is defined as “a formal or informal attachment between a teacher and a student or small group of students that goes beyond mere teaching or tutoring to include advice and guidance about many other issues and problems encountered by students” [1]. Therefore, a mentor with career and life experience can play an invaluable role in the personal and professional development of the mentee.
Medical schools worldwide have long recognised the benefits of mentoring, and many have developed formalised mentoring programmes for both undergraduate and postgraduate students. The benefits of such programmes extend beyond mentees to encompass mentors and the institutions themselves. A systematic review of worldwide mentoring programmes for medical students described the goals of these programmes as including professional development, emotional well-being, psychosocial support, exposure to specialties in medicine, and career advice [2].
Clinical mentoring, particularly peer mentoring between recent graduates and final-year students, offers practical guidance for internships, such as managing on-calls, navigating family meetings, and building professional relationships [3]. Furthermore, clinical mentoring can encourage students towards postgraduate specialisation and enhance subject matter understanding, regardless of their ultimate specialty choice [4].
Mentors can also play a critical role in modelling professional behaviours for mentees through interactions in formal and informal settings [5]. Mentoring benefits are often bidirectional; mentors, for instance, can enhance their own leadership and communication skills through the process. Given the documented decline of academic medicine worldwide, a mentorship programme can also be strategically employed to retain and recruit students interested in research careers [5].
The University of the West Indies (UWI) is a major regional institution in the Caribbean with four island sites for medical training: Jamaica (Mona Campus), Barbados (Cave Hill Campus), Trinidad (St. Augustine Campus), and the Bahamas [6]. The first three campuses provide the entire MBBS programme, whereas the Bahamas only offers the clinical phases (Years 4 and 5), requiring students to complete the preclinical phase (Years 1–3) at one of the other three campuses. Despite this multi-campus structure, there is no university-wide mentorship programme at the Faculty of Medical Sciences (FMS), UWI. Although a programme exists at the St. Augustine campus alongside an academic advising programme, formal mentorship programmes are absent at the Cave Hill, Mona, and Bahamas sites. Moreover, the importance of fostering a mentorship culture to support student well-being has previously been highlighted within UWI [7].
Developing a formal mentorship programme aligns with UWI’s Triple A Strategy of access, alignment, and agility [8]. Specifically, mentorship enhances access by fostering student development and potentially increasing post-graduate uptake to address regional specialty scarcities. It promotes alignment by connecting current students with alumni mentors, guiding career choices congruent with societal needs. Finally, it supports agility by adapting to student needs and equipping them with skills for training and employment opportunities.
This study aimed to assess the perceived need for a formal mentorship programme among students and staff within the FMS at UWI. Specific objectives were to (1) explore understanding of mentorship among students and potential mentors, (2) determine their willingness to participate, (3) identify preferences for mentor/mentee selection, and (4) describe preferred mentorship styles and structures.
2. Methods
2.1. Setting and Sampling Strategy
A cross-sectional study design was employed, targeting all currently enrolled undergraduate students and staff at the Faculty of Medical Sciences at all four sites during the period from February to May 2023. The target population included all actively enrolled undergraduate students across all years and programmes within the FMS, as well as full-time and part-time staff. An electronic survey form was distributed to all deaneries with invitations to the staff and student bodies to participate, with two additional follow-up reminders. No incentives were offered for survey completion. Informed consent was obtained electronically; proceeding beyond the first page of the anonymous survey signified agreement to participate.
2.2. Sample Size
Based on an expected response proportion of 50% for responses and a finite population size of 3600 for students and 937 for staff, a minimum of 348 students and 273 staff were required for the survey to estimate proportions with 95% confidence limits and 5% precision.
2.3. Instrument Development
The data collection tool was developed from a previous survey conducted at the St. Augustine Campus. Questions were developed surrounding themes and questions adapted from a review of the literature [5,9,10].
2.4. Data Analysis
Data were analysed using IBM SPSS Statistics for Windows, version 25.0 (Armonk, NY, USA: IBM Corp). Analysis primarily involved descriptive statistics (frequencies, percentages, means). Comparisons between groups for categorical variables were performed using Chi-square or Fisher’s exact tests, as appropriate. A p-value < 0.05 was deemed statistically significant.
2.5. Ethics
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved for all sites by the Campus Research and Ethics Committee, University of the West Indies, Cave Hill Campus (REF: CREC-CH.00070/06/2022), on 3 February 2023.
3. Results
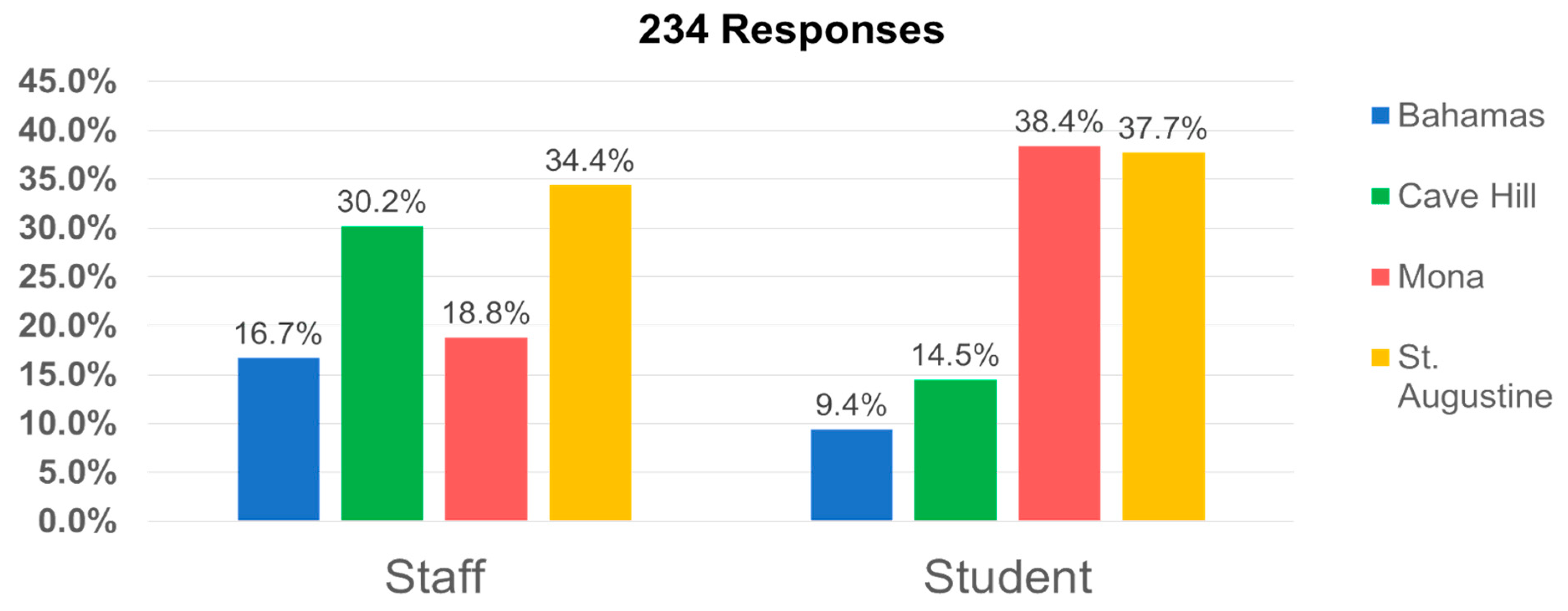
A total of 234 responses were received from the online survey conducted between February and May 2023, representing a 10% response rate from staff (96 respondents) and a 4.8% response rate from students (138 respondents). The distribution of responses varied across the campuses, as shown in Figure 1.
Figure 1.
Distribution of respondents by site.
The average age of staff respondents was 51.2 years, while students’ average age was 24.0 years. The gender distribution was predominantly female, with 55% among staff and 79% among students.
Among student participants, the largest proportion was from Year 5 (30.9%), followed by Year 2 (20.6%) and Year 3 (21.3%). Nearly all (97.0%) were full-time students. Staff respondents were primarily part-time (55.2%), with roles ranging from lecturers (43%) to senior lecturers (30%) and professors (15%). The majority of both students (88%) and staff (71%) were affiliated with the Bachelor of Medicine, Bachelor of Surgery (MBBS) programme.
Table 1 below summarises the comparison of the responses between staff and students regarding perceptions surrounding mentorship.

Table 1.
Comparison of staff’s and students’ perceptions towards mentoring.
3.1. Comparison Between Staff and Students
Both students and staff found mentorship helpful in several ways (Table 1). Staff were significantly more likely than students to believe mentoring was intended for high-potential individuals (p < 0.001). Conversely, students were significantly more likely to view mentoring as coaching for exams (p = 0.018). The majority of students (71%) and staff (92%) appreciated observing a positive role model. Mentorship also facilitated improvement in communication skills (46% students, 49% staff) and the attainment of clinical knowledge and skills (46% students, 68% staff). Half of the students found discussing exams and study techniques beneficial, while 46% of staff agreed. Opportunities for research were recognised by 33% of students and 54% of staff. Mentorship also provided a platform to discuss career choices (54% students, 78% staff) and network within the profession (54% students, 64% of staff). Lastly, 50% of students and 42% of staff found it helpful to discuss personal issues.
Regarding access, 29% of students reported having a mentor at the time of the survey, significantly fewer than the 65% of staff who reported having had a mentor previously (p < 0.001). Among those reporting negative experiences with a previous mentor, common issues included the mentor seeming unsure how to proceed (45% students, 43% staff) and mentors not listening or providing feedback (40% students, 43% staff). Some respondents felt their opinions were not valued (15% students, 14% staff), and many students (75%) felt that mentors did not spend sufficient time with them. A small percentage of students (5%) and 29% of staff reported that their mentor did not maintain professional boundaries. Some respondents did not get along with their mentors (10% students, 14% staff).
Regarding desired communication frequency, similar proportions of staff and students wanted communication “as needed.” One-quarter of students expressed a preference for meeting weekly, significantly more than their staff counterparts (p = 0.003). The majority of both groups favoured a blended (online and face-to-face) interaction style, with significantly more staff preferring this modality (p = 0.015).
Key perceived benefits for mentors included personal satisfaction (81%), leadership skill development (74%), and professional development (73%). Personal development (67%) and improved communication skills (62%) were also noted. Nearly half (48%) acknowledged teaching skill development as a benefit. Lastly, nearly half of the respondents (48%) acknowledged the development of teaching skills as a benefit of mentoring.
The survey also explored the potential benefits of mentorship to the Faculties of Medical Sciences (FMS) at UWI. Almost all respondents (98%) agreed that mentorship could provide positive role modelling. Other potential benefits included retention of students within DM programmes (67%), increased research output (63%), and recruitment of students in medical school (39%).
Most students (77%) and staff (89%) expressed interest in participating in a mentorship programme, with no significant gender preference for mentors or mentees. Most staff preferred mentoring two to five students, while most students (72%) preferred faculty members as mentors. The preferred relationship style was a blend of structured meetings and interaction as needed.
3.2. Differences Between Sites
No significant association was found between campus site and respondents’ understanding of what mentoring meant (p > 0.05 for all). Conversely, the association between campus affiliation and current student access to a mentor within the Faculty of Medical Sciences was statistically significant (p < 0.001), indicating differences across campuses. Among those with current mentor access at the time of the survey, the highest proportion was from the Bahamas (61.5%), followed by Cave Hill (52.6%), while Mona (30.2%) and St. Augustine (11.5%) had the lowest rates. Similarly, there was a significant association between campus affiliation and past student access to a mentor (p = 0.001). Among students who had past access to a mentor, the highest proportion was from Cave Hill (47.4%), followed closely by Bahamas (38.5%) and Mona (37.7%), while St. Augustine had the lowest access rate (5.8%). Staff reporting of having had a previous mentor did not significantly differ by site (p = 0.078), suggesting that differences in mentorship experience across campuses could be due to chance. The highest proportion was from Mona (88.9%), followed by Cave Hill (69.0%) and Bahamas (68.8%), and the lowest from St. Augustine (45.5%). For both populations, there were no differences across sites and mentorship relationship type, mentorship style, frequency, or gender preference. (p > 0.05 for all). Similarly, willingness to participate in a future programme did not significantly differ by site for students (p = 0.168) or staff (p = 0.343).
3.3. Associations Across Levels of Staff and Students
A significant association was found between past mentor access and the students’ year of study (p = 0.001). The proportion of students reporting past access to a mentor was 50.0% in Year 1, 12.5% in Year 2, 57.1% in Year 3, 17.2% in Year 4, and 57.1% in Year 5. However, current mentor access showed no significant association with year of study (p = 0.231). Mentoring style preferences (p = 0.139–0.683), communication frequency (p = 0.387), and preference for structured versus casual relationships (p = 0.423) also did not significantly vary by students’ year of study.
Staff employment status showed associations with certain mentorship outcomes. Full-time staff were significantly more likely than part-time staff to report that mentorship provided research opportunities (46.5% vs. 22.6%, p = 0.038). Conversely, part-time staff were slightly more likely to view mentorship as involving discussion of exam/study techniques (32.1% vs. 23.3%, p = 0.014). Part-time staff also more frequently reported mentorship as beneficial for attaining clinical knowledge and skills compared to full-time staff (49.1% vs. 32.6%, p < 0.001). Despite these differences, the vast majority of both full-time (88.4%) and part-time (86.8%) staff expressed interest in becoming a mentor, with no significant difference (p = 0.187).
Among academic staff (lecturers 49%, senior lecturers 34%, professors 17%), professors (85.7%) were significantly more likely to report mentorship providing research opportunities compared to lecturers (30%) and senior lecturers (50%) (p = 0.049). However, academic rank was not significantly associated with the desire to become a mentor (p = 0.753), having had a mentor (p = 0.094), or the perceived usefulness of mentorship (p = 0.222). Although non-significant, 85.7% of professors reported having had mentors compared to 65.0% of lecturers and 78.6% of senior lecturers, and all professors (100.0%) found their mentorship useful compared to 55.0% of lecturers and 78.6% of senior lecturers.
4. Discussion
This study highlights predominantly positive perceptions of mentorship among both students and staff at UWI FMS, aligning with findings from other medical education contexts [5,11]. Respondents valued mentorship particularly for observing positive role models, improving communication skills, and acquiring clinical knowledge. Mentorship was also seen as crucial for academic and career support, including exam preparation, study techniques, research opportunities, and career guidance. These perceived benefits are broadly consistent with the wider literature on medical student mentorship [10,11,12].
The results of this study also indicated that mentorship could positively impact the institution through enhanced role modelling, increased research output, improved student retention within degree programmes, and potential recruitment of medical students. This is consistent with reviews that have also highlighted that mentorship can provide medical students with increased research opportunities, guidance on career decisions, and enhanced professional and personal development, which can positively impact the institution [2].
Notably, a significant difference was observed in the availability of current mentors for students compared to past mentors for staff, with over twice as many staff members having had previous access to a mentor. The reasons for this may be multifactorial. Factors such as a downward trend in mentorship access, growing student-to-staff ratios, opportunities for continued mentoring among staff after formal medical training, and generational differences in the definition of a mentor may explain this mentorship gap.
However, this study also identified areas for improvement. Reports of negative experiences, such as mentors seeming unsure, not listening, or not dedicating sufficient time, align with existing literature on problematic mentoring relationships [13]. While reported by a minority, these experiences underscore the need for adequate mentor training and programme oversight to ensure effectiveness.
Despite the challenges, the survey results indicated that mentoring also offers significant benefits to the mentors themselves. Many mentors reported personal satisfaction and recognised the development of leadership and teaching skills as valuable outcomes of their mentoring roles. These findings underscore the reciprocal nature of mentorship, where mentors also gain valuable insights and professional growth through their mentoring experiences.
This study suggests that a preferred mentorship style blending “meeting as needed” and a structured approach indicates the importance of flexibility in mentorship arrangements. While this approach can cater to the unique needs and preferences of both mentees and mentors, it is important to set clear boundaries to avoid overdependence. Some authors have described the importance of being able to meet the needs of various individuals while at the same time providing structure within established codes of conduct [14].
In this study, student access to mentors varied across campuses, with some campuses showing higher access than others. This suggests that factors specific to each campus, such as resource availability, programme organisation, or institutional culture, may play a role in shaping students’ experiences with mentorship. A global perspective on mentorship in medical schools found important differences in mentorship goals within the international medical community, indicating that institutional settings can significantly influence mentorship experiences [2].
Student access to past mentors also varied by year of study, with first-year, third-year, and fifth-year students reporting higher proportions of past mentor access. This variation may reflect changes in students’ needs or priorities as they progress through their medical education, with different years presenting distinct challenges and opportunities for seeking mentorship. A study exploring the mentorship needs of fourth-year medical students applying for paediatrics residency found that these students have specific mentorship needs, highlighting how mentorship requirements can evolve throughout medical training [15].
Differences related to staff employment status also emerged. Full-time staff’s greater reporting of research opportunities through mentorship may reflect their differing roles and potentially greater research focus compared to part-time staff, aligning with findings linking mentorship to research productivity [12]. Within the staff, professors were significantly more likely to say that their mentorship provided research opportunities compared to lecturers and senior lecturers. This finding aligns with the typical career progression in academia, where professors often have a stronger emphasis on and involvement in research. Mentorship of junior faculty by seniors can enhance their progression and contribute to an institution’s mentorship culture [16].
4.1. Next Steps
The high level of interest expressed by both students and staff provides strong support for establishing and maintaining effective mentorship programmes across the region. As highlighted in a scoping review, ongoing assessment of mentoring dynamics and measurement of longitudinal outcomes for all stakeholders are crucial [17]. In the absence of a definitive “best practice” for mentorship, researchers have suggested key considerations for implementing and revising such programmes [18].
Addressing the negative experiences reported by some respondents requires mitigating strategies. This requires a multi-faceted approach, including a robust mentor selection process with screening and comprehensive training. Training should focus on setting clear expectations, providing constructive feedback, and avoiding detrimental behaviours [19]. Furthermore, careful mentor–mentee matching based on style, preferences, and goals, alongside clear reporting and monitoring mechanisms, can help address potential power imbalances and ensure adequate programme support [20].
Qualitative methods involving focus groups or in-depth interviews could provide deeper insights into the mentoring process, as utilised by other researchers [21]. Future research focusing on postgraduate students could also examine mentorship’s impact on specialty selection and their development as practitioners and future mentors.
4.2. Strengths and Limitations
This study represents the first regional assessment of both potential mentee and mentor willingness and perceptions regarding mentorship within the UWI FMS. The findings provide valuable data specific to this context, identifying preferences among both populations that can inform the design of tailored mentorship programmes.
The major limitations of this survey were its poor response rate and reliance on convenience sampling. Failure to attain the minimally calculated sample size also resulted in an under-powered study. This may have led to both type 1 and type 2 errors, as well as biased prevalences. Studies on graduate medical students found that higher response rates were achieved through strong evaluator–participant relationships, well-timed surveys, and persistent follow-ups [22]. Investment in university systems enabling closer student contact might also enhance participation. High response rates in other medical school surveys have been linked to strong faculty support, student representation, feedback mechanisms, protected completion time, incentives, and awareness campaigns [23].
Selection bias was a concern, which may limit the generalisability of the study’s findings to the entire student or staff population. The focus on MBBS students may not capture the perspectives of students in other allied health programmes within the FMS. Stratifying sampling techniques by programme and year can improve generalisability. Personalised invitations to randomly selected participants can also reduce selection bias [24].
5. Conclusions
This study underscores a clear perceived need and appreciation for the benefits of mentorship within the UWI FMS context. Both students and staff recognise its potential value for personal and professional development. Formalising or enhancing mentorship programmes across UWI FMS holds promise for fostering positive outcomes for mentors and mentees alike, contributing to the faculty’s overall growth and success. Optimising these experiences requires ongoing monitoring of relationships and outcomes, allowing the institution to strengthen its commitment to nurturing future medical professionals and fostering a supportive culture of continuous learning and professional development.
Author Contributions
Conceptualisation: S.M., P.H., A.G., V.S., M.F., S.G. and M.E. Data curation: S.M., P.H., A.G., V.S., M.F., S.G. and M.E. Formal analysis: S.M. Funding acquisition: not applicable. Methodology: S.M., P.H., A.G., V.S., M.F., S.G. and M.E. Project administration: S.M., P.H., A.G., V.S., M.F., S.G. and M.E. Visualisation: S.M., P.H., A.G., V.S., M.F., S.G. and M.E. Writing—original draft: S.M. Writing—review and editing: P.H., A.G., V.S., M.F., S.G. and M.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of The University of the West Indies, Cave Hill Campus, Barbados (Ref: CREC-CH.00070/06/2022 approved on 3rd February 2023).
Informed Consent Statement
All participants provided informed consent.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request. The research ethics committee reviewed the research protocol with jurisdiction before data collection.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported. No financial assistance was requested or obtained during the conduct of this study.
References
- Parker, L.; Vetter, D. Mentoring Each Other: Teachers Listening, Learning, and Sharing to Create More Successful Classrooms; Pembroke Publishers Limited: Toronto, ON, Canada, 2020; p. 141. [Google Scholar]
- Atlas, A.; Seltzer, E.; Watters, A.; Riley, B.; Chan, T. A Global Perspective of Mentorship in Medical Schools: Systematic Review from 2014–2019. Med. Sci. Educ. 2021, 31, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Dalgaty, F.; Guthrie, G.; Walker, H.; Stirling, K. The Value of Mentorship in Medical Education. Clin. Teach. 2017, 14, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Kashkoush, A.; Feroze, R.; Myal, S.; Prabhu, A.V.; Sansosti, A.; Tonetti, D.; Agarwal, N. Fostering Student Interest in Neurologic Surgery: The University of Pittsburgh Experience. World Neurosurg. 2017, 108, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Nimmons, D.; Giny, S.; Rosenthal, J. Medical Student Mentoring Programs: Current Insights. Adv. Med. Educ. Pract. 2019, 10, 113–123. [Google Scholar] [CrossRef] [PubMed]
- University of the West Indies. UWI Campuses. Available online: https://www.uwi.edu/campuses.php (accessed on 28 July 2023).
- University of the West Indies. Academic Advising Symposium 2020. Available online: http://conferences.sta.uwi.edu/aam2020/ (accessed on 28 July 2023).
- University of the West Indies. Triple A Strategy, 2017–2022. Available online: https://www.uwi.edu/uop/sites/uop/files/triple%20A%202022%20strategy%20framework.pdf (accessed on 28 July 2023).
- Minor, S.; Bonnin, R. What Do Medical Students Want from a Mentor? PRiMER 2022, 6, 552177. [Google Scholar] [CrossRef] [PubMed]
- Radha Krishna, L.K.; Renganathan, Y.; Tay, K.T.; Tan, B.J.X.; Chong, J.Y.; Ching, A.H.; Prakash, K.; Quek, N.W.S.; Peh, R.H.; Chin, A.M.C.; et al. Educational Roles as a Continuum of Mentoring’s Role in Medicine–A Systematic Review and Thematic Analysis of Educational Studies from 2000 to 2018. BMC Med. Educ. 2019, 19, 439. [Google Scholar] [CrossRef] [PubMed]
- Dimitriadis, K.; von der Borch, P.; Störmann, S.; Meinel, F.G.; Moder, S.; Reincke, M.; Fischer, M.R. Characteristics of mentoring relationships formed by medical students and faculty. Med. Educ. Online 2012, 17, 17242. [Google Scholar] [CrossRef] [PubMed]
- Farkas, A.H.; Allenbaugh, J.; Bonifacino, E.; Turner, R.; Corbelli, J.A. Mentorship of US Medical Students: A Systematic Review. J. Gen. Intern. Med. 2019, 34, 2602–2609. [Google Scholar] [CrossRef] [PubMed]
- Limeri, L.B.; Asif, M.Z.; Bridges, B.H.T.; Esparza, D.; Tuma, T.T.; Sanders, D.; Morrison, A.J.; Rao, P.; Harsh, J.A.; Maltese, A.V.; et al. “Where’s My Mentor?!” Characterizing Negative Mentoring Experiences in Undergraduate Life Science Research. CBE Life Sci. Educ. 2019, 18, ar61. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.S.; Teo, S.W.; Pei, Y.; Sng, J.H.; Yap, H.W.; Toh, Y.P.; Krishna, L.K.R. A Framework for Mentoring of Medical Students: Thematic Analysis of Mentoring Programmes between 2000 and 2015. Adv. Health Sci. Educ. 2018, 23, 671–697. [Google Scholar] [CrossRef] [PubMed]
- Lester, T.R.; Rassbach, C.E.; Blankenburg, R. What Are the Unique Mentorship Needs of Fourth-Year Medical Students Applying to Pediatrics Residency? Acad. Pediatr. 2020, 20, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Choi, A.M.K.; Moon, J.E.; Steinecke, A.; Prescott, J.E. Developing a Culture of Mentorship to Strengthen Academic Medical Centers. Acad. Med. 2019, 94, 630. [Google Scholar] [PubMed]
- Ng, Y.X.; Koh, Z.Y.K.; Yap, H.W.; Tay, K.T.; Tan, X.H.; Ong, Y.T.; Tan, L.H.E.; Chin, A.M.C.; Toh, Y.P.; Shivananda, S.; et al. Assessing Mentoring: A Scoping Review of Mentoring Assessment Tools in Internal Medicine between 1990 and 2019. PLoS ONE 2020, 15, e0232511. [Google Scholar] [CrossRef]
- Fornari, A.; Murray, T.S.; Menzin, A.W.; Woo, V.A.; Clifton, M.; Lombardi, M.; Shelov, S. Mentoring Program Design and Implementation in New Medical Schools. Med. Educ. Online 2014, 19, 24570. [Google Scholar] [CrossRef] [PubMed]
- Eby, L.T.; McManus, S.E.; Simon, S.A.; Russell, J.E.A. The Protege’s Perspective Regarding Negative Mentoring Experiences: The Development of a Taxonomy. J. Vocat. Behav. 2000, 57, 1–21. [Google Scholar] [CrossRef]
- Tuma, T.T.; Adams, J.D.; Hultquist, B.C.; Dolan, E.L. The Dark Side of Development: A Systems Characterization of the Negative Mentoring Experiences of Doctoral Students. CBE Life Sci. Educ. 2021, 20, ar16. [Google Scholar] [CrossRef] [PubMed]
- Pölczman, L.; Jámbor, M.; Győrffy, Z.; Purebl, G.; Végh, A.; Girasek, E. A qualitative study of mentors’ perceptions and experiences of a near-peer mentoring program for medical students. Front. Educ. 2024, 9, 1372697. [Google Scholar] [CrossRef]
- Ericson, A.; Bonuck, K.; Green, L.A.; Conry, C.; Martin, J.C.; Carney, P.A. Optimizing Survey Response Rates in Graduate Medical Education Research Studies. Fam. Med. 2023, 55, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Javidan, A.P.; Rai, Y.; Cheung, J.; Patel, R.V.; Kulasegaram, K.M. Six ways to maximize survey response rates: Lessons from a medical school accreditation survey in a Canadian setting. Can. Med. Educ. J. 2023, 14, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Shiyab, W.; Ferguson, C.; Rolls, K.; Halcomb, E. Solutions to address low response rates in online surveys. Eur. J. Cardiovasc. Nurs. 2023, 22, 441–444. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Academic Society for International Medical Education. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).