Abstract
The incidence of obesity is increasing worldwide. Body mass index (BMI) is a common method of diagnosing obesity, but research on judging the appropriate body weight of Chinese children aged 3–6 years is still lacking. Bioelectrical impedance analysis (BIA) is a safe, accurate, reliable and inexpensive method for screening overweight and obesity. The objectives of this research were to reveal the consistency between BMI and BIA in assessing the obesity characteristics of children aged 3–6 years. In this study, preschool boys (n = 392) and girls (n = 309) aged 3–6 years were recruited from kindergartens in Zhejiang province of China, and a survey of BMI and BIA, which was measured by InBody J20, was completed. BMI and BIA were analyzed by Pearson correlation analysis and linear regression analysis. The linear relationship between rates and a regression equation were established by using the Kappa coefficient to test the consistency between BMI and body fat percentage. The BMI of boys and girls decreased from 19.2 ± 4.9 and 18.1 ± 2.4 at the age of 3 to 14.1 ± 3.3 and 15.1 ± 3.3 at the age of 6 and showed a downward trend as age increased. The correlation between BMI and body fat percentage was 0.533 for boys and 0.539 for girls. The Kappa coefficient test results of BMI and body fat percentage showed that Kappa value = 0.339, p < 0.05, indicating that the diagnostic results of BMI and body fat percentage were consistent, but the consistency was general.
1. Introduction
Globally, the obesity epidemic has become a major public health problem, and the number of school-age children and adolescents has risen by more than 10-fold in just 40 years, from 11 million to 124 million [1]. Body mass index (BMI) is an indicator commonly used to judge whether a human body is obese. However, the use of BMI to assess body fat content is flawed [2]. First of all, height is an important part of the BMI calculation formula. Children and adolescents or shorter adults will have a higher BMI, and BMI easily confuses muscle and adipose tissue. Carpenter [3] also found that BMI is less sensitive to the detection of general obesity. There are few studies comparing the relationship between children’s BMI and bioelectrical impedance analysis (BIA) results. There is no clear answer regarding the consistency between BMI and BIA in diagnosing childhood obesity. Therefore, the purpose of this study was to reveal the consistency between BMI and BIA in diagnosing obesity in children aged 3–6 years and provide a scientific basis for the future use of BMI to diagnose overweight and obesity in children aged 3–6 years.
2. Subjects and Methods
2.1. Subjects
According to the random overall sampling method, 701 children aged 3–6 in 4 kindergartens in Hangzhou city of China were tested for body shape and body fat. More information is provided in Table 1.

Table 1.
Years and gender distribution of sample.
2.2. Methods
We used InBody J20 produced by Best Company in South Korea to test the body composition of children. The test parameters include: height, weight, total body water, body fat, protein, inorganic salts, etc. Data collection time: May–July in 2019.
We used Pearson correlation to analyze the correlation between BMI and body fat percentage and used the Kappa coefficient to test the consistency between BMI and body fat percentage. The Kappa consistency test, that is, the consistency level test, is an examination of whether two ordinal variables have the same level. The Kappa value, that is, the inter-rater coefficient of internal consistency, is an important indicator for evaluating the degree of consistency. When the Kappa value is between 0.8 and 1.0, the consistency between the two indicators is very good; when it is between 0.61 and 0.8, the consistency is good; when it is between 0.41 and 0.6, the consistency is medium; when it is between 0.21 and 0.4, the consistency is general; and when it is between 0 and 0.2, the consistency is poor. A Kappa value equal to 0 indicates that the results of the diagnostic test are completely determined by random factors.
3. Results
3.1. The Height, Body Weight and BMI of the Subjects
Boys and girls grew from 98.5 ± 0.1 cm and 97.5 ± 0.1 cm at the age of 3 to 119.6 ± 0.1 cm and 118.6 ± 0.1 cm at the age of 6, respectively (Table 2). There was a significant gender difference in height after the age of 5 (p < 0.05).

Table 2.
Gender difference in height ( ± SD, cm).
The body weight of boys and girls increased from 18.3 kg and 17.2 kg at the age of 3 to 20.1 kg and 21.1 kg at the age of 6, respectively. There was no gender difference in the weight of boys and girls at any age (p > 0.05, Table 3).

Table 3.
Gender difference in body weight ( ± SD, kg).
The mean BMI for boys was 16.0 kg/m2, and the mean for girls was 16.5 kg/m2. For all of the children, there was no gender difference between the two groups (p > 0.05). However, for the 6-year-old group, there was a significant difference between boys and girls (p < 0.01). The BMI of children aged 3~6 years showed a general downward trend with age (Table 4).

Table 4.
Gender difference in BMI ( ± SD, kg/m2).
3.2. Analysis of Body Composition of Children Aged 3~6
The body composition of children aged 3–6 generally remained stable with the increase in age (Table 5 and Table 6). However, there was no gender difference, p > 0.05.

Table 5.
Body composition of boys aged 3~6 ( ± SD, n = 392).

Table 6.
Body composition of girls aged 3~6 ( ± SD, n = 309).
There was no gender difference in the body fat percentage of boys and girls (Table 7, p = 0.328, p > 0.05). The body fat percentage of children aged 3–4 was higher than that of 4.5–6-year-old subjects, and the difference was statistically significant (p < 0.01). The percentage of body fat of children aged 3–6 years showed a downward trend with age (Figure 1).

Table 7.
Gender difference in body fat percentage ( ± SD, %).
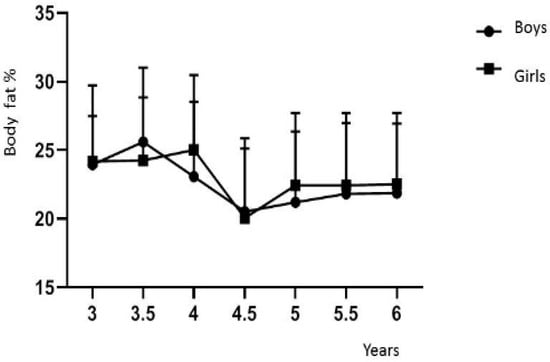
Figure 1.
Body fat percentage of children aged 3~6.
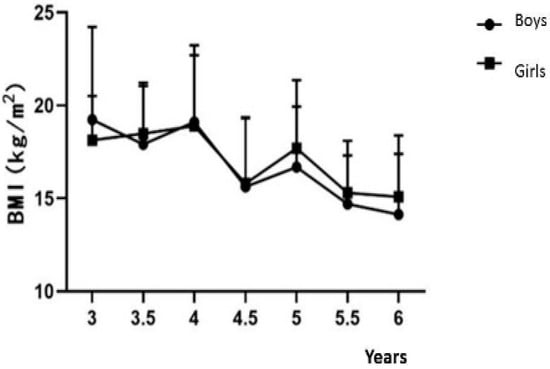
Figure 2.
BMI of children aged 3~6.
3.3. Kappa Coefficient Consistency Test
The correlation between BMI and body fat percentage was 0.533 for boys and 0.539 for girls (p < 0.05). Kappa is an important indicator of inter-rater reliability and a coefficient of internal consistency. The consistency test results of the Kappa coefficient of BMI and body fat percentage showed that Kappa value = 0.339, p < 0.05 (Table 8), indicating that the diagnostic results of BMI and body fat percentage were consistent, but the Kappa value was between 0.21 and 0.4, indicating that the consistency was general.

Table 8.
Kappa coefficient consistency test for BMI and BIA body fat.
4. Discussion
Zhao et al. [4] found that BMI is more reliable as a body fat indicator to predict adiposity in children. Unlike adults, BMI during childhood is generally attributed to the lean component rather than to the fat component of BMI [5]. Our findings may aid future obesity monitoring and intervention in children, and we may need multiple methods to measure and evaluate childhood obesity. We should combine BIA and BMI for screening obesity and overweight in young adults [6]. In the future, it is necessary to develop simpler and more effective methods for diagnosing obesity in children aged 3–6 years.
Author Contributions
Conceptualization, Q.C.; methodology, S.M.; writing—review and editing, Z.X.; supervision, M.C.; project administration, Q.C.; funding acquisition, M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a grant (18YJA890017) from Humanities and Social Science Research Fund Project of China’s Education Ministry. The authors are thankful to Zhejiang Normal University for the support.
Institutional Review Board Statement
The studies involving human participants were reviewed and approved by Ethical approval was obtained from the Faculty of Medicine ethics committee of Zhejiang Normal University (ZSDR2019013).
Informed Consent Statement
Informed consent was obtained from all legal guardians of subjects involved in the study.
Data Availability Statement
All data and models that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lim, H.J.; Xue, H.; Wang, Y. Handbook of Eating and Drinking: Interdisciplinary Perspectives. Global Trends Obes. 2020, 1217–1235. [Google Scholar]
- Shah, N.R.; Braverman, E.R. Measuring adiposity in patients: The utility of body mass index (BMI), percent body fat, and leptin. PLoS ONE 2012, 7, e33308. [Google Scholar] [CrossRef]
- Carpenter, C.L.; Yan, E.; Chen, S.; Hong, K.; Arechiga, A.; Kim, W.S.; Heber, D. Body fat and body-mass index among a multiethnic sample of college-age men and women. J. Obes. 2013, 2013, 790654. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Zhang, Y. Body mass index (BMI) predicts percent body fat better than body adiposity index (BAI) in school children. Anthropol. Anz. 2015, 72, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Maynard, L.M.; Wisemandle, W.; Roche, A.F.; Chumlea, W.C.; Guo, S.S.; Siervogel, R.M. Childhood body composition in relation to body mass index. Pediatrics 2001, 107, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Hung, S.P.; Chen, C.Y.; Guo, F.R.; Chang, C.I.; Jan, C.F. Combine body mass index and body fat percentage measures to improve the accuracy of obesity screening in young adults. Obes. Res. Clin. Pract. 2017, 11, 11–18. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).