Abstract
Background: Breakthrough infections (BTIs) continue to occur among healthcare workers (HCWs) despite full COVID-19 vaccination, raising concerns about ongoing vulnerability in this high-risk group. In addition to initial BTIs, breakthrough reinfections (BTRs) have emerged as a challenge, with some HCWs experiencing multiple episodes of infection after vaccination. This study investigated the factors influencing breakthrough infection and reinfection rates among HCWs between January 2021 and December 2022 in Davao City, Philippines. Methods: This retrospective cohort study was conducted using secondary data from the Davao City Epidemiological Surveillance Unit, approved by the Department of Health. This study included 1011 fully vaccinated HCWs from various congressional districts. Results: BTI was observed in all HCWs included in the study. However, BTRs varied across occupational groups: medical technologists showed the highest reinfection rate (22.37%), followed by physicians (13.48%), and nurses/nurse aides (10.14%). Booster vaccination significantly reduced BTRs (5.83% vs. 11.18%, p = 0.0267). Occupation and institutional type were significant factors, with higher rates reported by physicians and in public hospitals (p = 0.0002 and p = 0.0041, respectively). The vaccine manufacturer, sex, age, and booster type showed no significant differences. Conclusion: These findings highlight the importance of targeted interventions for high-risk HCWs and emphasize the effectiveness of the booster vaccination.
1. Introduction
The COVID-19 pandemic has posed unprecedented challenges to healthcare systems worldwide, with healthcare workers (HCWs) at the forefront of the response facing significant risks of infection [1,2]. Despite the rapid rollout of vaccines, breakthrough infections (BTIs), defined as laboratory-confirmed SARS-CoV-2 infections occurring at least 14 days after full vaccination, continue to occur among HCWs, particularly in high-risk settings, such as hospitals and clinics [3,4,5]. Breakthrough infections have been reported following direct patient care, aerosol-generating procedures, and even during outbreaks among highly vaccinated staff, often resulting in mild or asymptomatic cases. However, they still pose risks of nosocomial transmission and workforce disruption.
Of growing concern are breakthrough reinfections (BTRs), in which HCWs experience multiple episodes of SARS-CoV-2 infection after completing their vaccination series [6,7,8]. Such cases highlight the ongoing vulnerability of HCWs to repeated exposure, their potential for waning immunity, and the emergence of new viral variants that may evade vaccine-induced protection. Understanding the factors contributing to both breakthrough infections and reinfections is essential for developing targeted strategies to protect HCWs and to maintain the resilience of healthcare services.
Recent studies have highlighted occupational exposure, adherence to infection prevention practices, and vaccine effectiveness as possible factors influencing the risk of breakthrough infections among HCWs [9,10,11,12]. Data from diverse healthcare settings, particularly in developing countries, remain limited. This knowledge gap hinders the development of context-specific interventions to mitigate the risk of infection among HCWs. As with many other countries, the Philippines implemented a comprehensive vaccination program for HCWs [13,14]. However, the effectiveness of this program in real-world settings, particularly in the face of emerging variants and waning immunity, requires further investigation. Davao City, as a major urban center in the southern Philippines, provides a unique context for studying these dynamics, offering insights that may be applicable to similar settings in the region.
This study aimed to investigate the key factors associated with BTIs and BTRs among fully vaccinated HCWs in Davao City, focusing on the roles of occupation, institutional setting, and booster vaccination status. The findings of this study have the potential to inform targeted interventions for high-risk HCW groups, guide booster vaccination strategies, and contribute to a broader understanding of the COVID-19 transmission dynamics in healthcare settings. This research is particularly timely as healthcare systems continue to address the ongoing challenges of the pandemic and the need to protect their workforce while maintaining essential services.
2. Methodology
2.1. Study Design
We performed a retrospective cohort study, following a group of 1011 fully vaccinated HCWs from the time of their full vaccination, between January 2021 and December 2022, to assess the incidence and risk factors of SARS-CoV-2 infection in BTIs and BTRs. This study followed the STROBE guidelines for observational research. All studies were performed in accordance with relevant guidelines and regulations. The Research Ethics Committee of the University of the Immaculate Conception approved this study by 18 October 2021 (No. 351/M-8). The need for informed consent was waived by the Ethics Committee of the University of Immaculate Conception.
2.2. Study Population
Figure 1 presents a consort flow diagram of cohort selection and analysis. The Davao City Epidemiological Surveillance Unit of the Department of Health, Philippines, pro-vided data on 1295 fully vaccinated HCWs. A comprehensive screening process was conducted to assess eligibility based on the predetermined inclusion and exclusion criteria.
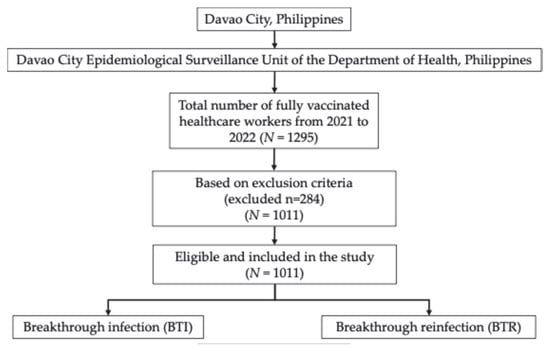
Figure 1.
Consort chart showing cohort selection for analysis in Davao City, Philippines, 2021–2022 (N = 1011).
Inclusion criteria:
- Fully vaccinated HCWs;
- Complete and accurate vaccination records for both first and second doses.
Exclusion criteria:
- A history of pre-vaccination infection;
- Second vaccine dose administered but date not recorded;
- No record of second vaccine dose;
- Complete second dose data but incomplete first dose data;
- Missing records for both first and second doses.
Based on these criteria, 1011 HCWs were included in the analysis. This refined cohort, representing a significant portion of the initial sample, ensured a robust dataset for investigating breakthrough infections and related factors among healthcare workers in Davao City. A careful selection process will enhance the integrity and reliability of the data for further studies.
2.3. Study Period
The study period was from January 2021 to December 2022, encompassing the first two years of the COVID-19 pandemic, which was driven by the alpha, delta, and, to a lesser extent, omicron variants of SARS-CoV-2. During this period, all HCWs in the Philippines who were suspected or confirmed to have SARS-CoV-2 infection had free access to PCR testing and subsequent treatment.
2.4. Data Source
Data on COVID-19 vaccination (dates, vaccine type, and manufacturer for each vaccination episode) and SARS-CoV-2 testing dates (results and dates) were retrieved from Davao City Epidemiological Surveillance Unit, Department of Health, Philippines. The analysis focused on the incidence of breakthrough infections from 2021 to 2022, assessing factors such as the age, sex, occupation, and booster status of HCWs. In this study, SARS-CoV-2 infection was identified using qualitative assays because quantitative data, including viral load measurements, were not available.
2.5. Exposures
For the exposure variables, we considered both the primary series of COVID-19 vaccines and booster doses. The COVID-19 primary vaccine series was defined as the vaccine administered as the first dose for 1-dose series and the second dose for 2-dose series. A vaccine booster was defined as any additional SARS-CoV-2 vaccine dose received after completion of the primary vaccination series against COVID-19.
2.6. Outcomes
Breakthrough infections were defined as laboratory-confirmed SARS-CoV-2 infections occurring at least 14 days after the completion of the full vaccination series. In this study, all HCWs experienced at least one BTI. To provide further distinction, we use the term “breakthrough reinfections (BTRS)” to describe HCWs who, after being fully vaccinated, contracted SARS-CoV-2 (breakthrough infection) and subsequently became infected again (reinfection), with both infections occurring after vaccination and confirmed as distinct episodes [15,16]. The detection of BTIs and BTRs was based on positive SARS-CoV-2 results from either RT-PCR or antigen testing as recorded in the surveillance database. Symptom severity was assessed and classified as asymptomatic, mild, or moderate, based on available clinical records.
2.7. Statistical Analysis
All data were analyzed using the GraphPad Prism software (version 10). Descriptive statistics were used for the demographic variables. Fisher’s exact and χ2 tests were used to identify the associated risk factors for developing SARS-CoV-2 BTRs. Statistical significance was set to p ≤ 0.05.
3. Results
3.1. Demographic Characteristics of the Healthcare Workers in Davao City, Philippines
The study included 1011 HCWs, with the majority being female (69.93%, n = 707) compared to male (30.07%, n = 304). Most HCWs were under 40 years old (80.61%, n = 815), while the rest were over 40 years old (19.39%, n = 196). Regarding occupation, nurses and nurse aids comprised the largest group (41.94%, n = 424), followed by physicians (22.75%, n = 230), other occupations (15.23%, n = 154), other healthcare workers (12.56%, n = 127), and medical technologists (7.52%, n = 76). HCWs were primarily from private hospitals (47.28%, n = 478), public hospitals, and health facilities (40.36%, n = 408), with a smaller proportion from outpatient centers and non-medical institutions (12.36%, n = 125).
Sinovac was the most common vaccine type (67.26%, n = 680), followed by AstraZeneca (16.72%, n = 169), and Pfizer-BioNTech (13.35%, n = 135). Other vaccine types, including Moderna, SinoPharm, Gamaleya, and Janssen, were administered to a small percentage of HCWs. Regarding booster shots, 20.38% (n = 206) of the HCWs received a booster, with the majority opting for heterologous boosters (74.757%, n = 154) compared to homologous boosters (25.243%, n = 52). All the data are presented in Table 1.

Table 1.
Demographic characteristics and associated risk factor of breakthrough reinfections (BTRs) among fully vaccinated healthcare workers in Davao City, Philippines.
3.2. Incidence of Breakthrough Infections Among Healthcare Workers in Davao City, Philippines
All HCWs in this study experienced at least one BTI after vaccination, regardless of their role: physicians, nurses/nurse aides, medical technologists, other healthcare workers, or nonclinical staff. However, the rate of breakthrough reinfections (defined as a series of reinfections after the last vaccination) varied significantly between the groups (Table 1). Medical technologists had the highest rate of BTR at 22.37% (n = 17/76), followed by physicians at 13.48% (n = 31/230) and nurses/nurse aides at 10.14% (n = 43/424). Other healthcare workers had the lowest rate among clinical staff at 3.94% (n = 5/127), while non-clinical workers also showed a relatively low rate of 5.84% (n = 9/154).
3.3. Associated Risk Factors of Vaccine Breakthrough Infections
The data presented in Table 1 reveal significant differences in BTR rates among fully vaccinated individuals based on several factors. Notably, individuals who received booster shots had a BTR rate of 5.83% (n = 12), compared to 11.18% (n = 90) among those without boosters (p = 0.0267). Based on symptom classification, among those who received booster shots, asymptomatic cases were (n = 9) and mild or moderate cases were (n = 3). Among those without boosters, asymptomatic cases were (n = 61) and mild or moderate cases were (n = 29). Occupation also played a significant role, with medical technologists showing the highest rate of BTRs among the HCWs (p = 0.0002). The type of institution was another important factor, with public hospitals and health facilities reporting higher BTR rates than private hospitals and outpatient centers (p = 0.0041). Interestingly, the vaccine manufacturer, sex, and age did not show statistically significant differences in BTR rates. The booster types (homologous vs. heterologous) did not show a significant difference, although the sample size for this comparison was relatively small.
4. Discussion
Breakthrough SARS-CoV-2 infections in vaccinated individuals remain a significant concern during the ongoing COVID-19 pandemic. Data from Davao City, Philippines, provides valuable insights into the factors influencing BTI and BTR rates among HCWs, contributing to our understanding of vaccine effectiveness and the need for targeted interventions.
This study revealed significant differences in the BTR rates based on several factors. Notably, individuals who received booster shots demonstrated significant BTRs (5.83%) compared to those who did not receive booster shots (11.18%). This finding aligns with previous research indicating that booster doses can significantly reduce BTR cases among HCWs compared to those with only primary vaccination [17,18,19].
While our results showed variation in reinfection rates by profession, it is important to recognize that these differences are likely attributable to the varying frequency and intensity of contact with infected patients that are inherent to each healthcare role, rather than to the professional title alone. Occupation emerged as a crucial factor (p = 0.0002), with medical technologists exhibiting the highest BTR rate of 22.37%, which is consistent with findings from other studies that identified laboratory personnel as a high-risk group because of their frequent handling of potentially infectious specimens [20,21,22]. This elevated risk likely stems from challenges associated with maintaining rigorous safety protocols when processing large volumes of COVID-19 samples. Physicians (13.48%) and nurses/nurse aides (10.14%) also reported relatively elevated BTR rates, which aligns with their roles in direct patient care, involving prolonged close contact with infected individuals. The frequency and duration of patient contact, especially in COVID-19-positive cases, are key determinants of infection risk among these professionals. In contrast, other healthcare workers (3.94%) and non-clinical staff (5.84%) experienced markedly lower reinfection rates, which is likely attributable to reduced direct patient interaction and potentially stricter compliance with infection control measures.
It is also essential to consider the methods used to protect HCWs during patient interactions [12]. Standard infection prevention protocols, such as the consistent use of medical masks, face shields, gowns, gloves, and adherence to hand hygiene, are critical for reducing transmission risk. Variability in the availability, proper use, or adherence to these protective measures across different roles and institutions may contribute to the observed differences in infection rates. The higher BTR rates among medical technologists, physicians, and public healthcare facilities emphasize the need for targeted interventions including enhanced protective measures, routine testing protocols, and prioritized access to booster vaccination programs for high-risk groups. The type of institution also played a significant role [23], with public hospitals and health facilities reporting higher BTI rates than private hospitals and outpatient centers (p = 0.0041). This disparity may reflect differences in resource availability, patient volume, and adherence to infection prevention practices across healthcare settings.
In addition to these factors, the role of hospital equipment, particularly air filtration and purification systems such as HEPA filters, may also significantly influence the incidence of infection. Recent studies have demonstrated that the use of HEPA filters in clinical environments, such as dental clinics, can substantially reduce the risk of airborne SARS-CoV-2 infection compared to that in clinics without such equipment [24,25,26]. Therefore, differences in the presence or quality of air purification systems between public and private institutions could be an important yet unmeasured contributor to the observed variation in BTR rates. Although our study did not collect data on the use of HEPA filters or other air purification systems, this should be considered a potential confounder and may help explain some of the differences observed between institutions. Future studies should include these environmental factors for a more comprehensive assessment of the risk of infection.
Interestingly, the study found no statistically significant differences in BTR rates based on the vaccine manufacturer, sex, or age. This contrasts with previous research suggesting age-related variations in vaccine effectiveness [27]. The lack of a significant difference between homologous and heterologous boosters is noteworthy, although the small sample size for this comparison warrants cautious interpretation.
The effectiveness of booster doses in reducing BTRs aligns with the broader understanding of waning immunity. Studies have shown that antibody levels decline within 3-6 months post vaccination, increasing susceptibility to BTIs and BTRs, particularly during periods of high transmission or in the presence of immune-evasive variants [28,29]. The significant reduction in breakthrough cases among boosted individuals supports the implementation of booster campaigns as a key strategy for maintaining protection against SARS-CoV-2.
A particularly notable finding in this study was that all HCWs experienced at least one BTI during 2021–2022. This universal exposure among HCWs can be attributed to several contextual factors unique to Davao City. The city has experienced multiple surges in COVID-19 cases, with high community transmission rates driven by the emergence of variants such as delta and omicron. The persistently high number of cases placed immense pressure on the local healthcare system, which is characterized by a limited number of hospitals and healthcare facilities relative to the patient load. As a result, hospitals became overcrowded and patient-to-staff ratios increased, forcing HCWs to care for more patients, thereby increasing their cumulative exposure to SARS-CoV-2. This constant exposure was further exacerbated by staff shortages, requiring HCWs to work extended shifts with minimal rest, which could lead to fatigue and potential lapses in infection control practices. Additionally, periodic shortages of personal protective equipment (PPE) and inconsistent access to advanced infection control resources, such as air purification systems, likely increased the risk of infection [30,31]. These factors combined to create an environment in which even fully vaccinated HCWs, despite adherence to protective measures, faced a high likelihood of BTI.
The observed BTI rate among HCWs in our study was considerably higher than those reported in similar studies from other regions and countries. Studies from Italy, India, and Israel have reported BTI rates among vaccinated HCWs ranging from 2.6% to 18.6% [30,31]. However, a recent study in Bangladesh during the omicron wave found that more than 50% of vaccinated hospital-based HCWs experienced breakthrough infections, and overweight and obesity were identified as significant risk factors [32]. However, it is crucial to interpret these results cautiously because of the potential confounding variables not accounted for in the study, such as community transmission dynamics and individual behaviors outside the workplace. It is also important to note that, while both PCR and antigen tests are used to detect breakthrough infections in real-world studies, PCR remains the gold standard for confirming acute SARS-CoV-2 infection. Future research should address these limitations by investigating additional factors affecting BTR rates and considering larger sample sizes for comparisons between different booster strategies.
5. Conclusions
Based on this retrospective cohort study of fully vaccinated HCWs in Davao City, Philippines, breakthrough infections and reinfections persisted during the pandemic, with higher rates observed among those in clinical roles and in public healthcare settings, likely reflecting the more frequent contact with infected patients inherent to these occupations. Booster vaccination is associated with a significant reduction in reinfection rates, thereby emphasizing its protective benefits. These findings highlight the need for targeted booster programs and reinforced infection prevention strategies, especially for HCWs with high patient exposure, to better safeguard the healthcare workforce amid ongoing viral circulation.
Author Contributions
Conceptualization, A.A.H.J. and J.A.H.R.; methodology, A.A.H.J. and J.A.H.R.; software, A.A.H.J. and J.A.H.R.; validation, A.A.H.J. and J.A.H.R., R.J.T.S. and A.R.C.S.; formal analysis, A.A.H.J., J.A.H.R., R.J.T.S. and A.R.C.S.; investigation, A.A.H.J. and J.A.H.R., R.J.T.S. and A.R.C.S.; writing—original draft preparation, A.A.H.J., J.A.H.R., R.J.T.S. and A.R.C.S.; writing—review and editing, A.A.H.J. and J.A.H.R.; visualization, A.A.H.J. and J.A.H.R.; supervision, A.A.H.J.; project administration, A.A.H.J.; funding acquisition, A.A.H.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the University of the Immaculate Conception Research and Innovation Center.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the University of the Immaculate Conception (No. 351/M-8, 18 October 2021).
Informed Consent Statement
Patient consent was waived because this study exclusively utilized secondary data provided by The Davao City Epidemiological Surveillance Unit of the Department of Health, Philippines. No human participants were directly involved, and all data analyzed were collected for public health surveillance purposes.
Data Availability Statement
Dataset available on request from the authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Yang, Y.P.; Pan, S.J.; Zhang, M.X.; Chen, H.X.; Tung, T.H. The Impact of COVID-19 Pandemic on Healthcare Workers under the “Ten New Guidelines” in Taizhou, China. Prev. Med. Rep. 2024, 37, 102550. [Google Scholar] [CrossRef]
- Smallwood, N.; Harrex, W.; Rees, M.; Willis, K.; Bennett, C.M. COVID-19 Infection and the Broader Impacts of the Pandemic on Healthcare Workers. Respirology 2022, 27, 411–426. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Lee, J.; Ta, C.; Soroush, A.; Rogers, J.R.; Kim, J.H.; Natarajan, K.; Zucker, J.; Perl, Y.; Weng, C. Risk Factors Associated With SARS-CoV-2 Breakthrough Infections in Fully MRNA-Vaccinated Individuals: Retrospective Analysis. JMIR Public Health Surveill. 2022, 8, e35311. [Google Scholar] [CrossRef]
- Liu, C.; Lee, J.; Ta, C.; Soroush, A.; Rogers, J.R.; Kim, J.H.; Natarajan, K.; Zucker, J.; Weng, C. A Retrospective Analysis of COVID-19 MRNA Vaccine Breakthrough Infections—Risk Factors and Vaccine Effectiveness. medRxiv 2021. [Google Scholar] [CrossRef]
- Gopinath, S.; Ishak, A.; Dhawan, N.; Poudel, S.; Shrestha, P.S.; Singh, P.; Xie, E.; Tahir, P.; Marzaban, S.; Michel, J.; et al. Characteristics of COVID-19 Breakthrough Infections among Vaccinated Individuals and Associated Risk Factors: A Systematic Review. Trop. Med. Infect. Dis. 2022, 7, 81. [Google Scholar] [CrossRef] [PubMed]
- Pilz, S.; Theiler-Schwetz, V.; Trummer, C.; Krause, R.; Ioannidis, J.P.A. SARS-CoV-2 Reinfections: Overview of Efficacy and Duration of Natural and Hybrid Immunity. Environ. Res. 2022, 209, 112911. [Google Scholar] [CrossRef]
- Abu-Raddad, L.J.; Chemaitelly, H.; Bertollini, R. Severity of SARS-CoV-2 Reinfections as Compared with Primary Infections. New Engl. J. Med. 2021, 385, 2487–2489. [Google Scholar] [CrossRef]
- Hall, V.J.; Foulkes, S.; Saei, A.; Andrews, N.; Oguti, B.; Charlett, A.; Wellington, E.; Stowe, J.; Gillson, N.; Atti, A.; et al. COVID-19 Vaccine Coverage in Health-Care Workers in England and Effectiveness of BNT162b2 MRNA Vaccine against Infection (SIREN): A Prospective, Multicentre, Cohort Study. Lancet 2021, 397, 1725–1735. [Google Scholar] [CrossRef]
- Perez-Garcia, F.; Perez-Zapata, A.; Arcos, N.; De La Mata, M.; Ortiz, M.; Simón, E.; Hervás Fernández, I.; González Ventosa, V.; Muñoz Monte, M.; González Arroyo, J.; et al. Severe Acute Respiratory Coronavirus Virus 2 (SARS-CoV-2) Infection among Hospital Workers in a Severely Affected Institution in Madrid, Spain: A Surveillance Cross-Sectional Study. Infect. Control Hosp. Epidemiol. 2021, 42, 803–809. [Google Scholar] [CrossRef]
- Buonafine, C.P.; Paiatto, B.N.M.; Leal, F.B.; de Matos, S.F.; de Morais, C.O.; Guerra, G.G.; Martuchelli, M.V.V.; Oliveira, D.B.L.; Durigon, E.L.; Soares, C.P.; et al. High Prevalence of SARS-CoV-2 Infection among Symptomatic Healthcare Workers in a Large University Tertiary Hospital in São Paulo, Brazil. BMC Infect. Dis. 2020, 20, 1–8. [Google Scholar] [CrossRef]
- Stead, D.; Adeniyi, O.V.; Singata-Madliki, M.; Abrahams, S.; Batting, J.; Jelliman, E.; Parrish, A. Cumulative Incidence of SARS-CoV-2 and Associated Risk Factors among Healthcare Workers: A Cross-Sectional Study in the Eastern Cape, South Africa. BMJ Open 2022, 12, e058761. [Google Scholar] [CrossRef] [PubMed]
- Dzinamarira, T.; Mhango, M.; Dzobo, M.; Ngara, B.; Chitungo, I.; Makanda, P.; Atwine, J.; Nkambule, S.J.; Musuka, G. Risk Factors for COVID-19 among Healthcare Workers. A Protocol for a Systematic Review and Meta-Analysis. PLoS ONE 2021, 16, e0250958. [Google Scholar] [CrossRef]
- Cordero, D.A. “Leaving” Resilience for the Future? Exploring the Difficulty of Achieving Herd Immunity against COVID-19 in the Philippines. J. Public Health 2022, 44, e652–e653. [Google Scholar] [CrossRef] [PubMed]
- Cedeño, T.D.D.; Rocha, I.C.N.; Miranda, A.V.; Lim, L.T.S.; Buban, J.M.A.; Cleofas, J.V. Achieving Herd Immunity against COVID-19 in the Philippines. Public Health Chall. 2023, 2, e61. [Google Scholar] [CrossRef]
- Hasan, D.A.; Maulud, S.Q.; Jalal, P.J.; Priyanka; Choudhary, O.P. SARS-CoV-2 Vaccine Breakthrough Reinfection in a Health-Care Worker of Iraq: A Case Report. Hum. Vaccin Immunother. 2022, 18, 2055947. [Google Scholar] [CrossRef]
- Shastri, J.; Parikh, S.; Aggarwal, V.; Agrawal, S.; Chatterjee, N.; Shah, R.; Devi, P.; Mehta, P.; Pandey, R. Severe SARS-CoV-2 Breakthrough Reinfection With Delta Variant After Recovery From Breakthrough Infection by Alpha Variant in a Fully Vaccinated Health Worker. Front. Med. 2021, 8, 737007. [Google Scholar] [CrossRef] [PubMed]
- Skrzat-Klapaczyńska, A.; Bieńkowski, C.; Kowalska, J.; Paciorek, M.; Puła, J.; Krogulec, D.; Stengiel, J.; Pawełczyk, A.; Perlejewski, K.; Osuch, S.; et al. The Beneficial Effect of the COVID-19 Vaccine Booster Dose among Healthcare Workers in an Infectious Diseases Center. Vaccines 2022, 10, 552. [Google Scholar] [CrossRef]
- Oster, Y.; Benenson, S.; Nir-Paz, R.; Buda, I.; Cohen, M.J. The Effect of a Third BNT162b2 Vaccine on Breakthrough Infections in Health Care Workers: A Cohort Analysis. Clin. Microbiol. Infect. 2022, 28, 735.e1–735.e3. [Google Scholar] [CrossRef]
- Spitzer, A.; Angel, Y.; Marudi, O.; Zeltser, D.; Saiag, E.; Goldshmidt, H.; Goldiner, I.; Stark, M.; Halutz, O.; Gamzu, R.; et al. Association of a Third Dose of BNT162b2 Vaccine with Incidence of SARS-CoV-2 Infection among Health Care Workers in Israel. JAMA 2022, 327, 341. [Google Scholar] [CrossRef]
- Moosavi, S.; Namdar, P.; Moghaddam Zeabadi, S.; Akbari Shahrestanaki, Y.; Ghalenoei, M.; Amerzadeh, M.; Kalhor, R. Healthcare Workers Exposure Risk Assessment in the Context of the COVID-19: A Survey among Frontline Workers in Qazvin, Iran. BMC Health Serv. Res. 2023, 23, 1–7. [Google Scholar] [CrossRef]
- Atnafie, S.A.; Anteneh, D.A.; Yimenu, D.K.; Kifle, Z.D. Assessment of Exposure Risks to COVID-19 among Frontline Health Care Workers in Amhara Region, Ethiopia: A Cross-Sectional Survey. PLoS ONE 2021, 16, e0251000. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.S.; Ntlebi, V.; Made, F.; Sanabria, N.; Vetten, M.; Joseph, J.; Chin, G.; Jones, D.; Tlotleng, N. COVID-19 Cases among Medical Laboratory Services Staff in South Africa, 2020–2021: A Cohort Study. PLoS ONE 2022, 17, e0268998. [Google Scholar] [CrossRef] [PubMed]
- Issah, M.A.; Atinga, R.A.; Baku, A.A. Adherence to COVID-19 Protocols: A Comparative Study of Public and Private Hospitals in Ghana. Public. Health Pract. 2024, 7, 100463. [Google Scholar] [CrossRef]
- Sarapultseva, M.; Hu, D.; Sarapultsev, A. SARS-CoV-2 Seropositivity among Dental Staff and the Role of Aspirating Systems. JDR Clin. Trans. Res. 2021, 6, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Conway Morris, A.; Sharrocks, K.; Bousfield, R.; Kermack, L.; Maes, M.; Higginson, E.; Forrest, S.; Pereira-Dias, J.; Cormie, C.; Old, T.; et al. The Removal of Airborne SARS-CoV-2 and Other Microbial Bioaerosols by Air Filtration on COVID-19 Surge Units. Clin. Infect. Dis. 2021, 75, e97–e101. [Google Scholar] [CrossRef]
- Lindsley, W.G.; Derk, R.C.; Coyle, J.P.; Martin, S.B.; Mead, K.R.; Blachere, F.M.; Beezhold, D.H.; Brooks, J.T.; Boots, T.; Noti, J.D. Efficacy of Portable Air Cleaners and Masking for Reducing Indoor Exposure to Simulated Exhaled SARS-CoV-2 Aerosols—United States, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 972–976. [Google Scholar] [CrossRef]
- Dingemans, J.; van der Veer, B.M.J.W.; Gorgels, K.M.F.; Hackert, V.; den Heijer, C.D.J.; Hoebe, C.J.P.A.; Savelkoul, P.H.M.; van Alphen, L.B. Investigating SARS-CoV-2 Breakthrough Infections per Variant and Vaccine Type. Front. Microbiol. 2022, 13, 1027271. [Google Scholar] [CrossRef]
- Evans, J.P.; Zeng, C.; Carlin, C.; Lozanski, G.; Saif, L.J.; Oltz, E.M.; Gumina, R.J.; Liu, S.L. Neutralizing Antibody Responses Elicited by SARS-CoV-2 MRNA Vaccination Wane over Time and Are Boosted by Breakthrough Infection. Sci. Transl. Med. 2022, 14, eabn8057. [Google Scholar] [CrossRef]
- Chivu-economescu, M.; Vremera, T.; Ruta, S.M.; Grancea, C.; Leustean, M.; Chiriac, D.; David, A.; Matei, L.; Diaconu, C.C.; Gatea, A.; et al. Assessment of the Humoral Immune Response Following COVID-19 Vaccination in Healthcare Workers: A One Year Longitudinal Study. Biomedicines 2022, 10, 1526. [Google Scholar] [CrossRef]
- Bergwerk, M.; Gonen, T.; Lustig, Y.; Amit, S.; Lipsitch, M.; Cohen, C.; Mandelboim, M.; Levin, E.G.; Rubin, C.; Indenbaum, V.; et al. Covid-19 Breakthrough Infections in Vaccinated Health Care Workers. New Engl. J. Med. 2021, 385, 1474–1484. [Google Scholar] [CrossRef]
- Sabnis, R.; Patil, A.; Shete, N.; Rastogi, A.K. Break-through COVID-19 Infection Rate with Indian Strain in Single-Center Healthcare Workers—A Real World Data 2021. MedRxiv 2021. [Google Scholar] [CrossRef]
- Akhter, M.; Roy, S.K.; Khair, A.; Karim, M.R.; Mojlish, U.K.F.K.; Ahmed, M.U.; Ali, L. SARS-COV-2 Breakthrough Infection and Its Covariates among Healthcare Providers of a Hospital in Bangladesh during the Omicron Wave. Heliyon 2024, 10, e37287. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).