The Feasibility of a Music Therapy Respiratory Telehealth Protocol on Long COVID Respiratory Symptoms
Abstract
1. Introduction
1.1. Past Studies in Music and Medicine
1.2. Music Therapy
2. Methods
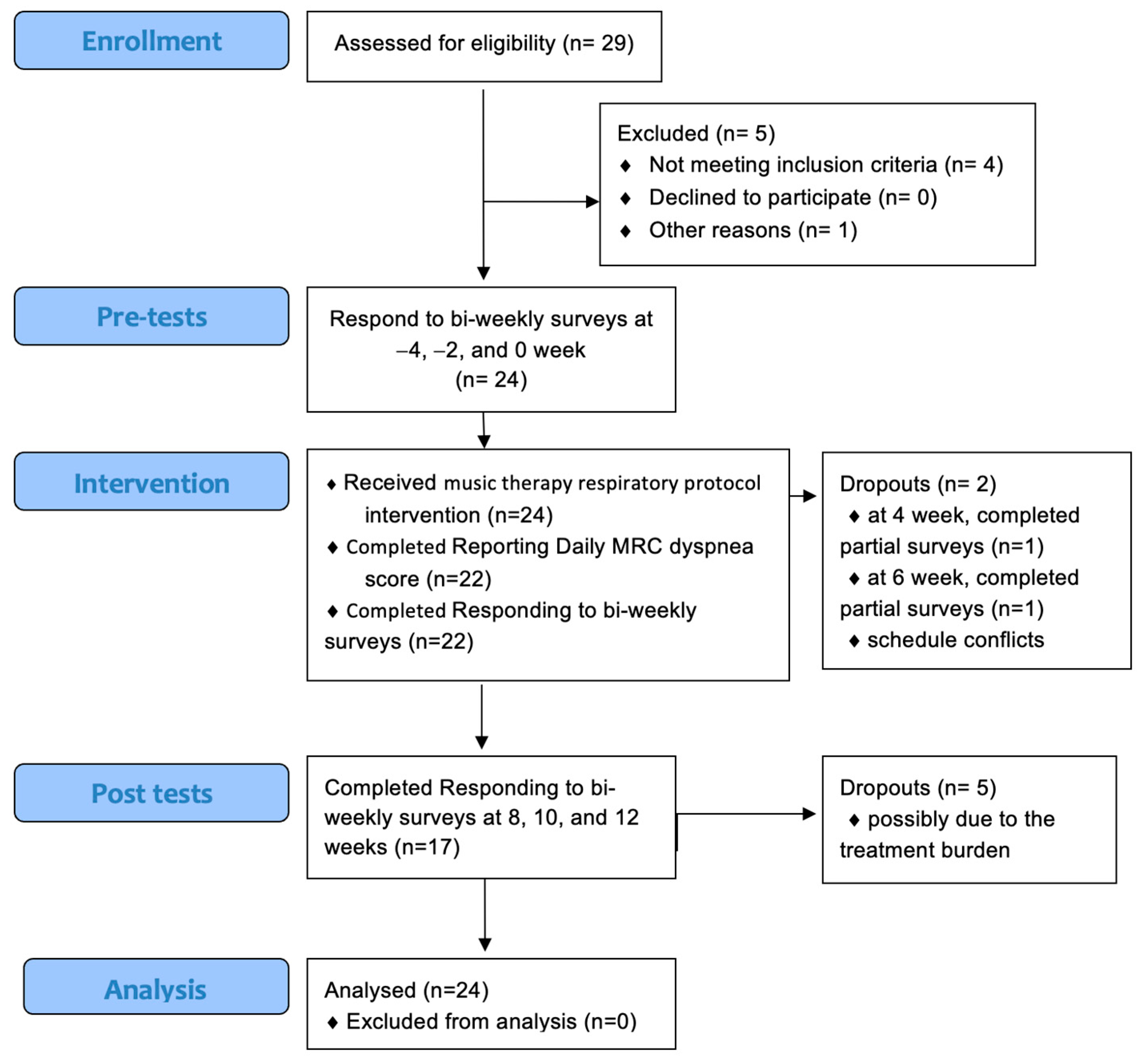
2.1. Study Design and Participants
2.2. Feasibility Measures
2.3. Procedure
Music Therapy Intervention
2.4. Outcome Measures
2.4.1. Primary Measures
2.4.2. Secondary Measures
2.5. Statistical Analysis
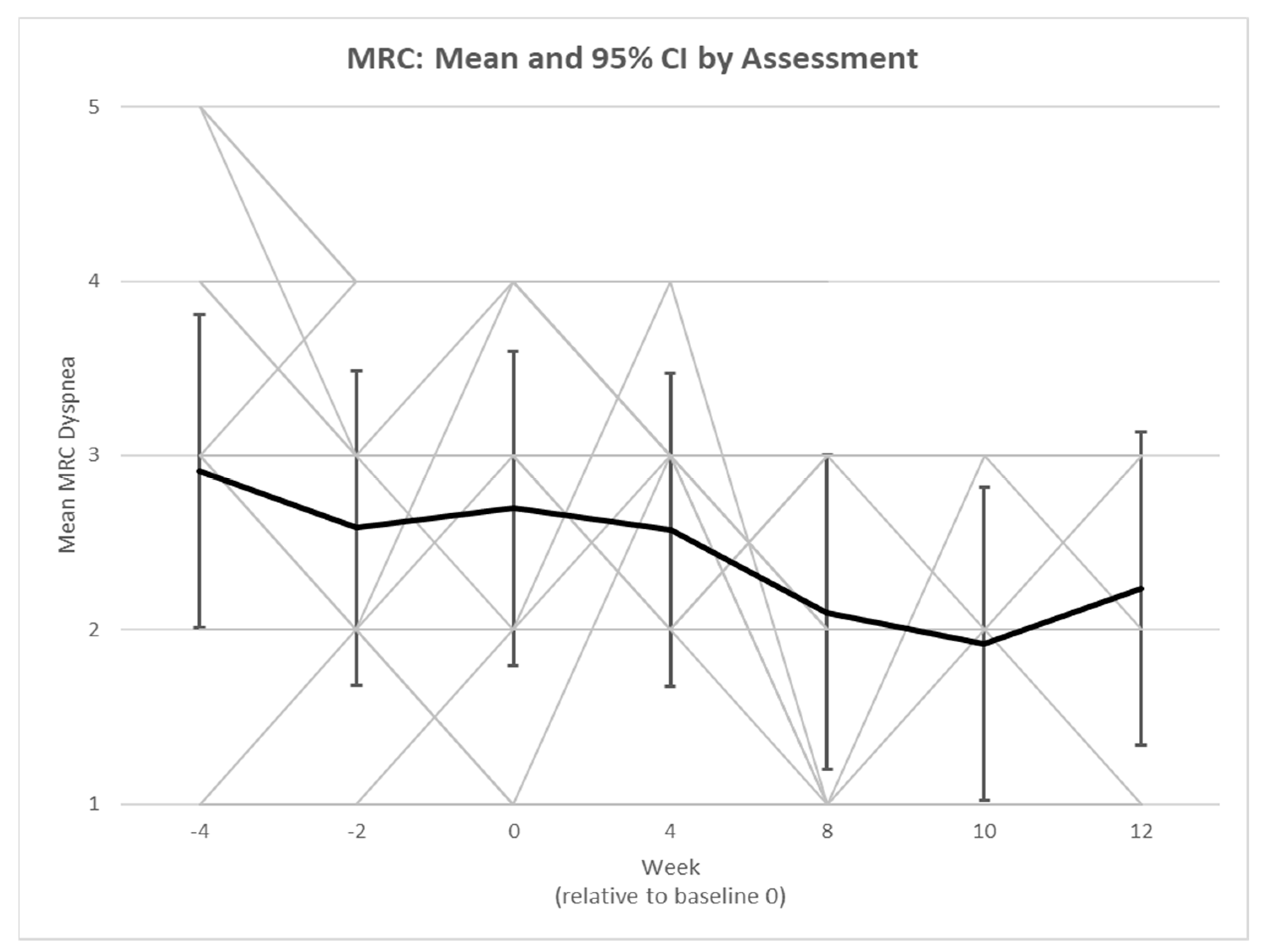
3. Results
3.1. Demographics
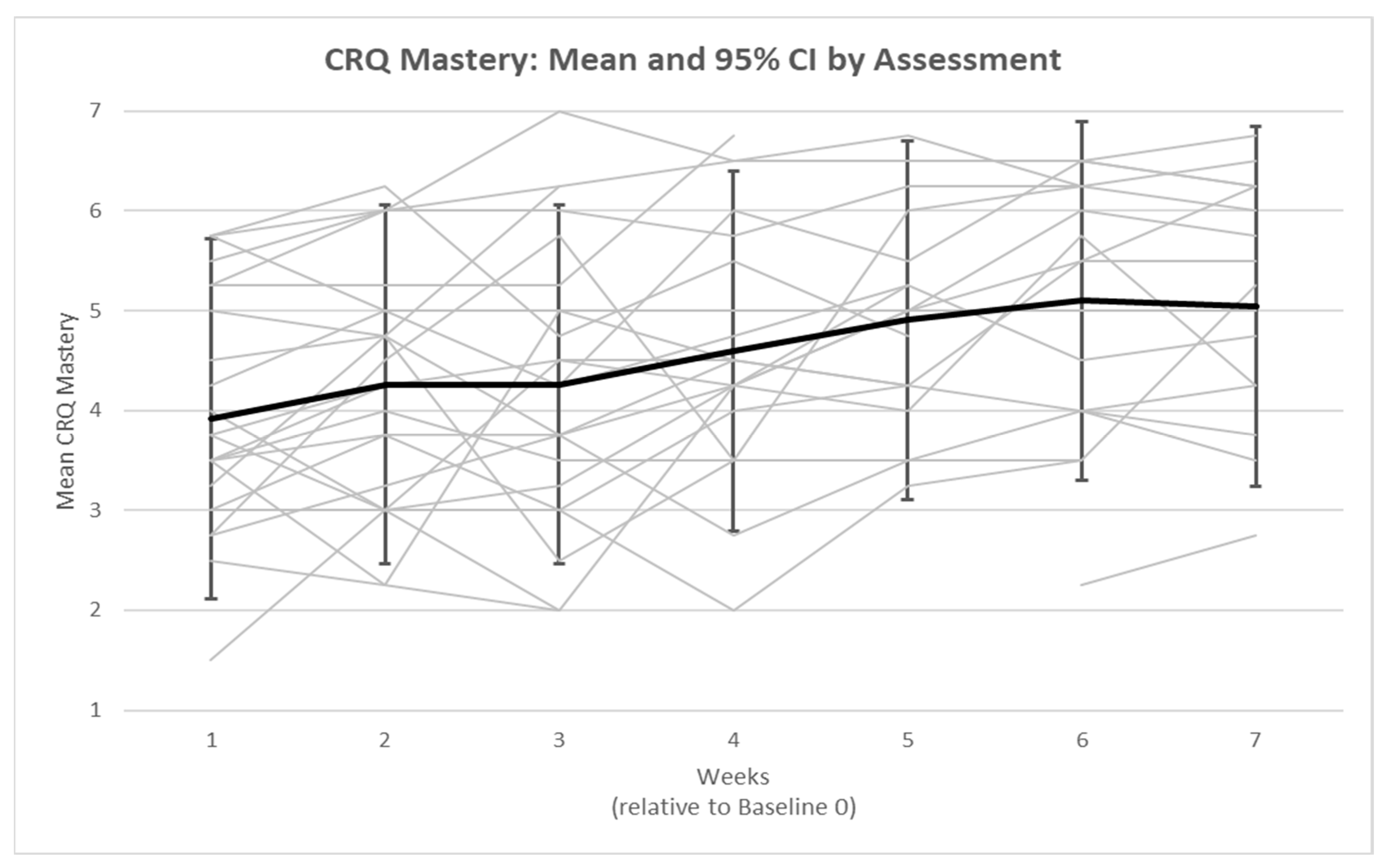
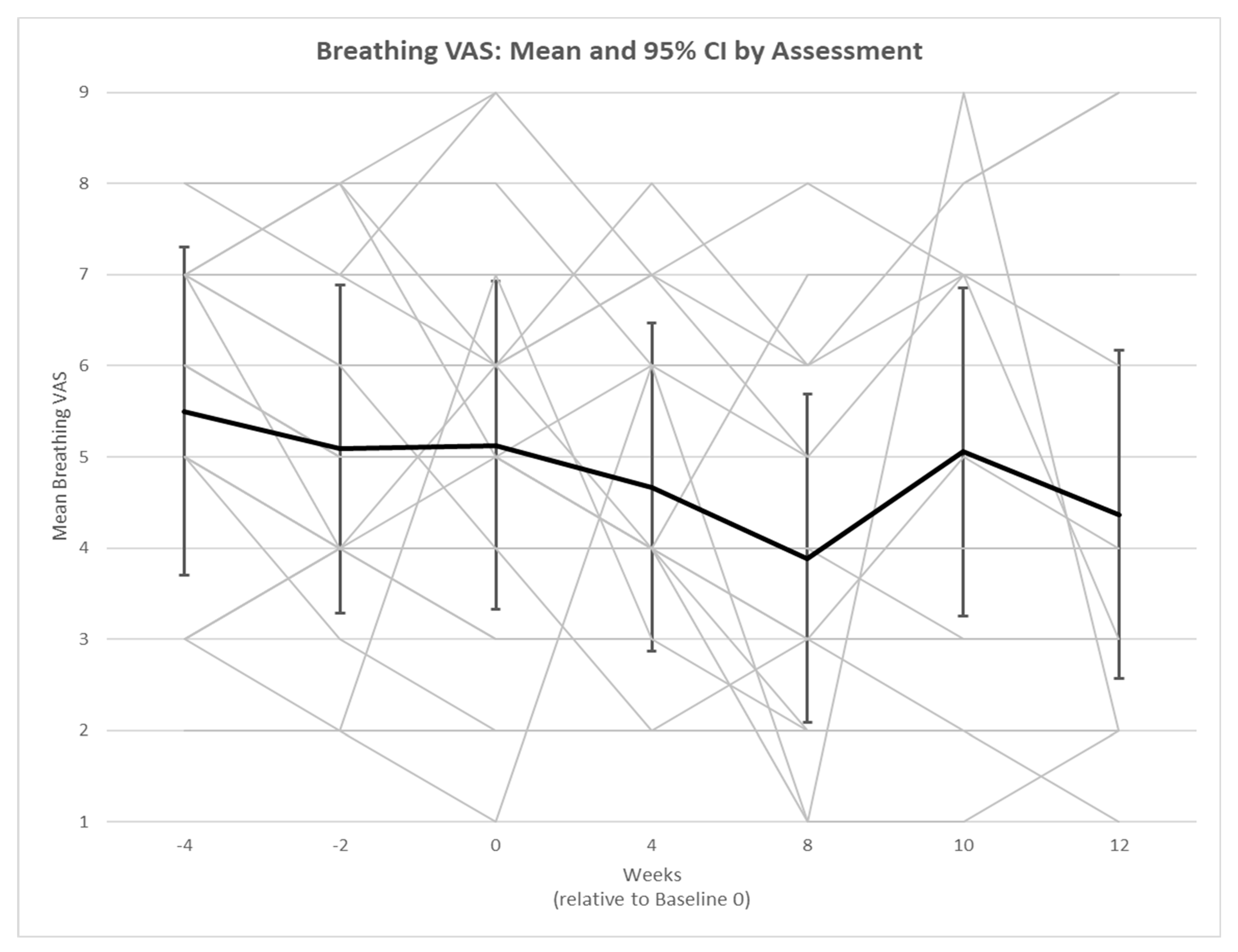
3.2. Secondary Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Number of COVID-19 Cases Reported to WHO. Updated 31 March 2024. Available online: https://data.who.int/dashboards/covid19/cases?n=c (accessed on 17 April 2024).
- Nearly One in Five American Adults Who Have Had COVID-19 Still Have “Long COVID”. Updated 22 June 2022. Available online: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/20220622.htm (accessed on 1 November 2023).
- Lambert, N.J.; Survivor Corps. COVID-19 “Long Hauler” Symptoms Survey Report; Indiana University School of Medicine: Indianapolis, IN, USA, 2020. [Google Scholar]
- Oronsky, B.; Larson, C.; Hammond, T.C.; Oronsky, A.; Kesari, S.; Lybeck, M.; Reid, T.R. A Review of Persistent Post-COVID Syndrome (PPCS). Clin. Rev. Allergy Immunol. 2023, 64, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Vance, H.; Maslach, A.; Stoneman, E.; Harmes, K.; Ransom, A.; Seagly, K.; Furst, W. Addressing Post-COVID Symptoms: A Guide for Primary Care Physicians. J. Am. Board. Fam. Med. 2021, 34, 1229–1242. [Google Scholar] [CrossRef] [PubMed]
- Bradt, J.; Dileo, C. Music interventions for mechanically ventilated patients. Cochrane Database Syst. Rev. 2014, 2014, CD006902. [Google Scholar] [CrossRef] [PubMed]
- Sliwka, A.; Wloch, T.; Tynor, D.; Nowobilski, R. Do asthmatics benefit from music therapy? A systematic review. Complement. Ther. Med. 2014, 22, 756–766. [Google Scholar] [CrossRef] [PubMed]
- Loewy, J.; Goldsmith, C.; Deshpande, S.; Sun, A.; Harris, J.; van Es, C.; Zvi, Z.B.; Dahmer, S. Music therapy in pediatric asthma improves pulmonary function while reducing hospitalizations. J. Asthma. 2021, 58, 674–682. [Google Scholar] [CrossRef]
- Canga, B.; Azoulay, R.; Raskin, J.; Loewy, J. AIR: Advances in Respiration—Music therapy in the treatment of chronic pulmonary disease. Respir. Med. 2015, 109, 1532–1539. [Google Scholar] [CrossRef]
- McNaughton, A.; Weatherall, M.; Williams, M.; McNaughton, H.; Aldington, S.; Williams, G.; Beasley, R. Sing Your Lungs Out-a community singing group for chronic obstructive pulmonary disease: A 1-year pilot study. BMJ Open 2017, 7, e014151. [Google Scholar] [CrossRef]
- Hart, M.K.; Stewardson, E.; Jamil, A.K.; Tecson, K.M.; Millard, M.W. Usefulness of harmonica playing to improve outcomes in patients with chronic obstructive pulmonary disease. Bayl. Univ. Med. Cent. Proc. 2020, 33, 178–182. [Google Scholar] [CrossRef]
- Cahalan, R.M.; Meade, C.; Mockler, S. SingStrong—A singing and breathing retraining intervention for respiratory and other common symptoms of long COVID: A pilot study. Can. J. Respir. Ther. 2022, 58, 20–27. [Google Scholar] [CrossRef]
- Philip, K.E.J.; Owles, H.; McVey, S.; Pagnuco, T.; Bruce, K.; Brunjes, H.; Banya, W.; Mollica, J.; Lound, A.; Zumpe, S.; et al. An online breathing and wellbeing programme (ENO Breathe) for people with persistent symptoms following COVID-19: A parallel-group, single-blind, randomised controlled trial. Lancet Respir. Med. 2022, 10, 851–862. [Google Scholar] [CrossRef]
- Tuttle, S. After Covid, Playing Trumpet Taught Me How to Breathe Again. New York Times. 29 November 2022. Available online: https://www.nytimes.com/2022/11/29/magazine/community-band.html (accessed on 1 November 2023).
- Bell, B. Musical Instrument Therapy to Treat Long-term Effects of COVID on Long Island. ABC 7. 30 July 2021. Available online: https://abc7ny.com/music-therapy-musical-instrument-covid-effects-long-term/10919127/ (accessed on 1 November 2023).
- American Music Therapy Association. AMTA Official Definition of Music Therapy. Updated 2005. Available online: https://www.musictherapy.org/about/musictherapy/ (accessed on 1 November 2023).
- Loewy, J. Underlying Music Mechanisms Influencing the Neurology of Pain: An Integrative Model. Brain Sci. 2022, 12, 1317. [Google Scholar] [CrossRef]
- Mahler, D.A.; Wells, C.K. Evaluation of clinical methods for rating dyspnea. Chest 1988, 93, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.E.; Singh, S.J.; Sewell, L.; Guyatt, G.H.; Morgan, M.D. Development of a self-reported Chronic Respiratory Questionnaire (CRQ-SR). Thorax 2001, 56, 954–959. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.C.; Jones, P.W. A comparison of the visual analogue scale and modified Borg scale for the measurement of dyspnea during exercise. Clin. Sci. 1989, 76, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Rial, W.Y.; Rickels, K. Short form of depression inventory: Cross-validation. Psychol. Rep. 1974, 34, 1184–1186. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Krupp, L.B.; LaRocca, N.G.; Muir-Nash, J.; Steinberg, A.D. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, L.P.; Orton, C.M.; Watson, N.A.; Gregson, F.K.A.; Haddrell, A.E.; Browne, W.J.; Calder, J.D.; Costello, D.; Reid, J.P.; Shah, P.L.; et al. Aerosol and droplet generation from performing with woodwind and brass instruments. Aerosol. Sci. Technol. 2021, 55, 1277–1287. [Google Scholar] [CrossRef]
- Pearlin, L.I.; Schooler, C. The structure of coping. J. Health Soc. Behav. 1978, 19, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Insights on COVID-19: The Impact of the Pandemic on Mental Health. Updated 2 August 2023. Available online: https://www150.statcan.gc.ca/n1/pub/82-003-x/2025004/article/00002-eng.htm (accessed on 1 November 2023).
| Variable | Number | Percentage (%) |
|---|---|---|
| Gender | ||
| Female | 17 | 70.8 |
| Male | 5 | 20.8 |
| Not reported | 2 | 8.4 |
| Age | ||
| Mean (SD), Range | 45.9 (13.6), 22–70 | |
| Race | ||
| Asian | 1 | 4.2 |
| Black or African American | 5 | 20.8 |
| White | 13 | 54.2 |
| More Than One Race | 1 | 4.2 |
| Not Reported | 4 | 16.6 |
| Mean Difference | p-Value | Cohen’s d | Confidence Intervals | |
|---|---|---|---|---|
| CRQ Dyspnea | 0.02 | 0.95 | 0.042 | [−0.57, 0.61] |
| CRQ Fatigue | 0.26 | 0.16 | −0.449 | [−0.11, 0.64] |
| CRQ Emotion | 0.03 | 0.88 | −0.023 | [−0.37, 0.42] |
| CRQ Mastery | 0.60 * | 0.01 | −0.602 | [0.17, 1.02] |
| Breathing VAS | −1.15 * | 0.01 | 0.625 | [−1.97, −0.33] |
| BDI-SF | −0.50 | 0.17 | 0.290 | [−1.22, 0.22] |
| GAD-7 | −0.09 | 0.90 | 0.087 | [−1.57, 1.38] |
| HADS Anxiety | −0.32 | 0.61 | 0.146 | [−1.60, 0.95] |
| HADS Depression | −0.29 | 0.61 | 0.095 | [−1.43, 0.86] |
| FSS Total | −3.55 | 0.29 | 0.490 | [−10.30, 3.20] |
| ESS | −1.24 | 0.11 | 0.419 | [−2.79, 0.30] |
| Eq_5d_5l | 4.90 | 0.19 | −0.282 | [−2.48, 12.27] |
| CDRISC Total | 1.67 | 0.35 | −0.243 | [−1.91, 5.25] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.; Loewy, J.V.; Spielman, L.; Chen, Z.; Raskin, J.M. The Feasibility of a Music Therapy Respiratory Telehealth Protocol on Long COVID Respiratory Symptoms. COVID 2025, 5, 107. https://doi.org/10.3390/covid5070107
Zhang J, Loewy JV, Spielman L, Chen Z, Raskin JM. The Feasibility of a Music Therapy Respiratory Telehealth Protocol on Long COVID Respiratory Symptoms. COVID. 2025; 5(7):107. https://doi.org/10.3390/covid5070107
Chicago/Turabian StyleZhang, Jingwen, Joanne V. Loewy, Lisa Spielman, Zijian Chen, and Jonathan M. Raskin. 2025. "The Feasibility of a Music Therapy Respiratory Telehealth Protocol on Long COVID Respiratory Symptoms" COVID 5, no. 7: 107. https://doi.org/10.3390/covid5070107
APA StyleZhang, J., Loewy, J. V., Spielman, L., Chen, Z., & Raskin, J. M. (2025). The Feasibility of a Music Therapy Respiratory Telehealth Protocol on Long COVID Respiratory Symptoms. COVID, 5(7), 107. https://doi.org/10.3390/covid5070107





